Abstract
Prostate cancer (PCa) remains as one of the most controversial issues in health care because of the dilemmas related to screening using Prostate Specific Antigen (PSA). A high number of false positive biopsies and an elevated rate of overdiagnosis are the main problems associated with PSA. New PCa biomarkers have been recently proposed to increase the predictive value of PSA. The published results showed that PCA3 score, Prostate Health Index and 4Kscore can reduce the number of unnecessary biopsies, outperforming better than PSA and the percentage of free PSA. Furthermore, 4Kscore provides with high accuracy an individual risk for high-grade PCa. High values of PHI are also associated with tumor aggressiveness. In contrast, the relationship of PCA3 score with aggressiveness remains controversial, with studies showing opposite conclusions. Finally, the development of molecular biology has opened the study of genes, among them TMPRSS2:ERG fusion gene and miRNAs, in PCa detection and prognosis.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Prostate cancer detection
- Biomarker
- PSA
- Prostate health index
- 4Kscore
- PCA3 score
- miRNAs
- Exosomal biomarkers
2.1 Introduction
Prostate cancer (PCa) is the second most common cancer in men worldwide, with an estimated 1.1 million new diagnosed cases and 307,000 deaths in 2012 [1]. Furthermore, PCa remains one of the most controversial issues in health care because of the dilemmas related to screening using Prostate Specific Antigen (PSA). PCa detection is difficult due to the limited specificity of PSA, with false positive results in patients with benign prostatic hyperplasia (BPH) as well as in patients with symptomatic and asymptomatic prostatitis. Therefore, biopsy is positive in around 25% of patients with PSA in the range between 2 and 10 μg/L.
PCa is a high prevalent tumor, with an increasing age-related incidence. A systematic review published in 2015 showed that the mean prevalence of incidental PCa in men who died of other causes increased from 5% (95% CI: 3–8%) at age < 30 years to 59% (95% CI:48–71%) by age > 79 years [2]. Therefore, a large proportion of PCa are latent, never progressing into aggressive carcinomas. In this regard, according to the Surveillance, Epidemiology, and End Results, the incidence rate of PCa increased from 94.0 in 1975, in the prePSA era, to 114.14 in 2012, while the death incidence along these years decreased from 30.97 to 19.57 [3]. Actually, PSA screening campaigns cause overdetection of insignificant tumors and thus overtreatment, too. Risks related to overdetection and overtreatment outweigh the potential benefits of screening campaigns.
Currently, PCa guidelines do not recommend the use of PSA as routine test for PCa screening or remark that early PSA testing should be decided considering potential benefits and harms. Debate about the opportunity of screening, nonetheless, goes on. Fleshner et al. [4] recently indicated that the abandonment of PSA screening would prevent all cases of overdiagnosis, but fail to prevent 100% of avoidable deaths, leading to a 13–20% increase in prostate-cancer-related deaths. These data show that harms associated with no screening must also be considered.
PCa is a highly heterogeneous disease in terms of clinical presentation. Different risk classification tools have been developed including biochemical and clinical factors to distinguish patients with PCa according to the prognosis. Epstein criteria [5] have been used to predict insignificant PCa, while the D’Amico classification [6] is used to predict biochemical recurrence after treatment according to biopsy Gleason score, PSA serum levels and the percentage of biopsy material involved with cancer. On the other hand, several authors have put into question if patients with Gleason 6 score must be labeled as cancer, although these tumors have the hallmarks of cancer from a pathologic perspective [7,8,9]. More recently, new genetic-based evidences confirm the heterogeneity of PCa. The researchers of Cancer Genome Atlas Research Network, analyzing a cohort of 333 tumors, confirmed the molecular heterogeneity of PCa, suggesting a molecular taxonomy in which 74% of PCa tumors are classified in one of seven subtypes defined by specific gene fusions (ERG, ETV1/4, FLI1) or mutations (SPOP, FOXA1, IDH1) [10]. Furthermore, Rubin et al. [11] observed a relationship between genomic amplifications, deletions and point mutations with the prognostic grade groups established in 2016 by the International Society of Urologic Pathology and the World Health Organization to update the Gleason score system.
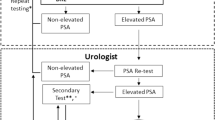
Active surveillance (AS) has become an alternative to curative therapy for PCa, decreasing the negative effects of overdiagnosis and overtreatment [12]. AS is a way to delay any kind of definitive treatment, applying it only if there is evidence of progression. The monitoring strategy program includes regular digital rectal examination (DRE), repeated prostate biopsies, and successive measurements of PSA serum levels to evaluate the PSA doubling time. The selection criteria used to include patients in an AS program are generally based on D’Amico classification of low-risk PCa (T1-T2a, PSA < 10 μg/L, Gleason score < 7), although some programs also include patients with intermediate risk. However, current available criteria to select patients for AS have a nontrivial risk of misclassification. Therefore, according to a study published by Palisaar et al. [13], current criteria failed around 20% to identify insignificant PCa from patients who had unfavorable tumor characteristics, with a high risk of early failure of AS programs and incurable PCa. The availability of more accurate inclusion criteria would lead to better select patients for AS, improving the outcome.
New PCa biomarkers have been recently proposed to increase the accuracy of PSA in the detection and prognosis of early PCa, distinguishing aggressive and nonaggressive PCa. The search for new subforms of PSA continued in recent years and new derivatives have been identified. Prostate health index (PHI) combines [-2]proPSA, free PSA (fPSA) and total PSA, while 4Kscore -or 4 kallicrein panel- includes total PSA, fPSA, intact PSA (iPSA), and human kallicrein. Furthermore, the development of molecular biology has opened the study of genes and the miRNAs associated with PCa. Our aim is to review the usefulness of these blood and urine new biomarkers in the management of early PCa.
2.2 PSA–Derived PCa Biomarkers
PSA, also called human kallicrein 3, is a glycoprotein of 30 kDa grouped in the kallicrein family. Because of its enzymatic action, PSA circulates into the blood bound to several protease inhibitors, such as α-1-antichymotrypsin and α-2-macroglobulin, whereas only a small fraction, that has been previously inactivated, circulates as free PSA. The percentage of free PSA to total PSA (%fPSA) is significantly decreased in patients with PCa, although an overlap of results is observed comparing patients with and without PCa. Nevertheless, according to a meta-analysis published in 2006, %fPSA only provides additional information in the decision to perform prostate biopsies when levels reach extreme values [14].
The free PSA (fPSA) fraction is also composed of three different subfractions: benign PSA (BPSA), iPSA, and proPSA. Whereas BPSA is associated with BPH, proPSA is related to PCa [15]. The native form of proPSA is [-7] proPSA, which contains a 7-amino acid N-terminal pro-leader peptide. Through the proteolytic cleavage of this peptide, promoted by the kallikreins hK2 and hK4, the other truncated forms of proPSA, known as [-2] [-4] and [-5] proPSA, are formed.
2.2.1 Prostate Health Index
The truncated forms of proPSA were identified in serum of patients with PCa in 1997, showing that proPSA is a significant fraction of fPSA [16]. Initial published results showed the usefulness of proPSA isoforms in the detection of PCa, reducing the number of negative biopsies in patients with PSA in the grey range. Table 2.1 shows data obtained in initial studies using non-commercial assays for the measurement of one or more isoforms of proPSA [17,18,19,20,21].
Beckman Coulter developed a robust commercial immunoassay for the measurement of [−2]proPSA, or p2PSA. According to results reported by Semjonow et al. [22] p2PSA is stable in serum stored at room temperature or refrigerated at 4 °C for a maximum of 48 h, although blood samples should be centrifuged within 3 h of blood draw. Numerous studies explored the usefulness of p2PSA in the management of early PCa, showing that the percentage of p2PSA in relation to fPSA (%p2PSA) is significantly elevated in patients with PCa. Furthermore, the Prostate Health Index (PHI), a new proPSA derivative indicator, has also yielded promising results in the detection of PCa. This new multiparametric index combines the concentration of p2PSA, fPSA, and total PSA according to the formula (p2PSA/fPSA)* √ total PSA.
Both %p2PSA and PHI demonstrated higher accuracy in predicting the presence of PCa at biopsy when compared with total PSA and %fPSA (Table 2.2) [23,24,25,26,27]. Additionally, %p2PSA and PHI showed a good relationship with the aggressiveness of the tumor, with higher levels in patients with Gleason score higher than 6. These results are confirmed by three meta-analyses published in 2013 and 2014, which concluded that PHI outperforms the accuracy obtained with PSA and %fPSA, showing an area under the curve (AUC) for PHI from 0.69 to 0.781 [28,29,30].
Furthermore, the accuracy of PHI in classifying and following patients with PCa on AS has been investigated. Cantiello et al. [31] reported that PHI predicts the pathologic Gleason score, extracapsular extension and seminal vesicles involvement in a series of 156 patients treated with radical prostatectomy. More recently, Heidegger et al. [32] showed that PHI levels were significantly elevated in those patients with an upgrade in final histology (pathologic Gleason score ≥ 7) in a cohort of 112 patients with biopsy Gleason score 6 treated with radical prostatectomy. Similarly, De la Calle et al. [33] reported an AUC for PHI of 0.815 to detect high-grade PCa (Gleason score ≥ 7). According to these authors, at 95% sensitivity for detecting aggressive PCa the optimal PHI cutoff was 24, which would help to avoid 41% of unnecessary biopsies. On the other hand, baseline and longitudinal %p2PSA and PHI provided improved prediction of biopsy reclassification during follow-up in a series of 167 patients included in a program of active surveillance, according to the results published by Tosoian et al. [34], while total PSA was not significantly associated with biopsy reclassification.
PHI was approved in June 2012 by the US Food and Drug Administration (FDA) for the detection of PCa in men older than 50, PSA between 4 and 10 μg/L, and a non-suspicious DRE. Furthermore, PHI is recommended by the National Comprehensive Cancer Network (NCCN) for patients who have never undergone biopsy or after a negative biopsy. According to NCCN, a PHI higher than 35 is related to a high probability of PCa.
2.2.2 Four–Kallikrein Panel
The four-kallikrein panel includes the measurement of total PSA, fPSA, iPSA and hK2, a protein with high homology to PSA. Several studies performed by the group led by Lilja and Vickers, from Memorial Sloan-Kettering Cancer Center, have evaluated this panel. The AUCs for the 4-kallikrein panel obtained in these studies were higher than those for a PSA based model for the detection of any PCa (AUCs from 0.674 to 0.832) as well as for the detection of high-grade PCa (Gleason score ≥ 7) (AUCs from 0.793 to 0.870) (Table 2.3) [35,36,37,38,39]. Similar results were obtained when DRE was added to those models, showing AUCs from 0.697 to 0.836 in the detection of any PCa and from 0.798 to 0.903 in the detection of high-grade PCa.
The 4Kscore, commercialized by Opko Diagnostics, is an algorithm which combines the four-kallicrein panel with patient age, DRE and history of prior biopsy to predict high-grade PCa. The NCCN Guidelines for PCa recommended the use of 4Kscore for the detection of high-grade tumors. This statistical score improves the specificity for predicting the risk of high-grade PCa, reducing the number of unnecessary biopsies. A prospective study developed in 26 urology centers across the United States, evaluating 1012 men undergoing a prostate biopsy, showed an AUC for 4Kscore of 0.82. The authors reported that 30% of biopsies could be saved using a cut-off value of 6%, delaying diagnosis for 1.3% of high-grade PCa patients [40]. Additionally, Kim et al. [41] recently reported that 4Kscore increased significantly the accuracy obtained using the Prostate Cancer Prevention Trial Risk Calculator from 0.73 to 0.79. On the other hand, the test has been shown useful for predicting high-grade PCa in patients with PSA higher than 10 μg/L or with positive DRE, according to a meta-analysis published by Vickers et al. [42]. The addition of the 4Kscore increased the AUC from 0.69 to 0.84 for patients with PSA higher than 10 μg/L and from 0.72 to 0.82 for patients with positive DRE.
Furthermore, Lin et al. [43] showed the ability of 4Kscore to predict high-grade PCa in men included in an AS program. Also, the test has been shown to predict the long term development of distant metastasis. Results published by Stattin et al. [44] showed that the measurement of 4Kscore at 50 and 60 years old allowed the classification of the patients into two groups according to the probability of developing distant metastasis 20 years later. According to this study, patients with 4Kscore higher than 5 at 50 years old and PSA ≥ 2 μg/L have a significant increased risk of developing distant metastasis. Also, patients with 4Kscore higher than 7.5 at 60 years old and PSA ≥ 3 μg/L have a significant increased risk of developing distant metastasis. The authors concluded that patients with a modest PSA elevation in midlife but a low-risk of high-grade PCa according to 4Kscore could be exempted from biopsy.
2.2.3 PSA Based Nomograms
Several nomograms to predict the likelihood of PCa at biopsy have been developed in last few years with the aim to reduce the number of unnecessary prostate biopsies. These nomograms are graphical representations of a multivariate logistic regression analysis based on specific characteristics of a patient and his disease. Nomograms used to predict PCa combines different demographic, clinical and biochemical variables, including age of the patient, family history of PCa, DRE, prostate volume and PSA serum levels. The Prostate Cancer Risk Calculator of the European Randomized Study of Screening for Prostate Cancer (ERSSPC) (http://www.prostatecancer-riskcalculator.com/) and the Prostate Cancer Prevention Trial (PCPT) based Cancer Risk Calculator (http://myprostatecancerrisk.com/) are among the most used nomograms.
The addition of new biomarkers to these web-based calculators could increase the accuracy for predicting positive prostate biopsies. Lughezzani et al. [45] developed a PHI based nomogram to predict PCa analyzing data from 729 patients who were scheduled for prostate biopsy following suspicious DRE and/or increased PSA. The accuracy increased from 0.73 to 0.80 when PHI was included to a multivariable logistic regression model based on patient age, prostate volume, DRE, and biopsy history. Results were externally validated by a multicenter European study including 833 patients, obtaining an AUC of 0.752 [46]. On the other hand, Filella et al. [47] showed that the accuracy increased from 0.762 to 0.815 when PHI and %p2PSA were added to a multivariable analysis based on patient age, prostate volume, total PSA, and %fPSA. Also, results published by Roobol et al. [48] showed that the addition of PHI to the Prostate Cancer Risk Calculator of the ERSSPC increased the accuracy from 0.65 to 0.72, although it did not increase the accuracy obtained using PHI alone (0.72). Finally, more recently, Loeb et al. [49] reported that adding PHI significantly improved the predictive accuracy of the PCPT and ERSPC risk calculators for aggressive PCa, obtaining an AUC of 0.746.
2.3 mRNA Biomarkers in Urine
Novel mRNA biomarkers have been described in urine, including the mRNAs for PCA3 and TMPRSS2:ERG fusion gene. More recently, positive results have been published for the SelectMDx test, which includes the mRNAs for DLX1, HOXC6 and KLK3 [50, 51].
2.3.1 PCA3
PCA3, previously referred as DD3, is one of the most studied PCa-specific genes, obtaining the FDA’s approval in 2012 with the intended use for men older than 50 who have one or more previous negative biopsies. PCA3 is a gene that is overexpressed in PCa tissue [52] and transcribes a long non-coding mRNA involved in PCa cell survival, through modulating the androgen receptor signal [53].
The PCA3 score is calculated as the ratio of PCA3 and PSA mRNAs measured using qRT-PCR in the urine obtained after performing a prostate massage to enrich the prostate cell content. The PSA mRNA is used to normalize the PCA3 mRNA signal and to confirm the specimen validity, controlling the abundance of prostate cells and prostate mRNA. Samples with insufficient PSA mRNA were considered inconclusive. The Progensa PCA3 test, commercialized by Hologic, is a semi-automated assay that includes isolation, amplification, hybridization and quantification of mRNA from PCA3 and PSA using the DTS systems.
A higher PCA3 score is associated with a high prevalence of PCa, improving the results obtained with total PSA [54]. AUCs from 0.63 to 0.87 were documented for PCA3 score in a meta-analysis published in 2010 by Ruiz-Aragón and Márquez-Peláez [55]. Table 2.4 lists similar results reported more recently by other studies [56,57,58,59,60]. The comparative effectiveness review published by Bradley et al. [61] analyzing 34 observational studies showed that PCA3 score is more discriminatory than total PSA, obtaining that at 50% specificity, sensitivities were 77% and 57%, respectively. Nevertheless, differences in accuracy between both tests are lower when the influence of the bias caused by the use of PSA in the selection of patients is minimized. Therefore, Roobol et al. [62] selected patients for biopsy when PSA was 3 μg/L or higher and/or PCA3 score was 10 or higher, showing that PCA3 carries out marginally better than PSA (AUCs of 0.635 and 0.581, respectively; p: 0.143).
The selection of the most appropriate cut-off for PCA3 remains highly controversial, although 35 is probably the most used cut-off score [55]. The clinical guideline of the NCCN also recommends 35 as the discriminating value to detect PCa, but the FDA suggests that a PCA3 score lower than 25 is associated with a decreased likelihood of a positive biopsy. In this regard, Roobol et al. [62] indicated that 51.7% of biopsies could have been avoided using a cut-off of 35, but the authors underlined that 32% of all PCa and 26.3% of aggressive PCa were missed. Furthermore, according to Bradley et al. [61], the number of missed tumors is reduced significantly from 39% to 6% when the traditional cut-off of 35 is changed for 10, showing that 22% of biopsies were saved using this cut-off.
False positive results are an additional problem using PCA3 score, because a very high PCA3 score does not ensure the existence of PCa. Haese et al. [63] evaluated PCA3 in 463 men with one or two negative biopsies scheduled for repeat biopsy, and found that the probability of a positive repeat prostate biopsy was only of 47% in patients with PCA3 score > 100. Also, Schröder et al. [64] reported a low positive predictive value (38.9%) in a cohort of 56 men with PCA3 score of >100 at previous screens, although significant efforts to detect a PCa were subsequently performed.
Contradictory results have been published by different authors regarding the relationship of PCA3 with the aggressiveness of PCa (Table 2.4). A large study including 3073 men who underwent PCA3 analysis before initial prostate biopsy showed that PCA3 score was significantly associated with biopsy Gleason score [59], although the ROC analysis demonstrated that PCA3 did not significantly outperform PSA in the prediction of high-grade PCa (AUC 0.682 vs. 0.679, respectively, p = 0.702). Furthermore, Auprich et al. [65] showed that PCA3 score failed to add supplementary information to predict aggressive PCa in a series of 305 patients treated with radical prostatectomy, even if the authors obtained a significantly higher median PCA3 in patients with pathological Gleason score 7 or higher. According to these authors, difficulties to pass PCA3 into urine appear in tumors with a high Gleason score because glandular differentiation is lost.
2.3.2 TMPRSS2:ERG Fusion Gene
Recurrent chromosomal rearrangements have been observed in several hematologic malignancies and more recently in solid tumors, including PCa. Approximately 50% of these tumors are associated with fusions involving the androgen-regulated TMPRSS2 gene with the ETS family transcription factor family members, particularly ERG and ETV1 [66]. The recent publication of the Cancer Genome Atlas molecular taxonomy of PCa identifies ETS-rearrangements as the most common subtype, involving 58% of tumors [10]. These rearrangements result in overexpression of the ETS family transcription factors, which induces neoplastic phenotype [67]. Furthermore, recent results showed that TMPRSS2-ERG fusion increases cell migration and promotes cancer metastases in bone [68].
The TMPRSS2:ERG gene rearrangements are detected in urine samples obtained after a prostate massage using qRT-PCR. Levels of PSA mRNA are used for control and normalization purposes, and the results are presented as a TMPRSS2:ERG score. The combination of the TMPRSS2:ERG and PCA3 scores has been proposed as a way to improve the prediction of the presence of PCa on the biopsy. A recent review underlined that both biomarkers provides provides 90% specificity and 80% sensitivity in the detection of PCa [69]. A prospective multicentre evaluation including 443 patients who underwent prostate biopsy underlined that the AUC obtained using the ERSPC risk calculator increased from 0.799 to 0.842 when PCA3 and TMPRSS2:ERG scores were added [70]. Additionally, this study reported that TMPRSS2-ERG, but not PCA3, was associated with the biopsy Gleason score and the tumor clinical stage. Moreover, the authors found that TMPRSS2-ERG fusion gene was an independent predictor of extracapsular extension of the tumor in a subgroup of 61 patients treated with radical prostatectomy. However, no significant association was found with pathologic Gleason score or seminal vesicle invasion.
More recently, Tomlins et al. [71] showed the value of PCA3 and TMPRSS2:ERG scores when they were added to the PCPT risk calculator in a cohort of 1244 patients. The AUC increased from 0.639 to 0.762 when both tests were added. Moreover, this study underlined the value of these biomarkers to predict high-risk PCa, with an AUC of 0.779. Similarly, a recent multicenter prospective study published by Sanda et al. [72] showed that 42% of unnecessary prostate biopsies would have been avoided combining PCA3 and TMPRSS2:ERG scores. Furthermore, PCA3 was significantly higher in patients with Gleason score ≥ 7 versus patients with Gleason score 6. No differences between both groups of patients were found for TMPRSS2:ERG. These results were discussed by Stephan et al. [73], who underlined that the combination of PCA3 and PHI outperformed the accuracy obtained using PCA3 and TMPRSS2:ERG.
2.4 Exosomal and Non Exosomal miRNAs
2.4.1 MiRNAs Biogenesis, Function and Target Prediction
MicroRNAs (miRNAs) are small, from 18 to 25 nucleotides non-coding RNA molecules that regulate post-transcriptionally gene expression. MiRNAs are derived from so-called pri-miRNA. After being transcribed by RNA polymerase II, pri-miRNA is cleaved by nuclear RNase III Drosha-DGCR8 complex to produce pre-miRNA, which is exported from the nucleus into the cytoplasm by Exportin-5 and Ran-GTP61 and further processed by another endonuclease Dicer to generate mature double-stranded miRNA. Afterwards, the functional strand of the mature miRNA is loaded with Argonaute (AGO) proteins into the RISC (RNA induced silencing complex), where miRNA drives RISC to bind the 3’ UTR of a mRNA target, resulting thus in either mRNA cleavage, translational repression or deadenylation. Contrarily, the not functional strand is usually degraded.
Approximately 60% mRNAs can be regulated by miRNAs [74]. Each miRNA can regulate hundreds of genes through base pairing to mRNAs [75]. Moreover, a particular gene can be targeted by multiple miRNAs [76, 77]. Therefore, a miRNA can participate in multiple biological processes by regulating the expression of its target genes [78].
Several tools for target prediction have been developed to understand the molecular mechanisms of miRNA-mediated interactions. Those tools are based on certain assumptions, such as the base complementarity in the 3’UTR, thermodynamic stability, target-site accessibility, and evolutionary conservation of miRNA binding sites. One example of the most used computational prediction is TargetScan [79], which was applied to predict miRNA target sites conserved among orthologous 3′ UTRs of vertebrates. However, TargetScan only considers stringent seeds ignoring many potential targets. The intersection of PicTar [80] and TargetScan predictions is recommended in order to achieve both high sensitivity and high specificity.
More recently, Cava et al. [81] described a new software tool, called SpidermiR, which allows to access to both Gene Regulatory Networks and miRNAs in order to obtain miRNA–gene–gene and miRNA–protein–protein interactions. Moreover, SpidermiR integrates this information with differentially expressed genes obtained from The Cancer Genome Atlas through a R/Bioconductor package.
2.4.2 MiRNA in Body Fluids
The last release of miRBase (June, 2014) contains 1881 precursors and 2588 mature human miRNA sequences [82]. The aberrant expression of certain miRNAs has been associated with several cancers including PCa [83]. The dysregulation of miRNAs in cancer could be caused by several genomic anomalies such as chromosomal translocation, epigenetic alterations, as well as miRNA biogenesis machinery dysfunction, which subsequently affects transcription of primary miRNA, its processing to mature miRNAs, and interactions with mRNA targets [84, 85].
Since the initial study of Mitchell et al. [86] in 2008 showing that miRNAs from PCa cells are released into the circulation, different groups have identified several miRNAs signatures with utility in the detection and prognosis of PCa in body fluids (Table 2.5). Specific miRNA signatures in body fluids have been correlated with aggressiveness and response to therapy [86,87,88,89,90,91,92]. Nevertheless, there is a lack of concordance across the different studies, probably due to methodological differences that affect several steps of the miRNA analysis from the sample collection to the post-analytical phase. Although the substantial differences among the panels, miR-141, miR-375 and miR-21 are regularly reported in various studies [93].
Mitchell et al. [86] showed that serum levels of miR-141 can distinguish PCa patients from healthy controls, supporting the potential role of this miRNA as a diagnostic marker for PCa. The upregulation of miR-141 in PCa patients was confirmed in later studies [94,95,96,97]. At the moment, the widest study about the clinical usefulness of circulating miRNAs has been performed by Mihelich et al. [87], measuring the levels of 21 miRNAs in 50 BPH patients and 100 PCa patients in stages T1–T2, classified according to the Gleason score. High levels of 14 miRNAs were exclusively present in the serum from patients with low-grade PCa or BPH, compared to men with high-grade PCa who had consistently low levels. The expression levels of the 14 miRNAs were combined into a miR Score to predict absence of high-grade PCa among PCa and BPH patients. Furthermore, the authors developed the miR Risk Score based on 7 miRNAs (miR-451, miR-106a, miR-223, miR-107, miR-130b, let-7a and miR-26b) in plasma samples to accurately classify the patients with low-risk of biochemical recurrence. Similarly, Chen et al. [88] found that a panel of five circulating miRNAs (miR-622, miR-1285, let-7e, let-7c, and miR-30c) were significantly different in PCa patients compared to BPH and healthy controls with high accuracy in both identification and validation cohorts. Besides, Cheng et al. [89] identified five serum miRNAs (miR-141, miR-200a, miR-200c, miR-210, and miR-375) associated with metastatic castration resistant PCa. Sharova et al. [90] analysed the levels of circulating miRNAs in patients with elevated PSA who were diagnosed with either localised PCa or BPH upon biopsy and found that miR-106a/miR-130b and miR-106a/miR-223 ratios were significantly different between PCa and BPH groups, concluding that the analysis of the circulating miR-106a/miR-130b (AUC: 0.81) and miR-106a/miR-223 ratios (AUC: 0.77) may reduce the costs and morbidity of unnecessary biopsies. Recently, Al-Qatati et al. [91] using a RT-qPCR based array established a unique expression profile of circulating cell-free miRNAs to differentiate between PCa patients at intermediate versus high-risk for recurrence or death after radical prostatectomy. Particularly, miR-16, miR-148a, and miR-195 were tightly associated with high Gleason score. Those miRNAs are involved in the regulation of the PI3K/Akt signaling pathway and may be promising therapeutic targets for high-risk PCa. Otherwise, Salido-Guadarrama et al. [92] identified a miR-100/200b signature in urine pellet comparing 73 patients with high-risk PCa and 70 patients with BPH. The AUC for this signature (0.738) was higher than the obtained AUCs for total PSA (0.681) and %fPSA (0.710). Furthermore, when the miR-100/200b signature was included to a multivariate model based on age, DRE, total PSA and %fPSA, the AUC increased from 0.816 to 0.876. Another recent study about miRNAs in urine is the one carried out by Fredsøe et al. [98] who identified several deregulated miRNAs in cell-free urine samples from PCa patients and suggested a novel diagnostic three-miRNA model (miR-222-3p*miR-24-3p/miR-30c-5p) that distinguished BPH and PCa patients with an AUC of 0.95 in a first cohort, and was successfully validated in a second independent cohort (AUC 0.89). Besides, the authors reported a novel prognostic three-miRNA model (miR-125b-5p*let-7a-5p/miR-151-5p) that predicted time to biochemical recurrence after radical prostatectomy independently of routine clinicopathological parameters.
Particularly, Metcalf et al. [99] designed and validated a novel peptide nucleic acids (PNAs) based fluorogenic biosensor for the detection of endogenous concentrations of circulating miRNAs in serum for PCa detection with high affinity and specificity, which does not require any amplification step and involves minimal or no sample processing. The sensing technology is based on oligonucleotide-templated reactions where the only miRNA of interest serves as a matrix to catalyze an otherwise highly unfavorable fluorogenic reaction. The authors used this technology in the serum of 16 PCa patients, finding elevated levels of miR-141 and miR-375 in patients with active cancer compared to patients in remission, with the highest levels detected in metastatic PCa patients. The same RNA samples were analyzed using gold standard RT-qPCR to validate this novel technology and the results were comparable. However, this technology offers the advantages of being low-cost, isothermal and that it is practicable for incorporation into portable devices. Besides, a new feature of this technology is that PNA probes are also capable of detecting miR-precursors, which would indicate that the sum of mature and precursor miRNAs can also be used as a specific biomarker for PCa. Although tests were initially performed on extracted RNA from serum samples, similar results were also obtained when using the probes directly in serum without any amplification and any processing steps.
2.4.3 miRNAs in Exosomes
Exosomes are the smallest (30–150 nm) extracellular vesicles (EV) derived from multivesicular bodies and are involved in intercellular communication, since cells use them to exchange proteins, lipids and nucleic acids [100, 101]. Exosomes are either released from normal or neoplastic cells, being considered to play a fundamental role in many physiological and pathological processes [102]. Exosomes contain mRNA, miRNAs and DNA so the transfer of this kind of information and oncogenic signaling to the tumor microenvironment modulate the tumor progression, the angiogenic proliferation, the formation of the metastasis [103] and even the suppression of immune responses [104].
Several studies have suggested that exosomes obtained from blood and urine are a consistent source of miRNA for disease biomarker detection [105,106,107,108], although other researchers highlight that exosomes in standard preparations do not carry biologically significant amount of miRNAs [109]. Actually, RNA sequencing analysis of plasma-derived exosomes revealed that miRNAs are the most abundant exosomal RNA species [100]. The miRNA content of EV reflects the miRNA expression profile of the cells they originated from [110]. Nevertheless, according to Arroyo et al. [111], vesicle associated miRNAs only represents a minority, while around 90% of miRNAs in the circulation is present in a non-membrane-bound form. Contrarily, Gallo et al. [112] showed that the concentration of miRNAs was consistently higher in exosomal fractions as compared to exosome-depleted serum. Cheng et al. [105] performed deep sequencing of miRNAs in exosomal and total cell-free RNA fractions in human plasma and serum and found that exosomes are enriched in miRNAs and provide a consistent source of miRNAs for biomarker discovery. Besides, the same authors found that deep sequencing of exosomal and total cell-free small RNAs in human urine showed a significant enrichment of miRNAs in exosomes.
In fact, few reports have evaluated the exosomal miRNAs utility for PCa detection and prognosis. Li et al. [113] showed that the level of the miR-141 was significantly higher in exosomes compared with whole serum. Besides, according to these authors the level of serum exosomal miR-141 was significantly higher in PCa patients compared with BPH patients and healthy controls, finding the most elevated levels in patients with metastatic PCa. Moreover, Huang et al. [114] found that the levels of plasma exosomal miR-1290 and miR-375 were significantly associated with poor overall survival. The addition of these new biomarkers into a clinical prognostic model improved predictive performance with a time-dependent AUC increase from 0.66 to 0.73. Furthermore, Foj et al. [115] reported that miR-21, miR-375 and let-7c were significantly upregulated in PCa patients versus healthy subjects in urinary exosomes. Additionally, these miRNAs were found significantly deregulated in intermediate/high-risk PCa versus low-risk/healthy subjects in urinary exosomes. Similarly, Samsonov et al. [116] indicated that miR-21, miR-141 and miR-574 were upregulated in PCa patients compared with healthy controls in urinary exosomes isolated by a lectin-based exosomes agglutination method. Nevertheless, only miR-141 was found significantly upregulated when urinary exosomes were isolated by differential centrifugation.
Recently, a high-throughput, spherical nucleic acid-based miRNA expression profiling platform called the Scano-miR bioassay was developed to measure the expression levels of miRNAs with high sensitivity and specificity. The Scano-miR can detect miRNA biomarkers down to 1 femtomolar concentrations and distinguishes perfect miRNA sequences from those with single nucleotide mismatches [117]. Alhasan et al. [118] used the Scano-miR platform to study the exosomal miRNA profiles of serum samples from patients with very high-risk PCa and compared them with the miRNA profiles from healthy individuals and patients with low-risk PCa. The authors identified and validated a unique molecular signature specific for very high-risk PCa. This molecular signature can differentiate patients who may benefit from therapy from those who can be derived to active surveillance. Five miRNA PCa biomarkers (miR-200c, miR-605, miR-135a*, miR-433, and miR-106a) were identified to differentiate low-risk from high and very high-risk PCa.
Due to the discordant results and the lack of overlapping across the different studies, more large-scale studies are needed before clinical application of miRNAs as biomarkers for PCa management. Furthermore, new advances in standardization of all the steps in the process of miRNA analysis are required to improve knowledge on these new biomarkers.
2.5 Conclusion
The published results show that PCA3 score, PHI and 4Kscore can reduce the number of unnecessary biopsies, outperforming better than total PSA and %fPSA. Furthermore, in this review, we have underlined the relationship of these new biomarkers with PCa aggressiveness. The 4Kscore provides with high accuracy an individual risk for high-grade PCa. Also, high values of PHI are associated with tumor aggressiveness. In contrast, the relationship of PCA3 score with aggressiveness remains controversial, with studies showing opposite conclusions. Auprich et al. [119] suggested that the pass of PCA3 into urine is difficult in undifferentiated tumors because of their glandular differentiation lost. In consequence, the PCA3 score measured in urine could be low. On the other hand, more results are necessary to validate the usefulness of TMPRSS2:ERG fusion gene and the exosomal and non-exosomal miRNAs. In addition, new efforts to standardize the methodology used in the measurement of miRNAs are required. Moreover, isolation of exosomes requires easier and more reproducible methods.
Comparison studies among these biomarkers are also necessary to elucidate which of them to select. At the moment, few studies have been reported at this regard, although the performance of PHI and 4Kscore seems similar according to the published results. In this sense, a recent meta-analysis based on twenty-eight studies including 16,762 patients documented comparable AUCs for 4Kscore and PHI in the detection of high-grade PCa (AUCs of 0.81 and 0.82, respectively) [120]. The same conclusion was reported by Nordström et al. [121] evaluating 211 patients undergoing initial or repeat prostate biopsy. The authors showed AUCs in the prediction of high-grade PCa of 0.718 for 4Kscore and 0.711 for PHI.
In contrast, available studies comparing PHI and PCA3 score showed non-conclusive results. Scattoni et al. [122] performed a head-to-head comparison of both biomarkers concluding that PHI was significantly more accurate than the PCA3 score for predicting PCa (AUC 0.70 vs. 0.59). These differences were also observed for predicting PCa in the initial biopsy (AUCs of 0.69 vs 0.57, respectively) and in the repeat biopsy (AUCs of 0.72 vs 0.63, respectively). Conversely, Stephan et al. [123] reported AUCs of 0.74 vs. 0.68 for PCA3 score and PHI, respectively. According to this group, the performance of PCA3 score was slightly better in patients submitted to repeated biopsies than in the first biopsy (AUCs of 0.77 vs 0.70, respectively), while no appreciable differences were reported for PHI between both groups (AUCS of 0.69 vs 0.68, respectively).
To our knowledge, only Vedder et al. [124] performed a study comparing PCA3 score and the 4Kscore. The authors showed that the 4Kscore outperforms the PCA3 score (AUC 0.78 vs. 0.62) in men with elevated PSA, although the accuracy of the PCA3 score was higher in the global population (AUC 0.63 for PCA3 vs. 0.56 for the 4Kscore). Additionally, the authors showed that PCA3 score slightly added value to a multivariate model, increasing the AUC from 0.70 to 0.73. The value of 4Kscore in this regard was minimal, increasing the AUC from 0.70 to 0.71.
Currently, these biomarkers have been recommended by different guidelines [125,126,127], underlying that they outperform PSA and %fPSA in PCa detection. Furthermore, several studies suggest the value of these biomarkers to increase the predictive accuracy of multivariate models based on classical clinicopathologic variables. Moreover, magnetic resonance imaging (MRI) emerges as a new tool in PCa management, increasing the detection of clinically significant disease. The combined role of these biomarkers together with MRI data should be investigated from an integrated point of view [128]. In summary, available literature shows promising advances in PCa biomarker research. However, large prospective multicenter studies comparing PHI, 4Kscore and PCA3 score are necessary to further elucidate their role in the management of early PCa. Finally, careful validation of emerging biomarkers such as miRNAs and improvement in exosomal isolation are required. The development of these new alternatives could open a new scenario for PCa management in the era of personalized medicine.
References
Ferlay J, Steliarova-Foucher E, Lortet-Tieulent J, Rosso S, Coebergh JW, Comber H et al (2013) Cancer incidence and mortality patterns in Europe: estimates for 40 countries in 2012. Eur J Cancer 49:1374–1403
Bell KJ, Del Mar C, Wright G, Dickinson J, Glasziou P (2015) Prevalence of incidental prostate cancer: a systematic review of autopsy studies. Int J Cancer 137:1749–1757
Howlader N, Noone AM, Krapcho M, et al, eds. (2015) SEER cancer statistics review, 1975–2012, based on November 2014 SEER data submission. National Cancer Institute, Bethesda;. Available at: https://seer.cancer.gov/archive/csr/1975_2012/results_merged/sect_23_prostate.pdf. Accessed 4 July 2017
Fleshner K, Carlsson SV, Roobol MJ (2017) The effect of the USPSTF PSA screening recommendation on prostate cancer incidence patterns in the USA. Nat Rev Urol 14:26–37
Epstein JI, Walsh PC, Carmichael M, Brendler CB (1994) Pathologic and clinical findings to predict tumor extent of nonpalpable (stage T1c) prostate cancer. JAMA 271:368–374
D’Amico AV, Whittington R, Malkowicz SB et al (1998) Biochemical outcome after radical prostatectomy, external beam radiation therapy, or interstitial radiation therapy for clinically localized prostate cancer. JAMA 280:969–974
Carter HB, Partin AW, Walsh PC, Trock BJ, Veltri RW, Nelson WG et al (2012) Gleason score 6 adenocarcinoma: should it be labeled as cancer? J Clin Oncol 30:4294–4296
Kulac I, Haffner MC, Yegnasubramanian S, Epstein JI, De Marzo AM (2015) Should Gleason 6 be labeled as cancer? Curr Opin Urol 25:238–245
Eggener SE, Badani K, Barocas DA, Barrisford GW, Cheng JS, Chin AI et al (2015) Gleason 6 prostate Cancer: translating biology into population health. J Urol 194:626–634
Cancer Genome Atlas Research Network (2015) The molecular taxonomy of primary prostate Cancer. Cell 163:1011–1025
Rubin MA, Girelli G, Demichelis F (2016) Genomic correlates to the newly proposed grading prognostic groups for prostate Cancer. Eur Urol 69:557–560
Tosoian JJ, Carter HB, Lepor A, Loeb S (2016) Active surveillance for prostate cancer: current evidence and contemporary state of practice. Nat Rev Urol 13:205–215
Palisaar JR, Noldus J, Löppenberg B, von Bodman C, Sommerer F, Eggert T (2012, Sep) Comprehensive report on prostate cancer misclassification by 16 currently used low-risk and active surveillance criteria. BJU Int 110(6 Pt B):E172–E181
Lee R, Localio AR, Armstrong K, Malkowicz SB, Schwartz JS (2006) A meta-analysis of the performance characteristics of the free prostate-specific antigen test. Urology 67:762–768
Mikolajczyk SD, Millar LS, Wang TJ et al (2000) A precursor form of prostate-specific antigen is more highly elevated in prostate cancer compared with benign transition zone prostate tissue. Cancer Res 60:756–759
Mikolajczyk SD, Grauer LS, Millar LS et al (1997) A precursor form of PSA (pPSA) is a component of the free PSA in prostate cancer serum. Urology 50:710–714
Mikolajczyk SD, Rittenhouse HG (2003) Pro PSA: a more cancer specific form of prostate specific antigen for the early detection of prostate cancer. Keio J Med 52:86–91
Sokoll LJ, Chan DW, Mikolajczyk SD, Rittenhouse HG, Evans CL, Linton HJ et al (2003) Proenzyme psa for the early detection of prostate cancer in the 2.5-4.0 ng/ml total psa range: preliminary analysis. Urology 61:274–276
Khan MA, Partin AW, Rittenhouse HG, Mikolajczyk SD, Sokoll LJ, Chan DW et al (2003) Evaluation of proprostate specific antigen for early detection of prostate cancer in men with a total prostate specific antigen range of 4.0 to 10.0 ng/ml. J Urol 170:723–726
Stephan C, Meyer HA, Kwiatkowski M, Recker F, Cammann H, Loening SA et al (2006) A (−5, −7) proPSA based artificial neural network to detect prostate cancer. Eur Urol 50:1014–1020
Filella X, Alcover J, Molina R, Luque P, Corral JM, Augé JM et al (2007) Usefulness of proprostate-specific antigen in the diagnosis of prostate cancer. Anticancer Res 27:607–610
Semjonow A, Kopke T, Eltze E, Pepping-Schefers B, Burgel H, Darte C (2010) Pre-analytical in-vitro stability of [−2]proPSA in blood and serum. Clin Biochem 43:926–928
Catalona WJ, Partin AW, Sanda MG, Wei JT, Klee GG, Bangma CH et al (2011) A multicenter study of [−2]pro-prostate specific antigen combined with prostate specific antigen and free prostate specific antigen for prostate cancer detection in the 2.0 to 10.0 ng/ml prostate specific antigen range. J Urol 185:1650–1655
Stephan C, Vincendeau S, Houlgatte A, Cammann H, Jung K, Semjonow A (2013) Multicenter evaluation of [−2]proprostate-specific antigen and the prostate health index for detecting prostate cancer. Clin Chem 59:306–314
Lazzeri M, Haese A, de la Taille A, Palou J, McNicholas T, Lughezzani G et al (2013) Serum isoform [−2]proPSA derivatives significantly improve prediction of prostate cancer at initial biopsy in a total PSA range of 2-10 ng/ml: a multicentric European study. Eur Urol 63:986–994
Filella X, Foj L, Augé JM, Molina R, Alcover J (2014) Clinical utility of %p2PSA and prostate health index in the detection of prostate cancer. Clin Chem Lab Med 52:1347–1355
Loeb S, Sanda MG, Broyles DL, Shin SS, Bangma CH, Wei JT et al (2015) The prostate health index selectively identifies clinically significant prostate cancer. J Urol 193:1163–1169
Filella X, Giménez N (2012) Evaluation of [−2]proPSA and prostate health index (phi) for the detection of prostate cancer: a systematic review and meta-analysis. Clin Chem Lab Med 15:1–11
Wang W, Wang M, Wang L, Adams TS, Tian Y, Xu J (2014) Diagnostic ability of %p2PSA and prostate health index for aggressive prostate cancer: a meta-analysis. Sci Rep 4:5012
Bruzzese D, Mazzarella C, Ferro M, Perdonà S, Chiodini P, Perruolo G et al (2014) Prostate health index vs. percent free prostate-specific antigen for prostate cancer detection in men with “gray” prostate-specific antigen levels at first biopsy: systematic review and meta-analysis. Transl Res 164:444–451
Cantiello F, Russo GI, Ferro M, Cicione A, Cimino S, Favilla V et al (2015) Prognostic accuracy of Prostate Health Index and urinary Prostate Cancer Antigen 3 in predicting pathologic features after radical prostatectomy. Urol Oncol 33(163):e15–e23
Heidegger I, Klocker H, Pichler R, Pircher A, Prokop W, Steiner E et al (2017 Mar 21) ProPSA and the prostate health index as predictive markers for aggressiveness in low-risk prostate cancer-results from an international multicenter study. Prostate Cancer Prostatic Dis 20:271–275. https://doi.org/10.1038/pcan.2017.3
De la Calle C, Patil D, Wei JT, Scherr DS, Sokoll L, Chan DW et al (2015) Multicenter evaluation of the prostate health index to detect aggressive prostate cancer in biopsy naïve men. J Urol 194:65–72
Tosoian JJ, Loeb S, Feng Z, Isharwal S, Landis P, Elliot DJ et al (2012) Association of [−2]proPSA with biopsy reclassification during active surveillance for prostate cancer. J Urol 188:1131–1136
Vickers AJ, Cronin AM, Aus G, Pihl CG, Becker C, Pettersson K et al (2008) A panel of kallikrein markers can reduce unnecessary biopsy for prostate cancer: data from the European randomized study of prostate Cancer screening in Göteborg. Sweden BMC Med 6:19
Vickers A, Cronin A, Roobol M, Savage C, Peltola M, Pettersson K et al (2010) Reducing unnecessary biopsy during prostate cancer screening using a four-kallikrein panel: an independent replication. J Clin Oncol 28:2493–2498
Vickers AJ, Cronin AM, Roobol MJ, Savage CJ, Peltola M, Pettersson K et al (2010) A four-kallikrein panel predicts prostate cancer in men with recent screening: data from the European randomized study of screening for prostate Cancer, Rotterdam. Clin Cancer Res 16:3232–3239
Vickers AJ, Cronin AM, Aus G, Pihl CG, Becker C, Pettersson K et al (2010) Impact of recent screening on predicting the outcome of prostate cancer biopsy in men with elevated prostate specific antigen: data from the European randomized study of prostate Cancer screening in Gothenburg, Sweden. Cancer 116:2612–2620
Vickers AJ, Gupta A, Savage CJ, Pettersson K, Dahlin A, Bjartell A et al (2011) A panel of kallikrein marker predicts prostate cancer in a large, population-based cohort followed for 15 years without screening. Cancer Epidemiol Biomark Prev 20:255–261
Parekh DJ, Punnen S, Sjoberg DD, Asroff SW, Bailen JL, Cochran JS et al (2015) A multi-institutional prospective trial in the USA confirms that the 4Kscore accurately identifies men with high-grade prostate cancer. Eur Urol 68:464–470
Kim EH, Andriole GL, Crawford ED, Sjoberg DD, Assel M, Vickers AJ et al (2017) Detection of high grade prostate cancer among PLCO participants using a prespecified 4-Kallikrein marker panel. J Urol 197:1041–1047
Vickers A, Vertosick EA, Sjoberg DD, Roobol MJ, Hamdy F, Neal D et al (2017) Properties of the 4-Kallikrein panel outside the diagnostic gray zone: meta-analysis of patients with positive digital rectal examination or prostate specific antigen 10 ng/ml and above. J Urol 197(3 Pt 1):607–613
Lin DW, Newcomb LF, Brown MD, Sjoberg DD, Dong Y, Brooks JD et al (2016 Nov 23) Evaluating the Four Kallikrein Panel of the 4Kscore for prediction of high-grade prostate cancer in men in the Canary Prostate Active Surveillance Study. Eur Urol pii:S0302–2838(16):30850–30858
Stattin P, Vickers AJ, Sjoberg DD, Johansson R, Granfors T, Johansson M et al (2015) Improving the specificity of screening for lethal prostate cancer using prostate-specific antigen and a panel of kallikrein markers: a nested case-control study. Eur Urol 68:207–213
Lughezzani G, Lazzeri M, Larcher A, Lista G, Scattoni V, Cestari A et al (2012) Development and internal validation of a prostate health index based nomogram for predicting prostate cancer at extended biopsy. J Urol 188:1144–1150
Lughezzani G, Lazzeri M, Haese A, McNicholas T, de la Taille A, Buffi NM et al (2014) Multicenter european external validation of a prostate health index-based nomogram for predicting prostate cancer at extended biopsy. Eur Urol 66:906–912
Filella X, Foj L, Alcover J (2014) Aug é JM, Molina R, Jiménez W. The influence of prostate volume in prostate health index performance in patients with total PSA lower than 10 μ g/L. Clin Chim Acta 436:303–307
Roobol M, Vedder MM, Nieboer D, Houlgatte A, Vincendeau S, Lazzeri M et al (2015) Comparison of two prostate Cancer risk calculators that include the prostate health index. European Urology Focus 1:185–190
Loeb S, Shin SS, Broyles DL, Wei JT, Sanda M, Klee G et al (2017) Prostate health index improves multivariable risk prediction of aggressive prostate cancer. BJU Int 120:61–68
Leyten GH, Hessels D, Smit FP, Jannink SA, de Jong H, Melchers WJ et al (2015) Identification of a candidate gene panel for the early diagnosis of prostate Cancer. Clin Cancer Res 21:3061–3070
Hessels D, de Jong H, Jannink SA, Carter M, Krispin M, Van Criekinge W et al (2017) Analytical validation of an mRNA-based urine test to predict the presence of high-grade prostate cancer. Translational Medicine Communications 2:5. https://doi.org/10.1186/s41231-017-0014-8
Bussemakers MJ, van Bokhoven A, Verhaegh GW, Smit FP, Karthaus HF, Schalken JA et al (1999) DD3: a new prostate-specific gene, highly overexpressed in prostate cancer. Cancer Res 59:5975–5979
Lemos AE, Ferreira LB, Batoreu NM, de Freitas PP, Bonamino MH, Gimba ER (2016) PCA3 long noncoding RNA modulates the expression of key cancer-related genes in LNCaP prostate cancer cells. Tumour Biol 37:11339–11348
Filella X, Foj L, Milà M, Augé JM, Molina R, Jiménez W (2013) PCA3 in the detection and management of early prostate cancer. Tumour Biol 34:1337–1347
Ruiz-Aragón J, Márquez-Peláez S (2010) Assessment of the PCA3 test for prostate cancer diagnosis: a systematic review and metaanalysis. Actas Urol Esp 34:346–355
De la Taille A, Irani J, Graefen M, Chun F, de Reijke T, Kil P et al (2011) Clinical evaluation of the PCA3 assay in guiding initial biopsy decisions. J Urol 185:2119–2125
Crawford ED, Rove KO, Trabulsi EJ, Qian J, Drewnowska KP, Kaminetsky JC et al (2012) Diagnostic performance of PCA3 to detect prostate cancer in men with increased prostate specific antigen: a prospective study of 1962 cases. J Urol 188:1726–1731
Capoluongo E, Zambon CF, Basso D, Boccia S, Rocchetti S, Leoncini E et al (2014) PCA3 score of 20 could improve prostate cancer detection: results obtained on 734 Italian individuals. Clin Chim Acta 429:46–50
Chevli KK, Duff M, Walter P, Yu C, Capuder B, Elshafei A et al (2014) Urinary PCA3 as a predictor for prostate cancer in a cohort of 3073 men undergoing initial prostate biopsy. J Urol 191:1743–1748
Foj L, Milà M, Mengual L, Luque P, Alcaraz A, Jiménez W et al (2014) Real-time PCR PCA3 assay is a useful test measured in urine to improve prostate cancer detection. Clin Chim Acta 435:53–58
Bradley LA, Palomaki GE, Gutman S, Samson D, Aronson N (2013) Comparative effectiveness review: prostate cancer antigen 3 testing for the diagnosis and management of prostate cancer. J Urol 190:389–398
Roobol MJ, Schröder FH, van Leeuwen P, Wolters T, van den Bergh RC, van Leenders GJ et al (2010) Performance of the prostate cancer antigen 3 (PCA3) gene and prostate-specific antigen in prescreened men: exploring the value of PCA3 for a first-line diagnostic test. Eur Urol 58:475–481
Haese A, de la Taille A, van Poppel H, Marberger M, Stenzl A, Mulders PF et al (2008) Clinical utility of the PCA3 urine assay in European men scheduled for repeat biopsy. Eur Urol 54:1081–1088
Schröder FH, Venderbos LD, van den Bergh RC, Hessels D, van Leenders GJ, van Leeuwen PJ et al (2014) Prostate cancer antigen 3: diagnostic outcomes in men presenting with urinary prostate cancer antigen 3 scores ≥ 100. Urology 83:613–616
Auprich M, Chun FK, Ward JF, Pummer K, Babaian R, Augustin H et al (2011) Critical assessment of preoperative urinary prostate cancer antigen 3 on the accuracy of prostate cancer staging. Eur Urol 59:96–105
Tomlins SA, Rhodes DR, Perner S, Dhanasekaran SM, Mehra R, Sun XW et al (2005) Recurrent fusion of TMPRSS2 and ETS transcription factor genes in prostate cancer. Science 310:644–648
Deplus R, Delliaux C, Marchand N, Flourens A, Vanpouille N, Leroy X et al (2017) TMPRSS2-ERG fusion promotes prostate cancer metastases in bone. Oncotarget 8:11827–11840
Tomlins SA, Laxman B, Dhanasekaran SM, Helgeson BE, Cao X, Morris DS et al (2007) Distinct classes of chromosomal rearrangements create oncogenic ETS gene fusions in prostate cancer. Nature 448:595–599
Sanguedolce F, Cormio A, Brunelli M, D'Amuri A, Carrieri G, Bufo P et al (2016) Urine TMPRSS2: ERG fusion transcript as a biomarker for prostate Cancer: literature review. Clin Genitourin Cancer 14:117–121
Leyten GH, Hessels D, Jannink SA, Smit FP, de Jong H, Cornel EB et al (2014) Prospective multicentre evaluation of PCA3 and TMPRSS2-ERG gene fusions as diagnostic and prognostic urinary biomarkers for prostate cancer. Eur Urol 65:534–542
Tomlins SA, Day JR, Lonigro RJ, Hovelson DH, Siddiqui J, Kunju LP et al (2016) Urine TMPRSS2:ERG plus PCA3 for individualized prostate cancer risk assessment. Eur Urol 70:45–53
Sanda MG, Feng Z, Howard DH, Tomlins SA, Sokoll LJ, Chan DW et al (2017 May 18) Association between combined TMPRSS2:ERG and PCA3 RNA urinary testing and detection of aggressive prostate Cancer. JAMA Oncol 3:1085–1093. https://doi.org/10.1001/jamaoncol.2017.0177
Stephan C, Cammann H, Jung K (2015) Re: Scott a. Tomlins, John R. Day, Robert J. Lonigro, et al. urine TMPRSS2:ERG plus PCA3 for individualized prostate Cancer risk assessment. Eur Urol 68:e106–e107
Friedman RC, Farh KK, Burge CB, Bartel DP (2009) Most mammalian mRNAs are conserved targets of microRNAs. Genome Res 19:92–105
Schaefer A, Jung M, Kristiansen G, Lein M, Schrader M, Miller K et al (2010) MicroRNAs and cancer: current state and future perspectives in urologic oncology. Urol Oncol 28:4–13
Brennecke J, Stark A, Russell RB, Cohen SM (2005) Principles of microRNA-target recognition. PLoS Biol 3:e85
Filipowicz W, Bhattacharyya SN, Sonenberg N (2008) Mechanisms of posttranscriptional regulation by microRNAs: are the answers in sight? Nat Rev Genet 9:102–114
Santarpia L, Nicoloso M, Calin GA (2010) MicroRNAs: a complex regulatory network drives the acquisition of malignant cell phenotype. Endocr Relat Cancer 17:51–75
Lewis B, Shih I, Jones-Rhoades MW, Bartel DP, Burge CB (2003) Prediction of Mammalian MicroRNA Targets. Cell 115:787–798
Krek A, Grün D, Poy MN, Wolf R, Rosenberg L, Epstein EJ et al (2005) Combinatorial microRNA target predictions. Nat Genet 37:495–500
Cava C, Colaprico A, Bertoli G, Graudenzi A, Silva TC, Olsen C et al (2017) SpidermiR: an R/Bioconductor package for integrative analysis with miRNA data. Int J Mol Sci 18(2):27. https://doi.org/10.3390/ijms18020274
Griffiths-Jones S (2006) miRBase: the microRNA sequence database. Methods Mol Biol Clifton NJ 342:129–138
Krol J, Loedige I, Filipowicz W (2010) The widespread regulation of microRNA biogenesis, function and decay. Nat Rev Genet 11:597–610
Calin GA, Croce CM (2006) MicroRNA signatures in human cancers. Nat Rev Cancer 6:857–866
Decatur WA, Fournier MJ (2002) rRNA modifications and ribosome function. Trends Biochem Sci 27:344–351
Mitchell PS, Parkin RK, Kroh EM, Fritz BR, Wyman SK, Pogosova-Agadjanyan EL et al (2008) Circulating microRNAs as stable blood-based markers for cancer detection. Proc Natl Acad Sci U S A 105:10513–10518
Mihelich BL, Maranville JC, Nolley R, Peehl DM, Nonn L (2015) Elevated serum microRNA levels associate with absence of high-grade prostate cancer in a retrospective cohort. PLoS One 10:e0124245
Chen ZH, Zhang GL, Li HR, Luo JD, Li ZX, Chen GM et al (2012) A panel of five circulating microRNAs as potential biomarkers for prostate cancer. Prostate 72:1443–1452
Cheng HH, Mitchell PS, Kroh EM, Dowell AE, Chery L, Siddiqui J et al (2013) Circulating microRNA profiling identifies a subset of metastatic prostate cancer patients with evidence of cancer-associated hypoxia. PLoS One 8:e69239
Sharova E, Grassi A, Marcer A, Ruggero K, Pinto F, Bassi P et al (2016) A circulating miRNA assay as a first-line test for prostate cancer screening. Br J Cancer 114:1362–1366
Al-Qatati A, Akrong C, Stevic I, Pantel K, Awe J, Saranchuk J et al (2017) Plasma microRNA signature is associated with risk stratification in prostate cancer patients. Int J Cancer 141:1231–1239
Salido-Guadarrama AI, Morales-Montor JG, Rangel-Escareño C, Langley E, Peralta-Zaragoza O, Cruz Colin JL et al (2016) Urinary microRNA-based signature improves accuracy of detection of clinically relevant prostate cancer within the prostate-specific antigen grey zone. Mol Med Rep 13:4549–4560
Filella X, Foj L (2017) miRNAs as novel biomarkers in the management of prostate cancer. Clin Chem Lab Med 55:715–736
Selth LA, Townley S, Gillis JL, Ochnik AM, Murti K, Macfarlane RJ et al (2012) Discovery of circulating microRNAs associated with human prostate cancer using a mouse model of disease. Int J Cancer 131:652–661
Brase JC, Johannes M, Schlomm T, Falth M, Haese A, Steuber T et al (2011) Circulating miRNAs are correlated with tumor progression in prostate cancer. Int J Cancer 128:608–616
Nguyen HC, Xie W, Yang M, Hsieh CL, Drouin S, Lee GS et al (2013) Expression differences of circulating microRNAs in metastatic castration resistant prostate cancer and low-risk, localized prostate cancer. Prostate 73:346–354
Bryant RJ, Pawlowski T, Catto JW, Marsden G, Vessella RL, Rhees B et al (2012) Changes in circulating microRNA levels associated with prostate cancer. Br J Cancer 106:768–774
Fredsøe J, Rasmussen AKI, Thomsen AR, Mouritzen P, Høyer S, Borre M et al (2017 Mar 9) Diagnostic and prognostic microRNA biomarkers for prostate cancer in cell-free urine. Eur Urol Focus. https://doi.org/10.1016/j.euf.2017.02.018
Metcalf GA, Shibakawa A, Patel H, Sita-Lumsden A, Zivi A, Rama N et al (2016) Amplification-free detection of circulating microRNA biomarkers from body fluids based on fluorogenic oligonucleotide-templated reaction between engineered peptide nucleic acid probes: ppplication to prostate cancer diagnosis. Anal Chem 88:8091–8098
Huang X, Yuan T, Tschannen M, Sun Z, Jacob H, Du M et al (2013) Characterization of human plasma-derived exosomal RNAs by deep sequencing. BMC Genomics 14:319
Raposo G, Stoorvogel W (2013) Extracellular vesicles: exosomes, microvesicles, and friends. J Cell Biol 200:373–383
Théry C, Boussac M, Véron P, Ricciardi-Castagnoli P, Raposo G, Garin J et al (2001) Proteomic analysis of dendritic cell-derived exosomes: a secreted subcellular compartment distinct from apoptotic vesicles. J Immunol 166:7309–7318
Simons M, Raposo G (2009) Exosomes–vesicular carriers for intercellular communication. Curr Opin Cell Biol 21:575–581
Keller S, Sanderson MP, Stoeck A, Altevogt P (2006) Exosomes: from biogenesis and secretion to biological function. Immunol Lett 107:102–108
Cheng L, Sun X, Scicluna BJ, Coleman BM, Hill AF (2014) Characterization and deep sequencing analysis of exosomal and non-exosomal miRNA in human urine. Kidney Int 86:433–444
Cheng L, Sharples RA, Scicluna BJ, Hill AF (2014 Mar) Exosomes provide a protective and enriched source of miRNA for biomarker profiling compared to intracellular and cell-free blood. J Extracell Vesicles 26:3. https://doi.org/10.3402/jev.v3.23743
Mall C, Rocke DM, Durbin-Johnson B, Weiss RH (2013) Stability of miRNA in human urine supports its biomarker potential. Biomark Med 7:623–631
Hessvik NP, Sandvigm K, Llorente A (2013) Exosomal miRNAs as biomarkers for prostate Cancer. Front Genet 4:36
Chevillet JR, Kang Q, Ruf IK, Briggs HA, Vojtech LN, Hughes SM et al (2014) Quantitative and stoichiometric analysis of the microRNA content of exosomes. Proc Natl Acad Sci U S A 111:14888–14893
Skog J, Würdinger T, van Rijn S, Meijer DH, Gainche L, Sena-Esteves M et al (2008) Glioblastoma microvesicles transport RNA and proteins that promote tumour growth and provide diagnostic biomarkers. Nat Cell Biol 10:1470–1476
Arroyo JD, Chevillet JR, Kroh EM, Ruf IK, Pritchard CC, Gibson DF et al (2011) Argonaute2 complexes carry a population of circulating microRNAs independent of vesicles in human plasma. Proc Natl Acad Sci U S A 108:5003–5008
Gallo A, Tandon M, Alevizos I, Illei GG (2012) The majority of microRNAs detectable in serum and saliva is concentrated in exosomes. PLoS One 7:e30679
Li Z, Ma YY, Wang J, Zeng XF, Li R, Kang W et al (2015) Exosomal microRNA-141 is upregulated in the serum of prostate cancer patients. Onco Targets Ther 9:139–148
Huang X, Yuan T, Liang M, Du M, Xia S, Dittmar R et al (2015) Exosomal miR-1290 and miR-375 as prognostic markers in castration-resistant prostate cancer. Eur Urol 67:33–41
Foj L, Ferrer F, Serra M, Arévalo A, Gavagnach M, Giménez N et al (2017) Exosomal and non-Exosomal urinary miRNAs in prostate Cancer detection and prognosis. Prostate 77:573–583
Samsonov R, Shtam T, Burdakov V, Glotov A, Tsyrlina E, Berstein L et al (2016) Lectin-induced agglutination method of urinary exosomes isolation followed by mi-RNA analysis: application for prostate cancer diagnostic. Prostate 76:68–79
Alhasan AH, Kim DY, Daniel WL, Watson E, Meeks JJ, Thaxton CS et al (2012) Scanometric microRNA array profiling of prostate cancer markers using spherical nucleic acid-gold nanoparticle conjugates. Anal Chem 84:4153–4160
Alhasan AH, Scott AW, Wu JJ, Feng G, Meeks JJ, Thaxton CS et al (2016) Circulating microRNA signature for the diagnosis of very high-risk prostate cancer. Proc Natl Acad Sci U S A 113:10655–10660
Auprich M, Bjartell A, Chun FK, de la Taille A, Freedland SJ, Haese A et al (2011) Contemporary role of prostate cancer antigen 3 in the management of prostate cancer. Eur Urol 60:1045–1054
Russo GI, Regis F, Castelli T, Favilla V, Privitera S, Giardina R et al (2017) A systematic review and meta-analysis of the diagnostic accuracy of prostate health index and 4-kallikrein panel score in predicting overall and high-grade prostate cancer. Clin Genitourin Cancer 15:429–439
Nordström T, Vickers A, Assel M, Lilja H, Grönberg H, Eklund M (2015) Comparison between the four-kallikrein panel and prostate health index for predicting prostate Cancer. Eur Urol 68:139–146
Scattoni V, Lazzeri M, Lughezzani G, de Luca S, Passera R, Bollito E et al (2013) Head-to-head comparison of prostate health index and urinary PCA3 for predicting cancer at initial or repeat biopsy. J Urol 190:496–501
Stephan C, Jung K, Semjonow A, Schulze-Forster K, Cammann H, Hu X et al (2013) Comparative assessment of urinary prostate cancer antigen 3 and TMPRSS2:ERG gene fusion with the serum [−2]proprostate-specific antigen-based prostate health index for detection of prostate cancer. Clin Chem 59:280–288
Vedder MM, de Bekker-Grob EW, Lilja HG, Vickers AJ, van Leenders GJ, Steyerberg EW et al (2014) The added value of percentage of free to total prostate-specific antigen, PCA3, and a kallicrein panel to the ERSPC risk calculator for prostate Cancer in prescreened men. Eur Urol 66:1109–1115
Prostate Cancer Early Detection (2017) National Cancer Comprehensive Network Clinical Practice Guidelines in Oncology. Version I. 2017. Available online: https://www.nccn.org/professionals/physician_gls/pdf/prostate_detection.pdf (Accessed on 18 August 2017)
Mottet N, Bellmunt J, Briers E, Bolla M, Cornford P, de Santis M, et al. (n.d.) EAU Guideliness prostate cancer. Available online: http://uroweb.org/guideline/prostate-cancer/ (Accessed on 18 August 2017)
Vickers AJ, Eastham JA, Scardino PT, Lilja H (2016) The memorial Sloan Kettering Cancer center recommendations for prostate Cancer screening. Urology 91:12–18
Watson MJ, George AK, Maruf M, Frye TP, Muthigi A, Kongnyuy M et al (2016) Risk stratification of prostate cancer: integrating multiparametric MRI, nomograms and biomarkers. Future Oncol 12:2417–2430
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Filella, X., Foj, L. (2018). Novel Biomarkers for Prostate Cancer Detection and Prognosis. In: Schatten, H. (eds) Cell & Molecular Biology of Prostate Cancer. Advances in Experimental Medicine and Biology, vol 1095. Springer, Cham. https://doi.org/10.1007/978-3-319-95693-0_2
Download citation
DOI: https://doi.org/10.1007/978-3-319-95693-0_2
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-95692-3
Online ISBN: 978-3-319-95693-0
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)