Abstract
Health care payers (self-insured employers, insurance companies, state Medicaid agencies, etc.) are increasingly playing a role as thoughtful purchasers of health care. In these new value-based purchasing (VBP) initiatives, the focus is on paying for value rather than volume of services, an endeavor necessitating robust health information technology (IT). Successful efforts to implement VBP methodologies, from pay for performance to global budgets, entail a coevolution of technology; practice change designed to achieve benchmarks; and ongoing improvement against strategic quality measures. Ideally, this integrated approach to health system redesign will align technology, workflow, and quality with the goal of improving health outcomes. A key goal of VBP is for payers and purchasers to balance provider incentives and accountability in a way that supports patient-centered care and consumer engagement. Involving consumers (e.g., beneficiaries, patients, and caregivers) in the design and implementation of health IT is one important tactic to ensure the tools and programs that are developed are responsive to consumer’s needs. Promising future directions include efforts to incorporate social determinants of health into care and VBP, and developing a broader perspective on whole-person care. Both are only possible with robust consumer-facing health IT. The ultimate goal for policy and practice is to engage consumers and patients the design and implementation of health IT systems and VBP programs that promote health and well-being.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Alternative Payment Models Person-Centered Care
- Value-Based Purchasing
- Quality payment program
- Person-centered thinking
- Health IT
- Triple aim
- Pay for Performance
- Global budgets
- Consumerism
- Patient Portals
Purchasers’ Role and Tools to Promote Value-Based Purchasing
Health care payers (self-insured employers, insurance companies, state Medicaid agencies, etc.) are increasingly playing a role as thoughtful purchasers of health care. Health care purchasers have a substantial role to play in achieving the “triple aim ” of healthcare—better care, smarter spending, and healthier people (Centers for Medicare and Medicaid Services, 2016a, 2016b, 2016c). As defined by the Agency for Healthcare Research and Quality, “Purchasers” are public and private sector entities that subsidize, arrange and contract for—and in many cases bear the risk for—the cost of health care services received by a group of beneficiaries (AHRQ, 2002). This new approach is often referred to as value-based purchasing (VBP), a model in which the focus is on paying for value rather than volume of services.
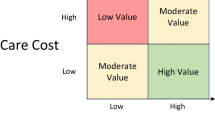
Here, it should be clarified that the concept of value-based purchasing entails strategies to hold providers accountable for both cost and quality of care :
Value-based purchasing brings together information on the quality of health care, including patient outcomes and health status, with data on the dollar outlays going towards health. It focuses on managing health care utilization to reduce inappropriate or unnecessary care and to identify and reward the best-performing providers. This strategy can be contrasted with more limited efforts to negotiate price discounts, which reduce costs but do little to ensure that quality of care is improved." (Rybowski & Eichler, 1997)
Most often, VBP models operate by enacting provider contracts that incentivize health care providers to achieve a set of targeted activities (e.g., ensure children receive all required immunizations) or health outcomes (e.g., reduce obesity rates). These health outcomes are usually assessed with respect to validated quality measures , which require uniform data collection and may require sophisticated calculations to adjust risk for patient acuity. These provider contracts may also be structured to provide bonuses for decreasing low-value care, such as the percentage of low-acuity visits to the emergency room, a goal intended to encourage provider and patient communication and care coordination.
As illustrated by the example above, VBP models necessitate robust health IT (Adler-Milstein, Embi, Middleton, Sarkar, & Smith, 2017). Successful efforts to implement VBP methodologies—from pay for performance to global budgets —entail a coevolution of technology, changes in practice patterns and workflow, and quality measurement strategies designed to promote improvement over time (see “Purchasers’ Role and Tools to Promote Value-Based Purchasing”). Ideally, this approach to health system redesign will also demonstrate a variety of ways in which VBP can incorporate consumer health IT to improve health outcomes (Fig. 15.1).
Case Study: The US’ Clarion Call to Improve Quality
In the early 2000s, poor quality care , including medical errors and suboptimal health outcomes, led to a clarion call for investment in infrastructure to shift the paradigm from paying for volume of services to value of services (McGinnis et al., 2002; IOM, 2000). Purchasers’ role in leading this transformation has been viewed as a critical component of delivery system reform due to the substantial role purchasers play in deciding which plans and services to select. As of 2015, public and private healthcare purchasers, including employers and public insurance providers purchase insurance on behalf of 82% non-elderly Americans (Kaiser Family Foundation, 2016).
Due to the extensive reach of employer-based coverage, combined with public coverage through state Medicaid programs and Medicare, the USA provides an effective example of the roles purchasers can play to promote VBP to measure, monitor, and improve the quality of care . Arguably, the US’ ability to bend the “cost curve” for the US health spending is highly dependent on effectively deploying VBP strategies, which in turn will depend on the extent to which consumers and providers are given useful tools to guide practice change . For this reason, the majority of examples of VBP strategies discussed in this chapter are based in the USA.
As shown in Fig. 15.2, there are multiple goals of VBP . Over the short or intermediate-term, purchasers aim to promote opportunities for consumers to elect high-quality providers and services, choose appropriate utilization of services (and decrease low-value care), increase healthy behaviors including diet and exercise, and see a reduction in medical errors. Over the longer term, goals articulated by purchasers with respect to VBP strategies include increased health status and consumer satisfaction; decreased cost; and increased competitiveness for workers due to employee’s selecting benefit packages that provide higher-quality services.
All of these VBP efforts utilize strategies designed to influence the decisions or behavior of individual consumers (i.e., employees, beneficiaries, and patients), and/or health care entities, usually providers and/or plans. Ideally, VBP strategies integrate efforts to support change at both the consumer and provider levels.
Health IT, the Foundation of Value-Based Purchasing
The Health Information Technology for Economic and Clinical Health (HITECH) Act, enacted as part of the American Recovery and Reinvestment Act of 2009, provided financial incentives and technical support for providers to implement and use electronic health records (EHRs) . This legislation conceptualized the notion of “meaningful use,” that is, collection and application of electronic health data to improve health care practice and outcomes.
Improving the types of information available to providers and consumers reduces “information asymmetry ,” in which information among parties is unequal and therefore power dynamics are unbalanced. One recurring example of information asymmetry in healthcare is that information on an individuals’ care is not always readily available to all involved parties. Clinicians often have more information on a clinical diagnosis than the patient, which can preclude the patient from taking a more active role in his/her care. Providers may have a limited view into an individual’s health status or life circumstances if they are not part of a patient’s regular care team.
Consider care provided to a patient experiencing an acute episode of care such as an asthma attack . To the extent the asthma attack is precipitated by environmental factors, or a lack of access to needed medications, a treating clinician may be at a disadvantage to provide the best care or treat the problem in a way that will prevent subsequent acute episodes. Health IT can address this asymmetry by providing the patient’s history of care, medications, and history of medication refills, as well as information on how to reach the patient’s primary care provider or care coordinator. Such health IT tools can ensure that health information is available to both providers and consumers at the right place and time in order to improve care and maximize healthy outcomes. This type of approach can also link together providers and patients to create virtual care teams and improve transitions of care. This is sometimes referred to as providing “actionable information ” to providers and consumers.
Many VBP programs are structured to explicitly reward providers for addressing the root cause of acute health problems and seek solutions that promote health. Pay for performance programs that incentivize a reduction in hospital readmissions within 30 days is one example of this type of model.
However, information alone is not sufficient to change provider or consumer behavior. Information must be used in new ways to highlight opportunities to reduce waste and improve care, and to facilitate coordination care for complex medical conditions. Doing so will necessitate a change in workflows in the clinic, which will undoubtedly disrupt patterns of the current medical practice. Incentivizing a significant change in practice patterns and workflow requires that strong incentives are part of new purchasing models.
Health IT is foundational to VBP because provider and consumer-facing technology creates a capability to set goals and measure improvement against set benchmarks. Changes in the culture of healthcare delivery are more likely to be sustained if stakeholders have a full understanding of the expectations and outcomes against which performance will be measured (e.g., quality measures).
As discussed in the following sections, there are new opportunities for consumers to be actively engaged in the design, implementation, and ongoing evaluation of VBP. It is now possible to ensure that VBP programs are responsive to consumer needs. Some of these innovations are based on health reforms in the Affordable Care Act, some on opportunities in consumer informatics , and some due to significant investments in developing structured approaches to consumer and patient engagement in disability rights and services, health care, and health research.
Purchasers’ efforts to engage consumers in the design and deployment of health IT for VBP can borrow heavily from these cross-sectoral efforts since purchasing methodologies strive to support evidence-based medicine and best-in-class care. This research gives purchasers the confidence in their ability to set sustainable rates and payment incentives. Consumer engagement , health IT, and VBP models are creating new opportunities to measure and improve how care is organized, financed, and delivered.
Making the Most of Health IT to Engage Providers and Consumers
A key principle of delivery system transformation is the need for payers and purchasers to balance appropriate incentives and accountability while supporting patient-centered care and consumer engagement. While the theory of consumer-facing strategies for delivery system transformation is laudable, in practice, most consumers do not understand the major changes underway in the health care system. Furthermore, consumers are not well prepared to navigate this new terrain, either in terms of understanding the goals of VBP or their personal role. All are areas in which healthcare consumers can be more actively engaged in care, as well as the design of future VBP programs.
Implementation of diverse VBP programs has demonstrated the value of health IT to reduce information asymmetry, and engage providers as well as consumers in strategies to promote health (Manary, Staelin, Kosel, Schulman, & Glickman, 2014). Yet, health care purchasers have significant improvement to make in order to integrate consumer perspectives into the design of VBP. This section explores two approaches to engage consumers and providers in VBP: applying the so-called patient-centeredness and design thinking in principle and practice; and creating robust mechanisms for consumer feedback as value-based purchasing models evolve.
Person-Centered Care
As purchasers consider approaches to promote overall health and well-being, it is useful to embrace person-centered care as an underlying principle of VBP. “Person-centered care” and “patient-centered care” will be used synonymously in this discussion about ways to engage health care consumers, be they patients, community-members seeking assistance with health or social services, or caregivers.
The term “patient-centered care” originated more than a quarter century ago, and was identified as one of the six pillars of high-quality healthcare by the National Academy of Medicine (formerly the Institute of Medicine) in its landmark report, “Crossing the Quality Chasm.” (IOM, 2000) Patient-centered care is a philosophy that sees patients as equal partners in care with the goal of ensuring that care decisions are appropriate to meet individual needs, values, and preferences.
Patient-centered care focuses on compassion, dignity, and respect, emphasizing independence and decisional autonomy (The Health Foundation, 2014). Consumer-reported measures of patient-centered care and patient experience (including satisfaction ratings) are increasingly being reported alongside quality measures and scorecards . There is strong evidence that patient-centeredness is correlated with higher-quality care as well as improved outcomes (McMillan et al., 2013).
Person-centered thinking is a related concept used primarily in the social service sector. Person-centered thinking supports positive control and self-direction. The goal is to promote the greater likelihood that service plans will be used and acted on, and will be updated on an ongoing basis; and that the client or consumer’s ability to lead a fulfilling, independent life is maximized (District of Columbia Department of Disability Services, n.d.). Due to the philosophical similarities between the two concepts, this discussion will not address the nuances of the person-centered thinking separate from patient-centered care. Nonetheless, it is important to understand both concepts and find ways to bring healthcare and social services together to design IT strategies that promote health.
It is important for leaders to review systems and services and take time to assess the degree to which patient-centered care is embedded in current programs. This can be done with any number of approaches to measuring the person-centeredness. For example, a 2014 systematic review of the literature by the Health Foundation in the UK cites numerous resources—and more than 150 internationally recognized measures (The Health Foundation, 2014). These measures are available to assist programs and organizations in assessing their orientation to patient-centered care.
Overall, initial assessment of the patient-centeredness of existing programs is a foundational step to design VBP programs. Choosing to incorporate program designs and Health IT tools that are patient-centered can significantly enhance the value of healthcare programs aimed at improving outcomes. While organizations identify a deficit in patient-centered care , there are trainings for organizations or individuals to enhance patient-centeredness.
Design Thinking
“Design thinking ” (and the corollary concept of user-centered design) is increasingly invoked as an approach to build person-centered technology. Design thinking is grounded in ethnography, by observing people in their environment, and developing solutions that improve or enhance the way they live their lives.
As a simple example, a design thinking approach to presenting information on an individual’s current health status (e.g., weight and blood pressure) could involve a conversation about individual health goals, followed by observation of a recipient reviewing a mockup of the information. Based on feedback from these sessions to identify aspects that may be confusing or cryptic, information can be redesigned and presented in a way that the consumer can better understand, such as simplified language, or visuals.
With respect to designing health IT to support programs and a system of care that promote individuals’ health, patient-centered care and design thinking are complementary concepts for healthcare leaders. Both should be assessed and addressed in the early stages of creating VBP programs.
Engaging Consumers in the Design of Health IT and VBP
Involving beneficiaries and patients in the design and implementation of health IT is another strategy to ensure that the technological tools that support VBP programs are responsive to consumers’ needs.
In recent years, extensive work has been done in the context of patient-centered outcomes research to implement human-centered design principles in “learning health systems” (Foraker et al., 2015; Hartzler, Chaudhuri, Fey, Flum, & Lavallee, 2015; Payne, 2013; Revere, Dixon, Hills, Williams, & Grannis, 2014). This work is a relatively early proof of concept that consumers can be actively engaged in technology development for complex health programs, with broader implications for policy. Many of these efforts have generated methodologies for engaging consumers in software development and borrow from the agile approach to software development.
Figure 15.3 illustrates one framework for conceptualizing integrated design of VBP and Health IT, highlighting specific steps of the development process that can integrate feedback from consumers effectively.
A recent example illustrates the value of engaging end-users, particularly consumers, in the design of health IT tools deployed to motivate behavior change and improve quality. Hartzler and colleagues at the University of Washington provide a step-by-step process that they applied with clinical end-users to assess information needs and design a dashboard for Washington State’s Surgical Care and Outcomes Assessment Program (SCOAP) spinal care registry (Hartzler et al., 2015).
The authors used a three-step human-centered design process to gather feedback on end-user preferences for the tool in which they sought to:
Understand the context of Health IT uses, including stakeholder interviews to provide the context in which the dashboard would be used to facilitate a conversation between patient and provider;
Build consensus through an iterative process of understanding user needs, determining design priorities, and sharing design prototypes to, and finalizing prototypes; and.
Establish design specifications for PRO Dashboard implementation including personalizing design prototypes.
This process and method is highly generalizable to the development of robust Health IT tools used to support VBP models. While Hartzler and colleagues did not explicitly employ this process with consumers for the Spine SCOAP project , their human-centered design methodology is highly transferrable to a consumer-facing strategy.
Patient Portals and Feedback Loops: Putting Individuals in Charge of their Own Health Information
Given the myriad applications for health IT in the care delivery context, the challenge for payers and purchasers is to identify which technologies truly put individuals in charge of their own information and build these into VBP programs. A first step may be to educate consumers on the paradigm shift in progress, as many may be unfamiliar with the notion and importance of moving from a volume-driven system to a value-driven one.
Beyond patient education, purchasers can progress towards developing consumer health IT and provider-mediated systems that put consumers at the center of their care, including system capabilities that allow patients to monitor and measure care and health outcomes. Prevalent examples include patient portals and the use of the EHR to collect patient feedback from patient-reported outcomes (PROSs) , which can be used to monitor individual outcomes and guide a course of care (Snyder & Wu, 2017), as well as support quality measurement and reporting.
Price transparency tools are another technological approach to reduce information asymmetry. While these are promising strategies, the implementation of these approaches remains highly varied across practice.
Patient Portals
Some notable successes have been achieved within specific programs implementing ePHRs or “electronic personal health records” and patient portals. There is growing evidence that access and use of portals for visit summaries, lab testing, and facilitating email communication with providers may result in higher patient satisfaction and improved outcomes (Lyles et al., 2016).
The availability of ePHRs to complement electronic health records is a relatively recent phenomenon, owing to the development of ePHRs by Microsoft and Google, combined with support from large insurers such as Blue Cross/Blue Shield. The current drivers of ePHRs and patient portals are requirements of CMS’ meaningful use program.
Although the regulatory requirements are subject to change, the capabilities and concepts entailed in meaningful use deserve review, since they directly support patient-centered care:
-
Clinical summaries provided to the patient after each visit,
-
Secure messaging (SM) between patient and provider,
-
The ability to view, download, and transmit personal health record data,
-
Patient-specific education,
-
Patient reminders for preventative services, and.
-
Medication reconciliation (Irizarry, DeVito Dabbs, & Curran, 2015).
These types of health IT system features provide core infrastructure to support VBP programs. A patient who can engage in secure messaging, view personal health data, and receive preventive care reminders is apt to be more engaged in wiser health-care decision-making, including individual purchasing decisions.
From purchasers’ perspectives, engaging consumers to attain their feedback on care and care needs has potential to drive a virtuous cycle of direct consumer measurement and evaluation, which then informs the design of services that promote health . Patient portals are one way to ensure ongoing ability to exchange of information between consumers—including patients and caregivers—and providers.
However, a 2015 literature review of 120 articles summarizes a mixed experience with patient portals’ results in terms of the ability to promote patient engagement and ideal features of patient centeredness such as self-efficacy (Irizarry et al., 2015). Sorondo and colleagues report similar results based on the use of a patient portal to collect wellness information at Eastern Maine Medical Center from 2013 to 2016 (Sorondo et al., 2016), which the authors attribute, in part, to system-level challenges.
The key impediments to successful and widespread implementation of patient portals identified by Sorondo and colleagues include: (1) adoption by providers, (2) the ease of use of the technology, and (3) a lack of full integration with clinical EHR systems . VBP programs should be mindful of these challenges if consumer participation via patient portals is a core component of a consumer-facing strategy.
Patient-Reported Outcomes
Patient-reported outcomes (PROs) are another useful method of promoting patient engagement and feedback. PROs can put the patients’ voice at the center of care, since they are designed to collect patients’ self-reports of symptoms and experiences using structured, scientifically validated survey instruments. PROs enable providers/health systems to use a variety of forms of health IT to gather meaningful feedback from patients and consumers. PROs have flexibility to be reported in real time, yet can be collected separately from a healthcare encounter.
An increasing range of options for collecting PROs using health IT are currently available—via cell phone (Adler et al., 2016), interactive voice response (IVR) , to data collection via iPad (Wilcox, Gallagher, & Bakken, 2013), patient portals, and kiosks. PROs can also support quality measurement of progress towards a clinical outcome (Centers for Medicare and Medicaid Services, 2016a, 2016b, 2016c; Chenok, Teleki, SooHoo, Huddleston, & Bozic, 2015; Lavallee et al., 2016; National Quality Forum, 2013).
Use of PROs is particularly promising for self-reports of symptoms in which medical diagnostics and imaging may be less predictive of symptom reduction. Mental health status, and pain and functioning (e.g., for knee and hip replacement) are two examples of conditions for which self-reported symptoms are generally valid measures of burden of illness (Mitchell, Yadegarfar, Gill, & Stubbs, 2016; Rolfson et al., 2016).
As discussed in PCORI’s new Users’ Guide for Integrating Patient-Reported Outcomes in Electronic Health Records (Snyder & Wu, 2017), PRO data is increasingly used within EHRs to provide ongoing feedback regarding patients’ direct reports of symptoms, functioning, and health-related quality of life. As PRO measures are developed and validated for use by payers and purchasers, there is growing interest in using dynamic strategies via mobile technology to measure care quality and outcomes, rather than more general patient-generated health information or satisfaction data reported via survey.
Similarly, at the provider level, new technologies are being developed to integrate PROs from the EHR directly into measures reported to federal payers such as CMS, including the National Institutes of Health’s PROMIS System (National Institutes of Health, 2017). Newer tools such as the Clinical Quality Measure Aligned Population Health Reporting Tool (CAliPHR) ease the burden of reporting for providers, thus making it practical for purchasers to require PROs as a component of value-based purchasing models (Chesapeake Regional Information System for Our Patients, n.d.).
PROs are also being used by organizations to predict the need for future resources. Bayliss and colleagues reported a novel implementation of the Brief Health Questionnaire used to predict resource needs for newly enrolled beneficiaries within Kaiser Permanente Colorado (Bayliss et al., 2016). The authors demonstrated that the 10-item questionnaire, covering self-reported health status, functional limitations, medication use, presence of 0–4 chronic conditions, self-reported emergency department (ED) use during the prior year, and lack of prior insurance, was significantly predictive of high-cost care.
As sophistication using and implementing PROs in practice grows (e.g., within the EHR or other IT systems), purchasers may soon have patient-reported quality measures that can be used to differentiate important health outcomes. If this trend comes to pass, purchasers will likely require that an increasing number of quality measures included in VBP contracts are based on PROs. Such a strategy would ensure that the patient voice is reflected in the outcomes used by VBP programs to motivate behavior change among providers.
Interactive Tools to Promote Price Transparency
Finally, interactive tools to promote price transparency , budgeting, and service comparisons are becoming available to reduce information asymmetry with respect to cost and quality of services. Numerous websites now provide cost-comparison information on health plans, distinct services such as joint replacement, pregnancy care, or diagnostic imaging, and some provide detailed cost information to inform consumers about the quality of outcomes as well as out of pocket costs (Consumer Reports, 2016).
While this is a dynamic area with new market entrants seeking ways to provide information on prices to health care consumers, it is unclear how consumers are responding to such services. A 2016 Consumer Reports’ review of 20 cost estimator tools (including five stand-alone services such as FAIR health) demonstrates that few consumers currently use these tools (Consumer Reports, 2016). This lesson has been underscored by the experience of companies such as Castlight Health, which has faced challenges meeting market expectations. Castlight provides employees with information about the price and quality of services offered by healthcare providers. Castlight was touted as an opportunity to revolutionize consumer understanding of health care prices and quality, as evidenced by a $2 billion valuation at its initial public offering in 2014 (Seeking Alpha, 2014). However, it remains to be seen whether the company—or other similar ventures—will achieve anticipated returns and substantially change consumer behavior.
Nonetheless, the expectation is that price transparency will improve as data sources mature. The presumption is that high-deductible health plans and other approaches to reducing moral hazard by requiring consumers to have more financial “skin in the game” will reduce inappropriate utilization and improve health outcomes. However, it does not seem that we have yet reached an appropriate balance between available information and incentives to use data on price and quality (Kliff, 2015). For VBP programs interested in integrating consumer-facing strategies, it will likely require time and attention to build price transparency tools into an effective and well-coordinated system of care.
Emerging Trends and Future Opportunities: Incorporating Life Circumstance into VBP through Consumer Health IT
Collection and use of social determinants of health data, or life circumstance data, has been identified as a promising next step for VBP (Spencer, Freda, McGinnis, & Gottleib, 2016). Socioeconomic and environmental aspects of individuals’ lives, such as food availability, housing, safety, transportation, and family circumstances, as well as personal characteristics have bearing on an individual’s ability to access health care and their ability to be healthy and stay healthy.
The National Academy of Medicine , among others, has suggested that 80% of factors contributing to health and wellness fall outside the realm of clinical influence (IOM, 2003). In response, health and social service sectors recognize a pressing need to incorporate life circumstance and a broader perspective on the whole person into care delivery. Incorporating these data across sectors is only possible with effective health information exchange (HIE) .
Purchasers would do well to attend to life circumstance when designing tools that support their consumers’ choices about healthcare consumption. For example, a consumer who lacks reliable transportation to a clinician’s office may defer or delay necessary care, possibly ending up in an emergency room. This could be attenuated through virtual visits or telemedicine : thus, purchasers designing VBP approaches should consider the ways in which social determinants drive health care choices for their particular population. This is a particularly important consideration in rural areas and for vulnerable or disadvantaged populations.
Consumer-facing health IT is a likely path to collect and share information on life circumstances. Using a structured approach to data collection, consumer information can be collected to better assess health needs, promote effective referral patterns and transitions of care, and close the loop with respect to participation in health programs.
Yet, significant challenges impede collection and use of these data to promote behavior change among providers and health care consumers. Some stakeholders have sought to minimize barriers to collecting social determinants by proposing strategies to collect this data in a structured, unified way so that the information can be used in multi-sector collaborations.
As one example, the National Association of Community Health Centers has developed the Protocol for Responding to and Assessing Patients’ Assets, Risks, and Experiences (PRAPARE) , which many organizations are adopting as a standardized approach to screen for social determinants of health (National Association of Community Health Centers, 2016). Nonetheless, many organizations use unique measures they have developed to meet their client’s service needs, and may be reluctant to discontinue current data collection that they perceive meets their needs.
The degree of variation in measures used by health and social programs has led to a patchwork of diffuse measures of related concepts such as housing insecurity, food insecurity, health literacy, access to transportation, stress, and so forth. In a recent meeting convened by the Department of Health Care Finance in the District of Columbia (DC’s Medicaid program), stakeholders identified more than 50 tools to measure domains of social determinants. The underlying differences in approaches to measuring social factors that influence health makes it difficult for purchasers to coalesce around common measures. Without common, accepted measures, it will be difficult for purchasers to benchmark quality or design VBP programs that reward providers for addressing life circumstances as part of the care process.
A related consideration is the need to design value-based measures that present a uniform set of goals. It is unclear as yet what level of health improvement can be expected based on interventions to address social determinants of health , such as permanent supportive housing, programs to provide supplemental nutrition, educational interventions, etc., and other relevant factors (Spencer et al., 2016). As a consequence, risk adjustment models, and rate setting methods that incorporate data on social determinants—both core components of a value-based purchasing program —are not widely available.
A number of ventures and publications suggest that focused attention to social determinants will bear fruit in the coming years. An influential series of publications from the National Academy of Medicine on “Vital Directions for Health and Health Care” includes recommendations related to purchasing strategies and health inequities, observing that, “Differential access to high-quality health care services can create health disparities . These inequities can be rectified by aligning reimbursement strategies to increase access, by expanding the array of services that are reimbursed, and by improving the quality and efficiency of services. Better links between health care and public health activities could increase the effects of health expenditures” (Adler et al., 2016).
In addition, a set of new grant programs sponsored by the Robert Wood Johnson Foundation Data Across Sectors for Health (DASH) programs, the US Office for the National Coordinator Community Health Peer Learning Program, and projects sponsored by the Patient-Centered Outcomes Research Institute, such as the PArTNER grant, seek to improve our understanding of how best to employ consumer-facing technology to collect and use data on life circumstance. Savvy purchasers could leverage the results of these efforts to understand the impact of feedback from consumers on nonclinical factors on health and wellness.
Summary/Conclusions: Paying for Technology–Enabled, Whole–Person Care
Transforming the health system to pay for value rather than volume of care entails complex interactions to implement new Health IT tools, change workflow and current practice patterns (Patterson et al., 2015), and integrate the voice of the patient/consumer. Purchasers and healthcare stakeholders will need to work together to monitor and address feedback from providers and consumers. The goal is see a coevolution of technology, changes in practice patterns and workflow, and quality measurement through continuous adjustment and improvement over time. As purchasers pursue this new model, it will be critical to routinely assess the extent to which VBP programs and their underlying technologies are patient-centered. Pursuing user-centered design principles to develop and test consumer-facing applications with patients and caregivers is equally important.
Finally, development and implementation of robust, validated approaches to measure and monitor consumer experience directly will be important to the entire health care enterprise. Such approaches will have the corollary benefit of promoting price transparency and minimizing information asymmetry for purchasers, providers, and patients alike. Patient portals, PROs, and quality measures that integrate patient feedback into the patient’s electronic record are all promising strategies that leverage consumer health IT. Many of the approaches to integrate patient feedback into ongoing measurement and quality reporting via the EHR are still in their infancy, yet there is reason for optimism as delivery systems such as Kaiser Permanente, Intermountain Healthcare systematize this type of feedback (Snyder & Wu, 2017).
Well-designed payment models that successfully leverage health IT will enable a new perspective on consumer needs and experience. Purchasers stand to gain from these perspectives as they develop VBP programs that appropriately align incentives and approaches to meaningfully improve health care quality and outcomes. Integrating consumer health IT with VBP is a frontier with few successful exemplars to date, yet this is necessary work with a promising future. Ensuring that payment models support consumers to become more active participants in their care is a necessary component of these efforts. Together, consumer health IT and value-based purchasing are critical steps towards sustainably transforming the health system to achieve higher quality and better health outcomes.
References
Adler, J., Saeed, S. A., Eslick, I. S., Provost, L., Margolis, P. A., & Kaplan, H. C. (2016). Appreciating the nuance of daily symptom variation to individualize patient care. eGEMs, 4(1), 1247. https://doi.org/10.13063/2327-9214.1247
Adler, N., Cutler, D.M., Fielding, J, Galea, S., Glymour, M., Koh, H., Satcher, D. (2016). Addressing social determinants of health and health disparities a vital direction for health and health care. National Academy of Medicine, September 2016. Washington, DC.
Adler-Milstein, J., Embi, P., Middleton, B., Sarkar, I. N., & Smith, J. (2017). Crossing the health IT chasm: Considerations and policy recommendations to overcome current challenges and enable value-based care. JAMA, 24, 1–8. https://doi.org/10.1093/jamia/ocx017
Agency for Healthcare Research and Quality (2002). Evaluating the impact of value-based purchasing: A guide for purchaser: A guide for purchasers. Retrieved April 15, 2017, from http://archive.ahrq.gov/professionals/quality-patient-safety/quality-resources/value/valuebased/evalvbp1.html
Bayliss, E. A., Powers, J. D., Ellis, J. L., Barrow, J. C., Strobel, M., & Beck, A. (2016). Applying sequential analytic methods to self-reported information to anticipate care needs. eGEMs, 4(1), 1258. https://doi.org/10.13063/2327-9214.1258
Centers for Medicare and Medicaid Services. (2016a). A Blueprint for the CMS Measures Management System, Version 11.2. Centers for Medicare and Medicaid Services. Retrieved April 15, 2017, from https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/MMS/Downloads/Blueprint112.pdf
Centers for Medicare and Medicaid Services. (2016b). Delivery System Fact Sheet, Consumer-Facing Healthcare Cost and Quality Tools. A Consumer Reports Issue Brief. Retrieved April 15, 2017, from http://nyshealthfoundation.org/uploads/resources/consumer-facing-health-care-cost-quality-tools-consumer-reports-brief.pdf
Centers for Medicare and Medicaid Services. (2016c, January 26). Better care, Smarter spending, Healthier people: Improving our health care delivery system. Retrieved April 15, 2017, from https://www.cms.gov/newsroom/mediareleasedatabase/fact-sheets/2015-fact-sheets-items/2015-01-26.html.
Chenok, K., Teleki, S., SooHoo, N. F., Huddleston, J., & Bozic, K. J. (2015). Collecting patient-reported outcomes: Lessons from the California joint replacement registry. eGEMs, 3(1), 1196. https://doi.org/10.13063/2327-9214.1196
Chesapeake Regional Information System for Our Patients. (n.d.). CQM-Aligned population health reporting. Retrieved May 1, 2017, from https://crisphealth.org/services/cqm-aligned-population-health-reporting-caliphr-tool/
Consumer Reports. Get Safe, Effective Care for a Fair Price. (2016). Consumer Health Choices. Retrieved May 17, 2017, from http://consumerhealthchoices.org/smarter-safer-patients/
District of Columbia Department of Disability Services. (n.d.). Person-centered thinking philosophy. Retrieved April 15, 2017, from https://dds.dc.gov/page/person-centered-thinking-philosophy
Foraker, R. E., Kite, B., Kelley, M. M., Lai, A. M., Roth, C., Lopetegui, M. A., … Payne, P. R. O. (2015). EHR-based visualization tool: Adoption rates, satisfaction, and patient outcomes. eGEMs, 3(2), 1159. https://doi.org/10.13063/2327-9214.1159
Hartzler, A. L., Chaudhuri, S., Fey, B. C., Flum, D. R., & Lavallee, D. (2015). Integrating patient-reported outcomes into spine surgical care through visual dashboards: Lessons learned from human-centered design. eGEMs, 3(2), 1133. https://doi.org/10.13063/2327-9214.1133
Institute of Medicine. (2000). Crossing the quality chasm: A new health system for the 21st century). Washington, DC. Retrieved April 15, 2017, from http://www.nap.edu/books/0309072808/html/
Institute of Medicine. (2003). The future of the public’s health in the 21st century. Washington, DC: The National Academies Press. https://doi.org/10.17226/10548
Irizarry, T., DeVito Dabbs, A., & Curran, C. R. (2015). Patient portals and patient engagement: A state of the science review. Journal of Medical Internet Research, 17(6), e148. https://doi.org/10.2196/jmir.4255
Kaiser Family Foundation. (2016). Kaiser Family Foundation estimates based on the Census Bureau's March 2014, March 2015, and march 2016 current population survey (CPS: Annual Social and Economic Supplements).
Kliff, S. (2015, October 29). I thought people should shop for more healthcare. Then I Tried It.” Vox Media. Retrieved May 10, 2017, from https://www.vox.com/2015/10/19/9567991/health-care-shopping-mri
Lavallee, D., Chenok, K. E., Love, R. M., Petersen, C., Holve, E., Segal, C. D., & Patricia, D. (2016). Franklin, incorporating patient-reported outcomes into health care to engage patients and enhance care. Health Affairs (Millwood), 35(4), 575–582. https://doi.org/10.1377/hlthaff.2015.1362
Lyles, C. R., Allen, J. Y., Poole, D., Tieu, L., Kanter, M. H., & Garrido, T. (2016). “I want to keep the personal relationship with my doctor”: Understanding barriers to portal use among African Americans and Latinos. Journal of Medical Internet Research, 18(10), e263. https://doi.org/10.2196/jmir.5910
Manary, M., Staelin, R, Kosel, K., Schulman, K., & Glickman, S. (2014). Organizational characteristics and patient experiences with hospital care. American Journal of Medical Quality, 30(5), 432–440. doi:https://doi.org/10.1177/1062860614539994.
McGinnis, J. M., Williams-Russo, P., & Knickman, J. R. (2002). The case for more active policy attention to health promotion. Health Affairs (Millwood), 21, 78–93.
McMillan S.S., Kendall E., Sav A., King M.A, Whitty J.A. Kelly F., Wheeler A.J. (2013). Patient-centered approaches to health care: a systematic review of randomized controlled trials. Med Care Res Rev.
Mitchell, A. J., Yadegarfar, M., Gill, J., & Stubbs, B. (2016). Case finding and screening clinical utility of the patient health questionnaire (PHQ-9 and PHQ-2) for depression in primary care: A diagnostic meta-analysis of 40 studies. BJPsych Open, 2(2), 127–138. https://doi.org/10.1192/bjpo.bp.115.001685
National Association of Community Health Centers. (2016). What is PRAPARE? Retrieved May 17, 2017, from http://www.nachc.org/research-and-data/prapare/
National Institutes of Health. (2017). Patient reported outcomes measurement information system (PROMIS). Retrieved May 1, 2015, from http://www.nihpromis.org/measures/availableinstruments
National Quality Forum. (2013). Patient-Reported Outcomes (PROs) in Performance Measurement. Retrieved May 1, 2017, from https://www.qualityforum.org/Publications/2012/12/PatientReported_Outcomes_in_Performance_Measurement.aspx
Patterson, E. S., Lowry, S. Z., Ramaiah, M., Gibbons, M. C., Brick, D., Calco, R., & Ferrer, J. A. (2015). Improving clinical workflow in ambulatory care: Implemented recommendations in an innovation prototype for the Veteran’s health administration. eGEMs, 3(2), 1149. https://doi.org/10.13063/2327-9214.1149
Payne, P. R. O. (2013). Advancing user experience research to facilitate and enable patient-centered research: Current state and future directions. eGEMs, 1(1), 1026. https://doi.org/10.13063/2327-9214.1026
Revere, D., Dixon, B. E., Hills, R., Williams, J. L., & Grannis, S. J. (2014). Leveraging health information exchange to improve population health reporting processes: Lessons in using a collaborative-participatory design process. EGEMS, 2(3), 1082. https://doi.org/10.13063/2327-9214.1082
Rolfson, O., Wissig, S., van Maasakkers, L., Stowell, C., Ackerman, I., Ayers, D., & Franklin, P. D. (2016). Defining an international standard set of outcome measures for patients with hip or knee osteoarthritis: Consensus of the international consortium for health outcomes measurement hip and knee osteoarthritis working group. Arthritis Care & Research, 68(11), 1631–1639. https://doi.org/10.1002/acr.22868
Rybowski, M, Eichler R. (1997). Theory and reality of value-based purchasing: Lessons from the pioneers. Rockville, MD: Agency for Health Care Policy and Research. AHCPR Publication No. 98–0004.
Seeking Alpha. (2014, March 18). U.S. IPO recap: Castlight Health's 149% pop shows healthy tech demand. Retrieved May 15, 2017, from https://seekingalpha.com/article/2094893-u-s-ipo-recap-castlight-healths-149-percent-pop-shows-healthy-tech-demand
Snyder, C., Wu, A (Eds). (2017). Users guide to integrating patient reported outcomes in electronic health records. Patient Centered Outcomes Research Institute.
Sorondo, B., Allen, A., Bayleran, J., Doore, S., Fathima, S., Sabbagh, I., & Newcomb, L. (2016). Using a patient portal to transmit patient reported health information into the electronic record: Workflow implications and user experience. eGEMs, 4(3), 1237. https://doi.org/10.13063/2327-9214.1237
Spencer, A., Freda, B, McGinnis, T, Gottleib, L. (2016, December). Measuring social determinants of health among medicaid beneficiaries: Early state lessons. Center for Health Care Strategies. Retrieved May 3, 2017, from http://www.chcs.org/media/CHCS-SDOH-Measures-Brief_120716_FINAL.pdf
The Health Foundation. (2014). Helping measure person-centred care. Evidence Review. Retrieved April 15, 2017, from http://www.health.org.uk/sites/health/files/HelpingMteasurePersonCentredCare.pdf
Wilcox, A. B.; Gallagher, K.; and Bakken, S. (2013). Security approaches in using tablet computers for primary data collection in clinical research. eGEMs, 1(1), 7. doi: https://doi.org/10.13063/2327-9214.1008.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Holve, E. (2019). Leveraging Consumer Health IT to Incentivize Engagement and Shared Accountability in Value-Based Purchasing. In: Edmunds, M., Hass, C., Holve, E. (eds) Consumer Informatics and Digital Health. Springer, Cham. https://doi.org/10.1007/978-3-319-96906-0_15
Download citation
DOI: https://doi.org/10.1007/978-3-319-96906-0_15
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-96904-6
Online ISBN: 978-3-319-96906-0
eBook Packages: MedicineMedicine (R0)