Abstract
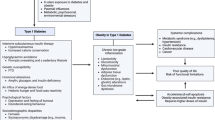
The accumulation of excess fat (adiposity) leads to significant physical, metabolic, hormonal, and psychological changes, which, when combined, define a chronic disease. Thus, treatment must be designed to increase the amount of metabolically functional adipose tissue and combat adiposopathy, instead of merely addressing the complications of this disease. To better address this issue, one should view overweight, obesity, and adiposopathy as a spectrum of what can be a preventable and treatable biological disease. Following this approach, a clinic should adopt a model of treatment similar to those of other long-term endocrine diseases such as diabetes and hypertension. As public and professional attitudes toward obesity begin to reflect the research that documents it is a chronic illness, there exists an opportunity to develop clinics specifically focused on the treatment of patients with obesity or overweight. The unique needs of patients with obesity or overweight, along with the growing obesity rates in America, are a further impetus for the establishment of endocrine practices focused on their long-term treatment. In doing so, not only will a dedicated bariatric endocrine clinic be more effective in the treatment of patients with obesity but also work toward correcting the social stigmatization of obesity which has contributed to the inadequacies of treatment.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
FormalPara Pearls of Wisdom-
Overweight and obesity should be treated with the same model of chronic disease management used for other endocrine and metabolic diseases.
-
The treatment of overweight and obesity must address the social and medical stigmas. Patients with overweight and obesity require special accommodations within the clinic that are essential to success.
-
The desired goal is not merely weight loss but a return of normal metabolism and adipocyte function.
-
Realistic goals specific to each patient will better ensure success and deter relapse.
8.1 Introduction
An effective bariatric endocrinology practice is designed to address the unique neuro-endocrinological considerations of its patients in addition to practical and structural needs required to best facilitate their treatment and ensure the financial success of the clinic itself. The ideal clinic requires the right infrastructure and properly trained staff. An individual encounter should be tailored to mainstream the care of patients with obesity or overweight. The encounter itself necessitates its own nuanced approach with a special focus being given to the patient’s medical and pharmacological history, and regular risk re-stratification, including laboratory testing.
Much like the treatment of diabetes and other endocrine diseases, behavior modification is an essential component not only in the treatment of patients with obesity but also in gauging the success of the course of treatment. A bariatric clinic should offer nutritional and physical activity education for the patient and family and develop realistic, goal-based plans.
It is important to recognize that, as with other chronic endocrine conditions, regular follow-up appointments are essential to assure adherence with the plan of treatment and for ultimate success in the management of the patient with obesity or overweight. Several studies have demonstrated that after initial evaluation, patients with obesity or overweight that were asked to follow-up every month with a dedicated nurse, in order to be weighed and discuss treatment, yielded higher rates of success and adherence to the regimen. Developing long-term strategies for treatment with regular re-evaluation and re-stratification will break from historically short-sighted approaches treating overweight, obesity, and adiposopathy.
8.2 Infrastructure: Clinic, Equipment, and Staff Training
In a study of patients with a body mass index (BMI) greater than 55 kg/m2, 68% of those surveyed reported delay in seeking professional treatment to manage their obesity. The reasons for this delay included past instances of disrespectful treatment, feelings of embarrassment, or inadequate accommodations. An adequate clinic setting in order to promote success in the treatment of obesity or overweight is of paramount importance. A welcoming, sensitive, front desk and nursing staff is integral to maintaining a positive atmosphere. Since many patients with obesity or overweight experience psychological issues often exacerbated by the social stigma surrounding obesity, it is important that all staff members are trained to use “patient-first” language.
In a clinic-based study, 53% of the patients reported inappropriate comments from their doctors about their weight, and doctors were the second most common source of stigma (69%), following family (72%). Stigma and bias refer to negative attitudes that affect our interpersonal interactions and activities in a detrimental way. Stigma may come in several forms, including verbal types of bias (ridicule, teasing, insults, stereotypes, and derogatory names), physical stigma (touching, grabbing, or other aggressive behavior), or other barriers and obstacles due to weight such as medical equipment that is too small or unsafe for patients with obesity or overweight. It is necessary to make patients comfortable as a preliminary step to proper treatment. Strategies should be implemented in the clinical setting in order to reduce weight stigma and improve attitudes within the clinical setting.
The concept of obesity as an illness extends into how the terms “overweight” and “obesity” are used in the clinical setting. These terms should not be used as adjectives and instead referred to only as medical conditions that the patients are being treated for. Thus, “obese patient” would be replaced with “patient with obesity.” The staff should be conscious not to suggest any judgment in their language, gestures, even when the patient is not present, as these may be perceived as disrespectful of the patient’s condition. These initial interactions are an important component of the patient encounter and can help shape it in a positive manner. The same sensitivity applies to the nursing staff’s training in the morphometric assessment of patients, as the habitus of patients with obesity or overweight might present certain difficulties during examination. This will ensure not only consistent measurements but also the comfort of the patient. Staff should be well trained to measure a blood pressure cuff, how to obtain a proper height measurement for the calculation of the BMI, and how to adequately measure waist and hip circumferences.
Due to the size and weight of patients with obesity or overweight, a bariatric endocrinology clinic will need to offer an accommodating workspace ideally suited for the needs of both patient and staff. Wide door frames, hallways, and examination rooms will accommodate severe corpulence and steel-reinforced furniture designed to handle large weights is ideal for waiting and examination rooms. Building entry points need to be designed with comfortable ramps featuring handrails. Doors for examination rooms are recommended to be 3 feet 6 inches wide and the recommended opening size for patient rooms and procedure areas is 4 feet. Paired doors or sliding doors can be used as an alternative. Ample sized, weight-tested wheelchairs should be available to transport patients by the front door. In areas where oversize wheelchairs are to be used, a 72-inch turning radius is recommended, in lieu of the 60-inch radius generally required by the American with Disabilities Act (ADA). In general, it is recommended that 10–20% of general seating in the waiting areas should be specified in bariatric sizes, due to the fact that patients with obesity often times will be accompanied by family members who will require similar types of accommodations.
Bathroom doors and facilities should be equally accommodating to the patient with overweight or obesity. Vitreous China toilets have a maximum capacity of about 300 pounds. The most common solution on the market today is floor-mounted stainless steel toilets. Both toilets and sinks should be floor mounted, and the center line for toilets should be 24 inches versus 18 inches on the center line for a standard toilet. Bathrooms should also be equipped with weight-tested bars or handles on the walls to assist patients and reduce the risk of injury.
A large-sized platform scale (able to accommodate up to 800 pounds) is necessary, as the standard models are unable to handle the weight of many patients. Hydraulic examination tables will also assist patients who have limited mobility as a result of their excess mass, rising from normal sitting level to a height ideal for the examiner. Many other items of standard clinical equipment are not able to accommodate patients with severe obesity. A dedicated bariatric clinic should have examination gowns, blood pressure cuffs, and measuring tapes in extra-large sizes. These fittings along with a thoroughly trained staff will ensure an atmosphere conducive to a comfortable patient encounter. Since many of those with obesity or overweight qualify as having a disability under the ADA, it is important to review the other recommendations outlined in its guidelines. The ADA guide is available from the US Department of Justice.
Contingency plans for emergencies should be in place and well rehearsed. An often-unrecognized need when treating patients with severe obesity is the safety of the health-care professionals who care for them. The National Safety Council reports that the health-care worker is 41% more likely than the average worker to need time off because of serious occupational injuries. An estimated 12% of nurses annually leave their profession due to back injuries. Thus, proper training of the health-care workers on how to prevent this type of injuries when assisting patients around the clinic is essential. OSHA injury prevention guidelines should be reviewed for this purpose. Training in how to physically assist patients with overweight or obesity (such as boosting and lifting) will help prevent any serious injuries to the staff while avoiding discomfort for the patient. In the instance of a medical emergency, an alarm system should be used to notify staff so that multiple staff members can be on hand to assist any patient with excess body weight. Incorporation of this training into evacuation procedures is also important. Staff should be familiar with the necessary procedures to lift a patient weighing over 400 pounds onto a gurney, if needed during an evacuation or medical emergency.
These accommodations are recommended for an ideal clinic that treats patients with obesity or overweight. While financial or structural considerations might limit a clinic’s ability to follow all of these recommendations, the patient’s safety and comfort should be the priority.
8.3 Team Approach to Obesity
Continuing to use the treatment model of chronic endocrine diseases, the team approach is integral to effective long-term lifestyle modification. Access to a variety of educational materials will greatly benefit patients and meet individual needs. Printed and electronic educational materials can greatly enhance patient education in the clinic. Web-based materials can provide patients access to ongoing education between visits. Providing these materials will also aid in recruiting and engaging relatives in the treatment plan. Both at home and at work, the involvement of individuals to support patient behavior change is desirable. Support from others ensures that patients adhere to treatment plans. Other tools such as pedometers or web/mobile applications can allow the patient or family members to track progress on a regular basis. Interactive tools can also provide motivational support to the patient. Monitoring, logging, and objectively measuring progress help achieve short-term, specific goals. In order to achieve long-term goals, it is essential to establish short-term objectives, as not to disenfranchise the patient. Setting goals for activity or weight loss will help the patient adhere to the long-term treatment plan.
Access to a specially designed health-care team is also essential. An ideally staffed clinic might include both well-trained front desk and nursing staff but also nutritionists/dieticians, mental health professionals, behavior counselors, physical therapists, rehabilitation consultants, and sleep and pain specialists. This will allow the clinic to address the multifaceted needs of each patient. A team approach is ideal to effectively treat and manage the many complications caused by obesity or overweight, which, when present, can prevent attainment of treatment goals. Many third-party providers do not cover dietician or nutritionist visits unless bundled with that of a physician. Thus, the team-based model of a bariatric clinic is also ideal for financial success. Providing access to other specialists such as bariatric surgeons and cardiologists in a multispecialty practice helps to meet the overhead of the team.
Group meetings for patients have also been shown to be beneficial. These group meetings can be held in the clinic. Alternatively, patients can be referred to commercial weight loss programs, which have been shown to be successful in conjunction with lifestyle modifications overseen by a medical professional. Commercial weight loss programs can be an alternative for endocrinology clinics with staff or financial limitations, where an in-clinic dietician or other specialist is not feasible. Support groups and group classes have been shown to help engage patients and inspire adherence and dedication to the treatment plan. In-office classes, referral to physical activity education, or health-centric cooking courses can help educate patients to make better choices in their daily lives.
It is important that the team approach encompasses not only trained professionals but also the patient’s family as well. A patient with an invested family network will better adhere to treatment recommendations and have improved outcomes. Awareness of ethnic, cultural, religious, educational, and social differences among patients is also important in discussing meal plan guidelines, as these may provide additional obstacles or advantages to each treatment plan.
8.4 Patient Encounter
Patient encounter provides opportunities for risk stratification (including an obesity-focused review of the medical history), building patient satisfaction and trust, validation of charges, and documentation of all work.
The obesity-focused history will cover any major life events that might have coincided with weight gain. Past events such as changes in career or marital status, medications, pregnancies, and lifestyle are all important to document. Additionally, current habits determine an individual patient’s energy balance. A patient’s medication history will provide opportunities for intervention. There are medications that are well known to cause weight gain. A general strategy is to avoid them and substitute with alternatives that are associated with weight loss (Table 8.1).
A detailed history should also include documentation of current food intake, physical activity levels, and sleeping habits. A psychological assessment for mood disorders is important, as this may contribute to obesity or overweight, or complicate treatment.
Patient assessment should also look for complications of obesity and overweight because many become obstacles to effective weight loss. Sleep apnea, restrictive lung disease, fatigue, osteoarthritis, degenerative disc disease, angina pectoris, peripheral vascular disease, insulin resistance, and hypogonadism are examples of complications of obesity that become obstacles to effective weight loss. These, along with other complications, should be targeted not only to develop a course of treatment but also for billing purposes.
The physical examination of the patient encounter will encompass both standard measurements of height and weight, and if possible, the percentage of body fat. The patient’s BMI should be calculated, and the waist circumference (WC) should be measured, since they are the major factors in stratifying health risk in patients with obesity or overweight. The World Health Organization has defined obesity starting at a BMI of 25 kg/m2 for a Caucasian population, or 23 kg/m2 for an Asian population. While not all patients with obesity or overweight, as defined by BMI criteria, have metabolic diseases or excess adipose tissue, and conversely not all that have metabolic dysfunction have obesity or overweight, the correlation between the two is strong enough that it is clinically appropriate for diagnosis. Distribution of adipose tissue and measures of body composition add another dimension to the assessment of individual patients. Measuring WC is a strong tool for gauging the volume of intra-abdominal or visceral adipose tissue. Those with a WC above 40 inches are at a higher risk of both metabolic diseases, as well as cardiac disease. Figure 8.1 describes the proper way to measure WC, and Table 8.2 shows the accepted variations in WC by ethnic group.
A proper technique for measuring waist circumference. Locate the superior iliac crests and the lower rib margins and place the measuring tape around the abdomen above iliac crests, keeping the loop of the tape parallel to the floor. Ensure the measuring tape is snug but not compressing the skin. (Adapted from: Allison DB, Downey M, Atkinson RL, Billington CJ, Bray GA, Eckel RH, et al. Obesity as a disease: a white paper on evidence and arguments commissioned by the Council of the Obesity Society. Obesity (Silver Spring). 2008;16(6):1161–77. Epub 2008/05/10; used with permission)
A focused cardiovascular examination includes systolic and diastolic blood pressure readings (SBP/DBP), an electrocardiogram (ECG), as well as screening for dyspnea. Depending on clinical judgment, a full cardiovascular evaluation should be undertaken before a recommendation of increased activity is given to a patient. Since some pharmacological agents used to treat obesity and overweight have been associated with valvular heart disease in the past (fenfluramine and dexfenfluramine), a physical examination focused on heart sounds is essential before prescription of any weight loss medication.
The physical examination will reveal other complications of obesity or overweight, including musculoskeletal changes, edema, lymphedema, venous stasis, and skin changes (acanthosis nigricans, hirsutism, skin tags, and striae) and disorders of regional fat distribution.
Further assessment of body composition can also be useful in diagnosing obesity and overweight. Though many third-party payers do not cover the measurements, they are useful in diagnosis and may provide an additional source of income to the practice if found to be sustainable. Methods such as bioelectrical impedance analysis (BIA), dual-energy X-ray absorptiometry (DEXA), and magnetic resonance imaging (MRI) can all be used to document body composition. Each method has different advantages and limitations that define its effectiveness as a diagnostic tool, and its financial feasibility.
The fat mass index (FMI) is a more precise way of evaluating fat mass. This requires that fat mass be measured, as can be done with DEXA. The patient’s FMI is defined as the fat mass in kilograms divided by the height in meters squared.
Laboratory testing should be conducted to stratify health risk. Laboratories are needed to document if there are causes of weight gain or an inability to lose weight, such as insulin resistance, thyroid disorders, and Cushing’s syndrome. For primary and secondary laboratory tests, see Table 8.3. Laboratory tests should all be ordered using diagnostic codes other than for obesity or overweight to avoid lack of coverage. Appropriate diagnoses for each test are included in Table 8.3.
Testing of the patient’s leptin-to-adiponectin ratio defines adipose tissue health. Leptin levels increase with increasing fat mass. Adiponectin levels drop with adipose tissue dysfunction. Trending the ratio documents the state of adipose tissue health for an individual over time. A ratio of leptin to adiponectin that increases over time signals progressive adipose tissue dysfunction (adiposopathy) and is a strong predictor of worsening metabolism. On the other hand a ratio of leptin to adiponectin that decreases over time signals improvement in adipose tissue function. Commercial assays for these two adipose tissue hormones are available from national reference laboratories.
8.5 Defining Success
The primary goal of treatment for patients with obesity or overweight is not weight loss on a scale. Rather, clinical endocrinology focuses on returning derangements of metabolism to normal, and this must now include adipose tissue dysfunction. Effective behavior modification is required for success in the long-term management of patients. The desired result is for the patient to achieve a negative energy balance.
Achieving a lean body weight is often an unrealistic goal in the management of overweight and obesity. A reduction of weight of 5–10% will reduce health risk drastically. This 5–10% reduction in body weight should be a desired goal for the ensuing 6–12 months of treatment. At any point in time, this goal of treatment should be reapplied to encourage ongoing weight loss. Most patients will not return to a lean BMI; hence, after any weight loss, the priority will be in the maintenance of the achieved lower weight. It is important to continue to set long-term realistic goals and to encourage decreased caloric intake and a higher amount of physical activity. This emphasis should replace the traditional adage of “diet and exercise” which suggests short-term measures and more immediate results.
Lifestyle changes will be easier to implement, and when stressed repeatedly, more likely to be integrated into the patient’s daily habits if they are realistic, achievable, sustainable, and incremental over time. For example, it is best to recommend small amounts of physical activity repeatedly over the day, as opposed to one instance of prolonged physical activity. The use of stairs instead of an escalator or elevator, and parking further from entrances, each increases physical activity without the stigma of “exercise.” Similarly, a decrease in caloric intake can be implemented as a decrease in calorie-dense foods and not necessarily the volume or frequency of meals. There are several clinical strategies that can be implemented to restrict caloric intake by making the patient more aware of serving sizes and eating habits. Small changes such as reducing the size of the physical plate, avoiding buffets or self-service tables, and prereducing restaurant portions in to-go containers can greatly reduce intake without drastically changing the patient’s lifestyle.
Since these modifications won’t result in immediate or drastic results, it is important that patients understand the concept of obesity as a chronic illness. Overweight, obesity, and adiposopathy do not have short-term solutions. Their treatment should be framed in this context so that patients do not become disillusioned and adhere to their treatment plan in the long term. Once the desired weight loss has been achieved, a program of weight maintenance will need to be implemented. Success in both achieving weight loss and maintaining lower weight should be individualized to the patient. Since the rate of recidivism is high in the treatment for obesity and overweight, it is important to incorporate certain components of behavior therapy, such as relapse prevention, which will prepare the patient to expect setbacks and view them as temporary. It is also important to highlight the patient’s success and not to chastise mistakes. This approach can be effective in treating even severe obesity and can produce significant results over long periods of time.
8.6 Financial Management of a Bariatric Endocrinology Clinic
As obesity and overweight rates have risen in the United States, coverage for bariatric care has often been deemed too expensive for employers to offer to their employees and has been excluded for coverage in order to reduce health-care premiums. Until recently, this approach has also been reflected in most federal and state-funded coverage plans including Medicare. As a result, office visits, medical nutrition therapy, and pharmacotherapy for overweight and obesity have been excluded from coverage by most health plans.
In 2013, obesity and overweight were recognized by the American Medical Association as a disease continuum. Shifting of health-care resources from treatment to prevention, chiefly through the implementation of provisions of the Affordable Care Act (ACA), has set a precedent for the work of dedicated bariatric clinics to soon be covered through the International Classification of Diseases (ICD) codes for obesity and overweight. Until then, it is imperative that a clinic bill for medical care of the many complications of obesity. As of the publication of this textbook, third-party payer coverage of the billing codes for obesity or overweight is inconsistent, but there is consistent coverage for major complications. Billing codes for obesity and overweight should still be used in regard to billing.
It is important for a clinic to know what the local market will bear. The team-based approach is the most beneficial for treatment; however, many third-party payers may not cover the costs of specialists. Laboratory testing as well as other screenings can be costly and, due to gaps in coverage, may ultimately be the patient’s financial responsibility; therefore, being able to gauge the makeup of the practice patient base is vital to success. A successful patient encounter is one that will foremost be beneficial to the patient and also be financially successful for the practice. Ideally, medical care for overweight, obesity, and adiposopathy would not be subsidized by the clinic. Thus, it is important that each encounter meets the overhead of the practice.
8.7 Conclusion
Overweight, obesity, and adiposopathy are chronic illnesses for which there is no cure. The goal of treatment will always be maintenance of a healthy lifestyle and the return of adipose tissue to proper function. Meeting these goals will result in a loss of excess fat mass. The models of care used for other chronic endocrine diseases should be applied to the treatment of overweight, obesity, and adiposopathy. The proper clinic and staff play a pivotal role in helping patients achieve long-term success. Bariatric endocrinology practices will be crucial in changing the prevailing attitudes of health-care professionals about patients with obesity.
Reading List
Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009;120(16):1640–5. Epub 2009/10/07.
Collingnon A. Strategies for accommodation obese patients in a acute care setting. AAH J [Internet]. 2008 [Cited 2015 June 1]. Available from http://www.aia.org/practicing/groups/kc/AIAS076325.
de Koning L, Merchant AT, Pogue J, Anand SS. Waist circumference and waist-to-hip ratio as predictors of cardiovascular events: meta-regression analysis of prospective studies. Eur Heart J. 2007;28:850–6.
Gudzune KA, Doshi RS, Mehta AK, Chaudhry ZW, Jacobs DK, Vakil RM, et al. Efficacy of commercial weight-loss programs: an updated systematic review. Ann Intern Med. 2015;162:501–12. https://doi.org/10.7326/M14–2238.
Latner JD, Stunkard AJ. Getting worse: the stigmatization of obese children. Obes Res. 2003;11:452–6.
Neumark-Sztainer D, Story M, Faibisch L. Perceived stigmatization among overweight African-American and Caucasian adolescent girls. J Adolesc Health. 1998;23:264–70.
Neumark-Sztainer D, Story M, Harris T. Beliefs and attitudes about obesity among teachers and school health care providers working with adolescents. J Nutr Educ. 1999;31:3–9.
Puhl R, Brownell KD. Bias, discrimination, and obesity. Obes Res. 2001;9:788–805.
Puhl R, Brownell KD. Psychosocial origins of obesity stigma: toward changing a powerful and pervasive bias. Obes Rev. 2003;4:213–27.
Roehling MV. Weight-based discrimination in employment: psychological and legal aspects. Pers Psychol. 1999;52:969–1017.
Schwartz MB, O’Neal H, Brownell KD, Blair S, Billington C. Weight bias among health professionals specializing in obesity. Obes Res. 2003;11:1033–9.
Shaw K, O’Rourke P, Del Mar C, Kenardy J. Psychological interventions for overweight or obesity. Cochrane Database of Syst Rev. 2005;(2): CD003818.
Use of Workers’ Compensation Data for Occupational Safetey and Health. Proceedings from June 2012 workshop. DHHS (NIOSH) publication no. 2013–147. Cincinnati.
Vazquez G, Duval S, Jacobs DR Jr, Silventoinen K. Comparison of body mass index, waist circumference, and waist/hip ratio in predicting incident diabetes: a meta-analysis. Epidemiol Rev. 2007;29:115–28.
Vega GL, Grundy SM. Metabolic risk susceptibility in men is partially related to adiponectin/leptin ratio. J Obes. 2013;2013:409679. https://doi.org/10.1155/2013/409679.
Wignall D. Design as a critical tool in bariatric patient care. J Diabetes Sci Technol. 2008;2(2):263–7.
Williams DS. Bariatr Nurs Surg Patient Care. 2008;3(1):39–40. https://doi.org/10.1089/bar.2008.9993.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Hartman, I. (2019). Evaluation and Management of the Patient with Obesity or Overweight. In: Gonzalez-Campoy, J., Hurley, D., Garvey, W. (eds) Bariatric Endocrinology. Springer, Cham. https://doi.org/10.1007/978-3-319-95655-8_8
Download citation
DOI: https://doi.org/10.1007/978-3-319-95655-8_8
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-95653-4
Online ISBN: 978-3-319-95655-8
eBook Packages: MedicineMedicine (R0)