Abstract
Treatment of prostate cancer has evolved significantly over the last decade. Active surveillance has been established as the primary treatment for low risk disease. National and international guidelines state that for a patient with low risk localized prostate cancer, brachytherapy (BT), external beam radiotherapy (EBRT) and radical prostatectomy (RP) are appropriate monotherapy options and the outcomes data do not provide a clear-cut evidence for the superiority of any one treatment. Available evidence suggests that there is no difference in clinical progression, incidence of metastases or overall survival between RP or EBRT for low risk patients. Similarly, the paradigm for intermediate risk prostate cancer has shifted with introduction of low-tier and high tier intermediate risk categories. While the low-tier intermediate risk patients are treated with one of many available treatment modalities and difference in clinical outcomes has been shown for those receiving prostatectomy or radiotherapy; high-tier intermediate risk patients, on the other hand have better outcome with combination of EBRT and BT. There is emerging, albeit early evidence that hypofractionated radiotherapy regimens may be appropriate choice in select low-risk and low-tier intermediate risk patients as monotherapy, as well as for select high-tier intermediate risk patients in combination with brachytherapy. In this chapter, we summarize key clinical series and trials to highlight differences in the outcomes among various treatment modalities utilized for treatment of localized prostate cancer and compare those to extreme hypofractionated regimens also known as stereotactic body radiotherapy (SBRT).
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Stereotactic Body Radiotherapy (SBRT)
- Intermediate-risk Patients
- Prostate SBRT
- Tumor Control Outcomes
- Hypofractionated Regimen
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
FormalPara Learning Objectives and Outline-
1.
To understand radiobiology of prostate cancer and role of higher dose per fraction in its treatment
-
2.
To summarize clinical outcomes of patients treated with
-
a.
Prostatectomy
-
b.
Conventional fractionated EBRT
-
c.
Moderate hypofractionated EBRT
-
d.
Brachytherapy (HDR and LDR)
-
e.
Proton beam therapy
-
f.
Extreme hypofractionation aka SBRT
-
a.
-
3.
Conclusion
7.1 Radiobiological Consideration in Prostate Cancer and Support for Hypofractionation
Probability of cell kill from radiation is estimated based on ratio of intrinsic radiosensitivity to repair capacity of a particular tissue. Linear quadratic model is the most widely accepted model that fits probability of surviving fraction of cells after a given dose of radiation. Alpha (α) and beta (β) are the constants that represent intrinsic radiosensitivity and repair capacity and can be derived by fitting linear quadratic model to function of cell survival probability plotted against the radiation dose. The actual values of alpha (α) and beta (β) are difficult to ascertain, therefore, based on best fit model a ratio of α/β is reported, where early responding tissues are generally characterised by a high α/β ratio and late responding tissues are defined by a low α/β ratio. Tumors, generally are considered early responding tissues with α/β ratio of >8, while normal tissue complication probability is calculated based on assumption that α/β ratio for normal tissues is <4 and thus are considered late responding tissues. Radiobiological studies have shown as α/β ratio decreases, there is increased sensitivity to dose per fraction. Therefore, in most cancers, adjacent late responding tissues are more sensitive to increased dose per fraction than the tumors. For this reason, most radiation regimens utilize small daily fraction sizes (1–2 Gy) to maximize the therapeutic ratio, with reduction in late complications without any compromise in tumor control.
Prostate cancer, on the other hand has unique radiobiology, first suggested by Brenner and Hall who observed that biochemical control was similar for 70 Gy given in 1–2 Gy fractions and I-125 brachytherapy using a prescription dose of 144 Gy [1]. Subsequent studies by others have demonstrated that the α/β ratio for prostate cancer ranges between 1.5 and 1.85 [2, 3]. This low α/β ratio predicts a greater capacity for repair between fractions, with an accompanying greater relative sparing with smaller fraction sizes. Therefore, a higher dose of radiation per fraction may be particularly effective in causing prostate cancer cell death. Table 7.1 illustrates biological effective doses for various dose fractionation regimens used in prostate cancer including low dose rate brachytherapy using iodine-125 (I-125) seeds.
In recent years it has become evident that hypofractionated radiotherapy regimens can provide excellent tumor control with limited toxicity to surrounding tissue, although the long-term results are yet to become available. In this chapter, we aim to summarize available tumor control data for various treatment modalities being employed for localized low- and intermediate-risk prostate cancer and compare those outcomes to early results with those obtained with extreme hypofractionated regimens also known as stereotactic body radiotherapy (SBRT).
7.2 Clinical Outcomes with Various Treatment Modalities
7.2.1 Surgery
Radical prostatectomy (RP) is considered one of the standards for men with low and intermediate risk prostate cancer. Last two decades has seen significant progress in RP methodology with introduction of laparoscopic RP in late 1990s [4] and robot assisted RP in early 2000s [5]. There are multiple older series that report clinical outcomes with RP, however, most of them are open procedures and include patients from prior to PSA-screening era. Selected publications, with large enough patient numbers from contemporary, post-PSA screening era with modern surgical techniques are summarized in Table 7.2. In these series, median follow-up ranged from 4 to 10 years. Biochemical relapse free survival (bRFS) for low-risk disease ranged from 79% at 5 years at University of Toronto [6] to 97% at 5 years from Johns Hopkins University [7]. Corresponding 10-year bRFS rates ranged from 64 to 95%. Whereas the bRFS for intermediate-risk disease ranged from 59% at 5 years at University of Toronto to 72% at 10 years from Johns Hopkins University.
Summary
Surgery is the oldest and most established treatment option for low- and intermediate risk prostate patients. With recent advances in surgical techniques and introduction of laparoscopic and robotic-assisted prostatectomy techniques, there has been some improvement in tumor control outcomes. Modern prostatectomy series report a 10-year median (range) biochemical relapse free survival of 86% (64–95%). Similarly, for intermediate risk patients treated with RP, median 10-year bRFS is reported to be 61% (59–72%).
7.2.2 Conventionally Fractionated Radiotherapy
Early studies reporting clinical outcomes of prostate cancer with conventional fraction were dismal. As the understanding of prostate cancer biology improved over the last three decades, the clinical outcomes improved as reported by multiple randomized control trials and institutional series, summarized in Table 7.3. Zelefsky et al. [13] reported on 1100 patients from Memorial Sloan Kettering Cancer Center (MSKCC) undergoing dose escalation with conventional fractionation. They found that with doses higher than 75.6 Gy there was statistically significant improvement in biochemical relapse free (bRFS) in both low and intermediate risk patients; 5-year bRFS was 90 and 70%, respectively. Results of four randomized control trials confirmed that the higher doses are required to achieve better tumor control outcome in localized prostate cancer [14,15,16,17]. Other institutional series further consolidated that higher dose delivered to the localized prostate cancer in conventional fractionation resulted in statistically significant improvement in bRFS [18,19,20].
Kalbasi et al. [21] performed a retrospective comparative effectiveness study of all prostate cancer patients registered in National Cancer Database (NCDB) from 2004 to 2006. Authors analysed 12,229 low-risk and 16,714 intermediate-risk patients and reported 7-year OS of 86 and 82%, respectively, for those treated with EBRT dose ≥75.6 Gy. In propensity score matched analysis, dose escalated EBRT (≥75.6 Gy) was associated with statistically significant improvement in OS for intermediate risk patients (HRs 0.84; p < 0.001), but not for low risk patients.
Summary
Multiple randomized trials and large institutional series have now confirmed that the higher doses of radiation are required to improve bRFS and OS for patients with localized low and intermediate risk prostate cancer. Traditionally, using the conventional fractionation regimens, the higher doses were achievable only by increasing the number of fractions, which implies that patients would come for more than 8 weeks of daily treatments. These additional treatments are not only burdensome for the patient and family, but can also pose challenge for busy radiotherapy centers.
7.2.3 Moderately Hypofractionated Radiotherapy
Moderate hypofractionation for prostate cancer has cautiously been introduced into clinical practice, with the hope of reducing overall treatment time, while maintaining efficacy. Early institutional series laid the ground work for three randomized clinical trials that demonstrated that moderate hypofractionation results in excellent tumor control, acceptable toxicity and increased convenience to patients compared to standard fractionation. Thus, these regimens have been accepted as the new standard as a monotherapy option for favorable intermediate risk patients or as a part of combination with androgen deprivation therapy (ADT) for unfavorable intermediate or high risk patients undergoing treatment with external beam radiotherapy. Table 7.4 summarizes the key clinical trial and pertinent results from moderate hypofractionation series.
RTOG 0415 assessed the role of moderate hypofractionation in low-risk patients in a randomized control trial [23]. Total of 1115 patients were randomized to either receive 73.8 Gy in 41 fractions or 70 Gy in 28 fractions. At a median follow up of 5.8 years, there was no difference in disease free survival (85.3 vs. 86.3%) and acute toxicity between two arms. CHiPP trial is the largest randomized trial, that included 3216 men from the United Kingdom with localized prostate cancer that either received 74 Gy in 37 fractions, 60 Gy in 20 fractions or 57 Gy in 19 fractions [24]. Fifteen percent and 73% of them were low- and intermediate-risk patients, respectively. Five-year biochemical and clinical failure free rates were similar across all three arms: 88.3% in 74 Gy group, 90.6% in 60 Gy group and 85.9% Gy in 57 Gy group. Although there was no difference in late gastrointestinal (GI) toxicity (11.9% vs. 13.4%), there was, however, a trend towards slightly higher genitourinary (GU) toxicity at 5 years with hypofractionated regimen 11.7 versus 9.1% (HR = 1.34, p = 0.07).
In trial by Pollack et al. [25] 303 men with localized intermediate- (66%) and high-risk (34%) disease were randomized to either receive conventionally fractionated RT (76 Gy in 38 fractions) or hypofractionated RT (60.2 Gy in 26 fractions) between 2002 and 2006; low-risk patients were excluded. The 5-year biochemical and clinical disease failure was similar in both arms, 21.4 versus 23.3% and there was no significant difference in acute or late GI or GU toxicity. In the Canadian PROFIT trial 1206 intermediate risk patients were randomly assigned to either receive 78 Gy (standard) or 60 Gy (short) course radiotherapy in 39 or 20 fractions, respectively [26]. Five-year bRFS rate was 85% for both arms (HR = 0.96). The investigators noted a significant increase in grade 2 of higher acute GI toxicity in short arm compared to standard arm, 16.7 vs. 10.5% (p = 0.003); conversely, for late grade 2 of higher toxicity occurred more frequently in standard arm versus short arm, 13.7 versus 8.9%, respectively (p = 0.006). Acute and late grade 2 or higher GU toxicities were similar in both arms. The authors concluded that short fractionation is not inferior to the standard fractionated radiotherapy for intermediate risk patients and is more convenient for patients.
Contrary to other trials, in HYPRO Trial, a phase three randomized non-inferiority trial that compared 78 Gy in 39 fractions to 64.6 Gy in 19 fractions in 820 intermediate and high-risk patients [27], the investigators reported a significantly higher grade 3 or worse late GU toxicity in hypofractionation arm (19.0 vs. 12.9%, p = 0.021). Late grade 2 or worse GI toxicity was similar between two arms at 17.7 and 21.9%. Nonetheless, the investigators could not reject inferiority because the hazard ratios for both GU and GI toxicity were higher than their initial hypothesis. Furthermore, due to high grade 3 or worse GU toxicity observed at 3 years, investigators concluded that non-inferiority of hypofractionation could not be confirmed. It is important to note that only one quarter of the patients in this trial were intermediate risk and remainder were high-risk patients that required long term ADT as well as inclusion of seminal vesicles in the treatment volume. Additionally, the hypofractionation dose in this trial was higher than other contemporary hypofractionation trials, which may explain higher incidence of toxicity. Lastly, the HR for non-inferiority was set much lower in this trial compared to others.
Royce et al. [28] recently conducted a meta-analysis of these 3 non-inferiority randomized trials that evaluated moderately hypofractionated regimens (2.4–4 Gy) compared to conventionally fractionated regimens (1.8–2 Gy). Sixty five percent of patients were intermediate risk (n = 3553). Based on random effects model, hypofractionated RT had significantly improved disease-free survival (HR 0.89, p = 0.047) compared to conventionally fractionated RT, however there was no difference in OS. Authors also noted that there was increased grade 2 or higher acute GI toxicity with hypofractionation (RR = 1.42, p = 0.002), but it did not translate into higher late toxicity. A trend towards an increase late G2 or higher GU toxicity was observed with hypofractionation (RR = 1.18, p = 0.08).
Summary
Randomized trials have now demonstrated that moderately hypofractionated radiotherapy regimens can provide excellent tumor control and are much more convenient for the patients, compared to conventionally fractionated radiotherapy regimens. The reported bRFS survival ranged from 90.9 to 93.7% 5 years for low-risk disease and 85–86% at 5 years for intermediate-risk disease.
7.2.4 Brachytherapy
Brachytherapy (BT) is an excellent treatment modality as monotherapy for low-risk patients as well as favorable intermediate risk patients. Furthermore, BT when combined with either EBRT or ADT (or both) is one of the standard treatment options for intermediate- and selected high-risk patients, especially after publication of ASCENDE-RT trial (Morris et al. Red Journal 2017). Tables 7.5 and 7.6 summarize contemporary series that report long term tumor control outcomes for patients treated with low dose rate (LDR) and high dose rate brachytherapy (LDR), respectively.
7.2.4.1 Low Dose Rate Brachytherapy
With improvement in brachytherapy approach using trans-rectal ultrasound (TRUS) in the 1980s and introduction of stable low energy radioisotopes, LDR brachytherapy became an established and popular treatment modality for low risk and favorable intermediate risk prostate cancer. Zelefsky et al. [29] reported long-term results of 2693 patients with localised prostate cancer treated with I-125 or palladium-103 (Pd-103) implantation by pooling data from 11 institutions across the US and Canada. At median followup of 5.3 years, 8-year bRFS was 82 and 70% for low- and intermediate-risk patients treated with LDR monotherapy alone. The Seattle group has the longest reported outcomes of low-, intermediate- and high-risk patients treated with LDR monotherapy with I-125 seeds [30]. At median follow up of 11.3 years, they reported 15-year bRFS of 85.9 and 79.9% for low risk (n = 158) and intermediate risk (n = 44) patients, respectively. Others have similarly reported excellent institutional results of patients treated with LDR brachytherapy with or without short term (6 month) androgen deprivation therapy [31,32,33,34,35]. The median (range) bRFS for low-risk patients treated with LDR brachytherapy with or without ADT is reported to be 87% (82–94%) at a median of 10 years (5–15 years) follow up. Outcome for intermediate-risk patients treated with LDR brachytherapy with or without ADT were 83% (70–97%) at median follow up of 6.5 years (5–15 years).
While the above reported results are from retrospective registries, only two prospective trials of LDR monotherapy for intermediate risk patients have been reported so far [36, 37]. Results from RTOG 0232 study, where selected IR patients were randomized to receive either EBRT+LDR BT or BT alone have been presented in abstract form only [36]. At median follow up of 6.7 years, they showed that 5-year bRFS for IR patients treated with LDR monotherapy was 86%. Similarly, Frank et al. [37] in a prospective phase 2 trial reported 5-year bRFS of 93% for favorable IR patients treated with I-125, Pd-103 or Cs-131 monotherapy.
7.2.4.2 High Dose Rate Brachytherapy
High dose rate (HDR) brachytherapy has most commonly been used in the boost setting with EBRT for unfavorable intermediate- or high-risk patients. Demanes et al. [39] were the first to report utilization of HDR brachytherapy as monotherapy for localized prostate cancer by pooling patients from California Endocurietherapy Cancer Center (CET) and William Beaumont Hospital (WBH). Patients either received 42 Gy in six fractions in two separate implants, 1 week apart (CET) or 38 Gy in four fractions in a single implant (WBH). All patients were low risk or favourable intermediate risk. At median follow up of 5.2 years, 8-year bRFS was 97% with minimal G2 or worse GI toxicity and favorable G2 or worse GU toxicity (29%). Barkati et al. [40] performed phase 1 dose escalation study of delivering 30 Gy, 31.5 Gy, 33 Gy and 34.5 Gy in 3 fractions in a single implant and reported 5-year bRFS of 85% in favorable IR patients treated with HDR monotherapy. They, however, observed a high rate late urinary retention due to urethral stricture (9%). Hoskin et al. [41] reported their dose escalation study from United Kingdom, that included mostly intermediate and high risk patients and majority of them received ADT. With favorable GI and GU toxicity profile, they reported 4-year bRFS of 95% for intermediate risk patients. Most importantly they reported feasibility of delivering HDR monotherapy in two fractions using CT and MRI based planning techniques. Zamboglou et al. has so far reported the largest series of men with localized prostate cancer undergoing HDR brachytherapy [42]. Eighty-nine percent were low- and intermediate-risk patients. They reported cumulative 5- and 8-year bRFS of 94% and 90%, respectively for entire cohort, with low grade 3 or worse late GI and GU toxicity.
In recent years there have been multiple institutional reports confirming favourable bRFS outcomes with acceptable GU and GI toxicity with HDR brachytherapy [43,44,45,46,47,48,49]. Most authors have reported bRFS of 97% (66–98%) for combined cohorts of low- and intermediate risk patients and at median follow up 6.0 years (5.0–10.0 years). Others, who stratified patients according to the risk grouping report 95% bRFS at 5 years for low risk disease and 93% (90–96%) at 6.5 years (4–8 years) for intermediate risk disease.
Summary
Brachytherapy has proven to be an excellent treatment modality for low- and intermediate-risk prostate cancer. While, LDR has proven record in low-risk disease with established dose, HDR practice still has significant heterogeneity in terms of total dose and number of fractions. Median 10- and 6.5-year bRFS in low- and intermediate-risk patients treated with LDR is reported to be 87% (82–94%) and 83% (70–97%), respectively. Corresponding rates with HDR at 5- and 6.5-years are 96 and 93% (90–96%) for low-and intermediate risk patients, respectively. Even, though both LDR and HDR options are available for this cohort of patients, they are, however, limited mostly to large academic centers. Furthermore, interest in brachytherapy has been declining, in part due to decline in trained radiation oncologists who can perform brachytherapy. Improvement in external beam technologies and advent of moderate and extreme hypofractionation have further reduced its utilization in most recent decade.
7.2.5 Proton Beam Therapy
There has been an increased interest in utilizing favorable dose profile of proton beam to treat prostate cancer. The rationale for using protons in radiotherapy arises due to the physics that account for the way that conventional high energy x-rays (photons) and protons deposit their energy in the patient. Unlike x-rays, for proton beam therapy (PBT) the energy deposited per unit distance increases markedly as the proton slows down, producing a sharp peak (the Bragg peak) of energy at the end of the proton range. Very little energy is deposited distal to the Bragg peak. The beneficial effect of the Bragg peak is utilized to decrease the dose deposited outside the prostate, especially in the rectum, thus potentially resulting in lower toxicity.
Zeitman et al. [22] first utilized protons for dose escalation trial (RTOG 95-09) in low- (n = 115) and intermediate-risk (n = 68) patients. They successfully increased the dose to 79.2 CGE using conventional fractionation and reported excellent bRFS at 10 years: 92.9% for low-risk and 69.6% for intermediate-risk. University of Florida Health Proton Therapy Institute has published their experience in treating prostate cancer with protons in a series of publications and report 5 year bRFS of 99% for low-risk patients and 93–99% for intermediate risk patients [50,51,52]. The rate of grade 3 or worse GI and GU toxicity was very low in their cohorts: 0.5–1.0% and 1.7–4.8%, respectively. Recently, Japanese investigators have reported 8-year bRFS of 95% for low-risk patients and 87% for intermediate risk patients treated with 74 CGE using PBT [53]. They also reported very low rates of GI and GU toxicity.
Summary
Proton beam therapy is an emerging treatment modality for localized prostate cancer. Although initial data suggest good biochemical control rates [98% (93–99%) for low-risk patients and 93% (70–99%) for intermediate risk patient at 5 years], additional studies with longer term follow up are required to validate these findings. Furthermore, the PBT is being delivered with conventional fractionation regimen, that provides the same logistic challenges as the conventionally fractionated radiotherapy discussed earlier. Hypofractionated PBT regimens are being studied, but to date there are no published data available (Table 7.7).
7.2.6 Extreme Hypofractionation Aka SBRT
Hypofractionated radiotherapy for prostate cancer has been studied since the 1960s [54]. Early experience using 36 Gy delivered in 6 Gy fractions reported minimal acute and long-term toxicity with this approach. This early experience utilized relatively crude planning techniques as compared with more modern approaches, however despite this; hypofractionated therapy appeared to be safe. Since this early experience, many subsequent studies have demonstrated that toxicity of hypofractionated regimens using brachytherapy or external beam radiation appear at least comparable if not more favorable to conventionally fractionated regimens [39, 55,56,57,58,59]. Extreme hypofractionation and stereotactic techniques were not routinely utilized in treatment of prostate cancer until mid 2000s when significant developments in radiation planning and delivery were introduced. A medline/pubmed search using MESH terms “prostate” and “stereotactic radiotherapy” yielded only 42 results between 1995 and 2004, whereas 305 publications were found with same MESH terms for years 2005–2014, indicating significant increase in number of publications and interest in prostate SBRT. Baker et al. (Cancer 2016) analysed the US National Cancer Database on utilization of SBRT and found that in 2012 there were approximately 7.6 and 3.2% of patients were being treated SBRT at academic and comprehensive cancer centers, respectively across US, compared to zero in 2004
There are several advantages of SBRT, that have resulted in adoption of this technique:
-
1.
Low α/β ratio of 1.5 for prostate cancer indicates that potentially there may be higher effect of tumor control with hypofractionation compared to conventional fractionation.
-
2.
Due to rectal α/β ratio higher than prostate (3 vs. 1.5), late rectal complications may be decreased for a given level of tumor control
-
3.
Patient convenience and possibly improved quality of life with fewer fractions, compared to 7–9 weeks of treatments with conventional fractionation.
-
4.
Potential benefit of cost efficiency for cancer center as the equipment utilization and staffing may be more efficient with fewer fractions.
7.2.6.1 Early Results
While earlier publications focused on feasibility and toxicity of SBRT, recently clinical outcomes of patients being treated with SBRT have been reported and these are summarized in Table 7.8. King et al. [60] from UCLA, reported outcomes in 67 low-risk patients treated with 36.25 Gy in 5 fractions using Cyberknife™ technology. At median follow up of 2.7 years, 4-year bRFS was 94% with only 2 PSA and biopsy proven local failures. At median follow up of 3.7 years Mcbride et al. reported 3-year actuarial bPFS of 97.7% in 47 low risk patients treat at 4 different cancer centers with doses ranging between 36.35 to 37.5 Gy in 5 fractions [61]. Aluwini et al. [62] from Erasmus Cancer Center included both low (60%) and intermediate-risk (40%) patients and increased the dose to 38 Gy to entire prostate with integrated boost of 55 Gy to the dominant intra-prostatic lesion in 5 fractions. At median follow up of 23 months, 2-year biochemical control rate was 100% with acute grade 2 and 3 GI toxicity of 12 and 2% and late grade 2 higher GI toxicity of only 3%. Loblaw et al. reported results of prospective Phase I/II trial of delivering 35 Gy in 5 once weekly fractions in 29 days using linear accelerator-based treatment delivery systems [63]. The 5-year biochemical control in their low-risk cohort of patients was 98%. They also performed biopsies at 36 months from completion of treatment on all patients enrolled in the trial and found that 96% of the patients had negative biopsy.
Katz and Kang have published the largest SBRT series to date, that included 470 (324 low-risk and 153 intermediate-risk) patients treated with 35–36.25 Gy in 5 fractions [64]. Eleven percent of patients received 6 months of neoadjuvant and concurrent ADT. They reported 7-year actuarial bPFS of 95.6 and 89.6% for low- and intermediate risk patients, respectively. They further stratified their intermediate cohort into low-tier and high-tier groups and found that there was statistically significant difference in bPFS (93.5 vs. 79.3%) between the two groups. Updated results of 230 low-risk patients treated with either 35 Gy/5 fractions of 36.25 Gy/5 fractions were recently reported [65]. With a median follow up of 9 years, 10-year bDFS was 95.8% without any difference between two dose levels. The only difference reported was in G3 GU toxicity: 4 vs. 15% in 35 and 36.25 Gy cohorts, respectively.
Hannan et al. included 36% low-risk and 64% intermediate risk patients from five cancer centers across the US in phase I/II dose escalation trial [66]. They delivered 45 Gy (n = 15), 47.5 Gy (n = 15) and 50 Gy (n = 62) in 5 fractions and reported 3- and 5-year actuarial freedom from biochemical failure rate of 100 and 98.6% for the entire cohort. They, however, observed 7% rate of grade 3 of higher GI toxicity at 5 years, which was indeed higher than that reported in contemporary prostate cancer literature. Kotecha et al. recently reported their results of phase II trial of integrated dose escalation for dominant lesion in 24 high tier intermediate and high-risk patients [67]. They treated the entire prostate to 36.25 Gy, while boosting the dominant lesion to 50 Gy in 5 fractions. Sixty seven percent of patients received ADT for a median of 6 months (range 4–30.5 months). Early results indicate, 2-year bRFS of 95.8% at median follow of 25 months, with only 2 relapses both occurring in high risk patients.
Summary
SBRT demonstrates excellent early outcomes for patients with low and intermediate risk disease. Follow up is short to have meaningful comparison with other modalities. Nonetheless, available data suggests bRFS of 97% (94–98%) at 4.5 years for low-risk patients, 90% at 8 years for intermediate-risk patients and 99% (96–100%) at 2 years for patient cohorts with mixed low- and intermediate-risk patients. Pooled analysis of multiple phase I/II trials also show 5-year DFS of 95 and 84% for low- and intermediate-risk patients respectively [68]. These are promising results when compared to other modalities as illustrated in Fig. 7.1. Furthermore, given the convenience conferred by the SBRT regimens for patients and treatment centers it has become very attractive options. In the coming years, once more mature data is available, SBRT will become one of the standard treatment option as a monotherapy for low and intermediate risk patients.
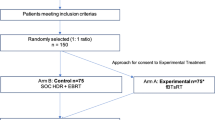
Combination of external beam radiotherapy with brachytherapy has established as standard treatment option for intermediate prostate cancer as demonstrated in ASCENDE-RT randomized trial [69]. There is adequate emerging evidence that SBRT, as it is well tolerated by the patients may be better treatment option for low-tier intermediate risk patients as monotherapy, as well as for high-tier intermediate risk patients in combination brachytherapy. This later hypothesis has been tested in prospective manner by the MSKCC group, but the results have not been published yet (personal communication). Furthermore, SBRT may also have a role in treatment of patients in high risk category. Recently published, multi-institutional retrospective analysis of high risk patients (GS 9-10) has also confirmed that combination of EBRT and brachytherapy results in improved local and distant control as well as there may be an improvement in overall survival [70]. SBRT should be studied in a prospective randomized manner to evaluate its efficacy against conventional EBRT in the setting of combined modality treatment of high risk patients.
7.3 Conclusion
With advancement in image guidance and availability of protective measures such as rectal spacer, SBRT has become relatively easy to deliver and convenient treatment choice for patients, with minimal toxicity. It is conceivable that in near future, SBRT would be the primary form of external beam treatment for prostate cancer patients.
Disclosures
Dr. Zelefsky serves as a consultant for Augmenix.
References
Brenner DJ, Hall EJ. Fractionation and protraction for radiotherapy of prostate carcinoma. Int J Radiat Oncol Biol Phys. 1999;43(5):1095–101.
Brenner DJ, Martinez AA, Edmundson GK, Mitchell C, Thames HD, Armour EP. Direct evidence that prostate tumors show high sensitivity to fractionation (low alpha/beta ratio), similar to late-responding normal tissue. Int J Radiat Oncol Biol Phys. 2002;52(1):6–13.
Dasu A. Is the alpha/beta value for prostate tumours low enough to be safely used in clinical trials? Clin Oncol (R Coll Radiol). 2007;19(5):289–301.
Schuessler WW, Schulam PG, Clayman RV, Kavoussi LR. Laparoscopic radical prostatectomy: initial short-term experience. Urology. 1997;50(6):854–7.
Binder J, Kramer W. Robotically-assisted laparoscopic radical prostatectomy. BJU Int. 2001;87(4):408–10.
Louis AS, Kalnin R, Maganti M, Pintilie M, Matthew AG, Finelli A, et al. Oncologic outcomes following radical prostatectomy in the active surveillance era. Can Urol Assoc J. 2013;7(7–8):e475–80.
Mullins JK, Feng Z, Trock BJ, Epstein JI, Walsh PC, Loeb S. The impact of anatomical radical retropubic prostatectomy on cancer control: the 30-year anniversary. J Urol. 2012;188(6):2219–24.
Røder MA, Berg KD, Gruschy L, Brasso K, Cancer IP. First Danish single-institution experience with radical prostatectomy: biochemical outcome in 1200 consecutive patients. Prostate Cancer. 2011;2011:5.
Diaz M, Peabody JO, Kapoor V, Sammon J, Urology RCG. Oncologic outcomes at 10 years following robotic radical prostatectomy. Eur Urol. 2015;67(6):1168–76.
Kane CJ, Im R, Amling CL, Presti JC, Aronson WJ, Terris MK, et al. Outcomes after radical prostatectomy among men who are candidates for active surveillance: results from the SEARCH database. Urology. 2010;76(3):695–700.
Menon M, Bhandari M, Gupta N, Lane Z, Peabody JO, Rogers CG, et al. Biochemical recurrence following robot-assisted radical prostatectomy: analysis of 1384 patients with a median 5-year follow-up. Eur Urol. 2010;58(6):838–46.
Nivedita B-D, Reuther AM, Zippe C, Klein EA. No difference in six-year biochemical failure rates with or without pelvic lymph node dissection during radical prostatectomy in low-risk patients with localized prostate cancer. Urology. 2004;63(3):528–31.
Zelefsky MJ, Fuks ZVI, Hunt M, Lee HJ, Lombardi D, Ling C, et al. High dose radiation delivered by intensity modulated conformal radiotherapy improves the outcome of localized prostate cancer. J Urol. 2001;166(3):876–81.
Pollack A, Zagars GK, Starkschall G, Antolak JA. Prostate cancer radiation dose response: results of the MD Anderson phase III randomized trial. Int J Radiat Oncol Biol Phys. 2002;53(5):1097–105.
Peeters S, Heemsbergen WD, Koper P, van Putten W, Slot A, Dielwart M, et al. Dose-response in radiotherapy for localized prostate cancer: results of the Dutch multicenter randomized phase III trial comparing 68 Gy of radiotherapy with 78 Gy. J Clin Oncol. 2006;24(13):1990–6.
Kuban DA, Tucker SL, Dong L, Starkschall G, Huang EH, Cheung MR, et al. Long-term results of the M. D. Anderson randomized dose-escalation trial for prostate cancer. Int J Radiat Oncol Biol Phys. 2008;70(1):67–74.
Heemsbergen WD, Abrahim A-M, Slot A, Dielwart MF, Lebesque JV. Long-term results of the Dutch randomized prostate cancer trial: impact of dose-escalation on local, biochemical, clinical failure, and survival. Radiother Oncol. 2014;110(1):104–9.
Zelefsky MJ, Yamada Y, Fuks Z, Zhang Z, Hunt M, Cahlon O, et al. Long-term results of conformal radiotherapy for prostate cancer: impact of dose escalation on biochemical tumor control and distant metastases-free survival outcomes. Int J Radiat Oncol Biol Phys. 2008;71(4):1028–33.
Eade TN, Hanlon AL, Horwitz EM, Buyyounouski MK, Hanks GE, Pollack A. What dose of external-beam radiation is high enough for prostate cancer? Int J Radiat Oncol Biol Phys. 2007;68(3):682–9.
Dearnaley DP, Sydes MR, Graham JD, Aird EG, Bottomley D, Cowan R, et al. Escalated-dose versus standard-dose conformal radiotherapy in prostate cancer: first results from the MRC RT01 randomised controlled trial. Lancet Oncol. 2007;8(6):475–87.
Kalbasi A, Li J, Berman A, Samuel S-M, Smaldone M, Uzzo RG, et al. Dose-escalated irradiation and overall survival in men with nonmetastatic prostate cancer. JAMA Oncol. 2015;1(7):897–906.
Zietman AL, Bae K, Slater JD, Shipley WU, Efstathiou JA, Coen JJ, et al. Randomized trial comparing conventional-dose with high-dose conformal radiation therapy in early-stage adenocarcinoma of the prostate: long-term results from proton radiation oncology group/american college of radiology 95-09. J Clin Oncol. 2010;28(7):1106–11.
Lee RW, Dignam JJ, Amin MB, Bruner DW, Low D, Swanson GP, et al. Randomized phase III noninferiority study comparing two radiotherapy fractionation schedules in patients with low-risk prostate cancer. J Clin Oncol. 2016;34(20):2325–32.
Dearnaley D, Syndikus I, Mossop H, Khoo V, Birtle A, Bloomfield D, et al. Conventional versus hypofractionated high-dose intensity-modulated radiotherapy for prostate cancer: 5-year outcomes of the randomised, non-inferiority, phase 3 CHHiP trial. Lancet Oncol. 2016;17(8):1047–60.
Pollack A, Walker G, Horwitz EM, Price R, Feigenberg S, Konski AA, et al. Randomized trial of hypofractionated external-beam radiotherapy for prostate cancer. J Clin Oncol. 2013;31(31):3860–8.
Catton CN, Lukka H, Gu C-SS, Martin JM, Supiot S, Chung PWMWM, et al. Randomized trial of a hypofractionated radiation regimen for the treatment of localized prostate cancer. J Clin Oncol. 2017;35(17):1884–90.
Aluwini S, Pos F, Schimmel E, Krol S, van der Toorn PP, de Jager H, et al. Hypofractionated versus conventionally fractionated radiotherapy for patients with prostate cancer (HYPRO): late toxicity results from a randomised, non-inferiority, phase 3 trial. Lancet Oncol. 2016;17(4):464–74.
Royce T, Lee D, Keum N, Permpalung N, Chiew CJ, Epstein S, et al. Conventional versus hypofractionated radiation therapy for localized prostate cancer: a meta-analysis of randomized noninferiority trials. Eur Urol Focus. 2017; https://doi.org/10.1016/j.euf.2017.10.011.
Zelefsky MJ, Deborah AK, Larry BL, Potters L, David CB, John CB, et al. Multi-institutional analysis of long-term outcome for stages T1-T2 prostate cancer treated with permanent seed implantation. Int J Radiat Oncol Biol Phys. 2007;67(2):327–33.
Sylvester JE, Grimm PD, Wong J, Galbreath RW, Merrick G, Blasko JC. Fifteen-year biochemical relapse-free survival, cause-specific survival, and overall survival following I(125) prostate brachytherapy in clinically localized prostate cancer: Seattle experience. Int J Radiat Oncol Biol Phys. 2011;81(2):376–81.
Morris WJ, Keyes M, Spadinger I, Kwan W, Liu M, McKenzie M, et al. Population-based 10-year oncologic outcomes after low-dose-rate brachytherapy for low-risk and intermediate-risk prostate cancer. Cancer. 2013;119(8):1537–46.
Herbert C, James WM, Keyes M, Hamm J, Lapointe V, McKenzie M, et al. Outcomes following iodine-125 brachytherapy in patients with Gleason 7, intermediate risk prostate cancer: a population-based cohort study. Radiother Oncol [Internet]. 2012;103(2):228–32.
Sekiguchi A, Ishiyama H, Satoh T, Tabata K, Komori S, Tsumura H, et al. 125Iodine monotherapy for Japanese men with low- and intermediate-risk prostate cancer: outcomes after 5 years of follow-up. J Radiat Res. 2014;55(2):328–33.
Kittel JA, Reddy CA, Smith KL, Stephans KL, Tendulkar RD, Ulchaker J, et al. Long-term efficacy and toxicity of low-dose-rate 125I prostate brachytherapy as monotherapy in low-, intermediate-, and high-risk prostate cancer. Int J Radiat Oncol Biol Phys. 2015;92(4):884–93.
Cosset J, Flam T, Belin L, Thiounn N, Pierrat N, Pontvert D, et al. Long-term results of permanent implant prostate cancer brachytherapy: a single-institution study of 675 patients treated between 1999 and 2003. Cancer Radiother. 2016;20(4):261–7.
Prestidge BR, Winter K, Sanda MG, Amin M, Bice WS, Michalski J, et al. Initial report of NRG oncology/RTOG 0232: a phase 3 study comparing combined external beam radiation and transperineal interstitial permanent brachytherapy with brachytherapy alone for selected patients with intermediate-risk prostatic carcinoma. Int J Radiat Oncol Biol Phys. 2016;96(2):S4.
Frank SJ, Pugh TJ, Blanchard P, Mahmood U, Graber WJ, Kudchadker RJ, et al. Prospective phase 2 trial of permanent seed implantation prostate brachytherapy for intermediate-risk localized prostate cancer: efficacy, toxicity, and quality of life outcomes. Int J Radiat Oncol Biol Phys. 2018;100(2):374–82.
Kollmeier MA, Fidaleo A, Pei X, Cohen G, Zaider M, Mo Q, et al. Favourable long-term outcomes with brachytherapy-based regimens in men ≤60 years with clinically localized prostate cancer. BJU Int. 2013;111(8):1231–6.
Demanes DJ, Martinez AA, Ghilezan M, Hill DR, Schour L, Brandt D, et al. High-dose-rate monotherapy: safe and effective brachytherapy for patients with localized prostate cancer. Int J Radiat Oncol Biol Phys. 2011;81(5):1286–92.
Barkati M, Williams SG, Foroudi F, Tai KH, Chander S, van Dyk S, et al. High-dose-rate brachytherapy as a monotherapy for favorable-risk prostate cancer: a Phase II trial. Int J Radiat Oncol Biol Phys. 2012;82(5):1889–96.
Hoskin P, Rojas A, Lowe G, Bryant L, Ostler P, Hughes R, et al. High-dose-rate brachytherapy alone for localized prostate cancer in patients at moderate or high risk of biochemical recurrence. Int J Radiat Oncol Biol Phys. 2012;82(4):1376–84.
Zamboglou N, Tselis N, Baltas D, Buhleier T, Martin T, Milickovic N, et al. High-dose-rate interstitial brachytherapy as monotherapy for clinically localized prostate cancer: treatment evolution and mature results. Int J Radiat Oncol Biol Phys. 2013;85(3):672–8.
Ghadjar P, Oesch SL, Rentsch CA, Isaak B, Cihoric N, Manser P, et al. Late toxicity and five year outcomes after high-dose-rate brachytherapy as a monotherapy for localized prostate cancer. Radiat Oncol. 2014;9:122.
Yoshioka Y, Suzuki O, Isohashi F, Seo Y. High-dose-rate brachytherapy as monotherapy for intermediate-and high-risk prostate cancer: clinical results for a median 8-year follow-up. Int J Radiat Oncol Biol Phys. 2016;94(4):675–82.
Jawad MS, Dilworth JT, Gustafson GS, Ye H, Wallace M, Martinez A, et al. Outcomes associated with 3 treatment schedules of high-dose-rate brachytherapy monotherapy for favorable-risk prostate cancer. Int J Radiat Oncol Biol Phys. 2016;94(4):657–66.
Hauswald H, Kamrava MR, Fallon JM, Wang P-CC, Park S-JJ, Van T, et al. High-dose-rate monotherapy for localized prostate cancer: 10-year results. Int J Radiat Oncol Biol Phys. 2016;94(4):667–74.
Patel S, Demanes DJ, Ragab O, Zhang M, Veruttipong D, Nguyen K, et al. High-dose-rate brachytherapy monotherapy without androgen deprivation therapy for intermediate-risk prostate cancer. Brachytherapy. 2017;16(2):299–305.
Strouthos I, Tselis N, Chatzikonstantinou G, Butt S, Baltas D, Bon D, et al. High dose rate brachytherapy as monotherapy for localised prostate cancer. Radiother Oncol. 2018;126(2):270–7.
Prada PJ, Cardenal J, Blanco AG, Anchuelo J, Ferri M, Fernández G, et al. High-dose-rate interstitial brachytherapy as monotherapy in one fraction for the treatment of favorable stage prostate cancer: toxicity and long-term biochemical results. Radiother Oncol. 2016;119(3):411–6.
Mendenhall NP, Hoppe BS, Nichols RC, Mendenhall WM, Morris CG, Li Z, et al. Five-year outcomes from 3 prospective trials of image-guided proton therapy for prostate cancer. Int J Radiat Oncol Biol Phys. 2014;88(3):596–602.
Bryant C, Smith TL, Henderson RH, Hoppe BS, Mendenhall WM, Nichols RC, et al. Five-year biochemical results, toxicity, and patient-reported quality of life after delivery of dose-escalated image guided proton therapy for prostate cancer. Int J Radiat Oncol Biol Phys. 2016;95(1):422–34.
Henderson RH, Bryant C, Hoppe BS, Nichols CR, Mendenhall WM, Flampouri S, et al. Five-year outcomes from a prospective trial of image-guided accelerated hypofractionated proton therapy for prostate cancer. Acta Oncol (Madr). 2017;56(7):1–8.
Takagi M, Demizu Y, Terashima K, Fujii O, Jin D, Niwa Y, et al. Long-term outcomes in patients treated with proton therapy for localized prostate cancer. Cancer Med. 2017;6(10):2234–43.
Collins CD, Lloyd-Davies RW, Swan AV. Radical external beam radiotherapy for localised carcinoma of the prostate using a hypofractionation technique. Clin Oncol (R Coll Radiol). 1991;3(3):127–32.
Katz AJ, Santoro M, Diblasio F, Ashley R. Stereotactic body radiotherapy for localized prostate cancer: disease control and quality of life at 6 years. Radiat Oncol. 2013;8:118.
Tang CI, Loblaw DA, Cheung P, Holden L, Oncology MG. Phase I/II study of a five-fraction hypofractionated accelerated radiotherapy treatment for low-risk localised prostate cancer: early results of pHART3. Clin Oncol (R Coll Radiol). 2008;20(10):729–37.
Martinez A, Gonzalez J, Spencer W, Gustafson G, Kestin L, Kearney D, et al. Conformal high dose rate brachytherapy improves biochemical control and cause specific survival in patients with prostate cancer and poor prognostic factors. J Urol. 2003;169(3):974–80.
Madsen BL, Hsi RA, Pham HT, Fowler JF, Esagui L, Corman J. Stereotactic hypofractionated accurate radiotherapy of the prostate (SHARP), 33.5 Gy in five fractions for localized disease: first clinical trial results. Int J Radiat Oncol Biol Phys. 2007;67(4):1099–105.
Bhattasali O, Chen LN, Woo J, Park J-WW, Kim JS, Moures R, et al. Patient-reported outcomes following stereotactic body radiation therapy for clinically localized prostate cancer. Radiat Oncol. 2014;9(1):52.
King CR, Brooks JD, Gill H, Presti JC. Long-term outcomes from a prospective trial of stereotactic body radiotherapy for low-risk prostate cancer. Int J Radiat Oncol Biol Phys. 2012;82(2):877–82.
McBride S, Wong D, Dombrowski JJ, Harkins B, Tepella P, Hanscom H, et al. Hypofractionated stereotactic body radiotherapy in low-risk prostate adenocarcinoma. Cancer. 2012;118(15):3681–90.
Aluwini S, van Rooij P, Hoogeman M, Kirkels W, Kolkman-Deurloo I-K, Bangma C. Stereotactic body radiotherapy with a focal boost to the MRI-visible tumor as monotherapy for low- and intermediate-risk prostate cancer: early results. Radiat Oncol. 2013;8:84.
Loblaw A, Cheung P, D'Alimonte L, Deabreu A, Mamedov A, Zhang L, et al. Prostate stereotactic ablative body radiotherapy using a standard linear accelerator: toxicity, biochemical, and pathological outcomes. Radiother Oncol. 2013;107(2):153–8.
Katz AJ, Kang J. Stereotactic body radiotherapy as treatment for organ confined low- and intermediate-risk prostate carcinoma, a 7-year study. Front Oncol. 2014;4:240.
Katz A. Stereotactic body radiotherapy for low-risk prostate cancer: a ten-year analysis. Cureus. 2017;9(9):e1668.
Hannan R, Tumati V, Xie X-J, Cho LC, Kavanagh BD, Brindle J, et al. Stereotactic body radiation therapy for low and intermediate risk prostate cancer-Results from a multi-institutional clinical trial. Eur J Cancer. 2016;59:142–51.
Kotecha R, Djemil T, Tendulkar RD, Reddy CA, Thousand RA, Vassil A, et al. Dose-escalated stereotactic body radiation therapy for patients with intermediate- and high-risk prostate cancer: initial dosimetry analysis and patient outcomes. Int J Radiat Oncol Biol Phys. 2016;95(3):960–4.
King CR, Freeman D, Kaplan I, Fuller D, Bolzicco G, Collins S, et al. Stereotactic body radiotherapy for localized prostate cancer: pooled analysis from a multi-institutional consortium of prospective phase II trials. Radiother Oncol. 2013;109(2):217–21.
Morris WJ, Tyldesley S, Rodda S, Halperin R, Pai H, Michael M, et al. Androgen suppression combined with elective nodal and dose escalated radiation therapy (the ASCENDE-RT trial): an analysis of survival endpoints for a randomized trial comparing a low-dose-rate brachytherapy boost to a dose-escalated external beam boost for high- and intermediate-risk prostate cancer. Int J Radiat Oncol Biol Phys. 2017;98(2):275–85.
Kishan AU, Cook RR, Ciezki JP, Ross AE, Pomerantz MM, Nguyen PL, et al. Radical prostatectomy, external beam radiotherapy, or external beam radiotherapy with brachytherapy boost and disease progression and mortality in patients with Gleason score 9-10 prostate cancer. JAMA. 2018;319(9):896–905.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Crown
About this chapter
Cite this chapter
Taggar, A.S., Mann, P., Zelefsky, M.J. (2019). Overview of Tumor Control Outcomes with Prostate SBRT for Low and Intermediate Risk Prostate Cancer and Comparison to Other Treatment Interventions. In: Zelefsky, M. (eds) Stereotactic Radiosurgery for Prostate Cancer. Springer, Cham. https://doi.org/10.1007/978-3-319-92453-3_7
Download citation
DOI: https://doi.org/10.1007/978-3-319-92453-3_7
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-92452-6
Online ISBN: 978-3-319-92453-3
eBook Packages: MedicineMedicine (R0)