Abstract
Jaundice in the newborn is one of the most common clinical issues encountered by providers in the nursery. While neonatal jaundice is a normal physiologic event, it may at times reach levels that can cause long-term and permanent sequelae. Recognition of the risk factors for hyperbilirubinemia, timely management and monitoring of jaundice, and the correct treatment decisions will help to prevent these sequelae. Management of jaundice in the nursery is also complicated by the need to predict the level of bilirubin not only in the nursery but also after discharge. This chapter will discuss risk factors for jaundice, screening tools, and management of patients who develop jaundice.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Jaundice, the clinical presentation of hyperbilirubinemia, remains one of the most common clinical problems in all of pediatrics. Nearly every baby has a rise in bilirubin, and in 60–84% of all babies [1, 2], it becomes clinically apparent so that the baby appears jaundiced to the observer. Jaundice is a normal physiologic event in the newborn, but the elevated bilirubin is almost always indirect (unconjugated) bilirubin which at high levels can enter into tissues (i.e., the brain). This rarely occurs, but if it does, serious complications with lifelong consequences (e.g., VIII nerve deafness, kernicterus) may result [3].
In the nursery, the provider is faced with a common occurrence, jaundice, which will usually not peak until after discharge and outside the hospital setting but which in rare circumstances may have a devastating effect on the baby. How to anticipate and manage jaundice and to provide a measured plan that will not lead to overtreatment but also prevent serious damage is a daily nursery dilemma. Anticipating that jaundice in some degree may appear in every baby, and having a designed approach to jaundice is basic to newborn care management.
Case Presentation
It’s Friday morning, and you are examining a 36-h-old neonate whose parents are anxious to go home. The baby is a male, 6 lb, 6 oz, 37 2/7 weeks of gestational age (accurate artificial insemination). The mother is 35 years old, G1P0, B+, and of Korean ethnicity with gestational diabetes.
There was prolonged rupture of the membranes for 37 h. She was induced with Pitocin and was delivered by vacuum extraction. Apgar score was 9/10.
The baby has been doing well. The weight is stable, and he is taking breast milk with supplementation. The exam is unremarkable except for a caput and ecchymosis on the scalp. The head and chest examinations are normal. The abdomen is soft, and there is no palpable liver or spleen. The baby has jaundice which covers the head, shoulders, and chest.
At this time you:
-
1.
Order a transcutaneous bilirubin.
-
2.
Order a total serum bilirubin.
-
3.
Discharge the patient with follow-up within 24 h.
-
4.
Place the baby under phototherapy.
Many nurseries have instituted universal screening for bilirubin prior to discharge. Babies may be screened by either transcutaneous bilirubin readings or by a heel stick serum bilirubin. (All published guidelines citing bilirubin values are based on heel stick determinations of bilirubin). If your nursery has a screening policy, then you would already have a pre-discharge value for bilirubin. If universal screening is not in place in your nursery, then as the provider you must have a systematic approach to assessing the level of jaundice and how to manage this issue during the nursery stay, at the time of discharge, and following discharge.
Visible jaundice to the chest at 36 h of life would warrant an assessment of bilirubin levels [4]. While clinical assessment of skin color can be an indicator of hyperbilirubinemia, accurate clinical assessment has wide variance and has been documented to have inconsistent correlation with laboratory values [5, 6]. Therefore performing a transcutaneous bilirubin [1] or drawing a serum bilirubin [2] would be the proper response.
Answer:
(1 or 2)
In this case a transcutaneous bilirubin was done and was reported as 12.5 mg/dL.
At this time you:
-
1.
Order a total serum bilirubin.
-
2.
Hold discharge and order a follow-up transcutaneous bilirubin in 4 h.
-
3.
Discharge the patient with a follow-up within 24 h.
-
4.
Place the baby under phototherapy.
Transcutaneous measurement of bilirubin is a screening test [7,8,9]. Correlation with serum bilirubin is accurate at lower levels but is less accurate at levels as they approach 15 mg/dL. The exact value for bilirubin is important, and clinical decisions may be very different over a narrow range of values. Therefore a total serum bilirubin [1] should be drawn at this time to be able to make the proper clinical decision.
Answer:
1
You order a serum bilirubin, and results return an hour later. The bilirubin is 10.4 mg/dL (indirect 9.9, direct 0.5). How would you manage this patient?
-
1.
Discharge with a follow-up on Monday (108 h of age).
-
2.
Discharge and follow up on Saturday (60 h of age).
-
3.
Follow in hospital with further serum bilirubin testing.
-
4.
Place under phototherapy.
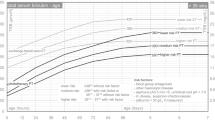
There are a number of tools available to help make your decision. The first is the Bhutani nomogram (Fig. 6.1) for the designation of risk for future hyperbilirubinemia [10]. As with all the nomograms and graphs used to manage neonatal jaundice, it is imperative that values are plotted on the graphs on an hour-to-hour basis. Bilirubin rises rapidly in the first 72 h of life, and what is considered normal at one time may be abnormal at another. A bilirubin of 10 mg/dL during the second day of life may be worrisome at 25 h of age and much less concerning at 47 h of age.
Estimation of risk for hyperbilirubinemia . Bilirubin values defining risk zones. The Bhutani nomogram delineates the risk zones (low, low intermediate, high intermediate, and high) for developing clinically significant hyperbilirubinemia (≥95th percentile for age) in term and late pre-term well neonates based on hour-specific serum bilirubin values. In addition to the risk zone, the clinician must consider risk factors present at the time of discharge. If risk factor(s) are present, the baby may still be at risk even if they fall in a lower risk factor zone [10]
Using the Bhutani nomogram, this baby with a bilirubin of 10.4 mg/dL plots out in the top of the high-intermediate zone.
The Bhutani nomogram is an indicator of risk and does not determine what treatment a baby should receive. The majority of babies (60%) who originally plot out in the high-risk zone will fall below the 95th percentile on future bilirubin measurements, while 79% of the high-intermediate group will have their bilirubin decrease on subsequent bilirubin determinations [10]. In the publication presenting the nomogram, it was reported that there was a little risk for subsequent hyperbilirubinemia for babies who were in the low-intermediate and low zones. Several subsequent reports have shown that these babies may also be at risk for hyperbilirubinemia requiring phototherapy [11, 12]. As emphasized in Dr. Bhutani’s original paper, the provider must not only determine the risk zone but also determine what risk factors are present and their potential effect on bilirubin metabolism (Table 6.1).
Without knowing the risk factors, a follow-up within 24 h of discharge (60 h of age) or keeping in the hospital for further observation is an acceptable choice. Discharge with a follow-up in 3 additional days might allow time for bilirubin to rise to critical levels. Placing a baby under phototherapy should be determined by the graphs contained in the phototherapy guidelines (Fig. 6.2).
Guideline for bilirubin threshold for initiation of phototherapy in hospitalized term and late preterm neonates. Graphic presentation of the guideline for the bilirubin level at which phototherapy should be initiated. At any given hour, the level to start phototherapy will vary depending on gestational age and presence of risk factors. Risk factors include ABO incompatibility, Rh incompatibility, other isoimmune hemolytic diseases, G-6-P-D (G6PD deficiency), asphyxia, lethargy, temperature instability, sepsis, acidosis, and albumin <3.0 m/dL (if measured) and differ from the risk factors for the development of hyperbilirubinemia [13]. Use total bilirubin. Do not subtract direct reacting or conjugated bilirubin; For well infants 35–37 6/7 week the clinician can adjust TSB levels for intervention around the medium risk line. It is an option to intervene at lower TSB levels for infants closer to 35 weeks and at higher TSB levels for those closer to 37 6/7 week; It is an option to provide conventional phototherapy in hospital or at home at TSB levels 2–3 mg/dL (35–50 mmol/L) below those shown but home phototherapy should not be used in any infant with risk factors
Answer:
2 or 3
How many risk factors were present in this patient?
-
1.
None
-
2.
2–5
-
3.
6–9
-
4.
≥10
Answer:
3
This patient had a large number of risk factors for subsequent hyperbilirubinemia, and this must be considered in decision-making. It should also be remembered that these are risk factors for developing hyperbilirubinemia and are different than those used when determining whether phototherapy and/or exchange transfusion are necessary [13, 14]. In the above case, many of the risk factors for subsequent hyperbilirubinemia were present and even the bilirubin was in the high-intermediate zone. Further observation in the hospital could certainly be an appropriate course of action. Discharge with close follow-up could also be considered. One risk factor not noted in the criteria below is a Friday discharge. You, as the responsible health-care provider, must be certain that there will be follow-up at the appropriate time. A follow-up bilirubin within 24 h is necessary in this case and might be determined with a transcutaneous reading (which would need a serum bilirubin done if in the high range) of serum bilirubin. A mechanism for bilirubin measurements on weekends should be in place if at risk newborns are to be discharged on Thursdays and Fridays.
The AAP guideline for hyperbilirubinemia [13, 14] makes recommendations for follow-up. Discharged newborns should be examined by a qualified health-care professional in the first few days after discharge to assess infant well-being and the presence or absence of jaundice. It is also helpful for other issues including the adequacy of feedings.
Infant discharged | Should be seen by age |
|---|---|
Before age 24 h | 72 h |
Between 24 and 47.9 h | 96 h |
Between 48 and 72 h | 120 h |
When and where this assessment will occur are determined by the age (in hours) at discharge, presence or absence of risk factors for hyperbilirubinemia (as above), and risk of other neonatal problems. For some newborns discharged before 48 h, two follow-up visits may be required. The first visit is between 24 and 72 h, and the second visit is between 72 and 120 h. Clinical judgment should be used in determining a follow-up. Earlier or more frequent follow-up should be provided for those who have risk factors for hyperbilirubinemia. Those discharged with few or no risk factors can be seen after longer intervals.
If appropriate follow-up cannot be ensured in the presence of elevated risk for developing hyperbilirubinemia, it may be necessary to delay discharge either until appropriate follow-up can be ensured or the period of greatest risk has passed (72–96 h).
The patient had a 10.4 bilirubin at 36 h of life. Is he a candidate for phototherapy?
-
1.
Yes
-
2.
No
Although this baby was only in the high-intermediate zone for risk, he is between 36 and 38 weeks. Whether or not to start phototherapy is not based on the risk zones from the Bhutani nomogram but from the criteria for the initiation of phototherapy published in the AAP guideline for hyperbilirubinemia [13].
Phototherapy would be considered at a lower level in a baby who is 35–37 6/7 weeks compared to a ≥38 week’s baby without risk. Another useful guide for determining the need for phototherapy is the application, BiliTool . This application incorporates the criteria from the AAP guidelines and is used by many clinicians [15].
As mentioned previously, the risk factors that are considered in the decision to start phototherapy differ from those for the risk of hyperbilirubinemia. These include the gestational age of the baby. The less mature the baby, the lower the threshold for initiation of phototherapy. Also the presence of hemolytic disease, including isoimmune hemolytic disease and G6PD deficiency, asphyxia, significant lethargy, temperature instability, sepsis, acidosis, or low albumin <3.0 mg/dL (if measured), would require starting phototherapy at a lower bilirubin level than in a baby with no risk factors.
Answer:
2
At this time the bilirubin level of 10.4 mg/dL is below the phototherapy value to initiate phototherapy in a neonate with medium risk (12.6 mg/dL).
An appropriate course of treatment might be:
-
1.
Start a non-intensive phototherapy.
-
2.
Start an intensive phototherapy.
-
3.
Continue to observe, and repeat bilirubin in 6–8 h.
-
4.
Discharge patient with follow-up in 24 h.
While some clinicians adjust the medium risk line on the phototherapy graph, starting phototherapy below the line for newborns closer to 35 weeks, the patient in this case is 37 2/7 weeks. It should also be remembered that the phototherapy graphs were designed to prevent kernicterus and have latitude in protecting the patient from developing complications of hyperbilirubinemia. In addition phototherapy is an intervention which for many years has been thought to be totally safe. However, new concerns are being raised. While phototherapy has been utilized for over 40 years in the United States, when originally introduced, the energy of the phototherapy lights was between 5 and 10 μw/cm2/nm. As the intensity of the lights has increased, their energy output (30–40 μw/cm2/nm) has increased as well. Will the increased intensity of the phototherapy lights utilized in the last several years lead to complications not seen previously? Recent reports of DNA breakage [16], precancerous skin lesions [17], and an increased risk of childhood cancer [18] should make clinicians aware that long-term complications may potentially be present and may now only begin to appear. Phototherapy also has several immediate side effects. It may interfere with maternal bonding, decrease the success of breastfeeding, and increase hospital length of stay [19]. With these factors in mind, phototherapy should not be started until the criteria for treatment are met. Continuing to observe and repeat bilirubin in 6–8 h is a prudent course of management.
Answer:
3
Following this treatment choice, two scenarios are possible.
Scenario 1:
A repeat serum bilirubin 8 h later (44 h of life) is repeated and is reported as 10.5 mg/dL.
-
1.
You are surprised because patients in the high-intermediate risk zone usually continue to increase and require phototherapy.
-
2.
You expected this result because the majority of patients in the high-intermediate zone infrequently cross the 95th percentile and don’t require phototherapy.
In Bhutani’s study on the experience with his nomogram, only 21% of babies in the high-intermediate group crossed over the 95th percentile on a subsequent bilirubin determination, and only 40% in the high-risk zone had a similar rise [10]. It should again be emphasized that the Bhutani nomogram is a measure of risk not a guide to therapy. While high risk in the nomogram is >95th percentile, the phototherapy graph (13) does not initiate phototherapy in a full-term baby without risk factors until the 99th percentile.
At this time the bilirubin level of 10.5 mg/dL is below the medium risk line for the initiation of phototherapy (at 44 h ta level of 12.6 mg/dL would require phototherapy).
Answer:
2
An appropriate course of treatment might be:
-
1.
Start a non-intensive phototherapy.
-
2.
Start an intensive phototherapy.
-
3.
Continue to observe and repeat bilirubin in 6–8 h.
-
4.
Discharge patient with follow-up in 24 h.
This baby’s levels have now remained stable over the last 8 h and are well below the levels would have needed to institute phototherapy . The clinical decision is to determine if levels have peaked and will remain stable or decrease or is there a risk of further significant increases will occur warranting phototherapy. If the baby is eating well, is not a setup for or at risk of hemolysis and the baby can be followed within the next 24 h, discharge is an appropriate choice. It should also be remembered that this patient is still being discharged at <48 h of age, making a visit necessary by 96 h. It would be appropriate for this baby to be seen the day following discharge.
Answer:
4
Scenario 2:
A repeat serum bilirubin 8 h later (44 h of life) is repeated and is reported as 14.5 mg/dL.
-
1.
Start a non-intensive phototherapy.
-
2.
Start an intensive phototherapy.
-
3.
Continue to observe and repeat bilirubin in 6–8 h.
-
4.
Discharge patient with follow-up in 24 h.
The baby has now crossed the threshold (12.6 mg/dL) for a baby at medium risk (35–37 6/7 weeks of gestation) for the start of phototherapy . When phototherapy is initiated in the hospital, it should be “intensive phototherapy .” Standard phototherapy delivers an intensity of light in the range of 5–10 mw/cm2/nm, while intensive phototherapy delivers an intensity of >30 mw/cm2/nm.
Answer:
2
The intensity of the phototherapy equipment depends on several factors.
-
1.
Type of light
-
2.
Number of lights
-
3.
Area covered by the lights
-
4.
Distance of the baby from the light
Every hospital should have a protocol as to what is meant by intensive phototherapy [13]. Is it double lights (which may be delivered by one device)? Is it light above and below the baby? Is it done in an Isolette or in a bassinet? All these factors will determine the dose of light the baby receives.
-
1.
Type of lights . A number of devices are effective in delivering light in the range of 430–490 nm. Special blue fluorescent tubes are the most efficient for use in traditional phototherapy units. Light-emitting diode (LED) lights are also in common use. Fiber-optic blankets and specially designed units for placement under the baby are also available.
-
2.
Numbers of lights . Several of the LED lights can deliver a single or double dose of light. Intensive phototherapy would usually require the double mode. Placing banks of fluorescent (special blue) lights can increase dosing, but surrounding the baby with banks of lights is often cumbersome. Systems that deliver light from below the baby can also increase the dosing of light. This may include placing the baby on a biliblanket or in a specially designed bassinet that can deliver light from below.
-
3.
Area covered by the lights can be increased by surrounding the baby with light as mentioned previously and assuring that the baby is centered in the field of light. Irradiance at the periphery is of the field of light which is far less than in the center.
-
4.
Distance from the light source to the baby . The further the light from the baby, the less the dose of light. While many hospitals place babies in an Isolette for phototherapy and an intensive dose of light can be delivered (>30 mw/cm2/nm), if necessary babies can be treated in an open bassinet and the lights brought closer to the baby to increase the intensity.
Intensive phototherapy with lights delivering a double dose of light from above and light from below is usually very effective in decreasing the bilirubin level. The effect is greater at the higher bilirubin levels when therapy is started and rates of decline of 0.5–1.0 mg/dL/h are not uncommon when the lights are first started.
Answer:
1, 2, 3, 4
The baby has been placed under the phototherapy lights. Which of the following should be done?
-
1.
Stop breastfeeding.
-
2.
Repeat bilirubin measurement in 2 h.
-
3.
Repeat bilirubin measurement in 4 h.
-
4.
Repeat bilirubin measurement in 6 h.
-
5.
Repeat bilirubin measurement in 8 h.
Breastfeeding should not be stopped but rather encouraged. In fact, increasing the frequency of feedings may be helpful in decreasing bilirubin levels. Other strategies may include taking the baby out from under the lights to allow for breastfeeding, using a biliblanket to wrap the baby during time-out from under the lights, and pumping the mother’s breast for milk to be bottle or spoon-fed (considered as a last alternative by some). Unless the baby is dehydrated, supplementing the baby with water, formula, or glucose water has no effect on unconjugated bilirubin levels because it is not water soluble [20].
The frequency of reassessing bilirubin levels is a clinical decision that involves several factors. If the level was approaching the value that would require exchange transfusion, more frequent evaluation might be considered. It would be unusual for bilirubin to continue to rise unless there is a hemolytic process as the underlying cause of the hyperbilirubinemia. In most cases intensive phototherapy can reduce bilirubin by 0.5–1.0 mg/dL/h. The higher the bilirubin at the initiation of phototherapy, the faster the decline.
Repeat levels, except in the situation cited above, do not need to be repeated for 6–8 h, giving the phototherapy an opportunity to have an effect.
Answer:
4 or 5
What laboratory test (s) would be ordered when a patient is placed under phototherapy?
-
1.
CBC with differential
-
2.
Reticulocytes
-
3.
Sepsis workup
-
4.
G6PD analysis
-
5.
Liver enzymes
-
6.
Direct bilirubin
-
7.
Coombs’ test
-
8.
Blood type
-
9.
Urine for reducing substance
Discussion: [13]
-
1.
CBC with differential: to determine if a hemolytic process is occurring and if sepsis might be a possibility.
-
2.
Reticulocytes: to determine if a hemolytic process is occurring.
-
3.
Sepsis workup: may be considered if suggested by history and physical exam.
-
4.
G6PD analysis: If family history ethnic or geographic origin suggest. Also if a poor response to phototherapy or unexplained hemolysis.
-
5.
Liver enzymes: not for indirect hyperbilirubinemia.
-
6.
Direct bilirubin: At this time total serum bilirubin should be fractionated (direct and indirect).
-
7.
Coombs’ test: If not previously done.
-
8.
Blood type: If not previously done.
-
9.
Urine for reducing substance: Galactosemia would be a rare cause of neonatal jaundice, and reducing substances in the urine could be an early indicator (most cases are now identified on newborn screening).
The level at initiation of phototherapy was 14.5 mg/dL. You would stop phototherapy at:
-
1.
14.5 mg/dL
-
2.
13.5 mg/dL
-
3.
12.5 mg/dL
-
4.
11.5 mg/dL
-
5.
10.5 mg/dL
The decision to decide when to stop phototherapy in a baby who is readmitted for hyperbilirubinemia is relatively straightforward. The decision to stop phototherapy in a baby who has been started during the original hospital stay is less clear. Most babies who are readmitted for hyperbilirubinemia are ≥72 h of age, and bilirubin levels are >18 mg/dL at the time of admission. Usually bilirubin conjugation has been established at this age, and the combination of light and maturation will result in a decrease of bilirubin to a safe and usually stable level. In cases of a readmitted baby, a level less than 13–14 mg/dL would be an appropriate level at which to discontinue phototherapy. It would also be appropriate to discharge the patient without a rebound bilirubin level (unless hemolysis is suspected) [13].
In the patient presented above and in whom phototherapy was initiated at 44 h of life during the initial hospital stay for a bilirubin of 14.5 mg/dL, would a subsequent decrease in bilirubin reflect the effect of the lights and/or the maturation of the liver?
If the repeat bilirubin remained at 14.5 mg/dL at 52 h, it would appear that the bilirubin levels would have continued to rise without phototherapy and are still above the line for phototherapy. The lights should be continued.
If at 52 h, bilirubin was 13.5 mg/dL, it would now be just below the threshold for phototherapy treatment. However after 8 h of phototherapy, the bilirubin level would have been expected to fall further, and the concern that the lights are just keeping up with jaundice levels should be considered. Phototherapy should be continued.
If the level fell to 12.5 mg/dL, this is more in line with the effect of phototherapy. The provider may feel both the lights and maturation of the liver have played a role. Discontinuation might be considered by some [21].
A decrease in the bilirubin to 11.5 mg/dL or below is certainly more reassuring and may indicate that both the lights and the maturation of liver conjugation may have had an effect. This level is well below the line for phototherapy. This level of jaundice would permit discontinuation of the lights [20].
Providers should remember that the proper graphs to use in making clinical decisions after phototherapy has been initiated or completed are the graphs for phototherapy and exchange transfusion. The Bhutani nomogram is used to assess risk for future jaundice and cannot be used after the use of phototherapy.
Answer:
3 or 4
Would you now order a rebound bilirubin?
-
1.
Yes
-
2.
No
If you are suspicious or knew that hemolysis was the cause of the jaundice, a rebound bilirubin level is indicated. Providers should also be aware that when phototherapy has been initiated early on in the nursery course, phototherapy may prevent increases in bilirubin. In babies with hemolysis, clinicians are comforted by bilirubin levels that fall below the line for phototherapy but need a rebound level to see if levels without lights will again start to increase. Since the phototherapy graph reflects the natural increase of bilirubin levels in the first days of life, a steady or decreasing level below the line for treatment may not reflect that hemolysis is continuing. The baby may not be able to keep levels in the safe zone without phototherapy. Even with a safe rebound level , these babies should be seen and evaluated within 24 h of discharge [13].
In babies where hemolysis is not the underlying cause for hyperbilirubinemia but who had phototherapy in the first 72–96 h of life during the birth admission, a bilirubin level should be measured within 24 h of discontinuing phototherapy. As mentioned above in babies readmitted for hyperbilirubinemia and in whom hemolysis is not thought to be the underlying cause of the hyperbilirubinemia, no rebound value is necessary.
Answer:
1
Clinical Pearls
-
1.
Follow the guidelines for follow-up even if a discharge bilirubin is done and may be considered safe.
-
2.
Use the Bhutani nomogram to assess risk, not treatment.
-
3.
Remember risk factors for the development of hyperbilirubinemia. Even babies in the low and low-intermediate zones with risk factors may develop hyperbilirubinemia. Late preterm and breast-fed babies are certainly among this group.
-
4.
Remember risk factors for initiation of phototherapy. They differ from those that put a baby at risk for hyperbilirubinemia.
-
5.
Use phototherapy graphs and their risk stratification to determine if phototherapy is necessary.
-
6.
Encourage breastfeeding. More frequent feedings and supporting the mother are vital to the success of breastfeeding and decreasing the incidence of jaundice.
-
7.
Don’t use phototherapy unless it is indicated (don’t treat prophylactically).
References
Keren R, Tremont K, Luan X, Cnaan A. Visual assessment of jaundice in term and late preterm infants. Arch Dis Child Fetal Neonatal El. 2009;94:F317–22.
Bhutani VK, Stark AR, Lazzeroni LC, Poland R, Gourly GR, Kazmierczak S, et al. Predischarge screening for severe hyperbilirubinemia identifies infants who need phototherapy. J Pediatr. 2013;162:477–82.e1.
Watchko JF, Tiribelli C. Bilirubin induced neurologic damage: mechanisms and management approaches. N Engl J Med. 2013;369:2021.
Kramer LI. Advancement of dermal icterus in the jaundiced newborn. Amer J Dis Child. 1969;118:454.
Moyer VA, Ahn C, Sneed S. Accuracy of clinical judgment in neonatal jaundice. Arch Pediatr Adolesc Med. 2000;154:391.
Tayaba R, Gribetz D, Gribetz D, Holzman IR. Noninvasive estimation of serum bilirubin. Pediatrics. 1998;102:E28.
Engle W, Jackson GL, Engle NG. Transcutaneous bilirubinometry. Semin Perinat. 2014;38:438.
Rubaltelli FF, Gourley GR, Loskamp N, Modi N, Roth-Kleiner M, Sender A, Vert P. Transcutaneous bilirubin measurement: a multicenter evaluation of a new device. Pediatrics. 2001;107:1264.
Taylor JA, Burgos AE, Flaherman V, Chung E, Simpson EA, Goyal NK, Von Kohorn I, Dhepyasuwan N, The Better Outcomes Through Research Network. Discrepancies between transcutaneous and serum bilirubin measurements. Pediatrics. 2015;135:224. https://doi.org/10.1542/peds.2014-1919.
Bhutani VK, Johnson L, Sivieri MS. Predictive ability of a pre-discharge serum bilirubin for subsequent significant hyperbilirubinemia in healthy term and near-term newborns. Pediatrics. 1999;103:6.
Bromiker R, Bin-Nun A, Schimmel MS, Hammerman C, Kaplan M. Neonatal hyperbilirubinemia in the low-intermediate-risk category on the bilirubin nomogram. Pediatrics. 2012;130:e470. https://doi.org/10.1542/peds.2012-0005.
Slaughter J, Annibale D, Suresh G. False-negative results of pre-discharge bilirubin screening to predict severe hyperbilirubinemia: a need for caution. Eur J Pediatr. 2009;168:1461.
American Academy of Pediatrics Subcommittee on Hyperbilirubinemia. Management of hyperbilirubinemia in the newborn infant 35 or more weeks of gestation. Pediatrics. 2004;114:297. https://doi.org/10.1542/peds.114.1.297.
Maisels MJ, Bhutani VK, Bogen D, Newman TB, Ar S, Watchko JF. Hyperbilirubinemia in the newborn infant ≥35 weeks’ gestation: an update with clarification. Pediatrics. 2009;124:1193. https://doi.org/10.1542/peds.2009-0329.
Longhurst C, Turner S, Burgos AE. Development of a web-based decision support tool to increase use of neonatal hyperbilirubinemia guidelines. Jt Comm J Qual Patient Saf. 2009;35:256.
Christensen T, Reitan JB, Kinn G. Single-strand breaks in the DNA of human cells exposed to visible light from phototherapy lamps in the presence and absence of bilirubin. J Photochem Photobiol B. 1990;7:337.
Csoma Z, Toth-Molnar E, Balogh K, et al. Neonatal blue light phototherapy and melanocytic nevi: a twin study. Pediatrics. 2011;128:e856.
Newman TB, Wickeremasinghe C, Walsh EM, Grimes BA, McCulloch CE, Kuzniewicz MW. Retrospective cohort study of phototherapy and childhood cancer in Northern California. Pediatrics. 2016;137:1.
Maisels MJ. Managing the jaundiced newborn. A persistent challenge. CMAJ. 2015;187:335.
Martinez JC, Otheguy L, Garcia H, Savorani M, Mogni B, Martinez JC Jr, Maisels MJ. Hyperbilirubinemia in the breast-fed newborn: a control trial of four interventions. Pediatrics. 1993;91:470.
Barak M, Berger I, Dollberg S, Mimouni FB, Mandel D. When should phototherapy be stopped? A pilot study comparing two targets of serum bilirubin concentrations. Acta Paediatri. 2009;98:277.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Rosenfeld, W. (2019). Jaundice in the Newborn. In: Martin, G., Rosenfeld, W. (eds) Common Problems in the Newborn Nursery. Springer, Cham. https://doi.org/10.1007/978-3-319-95672-5_6
Download citation
DOI: https://doi.org/10.1007/978-3-319-95672-5_6
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-95671-8
Online ISBN: 978-3-319-95672-5
eBook Packages: MedicineMedicine (R0)