Abstract
Primary hyperaldosteronism, or Conn’s syndrome, is a disorder of excessive secretion of aldosterone from the adrenal gland(s). The aldosterone excess results in sodium retention, volume expansion, and hypertension. Complications from long-standing disease include hypokalemia, arrhythmias, heart attack, and stroke.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Algorithmic Approach
-
A.
Primary hyperaldosteronism is the most common cause of secondary hypertension and should be suspected in patients with hypertension that is diagnosed earlier than age 35, severe (BP < 160/100), persistent despite >3 medications, and present along with hypokalemia and/or an adrenal incidentaloma [1].
-
B.
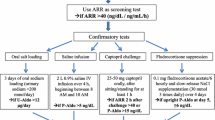
The first diagnostic assessment in patients with Conn’s syndrome requires demonstration of aldosterone excess along with suppressed plasma renin activity. Before measuring serum aldosterone levels and plasma renin activity, medications that can affect these measurements (e.g., angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, aldosterone receptor antagonists, and beta-blockers) are replaced with others (e.g., calcium channel blockers or alpha-adrenergic blockers) for several weeks. The aldosterone-to-renin ratio (ARR) is then calculated, with a ratio >20–40:1 along with an aldosterone level >15 ng/dL being suggestive of primary hyperaldosteronism (furthermore, an ARR >35 is 100% sensitive and 92% specific). If the ARR is equivocal but the diagnosis is still suspected, confirmatory testing may be performed (e.g., oral sodium loading, saline infusion, or captopril challenge testing) [1, 2].
-
C.
After establishing the diagnosis of hyperaldosteronism by biochemical studies, the next step is localizing the production to either a unilateral adenoma or bilateral hyperplasia. The imaging modality of choice is an “adrenal protocol” thin-cut computed tomography (CT) scan, which can demonstrate normal adrenal glands, thickened glands, or a unilateral adrenal mass [3]. An aldosterone-producing adenoma should be suspected in younger patients with hypertension whose CT scan reveals a unilateral adrenal mass and a contralateral normal adrenal gland.
-
D.
The laterality of aldosterone hypersecretion is then confirmed by bilateral adrenal venous sampling (AVS), which is the gold standard for distinguishing between unilateral and bilateral disease. The acquisition of AVS in every patient with primary hyperaldosteronism is controversial; however, many centers perform this routinely. Reliance on CT findings alone is questionable for two reasons: (1) aldosteronomas are typically small and may be missed (false negatives) and (2) non-aldosterone-secreting/nonfunctional adrenal adenomas increase with age (false positives). During AVS, aldosterone levels are obtained from the SVC, IVC, and adrenal veins. Cortisol levels are also obtained, with an adrenal vein to IVC cortisol ratio >2:1 confirming successful cannulation of the adrenal veins. The aldosterone-to-cortisol ratio between both adrenal veins is then compared. A ratio of more than 4:1 lateralizes unilateral hypersecretion and identifies the gland to be removed [4, 5].
-
E.
Hyperaldosteronism is typically cured by laparoscopic adrenalectomy ; however, blood pressure may remain elevated secondary to the vascular damage caused by the prior long-standing, severe hypertension. Factors predictive of the resolution of hypertension include female sex, body mass index (BMI) ≤25, hypertension lasting ≤6 years, prescription of ≤2 antihypertensive medications, and decline in plasma aldosterone by 10 ng/dL on postoperative day 1 [6, 7].

Algorithm 111.1
References
Harvey AM. Hyperaldosteronism: diagnosis, lateralization, and treatment. Surg Clinic N Am. 2014;94(3):643–56.
Yin G, Zhang S, Yan L, et al. One-hour upright posture is an ideal position for serum aldosterone concentration and plasma renin activity measuring on primary aldosteronism screening. Exp Clin Endocrinol Diabetes. 2012;120(7):388–94.
Bobanga ID, McHenry CR. Chapter 6. Imaging modalities for adrenal cortical tumors. In: Kebebew E, editor. Management of adrenal masses in children and adults. 1st ed. Switzerland: Springer; 2017.
Zeiger MA, Thompson GB, Duh Q-Y, Hamrahian AH, Angelos P, Elaraj D, et al. American Association of Clinical Endocrinologists and American Association of Endocrine Surgeons medical guidelines for the management of adrenal incidentalomas. Endocr Pract. 2009;15(Suppl 1):1–20.
Chao CT, Wu VC, Kuo CC, Lin YH, Chang CC, Chueh SJ, et al. Diagnosis and management of primary aldosteronism: an updated review. Ann Med. 2013;45(4):375–83.
Aranova A, Gordon BL, Finnerty BM, Zarnegar R, Fahey TJ. Aldosterone resolution score predicts long-term resolution of hypertension. Surgery. 2014;156(6):1387–92.
Swearingen AJ, Kahramangil B, Monteiro R, Krishnamurthy VD, Jin J, Shin JJ, et al. Analysis of postoperative biochemical values and clinical outcomes after adrenalectomy for primary aldosteronism. Surgery. 2017. https://doi.org/10.1016/j.surg.2017.10.045.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Bobanga, I., Bénay, C., Krishnamurthy, V.D. (2019). Primary Hyperaldosteronism (Conn’s Syndrome). In: Docimo Jr., S., Pauli, E. (eds) Clinical Algorithms in General Surgery . Springer, Cham. https://doi.org/10.1007/978-3-319-98497-1_111
Download citation
DOI: https://doi.org/10.1007/978-3-319-98497-1_111
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-98496-4
Online ISBN: 978-3-319-98497-1
eBook Packages: MedicineMedicine (R0)