Abstract
It is projected that the number of individuals with dementia will continue to increase over the next several decades, with no cure in sight. Consequently, a greater understanding of how to promote behavioral health and quality of life for these individuals is becoming increasingly important. A common approach in the field is symptom management through pharmacologic approaches to cognitive enhancement and treatment of behavioral changes. Rather than a purely medical approach to dementia care, interventions to improve quality of life should involve comprehensive, integrated care. This chapter discusses literature that describes an integrated, contextual model of dementia care, in which comorbid conditions are appropriately treated, adaptive behaviors are supported, and excess disability is rectified or prevented. Within the context of this model of dementia care, the current chapter also describes the importance of family caregiver quality of life and neurocognitive education, in order to improve treatment for individuals suffering from this insidious disease.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
It is estimated that the worldwide number of individuals with dementia will reach 135 million by 2050 (Rahman, 2017; Rizzi, Rosset, & Roriz-Cruz, 2014) without any indication of a cure on the horizon. The label “dementia” is a summary term for a group of symptoms that include decline from previous levels of functioning , difficulties in expressive and receptive language, impaired judgment, impaired ability to acquire and remember new information, and impaired visuospatial abilities (McKhann et al., 2011). The most prevalent neurocognitive disorders leading to dementia are Alzheimer’s disease (AD) (77%; Barker et al., 2002; Hebert, Weuve, Scherr, & Evans, 2013), vascular dementia (VaD) (15–20%; Barker et al., 2002; Centers for Disease Control and Prevention, 2006), and dementia with Lewy bodies (10–26%; Barker et al., 2002; Jellinger & Attems, 2011), with over 30% of dementia cases involving mixed neuropathology (e.g., AD with cerebrovascular disease or AD with Lewy body), (Jellinger & Attems, 2011; LoGiudice & Watson, 2014). Importantly, diagnostic labels generally are not informative for describing an individual patient’s current level of functioning or predicting the rate of disease progression. Increasing evidence indicates that lifestyle, general health status, and environmental factors such as caregivers’ skill and emotional well-being significantly impact the functioning and quality of life of persons with neurocognitive disorders (Lwi, Ford, Casey, Miller, & Levenson, 2017; Vance & Struzick, 2007). This chapter will describe a model of person-centered care for promoting the quality of life and behavioral health of persons with neurocognitive disorders and their families.
The decline in memory and verbal functioning , which are predominant in the majority of neurocognitive disorders, present significant assessment and treatment challenges as patients eventually become unable to describe their internal physiological and psychological states (e.g., whether they are experiencing pain, discomfort, or changes therein following treatment of comorbid condition). The integration of specialty care focused both on the accuracy of diagnosis and support for optimizing the quality of life for the patient and his/her family is now considered to be best practice (Galvin & Sadowsky, 2012; van Hout, Vernooij-Dassen, & Stalman, 2007). Primary care providers have a particularly important role in promoting the safety and quality of life of patients with dementia as they are on the front lines for responding to (a) patient and family members’ concerns regarding changes in cognition, affect, and behavior prior to the diagnosis of a neurocognitive disorder, (b) guiding patients and their families through the diagnostic process, c) responding to patients’ and/or family members’ reports of changes in functioning and the detection and treatment of comorbid conditions following diagnosis, and (d) collaborating with patients and their families over the course of what can be years of disease progression (Boustani, Peterson, Hanson, Harris, & Lohr, 2003).
Epidemiology and Diagnosis of Neurocognitive Disorders
Diagnostic Challenges and Age-Associated Complications
Neurocognitive disorders are age-associated diseases, with the majority of patients developing symptomatology after the age of 65 and the highest incidence rate in individuals between the ages of 80 and 84 (Prince et al., 2013). Recent improvements in detection sensitivity have resulted in a higher rate of early onset neurocognitive disease diagnosis, i.e., disease onset prior to age 65 (Lambert et al., 2014). Early onset of a neurocognitive disease can present diagnostic challenges as memory lapses are less likely to be salient to younger adults, and thus they are less inclined to seek assessment by a healthcare provider. The base rates of early onset neurocognitive disease are very low; the “typical” patient with a neurocognitive disorder is older (Hebert et al., 2013), is retired (Lambert et al., 2014), and has a higher number of comorbid conditions (Abizanda et al., 2014).
Differential diagnosis of specific neurocognitive disorders is crucial for treatment planning, understanding expected changes vs. unexpected changes in disease trajectory, and optimizing quality of life for patients. In 2012 the National Institute on Aging published updated diagnostic criteria in an effort to improve the diagnostic accuracy of all neurocognitive disorders (see McKhann, Albert, & Sperling, 2012). The revised criteria are based on a continuous model of differential diagnosis and now include guidelines for assessing the transition from no cognitive decline to mild cognitive impairment to meeting the criteria for dementia. Second, the revised criteria allow for the possibility that impairment in memory may not be the primary symptom in individuals presenting with neurocognitive decline and that patients’ predominant symptomatology may involve language, spatial ability, or executive function. Third, additional causes of cognitive impairment have been incorporated within the criteria (e.g., Lewy bodies, frontotemporal lobar degeneration).
Unfortunately, reliance on non-evidence-based diagnostic procedures (e.g., brief cognitive screening alone, diagnosis absent neurological examination, and neuroimaging) continues to be a problem in the field (Paterson, Takada, & Geschwind, 2012). A recent study by Beach, Monsell, Phillips, and Kukull (2012) evaluated clinical and neuropathology autopsy data for more than 1100 subject. The researchers found that, between 2005 and 2010, specificity of the exact disease ranged from 44.3% to 70.8%, depending on the diagnostic criteria used. The wide variability in diagnostic specificity speaks to the challenge of accurately identifying the etiology of neurocognitive symptoms. In contrast to standard practice, the integrated care model incorporates the expertise of specialists (neurologists, neuropsychologists), resulting in a more thorough and accurate diagnostic evaluation (Villars et al., 2010).
An integrated model of healthcare is characterized by a high degree of collaboration and communication between health professionals with the shared goal of optimizing patient health through a variety of prevention and intervention strategies . Treatment planning is comprehensive in addressing the biological, psychological, and social needs of the patient. Integrated healthcare teams include a diverse group of members (e.g., physicians, nurses, psychologists, social workers, and other health professionals; American Psychological Association, 2017). While involvement of an interdisciplinary team may increase healthcare costs in the short term, a pilot study investigated integrated care and found it to be economically effective in reducing costs in the long term (Bandurska et al., 2017). Reduced costs in the long term are realized through effective detection and management of comorbid conditions and associated prevention of excess disability, (Looman, Huijsman, Bouwmans-Frijters, Stolk, & Fabbricotti, 2016) and the prevention or delay of institutionalization (Dramé et al., 2011).
Unique Issues in the Treatment of Persons with Dementia
Dementia-Specific Challenges in Polypharmacy
Polypharmacy , defined as the use of two or more medications (see Brown, 2016; Gnjidic et al., 2012; Hovstadius & Petersson, 2012), is highly prevalent within geriatric healthcare, with more than one third of prescriptions in the United States being filled by individuals over the age of 65 (Marcum, Driessen, Thorpe, Gellad, & Donohue, 2014). Polypharmacy increases the risk of drug reactions and severe side effects (Brown, 2016; Norgaard, Jensen-Dahm, Gasse, Hansen, & Waldemar, 2017). Pharmacological intervention with patients with dementia typically includes both cognitive enhancing and psychotropic medications in addition to medications prescribed for comorbid age-associated conditions. A recent study of over 250,000 older adults found that individuals with a neurocognitive disorder had a significantly higher rate of polypharmacy, even when controlling for age, gender, and comorbidities, and that individuals experiencing polypharmacy were at higher risk for migraines, dizziness, and hypertension (Clague, Mercer, McLean, Reynish, & Guthrie, 2016).
Pharmacological Approaches to Cognitive Enhancement
Currently, there are four medications that have been approved by the FDA for individuals with neurocognitive disorder: donepezil, galantamine, rivastigmine, and memantine (Di Santo, Prinelli, Adorni, Caltagirone, & Musicco, 2013; Tan et al., 2014). A Cochrane meta-analysis was performed to evaluate treatment effects, including effects of these four medications on cognition and activities of daily living (ADLs) . Thirty-four (34) RCTs fit the criteria that included being written in English, published before 2012, and evaluated treatment effects of the four medications on individuals with neurocognitive disorders. Memantine had the greatest treatment effect throughout all studies , with the other three medications producing equivocal results when compared to the placebo (Di Santo et al., 2013). Many of the studies included within the meta-analysis did not examine patient functioning beyond 3 months, and therefore, long-term effects were not analyzed. The RCTs that did report long-term outcomes showed the medications had little to no effect on cognitive decline. Moreover, Geldmacher (2003) and Lopez et al. (2009) reported moderate improvement in cognition for individuals with Alzheimer’s disease using “cognitive enhancing” medications but found only minimal effects in 40% of the entire sample.
Several side effects (e.g., urinary incontinence, fatigue, dizziness, nausea) have been reported for each of the currently approved cognitive enhancing medications (Bond et al., 2012; Kim, Brown, Ding, Kiel, & Berry, 2011). Additionally, the cognitive enhancing medications have been reported to exacerbate confusion and increase the risk of falls and sleep problems, which already occur at high rates for patients with neurocognitive disorder (Kim et al., 2011; McKhann et al., 2011). The verbal deficits that develop during the course of degenerative neurocognitive disorders present challenges when family healthcare advocates and healthcare providers analyze the risks and benefits of medication and drug effects/side effects.
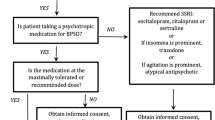
Pharmacological Management of Behavioral and Affective Changes
In recent years, the treatment of individuals with a neurocognitive disorder has become increasingly controversial due to the prevalent use of psychotropic medication for the management of what are commonly referred to as “non-cognitive psychiatric symptoms .” Over 25% of older adults diagnosed with a neurocognitive disorder are medicated with two or more psychotropic drugs (Norgaard et al., 2017). Antipsychotic medications have been the primary intervention for behavioral or “non-cognitive psychiatric symptoms” related to neurocognitive disorders (Chiu, Bero, Hessol, Lexchin, & Harrington, 2015; Kales, Gitlin, & Lyketsos, 2015; Molinari et al., 2010; Vasudev et al., 2015) despite FDA black box warnings against their use in the care of elderly persons with dementia due to the risk of serious adverse effects (Centers for Medicare & Medicaid Services, 2013; U.S. Food and Drug Administration, 2008). A recent study (Norgaard et al., 2017) reported that 25% of individuals with dementia were prescribed antipsychotic medication despite studies reporting that antipsychotics increase mortality and yield little, if any, positive effects (see Ballard et al., 2009; Maust et al., 2015). Alarmingly, a study of 559 individuals who were diagnosed with a neurocognitive disorder and prescribed psychotropic medication found that only 10% of the prescription and/or management of psychotropic drug use was appropriate. The three major categories of inappropriate use of psychotropic medications involved indication, inadequate evaluation, and therapy duration (van der Spek et al., 2016).
Maust et al. (2015) investigated mortality rates of 90,786 individuals over the age of 65 who were diagnosed with dementia and administered at least one antipsychotic, such as haloperidol, olanzapine, risperidone, and quetiapine. Outcome measures included the absolute change in mortality risk and the Veteran’s Affairs registries, based on mortality data obtained from the US National Death Index . The mortality risk of haloperidol and risperidone users was found to be almost double than that of nonusers. Moreover, findings at the 180-day outcome demonstrated the use of haloperidol for individuals with dementia was associated with 1 additional death for every 26 patients . In general, both antipsychotics and antidepressants statistically increased the risk of mortality for individuals with dementia, in comparison to nonusers (e.g., Ballard et al., 2009; Wang et al., 2014).
Numerous studies have evaluated both the short- and long-term effects of antipsychotics on behavioral and psychological symptoms for persons with dementia (e.g., Tampi, Tampi, Balachandran, & Srinivasan, 2016). Tampi and colleagues (2016) conducted a systematic review of meta-analyses that examined the use of antipsychotics in individuals with forms of dementia, including Alzheimer’s disease, Lewy bodies, and VaD . Inclusion criteria included being published in a peer-reviewed journal and examining psychotropic medication’s effect on individuals with dementia. Based on the eight studies included in the meta-analysis, Tampi and colleagues (2016) concluded that the use of antipsychotic drugs resulted in moderate improvements in psychosis (delusions and hallucinations) and improvements in agitation (i.e., physical aggression, verbal aggression, excitability, oppositional behavioral, and excessive motor activity) within the first 4 weeks; however, there were no long-term improvements, and severe adverse events were reported (e.g., cerebrovascular adverse events, Parkinsonism, sedation, gait disturbance, cognitive decline, pneumonia). These results further indicate that antipsychotics are contraindicated for the treatment of behavioral problems in persons with dementia, as there are limited short-term benefits and serious adverse effects, including premature death.
As mentioned earlier, monitoring of treatment effects (either positive or negative) is a significant challenge in the care of verbally impaired individuals. Monitoring the effects of antipsychotic medications presents a unique challenge as several of the side effects of antipsychotic medications mirror the symptoms of degenerative neurocognitive disorders (e.g., confusion, loss of language, etc.). Schneider, Dagerman, and Insel (2005) reported sedation (15–24% of the participants with dementia), confusion (11–18%), and cognitive disturbances (5–7%) as common adverse events related to atypical antipsychotic treatment, concluding that “adverse events offset the advantages in the efficacy of atypical antipsychotic drugs” (p. 1525). The most recent American Geriatric Society (AGS) Beers consensus criteria for safe medication use in the elderly recommend avoiding antipsychotics in the treatment of elderly with dementia, due to the increased mortality and cerebrovascular accident risk (Campanelli, 2012).
Healthcare Implications of Judgments of Quality of Life in Patients with Dementia
Quality of life (QoL) is a broad and multidimensional construct that encompasses physical, mental, social, and role functioning and health perceptions (Bowling et al., 2015). The World Health Organization defines QoL as an “…individual’s perceptions of their position in life in the context of the culture and value systems in which they live, and in relation to their goals, expectations, standards and concerns” (Bowling, 2001; World Health Organization, 1997). The importance of clear criteria and procedures for evaluating the QoL of persons with neurocognitive disorders is critical, as medical proxies often make decisions to treat or discontinue treatment of comorbid conditions based on their perceptions of the patient’s QoL. If a patient is experiencing excess disability (e.g., the patient appears to be in the advanced stage of a neurocognitive disorder but is actually evidencing the effects of sedation due to overmedication), the medical proxy may decide to discontinue treatment of a comorbid based on an incorrect condition(s). Additionally, care facilities are increasingly requiring that their staff measure QoL to create goals specifically focused on improving QoL for individuals with neurocognitive disorders (Beerens et al., 2014; Beerens, Zwakhalen, Verbeek, Ruwaard, & Hamers, 2013).
The American Academy of Neurology (Doody et al., 2001) and the World Alzheimer’s report (Prince, Comas-Herrera, Knapp, Guerchet, & Karagiannidou, 2016) propose that interventions to improve QoL should encompass comprehensive integrated care . As stated above, accurate diagnosis is crucial for developing an appropriate treatment plan. Yet research has consistently found that the diagnosis and treatment of individuals with dementia is often suboptimal for reasons including lack of differential diagnosis, inadequate treatment of comorbid conditions , and misattribution of excess disability due to treatable adverse medical or environmental events (see Doody et al., 2001; Odenheimer et al., 2013).
A “Contextual” Model of Dementia Care
The significant variability in functioning and rate of disease progression within neurocognitive disease diagnostic groups strongly suggests that lifestyle, environmental, and genetic variables impact the health and quality of life of persons with dementia (Brown, Lockwood, & Sonawane, 2005; Van Duijn et al., 1994). The contextual model of behavior posits that behavior is context bound and based on an interaction of the person’s learning and genetic histories with the current environment that sets the occasion for the production of the behavior (Catania, 1996). When applied to the functioning of persons with dementia, the goal of intervention is to support the maintenance of behavior in an individual who will inevitably experience devastating losses due to neurodegeneration. Strategies for promoting behavioral health are identified through an assessment of the individual’s learning history, current physiological status and behavioral repertoire, and the features of the current environment that support or inhibit the patient’s repertoire (Fisher, Drossel, Yury, & Cherup, 2007). A substantial body of literature indicates that the functioning of persons with neurocognitive disorders is influenced by environmental factors, including the affective responding of persons around them as well as sensory stimuli (see Buchanan, Christenson, Houlihan, & Ostrom, 2011; Fleming, Goodenough, Low, Chenoweth, & Brodaty, 2016). Following diagnosis, the behavior of patients with dementia is often misattributed to the underlying neuropathology, even when contextually appropriate. For example, if a verbally impaired patient responds in a distressed or “agitated” manner to negative affect and corrective feedback by a family member, the patient’s reaction (which would be considered a normal reaction to rude behavior in a cognitively healthy individual) is highly likely to be pathologized as a symptom of the disease. The administration of medications to reduce what is judged to be a behavioral “symptom” may accelerate reduction of the patient’s already diminishing repertoire (Garrison-Diehn, Rummel, & Fisher, 2013).
Numerous non-pharmacological interventions focused on supporting adaptive behavior and/or preventing problem behaviors by identifying and treating the underlying cause (e.g., pain, discomfort, over or understimulation, punitive caregiver behavior) have been shown to be efficacious (see Buchanan et al., 2011; Gitlin, Kales, & Lyketsos, 2012; Gitlin, Winter, Dennis, Hodgson, & Hauck, 2010).
Maintaining Adaptive Behavior While Preventing Excess Disability
Excess disability involves a decline in functioning that exceeds what would be expected based on an individual’s underlying medical condition (Dawson, Wells, & Kline, 1993). Over the course of degenerative neurocognitive disorders, excess disability is manifested in the premature loss of behavior (e.g., when a medication causes impairment in language or increased confusion; Yury & Fisher, 2007). Promoting behavioral health in persons with neurocognitive disorders often requires the detection, reduction, or prevention of premature declines in functioning and maintaining or restoring function (Fisher et al., 2007).
Behaviors that are viewed as challenging are commonly treated with approaches that aim to reduce or eliminate the behavior (Enns, Rhemtulla, Ewa, Fruetel, & Holroyd-Leduc, 2014) through environmental, physical, and/or chemical restraints. However, studies have demonstrated that these “restraint based” interventions can have serious adverse effects on individual with dementia including increased risk of falls and serious injury and premature death (see Baert, Gorus, Mets, Geerts, & Bautmans, 2011; Ballard et al., 2009; Neufeld et al., 1999).
Chemical restraints are defined as “any drug used for discipline or convenience and not required to treat medical symptoms” (U.S. Department of Health and Human Services, 2005). As explicated above, antipsychotics are commonly used to reduce behaviors that are judged to be a problem or “neuropsychiatric symptom ” among individuals diagnosed with a neurocognitive disorder, despite evidence of an increased risk of mortality associated with use of antipsychotics in this population (Ballard et al., 2009). The use of medication to decrease any behavior in individuals with a neurocognitive disorder is particularly concerning, even when targeting behavior that is viewed as problematic. The inappropriate use of medications for chemical restraint can lead to excess disability in the form of a premature reduction in an individual’s behavioral and verbal repertoire (Fisher et al., 2007).
Unlike restraint-based approaches, treatment goals within the contextual model of dementia care focus on maintaining an individual’s behavioral repertoire. Within the behavioral model, effective approaches to treatment assess the functional relevance of all behaviors, including ones labeled as challenging. Treatments focused on supporting adaptive behavior and preventing rather than eliminating challenging behavior ultimately reduce excess disability or prevent it altogether.
Family caregivers play a critically important role in promoting the health of persons with dementia as they are in a position of observing and reporting information about changes in cognitive and behavioral health (e.g., as reflected in changes in the patient’s verbal responding and ability to complete self-care and more complex tasks such as managing finances and medications) and safety (e.g., based on observations of impaired driving and/or confusion in the use of potentially dangerous machinery and household appliances) . To illustrate, abrupt changes in long-standing high-frequency behaviors may help family caregivers and healthcare providers detect adverse medical and/or environmental events (an abrupt decline in a patient’s appetite, verbal expressiveness, or activity level may indicate an acute condition such as an infection or medication side effect). In addition, family caregivers and their relationship (both the relationship history and current relationship) with the patient are critical features of the context of the patient’s experience.
Barriers to Maintaining Adaptive Behavior
The multifaceted nature of dementia symptoms and comorbidities in individuals with a neurocognitive disorder contribute to the difficulty in detecting adverse effects. Adverse events may be physiological and psychological (Andreassi, 2013; Fauth & Gibbons, 2014). Psychological events include, but are not limited to, depression, anxiety, hallucinations (mostly seen in dementia with Lewy Bodies), and apathy (Fauth & Gibbons, 2014). Physiological adverse events include, but are not limited to, pain, insomnia, and confusion (Andreassi, 2013). Both psychological and physiological adverse events have been reported as significant barriers to maintaining adaptive behavior in individuals with neurocognitive disorder.
Depression
Depression occurs at significantly higher rates in elderly persons with dementia when compared to cognitively healthy elderly. A recent study of rates of depression (depression assessed using the Cornell Scale of Depression) within a sample of 1000 individuals with dementia found that 50.2% of participants had a score that was considered in the clinically significant range for depression (Knapskog, Barca, & Engedal, 2014). A 34-site prospective study found that individuals with dementia were more than twice as likely than those with normal cognition to be diagnosed with depression (Snowden et al., 2015). Despite these high rates, a recent study found that only 18% of individuals who have depression and a neurocognitive disorder receive any form of treatment (Goodarzi, Mele, Roberts, & Holroyd-Leduc, 2017). The undertreatment of depression in this population may be due to the difficulties with detecting depression in a verbally impaired population and the misattribution of depression symptoms (e.g., social withdrawal, decline in activity, sleep disturbance, etc.) to neurodegeneration. This is troubling, as depression can have serious negative effects on an individual with neurocognitive impairment, including interfering with adaptive behavior. Beyond the personal suffering an individual with a neurocognitive disorder experiences, depression can exacerbate the symptoms of neurocognitive disorder (Alexopoulos, 2005). Moreover, the comorbid depression in individuals with neurocognitive disorder can interfere with the individuals’ ability to complete activities and maintain healthy relationships with people around them, both of which have been shown to improve QoL .
Pain
It is estimated that over 50% of individuals over the age of 65 experience regular pain (Achterberg et al., 2013). Pain is one of the most common precursors of excess disability and behavioral disturbance in individuals with a neurocognitive disorder. Progressive impairment in the ability to verbally label and report private experiences such as pain or discomfort presents a significant barrier to the health and quality of life of persons with dementia (see Achterberg et al., 2013; Husebo et al., 2008). As discussed earlier, these medications have been found to have substantial side effects including mortality, cerebrovascular events, and increased risk of falls (Ballard, Smith, Corbett, Husebo, & Aarsland, 2011). Moreover, the pain interferes with adaptive behavior, such as utilization of coping strategies, and acts as a catalyst to increase behavioral changes. In order to reduce and detect pain behaviors in a more strategic way, Achterberg and colleagues (2013) recommended the utilization of “pain teams” as opportunities for staff to consult with experts in neurocognitive care settings to develop collaborative treatment recommendations. Utilizing an integrated healthcare model would be potentially valuable in ensuring future improvements in the effective management of pain in individuals with neurocognitive disorder.
Promotion of Health to Improve Wellness for Individuals with Dementia
Behavioral activation is an evidence-based treatment for depression that has been found to be effective for every age group (Yon & Scogin, 2008). The key component of behavior activation is behavioral repertoire to increase contact with positive consequences. This may include engaging in more activities rather than being inactive, withdrawn, and avoidant (Snarski et al., 2011). Behavioral activation has been found to be efficacious for geriatric populations (Moss, Scogin, Di Napoli, & Presnell, 2012; Snarski et al., 2011; Yon & Scogin, 2008), which is important due to the high rates of isolation and decreases in engagement in activities for this population. The advantage of using a treatment such as behavioral activation to increase health and wellness is that it is a short-term therapy and easy to understand, due to its basic adherence of behavioral principles (Snarski et al., 2011). However, there are only a limited number of studies that have investigated behavioral activation with individuals with dementia. In a study of mental disorders in an older cohort, Snarski and colleagues (2011) found that behavioral activation decreased rates of depression for all mental disorders; however, there were only nine participants who were diagnosed with dementia, and there was no between group analysis. To our knowledge, there is no RCT that has investigated behavioral activation in individuals with any neurocognitive disorder. Notwithstanding, in promoting health and wellness in individuals with dementia, exercise (a possible activity for behavioral activation) has been found to be efficacious with this population.
Activity level tends to be inversely correlated with age but highly correlated with quality of life, mood, and cognitive health in the elderly including those with a neurocognitive disorder (Rolland et al., 2007). Due to the heuristic that individuals with neurocognitive disorder are “fragile” and “too cognitively impaired” to participate in any type of exercise, these individuals are not given the opportunity to partake in exercises (Bauman, Merom, Bull, Buchner, & Fiatarone Singh, 2016). Teri and colleagues (2003) found that just 60 min of exercise per week for individuals with Alzheimer’s disease resulted in improved physical health and mood. Moreover, Rolland and colleagues (2007) conducted an RCT and found similar results as Teri et al. (2003). It was demonstrated that 1 h a day of exercise for individuals with Alzheimer’s disease resulted in a decrease in rates of decline in ADLs .
There has been a growing amount of research addressing mindfulness to improve and promote health and wellness in the medical setting. Mindfulness-based stress reduction (MBSR) is a protocol-based intervention that has been shown in numerous RCTs to be effective in reducing chronic pain (Hilton et al., 2017), cancer (Rush & Sharma, 2016), fibromyalgia (Lauche, Cramer, Dobos, Langhorst, & Schmidt, 2013), vascular disease (Abbott et al., 2014), HIV/AIDS (Riley & Kalichman, 2015), and depression (Gu, Strauss, Bond, & Cavanagh, 2015). An examination of the literature found that studies have used MBSR with older adults. Paller and colleagues (2015) conducted a unique study that evaluated the MBSR protocol in both individuals with dementia and their caregivers. This was a small prospective study (n = 17 patients; n = 20 caregivers) that found significant improvements in caregivers and individuals with dementia’s QoL and depression from pre- to posttest (p < 0.05). Moreover, the caregivers’ distress improved significantly from pre- to posttest (p < 0.05). To our knowledge, this pilot study was the first study that has demonstrated that MBSR can have a positive effect on both the caregiver and the individual with a neurocognitive disorder. This is important as studies have found that caregiver’s distress and mood can have an effect on the individual with the neurocognitive disorder (Thomas et al., 2006; Wetzels, Zuidema, De Jonghe, Verhey, & Koopmans, 2010).
Promoting the health and wellness of individuals with neurocognitive disorder should be a priority. As pharmaceutical interventions have been shown to have little effect and may cause a decrease health and wellness in individuals with neurocognitive impairment, a non-pharmaceutical approach is warranted. The studies above illustrate the positive effects of non-pharmaceutical interventions, including behavioral activation, exercise, and MBSR.
Promote Family Members/Caregiver QoL and Neurocognitive Education
Family members and/or caregivers for individuals with neurocognitive disorders play an intricate role in the care of these individuals as this disorder can cause severe disability (Gallagher-Thompson et al., 2012). It is estimated that 14.9 million people in the United States currently care for someone who has some form of dementia (Alliance, 2012). There are negative effects that have been associated with being a caregiver of an individual with a neurocognitive disorder, including increases in depression, anxiety, family conflict, social isolation, and role captivity (Judge, Yarry, Looman, & Bass, 2013; Molinari, 2006). These negative effects can create a strain on the caregiver-care receipt relationship and negatively affect the health of the care recipient. Numerous studies have evaluated different interventions designed to promote the behavioral health and quality of life of caregivers of individuals with neurocognitive disorder (see Judge et al., 2013; Schultz et al., 2003). The Resources for Enhancing Alzheimer’s Caregiver Health (REACH; Schultz et al., 2003) clinical trial and the Acquiring New Skills While Enhancing Remaining Strengths (ANSWERS; Judge et al., 2013) both investigated interventions for caregivers of individuals with Alzheimer’s disease . The trials of the interventions were rooted from a cognitive behavioral approach to psychoeducation and support of individuals with Alzheimer’s disease .
The REACH trial , a multicentered (six sites) trial, aimed to evaluate the effectiveness of social and behavioral interventions for caregivers of individuals with Alzheimer’s disease and other memory disorders (Schultz et al., 2003). The interventions that were utilized included individual information and support strategies, group support and family systems therapy, psychoeducational and skill-based training approaches, home-based environmental interventions, and enhanced technology support symptoms. These interventions were hypothesized to decrease grief and depression symptoms. All of the interventions yielded a statistically significant effect on normal grief symptoms. When examining the intervention components, cognitive and behavioral strategies were found to be most effective at reducing levels of complicated grief. Information and emotional support were most effective for addressing normal grief, and environmental modifications were most effective for ameliorating depressive symptoms (Holland, Currier, & Gallagher-Thompson, 2009). The results illustrate that a multitude of interventions may be warranted, based on the caregiver’s clinical repertoire and the care recipient’s risk factors.
The ANSWERS trial investigated interventions including education about dementia and memory loss, effective communication, managing memory, staying active, and recognizing emotions and behaviors for family caregivers of individuals with dementia. Interventions aimed at alleviating and reducing caregivers’ negative outcomes included educational and skill-based interventions, heightening caregiving efficacy, and reducing strain for family caregivers (Judge et al., 2013). The researchers found that the interventions were efficacious in improving key strain and psychosocial outcomes for caregivers. It should be noted that a strength-based approach was utilized when developing and implementing care goals, as well as educating the caregivers about neurocognitive disorders.
These two trials have set the groundwork for interventions in promoting family member’s/caregiver’s health and QoL . These trials investigated different interventions and demonstrated that non-pharmaceutical interventions (e.g., neurocognitive education, group support, family systems therapy, psychoeducational interventions) are efficacious in positively affecting the caregiver-care recipient relationship and improving QoL. More importantly, these positive effects were found with little to no side effects.
References
Abbott, R. A., Whear, R., Rodgers, L. R., Bethel, A., Coon, J. T., Kuyken, W., … Dickens, C. (2014). Effectiveness of mindfulness-based stress reduction and mindfulness based cognitive therapy in vascular disease: A systematic review and meta-analysis of randomised controlled trials. Journal of Psychosomatic Research, 76(5), 341–351.
Abizanda, P., Romero, L., Sanchez-Jurado, P. M., Martinez-Reig, M., Alfonso-Silguero, S. A., & Rodriguez-Manas, L. (2014). Age, frailty, disability, institutionalization, multimorbidity or comorbidity. Which are the main targets in older adults? The Journal of Nutrition, Health & Aging, 18(6), 622.
Achterberg, W. P., Pieper, M. J., van Dalen-Kok, A. H., De Waal, M. W., Husebø, B., Lautenbacher, S., … Corbett, A. (2013). Pain management in patients with dementia. Clinical Interventions in Aging, 8, 1471–1482.
Alexopoulos, G. S. (2005). Depression in the elderly. The Lancet, 365(9475), 1961–1970.
Alliance, F. C. (2012). Fact sheet: Selected caregiver statistics. San Francisco, CA: Family Caregiver Alliance.
American Psychological Association. (2017). Integrated Health Care. Retrieved from http://www.apa.org/health/integrated-health-care.aspx
Andreassi, J. L. (2013). Psychophysiology: Human behavior & physiological response. Mahwah, NJ: Lawrence Erlbaum Associates, Inc.
Baert, V., Gorus, E., Mets, T., Geerts, C., & Bautmans, I. (2011). Motivators and barriers for physical activity in the oldest old: A systematic review. Ageing Research Reviews, 10(4), 464–474.
Ballard, C., Hanney, M. L., Theodoulou, M., Douglas, S., McShane, R., Kossakowski, K., … Jacoby, R. (2009). The dementia antipsychotic withdrawal trial (DART-AD): Long-term follow-up of a randomised placebo-controlled trial. The Lancet Neurology, 8(2), 151–157.
Ballard, C., Smith, J., Corbett, A., Husebo, B., & Aarsland, D. (2011). The role of pain treatment in managing the behavioural and psychological symptoms of dementia (BPSD). International Journal of Palliative Nursing, 17(9), 420–424.
Bandurska, E., Damps-Konstanska, I., Popowski, P., Jedrzejczyk, T., Janowiak, P., Swietnicka, K., … Jassem, E. (2017). Impact of Integrated Care Model (ICM) on Direct Medical Costs in Management of Advanced Chronic Obstructive Pulmonary Disease (COPD). Medical Science Monitor, 23, 2850–2862.
Barker, W. W., Luis, C. A., Kashuba, A., Luis, M., Harwood, D. G., Loewenstein, D., … Graff-Radford, N. (2002). Relative frequencies of Alzheimer disease, Lewy body, vascular and frontotemporal dementia, and hippocampal sclerosis in the state of Florida brain Bank. Alzheimer Disease & Associated Disorders, 16(4), 203–212.
Bauman, A., Merom, D., Bull, F. C., Buchner, D. M., & Fiatarone Singh, M. A. (2016). Updating the evidence for physical activity: Summative reviews of the epidemiological evidence, prevalence, and interventions to promote “active aging”. The Gerontologist, 56(Suppl_2), S268–S280.
Beach, T. G., Monsell, S. E., Phillips, L. E., & Kukull, W. (2012). Accuracy of the clinical diagnosis of Alzheimer disease at National Institute on Aging Alzheimer disease centers, 2005–2010. Journal of Neuropathology & Experimental Neurology, 71(4), 266–273.
Beerens, H. C., Sutcliffe, C., Renom-Guiteras, A., Soto, M. E., Suhonen, R., Zabalegui, A., … RightTimePlaceCare Consortium. (2014). Quality of life and quality of care for people with dementia receiving long term institutional care or professional home care: The European RightTimePlaceCare study. Journal of the American Medical Directors Association, 15(1), 54–61.
Beerens, H. C., Zwakhalen, S. M., Verbeek, H., Ruwaard, D., & Hamers, J. P. (2013). Factors associated with quality of life of people with dementia in long-term care facilities: A systematic review. International Journal of Nursing Studies, 50(9), 1259–1270.
Bond, M., Rogers, G., Peters, J., Anderson, R., Hoyle, M., Miners, A., … Jeffreys, M. (2012). The effectiveness and cost-effectiveness of donepezil, galantamine, rivastigmine and memantine for the treatment of Alzheimer’s disease (review of technology appraisal no. 111): A systematic review and economic model. Health Technology Assessment (Winchester, England), 16(21), 1–470.
Boustani, M., Peterson, B., Hanson, L., Harris, R., & Lohr, K. N. (2003). Screening for dementia in primary care: A summary of the evidence for the US preventive services task force. Annals of Internal Medicine, 138(11), 927–937.
Bowling, A. (2001). Measuring disease. In A review of disease-specific quality of life measurement scales. Buckingham, UK: Open University Press.
Bowling, A., Rowe, G., Adams, S., Sands, P., Samsi, K., Crane, M., … Manthorpe, J. (2015). Quality of life in dementia: A systematically conducted narrative review of dementia-specific measurement scales. Aging & Mental Health, 19(1), 13–31.
Brown, L. G. (2016). Untangling polypharmacy in older adults. Medsurg Nursing, 25(6), 408–412.
Brown, R. C., Lockwood, A. H., & Sonawane, B. R. (2005). Neurodegenerative diseases: An overview of environmental risk factors. Environmental Health Perspectives, 113(9), 1250–1256.
Buchanan, J. A., Christenson, A., Houlihan, D., & Ostrom, C. (2011). The role of behavior analysis in the rehabilitation of persons with dementia. Behavior Therapy, 42(1), 9–21.
Campanelli, C. M. (2012). American Geriatrics Society updated beers criteria for potentially inappropriate medication use in older adults: The American Geriatrics Society 2012 beers criteria update expert panel. Journal of the American Geriatrics Society, 60(4), 616.
Catania, A. C. (1996). On the origins of behavior structure. Advances in Psychology, 117, 3–12.
Centers for Medicare & Medicaid Services. (2013). Atypical Antipsychotic Medications: Use in Adults. Retrieved from https://www.cms.gov/medicaremedicaid-coordination/fraud-prevention/medicaid-integrity-education/pharmacy-education-materials/downloads/atyp-antipsych-adult-factsheet.pdf
Chapman, D. P., Williams, S. M., Strine, T. W., Anda, R. F., & Moore, M. J. (2006). Dementia and its implications for public health. Preventing Chronic Disease, 3(2), A34.
Chiu, Y., Bero, L., Hessol, N. A., Lexchin, J., & Harrington, C. (2015). A literature review of clinical outcomes associated with antipsychotic medication use in north American nursing home residents. Health Policy, 119(6), 802–813.
Clague, F., Mercer, S. W., McLean, G., Reynish, E., & Guthrie, B. (2016). Comorbidity and polypharmacy in people with dementia: Insights from a large, population-based cross-sectional analysis of primary care data. Age and Ageing, 46(1), 33–39.
Dawson, P., Wells, D. L., & Kline, K. (1993). Enhancing the abilities of persons with Alzheimer’s and related dementias: A nursing perspective. New York, NY: Springer Publishing Company.
Di Santo, S. G., Prinelli, F., Adorni, F., Caltagirone, C., & Musicco, M. (2013). A meta-analysis of the efficacy of donepezil, rivastigmine, galantamine, and memantine in relation to severity of Alzheimer’s disease. Journal of Alzheimer’s Disease, 35(2), 349–361.
Doody, R. S., Stevens, J. C., Beck, C., Dubinsky, R. M., Kaye, J. A., Gwyther, L. M. S. W., … Cummings, J. L. (2001). Practice parameter: Management of dementia (an evidence-based review) report of the quality standards Subcommittee of the American Academy of neurology. Neurology, 56(9), 1154–1166.
Dramé, M., Fierobe, F., Lang, P. O., Jolly, D., Boyer, F., Mahmoudi, R., … Voisin, T. (2011). Predictors of institution admission in the year following acute hospitalisation of elderly people. The Journal of Nutrition. Health & Aging, 15(5), 399–403.
Enns, E., Rhemtulla, R., Ewa, V., Fruetel, K., & Holroyd-Leduc, J. M. (2014). A controlled quality improvement trial to reduce the use of physical restraints in older hospitalized adults. Journal of the American Geriatrics Society, 62(3), 541–545.
Fauth, E. B., & Gibbons, A. (2014). Which behavioral and psychological symptoms of dementia are the most problematic? Variability by prevalence, intensity, distress ratings, and associations with caregiver depressive symptoms. International Journal of Geriatric Psychiatry, 29(3), 263–271.
Fisher, J. E., Drossel, C., Yury, C., & Cherup, S. (2007). A contextual model of restraint–free care for persons with dementia. In P. Sturmey (Ed.), Functional analysis in clinical treatment (pp. 211–238). San Diego, CA: Elsevier.
Fleming, R., Goodenough, B., Low, L. F., Chenoweth, L., & Brodaty, H. (2016). The relationship between the quality of the built environment and the quality of life of people with dementia in residential care. Dementia, 15(4), 663–680.
Gallagher-Thompson, D., Tzuang, Y. M., Au, A., Brodaty, H., Charlesworth, G., Gupta, R., … Shyu, Y. I. (2012). International perspectives on nonpharmacological best practices for dementia family caregivers: A review. Clinical Gerontologist, 35(4), 316–355.
Galvin, J. E., & Sadowsky, C. H. (2012). Practical guidelines for the recognition and diagnosis of dementia. The Journal of the American Board of Family Medicine, 25(3), 367–382.
Garrison-Diehn, C., Rummel, C., & Fisher, J. E. (2013). A contextual approach to dementia Care in Alzheimer’s disease. In Case studies in clinical psychological science: Bridging the gap from science to practice (p. 279). Oxford, NY: Oxford University Press.
Geldmacher, D. S. (2003). Alzheimer’s disease: Current pharmacotherapy in the context of patient and family needs. Journal of the American Geriatrics Society, 51(5s2), S289–S295.
Gitlin, L. N., Kales, H. C., & Lyketsos, C. G. (2012). Nonpharmacologic management of behavioral symptoms in dementia. JAMA, 308(19), 2020–2029.
Gitlin, L. N., Winter, L., Dennis, M. P., Hodgson, N., & Hauck, W. W. (2010). A biobehavioral home-based intervention and the Well-being of patients with dementia and their caregivers: The COPE randomized trial. JAMA, 304(9), 983–991.
Gnjidic, D., Hilmer, S. N., Blyth, F. M., Naganathan, V., Waite, L., Seibel, M. J., … Le Couteur, D. G. (2012). Polypharmacy cutoff and outcomes: Five or more medicines were used to identify community-dwelling older men at risk of different adverse outcomes. Journal of Clinical Epidemiology, 65(9), 989–995.
Goodarzi, Z. S., Mele, B. S., Roberts, D. J., & Holroyd-Leduc, J. (2017). Depression case finding in individuals with dementia: A systematic review and meta-analysis. Journal of the American Geriatrics Society., 65(5), 937.
Gu, J., Strauss, C., Bond, R., & Cavanagh, K. (2015). How do mindfulness-based cognitive therapy and mindfulness-based stress reduction improve mental health and wellbeing? A systematic review and meta-analysis of mediation studies. Clinical Psychology Review, 37, 1–12.
Hebert, L. E., Weuve, J., Scherr, P. A., & Evans, D. A. (2013). Alzheimer disease in the United States (2010–2050) estimated using the 2010 census. Neurology, 80(19), 1778–1783.
Hilton, L., Hempel, S., Ewing, B. A., Apaydin, E., Xenakis, L., Newberry, S., … Maglione, M. A. (2017). Mindfulness meditation for chronic pain: Systematic review and meta-analysis. Annals of Behavioral Medicine, 51(2), 199–213.
Holland, J. M., Currier, J. M., & Gallagher-Thompson, D. (2009). Outcomes from the resources for enhancing Alzheimer’s caregiver health (REACH) program for bereaved caregivers. Psychology and Aging, 24(1), 190.
Hovstadius, B., & Petersson, G. (2012). Factors leading to excessive polypharmacy. Clinics in Geriatric Medicine, 29(2), 159–172.
Husebo, B. S., Strand, L. I., Moe-Nilssen, R., BorgeHusebo, S., Aarsland, D., & Ljunggren, A. E. (2008). Who suffers most? Dementia and pain in nursing home patients: A cross-sectional study. Journal of the American Medical Directors Association, 9(6), 427–433.
Jellinger, K. A., & Attems, J. (2011). Prevalence and pathology of dementia with Lewy bodies in the oldest old: A comparison with other dementing disorders. Dementia and Geriatric Cognitive Disorders, 31(4), 309–316.
Judge, K. S., Yarry, S. J., Looman, W. J., & Bass, D. M. (2013). Improved strain and psychosocial outcomes for caregivers of individuals with dementia: Findings from project ANSWERS. The Gerontologist, 53(2), 280–292.
Kales, H. C., Gitlin, L. N., & Lyketsos, C. G. (2015). State of the art review: Assessment and management of behavioral and psychological symptoms of dementia. The BMJ, 350, h369.
Kim, D. H., Brown, R. T., Ding, E. L., Kiel, D. P., & Berry, S. D. (2011). Dementia medications and risk of falls, syncope, and related adverse events: Meta-analysis of randomized controlled trials. Journal of the American Geriatrics Society, 59(6), 1019–1031.
Knapskog, A. B., Barca, M. L., & Engedal, K. (2014). Prevalence of depression among memory clinic patients as measured by the Cornell scale of depression in dementia. Aging & Mental Health, 18(5), 579–587.
Lambert, M. A., Bickel, H., Prince, M., Fratiglioni, L., Von Strauss, E., Frydecka, D., … Reynish, E. L. (2014). Estimating the burden of early onset dementia; systematic review of disease prevalence. European Journal of Neurology, 21(4), 563–569.
Lauche, R., Cramer, H., Dobos, G., Langhorst, J., & Schmidt, S. (2013). A systematic review and meta-analysis of mindfulness-based stress reduction for the fibromyalgia syndrome. Journal of Psychosomatic Research, 75(6), 500–510.
LoGiudice, D., & Watson, R. (2014). Dementia in older people: An update. Internal Medicine Journal, 44(11), 1066–1073.
Looman, W. M., Huijsman, R., Bouwmans-Frijters, C. A., Stolk, E. A., & Fabbricotti, I. N. (2016). Cost-effectiveness of the ‘Walcheren integrated care Model’intervention for community-dwelling frail elderly. Family Practice, 33(2), 154–160.
Lopez, O. L., Becker, J. T., Wahed, A. S., Saxton, J., Sweet, R. A., Wolk, D. A., … Dekosky, S. T. (2009). Long-term effects of the concomitant use of memantine with cholinesterase inhibition in Alzheimer disease. Journal of Neurology, Neurosurgery & Psychiatry, 80(6), 600–607.
Lwi, S. J., Ford, B. Q., Casey, J. J., Miller, B. L., & Levenson, R. W. (2017). Poor caregiver mental health predicts mortalilty of patients with neurodegenerative disease. Proceedings of the National Academy of Science, 201701597. https://doi.org/10.1073/pnas.1701597114
Marcum, Z. A., Driessen, J., Thorpe, C. T., Gellad, W. F., & Donohue, J. M. (2014). Effect of multiple pharmacy use on medication adherence and drug–drug interactions in older adults with Medicare part D. Journal of the American Geriatrics Society, 62(2), 244–252.
Maust, D. T., Kim, H. M., Seyfried, L. S., Chiang, C., Kavanagh, J., Schneider, L. S., & Kales, H. C. (2015). Antipsychotics, other psychotropics, and the risk of death in patients with dementia: Number needed to harm. JAMA Psychiatry, 72(5), 438–445.
McKhann, G. M., Albert, M. S., & Sperling, R. A. (2012). Changing diagnostic concepts of Alzheimer’s disease. In Alzheimer’s Disease-Modernizing Concept, Biological Diagnosis and Therapy, 28, 115–121 Karger Publishers.
McKhann, G. M., Knopman, D. S., Chertkow, H., Hyman, B. T., Jack, C. R., Kawas, C. H., … Mohs, R. C. (2011). The diagnosis of dementia due to Alzheimer’s disease: Recommendations from the National Institute on Aging-Alzheimer’s association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimer’s & Dementia, 7(3), 263–269.
Molinari, V., Chiriboga, D., Branch, L. G., Cho, S., Turner, K., Guo, J., & Hyer, K. (2010). Provision of psychopharmacological services in nursing homes. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 65(1), 57–60.
Molinari, V. A. (2006). Caregiver burden. In S. M. Lobo Prabhu, V. A. Molinari, & J. W. Lomax (Eds.), Supporting the caregiver in dementia: A guide for health care professionals (pp. 64–81). Baltimore, MD: The Johns Hopkins University Press.
Moss, K., Scogin, F., Di Napoli, E., & Presnell, A. (2012). A self-help behavioral activation treatment for geriatric depressive symptoms. Aging & Mental Health, 16(5), 625–635.
Neufeld, R. R., Libow, L. S., Foley, W. J., Dunbar, J. M., Cohen, C., & Breuer, B. (1999). Restraint reduction reduces serious injuries among nursing home residents. Journal of the American Geriatrics Society, 47(10), 1202–1207.
Norgaard, A., Jensen-Dahm, C., Gasse, C., Hansen, E. S., & Waldemar, G. (2017). Psychotropic polypharmacy in patients with dementia: Prevalence and predictors. Journal of Alzheimer’s Disease, 56(2), 707–716.
Odenheimer, G., Borson, S., Sanders, A. E., Swain-Eng, R. J., Kyomen, H. H., Tierney, S., … Johnson, J. (2013). Quality improvement in neurology dementia management quality measures. Neurology, 81(17), 1545–1549.
Paller, K. A., Creery, J. D., Florczak, S. M., Weintraub, S., Mesulam, M. M., Reber, P. J., ... O’Hara, M. (2015). Benefits of mindfulness training for patients with progressive cognitive decline and their caregivers. American Journal of Alzheimer’s Disease & Other Dementias®, 30(3), 257–267.
Paterson, R. W., Takada, L. T., & Geschwind, M. D. (2012). Diagnosis and treatment of rapidly progressive dementias. Neurology: Clinical Practice, 2(3), 187–200.
Prince, M., Bryce, R., Albanese, E., Wimo, A., Ribeiro, W., & Ferri, C. P. (2013). The global prevalence of dementia: A systematic review and metaanalysis. Alzheimer’s & Dementia, 9(1), 63–75.
Prince, M., Comas-Herrera, A., Knapp, M., Guerchet, M., & Karagiannidou, M. (2016). World Alzheimer report 2016: Improving healthcare for people living with dementia: Coverage, quality and costs now and in the future. London, UK: Alzheimer’s Disease International (ADI).
Rahman, S. (2017). Enhancing health and wellbeing in dementia: A person-centered integrated care approach. London, UK: Jessica Kingsley Publishers.
Riley, K. E., & Kalichman, S. (2015). Mindfulness-based stress reduction for people living with HIV/AIDS: Preliminary review of intervention trial methodologies and findings. Health Psychology Review, 9(2), 224–243.
Rizzi, L., Rosset, I., & Roriz-Cruz, M. (2014). Global epidemiology of dementia: Alzheimer’s and vascular types. BioMed Research International, 2014, 8.
Rolland, Y., Pillard, F., Klapouszczak, A., Reynish, E., Thomas, D., Andrieu, S., … Vellas, B. (2007). Exercise program for nursing home residents with Alzheimer’s disease: A 1-year randomized, controlled trial. Journal of the American Geriatrics Society, 55(2), 158–165.
Rush, S. E., & Sharma, M. (2016). Mindfulness-based stress reduction as a stress management intervention for cancer care: A systematic review. Journal of Evidence-Based Complementary & Alternative Medicine., 2156587216661467, 22(2), 348–360.
Schneider, L. S., Dagerman, K. S., & Insel, P. (2005). Risk of death with atypical antipsychotic drug treatment for dementia: Meta-analysis of randomized placebo-controlled trials. JAMA, 294(15), 1934–1943.
Schultz, R., Belle, S. H., Czaja, S. J., Gitlin, L. N., Wisniewski, S. R., & Ory, M. G. (2003). Introduction to the special section on resources for enhancing Alzheimer’s caregiver health (REACH). Psychology and Aging, 18(3), 357.
Snarski, M., Scogin, F., DiNapoli, E., Presnell, A., McAlpine, J., & Marcinak, J. (2011). The effects of behavioral activation therapy with inpatient geriatric psychiatry patients. Behavior Therapy, 42(1), 100–108.
Snowden, M. B., Atkins, D. C., Steinman, L. E., Bell, J. F., Bryant, L. L., Copeland, C., & Fitzpatrick, A. L. (2015). Longitudinal association of dementia and depression. The American Journal of Geriatric Psychiatry, 23(9), 897–905.
Tampi, R. R., Tampi, D. J., Balachandran, S., & Srinivasan, S. (2016). Antipsychotic use in dementia: A systematic review of benefits and risks from meta-analyses. Therapeutic Advances in Chronic Disease, 7(5), 229–245.
Tan, C. C., Yu, J. T., Wang, H. F., Tan, M. S., Meng, X. F., Wang, C., … Tan, L. (2014). Efficacy and safety of donepezil, galantamine, rivastigmine, and memantine for the treatment of Alzheimer’s disease: A systematic review and meta-analysis. Journal of Alzheimer’s Disease, 41(2), 615–631.
Teri, L., Gibbons, L. E., McCurry, S. M., Logsdon, R. G., Buchner, D. M., Barlow, W. E., … Larson, E. B. (2003). Exercise plus behavioral management in patients with Alzheimer disease: A randomized controlled trial. JAMA, 290(15), 2015–2022.
Thomas, P., Lalloué, F., Preux, P. M., Hazif-Thomas, C., Pariel, S., Inscale, R., … Clément, J. P. (2006). Dementia patients caregivers quality of life: The PIXEL study. International Journal of Geriatric Psychiatry, 21(1), 50–56.
United States Department of Health and Human Services. (2005). Glossary: Definition of restraints. Retrieved from http://www.medicare.gov/Glossary/ShownTerm.asp?Languge=English&term=restraints
U.S. Food and Drug Administration. (2008). Information for Health Care Professionals: Conventional Antipsychotics. Retrieved from https://wayback.archiveit.org/7993/20170722190727/. https://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/ucm124830.htm
van der Spek, K., Gerritsen, D. L., Smalbrugge, M., Nelissen-Vrancken, M. H., Wetzels, R. B., Smeets, C. H., … Koopmans, R. T. (2016). Only 10% of the psychotropic drug use for neuropsychiatric symptoms in patients with dementia is fully appropriate. The PROPER I-study. International Psychogeriatrics, 28(10), 1589–1595.
Van Duijn, C. M., Clayton, D. G., Chandra, V., Fratiglioni, L., Graves, A. B., Heyman, A., … Rocca, W. A. (1994). Interaction between genetic and environmental risk factors for Alzheimer’s disease: A reanalysis of case-control studies. Genetic Epidemiology, 11(6), 539–551.
van Hout, H. P., Vernooij-Dassen, M. J., & Stalman, W. A. (2007). Diagnosing dementia with confidence by GPs. Family Practice, 24(6), 616–621.
Vance, D. E., & Struzick, T. C. (2007). Addressing risk factors of cognitive impairment in adults aging with HIV: A social work model. Journal of Gerontological Social Work, 49(4), 51–77.
Vasudev, A., Shariff, S. Z., Liu, K., Burhan, A. M., Herrmann, N., Leonard, S., & Mamdani, M. (2015). Trends in psychotropic dispensing among older adults with dementia living in long-term care facilities: 2004–2013. The American Journal of Geriatric Psychiatry, 23(12), 1259–1269.
Villars, H., Oustric, S., Andrieu, S., Baeyens, J. P., Bernabei, R., Brodaty, H., … Frisoni, G. (2010). The primary care physician and Alzheimer’s disease: An international position paper. The Journal of Nutrition, Health & Aging, 14(2), 110–120.
Wang, J., Yu, J. T., Wang, H. F., Meng, X. F., Wang, C., Tan, C. C., & Tan, L. (2014). Pharmacological treatment of neuropsychiatric symptoms in Alzheimer’s disease: A systematic review and meta-analysis. Journal of Neurology, Neurosurgery & Psychiatry, 86(1), 101–109 jnnp-2014.
Wetzels, R. B., Zuidema, S. U., De Jonghe, J. F. M., Verhey, F. R. J., & Koopmans, R. T. C. M. (2010). Determinants of quality of life in nursing home residents with dementia. Dementia and Geriatric Cognitive Disorders, 29(3), 189–197.
World Health Organization. (1997). Measuring quality of life. In Division of mental health and prevention of substance abuse. Geneva, Switzerland: World Health Organization.
Yon, A., & Scogin, F. (2008). Behavioral activation as a treatment for geriatric depression. Clinical Gerontologist, 32(1), 91–103.
Yury, C. A., & Fisher, J. E. (2007). Meta-analysis of the effectiveness of atypical antipsychotics for the treatment of behavioural problems in persons with dementia. Psychotherapy and Psychosomatics, 76(4), 213–218.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Singer, J., Chong, A., Hisaka, R., Fisher, J.E. (2018). Promoting the Behavioral Health of Persons with Neurocognitive Disorders. In: Duckworth, M., O'Donohue, W. (eds) Behavioral Medicine and Integrated Care. Springer, Cham. https://doi.org/10.1007/978-3-319-93003-9_16
Download citation
DOI: https://doi.org/10.1007/978-3-319-93003-9_16
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-93002-2
Online ISBN: 978-3-319-93003-9
eBook Packages: Behavioral Science and PsychologyBehavioral Science and Psychology (R0)