Abstract
Central vertigo is vertigo that arises due to an abnormality in the central nervous system (CNS). Traditionally, and on some anatomic and functional grounds, the vestibular system and by implication the causes of vertigo have been divided into the central and peripheral subcategories. Peripheral causes of vertigo involve the semicircular canal and saccule/ utricle. Central causes of vertigo are primarily located in the brainstem and the 8th nerve. This is not surprising given the centrality of connections from the peripheral system that relay in the brainstem including postural control, eye movements, spinal reflexes, and the adjacent cerebellum with which it connects intimately.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Central vertigo is vertigo that arises due to an abnormality in the central nervous system (CNS). Traditionally, and on some anatomic and functional grounds, the vestibular system and by implication the causes of vertigo have been divided into the central and peripheral subcategories. Peripheral causes of vertigo involve the semicircular canal and saccule/ utricle. Central causes of vertigo are primarily located in the brainstem and the 8th nerve. This is not surprising given the centrality of connections from the peripheral system that relay in the brainstem affecting postural control, eye movements, spinal reflexes, and the adjacent cerebellum with which it connects intimately.
A plethora of disease entities implicate the brainstem. Included in this exhaustive list are common and uncommon diseases including vascular disorders (strokes, aneurysm, basilar ectasia), inflammatory disorders (multiple sclerosis, Miller Fisher variant of Guillain-Barre acute demyelinating polyneuropathy, Whipple’s disease), degenerative disorders (Parkinson’s disease, progressive supranuclear palsy, multisystem atrophy, spinocerebellar atrophy, Friedreich’s ataxia), tumors (8th nerve tumors, meningiomas of the CP angle, gliomas of the brainstem, and astrocytomas of the cerebellum), nutritional deficiencies (thiamine), and toxic/metabolic anomalies (metronidazole overdose). We have chosen to concentrate on the evidence for a number of selective disorders.
Vascular Causes of Central Vertigo
Introduction
Dizziness/vertigo is a common presentation of a cerebrovascular accident (CVA), particularly in the posterior circulation. Thirty-seven percent of posterior strokes can be initially misdiagnosed compared with 16% of anterior strokes (P < 0.001) [1]. Furthermore, atypical symptoms associated with posterior circulation strokes lead to misdiagnoses with two- and fourfold higher risk of misdiagnosis [1, 2].
Twenty percent of all ischemic strokes involve regions of the brain supplied by the vertebrobasilar (posterior) circulation [3]. Vertigo has been described as the most common symptom of vertebrobasilar insufficiency [3]. In a recent study, it was found that the patients who visited the emergency department with dizziness/vertigo had a twofold (95% CI, 1.35–2.96; P < 0.001) higher risk of stroke than those without dizziness/vertigo during a follow-up of 3 years [4]. It was also demonstrated that the patients hospitalized with isolated vertigo have a 3.01 times (95% CI, 2.20–4.11; P < 0.001) higher risk for stroke than the general population during the 4-year follow-up [4]. Patients with vertigo who had three or more risk factors were found to have a 5.51-fold higher risk for stroke (95% CI, 3.10–9.79; P < 0.001) than those without risk factors [4].
Another study in California showed that the incidence rate for cerebrovascular events in ED patients discharged after vertigo was highest in the first month (30.2 [24.4–37.0] per 10,000 person-months) and then decreased during the study period to 6.5 (5.3–8.0) events per 10,000 person-months) thereafter [5].
Vertebrobasilar Insufficiency
The brainstem, cerebellum, and peripheral labyrinths are all supplied by the vertebrobasilar arterial system.
The vertebrobasilar arterial system originates with the union of the two vertebral arteries to form the basilar artery. The cerebellum is supplied by the posterior inferior cerebellar artery (PICA), which arises from the vertebral artery, and the anterior inferior cerebellar (AICA) and the superior cerebellar arteries (SCA) which arise from the basilar artery (Fig. 25.1).
Brainstem Infarct (Associated with Hearing Loss)
The AICA usually arises from the caudal third of the basilar artery and supplies the inner ear, lateral pons, middle cerebellar peduncle, and anterior inferior cerebellum, including the flocculus [6]. It is an important artery for the blood supply to the peripheral and central vestibular structures; thus, its occlusion commonly results in vertigo of either peripheral or central etiology [7]. AICA infarction is characterized by acute audiovestibular loss with or without other neurological symptoms and signs of brainstem or cerebellar involvement [7].
One study demonstrated nearly all (98%) patients with AICA territory infarction presented with acute onset of prolonged (>24 h) vertigo and had a vestibular dysfunction of peripheral, central, or combined origin, with ocular, motor, or vestibular signs, seen in a third of the study population [7]. This was attributed to the fact that AICA supplies the peripheral vestibular structures such as the inner ear and CN VIII as well as the central vestibular structures. In lieu of this complete AICA infarction usually results in combined peripheral and central vestibular damage in addition to symptoms of hearing loss, facial weakness, sensory loss, gait ataxia, and cerebellar dysmetria [7]. However, it is difficult to determine the exact mechanism responsible for prolonged vertigo in patients with AICA infarction as ischemia of any of the structures supplied by AICA can lead to vertigo [7]. In another study, 65% of the subjects with AICA infarction had a unilateral weakness to caloric stimulation, which suggests that the vertigo resulted from a peripheral vestibular structure dysfunction, while in 33% of the subjects, a normal caloric response was elicited, which points to vertigo resulting due to ischemia to the central vestibular structures [7].
Patients with cerebellar infarcts often report dizziness, occasionally in conjunction with frank vertigo, blurred vision, difficulty walking, and vomiting. Other commonly reported symptoms include gait instability, ataxia, hypotonia ipsilateral to the side of the lesion, and notably, nystagmus [3]. Patients with pure cerebellar infarcts do not typically have hemiparesis or hemisensory loss [3]. In a study [8] of patients with vertigo due to vertebrobasilar insufficiency, 62% had a history of at least one isolated episode of vertigo, and 19% developed vertigo as the initial symptom. Patients with infarction in the territory of anterior inferior cerebellar artery (AICA) may have isolated recurrent vertigo, fluctuating hearing loss, and/or tinnitus (similar to Meniere’s disease) as the initial symptoms 1–10 days prior to the permanent infarction [8].
Labyrinthine Infarction
The blood supply to the inner ear originates from the internal auditory artery (IAA), a branch of the anterior inferior cerebellar artery. Thus vertebrobasilar ischemic stroke can present with vertigo and hearing loss due to infarction of the inner ear [9]. The IAA supplies the cochlea and vestibular labyrinth, resulting in loss of auditory and vestibular function when occluded [10], and being an end artery, the labyrinth is particularly susceptible to ischemia due to limited collateral circulation from the otic capsule [9, 11]. Internal auditory artery infarction mostly occurs due to thrombotic narrowing of the AICA itself or in the basilar artery at the orifice of the AICA [9].
Sudden onset of unilateral deafness and vertigo should prompt a suspicion of labyrinthine infarction particularly in the elderly [12]. A definite diagnosis is not possible as an MRI cannot visualize the inner ear [12]. However, the apical region of the cochlea is more vulnerable to ischemia, and this may be clinically detected with the presence of low-frequency hearing loss [12].
Brainstem Infarct (No Hearing Loss)
Posterior Inferior Cerebellar Artery
Infarction in the dorsolateral medulla (Wallenberg’s syndrome) commonly involves the inferior and medial vestibular nuclei and usually manifests with nausea/vomiting, vertigo, and imbalance [9]. Vertigo in the lateral medullary infarction is usually associated with other neurologic symptoms or signs, but a tiny infarct in the lateral medulla can present with vertigo without other localizing symptoms [9, 13].
One study reported that about 11% (25/240) of patients with isolated cerebellar infarction presented as isolated vertigo only and most (24/25, 96%) patients with isolated vertigo had an infarct in the territory of the medial branch of the PICA including the nodulus [14]. It has also been reported that the caudal cerebellum in the medial branch of the PICA is the most common site responsible for central isolated vertigo of a vascular cause [3].
Acute Vestibular Syndrome (AVS)
Acute vestibular syndrome can be described as sudden onset of dizziness accompanied by nausea or vomiting, unsteady gait, nystagmus, and intolerance to head motion that persists for a day or more [15]. Isolated acute vestibular syndrome (with or without hearing loss) may be defined as vertigo/dizziness occurring in the absence of focal neurologic signs such as hemiparesis, hemisensory loss, or gaze palsy [16].
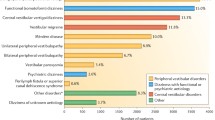
Most lesions that result in AVS from a stroke etiology occur within the territory of the PICA [15]. A systematic review assessed the central causes of AVS as follows: cerebrovascular event in posterior fossa (83%), ischemic stroke (cerebellum or brainstem) (79%), hemorrhage (cerebellum or brainstem) (4%), multiple sclerosis (11%), and other central/equivocal causes (6%) [16].
An infarction in the brainstem localized to the vestibular nuclei may mimic an acute peripheral vestibulopathy. These must be differentiated from AVS due to other causes (vestibular neuronitis, Meniere’s) with careful clinical examination including HINTS (head impulse, nystagmus, and test of skew) testing and caloric testing [17, 18]. A normal head impulse and normal caloric point to a central cause of AVS [17, 18]. These criteria initially proposed by Newman-Toker’s group have been subsequently validated by other groups. In the initial paper, the diagnostic utility of the signs includes normal horizontal HIT, skew deviation, abnormal vertical smooth pursuit, and central-type nystagmus at the bedside: they found a 100% sensitivity and 96% specificity for stroke if one of those signs was present in AVS [15, 16, 19,20,21,22].
Nonvascular Causes of Central Vertigo
There are several nonvascular causes of central vertigo. Some are well established in their pathophysiology; others are still not well understood with little data available on them. A literature review study reported that none of its included studies was large enough to identify rare causes such as post-CNS infections [16].
Tumors
Tumors of the cerebellopontine angle often cause vertigo. Vestibular schwannoma (VS) is the most frequent benign lesion that occurs at the cerebellopontine angle, representing about 90% of tumors at this site [23, 24]. A bilateral occurrence of VS is usually associated with neurofibromatosis type II. NF2 is an autosomal dominant tumor-suppressor syndrome characterized by schwannomas, meningiomas, and ependymomas that develop throughout the central and peripheral nervous systems [23]. However, the mechanism differs for different tumor types [25].Vertigo may result from a lesion of the labyrinth, compression or invasion of the endolymphatic sac, compression of the vestibular nerve, cerebellar compression, or compression of key blood supply to the vestibular organs [25].
A study [26] to characterize the clinical picture obtained with vestibular schwannomas in 122 subjects showed that only half of them reported vertigo attacks, the predominant features being hearing loss (94%) and tinnitus (83%). The vertigo associated with VS differed however from other causes by the absence or low intensity of nausea [26]. The duration of vertigo attacks ranged from 5 min to 4 h, with the intensity varying from mild to moderate. Occurrence of vertigo was not associated with duration of disease or size of tumor [26].
Microvascular compression of the vestibulocochlear nerve is also known to cause disabling vertigo usually at the cerebellopontine angle. Comorbid symptoms include tinnitus, hearing loss, and imbalance. Successful treatment may be accomplished through microvascular decompression [27]. Compressional symptoms have been attributed largely to the wide variability in the anatomy of the neurovascular complex of the cerebellopontine angle [27]. Attempts to link the symptomatic presentation to the anatomical location of the vestibulocochlear nerve compression site are yet to produce conclusive data [27, 28] (Fig. 25.2).
Vestibular Migraine
There is a definite association between vertigo and migraine; however, the pathophysiologic mechanism remains largely unclear [29]. Using the classification and diagnostic criteria [30] for diagnosis of migraine, vertigo was redefined as being a form of migraine aura, and the duration of aura was extended [30]. A diagnosis of migraine with aura is often made when vertigo occurs within 60 min before or after the onset of headache [29].
Recent collaboration between the Bárány Society and the International Headache Society has led to establishing the newest diagnostic criteria for VM with subsequent creation of the classification systems of VM [31, 32]. This features updates to the diagnostic criteria, the type of dizziness, duration, and intensity of dizziness [32].
Savundra et al. [29] retrospectively analyzed 363 patients who presented to a neurotology clinic with vertigo and found 116 patients (32%) possessed migraines. Eighty-five percent of these had no other explanations for their vertigo in contrast to only 51% of nonmigraineurs with idiopathic vertigo, suggesting that in a large proportion of patients with vertigo, VM is underdiagnosed. These underdiagnoses may be due to several factors, including the wide variability in presentation of patients with VM, lack of a widely accepted pathophysiologic model linking migraine and vertigo, and significant overlap with depression or anxiety [29, 31].
The study also noted significantly higher prevalence of a central vestibular disturbance and of a combined central and peripheral vestibular disturbance in migraineurs with vertigo [29]. Migraineurs with vertigo may also experience transient vestibular dysfunction occurring at any site between the end organ and the cerebral cortex [29]. Likely causes include ischemia of the labyrinth, vestibular nerve, vestibular nuclei, reticular activating system or cerebellar modulating pathways [29, 33]. Other possibilities include ischemia at the cortical level at the temporoparietal junction, anterior cingulate gyrus, and primary sensory cortex [29, 33]..
Demyelinating Disorder
Demyelinating disorders like multiple sclerosis (MS), although uncommon, have been estimated to be the cause of central vertigo in 10–15% of cases [16, 34]. These are largely attributed to demyelinating plaques within and around the 8th nerve fascicle or vestibular nuclei [35, 36]. MS patients have been reported to develop vertigo either as an initial symptom or during the course of the disease, with several reporting chronicity [37].
Acute symptoms of vertigo in MS may be classified into two groups: acute vestibular syndrome and positional vertigo [38]. It is widely accepted that the major cause of AVS in MS is due to damage of the vestibular nucleus or fascicular portion of the 8th CN by a lesion in the lower pons or upper medulla [39].
In a study [38] of patients presenting with AVS, 4% of the study population were identified with demyelinating disease as the cause of vertigo, with AVS occurring in demyelinating attacks in all the subjects. The most prominent clinical features were ocular motility limitation and vertical nystagmus. This, along with a normal h-HIT, suggested the presence of central localization in the subjects. MRI revealed lesions throughout the brainstem and in each cerebellar peduncle, with more than half showing gadolinium enhancement. All the lesions were noted to occur in anatomic structures involved in vestibular signaling (Fig. 25.3).
Representative axial T2-weighted brain MRIs in subjects with MS presenting with acute vestibular syndrome. Axial MRI images include cuts caudal and cranial to the purported responsible lesion in order to present extent of visible demyelination [38]. (Picture credit: Springer link)
Metronidazole-Induced Central Vertigo
Metronidazole is relatively safe when used at appropriate doses, but prolonged use may result in peripheral neuropathies and cerebellar dysfunction. Patients with the condition often present with dizziness, vertigo, and headache [40]. MRI shows the unique characteristic of increased T2/FLAIR signal in the dentate and red nucleus [41,42,43]. This finding is only alternatively seen in Wernicke’s encephalopathy. Although the pathophysiology of metronidazole neurotoxicity remains unclear, most lesions secondary to metronidazole neurotoxicity are completely reversible.
Prior studies done in rats have shown axonal degeneration after treatment with metronidazole, with symmetric lesions in the cerebellar and cochlear nuclei [44, 45]. It was postulated that metronidazole and its metabolites bind to neuronal RNA and inhibit protein synthesis resulting in reversible axonal swelling [45]. Metronidazole also crosses blood-brain barrier and can result in imaging and histological findings similar to Wernicke’s encephalopathy [44] (Fig. 25.4).
Multiple axial magnetic resonance imaging of the brain in a 22-year-old male on metronidazole presenting with cerebellar symptoms. Axial T2 images (a, b) reveal symmetric areas of increased signal in the dentate (black arrows), the facial (yellow arrows), and the red nuclei (red arrows), bilaterally. Axial fluid attenuated inversion recovery images (c) showing similar changes with restricted diffusion noted on the diffusion-weighted image (d) [44]
Central Vestibulopathy After Heat Exposure
Heat exposure is a potentially fatal condition with the CNS being reported to be particularly susceptible to heat injury [46]. Jung et al. reported a case study of patients postexposure to extreme heat, in which subjects were noted to develop vertigo and imbalance about a week after heat exposure, with positive HITs bilaterally alongside signs of cerebellar dysfunction [46]. All patients showed abnormal downward corrective saccades during horizontal head impulses along with rare head-shaking nystagmus [46].
A postmortem study found a loss of cerebellar Purkinje cells in certain patients with heat stroke [47, 48]. Additionally, an increased expression of heat stroke proteins 72 (HSP 72) was present near residual Purkinje cells indicating a selective vulnerability [47, 48]. CT and MRIs have shown atrophy in the cerebellar hemisphere and vermis in patients with heat stroke [49]. Nystagmus is thought to be attributed to damage to the vestibulocerebellum [49].
Wernicke’s Encephalopathy (WE)
While oculomotor findings and memory dysfunction are the well-known correlates of thiamine deficiency, dizziness has also been described. Differential susceptibility of the vestibular systems to thiamine deficiency can be demonstrated using the head impulse testing [50].
Kwang et al. [50] studied two patients with thiamine deficiency, one with anoxia and the other from excessive alcohol consumption. They both presented with vertigo, ataxia, and psychomotor slowing among other symptoms. Vestibular function, assessed using the bithermal caloric testing, in the anorexic patient showed minimal responses in both ears initially, which markedly improved 6 months after thiamine replacement [50].
Neuropathological examinations of patients with WE have revealed lesions in the VN, especially in the medial VN (MVN), nucleus prepositus hypoglossi, nodulus, and uvula [50], with MVN being most vulnerable to thiamine deprivation [51]. Previous studies have attributed vestibular paresis in WE to be due to lesions in the vestibular nucleus [52] (Fig. 25.5).
T2-weighted MRIs of a patient with Wernicke’s showing symmetrical hyperintense lesions are shown at dorsal portions of the medulla, periaqueductal gray matter, and medial portions of both thalami [50]. (Picture credit: Journal of Neurology, Neurosurgery, and Psychiatry)
Epileptiform Activity
Vestibular symptoms may be associated with seizures, with those resulting directly from focal, intermittent epileptic discharges collectively known as epileptic vertigo [53]. They may present as an aura symptom preceding a seizure, may be the result of a side effect of antiepileptic medications, or may constitute the seizure itself [53, 54]. Vertigo and dizziness are also known to manifest in nonconvulsive status epilepticus (NCSE) [53], a picture consistent with transient neurological attack (TNA) [55].
Penfield et al. reported that electrical stimulation of the posterior half of the superior temporal gyrus and the parietotemporal junction produced vertiginous experiences similar to those of spontaneous seizures [54, 56].
In a recent study by Kim et al. [57] in which the importance of vertigo was assessed in epileptic patients using video-EEG monitoring, it was reported that cortical stimulation studies of patients with epilepsy identified both the temporal and parietal lobes as vestibular cortical areas [58]; however, epileptic discharges in patients with epileptic vertigo were observed in more expansive areas, including the frontal and temporoparieto-occipital junctional areas, suggesting either processing of vestibular-related input across large cortical regions or spread of excitation to or from nearby areas [59]. This study also revealed that vertigo or dizziness was the most frequently encountered first aura [57]. Patients with epileptic vertigo respond well to antiepileptics as depicted by Tarnutzer et al. [53] in which response rates to antiepileptic treatment were as high as 90%.
References
Arch AE, et al. Missed ischemic stroke diagnosis in the emergency department by emergency medicine and neurology services. Stroke. 2016;47(3):668–73.
Lever NM, et al. Missed opportunities for recognition of ischemic stroke in the emergency department. J Emerg Nurs. 2013;39(5):434–9.
Savitz SI, Caplan LR. Vertebrobasilar disease. N Engl J Med. 2005;352(25):2618–26.
Lee CC, et al. Risk of stroke in patients hospitalized for isolated vertigo: a four-year follow-up study. Stroke. 2011;42(1):48–52.
Kim AS, Fullerton HJ, Johnston SC. Risk of vascular events in emergency department patients discharged home with diagnosis of dizziness or vertigo. Ann Emerg Med. 2011;57(1):34–41.
Amarenco P, et al. Anterior inferior cerebellar artery territory infarcts. Mechanisms and clinical features. Arch Neurol. 1993;50(2):154–61.
Lee H, et al. Infarction in the territory of anterior inferior cerebellar artery: spectrum of audiovestibular loss. Stroke. 2009;40(12):3745–51.
Grad A, Baloh RW. Vertigo of vascular origin. Clinical and electronystagmographic features in 84 cases. Arch Neurol. 1989;46(3):281–4.
Kim JS, Lee H. Vertigo due to posterior circulation stroke. Semin Neurol. 2013;33(3):179–84.
Navi BB, et al. Application of the ABCD2 score to identify cerebrovascular causes of dizziness in the emergency department. Stroke. 2012;43(6):1484–9.
Oas JG, Baloh RW. Vertigo and the anterior inferior cerebellar artery syndrome. Neurology. 1992;42(12):2274–9.
Lee H, Yi HA, Baloh RW. Sudden bilateral simultaneous deafness with vertigo as a sole manifestation of vertebrobasilar insufficiency. J Neurol Neurosurg Psychiatry. 2003;74(4):539–41.
Kim JS. Vertigo and gait ataxia without usual signs of lateral medullary infarction: a clinical variant related to rostral-dorsolateral lesions. Cerebrovasc Dis. 2000;10(6):471–4.
Lee H, et al. Cerebellar infarction presenting isolated vertigo: frequency and vascular topographical patterns. Neurology. 2006;67(7):1178–83.
Kattah JC, et al. HINTS to diagnose stroke in the acute vestibular syndrome: three-step bedside oculomotor examination more sensitive than early MRI diffusion-weighted imaging. Stroke. 2009;40(11):3504–10.
Tarnutzer AA, et al. Does my dizzy patient have a stroke? A systematic review of bedside diagnosis in acute vestibular syndrome. CMAJ. 2011;183(9):E571–92.
Kim HA, Lee H. Isolated vestibular nucleus infarction mimicking acute peripheral vestibulopathy. Stroke. 2010;41(7):1558–60.
Chang TP, Wu YC. A tiny infarct on the dorsolateral pons mimicking vestibular neuritis. Laryngoscope. 2010;120(11):2336–8.
Chen L, et al. Diagnostic accuracy of acute vestibular syndrome at the bedside in a stroke unit. J Neurol. 2011;258(5):855–61.
Saber Tehrani AS, et al. Small strokes causing severe vertigo: frequency of false-negative MRIs and nonlacunar mechanisms. Neurology. 2014;83(2):169–73.
Edlow JA, Newman-Toker D. Using the physical examination to diagnose patients with acute dizziness and vertigo. J Emerg Med. 2016;50(4):617–28.
Nouh A, Remke J, Ruland S. Ischemic posterior circulation stroke: a review of anatomy, clinical presentations, diagnosis, and current management. Front Neurol. 2014;5:30.
Teggi R, et al. Vestibular assessment in patients with vestibular schwannomas: what really matters? Acta Otorhinolaryngol Ital. 2014;34(2):123–8.
Barbara M, et al. Double localization of a unilateral sporadic vestibular schwannoma. Acta Otorhinolaryngol Ital. 2008;28(1):34–7.
Franco-Vidal V, Negrevergne M, Darrouzet V. Vertigo and pathology of the cerebello-pontine angle. Rev Laryngol Otol Rhinol (Bord). 2005;126(4):223–6.
Kentala E, Pyykko I. Clinical picture of vestibular schwannoma. Auris Nasus Larynx. 2001;28(1):15–22.
Wuertenberger CJ, Rosahl SK. Vertigo and tinnitus caused by vascular compression of the vestibulocochlear nerve, not intracanalicular vestibular schwannoma: review and case presentation. Skull Base. 2009;19(6):417–24.
Ryu H, et al. Neurovascular compression syndrome of the eighth cranial nerve. Can the site of compression explain the symptoms? Acta Neurochir. 1999;141(5):495–501.
Savundra PA, et al. Migraine-associated vertigo. Cephalalgia. 1997;17(4):505–10. discussion 487.
Headache Classification Committee of the International Headache Society. Classification and diagnostic criteria for headache disorders, cranial neuralgias and facial pain. Cephalalgia. 1988;8(Suppl 7):1–96.
Headache Classification Committee of the International Headache, S. The international classification of headache disorders, 3rd edition (beta version). Cephalalgia. 2013;33(9):629–808.
O’Connell Ferster AP, Priesol AJ, Isildak H. The clinical manifestations of vestibular migraine: a review. Auris Nasus Larynx. 2017;44(3):249–52.
Bottini G, et al. Identification of the central vestibular projections in man: a positron emission tomography activation study. Exp Brain Res. 1994;99(1):164–9.
Zaffaroni M, Baldini SM, Ghezzi A. Cranial nerve, brainstem and cerebellar syndromes in the differential diagnosis of multiple sclerosis. Neurol Sci. 2001;22(Suppl 2):S74–8.
Commins DJ, Chen JM. Multiple sclerosis: a consideration in acute cranial nerve palsies. Am J Otol. 1997;18(5):590–5.
Frohman EM, et al. Vertigo in MS: utility of positional and particle repositioning maneuvers. Neurology. 2000;55(10):1566–9.
Rae-Grant AD, et al. Sensory symptoms of multiple sclerosis: a hidden reservoir of morbidity. Mult Scler. 1999;5(3):179–83.
Pula JH, Newman-Toker DE, Kattah JC. Multiple sclerosis as a cause of the acute vestibular syndrome. J Neurol. 2013;260(6):1649–54.
Schumacher GA. Demyelinating diseases as a cause for vertigo. Arch Otolaryngol. 1967;85(5):537–8.
Patel K, et al. Cerebellar ataxia following prolonged use of metronidazole: case report and literature review. Int J Infect Dis. 2008;12(6):e111–4.
Woodruff BK, Wijdicks EF, Marshall WF. Reversible metronidazole-induced lesions of the cerebellar dentate nuclei. N Engl J Med. 2002;346(1):68–9.
Bottenberg MM, et al. Metronidazole-induced encephalopathy: a case report and review of the literature. J Clin Pharmacol. 2011;51(1):112–6.
Ralph ED. Clinical pharmacokinetics of metronidazole. Clin Pharmacokinet. 1983;8(1):43–62.
Agarwal A, et al. Metronidazole-induced cerebellar toxicity. Neurol Int. 2016;8(1):6365.
Bradley WG, Karlsson IJ, Rassol CG. Metronidazole neuropathy. Br Med J. 1977;2(6087):610–1.
Jung I, et al. Delayed vestibulopathy after heat exposure. J Neurol. 2017;264(1):49–53.
Bouchama A, Knochel JP. Heat stroke. N Engl J Med. 2002;346(25):1978–88.
Bazille C, et al. Brain damage after heat stroke. J Neuropathol Exp Neurol. 2005;64(11):970–5.
Albukrek D, et al. Heat-stroke-induced cerebellar atrophy: clinical course, CT and MRI findings. Neuroradiology. 1997;39(3):195–7.
Choi KD, et al. The vestibulo-ocular reflexes during head impulse in Wernicke’s encephalopathy. J Neurol Neurosurg Psychiatry. 2007;78(10):1161–2.
Witt ED, Goldman-Rakic PS. Intermittent thiamine deficiency in the rhesus monkey. I. Progression of neurological signs and neuroanatomical lesions. Ann Neurol. 1983;13(4):376–95.
Furman JM, Becker JT. Vestibular responses in Wernicke’s encephalopathy. Ann Neurol. 1989;26(5):669–74.
Tarnutzer AA, et al. Clinical and electrographic findings in epileptic vertigo and dizziness: a systematic review. Neurology. 2015;84(15):1595–604.
Alpers BJ. Vertiginous epilepsy. Laryngoscope. 1960;70:631–7.
Nagayama M, et al. Novel clinical features of nonconvulsive status epilepticus. F1000Res. 2017;6:1690.
Penfield W, Kristiansen K. Seizure onset and the localization of epileptic discharge. Trans Am Neurol Assoc. 1948;73(73 Annual Meet):73–80.
Kim DW, Sunwoo JS, Lee SK. Incidence and localizing value of vertigo and dizziness in patients with epilepsy: video-EEG monitoring study. Epilepsy Res. 2016;126:102–5.
Guldin WO, Grusser OJ. Is there a vestibular cortex? Trends Neurosci. 1998;21(6):254–9.
Hewett R, et al. Benign temporo-parieto-occipital junction epilepsy with vestibular disturbance: an underrecognized form of epilepsy? Epilepsy Behav. 2011;21(4):412–6.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Lawal, O., Navaratnam, D. (2019). Causes of Central Vertigo. In: Babu, S., Schutt, C., Bojrab, D. (eds) Diagnosis and Treatment of Vestibular Disorders. Springer, Cham. https://doi.org/10.1007/978-3-319-97858-1_25
Download citation
DOI: https://doi.org/10.1007/978-3-319-97858-1_25
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-97857-4
Online ISBN: 978-3-319-97858-1
eBook Packages: MedicineMedicine (R0)