Abstract
Acute and procedural pain remain difficult for providers to treat. Like other complementary and alternative therapies, immersive virtual reality (VR) therapy has shown promising results. Although VR therapy for acute pain has been investigated since the 2000s, it is still in its infancy. Only recently have falling prices and increased accessibility made this technology available outside of academic institutions. This chapter explores the development, evidence, necessary requirements, and future directions of VR therapy, while addressing challenges faced when attempting to use VR therapy for acute and procedural pain.
A place, in this non-geographical sense, is a created thing, an ethnic domain made visible, tangible, sensible. As such it is, of course, an illusion. Like any other plastic symbol, it is primarily an illusion of self-contained, self-sufficient, perceptual space. But the principle of organization is its own: for it is organized as a functional realm made visible —the center of a virtual world. – Susanne K. Langer (1953)
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
The Problem with Pain
Over the past decades, we have witnessed the difficulties in treating pain responsibly. Spurred by a greater appreciation for its presence (Melzack 1990), we have seen great investment and effort in treating pain. Research in the field has contributed greater understanding of the underlying mechanisms of pain, the role of undertreated acute pain in the development of chronic pain, continued efforts toward more refined assessment tools (Bromley Milton et al. 2013), and ongoing attempts to improve pain-related outcomes. As such, accrediting bodies, payors, and professional associations have emphasized pain-related outcomes as significant (Gan et al. 2014). Today in the United States, it is estimated that the annual healthcare costs related to pain range from $560 to $635 billion dollars (Gaskin and Richard 2012). However, despite this enormous economic cost and use of resources, adequately treating pain remains difficult for the provider, especially in acute settings where pain is arguably experienced at its greatest intensity.
In the United States, approximately 100 million surgical procedures are performed annually (Cullen et al. 2009). With a greater awareness of the pain associated with procedures, we have relied heavily on opiate medications (Gan 2017). Even with the use of these powerful medications, attempts at relieving suffering from pain still often fall short (Apfelbaum et al. 2003; Gan 2017; Melzack 1990). In regard to the intensity of pain experienced, up to 75% of postsurgical patients report moderate/extreme acute pain even with associated treatment (Gan et al. 2014). Although there are many possible reasons for dissatisfaction with pain treatment, sufficient opiate doses are often limited by their side effects: sedation, life-threatening respiratory depression, nausea, vomiting, constipation, hallucinations, itching, tolerance requiring increasing doses, hyperalgesia making the pain experience worse, endocrine disruption with chronic use, and social stigmatization (Koppert and Schmelz 2007; McDaid et al. 2010; Oderda et al. 2003; Cheatle and Gallagher, Chap. 25, this volume). Even opiate-sparing medications (e.g., acetaminophen, nonsteroidal anti-inflammatory drugs) can have their own undesirable side effects including hepatotoxicity, nephrotoxicity, gastrointestinal bleeding, and possible effects on surgical site healing (McDaid et al. 2010; Datta and Manchikanti, Chap. 24, this volume).
As providers today, we have a greater awareness of the societal implications of our obligations to treat an individual’s reported pain responsibly. After decades of extra bottles with powerful, addictive, and potentially lethal unused pills sitting in families’ medicine cabinets, we find the United States in the midst of what is being called an opiate epidemic (Okie 2010; Rudd et al. 2016; Cheatle and Gallagher, Chap. 25, this volume). In 2014 alone, 47,055 drug overdose deaths occurred in the United States (Rudd et al. 2016). Additionally, between 1999 and 2014, overdose deaths have tripled with more than 60% of these attributed to opiates (Rudd et al. 2016). The diversion of prescription drugs and the patients’ transition into illicit opiates like heroin continues to be a major societal concern (Compton and Volkow 2006). The current president has even declared this a national emergency (Oliphant 2017), although offering few solutions after rephrasing this later as a national public health emergency (Davis 2017).
New Directions
As a result, many providers are realizing opiate prescriptions are far from a simple solution and are searching for ways to treat pain beyond traditional medications. Many are incorporating complementary and alternative medicine (CAM) therapies into their practice (Davis et al., Chap. 33, this volume). According to National Institutes of Health surveys, over 38% of adults utilized at least one CAM therapy into their care, and this percentage continues to increase (Barnes et al. 2008). In general, CAM therapies are low risk and carry the additional benefit of allowing for greater involvement and control in decision-making by patients and their families (Deng et al. 2004). The current National Comprehensive Cancer Network (NCCN) guidelines even recommend CAM therapies (when available) in their treatment guidelines (Swarm et al. 2013).
One complementary and alternative therapy that has been studied since the early 2000s in a wide variety of clinical settings is immersive virtual reality (VR). Although commonly thought of as a video game used solely for entertainment purposes, VR has demonstrated clinical therapeutic benefit with psychological disorders (Carlin et al. 1997; Garcia-Palacios et al. 2002; Mishkind et al. 2017), motor rehabilitation (Levin 2011; Neri et al. 2017), physical therapy (Carrougher et al. 2009), chronic pain conditions (Jones et al. 2016; Keefe et al. 2012; Trost et al. 2015), and acute pain conditions (Hoffman 2004; Hoffman et al. 2011; Morris et al. 2009), even when such pain is severe (Schmitt et al. 2011).
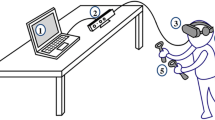
Until recently, the high cost of immersive VR systems precluded its widespread application and required proprietary software and specialized equipment. Early studies in clinical VR utilized large bulky systems (Fig. 29.1) that cost more than $90,000 (Hoffman et al. 2014). With the proliferation of high-definition screens used on mobile phones, the cost of producing high-quality VR headsets has fallen dramatically to less than a $1000. Today, readily available consumer VR systems not only have more impressive technical specifications, but they can be obtained at a fraction of the cost of the systems used in pioneering studies. The availability of mobile phone-based VR systems makes VR a potentially scalable non-pharmacologic complementary and alternative therapy. Although VR therapy shows exciting promise in a wide variety of clinical applications as mentioned above, this chapter will focus solely on its use for the treatment of acute pain.
What Is Virtual Reality?
The phrase “virtual reality” may sound like an oxymoron. However, to those who experience it firsthand, they quickly understand its meaning and significance. Much like the convincing nature of dreams argued by Rene Descartes (Descartes 1998), VR is an illusion that plays on the senses in a deliberate and convincing manner; however, instead of self-manifested dreams, the experience is facilitated within a computer simulation.
First coined by Jaron Lanier in the mid-1980s, “virtual reality” refers specifically to a user-computer interface that allows for real-time simulation of a computer-generated environment that users can interact with via multiple sensory channels in an intuitive manner (Lanier 2001). The immersive technology is designed to create an illusion of presence or an uncanny feeling of actually being “inside” a new computer-generated environment, as if it is a place being visited. Today with increasingly sophisticated camera technology, the phrase also refers to experiencing 360-degree videos from around the world in a similar fashion (Loomis 2016).
The idea for this technology was originally conceived in 1965 by Dr. Ivan Sutherland who is widely considered the father of computer graphics (Lanier 2001). Before the technological capability at the time, Sutherland proposed what he called the “Ultimate Display” (Sutherland 1965). With the proper programming, he imagined the device would allow the user to experience “the Wonderland in which Alice walked” (Sutherland 1965). Three years later he had created the first head-mounted display (HMD) capable of displaying his first “virtual world,” a phrase he borrowed from the aesthetic philosopher Susanne K. Langer (Langer 1953; Lanier 2001). This system was primitive and hardly the full realization of his vision for a device that would allow the user to feel fully immersed and interact with a computer-generated environment in a seamless and intuitive manner.
The Illusion of Presence
Sutherland envisioned a system advanced enough that users would feel so fully immersed in the computer environment that they would actually feel like they were present in this new virtual world. The feeling of presence in a virtual world is just that, a feeling. It is generally defined as a subjective state of consciousness and can only be measured by asking a user to rate their own subjective feeling of presence. This is generally asked by having the user indicate on a scale of 1–10 how much they felt like they were in the virtual environment, as if it was a place they visited. Since this is a subjective rating, it can vary over time within an individual and across individuals using the same VR experience (Bowman and McMahan 2007). At its core, presence is an illusion (Lombard and Ditton 2006; Slater and Wilbur 1997) that makes users feel their experience is not being mediated by computer technology, when in fact the entire experience is being mediated and constructed seamlessly in real-time within a computer.
The greater the feeling of presence in a VR system that is created among users, the more immersive the technology or experience is said to be. This means that hardware specifications can be looked at objectively to define one system as being more immersive than another system (Bowman and McMahan 2007). A wider field of view (FOV), increased refresh rates, and higher screen resolution are examples of hardware specifications that improve immersion and therefore should give a stronger subjective feeling of presence to a user. Likewise, involving more sensory input (visual, auditory, touch, smell, taste) into the interaction with the simulation should lead to a more immersive experience. However, the illusion of presence relies upon more than just brute computing power or hardware specifications and is an active area of research that is beyond the scope of this chapter (Bowman and McMahan 2007; Lombard and Ditton 2006; Loomis 2016; Malbos et al. 2012; Slater and Wilbur 1997).
Regardless of the specific VR system used, Gonzalez-Franco et al. proposed that the illusion of presence is only created when a VR system is able to influence one’s “bottom-up sensory processing, sensorimotor self-awareness frameworks, and top-down prediction manipulations” (Gonzalez-Franco and Lanier 2017). In the past, VR system hardware often fell short of the promise of creating an illusion of presence (Brooks 1999; Rosenblum 2000). However, today many current consumer model VR systems are readily available that create high-quality experiences and fulfill the vision Dr. Sutherland first imagined more than half a century ago at the dawn of computer graphics (Loomis 2016).
Immersive Virtual Reality and Pain Distraction
While ritual and magic were used commonly by ancient cultures, it is hard to say exactly when distraction began to be explored as a deliberate method of pain control. However, early texts and paintings can offer detailed accounts dating back to at least the thirteenth century (Stoelting and Miller 2007). Around the turn of the nineteenth century, Franz Anton Mesmer, a Vienna-trained physician, gained notoriety as well as skepticism for using atmosphere, the power of suggestion, and starring into his patients’ eyes to treat intractable pain, even their pain during surgeries (Hadfield 2015). Although Mesmerism is largely considered a pseudoscience with fantastical beliefs practiced by layman, the interplay of cognitive function and pain has remained an intense area of research (Fernandez and Turk 1989; Wiech et al. 2005).
Melzack and Wall first theorized in 1965 the Gate Control Theory of pain where they proposed several central nervous system activities, including attention, that moderate the perception of pain (Melzack and Wall 1965). To this extent, it has been demonstrated that pain requires attention (Eccleston and Crombez 1999) and that people have a limited attentional capacity (Kahneman 1973; McCaul and Malott 1984). The theory follows that if a person has limited attentional resources and if their attention is directed elsewhere, they will have fewer attention or cognitive resources available to process the incoming nociceptive signals and therefore will experience less pain. As a result, many studies have explored the effect of various forms of distraction on subjective ratings of pain intensity (Eccleston 2001; Fernandez and Turk 1989; Hodes et al. 1990; Vincent et al. 2010). Traditional forms of distraction (like music) have shown promise (Lee 2016), but ultimately a large meta-analysis questioned whether the magnitude of pain relief from music carried any clinical significance (Cepeda et al. 2006).
As a result, over the past two decades, research teams have investigated VR as a potentially more robust non-pharmacologic analgesic. The VR system is thought to offer potential therapeutic advantages in acute pain over other forms of distraction because of its ability to create multisensory distraction, while concurrently isolating a patient from their clinical setting and replacing it with a more attractive virtual environment. The HMD used in VR blocks a patient’s view of the immediate physical world by placing stereoscopic video screens in front of their eyes. Hospital noises are replaced by sound effects and music from the virtual environment using noise-canceling earphones. The immersive VR system also allows for varying degrees of interaction and as a system should convey the illusion of presence to the user that was described earlier. The idea is for the system to seemingly transport a patient away from their current hospitalized setting, taking their attention away from their painful procedures or conditions and focusing it into a pleasant computer-generated environment.
Interacting with VR then should use vast amounts of a person’s limited attentional resources. Indeed, in one initial experiment, Hoffman et al. found VR reduced performance on divided attention tasks (Hoffman et al. 2003a). Additionally, Hoffman et al. developed a novel VR system capable of functioning within the powerful magnet of a functional magnetic resonance imaging (MRI) device (Fig. 29.2) to investigate the underlying neural correlates of VR pain distraction (Hoffman et al. 2003b, c). In addition to reductions in reported subjective perceptions of pain during VR use, the fMRI during VR showed objective reductions in activity within brain areas related to pain perception and increased activity in cortical areas related to attentional processing (Fig. 29.3) (Hoffman et al. 2004a). These results are very similar to those previously seen in fMRI studies investigating other more traditional cognitive distractions (Bantick et al. 2002; Torta et al. 2017; Valet et al. 2004). Furthermore, functional MRI studies of experimental pain in human volunteers have shown that both systemic opiate therapy and VR distraction produce subjective and objective evidence of pain reduction when used in isolation, as well as additive analgesia when used in combination (Hoffman et al. 2007). These findings also suggest that systemic opiates and VR distraction may modify the pain experience through different neurophysiological mechanisms. Although these studies offer evidence that VR is a potentially powerful form of distraction, they also show us that VR is actually reducing the amount of pain-related brain activity.
An Evolving Understanding of VR Effects
Although distraction is an important aspect to the theory of how VR can allow users to better tolerate acute pain, this theory may prove to only be part of a larger mechanism. For instance, VR has shown success in treating chronic pain conditions (Jones et al. 2016; Keefe et al. 2012; Trost et al. 2015), something that a distraction mechanism does not fully explain. Additionally, people who use VR can report lingering effects after removing the HMD that range from euphoria to disillusionment and even report dissociation from actual objective reality (Aardema et al. 2010). These studies vary in their methodology, but their results raise questions of possible neurophysiologic changes which may account for the reductions in pain seen in acute pain applications (Gupta et al. 2017).
Additionally, our understanding of functional brain imaging is expanding as technologies to image the brain in real-time improve in both accuracy and precision. The field is changing quickly, and in the past decade, as the imaging modalities improve and are able to picture the entire white matter tracts between distant regions in great detail, we have begun to see a change from reductionist, structure-based correlations of pain to paradigm of greater network communications between brain areas of interest. Regardless, multiple imaging studies investigating attention and pain, including those using VR, find a consistent involvement of key brain areas related to the theorized “pain matrices,” executive attention centers, and emotion and affect centers (Torta et al. 2017). In other words, while distraction might play a large role in the mechanism of acute pain attenuation by VR, the representative brain areas of interest in pain distraction studies are also known to be involved in affect and emotion (Torta et al. 2017).
Perhaps the clearest evidence for the influence of VR on affect, emotion, and pain come from a recent study by Sharar et al. (2016). Previous studies have found that in addition to reduced reports of subjective pain with the use of VR, subjects also report increased levels of “fun” even during these painful events (Hoffman et al. 2011; Sharar et al. 2007). To investigate whether positive affect influences the effects seen in VR therapy, Sharar et al. exposed 74 volunteers to painful stimuli with and without the use of VR and also stratified their results on the circumplex model of affect spectrum, a validated and reliable measure of affect (Russell 1980). The authors found that during VR not only did all subjects report decreased pain, but those with positive affect were more likely to report reduced pain, experience greater pain reductions, report less anxiety, and report higher levels of “fun” during the experiment (Sharar et al. 2016). Thus, distraction may be an important aspect of VR therapy; it is likely mediated through multiple mechanisms, including effects on personal affect and emotion.
VR pain therapy is in its infancy and demands greater research to elucidate its underlying mechanisms more completely in order to create more effective VR pain therapy experiences. Until then its use as a powerful distraction tool remains an important framework when considering VR pain therapy experiences, software, and design. However, the ability to influence a positive affect and create emotional engagement in addition to physical and cognitive engagement will be an important consideration in the development of future VR therapy experiences and needs further investigation.
Immersiveness and Pain Relief
The more immersive a VR experience and system is, the greater the effects seen in pain attenuation. Research using experimental pain in human volunteers has shown greater analgesic effects achieved with increasing degrees of VR immersion when compared to less immersive VR systems (Hoffman et al. 2006, 2004b; Wender et al. 2009), traditional video games (Hoffman et al. 2000), and music alone (Johnson and Coxon 2016). The immersive nature and the corresponding illusion of presence is unique to VR among pain distraction methods, and the more immersive the system, the greater the reductions in reported pain. Although immersive experiences are possibly more distracting, these mechanisms are not fully understood.
Reductions in a patient’s pain and anxiety ratings during VR compared to Nintendo 64. VAS, visual analog scale; VR, virtual reality (Hoffman et al. 2000)
While there are many possible objective measures of what makes a system immersive (see above), it is generally thought that the more physical senses a system involves, the more immersive it is. Most VR therapy investigations have only used vision and sound to isolate their patients. Integrating more physical senses into a therapeutic experience remains to be investigated in VR pain therapy. Involving proprioception, touch, taste, and smell may carry additional reductions in reported pain. Theoretically, a more immersive experience in this manner should involve a greater cognitive load with less available attention for pain as described above. Additionally, involving non-noxious large-diameter (A-beta) neurons (using wind, water, temperature, etc.) into a VR experience may not only improve the immersive nature of the experience, but it could potentially carry benefits through the gate control theory where nociceptive signals are modulated (Melzack and Wall 1965), similar to how transcutaneous electrical nerve stimulation is thought to achieve benefit (Johnson 2007). This is an active area of investigation and deserves further study about how to actually create these immersive environments.
At its core, VR remains a technology that is used to mirror conscious perception by combining academic disciplines of all kinds with cutting edge technology to simulate reality (Lanier 2017). The experience of this simulated reality can be a revelation to those that experience it firsthand (Aardema et al. 2010; Lanier 2017). When everything familiar to you suddenly changes by entering an immersive VR environment, your singular experience cannot help but be acknowledged in that moment (Lanier 2017); It is in this way VR may serve as a form of psychotherapy, making a user aware of their own singular experience in ways never before possible. We may draw comparisons to mindfulness techniques, or “mindfulness meditation.” These techniques ask participants to turn their attention further within themselves, concentrating and acknowledging their fleeting random thoughts and moment-to-moment experiences in a deliberate fashion and reducing the cacophony of noise down to a violin. As a form of psychotherapy, mindfulness technique has shown promise in treating chronic pain conditions (Bawa et al. 2015; la Cour and Petersen 2015), yet its own mechanism is not fully understood (Zeidan et al. 2015). While not everyone finds a revelation in VR, the therapy might offer a psychotherapeutic advantage similar to mindfulness technique. To some patients, VR may offer a new change in the way they navigate their experience of pain, how they interpret it, and how they acknowledge it.
Clinical Evidence
Despite the widespread commercial and media focus in recent years on consumer-grade VR hardware and software – largely directed at gaming applications and supported by major commercial players in the computer and social media technology sectors (e.g., Microsoft, Google, Facebook/Oculus, Samsung) – the first clinical report demonstrating VR distraction analgesia was published almost two decades ago (Hoffman et al. 2000). Hoffman et al. (2000) compared the subjective analgesic benefit of immersive VR distraction to that of an interactive commercial video game (Nintendo 64) in two hospitalized teenage males undergoing painful wound care (wound debridement, skin staple removal, dressing change) following major cutaneous burn injuries. Both patients reported very significant reductions in their subjective pain experience and anxiety with VR distraction during their procedures (Fig. 29.4), and no side effects associated with the relatively crude VR systems of that era (e.g., simulator sickness). The authors concluded that the combination of the immersive VR experience that draws patients’ attention away from a concurrent painful stimulus (nociception), together with the physical exclusion from the sights and sounds of the immediate care environment afforded by the HMD, resulted in an effective non-pharmacologic pain therapy that was ideally suited to clinical settings of brief, procedural pain.
Since this first description, immersive VR distraction has been extensively studied in various acute procedural pain settings in pediatric and adult populations, including burn wound debridement, postburn rehabilitation, postoperative physical therapy, transurethral prostate surgery, dental care, vascular access, oncology care, emergency department procedures, and care for multiple traumatic injuries. The potential widespread analgesic benefit of using immersive VR across this spectrum of acute and procedural pain settings has been succinctly and recently reviewed elsewhere (Pourmand et al. 2017; Sulea et al. 2014). These reports consistently demonstrate the beneficial effects of VR distraction on various subjective assessments of the pain experience. Clinically meaningful pain relief (defined as ≥30% reduction in subjective pain reports (Farrar et al. 2000)) has been reported in each of the controlled trials, and side effects are both infrequent and mild. Furthermore, these reports demonstrate a consistent, beneficial analgesic effect of immersive VR over multiple days of use (Faber et al. 2013; Hoffman et al. 2001b; Schmitt et al. 2011), suggesting that the initial novelty associated with the technique is not a limiting factor in its clinical application.
Among these various clinical settings, pain management related to cutaneous burn care (e.g., burn wound care, postburn physical therapy) is the most extensively studied and carefully reviewed (Morris et al. 2009; Sharar et al. 2008). From this clinical setting, several highlights emerge that are relevant to its more widespread clinical applications. First, in settings of mild-to-moderate pain (e.g., passive range-of-motion physical therapy to stretch and loosen skin contractures), immersive VR may occasionally be sufficient as a stand-alone analgesic therapy. As such, this technique has the potential to eliminate the use and reliance upon some forms of pharmacologic therapy that are associated with adverse side effects or long-term complications (Datta and Manchikanti, Chap. 24, this volume). Specifically, VR distraction (like other non-pharmacologic pain therapies) in these settings may obviate the need for opioid analgesics, thereby reducing side effects of nausea, vomiting, itching, and dysphoria, as well as potential long-term complications of opioid dependence. This latter benefit is of particular emphasis in the current environment of rampant abuse of both recreational and prescription opioids.
Second, in settings of moderate-to-severe pain (e.g., burn wound debridement), VR analgesic techniques are best used as adjuncts to potent pharmacologic analgesic techniques (e.g., opioids, anxiolytics) because the “potency” of VR distraction is insufficient as a sole therapy. This multimodal approach is increasingly common in many clinical pain settings and also capitalizes on the potential complementary analgesic mechanisms of opioids and VR distraction, as noted above from functional brain imaging studies (Hoffman et al. 2007).
Third, clinical trials have consistently shown that procedural pain relief during VR distraction is associated with increased subjective ratings of “fun” – a surrogate outcome related to positive affect or emotional valence (Fig. 29.5), similar to the laboratory pain study reported above (Sharar et al. 2016). This is important because creating a more enjoyable experience in the clinical care setting can increase patient satisfaction with care, particularly during painful procedures that patients must undergo repetitively, and where reluctance to participate fully in such repeated therapeutic procedures may also negatively impact clinical care outcomes. For example, daily physical or rehabilitation therapy can improve long-term functional outcomes; however, low participation in such therapy due to fear of pain, lack of enjoyment, or inability to rationalize short-term discomfort for long-term benefit may reduce the likelihood of a successful long-term outcome. Thus, these reports that immersive VR distraction enhances patients’ willingness and motivation to participate in such painful therapies (Fig. 29.6) suggest a long-term clinical benefit of the therapy.
Mean pain and mood (fun) ratings during postburn, passive range-of-motion physical therapy in a population of 88 subjects receiving standard pharmacologic analgesia (dark bars) and standard pharmacologic analgesia plus immersive VR (light bars). GRS, graphic rating scale (Sharar et al. 2008)
Finally, recent technological developments in VR hardware and software have resulted in low-cost, lightweight VR delivery systems that can be powered by laptop and handheld devices (Hoffman et al. 2014). These developments suggest that VR analgesia therapy is poised to extend beyond the hospital or clinic environments to outpatient, non-healthcare settings (i.e., home care) or healthcare applications in low-resource environments or countries (Morris et al. 2010; Wiederhold et al. 2014).
Current Limitations
Despite consistent and encouraging results of VR use for pain in both adults and children across a wide variety of clinical settings, it is important to mention the current limitations. First, many studies are of small sample size, and the largest sizes range approximately from 75 to 100 participants (Mahrer and Gold 2009). Additionally, the range of methodologies, virtual environments, pain measures, exposure times, patient populations, and hardware specifications found in the current literature make results difficult to generalize.
Studying subjective pain has been and remains a difficult endeavor, especially in a clinical setting where a large number of variables can exist (Ohnhaus and Adler 1975; Younger et al. 2009). VR pain research is no different and has its own set of challenges. Similar to other CAM therapies, it can be difficult to design placebo-controlled trials, as blinding patients and researchers to VR exposure is extremely difficult. As such, when participants report subjective pain ratings during research studies, it is possible they are underreporting their pain, since generally most studies are not blinded. Additionally, research participants inherently self-select for VR studies through required consent processes which may lead to selection bias. However, despite these limitations, VR studies have consistently shown encouraging results from around the world in a variety of clinical settings over many years (Morris et al. 2009; Pourmand et al. 2017; Sharar et al. 2008; Sulea et al. 2014) and deserve further investigation, particularly as devices improve and lower prices expand access.
Logistical limitations also exist. Commercially available headsets can be hard to clean between uses and must adhere to hospital-specific disinfection guidelines that may require modification with water-proof face pads or disposable face barriers instead of the stock fabric face pads. Additionally, lower-cost headsets may include plastic lenses which will be damaged by alcohol-based cleaners. Headsets have improved in comfort but with extended use can become uncomfortable. Finally, in a sympathetically charged patient experiencing acute pain that causes them to sweat, a headset can quickly become uncomfortable and lead to lens fogging that could negate any beneficial VR experience.
Suggested Minimum Hardware Components
To achieve an immersive experience, VR technology generally relies upon a basic core set of components: stereoscopic visual lenses, audio provided through headphones, and some form of interactivity. Today interactivity is provided through simple hand controls and various motion tracking capabilities. Stereoscopic lenses provide 3-D images that are vital for creating an illusion of presence. Headphones, particularly noise-canceling models, help isolate a user away from their hospital environment.
Many devices available to consumers today offer all these components in a range of prices and computing power. Higher-end models rely on desktop computers with powerful graphic processors, while others are wireless and are powered by mobile telephones. New wireless stand-alone devices that do not require mobile phones are also becoming available. Consumer VR is currently in its infancy, yet changing quickly. High-definition screens and lenses are being developed specifically for VR hardware applications, and the associated components are also developing quickly. As a result, currently available hardware will likely be outdated very soon. However, based on previous clinical studies, we can make some minimum hardware suggestions (Table 29.1).
Clinical VR applications started two decades ago using components less capable than those listed in Table 29.1 and often at a much greater cost than what can be obtained by consumers today. However, those pioneering studies were still able to generate encouraging results despite hardware limitations. Today mobile phone-based systems have specifications exceeding the devices used in previous studies and are ideal for clinical applications because they are readily available, easy to use, easy to transport, and capable of being taken on and off quickly. More powerful computer-based devices can appear intimidating to unfamiliar patients, require multiple wires, require an extensive setup, and can be more prone to freezing if a user flips them on and off their head frequently. Despite these obstacles, higher-powered devices may be preferred since they can provide more immersive experiences, which should provide better reductions in reported pain (see above).
Contraindications and Relative Contraindications
Despite an appealing low side effect profile when compared to pharmacologic analgesics (see above), certain patients are usually excluded from therapeutic VR studies for various concerns that can be considered contraindications to VR therapy.
-
History of Seizures – A sensitivity to photoinduced or photosensitive seizures should be considered a contraindication to VR use. Aside from strobe-like flashing, certain 3-D graphic renderings and high contrast details can elicit seizures in those sensitive. So, while most VR sets today use high-frequency displays that produce virtually zero flicker or strobe-like effect, it is advisable to withhold VR from anyone that has experienced a photoinduced seizure.
-
Psychiatric and organic brain disorders – Since VR can produce realistic simulations, concerns arise about the creation of “false memories” and potential deliriogenic triggers in VR. As such, current research excludes patients that are prone to delirium or otherwise unable to cooperate with normal VR use.
-
Facial trauma – Unfortunately the inherent design of HMDs for VR may preclude their use in those patients with head trauma.
-
Contact precautions – VR use in clinical settings must abide by hospital or facility cleaning standards, and the device should not be used in patients with resistant infections. Current face pads on consumer models can be replaced with waterproof versions that are capable of being cleaned with germicidal solutions. However, one must be aware that some lower-end devices use plastic lenses that will fog with alcohol-based cleaning solutions.
-
Claustrophobia - Isolating effects of the HMD can cause anxiety in some patients and should be avoided.
-
Visual deficits – VR relies heavily on visual ques for its illusion of presence or immersive effects. As such those with poor vision and/or hearing may not receive benefit from VR therapy.
-
Susceptibility to motion sickness – VR is known to cause nausea in those susceptible to it (see below). As such its use should be avoided in those with a known history of motion sickness or who are currently experiencing nausea.
Simulator Sickness
The most bothersome potential problem encountered from the use of VR in a therapeutic setting is the potential for nausea. Minimizing nausea for therapeutic VR cannot be stressed enough since no matter how appealing it may be, no one will want to use a device that makes them sick. In the early 1990s, SEGA (once one of the largest video game companies) underestimated the catastrophic potential nausea could have on its pioneering and ambitious consumer VR system (Hecht 2016). The SEGA VR system was abandoned after considerable investment and fanfare when it was found to cause substantial nausea shortly before its release (Hecht 2016). However, as computers have become more powerful with time, simulator sickness is much less of a problem than it once was.
Simulator sickness is a term describing a feeling of nausea induced by using VR (Kennedy et al. 1993). It is similar to motion sickness encountered from the movement of a boat or in a car. Simulator sickness, however, is a byproduct of visual simulators and not necessarily from movement per se. It is generally a less intense discomfort and thought to result from a conflict between the vestibular, proprioceptive, and visual systems (Kennedy et al. 1993).
In the past, simulator sickness was largely the result of hardware systems that did not have enough computing and graphic processing power to keep up with the demands required from VR. Not only did this create a large chasm between VR expectations and available product, but also such underpowered devices resulted in latency. Latency is a delay in the movement of graphics on screen in response to the patient’s movement. Additionally, these older computers were only capable of low screen refresh rates, which when viewed on screens only inches from the eyes also resulted in nausea. Today with increasing refresh rates and powerful computer processors (even those within mobile phone-based systems), simulator sickness can largely be avoided if proper precautions are taken.
To pick a comfortable experience for a patient, it is important to take into account the actual design of the virtual environment and an individual’s susceptibility. Some consumer VR systems also work closely with developers to provide appropriate “comfort ratings.” We suggest using those experiences with high comfort ratings when these ratings are available. Table 29.2 summarizes some common causes of simulator sickness for reference that have been suggested to VR developers (“Oculus Rift Best Practices,” 2015). While developers cannot control individual predisposing factors, it is important to avoid using VR in those patients susceptible to motion sickness or who are already nauseous. Additionally, if a patient has a large disparity in vision between their eyes, this will not only minimize the 3-D effect of VR, but potentially can cause simulator sickness and eye strain. If patients with binocular disparity normally wear corrective lenses, they should also use them for the VR experience if possible.
After careful patient selection, nausea can be reduced through thoughtful environmental design. The study of simulator sickness, its causes, and potential solutions is beyond this chapter (Davis et al. 2014; Rebenitsch 2015). Briefly, however, nausea can be largely prevented by avoiding virtual environments or experiences with fast accelerations, intense visual flows, and fast-moving peripheral scenery and avoiding removing control of the “camera” or point of view away from the user (Davis et al. 2014). Additionally, it is suggested that users take frequent breaks from VR experiences as it is well established that the longer one stays in VR, the more likely one is to report nausea (Kennedy et al. 2000). However, the proper frequency and duration of these breaks has not been established and are largely based on individual patient factors. Interestingly, susceptibility to simulator sickness decreases with increasing VR use and exposure, so developers or those with more experience using VR are typically poor at assessing the potential for nausea (Welch 2002). As users gain more exposure to VR, they are able to experience more intense virtual experiences, but for patients in therapeutic settings, it is important to reduce the incidence of nausea as much as possible through careful patient selection and environmental design selection.
Designing Virtual Worlds
Perhaps the most exciting aspect of VR analgesic therapy is the design, creation, or selection of an immersive virtual environment to help a patient cope with their pain. Exactly what that environment should be has yet to be defined, but based on the research cited within this chapter, we can draw conclusions for the basic requirements of a VR therapeutic environment (Table 29.3). In short, the environment needs to be immersive and allow for interaction. Although this might seem obvious, some studies in the literature claim to use immersive VR, but under further scrutiny, they utilize passive video glasses that merely display movies without VR immersion.
The first immersive experience used for acute pain therapy was designed by Hoffman et al. (2000). The experience, SpiderWorld, was based on a VR program originally intended to treat arachnophobia through exposure therapy and reprogramed to give the user the ability to explore a virtual kitchen from a spider’s perspective (Hoffman et al. 2000). Based on these results, the first immersive VR software designed specifically for pain control was created at the University of Washington in Seattle (Hoffman et al. 2001a). SnowWorld (Fig. 29.7) featured an icy canyon a patient would effectively float through “on rails,” constantly being pushed along in a forward motion. The canyon was filled with snow-covered peaks, trees, and snowmen. Users could direct their view and throw snowballs with a computer mouse or spacebar. Headphones played music and included sound effects as thrown snowballs exploded on their intended targets. This archetypal program went on to be used in many clinical studies investigating VR effects on acute pain (Morris et al. 2009; Pourmand et al. 2017; Sharar et al. 2008; Sulea et al. 2014). Today, VR programs commercially available for acute pain therapy are similar to this original design: an “on rails” experience allowing the patient to fire projectiles at targets (Marchant 2017; Molteni 2017).
These VR experiences fulfill the basic requirements of an interactive and immersive VR experience delineated in Table 29.3. However, as mentioned above, the optimal VR experience for acute pain has yet to be defined. Furthermore, distinct types of pain and clinical scenarios may benefit from distinct types of experiences. For instance, an exploratory study investigating the use of VR for labor pain relief in unmedicated pregnant women used a soothing underwater scuba diving simulator where patients interacted by taking underwater photographs of curious manatees (Frey 2018). Future experiences may be tailored even further to address specific goals of therapy such as increasing range of motion in those with burns or arthritis by encouraging such movements in the VR setting, allowing patients to use the VR device while laying supine on an operating table, or encouraging deep breaths with an associated incentive spirometer in a patient with painful rib fractures. Novel approaches to VR pain are also investigating the incorporation of hypnosis (Askay et al. 2009), meditation, and biofeedback (Li et al. 2011). Ultimately, the optimal VR experience for VR pain relief has yet to be defined and requires further investigation.
Ivan Sutherland, a mathematician at heart, envisioned walking among equations and mathematically underpinned abstractions (Sutherland 1965). The VR pioneer Jaron Lanier envisioned users walking among each other’s dreams that we create and share in real-time with social connections (Lanier 2017). This remains an appealing vision as some patients do not like the idea of being isolated from close friends and family during VR pain therapy. Hunter Hoffman, the VR pain pioneer, envisions a future where VR environments can be selected for different therapeutic needs and procedures much like one can select movies to stream online (Marchant 2017). With further development, the optimal VR therapeutic pain experience may prove to be one that is entirely individualistic, tailored to a patient’s specific situational needs and desires, and possibly one that is created by the patient themselves. The future of VR therapy is wide open and will likely combine these visions for future therapeutic uses.
Today VR pain therapy uses environments that try to influence a positive affect by isolating a patient from the hospital environment, supplying aesthetically pleasing graphics, and allowing for a fun interaction in a distracting virtual environment. VR environments that adhere to the basic guidelines addressed in Table 29.3. have proven sufficient in previous studies for improved subjective pain ratings (6–9), but new and novel VR therapeutic experiences deserve investigation.
Future Directions
With national attention turned to prescription drug and opiate abuse, VR therapy offers a possible alternative and/or adjunct to existing pain therapies with few side effects. VR therapy promises new solutions and new opportunities to help alleviate patient’s suffering, especially in acute pain settings.
Although VR therapy has been studied for nearly two decades, its development is still thought to be in its early stages. Commercial headsets have only recently become available to the general public, and new devices are awaiting release. Technology continues to evolve, and immersive capabilities continue to improve at an exponential rate. New high-resolution screens, light-field display technology, and peripheral accessories will allow for greater degrees for immersion that theoretically will allow for a more robust VR pain relief experience.
Research continues into what constitutes an optimal VR therapeutic experience for pain therapy as well as the underlying mechanisms. Although current VR therapy has shown promising results in the literature, it is quite possible that with further development and research, VR pain experiences will appear quite different from the designs used today. Like consumer VR for entertainment purposes, the success of VR analgesic therapy will depend on the creation and investigation of new VR therapy content to appeal to a wide range of patients and clinical care settings.
Lastly, VR hardware and software have resulted in low-cost, lightweight VR systems that can be powered by laptop and handheld devices allowing for VR analgesia therapy to move out of the realm of labs and academic research institutions. Today, VR analgesia and therapy is poised to extend into diverse patient clinical settings, community hospitals, patients’ homes, and low-resource environments or countries, as costs continue to decrease and products become more accessible.
References
Aardema, F., O’Connor, K., Côté, S., & Taillon, A. (2010). Virtual reality induces dissociation and lowers sense of presence in objective reality. Cyberpsychology, Behavior, and Social Networking, 13(4), 429–435. https://doi.org/10.1089/cyber.2009.0164.
Apfelbaum, J. L., Chen, C., Mehta, S. S., & Gan, T. J. (2003). Postoperative pain experience: Results from a national survey suggest postoperative pain continues to be undermanaged. Anesthesia and Analgesia, 97(2), 534–540 Table of contents.
Askay, S. W., Patterson, D. R., & Sharar, S. R. (2009). Virtual reality hypnosis. Contemporary Hypnosis, 26(1), 40–47. https://doi.org/10.1002/ch.371.
Bantick, S. J., Wise, R. G., Ploghaus, A., Clare, S., Smith, S. M., & Tracey, I. (2002). Imaging how attention modulates pain in humans using functional MRI. Brain: A Journal of Neurology, 125(Pt 2), 310–319.
Barnes, P. M., Bloom, B., & Nahin, R. L. (2008). Complementary and alternative medicine use among adults and children: United States, 2007. National Health Statistics Reports, 12, 1–23.
Bawa, F. L. M., Mercer, S. W., Atherton, R. J., Clague, F., Keen, A., Scott, N. W., & Bond, C. M. (2015). Does mindfulness improve outcomes in patients with chronic pain? Systematic review and meta-analysis. The British Journal of General Practice: The Journal of the Royal College of General Practitioners, 65(635), e387–e400. https://doi.org/10.3399/bjgp15X685297.
Bowman, D. A., & McMahan, R. P. (2007). Virtual reality: How much immersion is enough? Computer, 40(7), 36–43. https://doi.org/10.1109/MC.2007.257.
Bromley Milton, M., Börsbo, B., Rovner, G., Lundgren-Nilsson, Å., Stibrant-Sunnerhagen, K., & Gerdle, B. (2013). Is pain intensity really that important to assess in chronic pain patients? A study based on the Swedish quality registry for pain rehabilitation (SQRP). PLoS One, 8(6), e65483. https://doi.org/10.1371/journal.pone.0065483.
Brooks, F. P. (1999). What’s real about virtual reality? IEEE Computer Graphics and Applications, 19(6), 16–27. https://doi.org/10.1109/38.799723.
Carlin, A. S., Hoffman, H. G., & Weghorst, S. (1997). Virtual reality and tactile augmentation in the treatment of spider phobia: A case report. Behaviour Research and Therapy, 35(2), 153–158.
Carrougher, G. J., Hoffman, H. G., Nakamura, D., Lezotte, D., Soltani, M., Leahy, L., Engrav, L. H., & Patterson, D. R. (2009). The effect of virtual reality on pain and range of motion in adults with burn injuries. Journal of Burn Care & Research: Official Publication of the American Burn Association, 30(5), 785–791.
Cepeda, M. S., Carr, D. B., Lau, J., & Alvarez, H. (2006). Music for pain relief. The Cochrane Database of Systematic Reviews, 2, CD004843. https://doi.org/10.1002/14651858.CD004843.pub2.
Compton, W. M., & Volkow, N. D. (2006). Abuse of prescription drugs and the risk of addiction. Drug and Alcohol Dependence, 83, S4–S7. https://doi.org/10.1016/j.drugalcdep.2005.10.020.
Cullen, K. A., Hall, M. J., & Golosinskiy, A. (2009). Ambulatory surgery in the United States, 2006. National Health Statistics Reports, 11, 1–25.
Davis, J. (2017, October 26). Trump declares opioid crisis a ‘health emergency’ but requests no funds. The New York Times. Retrieved from https://www.nytimes.com/2017/10/26/us/politics/trump-opioid-crisis.html
Davis, S., Nesbitt, K., & Nalivaiko, E. (2014). A systematic review of cybersickness. IE2014 Proceedings on the 2014 Conference on Interactive Entertainment. Newcastle, Australia; pp. 1–9. ISBN: 978-1-4503-2790-9
Deng, G., Cassileth, B. R., & Yeung, K. S. (2004). Complementary therapies for cancer-related symptoms. The Journal of Supportive Oncology, 2(5), 419–426 discussion 427-429.
Descartes, R. (1998). Discourse on method and meditations on first Philosophy (4th ed.). Indianapolis: Hackett Publishing Company.
Eccleston, C. (2001). Role of psychology in pain management. British Journal of Anaesthesia, 87(1), 144–152.
Eccleston, C., & Crombez, G. (1999). Pain demands attention: A cognitive-affective model of the interruptive function of pain. Psychological Bulletin, 125(3), 356–366.
Faber, A. W., Patterson, D. R., & Bremer, M. (2013). Repeated use of immersive virtual reality therapy to control pain during wound dressing changes in pediatric and adult burn patients. Journal of Burn Care & Research: Official Publication of the American Burn Association, 34(5), 563–568. https://doi.org/10.1097/BCR.0b013e3182777904.
Farrar, J. T., Portenoy, R. K., Berlin, J. A., Kinman, J. L., & Strom, B. L. (2000). Defining the clinically important difference in pain outcome measures. Pain, 88(3), 287–294.
Fernandez, E., & Turk, D. C. (1989). The utility of cognitive coping strategies for altering pain perception: A meta-analysis. Pain, 38(2), 123–135.
Frey, D. P., Bauer, M. E., Bell, C. L., Low, L. K., Hassett, A. L., Cassidy, R. B., & Boyer, K. D. (2018). Virtual reality analgesia in labor: The VRAIL pilot study—A preliminary randomized controlled trial suggesting benefit of immersive virtual reality analgesia in unmedicated laboring women. Anesthesia & Analgesia. https://doi.org/10.1213/ANE.0000000000003649.
Gan, T. J. (2017). Poorly controlled postoperative pain: Prevalence, consequences, and prevention. Journal of Pain Research, 10, 2287–2298. https://doi.org/10.2147/JPR.S144066.
Gan, T. J., Habib, A. S., Miller, T. E., White, W., & Apfelbaum, J. L. (2014). Incidence, patient satisfaction, and perceptions of post-surgical pain: Results from a US national survey. Current Medical Research and Opinion, 30(1), 149–160. https://doi.org/10.1185/03007995.2013.860019.
Garcia-Palacios, A., Hoffman, H., Carlin, A., Furness, T. A., & Botella, C. (2002). Virtual reality in the treatment of spider phobia: A controlled study. Behaviour Research and Therapy, 40(9), 983–993.
Gaskin, D. J., & Richard, P. (2012). The economic costs of pain in the United States. The Journal of Pain: Official Journal of the American Pain Society, 13(8), 715–724. https://doi.org/10.1016/j.jpain.2012.03.009.
Gonzalez-Franco, M., & Lanier, J. (2017). Model of illusions and virtual reality. Frontiers in Psychology, 8. https://doi.org/10.3389/fpsyg.2017.01125.
Gupta, A., Scott, K., & Dukewich, M. (2017). Innovative technology using virtual reality in the treatment of pain: Does it reduce pain via distraction, or is there more to it? Pain Medicine. https://doi.org/10.1093/pm/pnx109.
Hadfield, J. A. (2015). Introduction to psychotherapy: Its history and modern schools. London: Routledge.
Hecht, J. (2016). Optical dreams, virtual reality. Optics and Photonics News, 27(6), 24. https://doi.org/10.1364/OPN.27.6.000024.
Hodes, R. L., Howland, E. W., Lightfoot, N., & Cleeland, C. S. (1990). The effects of distraction on responses to cold pressor pain. Pain, 41(1), 109–114.
Hoffman, H. G. (2004). Virtual-reality therapy. Scientific American, 291(2), 58–65.
Hoffman, H. G., Doctor, J. N., Patterson, D. R., Carrougher, G. J., & Furness, T. A. (2000). Virtual reality as an adjunctive pain control during burn wound care in adolescent patients. Pain, 85(1–2), 305–309.
Hoffman, H. G., Garcia-Palacios, A., Patterson, D. R., Jensen, M., Furness, T., & Ammons, W. F. (2001a). The effectiveness of virtual reality for dental pain control: A case study. Cyberpsychology & Behavior: The Impact of the Internet, Multimedia and Virtual Reality on Behavior and Society, 4(4), 527–535. https://doi.org/10.1089/109493101750527088.
Hoffman, H. G., Patterson, D. R., Carrougher, G. J., & Sharar, S. R. (2001b). Effectiveness of virtual reality-based pain control with multiple treatments. The Clinical Journal of Pain, 17(3), 229–235.
Hoffman, H. G., Garcia-Palacios, A., Kapa, V., Beecher, J., & Sharar, S. R. (2003a). Immersive virtual reality for reducing experimental ischemic pain. International Journal of Human-Computer Interaction, 15(3), 469–486. https://doi.org/10.1207/S15327590IJHC1503_10.
Hoffman, H. G., Richards, T., Coda, B., Richards, A., & Sharar, S. R. (2003b). The illusion of presence in immersive virtual reality during an fMRI brain scan. Cyberpsychology & Behavior: The Impact of the Internet, Multimedia and Virtual Reality on Behavior and Society, 6(2), 127–131. https://doi.org/10.1089/109493103321640310.
Hoffman, H. G., Richards, T. L., Magula, J., Seibel, E. J., Hayes, C., Mathis, M., Sharar, S. R., & Maravilla, K. (2003c). A magnet-friendly virtual reality fiberoptic image delivery system. Cyberpsychology & Behavior: The Impact of the Internet, Multimedia and Virtual Reality on Behavior and Society, 6(6), 645–648. https://doi.org/10.1089/109493103322725423.
Hoffman, H. G., Richards, T. L., Coda, B., Bills, A. R., Blough, D., Richards, A. L., & Sharar, S. R. (2004a). Modulation of thermal pain-related brain activity with virtual reality: Evidence from fMRI. Neuroreport, 15(8), 1245–1248. https://doi.org/10.1097/01.wnr.0000127826.73576.91.
Hoffman, H. G., Sharar, S. R., Coda, B., Everett, J. J., Ciol, M., Richards, T., & Patterson, D. R. (2004b). Manipulating presence influences the magnitude of virtual reality analgesia. Pain, 111(1), 162–168. https://doi.org/10.1016/j.pain.2004.06.013.
Hoffman, H. G., Seibel, E. J., Richards, T. L., Furness, T. A., Patterson, D. R., & Sharar, S. R. (2006). Virtual reality helmet display quality influences the magnitude of virtual reality analgesia. The Journal of Pain, 7(11), 843–850. https://doi.org/10.1016/j.jpain.2006.04.006.
Hoffman, H. G., Richards, T. L., Van Oostrom, T., Coda, B. A., Jensen, M. P., Blough, D. K., & Sharar, S. R. (2007). The analgesic effects of opioids and immersive virtual reality distraction: Evidence from subjective and functional brain imaging assessments. Anesthesia and Analgesia, 105(6), 1776–1783., Table of contents. https://doi.org/10.1213/01.ane.0000270205.45146.db.
Hoffman, H. G., Chambers, G. T., Meyer, W. J., Arceneaux, L. L., Russell, W. J., Seibel, E. J., Richards, T. L., Sharar, S. R., & Patterson, D. R. (2011). Virtual reality as an adjunctive non-pharmacologic analgesic for acute burn pain during medical procedures. Annals of Behavioral Medicine, 41(2), 183–191. https://doi.org/10.1007/s12160-010-9248-7.
Hoffman, H. G., Meyer, W. J., Ramirez, M., Roberts, L., Seibel, E. J., Atzori, B., Sharar, S. R., & Patterson, D. R. (2014). Feasibility of articulated arm mounted oculus rift virtual reality goggles for adjunctive pain control during occupational therapy in pediatric burn patients. Cyberpsychology, Behavior, and Social Networking, 17(6), 397–401. https://doi.org/10.1089/cyber.2014.0058.
Johnson, M. (2007). Transcutaneous electrical nerve stimulation: Mechanisms, clinical application and evidence. Reviews in Pain, 1(1), 7–11. https://doi.org/10.1177/204946370700100103.
Johnson, S., & Coxon, M. (2016). Sound can enhance the analgesic effect of virtual reality. Royal Society Open Science, 3(3), 150567. https://doi.org/10.1098/rsos.150567.
Jones, T., Moore, T., & Choo, J. (2016). The impact of virtual reality on chronic pain. PLoS One, 11(12), e0167523. https://doi.org/10.1371/journal.pone.0167523.
Kahneman, D. (1973). Attention and effort. Englewood Cliffs: Prentice-Hall.
Keefe, F. J., Huling, D. A., Coggins, M. J., Keefe, D. F., Rosenthal, Z. M., Herr, N. R., & Hoffman, H. G. (2012). Virtual reality for persistent pain: A new direction for behavioral pain management. Pain, 153(11), 2163–2166. https://doi.org/10.1016/j.pain.2012.05.030.
Kennedy, R. S., Lane, N. E., Berbaum, K. S., & Lilienthal, M. G. (1993). Simulator sickness questionnaire: An enhanced method for quantifying simulator sickness. The International Journal of Aviation Psychology, 3(3), 203–220. https://doi.org/10.1207/s15327108ijap0303_3.
Kennedy, R. S., Stanney, K. M., & Dunlap, W. P. (2000). Duration and exposure to virtual environments: Sickness curves during and across sessions. Presence: Teleoperators and Virtual Environments, 9(5), 463–472. https://doi.org/10.1162/105474600566952.
Koppert, W., & Schmelz, M. (2007). The impact of opioid-induced hyperalgesia for postoperative pain. Best Practice & Research Clinical Anaesthesiology, 21(1), 65–83. https://doi.org/10.1016/j.bpa.2006.12.004.
la Cour, P., & Petersen, M. (2015). Effects of mindfulness meditation on chronic pain: A randomized controlled trial. Pain Medicine, 16(4), 641–652. https://doi.org/10.1111/pme.12605.
Langer, S. K. (1953). Feeling and form: A theory of art. New York: Charles Scribner’s Sons. http://www.worldcat.org/title/feeling-and-form-a-theory-of-art/oclc/3234538.
Lanier, J. (2001). Virtually there. Scientific American, 284(4), 66–75.
Lanier, J. (2017). Dawn of the new everything: Encounters with reality and virtual reality (1st ed.). New York: Henry Holt and Company.
Lee, J. H. (2016). The effects of music on pain: A meta-analysis. Journal of Music Therapy, 53(4), 430–477. https://doi.org/10.1093/jmt/thw012.
Levin, M. F. (2011). Can virtual reality offer enriched environments for rehabilitation? Expert Review of Neurotherapeutics, 11(2), 153–155. https://doi.org/10.1586/ern.10.201.
Li, A., Montaño, Z., Chen, V. J., & Gold, J. I. (2011). Virtual reality and pain management: Current trends and future directions. Pain Management, 1(2), 147–157. https://doi.org/10.2217/pmt.10.15.
Lombard, M., & Ditton, T. (2006). At the heart of it all: The concept of presence. Journal of Computer-Mediated Communication, 3(2). https://doi.org/10.1111/j.1083-6101.1997.tb00072.x.
Loomis, J. M. (2016). Presence in virtual reality and everyday life: Immersion within a world of representation. Presence: Teleoperators and Virtual Environments, 25(2), 169–174. https://doi.org/10.1162/PRES_a_00255.
Mahrer, N. E., & Gold, J. I. (2009). The use of virtual reality for pain control: A review. Current Pain and Headache Reports, 13(2), 100–109.
Malbos, E., Rapee, R. M., & Kavakli, M. (2012). Behavioral presence test in threatening virtual environments. Presence: Teleoperators and Virtual Environments, 21(3), 268–280. https://doi.org/10.1162/PRES_a_00112.
Marchant, J. (2017). Virtual-reality worlds filled with penguins and otters are a promising alternative to painkillers. Quartz. Retrieved from https://qz.com/973605/the-opioid-epidemic-could-be-cured-with-virtual-reality-worlds-that-let-patients-escape-their-pain/
McCaul, K. D., & Malott, J. M. (1984). Distraction and coping with pain. Psychological Bulletin, 95(3), 516–533.
McDaid, C., Maund, E., Rice, S., Wright, K., Jenkins, B., & Woolacott, N. (2010). Paracetamol and selective and non-selective non-steroidal anti-inflammatory drugs (NSAIDs) for the reduction of morphine-related side effects after major surgery: A systematic review. Health Technology Assessment, 14(17). https://doi.org/10.3310/hta14170.
Melzack, R. (1990). The tragedy of needless pain. Scientific American, 262(2), 27–33.
Melzack, R., & Wall, P. D. (1965). Pain mechanisms: A new theory. Science New York, NY, 150(3699), 971–979.
Mishkind, M. C., Norr, A. M., Katz, A. C., & Reger, G. M. (2017). Review of virtual reality treatment in psychiatry: Evidence versus current diffusion and use. Current Psychiatry Reports, 19(11). https://doi.org/10.1007/s11920-017-0836-0.
Molteni, M. (2017). Opioids Haven’t solved chronic pain. Maybe Virtual Reality Can. WIRED.
Morris, L. D., Louw, Q. A., & Grimmer-Somers, K. (2009). The effectiveness of virtual reality on reducing pain and anxiety in burn injury patients: A systematic review. The Clinical Journal of Pain, 25(9), 815–826. https://doi.org/10.1097/AJP.0b013e3181aaa909.
Morris, L. D., Louw, Q. A., & Crous, L. C. (2010). Feasibility and potential effect of a low-cost virtual reality system on reducing pain and anxiety in adult burn injury patients during physiotherapy in a developing country. Burns: Journal of the International Society for Burn Injuries, 36(5), 659–664. https://doi.org/10.1016/j.burns.2009.09.005.
Neri, S. G. R., Cardoso, J. R., Cruz, L., Lima, R. M., de Oliveira, R. J., Iversen, M. D., & Carregaro, R. L. (2017). Do virtual reality games improve mobility skills and balance measurements in community-dwelling older adults? Systematic review and meta-analysis. Clinical Rehabilitation, 31(10), 1292–1304. https://doi.org/10.1177/0269215517694677.
Oculus Rift Best Practices. (2015). In: Oculus VR, LLC.
Oderda, G. M., Evans, R. S., Lloyd, J., Lipman, A., Chen, C., Ashburn, M., Burke, J., & Samore, M. (2003). Cost of opioid-related adverse drug events in surgical patients. Journal of Pain and Symptom Management, 25(3), 276–283. https://doi.org/10.1016/S0885-3924(02)00691-7.
Ohnhaus, E. E., & Adler, R. (1975). Methodological problems in the measurement of pain: A comparison between the verbal rating scale and the visual analogue scale. Pain, 1(4), 379–384.
Okie, S. (2010). A flood of opioids, a rising tide of deaths. The New England Journal of Medicine, 363(21), 1981–1985. https://doi.org/10.1056/NEJMp1011512.
Oliphant, J. (2017, August 10, Thu 21:54:29 UTC). Trump declares national emergency on opioid abuse. Reuters. Retrieved from https://www.reuters.com/article/us-usa-trump-opioid/trump-declares-national-emergency-on-opioid-abuse-idUSKBN1AQ2AW
Pourmand, A., Davis, S., Lee, D., Barber, S., & Sikka, N. (2017). Emerging utility of virtual reality as a multidisciplinary tool in clinical medicine. Games for Health Journal, 6(5), 263–270. https://doi.org/10.1089/g4h.2017.0046.
Rebenitsch, L. (2015). Managing cybersickness in virtual reality. XRDS: Crossroads, The ACM Magazine for Students, 22(1), 46–51. https://doi.org/10.1145/2810054.
Rosenblum, L. (2000). Virtual and augmented reality 2020. IEEE Computer Graphics and Applications, 20(1), 38–39. https://doi.org/10.1109/38.814551.
Rudd, R. A., Seth, P., David, F., & Scholl, L. (2016). Increases in drug and opioid-involved overdose deaths — United States, 2010–2015. MMWR. Morbidity and Mortality Weekly Report, 65(5051), 1445–1452. https://doi.org/10.15585/mmwr.mm655051e1.
Russell, J. A. (1980). A circumplex model of affect. Journal of Personality and Social Psychology, 39(6), 1161–1178. https://doi.org/10.1037/h0077714.
Schmitt, Y. S., Hoffman, H. G., Blough, D. K., Patterson, D. R., Jensen, M. P., Soltani, M., Carrougher, G. J., Nakamura, D., & Sharar, S. R. (2011). A randomized, controlled trial of immersive virtual reality analgesia, during physical therapy for pediatric burns. Burns: Journal of the International Society for Burn Injuries, 37(1), 61–68. https://doi.org/10.1016/j.burns.2010.07.007.
Sharar, S. R., Carrougher, G. J., Nakamura, D., Hoffman, H. G., Blough, D. K., & Patterson, D. R. (2007). Factors influencing the efficacy of virtual reality distraction analgesia during Postburn physical therapy: Preliminary results from 3 ongoing studies. Archives of Physical Medicine and Rehabilitation, 88(12), S43–S49. https://doi.org/10.1016/j.apmr.2007.09.004.
Sharar, S. R., Miller, W., Teeley, A., Soltani, M., Hoffman, H. G., Jensen, M. P., & Patterson, D. R. (2008). Applications of virtual reality for pain management in burn-injured patients. Expert Review of Neurotherapeutics, 8(11), 1667–1674. https://doi.org/10.1586/14737175.8.11.1667.
Sharar, S. R., Alamdari, A., Hoffer, C., Hoffman, H. G., Jensen, M. P., & Patterson, D. R. (2016). Circumplex model of affect: A measure of pleasure and arousal during virtual reality distraction analgesia. Games for Health Journal, 5(3), 197–202. https://doi.org/10.1089/g4h.2015.0046.
Slater, M., & Wilbur, S. (1997). A framework for immersive virtual environments (FIVE): Speculations on the role of presence in virtual environments. Presence: Teleoperators and Virtual Environments, 6(6), 603–616. https://doi.org/10.1162/pres.1997.6.6.603.
Stoelting, R. K., & Miller, R. D. (2007). Basics of anesthesia (5th ed.). Philadelphia: Churchill Livingstone.
Sulea, C., Soomro, A., Boyd, C., & Wiederhold, B. K. (2014). Pain management in virtual reality: A comprehensive research chart. Cyberpsychology, Behavior and Social Networking, 17(6), 402–413. https://doi.org/10.1089/cyber.2014.1514.
Sutherland, I. E. (1965). The ultimate display. Proceedings of the International Federation of Information Processing Congress, 2, 506–508.
Swarm, R. A., Abernethy, A. P., Anghelescu, D. L., Benedetti, C., Buga, S., Cleeland, C., Deleon-Casasola, O. A., Eilers, J. G., Ferrell, B., Green, M., Janjan, N. A., Kamdar, M. M., Levy, M. H., Lynch, M., RM, M. D., Moryl, N., Nesbit, S. A., Paice, J. A., Rabow, M. W., Syrjala, K. L., Urba, S. G., Weinstein, S. M., Dwyer, M., Kumar, R., & National Comprehensive Cancer, N. (2013). Adult cancer pain. Journal of the National Comprehensive Cancer Network: JNCCN, 11(8), 992–1022.
Torta, D. M., Legrain, V., Mouraux, A., & Valentini, E. (2017). Attention to pain! A neurocognitive perspective on attentional modulation of pain in neuroimaging studies. Cortex, 89, 120–134. https://doi.org/10.1016/j.cortex.2017.01.010.
Trost, Z., Zielke, M., Guck, A., Nowlin, L., Zakhidov, D., France, C. R., & Keefe, F. (2015). The promise and challenge of virtual gaming technologies for chronic pain: The case of graded exposure for low back pain. Pain Management, 5(3), 197–206. https://doi.org/10.2217/pmt.15.6.
Valet, M., Sprenger, T., Boecker, H., Willoch, F., Rummeny, E., Conrad, B., Erhard, P., & Tolle, T. R. (2004). Distraction modulates connectivity of the cingulo-frontal cortex and the midbrain during pain—An fMRI analysis. Pain, 109(3), 399–408. https://doi.org/10.1016/j.pain.2004.02.033.
Vincent, E., Battisto, D., Grimes, L., & McCubbin, J. (2010). The effects of nature images on pain in a simulated hospital patient room. HERD, 3(3), 42–55.
Welch, R. B. (2002). Adapting to virtual environments. In K. M. Staney (Ed.), Handbook of virtual environments: Design, implementation, and applications (p. 1232). Mahwah: Lawrence Erlbaum Associates.
Wender, R., Hoffman, H. G., Hunner, H. H., Seibel, E. J., Patterson, D. R., & Sharar, S. R. (2009). Interactivity influences the magnitude of virtual reality analgesia. Journal of Cyber Therapy and Rehabilitation, 2(1), 27.
Wiech, K., Seymour, B., Kalisch, R., Stephan, K. E., Koltzenburg, M., Driver, J., & Dolan, R. J. (2005). Modulation of pain processing in hyperalgesia by cognitive demand. NeuroImage, 27(1), 59–69. https://doi.org/10.1016/j.neuroimage.2005.03.044.
Wiederhold, B. K., Soomro, A., Riva, G., & Wiederhold, M. D. (2014). Future directions: Advances and implications of virtual environments designed for pain management. Cyberpsychology, Behavior and Social Networking, 17(6), 414–422. https://doi.org/10.1089/cyber.2014.0197.
Younger, J., McCue, R., & Mackey, S. (2009). Pain outcomes: A brief review of instruments and techniques. Current Pain and Headache Reports, 13(1), 39–43.
Zeidan, F., Emerson, N. M., Farris, S. R., Ray, J. N., Jung, Y., McHaffie, J. G., & Coghill, R. C. (2015). Mindfulness meditation-based pain relief employs different neural mechanisms than placebo and sham mindfulness meditation-induced analgesia. Journal of Neuroscience, 35(46), 15307–15325. https://doi.org/10.1523/JNEUROSCI.2542-15.2015.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Frey, D., Sharar, S.R. (2018). Virtual Reality Therapy for Acute/Procedural Pain. In: Moore, R. (eds) Handbook of Pain and Palliative Care. Springer, Cham. https://doi.org/10.1007/978-3-319-95369-4_29
Download citation
DOI: https://doi.org/10.1007/978-3-319-95369-4_29
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-95368-7
Online ISBN: 978-3-319-95369-4
eBook Packages: Behavioral Science and PsychologyBehavioral Science and Psychology (R0)