Abstract
Hypertension is the result of multiple pathophysiological mechanisms influenced by diverse environmental and genetic parameters Regarding dietary parameters increased sodium intake, inadequate potassium consumption and alcohol play a key role for the pathogenesis and evolution of the hypertensive phenotype. Excess weight usually accompanied by lack of physical activity that characterizes modern lifestyle further contribute to blood pressure (BP) increase. Therefore, lifestyle and dietary interventions are important clinically in order to reduce BP and overall cardiovascular risk. Adoption of the DASH and the Mediterranean diets is related to reduction of BP independently of other lifestyle changes.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Body weight increase is closely related to blood pressure (BP) levels augmentation in almost a linear fashion [1], augmenting overall cardiovascular risk [2]. More specifically in the Framingham Heart Study, data regarding 45.000 subjects during a follow-up of 44 years showed that overweight and obese men had a 48% and 123% higher risk of developing hypertension compared to normal weight individuals. In the same manner, overweight and obese women compered to normal weight ones had a 70% and 175% higher risk for developing hypertension [3].
The important INTERSALT study performed in 10.074 adults 20–59 years old in 32 countries worldwide showed that an intake of more than 2.3 gr/day is linked with increased BP by 6 mmHg and diastolic by 2.5 mmHg [4]. In another cross-sectional work including more than 100,000 subjects from 18 countries it was found that for an increase of consumption of salt by 1 gr/day the systolic BP augments by 2.6 mmHg and diastolic BP by 1.8 mmHg [5]. Thus, the higher the intake of salt the higher by 25% the probability of being hypertensive as shown in a prospective study of 4500 normotensives [6, 7].
There is an inverse correlation between consumption of potassium and hypertension [6, 7]. In the NHANES study 1gr/day higher potassium was associated with lower systolic BP by 1.2 mmHg [8], while in another population the higher quartile of sodium/potassium ratio (7.9–9.7) had more increased systolic and diastolic BP by 8 mmHg and 7 mmHg, respectively compared to those in the lower quartile of sodium/potassium ratio (2.1–2.3) [9]. In this sense low consumption of potassium leads to hypertension [7] and more specifically this risk augments by 20% in the subjects with less than 2600 mg urine excretion for males and less than 2200 mg for females [10].
Although moderate alcohol intake compared to full abstinence is associated with higher HDL cholesterol levels and decreased risk for cardiovascular events, the correlation with BP is positive leading to higher hemodynamic load [11]. For each 10 gr of alcohol BP rises for approximately 11 mmHg and the latter is reversed after 2–4 weeks when no or minimal consumption is present [12]. In a randomized clinical study of 44 treated hypertensive men moderate compared to low alcohol consumption was linked to higher BP by 5 mmHg for systolic and 3 mmHg for the diastolic component [13]. Additionally a 45% increased risk for the development of hypertension is observed in normotensives who consumed more than 1 drink for more than 5 days per week compared to no alcohol [14].
Dietary Interventions for BP Lowering
Lifestyle changes are the pillars for both prevention and management of hypertension [15, 16]. In the PREMIER study, that was a randomized clinical study in 810 subjects >25 years old with systolic BP ranging 120–159 mmHg and diastolic BP 80–95 mmHg, on no antihypertensive medication, it was shown that after 6 months the behavioral intervention alone or with the adoption of the DASH diet lowered systolic BP by 3.7 mmHg and 4.3 mmHg, while diastolic BP was decreased by 1.7 mmHg and 2.6 mmHg respectively. The 18 months results concluded that the combination of the DASH diet with behavioral alterations compared to the latter alone are linked to 23% less possibilities for hypertension [17].
The current guidelines suggest for subjects with high normal BP to prevent the development of hypertension and for the hypertensive individuals with ow cardiovascular risk and no target organ damage to base their management on lifestyle/dietary interventions, whereas in those who drug therapy is initiated it should be always accompanied by non-pharmacological management [18]. In the innovative American guidelines for hypertension, subjects of low cardiovascular risk with hypertension grade1 should follow a healthy lifestyle without any medication taken [19]. The proposed in the guidelines dietary interventions are weight loss, decrease in sodium intake, increase in potassium consumption, reduction of alcohol and the adoption of a healthy dietary pattern like the DASH or the Mediterranean diet [18, 19].
Weight Loss and BP Control
Losing excess weight is directly related to BP levels reduction 38, 39, 40. In a meta-analysis of 25 randomized trials a weight loss of 5.1 kgr reduces systolic and diastolic BP by 4.4 mmHg and 3.6 mmHg respectively. The higher the decrease in weight the higher is the reduction of BP with 1 mmHg corresponding to the loss of approximately 1 kgr [20]. TOHP study was one of the largest randomized studies for the investigation of the effects of weight reduction on BP levels. In the weight reduction group with intense education the lost weight after 6 months was 4.4 kgr, in 18 months 2 kgr and after 3 years only 0.2 kgr, underscoring the difficulty in maintaining the positive results.
[21]. Compared to the control group in the abovementioned timepoints of the study systolic/diastolic BP was lowered by 3.7/2.7 mmHg, 1.8/1.3 mmHg and 1.3/0.9 mmHg [22]. After 7 years there was no difference in body weight but the risk of developing hypertension was 77% less in the intervention group [23].
The short-term effects of weight reduction on BP are rather beneficial, however there is a problem with the long-term results since 50% of subjects gain their initial weight before any intervention after a mean period of 3 years and this causes an increase in BP 45–47. In patients with morbid obesity drugs and bariatric surgery are therapeutic solutions although the impact on BP remain controversial [24, 25].
Sodium and BP Control
The reduction of salt to 2.300 mg per day is one of the most important dietary interventions for maintaining normal BP [18, 26, 27]. There are many randomized well-designed studies showing the beneficial effects of reducing dietary salt [7, 28,29,30,31,32,33,34,35,36,37,38]. In a recent meta-analysis reduction of salt intake from 4.500 mg to 1.500 mg per day decreases systolic BP by 1 mmHg, with no effects on diastolic BP in normotensives, whereas in hypertensive individuals the same salt restriction results in lower systolic/diastolic BP by 5.5/2.9 mmHg [39]. In these lines data from the ΤΟHP study reveal that restriction of sodium was lower than 1.150 mg per day for the 6 months of follow-up and 920 mg per day for 3 years compared to controls leading to lower BP [22]. In treated hypertensives the TONE study investigated the effects of weight reduction and sodium restriction <1.8 gr/day on BP levels. The combination of salt and weight decrease was accompanied by attenuated systolic BP of 5.3 mmHg and diastolic of 3.4 mmHg compared to controls [40]. Regarding cross-sectional studies excretion of sodium in the urine is closely associated with both the BP levels as well as the hypertension risk [41]. The INTERMAP study showed that in 4.680 adults 40–59 years showed that in China and Japan the sodium/potassium ratio was higher (6.0–6.8) in China and compared to Great Britain and America (2.2–3.1) and BP levels were higher in the Eastern compared to Western countries [42].
One of the most important trials on the way salt affects BP is the double-blind randomized trial of modest salt restriction in older people by Cappucio F et al., published more than 2 decades ago [43]. This crossover trial was conducted to examine the effect on BP of a modest reduction in salt intake from 10 g to 5 g per day in both hypertensive and normotensive individuals. The study was conducted in 47 older adults, aged 60 years or more, with systolic BP <210 mmHg and diastolic BP <115 mmHg on no drugs. For 2 weeks participants were told to reduce their salt intake to about 5 g (80 mmoles sodium) daily. Participants achieved this reduction by not adding salt at the table or in cooking, and by avoiding foods that contain large amounts of salt. After the 2 weeks of reduced sodium intake, participants were allocated in random order to take 12 Slow Sodium tablets daily (10 mmoles sodium per tablet) or 12 Slow Sodium matching placebo tablets daily. After 1 month, measurements were repeated, and participants crossed over to the opposite treatment for a further month. It should be noted that energy restriction was not suggested and an average reduction in sodium intake of 80 mmol/day (about 5 g salt) was associated with a reduction in both systolic BP and diastolic BP of 7.2 mmHg and 3.2 mmHg, respectively. There was no significant difference in the BP fall between 18 normotensives and 29 hypertensive participants (8.2/3.97 mmHg vs 6.6/2.7 mmHg) [43].
Based on the abovementioned results one could suggest that the fall of BP in this study is similar to that in the controlled-outcome trials of drug therapy in older hypertensive people for example with the use of thiazide diuretics. Additionally, a modest reduction in sodium intake is feasible and can be achieved over a long period, provided salt is not added to food or in cooking, and highly salted processed foods are avoided.
Two of the most recent meta-analyses of randomized, controlled clinical trials that have been performed in adults investigating the magnitude of the effect of salt reduction on BP found that the salt restriction has significant beneficial effects. Specifically, Graudal et al. found that a mean reduction of salt intake from 11.5 g to 3.8 g per day reduces significantly systolic BP by 5.5 mmHg and diastolic BP by 2.9 mmHg in people with hypertension, while in people without hypertension has very little or no effect [39]. He FJ et al. found that a mean reduction of salt intake of 4.4 g per day in people with hypertension reduces significantly systolic BP by 5.4 mmHg and diastolic BP by 2.8 mmHg. In normotensive individuals the same reduction of salt intake reduces significantly systolic BP by 2.4 mmHg and diastolic BP by 1.0 mmHg [26].
Potassium and BP Control
The augmented intake of potassium up to 3.500–5.000 mg per day through diet and not by supplements remains a recommendation for better BP levels, unless the subject has chronic kidney disease or taking drugs that reduce the excretion of sodium [2] [44]. Up to now there are several randomized studies on the above [45]. A meta-analysis showed that an intake of 3.500–4.700 mg potassium per day reduces systolic BP by 7.1 mmHg and diastolic BP by 4,0 mmHg, whereas there is no effect in normotensives [46]. Consistently, cross-sectional data suggest that potassium excretion in the urine is related to the BP levels and the risk of developing hypertension in the future [47]. The INTERSALT study showed that intake of more thatn 600 mg of potassium per day is linked to lower BP by 1 mmHg [48].
Dietary Patterns and BP Control
The real impact of diet on BP is not only due to the ingredients but also due to the patterns of diet that one follows. The diet patterns are mostly important clinically since they reflect better the dietary habits of each individuals and the interactions between foods consumed and other lifestyle parameters [49]. In this sense the effect of the totality of nutrients intake on the overall cardiovascular health as well as BP can be investigated through the study of the dietary patterns [50].
DASH Diet and BP
The DASH diet is associated with BP reduction 74 and is characterized by high consumption of fruits, vegetables and milk products with low fat content accompanied by low consumption of red meat. It is a diet rich in potassium, calcium, magnesium, proteins and fibers with low fat and cholesterol [51].
There are numerous randomized trials on the BP lowering impact of DASH diet in hypertension [51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71]. The historic study by Appel LJ et al., was a randomized, controlled-feeding clinical trial was conducted in order to test the effects on BP of three different diets: the control diet, the fruits-and-vegetables diet and the “combination” diet, which was rich in fruits, vegetables, and low-fat dairy products, now named the “DASH” diet [51]. The study was conducted in 459 adults with SBP <160 mmHg and DBP 80–95 mmHg. The assigned diets were prepared and given to the participants for 8 weeks. Sodium intake was kept constant at 3000 mg per day and it was the same among all three diets and body weight was maintained at constant levels. Among all subjects, the DASH diet reduced significantly systolic BP and diastolic BP by 5.5 and 3.0 mmHg, respectively, compared to the control diet and by 2.7 and 1.9 mmHg, respectively, compared to the fruits-and-vegetables diet. The results were more profound among the subjects with hypertension compared to the subjects without hypertension [51]. Specifically, among the 133 subjects with hypertension the DASH diet reduced significantly systolic BP and diastolic BP by 11.47 mmHg and 5.5 mmHg, respectively, more compared to the control diet and by 4.17 mmHg and 2.6 mmHg, respectively, more compared to the fruits-and-vegetables diet. Furthermore, among the 326 subjects without hypertension the DASH diet reduced significantly systolic BP and DBP by 3.57 mmHg and 2.1 mmHg, respectively, more compared to the control diet and by 2.77 mmHg and 1.8 mmHg, respectively, more compared to the fruits-and-vegetables diet. Given the findings of this pioneer studies one could comment that the gradient of BP reduction across diets indicates that some aspects of the fruits-and-vegetables diet reduced BP and that additional aspects of the combination (DASH) diet reduced it further. Known diet-related determinants of BP (sodium intake, body weight, and alcohol) could not be responsible for the reductions in BP, because changes in these potential confounders were small and similar for all the diets. Finally, regarding the composition of the diets compared the control and the fruits-and-vegetables diets contained more oils, table fats, salad dressings, and red meats and were higher in saturated fat, total fat, and cholesterol than was the DASH diet. The fruits-and-vegetables and the DASH diets contained relatively more servings of fruits, juices, vegetables, and nuts/seeds, and were higher in magnesium, potassium, and fiber than was the control diet [51]. Both the fruits-and-vegetables and DASH diets were low in sweets and sugar-containing drinks. The DASH diet contained a greater variety of fruits, and its high calcium content was obtained by increasing low-fat dairy products. It is worthy to note that the effect of an individual nutrient on BP levels may be too small to be detected. However, when several nutrients with small BP lowering effects are consumed together, the cumulative effect may be sufficient for detection. Also, people do not eat isolated nutrients, but they consume meals consisting of a variety of foods with complex combinations of nutrients. Thus, the approach of assessing whole dietary patterns, instead of assessing single nutrients or food items is considered more accurate [51]. However, the DASH clinical trial was not designed to identify the effective and ineffective components of this particular diet.
In a subgroup analysis of the DASH trial, the effect on the 24-h ambulatory hemodynamic load was tested and it was revealed that this dietary pattern reduces systolic/diastolic BP by 4.5/2.7 mmHg more than the control group. In the hypertensive setting compared to the normotensives the drop of BP was higher in the intervention arm [52]. More specifically, 24-h systolic/diastolic BP was more attenuated by 10.1/5/5 mmHg compared to the controls, whereas in normotensives DASH diet was accompanied by a lower 24-h systolic/diastolic BP by 2.3/1.6 mmHg [52].
The randomized cross-over DASH-Sodium study had the aim to investigate the impact of DAH on BP with the parallel restriction of sodium intake [53]. The study population were adults with baseline systolic BP 120–159 mmHg and diastolic BP 80–95 mmHg in whom the following interventions took place: control diet, DASH diet with three levels of sodium consumption: low, medium and high [53]. All meals were cooked and served in the participant for a period of 30 days and the energy intake was calculated foe each person in order to maintain stable weight. The results showed that the DASH diet with low sodium reduced BP by 3/1.6 mmHg compared to the DASH diet of high sodium. Additionally, the low sodium DASH diet was characterized by lower systolic/diastolic BP by 8.9/4.5 mmHg compared to the high sodium control diet [53].
When weight reduction is achieved while on DASH diet the BP lowering is enhanced [72, 73]. The ENCORE study was a randomized control trial in individuals with systolic BP of 130–159 mmHg and diastolic BP of 85–99 mmHg in whom the effect of DASH diet with or without weight loss on BP was investigated during a follow-up of 4 months. There were no directions regarding salt consumption and frequent dietary education and counseling took place. The DASH diet was related with lower BP by 7.7/3.6 mmHg compared to the control group, while when DASH was combined with weight loss the BP drop was more pronounced by 12.5/5.9 mmHg compared to controls at the end of the follow-up [62].
The cross-sectional data suggest that adoption of the DASH diet is linked with lower risk of hypertension and BP levels [74]. The difference in office BP between the higher and the lower quartile of compliance to the DASH pattern is 7.5 and 5.1 mmHg for men and women respectively, while the 24-h ambulatory data show a difference of 6.3 and 5.4 mmHg for men and women respectively [75].
In accordance to the previous, prospective works found that DASH diet is related with lower risk of future development of hypertension [76]. More specifically, in 2.751 normotensive subjects the upper quartile of compliance to the diet was associated with 15$ attenuated risk compared to the lower compliance quartile after a follow-up of 11 years [77].
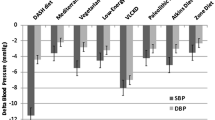
In a recent meta-analysis of randomized trials for the BP effect of DASH diet it was shown that it leads to a lowering of systolic/diastolic BP of 4.9/2.6 mmHg [71]. Two other meta-analyses by Saneei et al. and Siervo et al. found that the DASH diet reduces significantly SBP by 6.7/5.2 mmHg and DBP by 3.5/2.6 mmHg, respectively [78, 79].
Mediterranean Diet and BP
The Mediterranean diet is based on the high consumption of lipids derived from extra virgin (cold pressed) olive oil, vegetables including leafy green vegetables, fruits, cereals, nuts and pulses/legumes, moderate intakes of fish and other meat, dairy products and red wine, and low intakes of eggs and sweets [80, 81]. It is associated with lower BP and this is supported by randomized trials [82,83,84,85,86,87,88,89,90,91,92,93].
Focusing on the PREDIMED study that is the largest in this setting, it was conducted in 772 adults with high cardiovascular risk and comparisons were made between the Mediterranean diet with olive oil versus the same diet with nuts without any energy restriction for 3 months [86]. There were no advise given for salt restriction or physical activity. The results showed that the diet with nuts reduced systolic BP more by 7.1/2.6 mmHg compared to the low-fat group with no change in body weight in both arms [86].
In a subgroup analysis of 235 subjects of the PREDIMED study there was ambulatory 24-h BP monitoring after the intervention. In accordance to the office BP changes the 24-h systolic/diastolic BP was reduced more in the arm with the nuts intake [92]. In the same study there was no difference in the systolic BP after 4 years but the diastolic BP was lower in the nuts arm [94]. Importantly, subjects in the Mediterranean diet had less risk of developing hypertension compared to the control group after a 4 years follow-up [95].
A more recent randomized, parallel-group, controlled clinical trial was conducted in order to assess the effects on cardiovascular outcomes of two Mediterranean diets (MeDiets), one supplemented with extra-virgin olive oil and the other supplemented with mixed nuts, compared to a low-fat diet (control diet) [96]. The study was conducted in 7447 adults with type 2 diabetes or ≥3 cardiovascular risk factors. The participants of the two MeDiets groups, depending on the group assignment, were given for free either extra-virgin olive oil (1 L per week) or sachets of nuts (30 g per day: 15 g walnuts, 7.5 g hazelnuts and 7.5 g almonds) [96]. Participants in the two MeDiets groups received education to follow the MeDiet and consume the supplemental foods at the baseline and thereafter, once every 3 months in individual and group sessions, while those in the control group were given advice to reduce dietary fat. During the first 3 years of the trial they were given a leaflet explaining the low-fat diet on a yearly basis, but thereafter they were invited to individual and group sessions with the same frequency and intensity as those in the MeDiets groups [96]. Sodium intake was not restricted and energy restriction was not suggested, nor increase of physical activity was promoted. The primary end-point was a composite of myocardial infarction, stroke, and death from cardiovascular causes [96]. Additionally, secondary end-points were stroke, myocardial infarction, death from cardiovascular causes, and death from any cause. Participants were followed for a median of 4.8 years (interquartile range, 2.8–5.8). The multivariable-adjusted hazard ratios were 0.70 (0.54–0.92), p = 0.01 for the MeDiet supplemented with extra-virgin olive oil and 0.72 (0.54–0.96), p = 0.03 for the MeDiet supplemented with nuts, as compared to the low-fat diet with respect to the primary end-point [96]. Regarding components of the primary end-point, only the comparisons of stroke risk reached statistical significance: 0.67 (0.46–0.98), p = 0.04 for the MeDiet supplemented with extra-virgin olive oil and 0.54 (0.35–0.84), p = 0.006 for the MeDiet supplemented with nuts, as compared to the low-fat diet. During the 4-year follow-up participants allocated to the two MeDiets groups had significantly lower DBP than the participants in the low-fat diet group: −1.53 mmHg for the MeDiet supplemented with extra-virgin olive oil, and −0.65 mmHg for the MeDiet supplemented with nuts versus the low-fat diet. No between-group differences in changes of SBP were seen [96].
Based on these results among high-risk persons who were initially free of cardiovascular disease, an energy-unrestricted MeDiet supplemented with extra-virgin olive oil or nuts reduced the incidence of major cardiovascular events, for a relative risk reduction of approximately 30%. The findings support the benefits of the MeDiet for cardiovascular risk reduction. Perhaps there is a synergy among the nutrient-rich foods included in the MeDiet that fosters favorable changes in intermediate pathways of cardiometabolic risk, such as blood lipids, insulin sensitivity, resistance to oxidation, inflammation, and vasoreactivity. It should be noted that although the control group’s diet was meant to be low fat, the participants did not achieve this, possibly due to the relatively low level of dietary education and personalized counseling at the start of the study. Their inability to reach the <30% fat target could also reflect the difficulty patients have, in general, in decreasing fat content in their diet, which may mean the diet they maintained was a more realistic comparison. Therefore, the major between-group difference involved the supplemental items and consequently, the differences in outcomes observed between the MeDiets groups and the low-fat diet group might be attributed to the supplemental foods provided. The interventions in all three groups were intended to improve the overall dietary pattern. The good quality of the diet in the control group may have impaired the ability to find large between-group differences in BP changes. Thus, if there was a “true” control group (for example, with a typical Western dietary pattern, or with no intervention at all) the between-group differences both in stroke and BP would have been greater. Concerning BP, significant reductions were apparent in both SBP and DBP for all three groups during follow-up, but a greater reduction in DBP was found in the two MeDiets groups versus the low-fat diet group. This could partly explain the benefit of the MeDiets on clinical disease end-points, especially the reduction in incidence of stroke, a cardiovascular event clearly related to high BP. However, other mechanisms apart from BP also need to be considered.
The PREDIMED clinical trial fits well into the paradigm of focusing on dietary patterns instead of isolated foods or nutrients. Overall patterns better represent dietary practices found in free-living populations and provide useful epidemiological information with a high potential for acceptability, palatability, and future compliance.
The Mediterranean diet is characterized by a high consumption of total fat, mainly from olive oil and nuts, whole-grain cereals, legumes, fruits, and vegetables. It also includes moderate to high intake of fish, moderate intake of dairy products, poultry, and wine, consumed with meals along with low intake of red/ processed meats, and sweets. Consequently, the Mediterranean diet is rich in anti-oxidant and anti-inflammatory nutrients, fiber, ω-3 and mono-unsaturated fat and low in saturated fat and dietary cholesterol. Extra-virgin olive oil is an excellent source of mono-unsaturated fat. It also contains significant amounts of phenolic anti-oxidants and other phytochemicals (tocopherols, polyphenols). Nuts are rich in mono-unsaturated fat (mostly oleic acid), whereas walnuts are high in poly-unsaturated fatty acids (linoleic and a-linolenic acids). Nuts are also good sources of arginine, potassium, vitamin E and other bioactive compounds. This may help explain their beneficial health effects. From a public health perspective, a behavioral intervention coupled with an easy (free) access to representative healthy foods is a realistic test of the effectiveness to be attained with official policies and health promotion activities. The PREDIMED trial attempts to obtain relevant information for public health use, because the nutritional intervention is undertaken in free-living persons who receive information, motivation, support, and empowerment to modify their food habits in a real-life context, i.e. they continue to buy their foods and cook their meals. Such an intervention provides a real-life scenario that may be easily applied to public health policies.
Meta-analyses
Two meta-analyses of randomized, controlled clinical trials have been performed in adults investigating the magnitude of the effect of the MeDiet on blood pressure. Both found that the MeDiet has significant beneficial effects on SBP and DBP. Specifically, Ndanuko et al. and Nissensohn et al. found that the MeDiet reduces significantly SBP by 3.0/1.4 mmHg and DBP by 1.9/0.7 mmHg, respectively [71, 79].
Conclusions
Diet interventions are important in the overall reduction of cardiovascular risk and particular in the development and clinical impact of the hypertensive phenotype. The use of dietary consultation by means of promoting reduction of salt, maintenance of healthy weight and adoption of certain dietary patterns constitute the pillars of lifestyle management in hypertension. The DASH and the Mediterranean diet have proved their favorable effect on BP levels rendering them current health choices for the modern societies. Implementing such interventions in a large scale is an important and urgent clinically meaningful task nowadays in order to reduce hypertension and cardiovascular disease burden.
References
Jordan J, Yumuk V, Schlaich M, Nilsson PM, Zahorska-Markiewicz B, Grassi G, Schmieder RE, Engeli S, Finer N. Joint statement of the European Association for the Study of Obesity and the European Society of Hypertension: obesity and difficult to treat arterial hypertension. J Hypertens. 2012;30(6):1047–55.
Leggio M, Lombardi M, Caldarone E, Severi P, D'Emidio S, Armeni M, Bravi V, Bendini MG, Mazza A. The relationship between obesity and hypertension: an updated comprehensive overview on vicious twins. Hypertens Res. 2017;40(12):947–63.
Wilson PW, D’Agostino RB, Sullivan L, Parise H, Kannel WB. Overweight and obesity as determinants of cardiovascular risk: the Framingham experience. Arch Intern Med. 2002;162(16):1867–72.
Elliott P, Stamler J, Nichols R, Dyer AR, Stamler R, Kesteloot H, Marmot M. Intersalt revisited: further analyses of 24 hour sodium excretion and blood pressure within and across populations. Intersalt Cooperative Research Group. BMJ (Clinical research ed). 1996;312(7041):1249–53.
Mente A, O’Donnell MJ, Rangarajan S, McQueen MJ, Poirier P, Wielgosz A, Morrison H, Li W, Wang X, Di C, et al. Association of urinary sodium and potassium excretion with blood pressure. N Engl J Med. 2014;371(7):601–11.
Adrogue HJ, Madias NE. The impact of sodium and potassium on hypertension risk. Semin Nephrol. 2014;34(3):257–72.
Takase H, Sugiura T, Kimura G, Ohte N, Dohi Y. Dietary sodium consumption predicts future blood pressure and incident hypertension in the Japanese Normotensive General Population. J Am Heart Assoc. 2015;4(8):e001959.
Zhang Z, Cogswell ME, Gillespie C, Fang J, Loustalot F, Dai S, Carriquiry AL, Kuklina EV, Hong Y, Merritt R, et al. Association between usual sodium and potassium intake and blood pressure and hypertension among U.S. adults: NHANES 2005–2010. PloS one. 2013;8(10):e75289.
Rodrigues SL, Baldo MP, Machado RC, Forechi L, Molina Mdel C, Mill JG. High potassium intake blunts the effect of elevated sodium intake on blood pressure levels. J Am Soc Hypertens (JASH). 2014;8(4):232–8.
Kieneker LM, Gansevoort RT, Mukamal KJ, de Boer RA, Navis G, Bakker SJ, Joosten MM. Urinary potassium excretion and risk of developing hypertension: the prevention of renal and vascular end-stage disease study. Hypertension (Dallas, Tex : 1979). 2014;64(4):769–76.
Klatsky AL. Alcohol and cardiovascular mortality: common sense and scientific truth. J Am Coll Cardiol. 2010;55(13):1336–8.
Puddey IB, Beilin LJ. Alcohol is bad for blood pressure. Clin Exp Pharmacol Physiol. 2006;33(9):847–52.
Puddey IB, Beilin LJ, Vandongen R. Regular alcohol use raises blood pressure in treated hypertensive subjects. A randomised controlled trial. Lancet (London, England). 1987;1(8534):647–51.
Nunez-Cordoba JM, Martinez-Gonzalez MA, Bes-Rastrollo M, Toledo E, Beunza JJ, Alonso A. Alcohol consumption and the incidence of hypertension in a Mediterranean cohort: the SUN study. Rev Esp Cardiol. 2009;62(6):633–41.
Frisoli TM, Schmieder RE, Grodzicki T, Messerli FH. Beyond salt: lifestyle modifications and blood pressure. Eur Heart J. 2011;32(24):3081–7.
The treatment of mild hypertension study. A randomized, placebo-controlled trial of a nutritional-hygienic regimen along with various drug monotherapies. The Treatment of Mild Hypertension Research Group. Arch Intern Med. 1991;151(7):1413–23.
Elmer PJ, Obarzanek E, Vollmer WM, Simons-Morton D, Stevens VJ, Young DR, Lin PH, Champagne C, Harsha DW, Svetkey LP, et al. Effects of comprehensive lifestyle modification on diet, weight, physical fitness, and blood pressure control: 18-month results of a randomized trial. Ann Intern Med. 2006;144(7):485–95.
Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Bohm M, Christiaens T, Cifkova R, De Backer G, Dominiczak A, Redon J, Tsioufis C, Bueno H, et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens. 2013;31(7):1281–357.
Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, Depalma SM, Gidding S, Jamerson KA, Jones DW, et al. ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and Management of High Blood Pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018;71(19):2199–269.
Neter JE, Stam BE, Kok FJ, Grobbee DE, Geleijnse JM. Influence of weight reduction on blood pressure: a meta-analysis of randomized controlled trials. Hypertension (Dallas, Tex : 1979). 2003;42(5):878–84.
Stevens VJ, Obarzanek E, Cook NR, Lee IM, Appel LJ, Smith West D, Milas NC, Mattfeldt-Beman M, Belden L, Bragg C, et al. Long-term weight loss and changes in blood pressure: results of the Trials of Hypertension Prevention, phase II. Ann Intern Med. 2001;134(1):1–11.
Effects of weight loss and sodium reduction intervention on blood pressure and hypertension incidence in overweight people with high-normal blood pressure. The Trials of Hypertension Prevention, phase II. The Trials of Hypertension Prevention Collaborative Research Group. Arch Intern Med. 1997;157(6):657–67.
He J, Whelton PK, Appel LJ, Charleston J, Klag MJ. Long-term effects of weight loss and dietary sodium reduction on incidence of hypertension. Hypertension (Dallas, Tex : 1979). 2000;35(2):544–9.
Straznicky N, Grassi G, Esler M, Lambert G, Dixon J, Lambert E, Jordan J, Schlaich M. European Society of Hypertension Working Group on Obesity Antihypertensive effects of weight loss: myth or reality? J Hypertens. 2010;28(4):637–43.
Ryan DH. The pharmacological and surgical management of adults with obesity. J Fam Pract. 2014;63(7 Suppl):S21–6.
He FJ, Li J, Macgregor GA. Effect of longer term modest salt reduction on blood pressure: Cochrane systematic review and meta-analysis of randomised trials. BMJ (Clinical research ed). 2013;346:f1325.
Aburto NJ, Ziolkovska A, Hooper L, Elliott P, Cappuccio FP, Meerpohl JJ. Effect of lower sodium intake on health: systematic review and meta-analyses. BMJ (Clinical research ed). 2013;346:f1326.
MacGregor GA, Markandu ND, Sagnella GA, Singer DR, Cappuccio FP. Double-blind study of three sodium intakes and long-term effects of sodium restriction in essential hypertension. Lancet (London, England). 1989;2(8674):1244–7.
Benetos A, Xiao YY, Cuche JL, Hannaert P, Safar M. Arterial effects of salt restriction in hypertensive patients. A 9-week, randomized, double-blind, crossover study. J Hypertens. 1992;10(4):355–60.
Fotherby MD, Potter JF. Effects of moderate sodium restriction on clinic and twenty-four-hour ambulatory blood pressure in elderly hypertensive subjects. J Hypertens. 1993;11(6):657–63.
Cappuccio FP, Markandu ND, Carney C, Sagnella GA, MacGregor GA. Double-blind randomised trial of modest salt restriction in older people. Lancet (London, England). 1997;350(9081):850–4.
Gates PE, Tanaka H, Hiatt WR, Seals DR. Dietary sodium restriction rapidly improves large elastic artery compliance in older adults with systolic hypertension. Hypertension (Dallas, Tex : 1979). 2004;44(1):35–41.
Melander O, von Wowern F, Frandsen E, Burri P, Willsteen G, Aurell M, Hulthen UL. Moderate salt restriction effectively lowers blood pressure and degree of salt sensitivity is related to baseline concentration of renin and N-terminal atrial natriuretic peptide in plasma. J Hypertens. 2007;25(3):619–27.
Kojuri J, Rahimi R. Effect of “no added salt diet” on blood pressure control and 24 hour urinary sodium excretion in mild to moderate hypertension. BMC Cardiovasc Disord. 2007;7:34.
Dickinson KM, Keogh JB, Clifton PM. Effects of a low-salt diet on flow-mediated dilatation in humans. Am J Clin Nutr. 2009;89(2):485–90.
He FJ, Marciniak M, Visagie E, Markandu ND, Anand V, Dalton RN, MacGregor GA. Effect of modest salt reduction on blood pressure, urinary albumin, and pulse wave velocity in white, black, and Asian mild hypertensives. Hypertension (Dallas, Tex : 1979). 2009;54(3):482–8.
He J, Gu D, Chen J, Jaquish CE, Rao DC, Hixson JE, Chen JC, Duan X, Huang JF, Chen CS, et al. Gender difference in blood pressure responses to dietary sodium intervention in the GenSalt study. J Hypertens. 2009;27(1):48–54.
Liu F, Chen P, Li D, Yang X, Huang J, Gu D. Ambulatory blood pressure and blood pressure load responses to low sodium intervention in Han Chinese population. Clin Exp Hypertens. 2015;37(7):551–6.
Graudal NA, Hubeck-Graudal T, Jurgens G. Effects of low sodium diet versus high sodium diet on blood pressure, renin, aldosterone, catecholamines, cholesterol, and triglyceride. Cochrane Database Syst Rev. 2017;4:Cd004022.
Whelton PK, Appel LJ, Espeland MA, Applegate WB, Ettinger WH Jr, Kostis JB, Kumanyika S, Lacy CR, Johnson KC, Folmar S, et al. Sodium reduction and weight loss in the treatment of hypertension in older persons: a randomized controlled trial of nonpharmacologic interventions in the elderly (TONE). TONE Collaborative Research Group. JAMA. 1998;279(11):839–46.
Stamler J. The INTERSALT Study: background, methods, findings, and implications. Am J Clin Nutr. 1997;65(2 Suppl):626s–42s.
Zhou BF, Stamler J, Dennis B, Moag-Stahlberg A, Okuda N, Robertson C, Zhao L, Chan Q, Elliott P. Nutrient intakes of middle-aged men and women in China, Japan, United Kingdom, and United States in the late 1990s: the INTERMAP study. J Hum Hypertens. 2003;17(9):623–30.
Cappucio FP, Markandu ND, Carney C, Sagnella GA, MacGregor GA. Double-blind randomized trial of modest salt restriction in older people. Lancet. 1997;350:850–4.
Koliaki C, Katsilambros N. Dietary sodium, potassium, and alcohol: key players in the pathophysiology, prevention, and treatment of human hypertension. Nutr Rev. 2013;71(6):402–11.
Geleijnse JM, Kok FJ, Grobbee DE. Blood pressure response to changes in sodium and potassium intake: a metaregression analysis of randomised trials. J Hum Hypertens. 2003;17(7):471–80.
Aburto NJ, Hanson S, Gutierrez H, Hooper L, Elliott P, Cappuccio FP. Effect of increased potassium intake on cardiovascular risk factors and disease: systematic review and meta-analyses. BMJ (Clinical research ed). 2013;346:f1378.
Whelton PK, He J. Health effects of sodium and potassium in humans. Curr Opin Lipidol. 2014;25(1):75–9.
Dyer AR, Elliott P, Shipley M. Urinary electrolyte excretion in 24 hours and blood pressure in the INTERSALT Study. II. Estimates of electrolyte-blood pressure associations corrected for regression dilution bias. The INTERSALT Cooperative Research Group. Am J Epidemiol. 1994;139(9):940–51.
Tapsell LC, Neale EP, Satija A, Hu FB. Foods, nutrients, and dietary patterns: interconnections and implications for dietary guidelines. Adv Nutr (Bethesda, Md). 2016;7(3):445–54.
Jacobs DR Jr, Steffen LM. Nutrients, foods, and dietary patterns as exposures in research: a framework for food synergy. Am J Clin Nutr. 2003;78(3 Suppl):508s–13s.
Appel LJ, Moore TJ, Obarzanek E, Vollmer WM, Svetkey LP, Sacks FM, Bray GA, Vogt TM, Cutler JA, Windhauser MM, et al. A clinical trial of the effects of dietary patterns on blood pressure. DASH Collaborative Research Group. N Engl J Med. 1997;336(16):1117–24.
Moore TJ, Vollmer WM, Appel LJ, Sacks FM, Svetkey LP, Vogt TM, Conlin PR, Simons-Morton DG, Carter-Edwards L, Harsha DW. Effect of dietary patterns on ambulatory blood pressure : results from the Dietary Approaches to Stop Hypertension (DASH) Trial. DASH Collaborative Research Group. Hypertension (Dallas, Tex : 1979). 1999;34(3):472–7.
Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, Harsha D, Obarzanek E, Conlin PR, Miller ER 3rd, Simons-Morton DG, et al. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-Sodium Collaborative Research Group. N Engl J Med. 2001;344(1):3–10.
Lopes HF, Martin KL, Nashar K, Morrow JD, Goodfriend TL, Egan BM. DASH diet lowers blood pressure and lipid-induced oxidative stress in obesity. Hypertension (Dallas, Tex : 1979). 2003;41(3):422–30.
Nowson CA, Worsley A, Margerison C, Jorna MK, Frame AG, Torres SJ, Godfrey SJ. Blood pressure response to dietary modifications in free-living individuals. J Nutr. 2004;134(9):2322–9.
Appel LJ, Sacks FM, Carey VJ, Obarzanek E, Swain JF, Miller ER 3rd, Conlin PR, Erlinger TP, Rosner BA, Laranjo NM, et al. Effects of protein, monounsaturated fat, and carbohydrate intake on blood pressure and serum lipids: results of the OmniHeart randomized trial. JAMA. 2005;294(19):2455–64.
Marquez-Celedonio FG, Texon-Fernandez O, Chavez-Negrete A, Hernandez-Lopez S, Marin-Rendon S, Berlin-Lascurain S. Clinical effect of lifestyle modification on cardiovascular risk in prehypertensives: PREHIPER I study. Rev Esp Cardiol. 2009;62(1):86–90.
Nowson CA, Wattanapenpaiboon N, Pachett A. Low-sodium Dietary Approaches to Stop Hypertension-type diet including lean red meat lowers blood pressure in postmenopausal women. Nutr Res (New York, NY). 2009;29(1):8–18.
Al-Solaiman Y, Jesri A, Mountford WK, Lackland DT, Zhao Y, Egan BM. DASH lowers blood pressure in obese hypertensives beyond potassium, magnesium and fibre. J Hum Hypertens. 2010;24(4):237–46.
Malloy-McFall J, Barkley JE, Gordon KL, Burzminski N, Glickman EL. Effect of the DASH diet on pre- and stage 1 hypertensive individuals in a free-living environment. Nutr Metab Insights. 2010;3:15–23.
Harnden KE, Frayn KN, Hodson L. Dietary Approaches to Stop Hypertension (DASH) diet: applicability and acceptability to a UK population. J Hum Nutr Diet. 2010;23(1):3–10.
Blumenthal JA, Babyak MA, Hinderliter A, Watkins LL, Craighead L, Lin PH, Caccia C, Johnson J, Waugh R, Sherwood A. Effects of the DASH diet alone and in combination with exercise and weight loss on blood pressure and cardiovascular biomarkers in men and women with high blood pressure: the ENCORE study. Arch Intern Med. 2010;170(2):126–35.
Lin PH, Allen JD, Li YJ, Yu M, Lien LF, Svetkey LP. Blood pressure-lowering mechanisms of the DASH dietary pattern. J Nutr Metab. 2012;2012:472396.
Whitt-Glover MC, Hunter JC, Foy CG, Quandt SA, Vitolins MZ, Leng I, Hornbuckle LM, Sanya KA, Bertoni AG. Translating the Dietary Approaches to Stop Hypertension (DASH) diet for use in underresourced, urban African American communities, 2010. Prev Chronic Dis. 2013;10:120088.
Lima ST, da Silva Nalin de Souza B, Franca AK, Salgado Filho N, Sichieri R. Dietary approach to hypertension based on low glycaemic index and principles of DASH (Dietary Approaches to Stop Hypertension): a randomised trial in a primary care service. Br J Nutr. 2013;110(8):1472–9.
Wong MC, Wang HH, Kwan MW, Fong BC, Chan WM, Zhang DX, Li ST, Yan BP, Coats AJ, Griffiths SM. Dietary counselling has no effect on cardiovascular risk factors among Chinese Grade 1 hypertensive patients: a randomized controlled trial. Eur Heart J. 2015;36(38):2598–607.
Jenkins DJ, Jones PJ, Frohlich J, Lamarche B, Ireland C, Nishi SK, Srichaikul K, Galange P, Pellini C, Faulkner D, et al. The effect of a dietary portfolio compared to a DASH-type diet on blood pressure. Nutr Metab Cardiovasc Dis: NMCD. 2015;25(12):1132–9.
Sayer RD, Wright AJ, Chen N, Campbell WW. Dietary Approaches to Stop Hypertension diet retains effectiveness to reduce blood pressure when lean pork is substituted for chicken and fish as the predominant source of protein. Am J Clin Nutr. 2015;102(2):302–8.
Chiu S, Bergeron N, Williams PT, Bray GA, Sutherland B, Krauss RM. Comparison of the DASH (Dietary Approaches to Stop Hypertension) diet and a higher-fat DASH diet on blood pressure and lipids and lipoproteins: a randomized controlled trial. Am J Clin Nutr. 2016;103(2):341–7.
Kawamura A, Kajiya K, Kishi H, Inagaki J, Mitarai M, Oda H, Umemoto S, Kobayashi S. Effects of the DASH-JUMP dietary intervention in Japanese participants with high-normal blood pressure and stage 1 hypertension: an open-label single-arm trial. Hypertens Res. 2016;39(11):777–85.
Naseem S, Ghazanfar H, Assad S, Ghazanfar A. Role of sodium-restricted dietary approaches to control blood pressure in Pakistani hypertensive population. JPMA J Pak Med Assoc. 2016;66(7):837–42.
Azadbakht L, Mirmiran P, Esmaillzadeh A, Azizi T, Azizi F. Beneficial effects of a Dietary Approaches to Stop Hypertension eating plan on features of the metabolic syndrome. Diabetes Care. 2005;28(12):2823–31.
Kucharska A, Gajewska D, Kiedrowski M, Sinska B, Juszczyk G, Czerw A, Augustynowicz A, Bobinski K, Deptala A, Niegowska J. The impact of individualized nutritional therapy according to DASH diet on blood pressure, body mass and selected biochemical parameters in overweight/obese patients with primary arterial hypertension: a prospective randomized study. Kardiol Pol. 2017;76(1):158–65.
Wang HH, Wong MC, Mok RY, Kwan MW, Chan WM, Fan CK, Lee CL, Griffiths SM. Factors associated with grade 1 hypertension: implications for hypertension care based on the Dietary Approaches to Stop Hypertension (DASH) in primary care settings. BMC Fam Pract. 2015;16:26.
Harrington JM, Fitzgerald AP, Kearney PM, McCarthy VJ, Madden J, Browne G, Dolan E, Perry IJ. DASH diet score and distribution of blood pressure in middle-aged men and women. Am J Hypertens. 2013;26(11):1311–20.
Schulze MB, Hoffmann K, Kroke A, Boeing H. Risk of hypertension among women in the EPIC-Potsdam Study: comparison of relative risk estimates for exploratory and hypothesis-oriented dietary patterns. Am J Epidemiol. 2003;158(4):365–73.
Bai G, Zhang J, Zhao C, Wang Y, Qi Y, Zhang B. Adherence to a healthy lifestyle and a DASH-style diet and risk of hypertension in Chinese individuals. Hypertens Res. 2017;40(2):196–202.
Saneei P, Salehi-Abargouei A, Esmaillzadeh A, Azadbakht L. Influence of Dietary Approaches to Stop Hypertension (DASH) diet on blood pressure: a systematic review and meta-analysis on randomized controlled trials. Nutr Metab Cardiovasc Dis: NMCD. 2014;24(12):1253–61.
Siervo M, Lara J, Chowdhury S, Ashor A, Oggioni C, Mathers JC. Effects of the Dietary Approach to Stop Hypertension (DASH) diet on cardiovascular risk factors: a systematic review and meta-analysis. Br J Nutr. 2015;113(1):1–15.
Bach-Faig A, Berry EM, Lairon D, Reguant J, Trichopoulou A, Dernini S, Medina FX, Battino M, Belahsen R, Miranda G, et al. Mediterranean diet pyramid today. Science and cultural updates. Public Health Nutr. 2011;14(12a):2274–84.
Salas-Salvado J, Garcia-Arellano A, Estruch R, Marquez-Sandoval F, Corella D, Fiol M, Gomez-Gracia E, Vinoles E, Aros F, Herrera C, et al. Components of the Mediterranean-type food pattern and serum inflammatory markers among patients at high risk for cardiovascular disease. Eur J Clin Nutr. 2008;62(5):651–9.
Strazzullo P, Ferro-Luzzi A, Siani A, Scaccini C, Sette S, Catasta G, Mancini M. Changing the Mediterranean diet: effects on blood pressure. J Hypertens. 1986;4(4):407–12.
Esposito K, Marfella R, Ciotola M, Di Palo C, Giugliano F, Giugliano G, D’Armiento M, D'Andrea F, Giugliano D. Effect of a mediterranean-style diet on endothelial dysfunction and markers of vascular inflammation in the metabolic syndrome: a randomized trial. JAMA. 2004;292(12):1440–6.
Ros E, Nunez I, Perez-Heras A, Serra M, Gilabert R, Casals E, Deulofeu R. A walnut diet improves endothelial function in hypercholesterolemic subjects: a randomized crossover trial. Circulation. 2004;109(13):1609–14.
Vincent-Baudry S, Defoort C, Gerber M, Bernard MC, Verger P, Helal O, Portugal H, Planells R, Grolier P, Amiot-Carlin MJ, et al. The Medi-RIVAGE study: reduction of cardiovascular disease risk factors after a 3-mo intervention with a Mediterranean-type diet or a low-fat diet. Am J Clin Nutr. 2005;82(5):964–71.
Estruch R, Martinez-Gonzalez MA, Corella D, Salas-Salvado J, Ruiz-Gutierrez V, Covas MI, Fiol M, Gomez-Gracia E, Lopez-Sabater MC, Vinyoles E, et al. Effects of a Mediterranean-style diet on cardiovascular risk factors: a randomized trial. Ann Intern Med. 2006;145(1):1–11.
Rallidis LS, Lekakis J, Kolomvotsou A, Zampelas A, Vamvakou G, Efstathiou S, Dimitriadis G, Raptis SA, Kremastinos DT. Close adherence to a Mediterranean diet improves endothelial function in subjects with abdominal obesity. Am J Clin Nutr. 2009;90(2):263–8.
Athyros VG, Kakafika AI, Papageorgiou AA, Tziomalos K, Peletidou A, Vosikis C, Karagiannis A, Mikhailidis DP. Effect of a plant stanol ester-containing spread, placebo spread, or Mediterranean diet on estimated cardiovascular risk and lipid, inflammatory and haemostatic factors. Nutr Metab Cardiovasc Dis: NMCD. 2011;21(3):213–21.
Jones JL, Fernandez ML, McIntosh MS, Najm W, Calle MC, Kalynych C, Vukich C, Barona J, Ackermann D, Kim JE, et al. A Mediterranean-style low-glycemic-load diet improves variables of metabolic syndrome in women, and addition of a phytochemical-rich medical food enhances benefits on lipoprotein metabolism. J Clin Lipidol. 2011;5(3):188–96.
Damasceno NR, Perez-Heras A, Serra M, Cofan M, Sala-Vila A, Salas-Salvado J, Ros E. Crossover study of diets enriched with virgin olive oil, walnuts or almonds. Effects on lipids and other cardiovascular risk markers. Nutr Metab Cardiovasc Dis: NMCD. 2011;21(Suppl 1):S14–20.
Katsarou AL, Vryonis MM, Protogerou AD, Alexopoulos EC, Achimastos A, Papadogiannis D, Chrousos GP, Darviri C. Stress management and dietary counseling in hypertensive patients: a pilot study of additional effect. Prim Health Care Res Dev. 2014;15(1):38–45.
Domenech M, Roman P, Lapetra J, Garcia de la Corte FJ, Sala-Vila A, de la Torre R, Corella D, Salas-Salvado J, Ruiz-Gutierrez V, Lamuela-Raventos RM, et al. Mediterranean diet reduces 24-hour ambulatory blood pressure, blood glucose, and lipids: one-year randomized, clinical trial. Hypertension (Dallas, Tex : 1979). 2014;64(1):69–76.
Davis CR, Hodgson JM, Woodman R, Bryan J, Wilson C, Murphy KJ. A Mediterranean diet lowers blood pressure and improves endothelial function: results from the MedLey randomized intervention trial. Am J Clin Nutr. 2017;105(6):1305–13.
Toledo E, Hu FB, Estruch R, Buil-Cosiales P, Corella D, Salas-Salvado J, Covas MI, Aros F, Gomez-Gracia E, Fiol M, et al. Effect of the Mediterranean diet on blood pressure in the PREDIMED trial: results from a randomized controlled trial. BMC Med. 2013;11:207.
Estruch R. PREDIMED Study Investigators: primary prevention of cardiovascular disease with a Mediterranean diet. N Engl J Med. 2013;368(14):1279–90.
Estruch R, Ros E, Salas-Salvadó J, Covas MI, Corella D, Arós F, et al. Primary prevention of cardiovascular disease with a Mediterranean diet. N Engl J Med. 2013;368(14):1279–90.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Dimitriadis, K., Filippou, C., Tsioufis, C. (2019). The Role of Dietary Modifications in Controlling Blood Pressure. In: Papademetriou, V., Andreadis, E., Geladari, C. (eds) Management of Hypertension. Springer, Cham. https://doi.org/10.1007/978-3-319-92946-0_5
Download citation
DOI: https://doi.org/10.1007/978-3-319-92946-0_5
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-92945-3
Online ISBN: 978-3-319-92946-0
eBook Packages: MedicineMedicine (R0)