Abstract
En bloc resection is a surgical procedure aiming to remove a tumor mass in its entirety, fully covered by a continuous shell of healthy tissue. Oncological indications for this procedure are aggressive benign tumors (Enneking stage 3), like osteoblastoma and giant-cell tumor, and low-grade malignant tumors (Enneking stage IA and B), like chordoma and chondrosarcoma. In high-grade malignant tumors like osteosarcoma and Ewing sarcoma, en bloc resection must be combined with protocols of chemotherapy and radiotherapy (RT) in a multidisciplinary approach. En bloc resection can be an option in selected single metastases originating from tumors resistant to chemotherapy and radiation protocols, once the criteria of feasibility are fulfilled without functional sacrifices. The criteria of feasibility of tumor-free margins in the lumbar spine include one pedicle free from tumor and a part of the posterior arch allowing room to release the thecal sac. The Weinstein-Boriani-Biagini (WBB) staging system can be helpful in providing standardized strategies according to tumor extension and location. A strong consideration of the role of margins in the local and systemic prognosis can include in the en bloc resection even relevant anatomical structures (nerve roots, dura, arteries, and veins) when they are infiltrated by the tumor or are running along the tumor margins.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Spine tumor
- Lumbar spine
- En bloc resection
- Spondylectomy
- Surgical technique
- WBB staging system
- Enneking staging system
Introduction
The Enneking staging system [1] is a valid and reproducible tool for understanding and staging the biological behavior of bone and soft tissue tumors and for deciding the appropriate surgical procedure from an oncological point of view. This system is based on histological diagnosis and on clinical, laboratory, and imaging studies. One of the most relevant issues is also proposing a common terminology to the multidisciplinary team who take care of these diseases. Throughout this chapter, we make reference to Enneking’s oncological terminology.
En bloc resection can be defined as a surgical procedure aiming to remove a tumoral mass in its entirety, fully covered by a continuous shell of healthy tissue. This shell is called “margin” and qualifies the procedure from an oncological point of view, affecting the local and systemic prognosis [2, 3]. This procedure became the golden standard in the treatment of bone tumors of the limbs in the 1970s, after the introduction of the protocols of neo-adjuvant chemotherapy . The effects of these new drugs on the tumoral mass (volume reduction, harder consistency) allowed development of techniques of surgical resection of the tumor without sacrificing the limb (so-called “limb salvage procedures”) [4].
The problems to be faced in planning to perform in the spine a procedure fulfilling the same oncological criteria are included in the definition. Spinal cord, cauda equina, nerve roots, aorta, cava, vertebral artery, and so on can run inside the tumor margin or be involved by the tumor. These anatomical constraints can prevent a tumor-free margin en bloc resection, unless relevant sacrifices are accepted and important structures representing the margins are resected in the same specimen (Fig. 21.1).
Further, it should be considered that the epidural space is continuous from the foramen magnum to the sacrum, thus preventing not only a “radical” resection according to Enneking’s terminology [4] (defined as en bloc removal of the tumor together with the whole compartment of origin) but even a difficult evaluation of the margins if the tumor encroaches the canal (Fig. 21.2).
Indications and Margins
En bloc resection is recommended in cases of benign aggressive (Enneking stage 3) tumors (i.e., osteoblastomas and giant-cell tumors) and low-grade malignant tumors (Enneking stage IA and B) like chordomas and chondrosarcomas. In high-grade malignancies (Enneking stage II) like osteosarcoma and Ewing sarcoma, chemotherapy and radiotherapy (RT) have a very relevant and essential role.
Once the resection is performed, the pathologist must carefully evaluate the tumor margins [2, 5], defined as “wide” (a relevant barrier like a fascia or at least healthy bone 1-cm thick), “marginal” (a thin barrier like periosteum), or “intralesional”.
“Intralesional” resection is defined as when the surgeon incidentally or intentionally violates the tumor. Violation of the margins significantly worsens the prognosis [6]. Intentional intralesional resection may be an option when obtaining a surgical margin requires resection of functionally relevant tissue that is closely contiguous to the tumor or has been infiltrated by the tumor [7].
In cases where the tumor is growing in the epidural space, one may consider resecting the dura together with the tumor to achieve a tumor-free margin resection [8]. Dura covering the scar is only expected when the epidural space is occupied by scar, a frequent finding in cases of tumor recurrence. A cost-benefit assessment is required in situations where diagnosis and staging indicate the need for a wide margin that includes a structure such as a nerve root, whose sacrifice will result in functional or neurological compromise. The patient must be fully informed regarding the expected functional loss as well as the risk of recurrence with intentional intralesional resection. Specific techniques of en bloc resection have been published with the sacrifice of these structures: dura [8], cervical nerve roots [9, 10], cauda equina [11], spinal cord [12], major vascular structures, and visceral organs [13].
In addition, the decision-making process should also consider that the rates of complications and tumor recurrence are significantly higher for revision surgery [14, 15]. If the patient opts for preservation of the critical structure, adjuvant therapy is indicated. In patients with spinal metastases, surgery may be indicated in cases where tumors are resistant to radiation-based treatment and/or chemotherapy or there is current or impending risk of spinal instability or cord compression [16, 17]. En bloc resection with the primary goal of achieving complete local control should only be performed in selected cases of spinal metastases [18, 19]. The primary goal in these patients is to preserve or improve function and quality of life without unnecessary morbidity; thus, in principle, no functionally significant nerve root, for example, should be sacrificed when resecting a metastasis. In the authors’ experience, the indication to en bloc resection is appropriate in single localizations, with full tumor control at the primary site and no involvement of visceral organs, best after long-term, disease-free evolution [20]. The key point in this decision is the lack of sensitivity to medical oncology or radiation oncology treatments; alternatively, less aggressive surgery could be combined with these treatments, reducing the surgical morbidity without reducing the possibility to local cure.
Surgical Planning
Surgical planning of en bloc resection in the spine, as in any other skeletal location, should be decided on a case-by-case basis, related to the tumor extension and to the need of margin appropriate to the tumor aggressiveness. Bertil Stener was the first to apply to the spine the oncologic principles generally accepted for gastrointestinal tumors [21, 22]. His detailed reports of the surgical planning of en bloc resections are still an extremely useful and exhaustive guide to this procedure.
Conversely, Roy-Camille [23] and Tomita [24] popularized the techniques of en bloc resection by posterior approach without a specific concern on tumor extension and margin fulfilling. The Weinstein-Boriani-Biagini (WBB) surgical system for staging extensions of primary bone tumors of the spine (Fig. 21.3) was proposed in 1997 [25], adopted in several spine oncology centers and subjected to clinical evaluations [26]. More recently, the WBB system has been submitted to a study of reliability and validity by an international multidisciplinary group of spine tumor experts [27], resulting in a moderate interobserver reliability and substantial intraobserver reliability. The WBB staging system [25] focuses on the extent and location of the tumor. In the transverse plane, the vertebra is divided into 12 radiating zones (numbered 1 to 12 in an anti-clockwise order) and into five layers from the prevertebral to the dural involvement (A to E). The longitudinal extent of the tumor is recorded by identifying the specific vertebrae involved. This system allows for a more rational approach to the surgical planning, provided that all efforts are made to perform surgery along the required margins.
WBB surgical staging system . In the transverse (axial) plane, the vertebra is divided into 12 radiating zones (numbered 1 to 12 in a counterclockwise order) and 5 layers ((a) extracompartmental peripheral tumor; (b) outer intracompartmental tumor; (c) inner intracompartmental tumor; (d) tumor inside the epidural space; (e) intradural tumor)
The WBB staging system [25] can be helpful in standardizing the surgical planning of en bloc resection according to the region of the spine and the tumor extent and location. The great variability of these two parameters dictates that the same surgical procedure as proposed by Roy-Camille [23] and Tomita [24] cannot be performed in all cases and that surgical planning is usually different for each case [28].
The WBB-guided planning of en bloc resection for spine tumors identifies 7 types of procedures, with several subgroups, ending in a total of 10 different surgical strategies. The types are defined by the approach or the combination of approaches: single anterior approach (type 1); single posterior approach (type 2) including three subtypes (a, b, c); anterior and then posterior approach (type 3) with three subtypes (a, b, c); first posterior approach, followed by both side anterior approaches (type 4); first posterior approach and then simultaneous anterior and re-opening of posterior approach (type 5); anterior, posterior, and then simultaneous anterior (contralateral) and re-opening of posterior approach (type 6, mostly performed for L5); and posterior approach as the first step and anterior approach as the second step (type 7, Fig. 21.4).
En bloc lumbar spondylectomy with posterior decompression and anterior tumor resection. (Reprinted with permission from Marmor et al. [41])
Type 1
The single anterior approach (Fig. 21.5) allows one to perform en bloc resection only of small tumors of the thoracic and lumbar vertebral bodies. These must be enclosed inside sectors 8–5, arising from layer A and B but not extending to layer C. In this case, in fact, a posterior approach is required to provide an appropriate margin under direct visual control by entering the canal and releasing the dura. This approach involves three steps. First, provide the appropriate margin over the anterior tumor growth by releasing the anterior structures from the tumor pseudocapsule or leaving the selected anatomical structures as margin (I). These are also the cases of direct bone invasion by contiguous tumor. Second, perform an osteotomy between the tumor and the posterior wall (II). Third, finalize the en bloc resection (III).
Type 1 WBB-based en bloc resection . A single anterior approach allows one to perform en bloc resection of small tumors of the thoracic and lumbar vertebral bodies. These must be enclosed inside sectors 5–8, arising from layers A and B, without extension into layer C. In this case, a posterior approach is required to provide an appropriate margin, under direct visual control by entering the canal and releasing the dura. There are three steps: first, provide the appropriate margin over the growing anterior tumor by releasing the anterior structures from the tumor pseudocapsule (I); these are also the cases of direct bone invasion by contiguous tumor. Second, perform an osteotomy between the tumor and the posterior wall (II). Third, finalize the en bloc resection with removal of the tumor (III)
Type 2
The single posterior approach allows one to perform many different en bloc resections on tumors occurring in the posterior elements, either in the vertebral body or eccentrically located.
Type 2a
The single posterior approach is the obvious strategy to remove by en bloc resection a tumor arising in the posterior arch (Fig. 21.6a) in the cervical, thoracic, and lumbar spine. Criteria to achieve appropriate margins include sector 9 and 4 free from tumor. If the tumor grows in layer D, the margin will become intralesional during the release from the dura. This approach involves three steps: first, provide the appropriate margin over the tumor posteriorly growing by resecting inside the posterior muscles covering the tumor mass if it is expanding in layer A (I). The second step includes piecemeal excision of sectors 9 and 4 or osteotomy by wire saw or chisel or high-speed burr or ultrasound osteotome (II). This is obviously particularly delicate in the cervical spine, with higher risk of incidental violation of the margins. Once a transverse laminotomy is performed above and below, the tumor is released from the dura and the specimen is resected en bloc (III).
(a) Type 2a WBB-based en bloc resection. Single posterior approach is the best strategy to facilitate en bloc resection of a tumor arising from the posterior arch. Criteria to achieve an appropriate margin include sector 9 and 4 free from tumor. If the tumor grows in layer D, the margin will become intralesional during the release from the dura. There are three steps: first, provide the appropriate margin over the tumor growing posteriorly by resecting inside the posterior muscles covering the tumor mass if it is expanding in layer A (I); second, piecemeal excision of sectors 9 and 4 or osteotomy by wire saw, chisel, high-speed burr, or ultrasound osteotome (II). After performing a transverse laminotomy above and below, the tumor is released from the dura and the specimen is resected en bloc (III). (b) Type 2b WBB-based en bloc resection, single posterior approach. It allows removal by en bloc resection of a tumor arising in the vertebral body of a thoracic vertebra. Criteria to achieve appropriate margins include sector 9 or 4 free from tumor. If the tumor grows in layer D, the margin will become intralesional during the release from the dura. If the tumor grows in layer A, the margin will become intralesional during the release from the anterior structures. There are two steps. The first includes piecemeal excision of the posterior arch not involved by the tumor. At least four sectors are required, starting from sector 4 or from sector 9(I). Release from the dura and section of the nerve root(s) involved by the tumor. Second, blunt dissection of the anterior part of the vertebral body from the mediastinum, osteotomy, or discectomy above and below the tumor, full release from the dura, and finalizing the resection (II). (c) Type 2c WBB-based en bloc resection. Single posterior approach with sagittal osteotomy. A tumor eccentrically growing in thoracic or lumbar spine (Fig. 21.9) can be removed en bloc by single posterior approach, provided the body is not involved over sector 5 at left and over sector 8 at right. At least three sectors posteriorly must not be involved by the tumor (from 4 to 1–2 or from 12–11 to 9). There are four steps: first, provide appropriate margin over the tumor posteriorly growing by resecting inside the posterior muscles covering the tumor mass if it is expanding in layer A (I). The release will proceed laterally until the lateral side of the vertebral body. In the thoracic spine (Fig. 21.7), the pleura can be left on the tumor; in the lumbar spine (Fig. 21.9), the posterior part of the psoas must be dissected but the segmental vessels must be found and ligated. The second step is piecemeal excision of the posterior arch not involved by the tumor. Approach the canal, release the dura from the tumor (if the tumor grows in layer D, the margin will become intralesional), and section the nerve root(s) involved by the tumor. The third step includes carefully displacing the dura and performing an osteotomy from posterior to anterior in sector 8 or 5. The specimen is finally removed (IV)
Type 2b
The single posterior approach with different surgical sequences allows removal by en bloc resection of a tumor arising in the vertebral body of a thoracic vertebra (Fig. 21.6b). Criteria to achieve an appropriate margin include sector 9 or 4 free from tumor. If the tumor grows in layer D, the margin will become intralesional during the release from the dura. If the tumor grows in layer A, the margin will become intralesional during the release from the anterior structures. This is the most popular technique of en bloc resection of a spine tumor, described by Roy-Camille [23] and later by Tomita [24]. This technique involves two steps: first, piecemeal excision of the posterior arch not involved by the tumor. At least four sectors are required, starting from sector 4 or from sector 9 (I). Release from the dura and section the nerve root(s) involved by the tumor. Second, blunt dissection of the anterior part of the vertebral body from the mediastinum, osteotomy, or discectomy above and below the tumor, full release from the dura, and finalizing the resection (II). The same technique described in Fig. 21.6b is difficult to apply to lumbar vertebrae. Digital blunt dissection of the anterior circumference is demanding or impossible due to the psoas muscle, the dimension of the vertebral body, and the major vessels kept closely connected to the spine by the transverse segmental vessels running between vertebral body and psoas. In these cases, the approaches defined as types 3b and c (Fig. 21.7b, c) and 5 (Fig. 21.9) or 7 (see Fig. 21.11) seem more appropriate and safe.
(a) Type 3a WBB-based en bloc resection . When the tumor is growing anteriorly (layer A), an anterior approach must be performed as a first step to provide a wide/marginal margin under visual control. In tumors mostly occupying the vertebral body, the anterior approach can be the first step to release from mediastinum or retroperitoneal, eventually leaving involved structures as margin (I). A sheet of silastic or similar material can be left as protection. The second stage, posterior approach, involves piecemeal excision of the posterior arch not involved by the tumor (II). At least three to four sectors are required, starting from sector 4 or from sector 9. Release the dura from the tumor, section the nerve root(s) involved by the tumor, then provide the appropriate margin over the posteriorly growing tumor by resecting inside the posterior muscles covering the tumor mass if it is expanding in layer A (III). Finally, the specimen is removed by rotating around the dural sac (IV). (b) Type 3b WBB-based en bloc resection. In the cervical spine, three approaches can be required: posterior, anterior contralateral to the tumor side, and anterior on the tumor side. The combined simultaneous second and third approaches are required if the tumor is particularly huge, extending over the midline
The first step is in the prone position and involves piecemeal excision of the posterior arch not involved by the tumor. At least three sectors are required, starting from sector 4 or from sector 9(I). In case of tumor growing posteriorly and invading layer A, an appropriate margin must be provided by resecting inside the posterior muscles covering the tumor mass (II). Then release the dura from the tumor (if the tumor grows in layer D, the margin will become intralesional) and section the nerve root(s) crossing the tumor. The second and third steps are in supine position. In the second stage, a sagittal groove is performed in the vertebral body not occupied by the tumor (III), until the vertebral artery, which must be saved, as the other is involved by the tumor and must be sacrificed. The anterior margin is provided by leaving healthy soft tissue over the tumor mass (IV). Discectomies or transversal grooves in vertebral bodies are performed to define the upper and lower margins. The tumor is finally removed by the third approach (V) on finalizing the upper and lower discectomies or osteotomies, including ligation of the vertebral artery.
Type 2c
The single posterior approach with sagittal osteotomy is illustrated above (Fig. 21.6c). A tumor eccentrically growing in thoracic and lumbar spine can be removed en bloc by the single posterior approach (type 2c), provided the body is not involved over sector 5 at left and over sector 8 at right. At least three sectors posteriorly must be not involved by the tumor (from 4 to 1–2 or from 12–11 to 9). This approach involves four steps. First provide appropriate margin over the tumor posteriorly growing by resecting inside the posterior muscles covering the tumor mass if it is expanding in layer A (I). The release will proceed laterally until one reaches the lateral side of the vertebral body. In the thoracic spine, the pleura can be left on the tumor; in the lumbar spine, the posterior part of the psoas must be dissected, and the segmental vessels must be found and ligated. The second step is piecemeal excision of the posterior arch not involved by the tumor. It involves approach to the canal, release of the dura from the tumor (if the tumor grows in layer D, the margin will be intralesional), and section of the nerve root(s) involved by the tumor. The third step includes displacing the dura carefully and performing osteotomy from posterior to anterior in sector 8 or 5. The specimen is finally removed (IV).
Type 3a
Besides anterior approach first, posterior second should also be considered in cervical spine tumors partially occupying the vertebral body (not involving sector 6 and 7—otherwise type 4 is suggested) and the posterior arch (at least three sectors not involved) (Fig. 21.7a). The anterior approach is first performed to leave healthy tissue over the tumor growing in the lateral masses (I) and to perform a sagittal groove till the epidural space in the vertebral body (II).
Discectomies or transverse grooves in vertebral bodies are performed to define the upper and lower margins, including ligation of the vertebral artery. The second stage is a posterior approach. The third step provides appropriate margin over the tumor posteriorly growing by resecting inside the posterior muscles covering the tumor mass if it is expanding in layer A. The fourth step is a piecemeal excision of the posterior arch not involved by the tumor. At least three sectors are required, starting from sector 4 or from sector 9. This allows release of the dura from the tumor and section of the nerve root(s) involved by the tumor. Finally, the specimen is removed—once the upper and lower discectomies or osteotomies have been finalized—by rotating around the dural sac (V).
Type 3b
A sequential combination of two approaches (anterior first, posterior second) in the thoracic and in the lumbar spine is proposed (Fig. 21.7b) when the vertebral body tumor grows anteriorly in layer A; in this case, an anterior approach must be performed as the first step to provide a wide/marginal margin under visual control. In case of tumors mostly occupying the vertebral body, the anterior approach can be the first step to release from mediastinum in the thoracic spine or retroperitoneal in the lumbar spine, eventually leaving involved structures as margin (I). A sheet of silastic or similar can be left as protection. Second stage, posterior approach: piecemeal excision of the posterior arch not involved by the tumor (II). At least three to four sectors are required, starting from sector 4 or from sector 9. Release the dura from the tumor, section the nerve root(s) involved by the tumor, and then provide appropriate margin over the tumor posteriorly growing by resecting inside the posterior muscles covering the tumor mass if it is expanding in layer A (III). Finally, the specimen is removed by rotating around the dural sac (IV). This technique requires sectioning at least a nerve root in order to rotate the specimen around the thecal sac when removing from the posterior approach. If the nerve roots are not involved by the tumor and are functionally relevant, it is better to plan a type 5 resection (Fig. 21.8).
Type 4 WBB-based en bloc resection . This is completed in two stages, first posteriorly, followed by an anterior resection. In the posterior approach, the laminae and posterior elements are removed in a piecemeal fashion to remain clear of the tumor capsule. An appropriate margin is subsequently created by resection of the surrounding soft-tissue structures. In the anterior approach the contralateral anterior column structures are resected, and an appropriate margin is made circumferentially releasing the tumor from all surrounding soft-tissue structures and underlying dura. The tumor may then be delivered, en bloc, through the anterior exposure
Type 3c
The same sequence of approaches is followed: anterior first and posterior second in case of tumor eccentrically growing in the thoracic and lumbar spine (Fig. 21.7c) when sagittal osteotomy is considered safe for appropriate margin, without the need to remove the whole vertebral body. In the first step the anterior approach provides a wide/marginal margin under visual control, releasing from mediastinum in the thoracic spine or from peritoneal in the lumbar spine, eventually leaving involved structures as margin (I). Discectomies or transverse grooves in vertebral bodies are performed to define the upper and lower margins. A sheet of silastic or any other tissue can be left as protection, to be removed during the final tumor removal. Second stage, posterior approach: piecemeal excision of the posterior arch not involved by the tumor. At least three sectors are required, starting from sector 4 or from sector 9 (II). Then provide the appropriate margin over the tumor posteriorly growing by resecting inside the posterior muscles covering the tumor mass if it expands in layer A (III). Release of the dura from the tumor, section of the nerve roots crossing the tumor, and osteotomy posterior to anterior at some distance from the tumor in order to leave uninvolved bone as margin comprise step IV. The resected specimen can be finally removed (V) once the upper and lower discectomies or osteotomies are finalized.
Type 4
In some huge tumors of the cervical spine , extending over the midline, three approaches are required for a safe and oncologically appropriate surgery: first posterior; second anterior contralateral to the tumor side; and third anterior on the tumor side (Fig. 21.8). First step in the prone position: piecemeal excision of the posterior arch not involved by the tumor. At least three sectors are required, starting from sector 4 or from sector 9 (I). In case of tumor posteriorly growing, and invading layer A, an appropriate margin must be provided by resecting inside the posterior muscles covering the tumor mass (II). Then release the dura from the tumor (if the tumor grows in layer D, the margin will be intralesional) and section the nerve root(s) crossing the tumor. Second and third steps are in supine position, second stage. A sagittal grove is performed in the vertebral body not occupied by the tumor (III) till the vertebral artery, which must be saved, as the other is involved by the tumor and must be sacrificed. The anterior margin is provided by leaving healthy soft tissue over the tumor mass (IV). Discectomies or transverse grooves in vertebral bodies are performed to define the upper and lower margins [29, 30]. The tumor is finally removed by the third approach (V), once the upper and lower discectomies or osteotomies are finalized, including ligation of the vertebral artery.
Type 5
Two stages—posterior approach and contemporary anterior and posterior approaches (patient positioned on the side) —can be the most appropriate for lumbar tumors expanding anteriorly. This technique was described by Roy-Camille for lumbar tumors [31] and is associated with the highest rate of morbidity and complications [15]. As an advantage compared to Type 3a (Fig. 21.7b), no nerve roots are sacrificed if not involved by the tumor.
First steps in prone position: piecemeal excision of the posterior arch not involved by the tumor. At least three sectors are required, starting from sector 4 or from sector 9 (I) (Fig. 21.9). In case of tumor posteriorly growing, and invading layer A, an appropriate margin must be provided by resecting inside the posterior muscles covering the tumor mass (II). Then release the dura from the tumor (if the tumor grows in layer D, the margin will be intralesional) and section the nerve root(s) crossing the tumor. Discectomies or transversal grooves in vertebral bodies are performed to define the upper and lower margins. Second stage in lateral position includes antero-lateral approach (thoracotomy, thoraco-abdominal, retroperitoneal) and re-opening of the posterior approach. In order to provide appropriate margin over the tumor, it must remain covered by pleura or by psoas (III). Spiral wires are used to embolize the segmental arteries to make easier the release of the aorta on the contralateral side. On finalizing the upper and lower discectomies or osteotomies, the specimen is removed by combined maneuvers (IV).
Type 5 WBB-based en bloc resection . First steps in prone position: piecemeal excision of the posterior arch not involved by the tumor. At least three sectors are required, starting from sector 4 or from sector 9 (I). In a tumor posteriorly growing and invading layer A, an appropriate margin must be provided by resecting inside the posterior muscles covering the tumor mass (II). Then release the dura from the tumor (if the tumor grows in layer D, the margin will be intralesional) and section the nerve root(s) crossing the tumor. Discectomies or transversal grooves in vertebral bodies are performed to define the upper and lower margins. The Second stage is in lateral position. It includes antero-lateral approach (thoracotomy, thoraco-abdominal, retroperitoneal) and re-opening of the posterior approach. In order to provide appropriate margin over the tumor, it must remain covered by pleura or by psoas (III). Spiral wires are used to embolize the segmental arteries to ease the release of the aorta on the contralateral side. On finalizing the upper and lower discectomies or osteotomies, the specimen is removed by combined maneuvers (IV)
Type 6
Three approaches should be planned to resect a tumor of L5: first anterior on the contralateral side of the tumor; second posterior; and third contemporary anterior and posterior approaches (Fig. 21.10). The double anterior approach is required to safely release the aorta/cava bifurcation.
Type 6 WBB-based en bloc resection . To perform en bloc resection of a tumor of L5, a double anterior approach is mostly required to fully release the aorta/cava bifurcation. Our technique includes (1) anterior approach on the contralateral side of the tumor, (2) posterior approach, and (3) contemporary anterior and posterior approaches. The first step in supine position involves release of the aorta/cava bifurcation and partial discectomies or osteotomies to define upper and lower margins (I). The second stage in prone position involves piecemeal excision of the posterior arch not involved by the tumor. At least three sectors are required, starting from sector 4 or from sector 9 (II). In case of tumor growing posteriorly and invading layer A, an appropriate margin must be provided by resecting inside the posterior muscles covering the tumor mass (III). Then release the dura from the tumor (if the tumor grows in layer D, the margin will be intralesional) and section the nerve root(s) crossing the tumor. Discectomies or transverse grooves in vertebral bodies are performed. The third stage in lateral position involves a retroperitoneal approach and re-opening of the posterior approach. In step 4, provide appropriate margin over the tumor by leaving it covered by psoas. Then finalize the discectomies or transverse grooves in vertebral bodies to remove the specimen by the anterior approach (V)
First step in supine position: release the aorta/cava bifurcation and partial discectomies or osteotomies to define upper and lower margins (I). Second stage in prone position: piecemeal excision of the posterior arch not involved by the tumor. At least three sectors are required, starting from sector 4 or from sector 9 (II). In case of tumor posteriorly growing, and invading layer A, an appropriate margin must be provided by resecting inside the posterior muscles covering the tumor mass (III). Then release the dura from the tumor (if the tumor grows in layer D, the margin will be intralesional) and section the nerve root(s) crossing the tumor. Discectomies or transversal grooves in vertebral bodies are performed. Third stage in lateral position: retroperitoneal approach and re-opening of the posterior approach. The fourth stage includes providing appropriate margin over the tumor by leaving it covered by psoas. Then, finalize the discectomies or transversal grooves in vertebral bodies to remove the specimen by the anterior approach (V).
Type 7
This strategy came last in the author’s 25 years’ experience. It is indicated in thoracic and lumbar tumors growing anteriorly—even huge masses—in layer A without involvement of the canal (layer D) and without involvement of sectors 4 and 9 (Fig. 21.11). This strategy allows to remove huge tumors without torsion around the spinal cord but requires both pedicles free from tumor for appropriate margins. It is mandatory to achieve posteriorly a full release of posterior anatomical elements and spine–dural connection, as in supine position no access will be possible. First steps in prone position: piecemeal excision of the posterior arch and both pedicles and very careful full dura release. Discectomies or transverse grooves in vertebral bodies are performed to define the upper and lower margins. Second stage is in supine position. Step III is release of the anatomical structures from the tumor mass or even their sacrifice to provide appropriate margin under visual control. Arterial bypass can be performed in case of aorta involvement. On finalizing the upper and lower discectomies or osteotomies, the specimen is removed by combined maneuvers (IV).
Type 7 WBB-based en bloc resection . It is indicated in thoracic and lumbar tumors that are growing anteriorly—even huge masses—in layer A without involvement of the canal (layer D) and without involvement of sectors 4 and 9. This strategy allows removal of huge tumors without torsion around the spinal cord but requires both pedicles to be free from tumors for appropriate margins. It is mandatory to achieve by posterior approach a full release of posterior anatomical elements and spine–dural connection, as in the supine position no access will be possible. First steps in prone position are piecemeal excision of the posterior arch and both pedicles and very careful full dura release. Discectomies or transverse grooves in vertebral bodies are performed to define the upper and lower margins. The second stage is in supine position. Step 3 is release of the anatomical structures from the tumor mass or even their sacrifice to provide appropriate margin under visual control. Arterial bypass can be performed in case of aorta involvement. On finalizing the upper and lower discectomies or osteotomies, the specimen is removed by combined maneuvers (IV)
In planning the surgical procedure , the cord vascularity must be considered. During these procedures, particularly when the thoraco-lumbar resection is multilevel or the tumor particularly huge, the functional integrity of the spinal cord is at risk mostly due to the manipulation of the cord during maneuvers to deliver the tumor.
The role of the artery of Adamkiewicz as a single, exclusive feeding of the anterior spinal artery is controversial [32]. It seems reasonable that cord vascularity is not dependent on one artery. Previously we performed (unpublished data) angiographic studies before surgery to identify the radiculo-medullary artery feeding the artery of Adamkiewicz. In four cases the nerve root was sacrificed without any damage to cord vascularity. Since then, the role of such a study was felt to be less critical and did not affect the planning. Tomita and his group had the same experience and demonstrated on an animal model that the risk of cord ischemia is mostly related to the number of contiguous radicular arteries sacrificed rather than to a single artery [33,34,35]. It can be recommended to cut no more than three nerve roots bilaterally in the thoracic spine and avoid acute shortening or distraction during the resection [36].
Complications
The morbidity associated with en bloc resections is high, as the risks and complications of anterior spine surgery are combined with those of major posterior surgery. Tumor surgery also has specific morbidity related to the need for dissecting through muscle and not through anatomical planes; further, en bloc resection requires sacrificing not only the affected bone but also almost all connecting elements, creating full instability. Previous surgery and previous radiation therapy increase the risk of complications related to dissection. Infection is particularly threatening, due to the compromised immune status of many of these patients. Late aortic dissection is reported mostly in multi-operated cases including aorta release and submitted to monoportal high-dose conventional RT. Non-union is a common late complication due to the environment hostile to solid bony fusion. Mortality is not negligible, with a rate of 2.2% [15].
Case-Based Planning of Lumbar En Bloc Resection
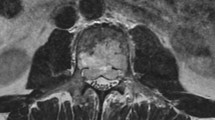
A 62-year-old male presents with complaints of back pain lasting 1 year. Previous standard radiograms were reported as negative. The standard radiogram performed at admittance (Fig. 21.12a) shows both L3 endplates as partially collapsed. The cancellous bone architecture of the body is altered with a pattern similar to columnar changes. Magnetic resonance imaging (MRI) (T2 weighted) shows multiple hyperlucent images in T12, L1, L3, L4, and L5. There is pathologic fracture of L3 with protrusion in the canal (Fig. 21.12b). The T1-weighted images show that only L3 changes from hyper- to hypolucent (Fig. 21.12c), consistent with the hypothesis of hemangiomas in T12, L1, L4, and L5. The transverse section of L3 shows that the tumor erodes the periphery of the vertebral body and expands into the psoas muscle (extracompartmental in layer A) and encroaches the canal (extracompartmental or tumor bulging in layer D). Computed tomography (CT) scan confirms the lytic lesion of L3 with erosion of the cortex (Fig. 21.13a). In L1 (Fig. 21.13b) and L4 (Fig. 21.13c), the images are consistent with hemangioma. The sagittal reconstruction (Fig. 21.13d) confirms the erosion of L3 with pathologic fracture and collapse of the cranial endplate. The pattern of the images in L1 and in L4 is more consistent with hemangioma. A CT-guided biopsy (Fig. 21.14) allows the histological diagnosis of chordoma. The Enneking staging is therefore IB (low-grade malignant, extracompartmental). The transverse image of the largest tumor extension is transferred on the WBB staging system. Sectors 4 to 9 to layers A to D (Fig. 21.15a). Oncological indication is en bloc tumor-free margin. To this purpose, a type 3b en bloc resection must be planned (Fig. 21.15b), including first an anterior approach in supine position to leave the appropriate margin by resection of the psoas under visual control (step I). After releasing the aorta and ligating cava, sacrifice the segmental lumbar vessels. Discectomies are performed after section of the anterior longitudinal ligaments at L2–L3 and at L3–L4. The second stage, posterior approach, involves intralesional piecemeal excision of sectors 3 to 10 (step II and III), release of the thecal sac by section of ligaments, and nerve root sacrifice, and sectioning the posterior longitudinal ligament and finalize the discectomies at L2–L3 and L3–L4. Step IV is the removal of the entire bloc.
L3 chordoma. (a) WBB staging of the lesion: sectors 9–4. Layers A to D and (b) WBB-based en bloc resection planning. The anterior growth requires visual control of the margins after releasing of the major vessels. Type 3a strategy: anterior approach first in supine position. Releasing of aorta and cava after sections of the segmental arteries and veins. Section of the psoas muscle above and below the tumor level, leaving a margin over the tumor anterior expansion. Section of the anterior longitudinal ligament and discectomies. Posterior approach as second stage in prone position, including removal of the healthy elements from sector 3–10, release of the thecal sac, section of the nerve roots involved in the tumor mass, and finalization of the discectomies and en bloc tumor removal
In Video 21.1, a series of animations detail the steps of the resection—anterior approach by midline transperitoneal approach in supine position and posterior approach by midline incision in prone position. Anterior reconstruction is achieved by a stackable carbon fiber cage (Fig. 21.16) connected to a couple of posterior rods fixed by pedicular screws. The full operative time was 10 h and 17 min. The coronal and sagittal alignment is correct on the standing full-spine radiogram (Fig. 21.17a, b).
Type 3a en bloc resection of L3 chordoma: reconstruction with carbon fiber (CF)-reinforced polyetheretherketone (PEEK) cage filled with autogenous graft and hydroxylapatite, connected with posterior implant. (a) Coronal orthostatic standing radiogram and (b) sagittal orthostatic standing radiogram confirming satisfactory 3D well-balanced reconstruction
Discussion and Conclusion
En bloc resection in the spine is a very demanding surgical procedure. This operation can be safely performed and achieve oncological effectiveness if some mandatory steps are followed:
-
1.
Diagnosis and staging must suggest that en bloc resection is the procedure of choice.
Since 30 years, the Enneking staging system has been adopted in many tumor centers, and many reports and reviews confirm its validity [37]. En bloc resection is proposed for benign aggressive (stage 3) [38] and for low-grade malignant tumors (stage I) [14]. For high-grade malignant tumors, en bloc resection is a valid option but must always be associated with chemotherapy or radiotherapy, according to the sensitivity of the specific tumor [39, 40]. Isolated spine metastases in patients in good general status, if not sensitive to radio and chemotherapy, can be considered for en bloc resection [19].
-
2.
Tumor extension and surgical anatomy must fulfill the criteria to perform a tumor-free margin en bloc resection safely and with acceptable functional loss.
The WBB staging system was proposed in 1997 [25] to stage primary spine tumors according to their extension, in order to easily share information on a computer-based terminology. This system was recently validated as reliable and reproducible by a multidisciplinary group of experts in spine oncology [27]. Seven groups of strategies to plan en bloc resection have been proposed to define the criteria of feasibility of this procedure according to tumor extension.
-
3.
Planning of the surgical procedure must consider the two previous points.
The surgical approach or combination and timing of approaches must be decided combining the required oncological margins and the criteria of feasibility by tumor extension and by spine region. If the margin is represented by relevant anatomical structures (dura, nerve roots, aorta, cava), a careful decision-making process will consider the improvement of prognosis versus the functional loss. In this process the patient willing will be obviously relevant. If the tumor is expanding anteriorly, the anterior approach is mandatory to leave a layer of healthy tissue over the tumor under visual control. A similar procedure must be adopted if a non-expandable anatomic structure is close to the anterior surface of the tumor. In the cervical spine and the lower lumbar spine, it is frequently necessary to combine multiple approaches due to the complexity of the anatomy.
-
4.
Morbidity
A high morbidity rate can be expected. Intraoperative bleeding affects the risk of cardiovascular failures, post-operative hematoma, delayed wound healing, and infection. Preoperative embolization is not helpful if extratumoral surgery is performed; tumor ischemia could conversely increase the vascularity on the periphery of the tumor. Patient and careful hemostasis, both of the epidural veins and of any vascular structure, is mandatory.
No more than three pairs of nerve roots should be sacrificed at the thoraco-lumbar junction in order to keep an appropriate cord vascularity. Manipulation of the dural sac, particularly at the end of these long procedures, can put the cord vascularity at risk for traction, torsion, and shortening.
Conclusion
En bloc resection in the lumbar spine is a demanding procedure, from both an oncologic and a surgical point of view. The essential surgical criteria for planning approaches and techniques are as follows.
-
Visual control is essential to achieve the required margin.
-
The most important anatomical structures must be released or resected for achieving an appropriate margin under visual control.
-
Combined simultaneous approaches are associated with higher morbidity and should be performed only when mandatory.
-
Cord vascularity must be considered in multisegmental resections.
-
Epidural bleeding can become a serious problem if underestimated.
-
Removal of the specimen must be planned by the best approach to avoid tractions, torsions, and shortening of the cord.
-
When intralesional surgery is planned or the risk of penetrating the tumor during resection is significant, selective arterial embolization is mandatory; however, when the surgeon anticipates a good probability of successful en bloc resection with oncological margins, tumor ischemia following embolization may induce peritumoral hyper-vascularization with increased risk of bleeding.
-
Hemostasis is essential; poorly controlled epidural bleeding increases the risk of cardiovascular failure at the last steps of such a long procedure.
References
Enneking WF. Muscoloskeletal tumor surgery. New York: Churchill Livingstone; 1983. p. 69–122.
Simon MA. Surgical Margins. In: Simon MA, Springfield D, editors. Surgery for bone and soft tissue Tumors. Philadelphia: Lippincott-Raven; 1998. p. 77–92.
Talac R, Yaszemski MJ, Currier BL, Fuchs B, Dekutoski MB, Kim CW, et al. Relationship between surgical margins and local recurrence in sarcomas of the spine. Clin Orthop Relat Res. 2002;397:127–32.
Rosen G. Pre-operative (neo-adjuvant) chemotherapy for osteogenic sarcoma: a ten years experience. Orthopedics. 1985;8:659–70.
Lador R, Gasbarrini A, Gambarotti M, Bandiera S, Ghermandi R, Boriani S. Surgeon’s perception of margins in spinal en bloc resection surgeries: how reliable is it? Eur Spine J. 2017 Feb 6; https://doi.org/10.1007/s00586-017-4967-0. [Epub ahead of print].
Boriani S, Weinstein JN. The role of “tumor-free margins” in the resection of spinal Tumors: who should be treating spine tumors? Semin Spine Surg. 2009;21:76–85.
Fisher CG, Saravanja DD, Dvorak MF, Rampersaud YR, Clarkson PW, Hurlbert J, et al. Surgical management of primary bone tumors of the spine: validation of an approach to enhance cure and reduce local recurrence. Spine. 2011;36(10):830–6.
Biagini R, Casadei R, Boriani S, Erba F, Sturale C, Mascari C, et al. En bloc vertebrectomy and dural resection for chordoma: a case report. Spine. 2003;28(18):E368–72.
Rhines LD, Fourney DR, Siadati A, Suk I, Gokaslan ZL. En bloc resection of multilevel cervical chordoma with C-2 involvement: case report and description of operative technique. J Neurosurg Spine. 2005;2(2):199–205.
Bailey CS, Fisher CG, Boyd MC, Dvorak MF. En bloc marginal excision of a multilevel cervical chordoma: case report. J Neurosurg Spine. 2006;4(5):409–14.
Keynan O, Fisher CG, Boyd MC, O'Connell JX, Dvorak MF. Ligation and partial excision of the cauda equina as part of a wide resection of vertebral osteosarcoma: a case report and description of surgical technique. Spine. 2005;30(4):E97–E102.
Murakami H, Tomita K, Kawahara N, Oda M, Yahata T, Yamaguchi T. Complete segmental resection of the spine, including the spinal cord, for telangiectatic osteosarcoma: a report of 2 cases. Spine. 2006;31(4):E117–22.
Druschel C, Disch AC, Melcher I, Engelhardt T, Luzzati A, Haas NP, et al. Surgical management of recurrent thoracolumbar spinal sarcoma with 4-level total en bloc spondylectomy: description of technique and report of two cases. Eur Spine J. 2012;21(1):1–9.
Boriani S, Saravanja D, Yamada Y, Varga PP, Biagini R, Fisher CG. Challenges of local recurrence and cure in low grade malignant tumors of the spine. Spine. 2009;34(22 Suppl):S48–57.
Boriani S, Bandiera S, Donthineni R, Amendola L, Cappuccio M, De Iure F, et al. Morbidity of en bloc resections in the spine. Eur Spine J. 2010;19(2):231–41.
Falicov A, Fisher CG, Sparkes J, Boyd MC, Wing PC, Dvorak MF. Impact of surgical intervention on quality of life in patients with spinal metastases. Spine. 2006;31(24):2849–56.
Patchell RA, Tibbs PA, Regine WF, Payne R, Saris S, Kryscio RJ, et al. Direct decompressive surgical resection in the treatment of spinal cord compression caused by metastatic cancer: a randomised trial. Lancet. 2005;366(9486):643–8.
Yao KC, Boriani S, Gokaslan ZL, Sundaresan N. En bloc spondylectomy for spinal metastases: a review of techniques. Neurosurg Focus. 2003;15(5):E6.
Tomita K, Kawahara N, Kobayashi T, Yoshida A, Murakami H, Akamaru T. Surgical strategy for spinal metastases. Spine. 2001;26(3):298–306.
Li H, Gasbarrini A, Cappuccio M, Terzi S, Paderni S, Mirabile L, et al. Outcome of excisional surgeries for the patients with spinal metastases. Eur Spine J. 2009;18(10):1423–30.
Stener B, Johnsen OE. Complete removal of three vertebrae for giant-cell tumour. J Bone Joint Surg Br. 1971;53(2):278–87.
Stener B. Complete removal of vertebrae for extirpation of tumors. Clin Orthop Relat Res. 1989;245:72–82.
Roy-Camille R, Saillant G, Bisserie´ M, et al. Resection vertebrale totale dans la chirurgie tumorale au niveau du rachis dorsal par voie posterieure pure. Rev Chir Orthop. 1981;67:421–30.
Tomita K, Kawahara N, Baba H, Tsuchiya H, Fujita T, Toribatake Y. Total en bloc spondylectomy. A new surgical technique for primary malignant vertebral tumors. Spine. 1997;22(3):324–33.
Boriani S, Weinstein JN, Biagini R. Primary bone tumors of the spine. Terminology and surgical staging. Spine. 1997;22(9):1036–44.
Hart RA, Boriani S, Biagini R, Currier B, Weinstein JN. A system for surgical staging and management of spine tumors. A clinical outcome study of giant cell tumors of the spine. Spine. 1997;22:1773–83.
Chan P, Boriani S, Fourney DR, Biagini R, Dekutoski MB, Fehlings MG, et al. An assessment of the reliability of the Enneking and Weinstein-Boriani-Biagini classifications for staging of primary spinal tumors by the spine oncology study group. Spine. 2009;34(4):384–91.
Boriani S. Subtotal and total vertebrectomy for tumours. In: Surgical techniques in orthopedics and traumatology. 55-070-A. Paris: Editions Scientifiques et Medicales Elsevier; 2000.
Kawahara N, Tomita K, Baba H, Toribatake Y, Fujita T, Mizuno K, et al. Cadaveric vascular anatomy for total en bloc spondylectomy in malignant vertebral tumors. Spine. 1996;21(12):1401–7.
Gasbarrini A, Simoes CE, Bandiera S, Amendola L, Barbanti Brodano G, Cappuccio M, et al. Influence of a thread wire saw guide and spinal cord protector device in “en bloc” vertebrectomies. J Spinal Disord Tech. 2012;25(2):E7–12.
Roy-Camille R, Mazel CH, Saillant G, Lapresle PH. Treatment of malignant tumors of the spine with posterior instrumentation. In: Sundaresan N, Schmidek HH, Schiller AL, Rosenthal DI, editors. Tumors of the spine. Diagnosis and clinical management. Philadelphia: W.B.Saunders; 1990. p. 473–92.
Murakami H, Kawahara N, Tomita K, Demura S, Kato S, Yoshioka K. Does interruption of the artery of Adamkiewicz during total en bloc spondylectomy affect neurologic function? Spine. 2010;35(22):E1187–92.
Fujimaki Y, Kawahara N, Tomita K, Murakami H, Ueda Y. How many ligations of bilateral segmental arteries cause ischemic spinal cord dysfunction? An experimental study using a dog model. Spine. 2006;31(21):E781–9.
Kato S, Kawahara N, Tomita K, Murakami H, Demura S, Fujimaki Y. Effects on spinal cord blood flow and neurologic function secondary to interruption of bilateral segmental arteries which supply the artery of Adamkiewicz: an experimental study using a dog model. Spine. 2008;33(14):1533–41.
Ueda Y, Kawahara N, Tomita K, Kobayashi T, Murakami H, Nambu K. Influence on spinal cord blood flow and function by interruption of bilateral segmental arteries at up to three levels: experimental study in dogs. Spine. 2005;30(20):2239–43.
Kawahara N, Tomita K, Kobayashi T, Abdel-Wanis ME, Murakami H, Akamaru T. Influence of acute shortening on the spinal cord: an experimental study. Spine. 2005;30(6):613–20.
Fisher CG, Andersson GB, Weinstein JN. Spine focus issue. Summary of management recommendations in spine oncology. Spine. 2009;34(22 Suppl):S2–6.
Harrop JS, Schmidt MH, Boriani S, Shaffrey CI. Aggressive “benign” primary spine neoplasms: osteoblastoma, aneurysmal bone cyst, and giant cell tumor. Spine. 2009;34(22 Suppl):S39–47.
Schwab J, Gasbarrini A, Bandiera S, Boriani L, Amendola L, Picci P, et al. Osteosarcoma of the mobile spine. Spine. 2012;37(6):E381–6.
Sciubba DM, Okuno SH, Dekutoski MB, Gokaslan ZL. Ewing and osteogenic sarcoma: evidence for multidisciplinary management. Spine. 2009;34(22 Suppl):S58–68.
Marmor E, Rhines LD, Weinberg JS, Gokaslan ZL. Total en bloc lumbar spondylectomy: Case report. J Neurosurg Spine. 2001;95:264–9.
Acknowledgment
It would not have been possible to conceive and finalize this chapter without the collaboration of Carlo Piovani. His work as an archivist and his original drawings are absolutely invaluable.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Electronic Supplementary Material
The steps of the resection (M4V 40379 kb)
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Karim Ahmed, A., Sciubba, D.M., Boriani, S. (2019). Lumbar En Bloc Resection. In: Sciubba, D. (eds) Spinal Tumor Surgery. Springer, Cham. https://doi.org/10.1007/978-3-319-98422-3_21
Download citation
DOI: https://doi.org/10.1007/978-3-319-98422-3_21
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-98421-6
Online ISBN: 978-3-319-98422-3
eBook Packages: MedicineMedicine (R0)