Abstract
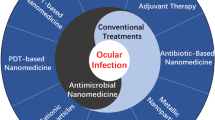
Microbial keratitis has long been associated with the activity of pathogenic microorganisms such as bacteria, fungi, parasites, and viruses, causing corneal epithelium disorder, decreased corneal material, and potential loss of vision. In fact, the ocular barriers have two contradictory roles during the infection pathway: the first involves protection of the eye from pathogens, while the second is involved in the obstruction of drug bioavailability. Here, we introduce a comprehensive overview of microbial keratitis as a world-wide concern and study some aspects of the mechanisms of microbial infection. We also review the role of the eye’s natural defenses toward pathogens. More importantly, we highlight the potential of nanoparticles as therapy against increased multi-drug resistant microbes and the ability of these treatments to achieve drug bioavailability. Hence, nano-therapy provides a promising treatment for microbial keratitis in the future.
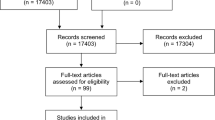
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Microbial keratitis
- Eye defenses
- Immune response
- Organic nanoparticles
- Metal nanoparticles
- Nanomedicine
- Cornea
- Drug delivery
- Infection
Introduction
Ocular illnesses are common all over the world, and sometimes they can reach an epidemic degree. Eye infections such as keratitis, ulceration, conjunctivitis, blepharitis, and dacryocystitis can cause damage to eye structures, decreased vision, reduced corneal transparency, scarring, and even blindness if not treated promptly [1].
Corneal ulceration is a pathological condition indicative of a disorder of the epithelium and lack of material in the cornea [2, 3]. It is a common ocular disease and the second most common cause of blindness (after cataracts) in non-industrialized poor countries [4]. This disease has several distinctive characteristics, such as purulent infiltration; formation of stromal pus; inflammation of the anterior segment; and eventually corneal tissue damage, beginning with the epithelial layer and leading to the stroma [5, 6]. Corneal ulceration can occur as a result of exogenous injuries such as chemical wounds, physical trauma, contact lens (CL) use, and the ‘dry eye phenomenon,’ or it can be because of endogenous infections such as microbial infections (bacteria, fungi, parasites, and viruses) [3, 6, 7].
In general, keratitis can be categorized according to location, severity, and reason for ulceration, including superficial punctate keratitis that leads to cell death, which is located on the surface of the cornea; interstitial keratitis (stromal keratitis) that affects the stroma of the cornea (deeper layers) and results from infections and immune responses; herpes simplex viral keratitis where the herpes virus is responsible for the occurrence of infection through sexual transmission; traumatic keratitis, which occurs after scarring caused by a corneal wound; and keratoconjunctivitis resulting from an infection on the cornea and the conjunctiva at the same time [8, 9].
The ability of microorganisms to invade and damage corneal tissues or cells depends on virulence factors and resistance of the host defense mechanisms [10]. The eye has strong defense barriers, including the tear film, corneal tissue feature, and immune responses, but these barriers may fail to address the factors causing the disease [11]. Therefore, immediate diagnosis, detection of the causative agent of the disease, and good management are important keys for the control of keratitis and corneal fibrosis [9, 12]. In attempting to find a target therapy, we have seen the evolution of different treatments for different types of keratitis, especially microbial keratitis. A therapeutic approach has recently emerged based on drug delivery using nano carriers. These nano carrier formulations not only increase the drug residence time and reduce the frequency of administration, they can also improve drug stability and bioavailability by surpassing the eye barriers and improving the therapeutic outcome of the drug [13]. One of the most interesting aspects of this treatment is the use of a nanoformulation either alone or combined with other drugs as an anti-microbial agent to fight corneal infections [14, 15]. In this respect, nanomedicine is a promising future solution to diagnose, manage, and treat eye diseases.
Microbial Keratitis
Microbial keratitis is one of the five most frequent causes of loss of eyesight in the world [16]. This inflammation occurs in the cornea as a result of various types of pathogenic microorganisms, including bacteria, fungus, viruses, and parasites. Notably, it is associated with a series of distinctive symptoms such as aches, blurred vision, redness, photophobia, frank opacity within the cornea, and rupture or discharge in serious cases [4, 9]. However, it is often difficult to differentiate between the various types of microbial keratitis because of the similarity of the disease symptoms [17].
In fact, microbial keratitis can cause changes in and damage to the corneal shape and structure, reduced vision, and transparency, and corneal scarring may also accompany healing even after pathogens are eliminated by antibiotics [1, 16]. Injuries, CLs, and chronic disease or compromised immune systems are considered the main risk factors for microbial keratitis [18,19,20].
Undoubtedly, the cornea is the most exposed part of the eye to the external environment. This can contribute to increased cases of corneal contamination with a microbial source [7]. Farming activities, handwork, and domestic services can give rise to increased contact or contamination with pathogens. Increased cases of microbial keratitis have been observed in agricultural communities, especially in rural areas afflicted with poverty and a lower standard of living. For instance, the percentage of keratitis cases in Nepal and India are 10 times higher than in the USA. Also, climate conditions, including temperature and humidity, can contribute to an increase in corneal pathogen infections [16]. Furthermore, differing ratios and severity of corneal infection cases in various areas in the world may be as a result of the epidemiology of the microbe. Hence, diagnosis of microbial keratitis depends on the pathogen type, and this is considered the essential key to control of microbial keratitis [9, 12].
Bacterial Keratitis
A bacterium is one of the most common pathogenic microorganisms to be implicated in several ocular diseases such as bacterial keratitis, corneal ulcer and abscess formation, and conjunctival congestion, and eventually may lead to corneal scarring, haze, or blindness [6]. It should be noted that Gram-negative bacteria (e.g., Pseudomonas aeruginosa and Chlamydia trachomatis) and Gram-positive bacteria (e.g., Staphylococcus aureus and Streptococcus pneumoniae) are the most virulent causes of keratitis [21, 22].
External sources (injuries, contact lenses, burns, etc.) and internal agents (diabetes, age, etc.) are the main causes of bacterial keratitis [3, 6, 7].This has been confirmed by several studies, including a study conducted in Indonesia that found the main reason for the occurrence of bacterial keratitis was trauma, with an incidence of 74.7%, followed by chronic eyesight disorder, contact lens, and corneal surgery, with 12.1%, 4%, and 2%, respectively [6]. Also, results of an Indian study showed agreement with these findings with most cases of bacterial infection resulting from mechanical trauma at 72.4%, whereas ocular disorder cases were implicated in 9.2% [23]. Furthermore, 38% were from corneal trauma, 29% from blepharitis, and 20% from contaminated pharmaceutical procedures [19].
Contact lenses can also cause microbial keratitis through bacterial contamination and increased chronic hypoxic stress (lack of oxygen) on the corneal epithelial layer, especially when lenses are used while sleeping [24]. This leads to reduced corneal sensitivity , decreased epithelial mitosis and adhesion, early epithelial desquamation, and weakness and thinning of the epithelial cells, which negatively affects the integrity of the cornea [8]. A study at the Jules Gonin Eye Hospital at the University of Lausanne in Switzerland showed that wearing contact lenses increased the incidence of bacterial keratitis by 36% and blepharitis by 21%, while wearing contact lenses increased corneal trauma by 20% [25].
The corneal epithelium is a formidable barrier against the spread of bacteria in the deep layers of the stroma because of the narrow space between superficial cells, various defense mechanisms such as innate and acquired immunity, and washing the eye with tear fluid [20, 26]. Bacterial keratitis occurs as a result of the discontinuity of the corneal epithelial layer or a disorder of the tear fluid system. Consequently, different types of pathogenic bacteria may enter the stroma, which consists of collagen types that have weak resistance against leukocyte enzymes and bacteria. After that, the epithelium and corneal stroma swell and are exposed to the necrosis process causing increased bacterial reproduction, inflammation, and partial or total ulceration at the wound site. This increases the possibility of corneal scarring [9].
Interestingly, the collapse of the corneal barrier helps the adhesion of bacteria to the corneal cell surface, which is the first step in creating the infection, and this adhesion often occurs between the host cell receptors and the pathogenic microorganism’s receptors. For instance, during infection, the adhesion process with Pseudomonas aeruginosa occurs by binding of the flagellum of the bacteria and the mucin on the host corneal epithelial cells [27]. Also, components of the extracellular matrix (ECM) such as laminin, fibronectin, and collagen can assist pathogens in adhesion, stimulation of inflammatory responses, colonization, and occupation of host tissue [28].
During the infection stages, the inflammatory response plays a controversial role. It has been observed that the T helper-1 (Th-1) leads to acute corneal necrosis, while Th-2 plays a positive role in reducing infection without corrosion . Both are responsible for inducing antibody production during the infection phase [29]. Notably, the severity of keratitis (mild, moderate, and acute) depends on the corneal situation and pathogen type [9].
In Gram-negative bacteria, the cell wall of the bacterium contains lipopolysaccharides (LPS) as a virulence factor, which stimulate secretion of different cytokines produced by inflammatory cells. Tear fluid also helps LPS to penetrate into the corneal tissues during an injury [30]. One study revealed that the LPS of Pseudomonas aeruginosa can induce production of tumor necrosis factor-alpha (TNF-α), macrophage inflammatory peptide 2 (MIP-2), and interleukin-1beta (IL-1β), and reduce IL-10 in a corneal mouse model. Thus, dysregulation of cytokines provides nutrients for bacterial growth, enhancing corneal damage and aggravating the disease [31]. Moreover, several studies have reported that the role of LPS in Pseudomonas aeruginosa was to stimulate the expression of toll-like receptors-4/5 (TLR-4/5). These receptors are present on corneal macrophages and have the ability to induce transcription of chemokines such as KC/CXCL1, and cytokines such as IL-1α and IL-1β. It has been observed in cases of corneal ulcers that there is an increased expression of TLR2, TLR4, TLR5, and TLR9, as well as Nod-like receptor type NLRP3 and NLRC4 inflammasomes [29, 32].
Gram-positive bacteria are no less dangerous than Gram-negative bacteria. For instance, Staphylococcus aureus can stimulate the expression of different pro-inflammatory cytokines like TNF-α, interleukin (IL-1β, IL-6, IL-8, and IL-12), MIP-2, and interferon-γ (IFN-γ), causing corneal inflammation in mouse models [33]. In brief, over 24–48 h after exposure to bacteria with strong virulence factors, the infection may develop rapidly and impact one or both eyes, leading to complete corneal damage if left untreated [9] (Fig. 10.1).
The mechanism of bacterial keratitis. (A) The basic structure of Pseudomonas aeruginosa. (B) Three layers of the tear film that protect the eye surface. (C) The adhesion between bacterial flagella and corneal mucin layer. (D) The role of lipopolysaccharide, which is located in the outer membrane of Gram-positive bacteria to induce an inflammatory response by T-helper cells (Th-1, Th-2) and Toll-like receptors (TLRs), in order to increase necrosis and damage the corneal epithelium. (E) The inflammatory response causes stimulation of chemokines, pro-inflammatory cytokines and the necrosis process, while reducing apoptosis, and eventually the invading bacteria reach the stroma layer. (F) The occurrence of bacterial keratitis cases because of increased division and proliferation of bacteria in the corneal stroma
Fungal Keratitis
Fungal (mycotic) keratitis is one of the most common types of keratitis in the world, especially in tropical regions. On a global level, many studies have shown that fungal keratitis prevalence in South India, Ghana, Bangladesh, South Florida, and Nepal is 44%, 37.6%, 36%, 35%, and 17%, respectively [34]. Several reports in India have shown that the proportion of mycotic keratitis cases was 36.7% in South, 36.3% in Western, 25.6% in North-Eastern, and 7.3% in Northern India [35]. In China, it has also been observed that there has been an increased rate of mycotic keratitis infection in the past decade. In contrast, fungal keratitis infection rates remain very low in Britain and Northern USA [34]. This was confirmed by a study at the University of Texas Southwestern (UTSW), which showed that the infection rate of fungal keratitis was low at 15% compared with the infection rate of 85% for bacterial keratitis [36].
Trauma, compromised immune systems, climate conditions , overpopulation, and frequent long-term use of antibiotics such as steroids, corticosteroids, etc. are the major factors exposing the eye to infection by different types of fungi [35]. There are more than 70 types of fungi that can cause fungal keratitis, but the most common of these are Candida spp., Aspergillus spp., and Fusarium spp. [37]. Some studies in India showed that different types of fungi cause corneal infection at various rates. It was found that the major fungal isolates were 27.9% Aspergillus spp. and 23.2% Fusarium spp. in Eastern India [35]. In the Kumaon region, Uttarakhand (India), pathogenic fungi led to keratitis cases by 57.6% Aspergillus spp., 33.3% Fusarium spp., 6.1% Penicillium spp., and 3.03% Candida spp. [23]. Fusarium spp., Aspergillus spp., Penicillium spp., and Candida spp. were the most common in South Kerala, with incidences of 37.1%, 26.3%, 20.1%, and 1.8%, respectively [38]. Additionally, the proportion of fungal keratitis caused by Fusarium spp. was 48.3% and by Aspergillus spp. was 27.6% in the western part of Uttar Pradesh [4]. Although fungal keratitis cases are low in advanced countries, it was found that Candida albicans (48%), Fusarium solani (10%), and Aspergillus fumigatus (7%) were the causal fungi in fungal keratitis in New York [39]. Also, a study in the UK found that fungal keratitis was caused by yeast in 57.5% of cases and filamentary fungi in 42.5% [40]. Generally, there are two important groups in medicine that associated with corneal infection are filamentous fungi and yeast. Fungal keratitis such as Candida and Aspergillus keratitis are occurring in individuals who are suffering from immunocompromised. Aspergillus species such as Aspergillus fumigatus, Aspergillus flavus, and Aspergillus niger, and Fusarium species are responsible for one-third cases of traumatic infectious keratitis [4].
Fungal keratitis occurs when the fungus invades the surface of the cornea. Innate immune cells begin to identify the etiology by pattern-recognition receptors (PRRs), especially type C lectin receptors (CLRs). It has been recently revealed that Dectin-1 in the cornea determines the identity of the attacking fungi [41]. Generally, a PRR-mediated inflammatory response promotes elimination of fungi and repair of corneal tissue, and determines Toll-like receptor types TLR2 and TLR4 [29].
TLRs are the major elements of the innate immune response that are indispensable in selecting fungal zymosan and mannan, and release host defense responses [42]. Also, TLRs play a crucial role in keeping the cornea healthy and transparent by controlling the neutrophil infiltration and expression of IL-1β, IL-6, IL-12, and TNF-α, as well as monocyte chemoattractant protein type MCP1/CCL2 and MIP-2/CXCL2 [29, 32]. Therefore, decreased TLRs can lead to exacerbation of infection by pathogenic fungi, while over-activation of TLRs gives rise to increased inflammation, tissue injury, and even corneal necrosis. In this situation , the clinical prognosis relies on pathogen virulence and host immune response in order to protect the cornea and prevent scarring [4, 32] (Fig. 10.2).
Corneal injury with fungal keratitis. (A) The shape of Candida albicans. (B) Attack of the fungus on the infected corneal surface with scratch. (C) Innate immune cells of the cornea begin to identify fungi and attack mechanisms by pattern-recognition receptors (PRRs) include C lectin (CLRs) and Dectin-1 receptors. (D) TLRs are responsible for determining fungal zymosan and mannan, maintain control of neutrophil infiltration and expression of cytokines (IL-1β, IL-6, IL-12, and TNF-α) and monocyte chemoattractant proteins (MCP-1/CCL2 and MIP-2/CXCL2). The immune response is crucial for the eradication or prevalence of keratitis
Parasitic Keratitis
The most common parasites causing keratitis are Acanthamoeba spp., Mirosporidia spp., and Onchocerca volvulus. Less common parasites that impact the cornea are Mansonella ozzardi, Leishmania spp., Gnathostoma spp., and Thelazia spp. [8]. Another causal parasite is Acanthamoeba species, which includes Acanthamoeba castellanii, A. polyphaga, A. culbertsoni, A. hatchetti, A. lugdunensis, A. palestinensis, A. rhysodes, A. quina, and A. griffin, all free-living protozoa in habitats such as water and moist soil [8, 43, 44]. The life cycle of Acanthamoeba species has several characteristics including effective movement, nutrition, and partition into two phases: trophozoite and cyst with a double cyst wall. The cyst phase provides Acanthamoeba spp. with high resistance to extreme conditions , drying, antibiotics, and sterilization materials such as chlorine [44]. In Acanthamoeba keratitis cases, there were increased numbers of Acanthamoeba trophozoites in the anterior stroma, while the cysts were more common in the deeper layers of stroma with a lower inflammatory response. The main symptoms that can appear in patients with parasitic keratitis include eye ache, redness, reduced vision, light sensitivity, explicit opacity within the cornea, stromal infiltrate, and repeated disintegration of the epithelial layer [8, 45].
It has been observed that the incidence of parasite ocular infection is increasing globally [17]. Generally, the infection occurs because of polluted water and minor trauma involving soil, especially in regions with poor economic and social conditions and in conjunction with cases of human immunodeficiency virus (HIV) [46]. One of the more prominent Acanthamoeba characteristics is the ability to adhere to contact lenses. This adhesion depends on several factors, including contact lens manufacture materials and sterilization solutions, the concentration of Acanthamoeba, exposure period, and life phase of protozoon [24]. It was noted in developed countries such as the USA that during 2003–2008, levels of Acanthamoeba keratitis increased fourfold, and this was related to the high use of contact lenses [47]. Hence, the use of contact lenses in conjunction with poor hygiene is a risk factor leading to increased rates of ocular inflammation with Acanthamoeba parasites, increasing from 62.5% to 95% [8]. Although the corneal epithelium is an important barrier against the invasion of the parasite , the use of contact lenses can cause small scratches on the cornea, which are essential for entry of Acanthamoeba.
Corneal scratches lead to increased expression of mannose glycoproteins in the epithelial layer and consequent development of Acanthamoeba keratitis [8]. Acanthamoeba has the ability to selectively associate with mannose saccharides instead of non-mannosylated neoglycoproteins such as galactose, lactose, fucose, and galactosamine. The binding between mannose-binding protein (MBP) as a transmembrane protein on the typical Acanthamoebae surface cell and mannose receptors can assist Acanthamoeba to invade corneal stroma and induce Acanthamoeba to produce the pathogenic protease enzymes [8, 47]. This happens via a complex series of events that involves the production of various enzymes such as collagenases and proteases [24]. These enzymes can cause basement membrane damage, stimulating cytolysis, enhancing the apoptosis process of corneal cellular elements, and increasing novel Acanthamoeba plasminogen activator (aPA) and inflammatory cytokines such as macrophage inflammatory proteins (MIPs), especially MIP133. In turn, MIP133 can give rise to different types of matrix metalloproteinases (MMPs) such as MMP1, MMP3, and MIP9 that have an important role in corneal fibrosis and corneal neovascularization. Consequently, penetration of proteases and collagenases into the stroma of the cornea and down to the deeper layers can lead to lysis of the collagen in the corneal stroma [8, 47, 48].
Generally, Acanthamoeba keratitis causes many histological changes such as ulceration of the corneal epithelium, lack of keratocytes in the stroma, and infection in two-thirds of the stroma with necrosis [8], which requires rapid therapeutic intervention to avoid losing sight [43] (Fig. 10.3).
The process of Acanthamoeba spp. keratitis (AK) . (A) The structure of Acanthamoeba spp. (B) The binding between mannose glycoproteins on the corneal epithelium and mannose receptors (MBP) on the surface of Acanthamoeba spp. (C) Acanthamoeba spp. releases protease and collagenase enzymes (virulence factor) to enhance destruction of the host (corneal layers). (D) Protease and collagenase enzymes lead to stimulating inflammatory cytokines, damaging the basement membrane, increasing apoptosis and cytolysis, and penetrate to the deep corneal stroma layer by lysis of the collagen. (E) Transformation of Acanthamoeba spp. from the trophozoite phase to the cyst phase and stability in the deep layer of the stroma causing AK
Viral Keratitis
Viral keratitis is a disease that results in reduced vision or blindness in developed countries such as the USA [49,50,51]. Rubeola virus and Vaccinia virus have been implicated in viral keratitis cases [52], but the Herpes simplex virus (HSV) has been considered the most common cause of this optical disease [49, 53]. Globally, HSV leads to 1.5 million cases of Herpes simplex keratitis, including 40,000 severe cases of weak or lost vision every year [49]. A study in the USA has confirmed that 90% of adults have a positive serum to the herpes virus and about 500,000 cases of ocular herpes simplex infection are active annually [54].
There are two important kinds of Herpes simplex virus (type 1 and 2), which have oversized and double-stranded DNA [55]. In particular, HSV-1 is a pathogen implicated in dangerous cases of eye inflammation . However, HSV-2 can also negatively affect the eye, especially in newborns [51]. The main feature of viral keratitis is chronic and frequent ocular inflammation [56]. This may be due to the ability of the virus to disappear from the host’s defenses causing frequent infection and irreversible corneal tissue damage [29]. Generally, Herpes simplex keratitis can cause harm in the anterior and posterior eye segments, and is most widespread in the cornea (dendritic ulcer ). Thereby, HSV may impact on any or all corneal layers with a recurrence of disease in 20–48% of cases, which can lead to corneal neovascularization (CNV) and corneal scarring [54].
Several factors can contribute to the development of herpetic stromal keratitis; some of these agents are well-known such as diabetes and auto-immune deficiency syndrome (AIDS), and others are still unclear or under study. In this sense, this disease has opportunistic properties [55]. Corneal infection starts after the inflammation of mucous membranes. This inflammation is caused by HSV-1 through the initial adhesion between the glycoprotein receptor type B and/or C of virus and heparan sulfate proteoglycan (HSPG) receptors of the corneal surface (host cell). This is followed by the secondary adhesion, which includes a series of interactions between virus receptors type GD, GH, GL, and GB, and the GD receptor on the cornea. This leads to the virus entering the host cell by fusion of the virion envelope with the membrane of an intracellular vesicle or the plasma membrane. After that, many processes occur, including releasing viral DNA and replicating in the nucleus, virus prevalence, inflammation, and apoptosis [57].
During infection, the infected and non-infected corneal epithelial cells enlist several leukocytes into the corneal stroma such as neutrophils, polymorphonuclear leukocytes (PMN), macrophages, dendritic cells, natural killer cells (NKs), and T-cells in order to induce an immune response. In extreme immune responses, release of some antagonist receptors such as IL-1 and TGF-B occurs, which are considered to be factors involved in immunosuppression, thus decreasing corneal neovascularization, and reducing inflammation. In contrast, some cytokines can be released, such as IL-2 and an antigen-presenting cell (APC), causing a negative impact on the corneal stroma by developing HSK cases. Consequently, the immune response has two contradictory roles: one that improves the corneal health and one causing damage [29] (Fig. 10.4).
The interactions of keratitis with Herpes simplex virus (HSV) . (A) The most important components of the Herpes simplex virus. (B) The initial adhesion between virus glycoprotein receptors type B (GB) or/and C (GC) and heparan sulfate proteoglycan receptors (HSPGs) on corneal epithelium. (C) In order to release virus from nucleocapsid and tegument to the host cytoplasm through membrane fusion (Lipid Bilayer Envelope), interaction between virus receptors (GD, GH, GL, and GB) and corneal receptors (GD) is required. (D) During the membrane fusion process, destruction of the corneal surface occurs with the increase in pro-inflammatory cells and cytokines, and the virus invasion continues into the deep stromal layers. Immunosuppressive factors can play a role in the immunology response. (E) Replication DNA and the prevalence of a virus allow for an increase in herpetic stromal keratitis cases
The Eye Defense Mechanisms
Tear Fluid
Tear fluid is a thin aquatic layer that covers the ocular surface. It is produced by the lacrimal gland located in the orbit over the lateral end of each eye and is also secreted from various tissues situated around the eye surface [58]. The tear fluid has many functions that are vital in the optical system. These functions include lubrication of the ocular surface, nutrition, providing growth factors to the corneal epithelium, a protective barrier against pathogens and the outside environment, and a refractive surface maintaining the ideal vision [59].
It is worth mentioning that the tear film is not a homogeneous entity and is divided into three distinct layers. The first layer is mucin , which is directly adjacent to the corneal surface with a thickness of 2.5–5 μm. It consists mostly of sugar-rich glycosylated proteins that are produced by epithelial cells and anchor to the epithelium. The gelatinous structure of the mucin maintains the wet surface easily and thereby contributes to the distribution of water after blinking [60, 61].
The second layer is an aqueous layer with a thickness of 4 μm. Lacrimal glands are responsible for secreting this layer. The main functions of the aqueous layer are preventing dehydration of the ocular surface, eliminating pathogens, protectection from pollution, as well as supplying nutrition to the cornea [60]. This layer is not a pure aqueous solution, but contains soluble and insoluble components , such as peptides, proteins, and electrolytes. The majority of proteins in tear fluid are lactoferrin, serum albumin, lipophilin, secretory immunoglobin A (IgG and IgA), beta-lysin, and the most abundant lysozyme and lipocalin [59]. Interestingly, the high availability of lysozyme in tear fluid is justified because lysozyme can inhibit microbial activity (antimicrobial) as a defense barrier by decomposing bacterial cell walls. Also, IgG and IgA in tear fluid neutralize some types of viruses and binding bacteria. This can reduce the microbe numbers in the tear film [11, 59, 62]. The change in the concentration of different proteins in the tear fluid reflects a normal or diseased case. The analysis of tear fluid with electrophoresis and chromatography has shown that diabetic patients have different patterns of tear protein compared to non-diabetic individuals [59].
The third layer of tear fluid is the lipid layer, which is relatively thin (0.015–0.160 μm) [63]. It is the outer layer of the tear fluid that has direct contact with the external environment. The lipid layer is secreted by small glands known as meibomian glands. These glands are located within the tarsal plates with many openings at the edge of the eyelids. This layer has several functions, such as decreasing surface tension of the tear film, reducing water evaporation, preventing the tear fluid from spilling over to the lid margins, and an antimicrobial function. Recent studies have shown that a deficiency of the tear fluid lipid layer is associated with the ‘dry eye syndrome’ [60]. Dry eye syndrome is defined as a multifactorial disease and is due to a disorder or unstable production of tear fluid, causing several symptoms such as increased discomfort and potential microbial infection, ocular surface harm , and vision disruption [64]. Hence, tear fluid promotes the protection of the cornea as the first line of defense against the external environment.
Corneal Tissue
The cornea is an effective shield against external factors. The corneal epithelium is the first layer of the cornea, and consists of five to seven layers of cells. It is strongly associated with the stroma. In brief, corneal epithelium includes the basal layer, which is the deepest layer and consists of columnar cells. This is followed by the wing layer that contains two or three layers and involves polyhedral cells (mostly prickle cells). Finally, the squamous layer (superficial layer) contains three or four layers (stratified squamous cells) with flattened nuclei. In the superficial layer, the tight junctions are considered an important feature that obstructs the entry or progress of microbes to the stromal tissue [65].
Epithelial cells can secrete various cytokines to stimulate ocular immune defenses to eliminate pathogens. It has been observed that interleukin-1α (IL-1α) is released from corneal epithelial cells after exposure to infectious factors or trauma [11]. In contrast, the excessive secretion of IL-1α may promote microbial invasion, corneal neovascularization, and corneal tissue damage. However, corneal epithelial cells are capable of modifying the excessive secretion of IL-1α by producing IL-1RII (gene therapy), which is the natural antagonist of IL-1α [66, 67]. Hence, corneal epithelial cells contribute to a reduction of leukocyte infiltration, changing the cytokine profile selectively, inhibiting corneal neovascularization cases, and maintaining optimal vision [11].
Corneal stroma also has a defensive capacity against germ invasion. Keratocytes exist within the stromal layer and can limit microbial activity (antimicrobial) and enhance corneal wound healing. This occurs through synthesizing interleukin type IL-6 under the effect of IL-1α and tumor necrosis factor-alpha (TNF-α)) [11, 68]. The interaction between IL-6 with IL-1α and TNF-α acts as a therapy against microbial keratitis. Furthermore, keratocytes play a role in attracting neutrophil cells located in the conjunctiva. It has been shown that the expression of IL-8 resulting from keratocytes , is considered to be a chemoattractant agent for neutrophils in HSV keratitis cases. Conversely, IL-8 is completely absent in the corneal epithelial layer in cases of herpes infection [11, 68, 69].
In addition, corneal nerves play a fundamental role in innate defense by delivering sensory information, which in turn supports the ocular protection process as reflexive movements such as tear production, secretions, and wound healing [70]. The release of neuropeptides is essential after sensations such as pain and discomfort in order to stimulate the activity of cytokines [11]. Under the pain response, two types of neuropeptides are produced from sensory corneal neurons: calcitonin gene-related peptide and substance peptide. Both neuropeptides induce an immune response to repel microbial invasion [71, 72]. All of the above demonstrates the vital role of the corneal tissue as a potent barrier against microbial activity.
Immune Response
The immune response plays a key role in corneal protection during exposure to various injuries. The immune response includes innate and acquired immunity, and each has a defensive stage. The innate immune response is related to the early defense stage, while the acquired immune response is associated with the late stage of defense [11].
The early defense stage begins after a few minutes to several hours to eliminate pathogens [73]. During this stage, the innate immune response dominates through releasing various defenses. Interferons (IFNs) are a group of defense proteins also known as cytokines that have a role against microbial attacks. These cytokines consist of several types, including IFN-α, IFN-β, and IFN-ɤ. Notably, IFN-α and IFN-β are secreted by leukocytes and fibroblasts, respectively, while IFN-ɤ is released by T-cells and natural killer (NK) cells [74]. The main interferon functions in the innate immune response are promoting the capacity of infected cells to produce required proteins for T-cells in order to limit microbial activity. This process occurs by stimulating the expression of major histocompatibility complex class-I molecules (MHC-1) and proteins . Additionally, the activated NK cells use IFN-α and IFN-β to target and eliminate microbes [11].
Immune cells have a critical role in the innate immune response. Neutrophils are one type of these cells and exist in the cornea normally. Neutrophil cells are responsible for protecting the ocular surface by phagocytosis and killing pathogenic microorganisms during the invasion. Neutrophil extravasation, also called diapedesis, refers to neutrophil movement out of the circulatory system toward damaged tissue or the infection site. In the cornea, this process occurs by moving neutrophils in the limbal vasculature endothelial cells through the adhesion with receptors located on vascular endothelial cells [73, 75]. Also, eosinophil cells have immunoglobulin-E (IgE) receptors on the surface and the complementary components, which in turn provide protection against parasites. Therefore, it is assumed that eosinophil activation is necessary for parasitic toxicity as part of the innate immune response [11]. Furthermore, macrophage cells play a fundamental role against microbial infection during the innate immune response, including phagocytosis, antigen-presenting capability, release of inflammatory cytokines, and modulating effects on T-cell [65]. It has been confirmed recently that macrophage cells are located in the conjunctiva and corneal stroma in mouse models [11]. In addition, NK cells are large granular lymphocytes that no antigen receptors on the surface. NK cells are capable of recognizing MHC class-I molecules and can lysis the target cells, which have small amounts of these molecules, such as tumor cells, virally infected cells, and undifferentiated cells [76, 77].
In contrast, the microbial infection may overwhelm the first defense and thus the efforts of the innate immune system may fail. For instance, a bacterium has the ability to replicate in 1 h, and it reaches 2 million organisms after 24 h, thus overwhelming the initial immune defenses. This leads to the second defense stage, known as acquired immunity, being stimulated, which can occur from 24 h to 48 h after initial infection, and the full response may take days [11].
When the body recognizes the non-self-antigen during acquired immunity, the Langerhans cells are already working on processing the foreign antigen and transferring it by MHC (class-l or class-ll) to the corneal surface [78]. Then, T-cells are stimulated through displaying the non-self-antigen on the MHC molecule by linking to the T-cell receptor, eventually leading to maturation of the T-cell to CD4+ or CD8+ depending on the class of MHC molecules, i.e., I or II, respectively. Thus, T-cells have two main functions: killing the external antigens (CD8 + −cytotoxic cells) or releasing cytokines (CD4+ T-helper cells) to bring effector cells. The most common effector cell is the macrophage that destroys microbes and stimulates inflammatory cells. Hence, in ocular diseases, the interrelationship between the innate and acquired immune systems is very important in cases of acute and chronic inflammatory responses [79, 80].
Nanoparticles for Use Against Ophthalmic Pathogens
In spite of the enormous development that the world has witnessed in the antimicrobial field since 1960, multiple infectious diseases remain a big challenge with regard to therapy [81].
In ophthalmology, topical application of medicine is considered the most popular approach [82]. However, this method has several limitations. The eye’s protection mechanisms (including the blink reflex, secretion from the lacrimal gland, and the structure of the corneal tissues) are highly efficient in preventing drug permeability and achievement of the desired treatment concentration at the target site [83]. Also, several antimicrobial compounds have difficulty passing through cell membranes. As these compounds have limited effectiveness within the cells, they have a weak impact on microbial activity. Thus, antibiotics may fail to eliminate pathogens, resulting in severe consequences and progression along the infection path from the fusion stage with early phagosomes, late endosomes, or with lysosomes (the pathogen elimination stage) to disease proliferation stage and chronic infection [81].
Furthermore, the evolution of microbial resistance to various antibiotics has made this an important global health issue. In addition, eye barriers and microbial resistance have led to the use of high doses of antibiotics , which can give rise to the generation of intolerable toxicity in healthy tissues [10].
Within this scenario, there are many pharmaceutical strategies such as gels, ointments, and viscous solutions that have been used with a view to enhancing and increasing bioavailability of traditional treatments on the ocular surface, but these strategies are not the best solution to overcome traditional therapy limitations [84]. Consequently, there is a need to design a new therapeutic approach that adopts the following principles: The first principle aims to achieve the ability to penetrate the corneal barriers, prolong the time on the eye surface with high bioavailability, and target the parts that harbor microbes. The second principle aims to overcome pathogen defenses [81, 82].
There is enough experimental evidence to show that nanoparticles have several unique physico-chemical and biological properties, including a small size on the nanometer scale, high permeability, increased surface area-to-volume ratio, a large capacity to deliver the drug, and lower toxicity in the cellular environment. Importantly, multiple ligands such as deoxyribonucleic acid (DNA), peptides, antibodies, molecular sensors, and therapeutic molecules can be transported to target sites by being loaded onto nanoparticles [85]. Recent studies show that the use of nanotechnology in ophthalmology applications can play a key role in passing through the ocular physical barriers, including the cornea, conjunctiva, sclera, and blood-retinal barriers [86, 87]. It has been recently shown that nanoparticles are a promising approach to treatment of a broad range of pathogenic microorganisms [81].
In brief, the small size of nanoparticles allows for easy penetration of the microbial cell membrane and exertion of antimicrobial activity, which includes limiting replication of DNA, obstructing cellular proteins, as well as the interaction between nanoparticles and the microbial membrane causing change and damage to the membrane structure, and, eventually, death of the pathogen [88, 89] (Fig. 10.5). However, these mechanisms are still under study and need further investigation.
Permeability of nanoparticles via the ocular barriers and their role to eliminate pathogens. Nanoparticles have the ability to overcome the corneal barriers (tear fluid and corneal tissue), reaching the microbe. Nanoparticles can easily penetrate microbial cell membranes, causing damage in the membrane structure, obstructing DNA replication and proteins, mitochondrial disruption, and reactive oxygen species (ROS) formation, stimulating apoptosis, and, eventually, lysis and death of the pathogenic microorganisms
Generally, nanoparticles are widely classified into organic and inorganic nanoparticles [90]. Some of the more well-known examples of nanomaterials as antimicrobials are discussed below.
Organic Nanoparticles
Chitosan
Chitosan is a linear polycationic polymer (N-deacetylated derivative) that is derived from chitin through treating crab or shrimp shells or other crustaceans with alkaline substances like sodium hydroxide (40–50% NaOH). Chitin is soluble in organic acids such as acetic acid, lactic acid, etc. as opposed to other solvents like water [91].
On the experimental level, chitosan has been used in nanoparticle formulations as a treatment against various diseases such as microbial keratitis [92]. This is due to the unique characteristics of chitosan such as being biocompatible, non-toxic, having a positive charge, and having a high absorption capacity, which make it an active agent against pathogens [93].
Chitosan’s efficiency as an antimicrobial agent is based on the interaction of chitosan (positive charge) with the microbial cell membrane (negative charge), leading to destabilization of the microbial membrane and leaking of proteinaceous and other intracellular constituents , followed by lysis and cell death [90]. It has been shown that the polysaccharide (N-carboxybutyl /cationic) in chitosan has the ability to interact and form complex compounds with acidic polymers that are implicated in the pathogenesis of bacteria. For instance, N-carboxybutyl interacts with lipopolysaccharides, which are present on the outer surface of Gram-negative bacteria, or with the peptidoglycan (teichoic acid) of Gram-positive bacteria, leading to limiting pathogen virulence factors [94]. Also, chitosan has a chelating ability through selectively binding with trace metals, and can thus inhibit toxin production and limit microbial growth. Furthermore, chitosan activates the host tissue defenses and acts as a water-binding agent as well as inhibiting several enzymes. It has been observed that chitosan penetration via microbial cell membranes and movement to the nuclei may allow binding with microbial DNA and interference with synthesis of the microbial mRNA and proteins , and, eventually, the disorder of the microbial replication process [91]. However, the details of this mechanism are still unclear and under investigation.
Poly-ɛ-lysine
Poly-ɛ-lysine is a cationic homo-polypeptide of L-lysine (high positive charge density). The positive charge allows for the formation of soluble complexes with macromolecules that are negatively charged. Notably, poly-ε-lysine nanoparticles can affect a wide range of bacteria, especially Gram-positive bacterial strains such as Bacillus coagulans and Bacillus subtilis [90]. This effect is attributed to the disruption of microbial membranes through electrostatic adsorption of a bacterial cell surface, then outer membrane stripping, followed by abnormal cytoplasm distribution and damage to the bacterial cell [95].
Quaternary Ammonium Compounds
Quaternary ammonium compounds are cationic polymers that consist of non-ionic polyethylene glycol chains with different molecular weights. Numerous studies have referred to the role of these compounds as antimicrobial agents against a broad spectrum of Gram-negative and -positive bacteria, fungi, parasites, and viruses depending on the chain length (N-alkyl chain). Also, the features of quaternary ammonium compounds such as polymer morphology, molecular charge density, binding affinity to quaternary compounds, and the solubility of poly-cations in water, can affect the microbial activity [96, 97].
Briefly, the quaternary ammonium compound mechanism as an antimicrobial occurs through weak electrostatic interactions between the positive charge of these polymers and the negative charge of bacterial membranes, followed by the hydrophobic compound tail being inserted into the hydrophobic core of the bacterial membrane leading to the denaturing of the structural protein , and eventually bacterial cell death [98].
N-halamine Compounds
N-halamine complexes consist of one or more nitrogen−halogen covalent bonds that can be made by the halogenation of amide, imide, or amine groups. In general, an N-halamine compound can have two groups: the first refers to inorganic groups such as phosphate, sulfate, etc., and the second group is organic such as an alkyl group, a carbonyl group, etc. Thus, the presence of these groups indicates if it is an inorganic and organic N-halamine structure [99].
The biocidal properties of N-halamine compounds may be due to the return of halide atoms in the chloramine group (>N − Cl) or the bromamine group (>N – Br) to the oxidation state. These oxidizing halogens act by using active element transfer directly to biological receptors or by free halogen dissociation and release into the aqueous media, causing the microbial cell inhibition [90, 99].
Inorganic Nanoparticles
Silver
Silver is one of the metallic elements that has intrinsic therapeutic properties. Previously, it had been widely used in different forms such as metallic silver, silver nitrate, and silver sulfadiazine to treat microbial infections, wounds, and burns. Nevertheless, the use of silver compounds decreased markedly as a result of antibiotic discovery. Due to the emergence and development of microbial resistance to antibiotics, there was a push to find a more integrated approach. Accordingly, the comeback of silver with a nano-metal formulation may provide a potential antimicrobial agent [89].
There are differences in the effects of pure ionic silver (Ag+) in various compounds such as silver nitrate/AgNO3 and silver nanoparticles (AgNPs) on bacterial activity. The use of the silver ion alone can create a low molecular weight area in the bacterial center as a defense mechanism against bacteria. This mechanism supports the bacterial DNA by providing protection from toxic materials when the bacterium senses membrane disturbance. In contrast, the region of low molecular weight did not form when treated with silver nanoparticles, thus proving the efficiency of AgNP as an antimicrobial agent [100].
The experimental evidence shows that the silver nanoparticle (AgNP) is effective against bacteria (Gram-negative and -positive), fungi, parasites, and viruses [90]. It has been shown that the effectiveness of AgNP as an antimicrobial agent depends on size, shape, ionic density and strength, pH condition, and capping agent [101].
A summary of AgNp’s working mechanism against microbes is presented here. The large surface area of AgNP provides better contact with pathogens and AgNP can easily attach to the microbial cell membrane. This is followed by penetration of AgNP into the microbial cell [89, 101]. It has been shown that the small size of AgNP allows it to break through microbial cell walls easily, including microbial biofilm layers [102]. Also, the presence of the positive charge on the Ag ions (Ag+) is considered to be the vital component for antimicrobial activity through the protein structure disruption by binding to thiol (carbon-bonded sulfhydryl/ R–SH) and amino groups [90]. The bacterial cell membrane consists of sulfur-containing proteins, which can interact with AgNP, which has Ag + ions [100]. This encourages increased permeability of the bacterial cell membrane, leaving the bacterium unable to regulate material transport via the plasma membrane. Furthermore, lipopolysaccharide molecules in the outer membrane of Gram-negative bacteria allow for permeability of the bacterial barrier . Recent studies have discussed the role of metals like Ag against E. coli as a Gram-negative model, and the results showed that the metal can cause outer membrane distortion, formation of irregular-shaped pits, and changes in the permeability of the membrane, leading to release of lipopolysaccharide molecules and other proteins in the membrane. Hence, the membrane structure of E. coli degrades during treatment with AgNP [103].
When the AgNP enters bacterial cells during treatment, AgNP molecules tend to react with sulfur-containing proteins and phosphorus-containing compounds like DNA. Thus, several complex processes occur, causing protein denaturation, loss of DNA replication, inhibiting cell division, and, eventually, cell disruption and death [100, 103].
Notably, AgNP can also affect bacteria by interacting with the mitochondrial membrane, causing the activation of apoptosis-related genes that induce apoptosis. Also, the mitochondrial damage generates reactive oxygen species (ROS) , which play an important role in DNA degradation [81]. In this context, it has been observed that the biosynthesis of AgNPs produced by Aspergillus niger has the ability to significantly inhibit E. coli by perforating the cell membrane, causing leakage of cell components, forming ROS, and, finally, bacterial cell death [104].
In ophthalmology research, the results have shown silver nanoparticles to have antimicrobial activity through inhibiting different microbes such as Pseudomonas aeruginosa, Staphylococcus aureus, and Acanthamoeba castellanii, which cause keratitis. In addition, the use of AgNPs in a solution form or incorporated into contact lenses can reduce bacterial availability, limit bacterial adhesion , and prevent bacterial colonies from forming (the lens surface colonization). This may prevent the correlation between microbial keratitis and contaminated contact lenses [105].
Gold
Recently, gold nanoparticles (AuNPs) have been described as promising agents for various biological applications. Several studies have investigated the role of AuNPs in order to find ideal ways to utilize their features in an antimicrobial manner. Notably, the main goal of using AuNPs is to overcome microbial resistance to antibiotics such as methicillin-resistant Staphylococcus aureus (MRSA) , which has serious virulence features [106]. Some researchers have confirmed that AuNPs are less effective against microorganisms when used alone compared to when used in combination with antibiotics such as vancomycin and ampicillin [90].
In brief, AuNPs can attack and eliminate microbes via two steps: The first step is inhibition of the metabolism process through increasing potential changes in the membrane surface morphology and reducing the synthesis of adenosine triphosphate (ATP). The second step is the collapse of the biological mechanism by declining the ribosome subunit for tRNA binding. At the same time, it has been shown that AuNPs have low toxicity to mammal cells. Thus, gold nanoparticles are considered suitable candidates to use against pathogens [107].
Nitric Oxide
Nitric oxide (NO) has been shown to have antimicrobial properties [108]. It has been recommended to use NO in a NO-nano formulation as a potential strategy against microbial activity. Nitric oxide is a diatomic free radical that plays an important role in the innate immune response by limiting infection [109]. It is worth mentioning that NONPs have high efficiency against a broad spectrum of Gram-negative and Gram-positive bacteria, as well as the ability to reduce the formation of bacterial biofilms. The antimicrobial activity of NO occurs by producing reactive nitrogen species (RNS) rather than ROS [90]. It has been confirmed that the NONPs can inhibit the activity of methicillin-resistant Staphylococcus aureus (MRSA) in in vitro and in vivo abscesses in a mouse model [109]. In this regard, NONPs may be useful therapeutics for microbial skin abscesses and microbial keratitis.
Conclusion
Microbial adhesion on the corneal surface is considered a critical step that results in infection after the destruction of corneal barriers by external or internal injury. The immune response (innate and acquired immunity) involves releasing cytokines, interferons, and NK cells. The immune response plays a key role in eliminating pathogens, but if it fails, microbes may enter the eye and cause corneal damage. It has been shown that microbial resistance to antibiotics and low drug bioavailability with the presence of side effects are the main factors aggravating microbial infections. Therefore, scientific research is directed towards finding successful medical management of microbial infections using a new technique known as nano-formulation such as use of nanoparticles. The evidence clearly indicates that the unique properties of organic and inorganic nanoparticles have the ability to disrupt the microbial cell membrane, cause nucleus (DNA) damage, overcome microbial resistance, and achieve ideal therapeutic properties.
Highlights
-
Microbial keratitis is a widespread disease at the global level and the main cause of blindness.
-
Corneal damage, pathogen adhesion, and the failure of eye immune defenses are considered the major causes of microbial keratitis.
-
In ophthalmology, traditional treatment limitations and increased microbial resistance have necessitated the discovery of a more integrated therapeutic approach.
-
The experimental evidence from several studies has shown the nanoparticle approach to be a promising therapy due to the ability of nanoparticles to provide a high level of bioavailability and eliminate pathogens.
References
Shahaby AF, Alharthi AA, El Tarras AE. Potential bacterial pathogens of red eye infections and their antibiotic susceptibility patterns in Taif, KSA. Int J Curr Microbiol App Sci (IJCMAS). 2015;4(11):383–93.
Bermudez MA, et al. Corneal epithelial wound healing and bactericidal effect of conditioned medium from human uterine cervical stem cells. Effect of CM-hUCESCs on wound healing in dry eye. Invest Ophthalmol Vis Sci. 2015;56(2):983–92.
Deepika J, Musaddiq M. Combination therapy on pathogenic bacteria from corneal ulcers. IJAR. 2015;1(11):878–81.
Singh D, et al. A retrospective study of fungal corneal ulcer from the western part of Uttar Pradesh. Int J Res Med Sci. 2015;3(4):880.
Janin-Manificat H, et al. Development of ex vivo organ culture models to mimic human corneal scarring. Mol Vis. 2012;18:2896.
Putri AM, Heryati S, Nasution N. Characteristics and predisposing factors of bacterial corneal ulcer in the National Eye Center, Cicendo Eye Hospital, Bandung from January to December 2011. Althea Med J. 2015;2(3):443–7.
Gebremariam TT. Bacteriology and risk factors of bacterial keratitis in Ethiopia. Health Sci J. 2015;9(5):1–6.
El-Sayed NM, Safar EH, Issa RM. Parasites as a cause of keratitis: need for increased awareness. Aperito J Ophthalmol. 2015;1:103.
Janumala H, Mandal AB, Sehgal PK. Bacterial keratitis-causes, symptoms and treatment: INTECH Open Access Publisher; 2012. https://scholar.google.com/scholar?hl=en&as_sdt=0%2C5&q=Janumala+H%2C+Mandal+AB%2C+Sehgal+PK.+Bacterial+keratitis-causes%2C+symptoms+and+treatment%3A+INTECH+Open+Access+Publisher%3B+2012&btnG=
Bouhenni R, et al. Proteomics in the study of bacterial keratitis. Proteomes. 2015;3(4):496–511.
Akpek E, Gottsch J. Immune defense at the ocular surface. Eye. 2003;17(8):949–56.
Krishna S, et al. Study of bacteriological profile of corneal ulcers in patients attending VIMS, Ballari, India. Int J Curr Microbiol App Sci. 2016;5(7):200–5.
Sharma OP, Patel V, Mehta T. Nanocrystal for ocular drug delivery: hope or hype. Drug Deliv Transl Res. 2016;6(4):399–413.
Salem HF, Ahmed SM, Omar MM. Liposomal flucytosine capped with gold nanoparticle formulations for improved ocular delivery. Drug Des Devel Ther. 2016;10:277.
Guzman M, Dille J, Godet S. Synthesis and antibacterial activity of silver nanoparticles against gram-positive and gram-negative bacteria. Nanomedicine. 2012;8(1):37–45.
O’Brien KS, et al. Microbial keratitis: a community eye health approach. Community Eye Health. 2015;28(89):1.
Lorenzo-Morales J, Khan NA, Walochnik J. An update on Acanthamoeba keratitis: diagnosis, pathogenesis and treatment. Parasite. 2015;22:10.
Wang N, et al. Bacterial spectrum and resistance patterns in corneal infections at a Tertiary Eye Care Center in South China. Int J Ophthalmol. 2016;9(3):384.
Daba KT. Bacteriology and risk factors of bacterial keratitis in Ethiopia. Archivos de Medicina. 2015;9(5):6.
Kautto L, et al. Glycan involvement in the adhesion of Pseudomonas aeruginosa to tears. Exp Eye Res. 2016;145:278–88.
Badawi AE, Moemen D, El-Tantawy NL. Epidemiological, clinical and laboratory findings of infectious keratitis at Mansoura Ophthalmic Center, Egypt. Int J Ophthalmol. 2017;10(1):61.
Giffard PM, et al. Chlamydia trachomatis genotypes in a cross-sectional study of urogenital samples from remote Northern and Central Australia. BMJ Open. 2016;6(1):e009624.
Chhangte L, Pandey S, Umesh. Epidemiological and microbiological profile of infectious corneal ulcers in Tertiary Care Centre, Kumaon Region, Uttarakhand. Int J Sci Res Publ. 2015;5(2):5.
Ibrahim YW, Boase DL, Cree IA. How could contact lens wearers be at risk of Acanthamoeba infection? A review. J Opt. 2009;2(2):60–6.
Schaefer F, et al. Bacterial keratitis: a prospective clinical and microbiological study. Br J Ophthalmol. 2001;85(7):842–7.
Taube M, et al. Pattern recognition receptors in microbial keratitis. Eye. 2015;29(11):1399.
Yuan Q, et al. Protective efficacy of a peptide derived from a potential adhesin of Pseudomonas aeruginosa against corneal infection. Exp Eye Res. 2016;143:39–48.
Singh B, et al. Human pathogens utilize host extracellular matrix proteins laminin and collagen for adhesion and invasion of the host. FEMS Microbiol Rev. 2012;36(6):1122–80.
Song J, et al. Ocular diseases: immunological and molecular mechanisms. Int J Ophthalmol. 2016;9(5):780–8.
Kumagai N, et al. Lipopolysaccharide-induced expression of intercellular adhesion molecule-1 and chemokines in cultured human corneal fibroblasts. Invest Ophthalmol Vis Sci. 2005;46(1):114–20.
Zhou Z, et al. Role of the Fas pathway in Pseudomonas aeruginosa keratitis. Invest Ophthalmol Vis Sci. 2010;51(5):2537–47.
Redfern RL, McDermott AM. Toll-like receptors in ocular surface disease. Exp Eye Res. 2010;90(6):679–87.
Hume EB, et al. A Staphylococcus aureus mouse keratitis topical infection model: cytokine balance in different strains of mice. Immunol Cell Biol. 2005;83(3):294–300.
Srinivasan M. Fungal keratitis. Curr Opin Ophthalmol. 2004;15(4):321–7.
Rautaraya B, et al. Diagnosis and treatment outcome of mycotic keratitis at a tertiary eye care center in eastern India. BMC Ophthalmol. 2011;11:39.
Truong D, et al. Microbial keratitis at an urban public hospital: a 10-year update. J Clin Exp Ophthalmol. 2015;6(6):7.
Zhou Q, et al. Development of a novel ex vivo model of corneal fungal adherence. Graefes Arch Clin Exp Ophthalmol. 2011;249(5):693–700.
Geethakumari P, Remya R, Reena A. Bacterial keratitis and fungal keratitis in South Kerala: a comparative study. Kerla J Ophthalmol. 2011;23(1):43–6.
Ritterband DC, et al. Fungal keratitis at the New York eye and ear infirmary. Cornea. 2006;25(3):264–7.
Tuft S, Tullo A. Fungal keratitis in the United Kingdom 2003–2005. Eye. 2009;23(6):1308–13.
Li C, et al. Expression of dectin-1 during fungus infection in human corneal epithelial cells. Int J Ophthalmol. 2014;7(1):34.
Guo H, Wu X. Innate responses of corneal epithelial cells against Aspergillus fumigatus challenge. FEMS Immunol Med Microbiol. 2009;56(1):88–93.
Feng X, et al. A rabbit model of Acanthamoeba keratitis that better reflects the natural human infection. Anat Rec. 2015;298(8):1509–17.
Scheid P, Schwarzenberger R. Acanthamoeba spp. as vehicle and reservoir of adenoviruses. Parasitol Res. 2012;111(1):479–85.
El-Sayed NM, et al. Acanthamoeba DNA can be directly amplified from corneal scrapings. Parasitol Res. 2014;113(9):3267–72.
Sridhar U, et al. Ocular Microsporidiosis–our experience in a Tertiary Care Centre in North India. Open J Ophthalmol. 2015;5(03):130.
Panjwani N. Pathogenesis of Acanthamoeba keratitis. Ocul Surf. 2010;8(2):70–9.
Clarke DW, Niederkorn JY. The pathophysiology of Acanthamoeba keratitis. Trends Parasitol. 2006;22(4):175–80.
Farooq AV, Shukla D. Herpes simplex epithelial and stromal keratitis: an epidemiologic update. Surv Ophthalmol. 2012;57(5):448–62.
Jester JV, et al. Confocal microscopic analysis of a rabbit eye model of high-incidence recurrent herpes stromal keratitis. Cornea. 2016;35(1):81–8.
Chou TY, Hong BY. Ganciclovir ophthalmic gel 0.15% for the treatment of acute herpetic keratitis: background, effectiveness, tolerability, safety, and future applications. Ther Clin Risk Manag. 2014;10:665–81.
Karsten E, Watson SL, Foster LJR. Diversity of microbial species implicated in keratitis: a review. Open Ophthalmol J. 2012;6(1):110–24.
Yun H, Lathrop KL, Hendricks RL. A central role for sympathetic nerves in herpes stromal keratitis in mice sympathetic nerves and HSK. Invest Ophthalmol Vis Sci. 2016;57(4):1749–56.
Tsatsos M, et al. Herpes simplex virus keratitis: an update of the pathogenesis and current treatment with oral and topical antiviral agents. Clin Exp Ophthalmol. 2016;44(9):824–37.
Sobol EK, et al. Case–control study of herpes simplex eye disease: Bronx epidemiology of human immunodeficiency virus eye studies. Cornea. 2016;35(6):801–6.
Jiang Y, et al. Dendritic cell autophagy contributes to herpes simplex virus-driven stromal keratitis and immunopathology. MBio. 2015;6(6):e01426-15.
Akhtar J, Shukla D. Viral entry mechanisms: cellular and viral mediators of herpes simplex virus entry. FEBS J. 2009;276(24):7228–36.
Uchino Y, et al. Impact of cigarette smoking on tear function and correlation between conjunctival goblet cells and tear MUC5AC concentration in office workers. Sci Rep. 2016;6:27699.
de Souza GA, de Godoy LM, Mann M. Identification of 491 proteins in the tear fluid proteome reveals a large number of proteases and protease inhibitors. Genome Biol. 2006;7(8):R72.
Cwiklik L. Tear film lipid layer: a molecular level view. Biochimic Biophys Acta Biomembr. 2016;1858(10):2421–30.
King-Smith E, et al. The thickness of the tear film. Curr Eye Res. 2004;29(4–5):357–68.
Wu YT, et al. Human tear fluid reduces culturability of contact lens-associated Pseudomonas aeruginosa biofilms but induces expression of the virulence-associated type III secretion system. Ocul Surf. 2017;15(1):88–96.
King-Smith PE, Hinel EA, Nichols JJ. Application of a novel interferometric method to investigate the relation between lipid layer thickness and tear film thinning. Invest Ophthalmol Vis Sci. 2010;51(5):2418–23.
Tsubota K, et al. New perspectives on dry eye definition and diagnosis: a consensus report by the Asia Dry Eye Society. Ocul Surf. 2017;15(1):65–76.
Underhill DM, Ozinsky A. Phagocytosis of microbes: complexity in action. Annu Rev Immunol. 2002;20(1):825–52.
Cubitt CL, Lausch RN, Oakes JE. Synthesis of type II interleukin-1 receptors by human corneal epithelial cells but not by keratocytes. Invest Ophthalmol Vis Sci. 2001;42(3):701–4.
Moore JE, et al. The inflammatory milieu associated with conjunctivalized cornea and its alteration with IL-1 RA gene therapy. Invest Ophthalmol Vis Sci. 2002;43(9):2905–15.
Qazi Y, Turhan A, Hamrah P. Trafficking of immune cells in the cornea and ocular surface: INTECH Open Access Publisher; 2012. https://scholar.google.com/scholar?hl=en&as_sdt=0%2C5&q=Qazi+Y%2C+Turhan+A%2C+Hamrah+P.+Trafficking+of+immune+cells+in+the+cornea+and+ocular+surface%3A+INTECH+Open+Access+Publisher%3B+2012&btnG=
Bolaños-Jiménez R, et al. Ocular surface as barrier of innate immunity. Open Ophthalmol J. 2015;9(1):49.
Cruzat A, Pavan-Langston D, Hamrah P. In vivo confocal microscopy of corneal nerves: analysis and clinical correlation. Semin Ophthalmol. 2010;25(5–6):171–7.
Tran MT, et al. Calcitonin gene-related peptide induces IL-8 synthesis in human corneal epithelial cells. J Immunol. 2000;164(8):4307–12.
Tran MT, Lausch RN, Oakes JE. Substance P differentially stimulates IL-8 synthesis in human corneal epithelial cells. Invest Ophthalmol Vis Sci. 2000;41(12):3871–7.
Ueno M, et al. Accelerated wound healing of alkali-burned corneas in MRL mice is associated with a reduced inflammatory signature. Invest Ophthalmol Vis Sci. 2005;46(11):4097–106.
Ivashkiv LB, Donlin LT. Regulation of type I interferon responses. Nat Rev Immunol. 2014;14(1):36–49.
Burg ND, Pillinger MH. The neutrophil: function and regulation in innate and humoral immunity. Clin Immunol. 2001;99(1):7–17.
Alberts B, et al. Molecular biology of the cell. 4th ed: Garland Science; 2002. Bray D. Cell movements: from molecules to motility. 2nd ed: Garland Science; 2000.
Moretta L, et al. Human natural killer cells: their origin, receptors and function. Eur J Immunol. 2002;32(5):1205–11.
Resch MD, et al. Dry eye and corneal langerhans cells in systemic lupus erythematosus. J Ophthalmol. 2015;2015:1–8.
Hamrah P, et al. Novel characterization of MHC class II–negative population of resident corneal Langerhans cell–type dendritic cells. Invest Ophthalmol Vsual Sci. 2002;43(3):639–46.
Unanue ER. Perspective on antigen processing and presentation. Immunol Rev. 2002;185(1):86–102.
Rai M, et al. Nanotechnology based anti-infectives to fight microbial intrusions. J Appl Microbiol. 2016;120(3):527–42.
Hao J, et al. Fabrication of a composite system combining solid lipid nanoparticles and thermosensitive hydrogel for challenging ophthalmic drug delivery. Colloids Surf B: Biointerfaces. 2014;114:111–20.
Ludwig A. The use of mucoadhesive polymers in ocular drug delivery. Adv Drug Deliv Rev. 2005;57(11):1595–639.
Rupenthal ID, Green CR, Alany RG. Comparison of ion-activated in situ gelling systems for ocular drug delivery. Part 1: physicochemical characterisation and in vitro release. Int J Pharm. 2011;411(1):69–77.
Chaurasia SS, et al. Nanomedicine approaches for corneal diseases. J Funct Biomater. 2015;6(2):277–98.
Reimondez-Troitiño S, et al. Nanotherapies for the treatment of ocular diseases. Eur J Pharm Biopharm. 2015;95:279–93.
Tandon A, et al. BMP7 gene transfer via gold nanoparticles into stroma inhibits corneal fibrosis in vivo. PLoS One. 2013;8(6):e66434.
Metruccio MM, et al. Pseudomonas aeruginosa outer membrane vesicles triggered by human mucosal fluid and lysozyme can prime host tissue surfaces for bacterial adhesion. Front Microbiol. 2016;7:871.
Rai M, Yadav A, Gade A. Silver nanoparticles as a new generation of antimicrobials. Biotechnol Adv. 2009;27(1):76–83.
LewisOscar F, et al. Algal nanoparticles: synthesis and biotechnological potentials. In: Algae-organisms for imminent biotechnology: InTech; 2016. https://scholar.google.com/scholar?hl=en&as_sdt=0%2C5&q=LewisOscar+F%2C+et+al.+Algal+nanoparticles%3A+synthesis+and+biotechnological+potentials.+In%3A+Algae-organisms+for+imminent+biotechnology%3A+InTech%3B+2016&btnG=
Rabea EI, et al. Chitosan as antimicrobial agent: applications and mode of action. Biomacromolecules. 2003;4(6):1457–65.
Fu T, et al. Ocular amphotericin B delivery by chitosan-modified nanostructured lipid carriers for fungal keratitis-targeted therapy. J Liposome Res. 2017;27(3):228–33.
Tavaria FK, et al. Influence of abiotic factors on the antimicrobial activity of chitosan. J Dermatol. 2013;40(12):1014–9.
Felt O, et al. Chitosan as tear substitute: a wetting agent endowed with antimicrobial efficacy. J Ocul Pharmacol Ther. 2000;16(3):261–70.
Lam SJ, et al. Antimicrobial polymeric nanoparticles. Prog Polym Sci. 2018;76:40–64.
Khowdiary M, et al. Synthesis, characterization and biocidal efficiency of quaternary ammonium polymers silver nanohybrids against sulfate reducing bacteria. J Mol Liq. 2017;230:163–8.
Jiao Y, et al. Quaternary ammonium-based biomedical materials: state-of-the-art, toxicological aspects and antimicrobial resistance. Prog Polym Sci. 2017;71:53–90.
Muñoz-Bonilla A, Fernández-García M. Polymeric materials with antimicrobial activity. Prog Polym Sci. 2012;37(2):281–339.
Hui F, Debiemme-Chouvy C. Antimicrobial N-halamine polymers and coatings: a review of their synthesis, characterization, and applications. Biomacromolecules. 2013;14(3):585–601.
Morones JR, et al. The bactericidal effect of silver nanoparticles. Nanotechnology. 2005;16(10):2346.
Ahmed S, et al. A review on plants extract mediated synthesis of silver nanoparticles for antimicrobial applications: a green expertise. J Adv Res. 2016;7(1):17–28.
Ramasamy M, Lee J. Recent nanotechnology approaches for prevention and treatment of biofilm-associated infections on medical devices. Biomed Res Int. 2016;2016:1–17.
Sondi I, Salopek-Sondi B. Silver nanoparticles as antimicrobial agent: a case study on E. coli as a model for Gram-negative bacteria. J Colloid Interface Sci. 2004;275(1):177–82.
Ninganagouda S, et al. Growth kinetics and mechanistic action of reactive oxygen species released by silver nanoparticles from Aspergillus Niger on Escherichia coli. Biomed Res Int. 2014;2014:1–9.
Willcox MD, et al. Ability of silver-impregnated contact lenses to control microbial growth and colonisation. J Opt. 2010;3(3):143–8.
Penders J, et al. Shape-dependent antibacterial effects of non-cytotoxic gold nanoparticles. Int J Nanomedicine. 2017;12:2457.
Shamaila S, et al. Gold nanoparticles: an efficient antimicrobial agent against enteric bacterial human pathogen. Nano. 2016;6(4):71108.
Hetrick EM, et al. Anti-biofilm efficacy of nitric oxide-releasing silica nanoparticles. Biomaterials. 2009;30(14):2782–9.
Han G, et al. Nitric oxide releasing nanoparticles are therapeutic for Staphylococcus aureus abscesses in a murine model of infection. PLoS One. 2009;4(11):e7804.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Al-Mashahedah, A., Kanwar, R.K., Kanwar, J.R. (2018). Advances in the Field of Microbial Infection in the Cornea and the Role of Nanotechnology in Treating Keratitis. In: Patel, J., Sutariya, V., Kanwar, J., Pathak, Y. (eds) Drug Delivery for the Retina and Posterior Segment Disease. Springer, Cham. https://doi.org/10.1007/978-3-319-95807-1_10
Download citation
DOI: https://doi.org/10.1007/978-3-319-95807-1_10
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-95806-4
Online ISBN: 978-3-319-95807-1
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)