Abstract
Stereotactic body radiotherapy (SBRT) has been shown to be an effective and well-tolerated treatment for patients with low- and intermediate-risk prostate cancer, however a number of questions remain unanswered. The aim of this chapter is to summarise ongoing prospective trials which will contribute to existing data, potentially leading to further advances in prostate SBRT. Crucially, large randomized trials will be described, which will directly compare outcomes with conventional treatments. Further work seeks to explore the benefit in high-risk patients, and to establish the role of androgen deprivation therapy (ADT) in combination with SBRT. A number studies are evaluating the use of intraprostatic dose escalation, while others are investigating the delivery of pelvic SBRT. In addition, given the particular radiobiology of prostate cancer and sensitivity to large fraction size, it is logical to consider research into more extreme hypofractionation, including single-fraction SBRT.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Stereotactic body radiotherapy (SBRT)
- Prostate cancer
- Prospective trials
- Dose escalation
- Hypofractionation
Evidence is building to support the use of stereotactic radiotherapy in the management of localised prostate cancer. However, a large number of uncertainties remain, highlighting the need for further prospective trials. This chapter will consider ongoing prospective trials which may influence the future of SBRT in localised prostate cancer. Eighty two trials have been identified following a search of http://clinicaltrials.gov and www.isrctn.com most recently performed in December 2017, using search terms: prostate SBRT; prostate stereotactic; prostate hypofractionation; prostate CyberKnife; prostate focal radiotherapy; and prostate dominant lesion. Trials investigating SBRT for reirradiation or in the preoperative or salvage radiotherapy setting have been excluded, and are not discussed within the scope of this chapter. The larger/most relevant remaining trials are summarised in Tables 14.1, 14.2 and 14.3.
14.1 SBRT in Low- and Intermediate-Risk Prostate Cancer
There is now a wealth of published data from non-randomised studies demonstrating the efficacy and safety of SBRT in low- and intermediate-risk prostate cancer, to be consistent with standard treatment modalities. However, many of these studies are retrospective in nature, and often with short follow up at the time of publication, making it difficult to draw accurate conclusions. Ongoing prospective trials therefore remain vital in this setting. There are a large number of ongoing non-randomised trials evaluating SBRT as monotherapy for low- and intermediate-risk patients. The majority of these are single-arm studies, delivering SBRT in five fractions most commonly at a prescribed uniform dose of 36.25 Gy (range 35–40 Gy) to the PTV. The larger of these studies with an expected accrual of at least 50 patients, are summarised in Table 14.1. Other trials evaluating the use of dose escalation and more extreme hypofractionation will be discussed later in this chapter.
In terms of multicentre trials, the phase II trial by Meier et al. [21] has completed accrual and has recently published 5 year outcomes in abstract form [22]. Over 300 low- and intermediate-risk patients were treated using CyberKnife with a prescription dose of 36.25 Gy in five fractions, aiming to deliver 40 Gy to the prostate. Results were encouraging demonstrating biochemical progression-free survival (bPFS) of 97.1% and low toxicity rates with no grade 3 gastrointestinal (GI) and 2% late genitourinary (GU) toxicity. Within the SMART trial [24] linac-based techniques were used, delivering a dose of 37 Gy in five fractions prescribed to the PTV. Results published this year at 27.6 months median follow up, demonstrated grade 3 late GI toxicity in one patient, and no grade 3 acute or late GU toxicity [25]. The Florida Robotic Radiosurgery Association are conducting a prospective observational trial involved a multi-institutional registry for prostate cancer SBRT, expecting to recruit 3000 patients [28]. The primary aim of this large study is to determine overall survival at 5 years follow up.
The number of current trials delivering SBRT using CyberKnife or linear accelerator are relatively equal. Linac-based techniques offer advantages in terms of treatment time and patient accessibility, however, it is unclear whether the choice of platform contributes to beneficial treatment outcomes. Lukka et al. were due to open a randomised trial in 2015 to compare SBRT in low/intermediate prostate cancer delivered with CyberKnife or with volumetric modulated arc therapy (VMAT) [9]. The primary objective is to assess patient acceptability of the trial, aiming to recruit 40 patients, although according to the clinicaltrials.gov listing, the recruitment status is currently unknown.
There are a variety of image guidance techniques employed within the trials (Table 14.1). Some of the linac-based trials include intra-fraction tracking of prostate motion using Calypso electromagnetic beacons [24, 26, 55]. Lagerwaard et al. are using stereotactic MR-guided adaptive radiation therapy (SMART) within a phase II trial, involving daily plan re-optimisation. In an interim analysis of 16 patients, they demonstrated that plan reoptimisation improved sparing of the rectum and bladder from high doses in around 20% of fractions [81]. A few trials have included the use of injectable rectal spacers or endorectal immobilisation devices in an attempt to reduce prostatic motion and improve rectal dosimetry. Kang et al. are comparing these techniques in a randomised trial, aiming to evaluate differences in toxicity rates [14].
14.2 Comparing SBRT with Standard Treatment
Ultimately, large randomised trials are required to directly compare prostate SBRT outcomes with conventional treatment modalities and fractionation. The Prostate Advances in Comparative Evidence (PACE) trial is an international, multicentre, phase III trial, sponsored by the Royal Marsden Hospital, consisting of two randomisation groups [1]. Within PACE A, low- and intermediate-risk patients are randomised between surgery with radical prostatectomy, and SBRT; or in PACE B randomised between SBRT and conventionally fractionated radiotherapy (Fig. 14.1). All patients are treated without androgen deprivation therapy (ADT). In keeping with the majority of published trials, SBRT patients are treated with 36.25 Gy in five fractions prescribed to the PTV, ensuring 40 Gy to the CTV, delivered with either CyberKnife or Linac based techniques. In the conventional radiotherapy arm, patients are treated with 78 Gy in 39 fractions or 62 Gy in 20 fractions, following publication of the CHHIP trial data in 2016 demonstrating moderate hypofractionation to be non-inferior to conventional fractionation [82]. Patients will be followed up over 10 years and be assessed with PSA, clinician reported measures of acute and late toxicity (CTCAE, RTOG) and patient reported quality of life scores (IIEF, Vaisey, IPSS, EPIC).
Given the difficulties of a surgery versus radiotherapy randomisation, PACE A recruitment has been lower than anticipated. As a result, the primary endpoint of this group has been changed from biochemical disease-free survival (bDFS) to a quality of life endpoint, in order to reduce the recruitment target to 234. In contrast PACE B has recruited exceptionally well, having opened in 40 centres in UK, Ireland and Canada. It has now closed to accrual, having reached the recruitment target of 858 patients by the end of 2017.
Four other randomised trials have been identified, comparing five fraction SBRT with conventionally fractionated or moderately hypofractionated EBRT. A small Hong Kong based phase II trial led by Poon, et al., is currently recruiting low- and intermediate-risk patients within the Asian population [6]. Randomisation is between IMRT 78 Gy in 38 fractions and SBRT 36.25 Gy in five fractions, with a primary outcome measure of health-related quality of lie (QOL) at 1 year. HEAT [4] is a multicentre randomised trial from the US which opened in 2013, hoping to recruit 456 patients to determine whether SBRT 36.25 Gy in five fractions is non-inferior to 70.2 Gy in 26 fractions in terms of biochemical or clinical failure rate at 2 years. A further US trial led by Ellis et al. which has yet to recruit will compare SBRT in five fractions and IMRT in 28 fractions with the aim of demonstrating superiority of SBRT in terms of GU/GI toxicity [5]. Early results from The RTOG 0938 trial by Lukka et al., have been published in abstract form in 2016 [2, 3]. 255 patients with low risk prostate cancer were randomised between SBRT, 36.25 Gy in five fractions or a hypofractionated dose of 51.6 Gy in 12 fractions. Both fractionations were well tolerated in terms acute and late toxicity, and patient-reported bowel and urinary outcomes at 1 year.
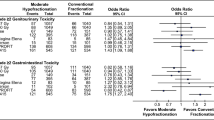
Although not strictly SBRT, HYPO is Scandinavian-based phase II randomised multicentre trial, comparing a highly hypofractionated schedule of 42.7 Gy in seven fractions on alternate days, with conventional fractionation (78 Gy in 39 fractions) [7]. Recruitment is now closed having accrued 1200 patients with intermediate-risk prostate cancer (stage T3a disease also permitted). Treatment delivery was with either 3D conformal radiotherapy or VMAT, without the use of concomitant ADT. Two-year acute and late toxicity data has been published with a median patient follow up of 4.2 years [83]. No significant difference in toxicity was found between the two arms at 2 years follow up, which included 866 patients. RTOG ≥ grade 2 urinary toxicity was 5.4 and 4.6% for the hypofractionated and conventional arms respectively, and bowel toxicity 2.2 versus 3.7%. In results presented at ESTRO (2018) ultra hypofractioanted schedule was shown to be non-inferior to conventional fractionation at 5 years, in terms of freedom from biochemical or clinical failure, with no significant difference in toxicity rate at 4 and 6 years.
LDR brachytherapy is a standard treatment option for suitable patients with low- and intermediate-risk prostate cancer. This is being compared to SBRT within a small randomised trial based in Finland (BRAVEROBO), now closed to recruitment [8]. Patients are randomised between LDR brachytherapy using I125 seeds, and SBRT 36.25 Gy in five fractions. The primary aim of this study is to detect any differences in acute and late toxicity between the two groups.
14.3 High-Risk Patients
Currently, there is limited data regarding the use of SBRT in high-risk prostate cancer, defined within the National Cancer Care Guidelines (NCCN) as patients with at least one high-risk feature: Gleason 8–10; clinical stage ≥T3a; or PSA >20 ng/ml [84]. Concerns about achieving adequate coverage or potential increased toxicity may have deterred the development of SBRT in this group given the higher risk of disease outside the prostate. Only a few published SBRT studies involve a mixed population which include a small percentage of high risk patients. The pooled multi-institutional analysis of 1100 patients by King et al. was encouraging, demonstrating 81% 5 year bPFS in the high-risk group which made up 11% of the population [85].
Four randomised trials have been identified, which include the delivery of prostate SBRT as monotherapy in high risk patients, all using a dose of 36.25 Gy in five fractions to the PTV (see Table 14.1). The ASSERT trial, which is a Canadian multi-centre trial, aims to compare toxicity from SBRT with a more conventionally fractionated schedule of 73.68 Gy in 28 fractions, in intermediate- and high-risk patients [15]. Table 14.3 summarises ongoing non-randomised trials involving high-risk patients. Of the 20 trials listed, eight have been identified delivering SBRT in five fractions to the prostate alone, where specified at a dose of 35–50 Gy. In some studies, this includes the delivery of a simultaneous integrated boost (SIB) to intraprostatic lesions. Four studies include a mixed group of low-, intermediate- and high-risk patients [59, 62, 63]. Nickers et al., are aiming to determine toxicity in the elderly population. In this trial, low- and intermediate-risk patients are treated at a dose of 36.25 Gy in five fractions which is increased to 37.5 Gy for high risk patients [63].
The largest trial specifically evaluating efficacy and safety of SBRT in the high-risk group, is a multicentre trial phase II trial led by King et al. [69]. They expect to recruit 220 patients, delivering SBRT to the prostate at a dose of 40 Gy in five fractions over 2 weeks. Concomitant androgen deprivation therapy (ADT) and SBRT to the pelvis using a dose of 25 Gy in five fractions, are given at the discretion of the treating clinician. Preliminary results have been published in abstract form in 2017 [70, 71]. Seventy three patients had been treated with a median follow up of 13.8 months. 32% received nodal irradiation and 63% received androgen deprivation therapy (ADT). Overall treatment was well tolerated with no grade 3 GU or GI toxicity seen. 2.7% had evidence of biochemical failure however longer follow up is required to evaluate the efficacy of treatment. The use of ADT or nodal irradiation did not appear to have a significant effect on toxicity, although numbers are too small to draw any conclusions about this. Trials investigating the use of ADT and pelvic SBRT will be discussed later in the chapter.
14.4 Dose Escalation
Dose escalation has been shown to improve biochemical disease-free survival and delay the need for systemic therapy following conventionally fractionated radiotherapy [86,87,88]. Pollack et al. demonstrated higher rates of freedom from biochemical failure and distant metastases in intermediate- and high-risk patients receiving 78 Gy compared to 70 Gy in 2 Gy fractions [87, 89]. Retrospectively collected data by Zelefsky et al., suggest that doses as high as 86.4 Gy are associated with improved outcomes in high-risk patients, even in combination with hormones [88]. However, any benefit from dose escalation does is likely to come with the disadvantage of increased toxicity [86, 87].
Potters et al., have completed accrual to a phase I study evaluating the tolerability of SBRT dose escalation in low- and intermediate-risk prostate cancer [38]. The study has been designed to recruit 7–15 patients to each of three dose levels: 40 Gy in five fractions, 45 Gy in five fractions, and 50 Gy in five fractions, escalating to the next dose level if no dose limiting toxicity (DLT) after 90 days in the first seven patients enrolled to a specific dose level. Acute toxicity results from the first two dose levels have been published in abstract form [39, 40]. Twelve patients received 40 Gy in five fractions and ten patients 45 Gy in five fractions. Acute grade 2 (CTCAE v3) GU toxicity was seen in 42 and 50% of patients in each dose level respectively, with no grade 3 toxicity and no ≥ grade 2 GI toxicity. Based on these results the dose was escalated to 50 Gy, the results of which are awaited.
There is not a clear argument for escalating to this dose level, particularly in low risk patients. Studies suggest prostate cancer to have an α/β ratio of <2, lower than that of the surrounding normal tissues and hence sensitive to hypofractionation [90,91,92]. Even assuming an α/β of 2, an SBRT dose of 36.25 Gy in five fractions has a biologically effective dose (BED) of 168, which is higher than 78 Gy in 39 fractions (BED 156), but has a slightly lower BED (124 vs. 130) in terms of late rectal toxicity, assuming an α/β of 3. Escalating the SBRT dose to 50 Gy in five fractions markedly increases the tumour BED to 305 but at the cost of increasing normal tissue BED to 216, hence increasing the risk of significant rectal toxicity. Dose escalation to 50 Gy has previously been evaluated by the Timmerman group who demonstrated significant toxicity in patients receiving higher dose [93, 94]. Over 6% of patients developed high-grade GI toxicity (≥ grade 3), including five patients who required a colostomy.
Heterogeneous planning techniques could enable dose to be escalated in areas not adjacent to sensitive structures. The PACE trial aims to cover at least 95% PTV with the 36.25 Gy prescription dose while delivering 40 Gy to at least 95% CTV [1]. The technique used by Stephans et al., involves the creation of a high dose PTV (HDPTV) which includes PTV > 3 mm from either urethra, bladder or rectum, and a low dose PTV (LDPTV) which includes PTV within 3 mm of these structures. 36.25 Gy in five fractions is prescribed to the LDPTV, and 50 Gy in five fractions to the HDPTV [59,60,61]. At 15 months follow up, treatment was well tolerated with low rates of acute and late toxicity in a cohort of 54 patients, of which 30 were high-risk [61]. One patient suffered grade 4 GU and GI toxicity due to prostatic infection, but did have particular risk factors of uncontrolled diabetes and very large prostate (>200 cc). Biochemical failure was seen in four patients (7.4%), all of which were in high-risk group.
Limiting dose escalation to the area of probable disease within the prostate could minimise toxicity and potentially improve efficacy, particularly since there is evidence from retrospective studies that local recurrence following radiotherapy occurs at the site of the primary tumour [95, 96]. In a study of 124 patients with MR imaging pre- and post-radiotherapy, Arrayeh et al. demonstrated the site of the dominant recurrent tumour to be in the same location as the original dominant tumour in eight of the nine patients with disease recurrence [96]. Recently reported results from the FLAME phase III demonstrate no significant increase in toxicity up to 2 years from combining an integrated boost up to 95 Gy to MRI-defined tumour with fractionated radiotherapy 77 Gy in 35 fractions to the entire prostate [97]. Aluwini et al., have previously reported their experience of using SBRT to apply a focal boost to MRI visible tumour [98]. Fifty patients were treated using CyberKnife at a dose of 38 Gy in four fractions, delivering an integrated boost to 14 patients with a dominant tumour nodule visible on MRI, to a mean dose of 47.8 Gy. 6% grade 3 late GU and no grade 3 GI toxicity overall, was reported at 23 months median follow up. Although the number of patients receiving the tumour boost was very small, no increase in toxicity was reported in this group.
Ongoing trials are evaluating the delivery of a simultaneous integrated boost (SIB) in five fractions. Fiveash et al. (RAD 1203) [41] have recruited 25 low/intermediate risk patients to a pilot trial primarily evaluating early toxicity from SBRT with integrated boost to the area in the prostate most likely to be harbouring disease. 36.25 Gy is prescribed to the whole prostate with an integrated boost of 40 Gy in five fractions. Six trials have been identified which aim to deliver a SIB to dominant lesions within the prostate, as defined by magnetic resonance imaging (MRI) [42, 44, 45, 66,67,68]. Four of these are currently recruiting. In the intermediate risk setting, Zelefsky et al. are conducting a phase I feasibility study, treating the whole prostate with 40 Gy in five fractions and applying a SIB of 45 Gy [44]. The SPARC trial which includes intermediate and high risk patients, aims to boost dominant tumour nodules up to 47.5 Gy in five fractions, while delivering 36.25 Gy to the prostate and proximal SV [67]. The primary outcome measure is acute GU toxicity up to 12 weeks post SBRT. In the phase I part of a study led by Herrara et al. in Switzerland, 36.25 Gy is given to the prostate, and the SIB dose is escalated from 45 Gy up to 50 Gy in five fractions, to determine the maximum tolerated dose [66]. Within phase II, patients are treated at the highest tolerated dose in order to determine rate of ≥ grade 2 acute toxicity (CTCAE v 4.0).
Ritter et al. use IMRT to combine urethral-sparing, and SIB techniques in a non-randomised phase I/II study, expecting to recruit 160 intermediate/low risk patients [45]. Patients that undergo a pre-treatment MRI are treated with 40 Gy in five fractions on alternate days to the prostate, with the dose to urethra, anterior rectal wall and bladder base limited to 36.25 Gy. A SIB of 42.5 Gy–45 Gy is delivered to MRI defined prostatic lesions. Patients unable to have a MRI are treated with a uniform dose of 36.25 Gy in five fractions. In an analysis of the first 16 patients, the SIB approach was found to be feasible in the ten patients able to undergo MRI [46]. At 8 months median follow up, there was no reported grade 3 or 4 toxicity, and only two patients with grade 2 acute urinary symptoms, although it is not reported which technique these patients were treated with.
14.5 Overall Treatment Time and Fractionation
The effect of overall treatment time in prostate SBRT is not yet known. Published and ongoing trials differ, with many using at least alternate day fractionation schedules. There is however no clear evidence that treating on consecutive days is detrimental, and either consecutive or alternate day fractionation is permitted with the PACE trial. Two multicentre randomised trials are evaluating the influence of weekly fractionation in comparison to alternate day fractionation. The Canadian-based PATRIOT trial has recruited 152 low- and intermediate-risk patients to receive prostate SBRT 40 Gy in five fractions, randomising between treatment over 11 or 29 days [10]. Toxicity (RTOG) and QOL (EPIC) results have been reported at median follow up of 13.1 months [11]. The 29-day arm was found to be superior in terms of patient-reported acute bowel and urinary toxicity, although no significant difference in late toxicity was found between the two schedules. A similar European trial by Mirabell et al. has also completed recruitment, randomising patients from all risk groups to receive 36.25 Gy in five fractions in either 9 days or 28 days [16].
Since prostate cancer is thought to have a low alpha/beta ratio, and therefore particularly sensitive to larger fraction size, the logical next step is to investigate the use of more extreme hypofractionation.
SBRT delivery using a dose of 38 Gy in four fractions has previously been reported [98, 99]. In two large trials led by Fuller et al., SBRT with CyberKnife is delivered at a dose of 38 Gy in four fractions, using a heterogeneous planning technique to emulate HDR brachytherapy [47, 50]. Five year outcomes from the multicentre trial have recently been published in abstract form, having completed accrual of 259 patients [48]. 100% bPFS was demonstrated in low risk patients and 88.5% in intermediate risk. 3% grade 3 GU toxicity and one case of grade 4 GU toxicity were demonstrated and although obstructive GU and GI QOL was similar to baseline, 10% urinary incontinence was detected compared to 2% at baseline. The second study continues to recruit, aiming for an accrual of 258 patients. Five year outcomes have been reported after treating 79 patients, demonstrating bPFS of 98% and 92% in low and intermediate risk patients respectively. Toxicity was acceptable although 6% late grade 3 GU toxicity was reported [51].
High-dose-rate brachytherapy (HDR-BT) delivered in either three fractions of 10.5 Gy or two fractions of 13 Gy, has been shown by Hoskin et al. to have acceptable rates of biochemical control and toxicity at 3 years post treatment [100]. Within the SBRT setting, recruitment is ongoing to an Italian-based phase I/II trial (eHYPO) investigating the tolerability and efficacy of three fraction SBRT, at a total dose of 40 Gy delivered on alternate days [54]. SBRT delivery is with VMAT using cone-beam CT (CBCT) with fiducial markers for image guidance, and includes insertion of rectal gel spacer and urinary catheter to aid accurate urethra delineation. In the 2STAR trial led by Loblaw et al., 26 Gy in 2 weekly fractions is given, aiming to determine QOL at 5 years [52].
At the most extreme, Hoskin et al. have also demonstrated acceptable levels of toxicity after single dose HDR-BT, although did note higher rates of urinary toxicity compared to a two fraction schedule, and in those patients treated with 20 Gy compared to a 19 Gy single-fraction [101]. Single fraction SBRT is currently being assessed in a phase II randomised control trial (PROSINT) led by Greco et al. in Portugal [12]. Using a urethral-sparing planning technique, intermediate-risk patients are randomised to receive SBRT with either 45 Gy in five fractions, or a 24 Gy single fraction. SBRT delivery is with VMAT, using rectal balloon immobilisation and urethral catheter loaded with beacon transponders for tracking. The accrual target is 30 patients, primarily to determine toxicity up to 5 years post treatment. In addition, a diffusion-weighted MRI is performed 15 min after the first treatment to determine early physiologic changes, and biopsy performed 2 years post treatment to evaluate pathologic response. A further single–arm trial (ONE-SHOT) by Zilli et al., was due to open in 2017 [55]. Using similar image guidance and planning techniques, they aim to deliver 19 Gy in one fraction to the prostate and proximal SV, and 17 Gy to the urethral planning risk volume (PRV).
14.6 Combining SBRT Boost with Conventional Radiotherapy
There is randomised trial evidence that an HDR-brachytherapy boost combined with EBRT can improve relapse-free survival compared with EBRT alone in intermediate- and high-risk prostate cancer [102]. Based on this data a number of trials are evaluating dose escalation using SBRT as a boost to the prostate in addition to conventionally fractionated EBRT. There is substantial variation in study design and SBRT dose used within these trials. In three trials treatment is allocated based on risk group. In a multicentre trial by Mantz et al. aiming for 350 patients, treatment low risk patients are treated with SBRT monotherapy, 40 Gy in five fractions, and intermediate risk patients with IMRT 45 Gy in 25 fractions over 5 weeks, followed by an SBRT boost of 22 Gy in four fractions [56]. Harsolia et al., aim to deliver 36.25 Gy in five fractions SBRT monotherapy to low/intermediate-risk patients, and 50.4 Gy in 28 fractions followed by an SBRT boost of 27.5 Gy in five fractions to high risk patients, with hormone therapy as indicated [79]. Hirsch et al., are using a three fraction SBRT boost of 21 Gy delivered following pelvic irradiation in high risk patients, combined with ADT [78]. In the BOOSTER trial the SBRT boost is given prior to EBRT and is escalated from an initial dose level of 20 Gy in two fractions to the PTV and 25 Gy to the GTV if identified [80]. Once acceptable toxicity has been established, the dose is escalated to a maximum of 24 Gy in two fractions to the PTV and 30 Gy to the GTV, with a primary outcome measure of ≥grade 3 RTOG acute toxicity rate.
Two randomised trials based in Poland aim to determine efficacy from delivery of a prostate boost using SBRT in comparison to standard fractionation. HYPOPROST is a large, multicentre trial aiming to randomise 465 patients to receive either a hypofractionated boost of 15 Gy in two fractions, or a conventionally fractionated boost of 30 Gy in 15 fractions, following IMRT to the whole pelvis using 46 Gy in 23 fractions in combination with ADT [19]. A further trial by Suwinski et al., which has not yet opened to recruitment, is due to compare conventional EBRT alone at 76–78 Gy in 38–39 fractions, with conventional EBRT 76–78 Gy in 38–39 fractions in addition to a boost of 20 Gy in two fractions given with brachytherapy or SBRT [18].
Within the BLaStM randomised trial, Pollack et al. are treating patients either with EBRT 76 Gy in 38 fractions and a SIB of 91.2 Gy in 38 fractions to the MRI defined GTV, or EBRT 76 Gy in 38 fractions preceded by a single stereotactic boost of 12–14 Gy to MRI defined GTV [20]. The primary aim of the trial is to compare the rate of pathologic complete response between the two treatment arms.
14.7 Pelvic SBRT
The role of prophylactic pelvic node irradiation remains controversial. Conventionally fractionated pelvic radiotherapy is sometimes considered in those patients at higher risk of harbouring micrometastatic disease within the pelvis, however, there is currently no conclusive evidence with regard to efficacy, and there is an associated increased risk of bowel toxicity. Ongoing trials are investigating the use of pelvic SBRT in high-risk patients. As previously mentioned, the trial for high risk patients by King et al. includes pelvic SBRT 25 Gy in five fractions to the pelvis, as directed by the treating clinician [69,70,71]. Treatment was well tolerated by the initial 23 patients who received pelvic SBRT, although median follow was short at 13.8 months [71].
In the FASTR trial, 16 high risk patients were treated with linac-based SBRT to the prostate and pelvic nodes, in combination with 12 months ADT [72, 73]. 40 Gy in 5 weekly fractions was delivered to the prostate and SV, and 25 Gy in 5 weekly fractions to the pelvic nodes. Unfortunately, the trial was terminated due to higher than expected toxicity at 6 months. There was no ≥ grade 3 acute toxicity but one patient suffered grade 3 late GU toxicity, and four patients experienced ≥ grade 3 late GI toxicity. As a result, the currently recruiting phase II trial (FASTR2) does not include pelvic SBRT and the prostate dose has been reduced to 35 Gy [64]. Possible factors contributing to the excessive toxicity include a large CTV-PTV margin of 5 mm, the use of CBCT without fiducial markers, and the inclusion of relatively frail patients within the study. Loblaw et al. have employed the same dose fractionation within the SATURN trial, delivering 40 Gy to the prostate/SV and 25 Gy to the pelvis in 5 weekly fractions, with 12–18 months of ADT [74]. In this trial, a 3 mm PTV margin has been applied to the prostate and 6 mm to the lymph nodes. Both CBCT and fiducial markers have been used for image guidance. Early results from 30 patients suggest that this schedule was reasonably well tolerated, demonstrating no ≥ CTCAE (version 3.0) grade 3 toxicity at 3 or 6 months [75]. At 6 months G2 late GI toxicity was reasonable at 6.9%, although G2 GU toxicity was 34.5% which seems high in comparison with conventionally fractioned or moderately hypofractionated pelvic IMRT as reported by Ferreira et al. [103].
Recently open to recruitment is the SPORT trial, which is a randomised trial evaluating the feasibility of SBRT in high risk prostate cancer, with or without elective nodal irradiation [17]. Thirty high-risk patients are expected to be randomised between SBRT 36.25 Gy in five fractions to the prostate and SV alone, and SBRT 36.25 Gy in five fractions to the prostate/SV in addition to SBRT 25 Gy in five fractions to the pelvic nodes. All patients are treated in combination with ADT. The primary outcomes of the study are to evaluate adequacy of recruitment rate over 2 years, acute toxicity, QOL, and the number of SBRT plans delivered as planned and on schedule. As part of the study blood, urine and prostate tissue will be taken for analysis to investigate potential predictive markers for patients at greater risk of toxicity.
14.8 Combining SBRT with Systemic Therapy
The role of androgen deprivation therapy (ADT) in combination with SBRT for localised prostate cancer is unclear. Evidence for using ADT with standard radiotherapy in low- and intermediate-risk patients is unconvincing, particularly now in the context of dose escalated radiotherapy [104, 105]. In view if this, many of the current prospective SBRT trials in this group, such as the PACE trial, do not include ADT. One exception is the multicentre trial by Tran et al., where 4 months ADT is given in combination with SBRT (36.25 Gy in five fractions) to intermediate-risk patients. Zelefsky et al., have recently commenced recruitment to a multicentre phase III randomised trial to compare SBRT alone or in combination with hormones, in intermediate-risk patients (those with only radiographic evidence of T3 disease are not excluded) [13]. SBRT is given to all patients at a dose of 40 Gy in five fractions, and patients randomised to the SBRT and hormones arm are additionally given 6 months treatment with Degaralix. The primary endpoint of the trial is to determine the number of patients with a positive biopsy at 2 years in intermediate-risk patients.
In high risk prostate cancer, there is greater evidence for the use of ADT in combination with high-dose radiotherapy, as demonstrated by results from the DART trial which supports the use of long-term ADT in these patients [106]. Where specified in currrently ongoing SBRT trials for high-risk patients, ADT is generally administered, either as mandated or at the discretion of the treating clinician (Tables 14.1 and 14.3). There is however variation in the duration of ADT given. In the ASSERT randomised trial, 6 months and 18 months ADT is given alongside SBRT for intermediate- and high-risk patients respectively [15]. In FASTR-2 the duration of leuprolide has been extended to 18 months from 12 months, as used in the initial FASTR protocol, following the reduction in SBRT dose and exclusion of pelvic node treatment as previously discussed [64, 72].
The development of novel androgen-directed therapies given in combination with LHRH analogues, have improved outcomes in castrate resistant metastatic prostate cancer [107, 108]. The next step is to evaluate any potential benefit in the adjuvant setting. The STAMPEDE trial has demonstrated a survival advantage from giving up-front Abiraterone in combination with LHRH analogues in patients presenting with advanced prostate cancer [109]. Notably, this benefit was also seen in those patients receiving radiotherapy for non- metastatic disease. The currently recruiting AASUR trial is combining Abiraterone and Apalutamide (ARN-509), with Leuprolide and SBRT to determine efficacy in very high risk localised prostate cancer [77]. Abiraterone works by inhibiting CYP17 which is an important enzyme involved in androgen production, and Apalutamide is a competitive androgen receptor antagonist. Patients begin the drug combination 3 months before SBRT, continuing for a total of 6 months.
14.9 Conclusion
SBRT research in localised prostate cancer is rapidly evolving. There is substantial evidence demonstrating SBRT to be a safe and effective treatment in low- and intermediate-risk patients, although questions remain regarding optimal technique, dose and fractionation. However, before SBRT can be internationally classified as a standard treatment option, it is vital to confirm at least equivalence with surgery and conventionally fractionated radiotherapy. Results of randomised trials such as the PACE trial are therefore eagerly anticipated.
Evidence for SBRT in high risk patients is much less developed, although the number of ongoing prospective trials in this setting is encouraging. Larger randomised trials are required to compare SBRT with conventional fractionation, and many questions remain with regard to dose, target coverage including the need for pelvic SBRT, and the potential benefit of combining SBRT with systemic therapy.
References
van As N. Prostate advances in comparative evidence (PACE). 2012. http://clinicaltrials.gov/ct2/show/NCT01584258.
Lukka H. Radiation therapy in treating patients with prostate cancer. 2011. http://clinicaltrials.gov/ct2/show/NCT01434290.
Lukka H, Stephanie P, Bruner D, Bahary JP, Lawton CAF, Efstathiou JA, et al. Patient-reported outcomes in NRG oncology/RTOG 0938, a randomized phase 2 study evaluating 2 ultrahypofractionated regimens (UHRs) for prostate cancer. Int J Radiat Oncol Biol Phys. 2016;94(1):2.
Abramowitz MP, Pollack A. Radiation hypofractionation via extended versus accelerated therpay (HEAT) for prostate cancer. 2013. http://clinicaltrials.gov/ct2/show/NCT01794403.
Ellis RE. Stereotactic body radiation therapy or intensity-modulated radiation therapy in treating patients with stage IIA-B prostate cancer. 2017. http://clinicaltrials.gov/ct2/show/NCT03367702.
Poon D. Stereotactic body radiotherpay vs intensity-modulated radiotherpay in prostate cancer. 2015. http://clinicaltrials.gov/ct2/show/NCT02339701.
Widmark A. Phase III study of hypofractionated radiotherapy of intermediate risk localised prostate cancer. 2008. https://www.isrctncom/ISRCTN45905321.
Vuolukka K. LDR brachytherapy versus SBRT for low and intermediate risk prostate cancer patients (BRAVEROBO). 2016. http://clinicaltrials.gov/ct2/show/NCT02895854.
Lukka H. Feasibility study of stereotactic body radiotherapy (SBRT) for localized prostate cancer: CyberKnife vs VMAT. 2015. http://clinicaltrials.gov/ct2/show/NCT02344667.
Ong A, Loblaw A. Prostate accurately targeted radiotherpay investogation of overall treatment time (PATRIOT). 2011. http://clinicaltrials.gov/ct2/show/NCT01423474.
Quon HC, Ong A, Cheung P, Chu W, Chung HT, Vesprini D, et al. PATRIOT trial: randomized phase II study of prostate stereotactic body radiotherapy comparing 11 versus 29 days overall treatment time. J Clin Oncol. 2015;33(Suppl 7):6.
Greco C. Phase II study of ultra-high-dose hypofractionated vs single-dose image-guided radiotherapy for prostate cancer (PROSINT). 2015. http://clinicaltrials.gov/ct2/show/NCT02570919.
Zelefsky MJ. Trial of ADT and SBRT versus SBRT for intermediate prostate cancer. 2017. http://clinicaltrials.gov/ct2/show/NCT03056638.
Kang JF. Formenti S. Randomized trial of image-guided stereotactic radiation therapy (IG-SRT) in prostate cancer. 2016. http://clinicaltrials.gov/ct2/show/NCT02911922.
Alexander AK, Kwan W. Androgen suppression with stereotactic body or external beam radiation therapy (ASSERT). 2015. http://clinicaltrials.gov/ct2/show/NCT02594072.
Miralbell R. Hypofractionated radiation therapy in prostate cancer. 2013. http://clinicaltrials.gov/ct2/show/NCT01764646.
Jain S. SPORT high-risk trial evaluating SABR in prostate cancer (SPORT). 2017 http://clinicaltrials.gov/ct2/show/NCT03253978.
Suwinski R. Conformal radiotherapy (CRT) alone versus CRT combined with HDR BT or stereotactic body radiotherapy for prostate cancer. 2013. http://clinicaltrials.gov/ct2/show/NCT01839994.
Milecki P. Comparing hypofractionated radiotherapy boost to conventionally fractionated (HYPOPROST). 2014. http://clinicaltrials.gov/ct2/show/NCT02300389.
Pollack A. Randomized MRI-guided prostate boosts via initial lattice stereotactic vs daily moderately hypofractionated radiotherAPY (BLaStM). 2014. http://clinicaltrials.gov/ct2/show/NCT02307058.
Meier R, Kaplan I, Sanda M. CyberKnife radiosurgery for organ-confined prostate cancer: homogenous dose distribution. 2008. https://clinicaltrials.gov/ct2/show/NCT00643994.
Meier R, Beckman A, Henning G, Mohideen N, Woodhouse SA, Cotrutz C, et al. Five-year outcomes from a multicenter trial of stereotactic body radiation therapy for low- and intermediate-risk prostate cancer. Int J Radiat Oncol Biol Phys. 2016;96(2):S33–S4.
Meier R, Beckman A, Kaplan I, Mohideen N, Shieh E, Henning G, et al. Stereotactic radiotherapy for organ-confined prostate cancer: early toxicity and quality of life outcomes from a multi-institutional trial. Int J Radiat Oncol Biol Phys. 2010;78(Suppl 3):S57.
Lee W. Stereotactic body radiotherapy (SBRT) for prostate cancer (SMART). 2009. https://clinicaltrials.gov/ct2/show/NCT00941915.
Boyer MJ, Papagikos MA, Kiteley R, Vujaskovic Z, Wu J, Lee WR. Toxicity and quality of life report of a phase II study of stereotactic body radiotherapy (SBRT) for low and intermediate risk prostate cancer. Radiat Oncol. 2017;12(1):14.
Spratt D. Hypofractionated stereotactic body radiation therapy (SBRT). 2011. https://clinicaltrials.gov/ct2/show/NCT01288534.
Jackson WC, Dess RT, Litzenberg DW, Li P, Schipper M, Rosenthal SA, et al. A multi-institutional phase II trial of prostate stereotactic body radiation therapy (SBRT) utilizing continuous real-time evaluation of prostate motion with patient reported quality of life. Prac Radiat Oncol. 2017;8(1):40–7.
Perman ML. Multi-institutional registry for prostate cancer radiosurgery (RPCR). 2010. http://clinicaltrials.gov/ct2/show/NCT01226004.
Tran P. Radiation and androgen ablation for prostate cancer. 2012. http://clinicaltrials.gov/ct2/show/NCT01517451.
Dunst J. Hypofractionated Radiosurgery for Localised Prostate Cancer (HYPOSTAT). 2015. http://clinicaltrials.gov/ct2/show/NCT02635256.
Jiang P, Krockenberger K, Vonthein R, Tereszczuk J, Schreiber A, Liebau S, et al. Hypo-fractionated SBRT for localized prostate cancer: a German bi-center single treatment group feasibility trial. Radiat Oncol. 2017;12:138.
Milecki P. Prospective evaluation of hypofractionated stereotactic RT using CyberKnife for patients with prostate cancer (CYBERPROST). 2017. http://clinicaltrials.gov/ct2/show/NCT03225235.
Collins S. Quality of life in patients with clinically localised prostate cancer treated with radiosurgery (PR-PROS). 2013. http://clinicaltrials.gov/ct2/show/NCT01766492.
Rashtian A. CyberKnife stereotactic radiosurgery for low and intermediate risk prostate cancer. 2014. http://clinicaltrials.gov/ct2/show/NCT02070952.
Woodhouse S. A phase II trial of CyberKnife steretactic radiosurgery to prostate tumours. 2014. http://clinicaltrials.gov/ct2/show/NCT02225262.
Chua M. Stereotactic body radiotherapy for organ confined prostate cancer. 2014. http://clinicaltrials.gov/ct2/show/NCT02313298.
Heron D. Hypofractionated SBRT for prostate cancer. 2009. http://clinicaltrials.gov/ct2/show/NCT00977860.
Potters L. SBRT for organ confined prostate cancer. 2016. http://clinicaltrials.gov/ct2/show/NCT02653248.
Ghaly M, Marrero M, Vijeh L, Montchal E, Lee L, Potters L. Phase I dose-escalation study of (SBRT) for localizes prostate cancer. Int J Radiat Oncol Biol Phys. 2012;84(3):S391.
Ghaly MV, Marrero L, Montchal E, Marrero M, Potters L. Phase I dose-escalation study of stereotactic body radiotherapy (SbRT) for organ confined prostate cancer. J Radiosurg SBRT. 2013;2(Suppl 2.1):149–50.
Fiveash J. Pilot trial evaluating stereotactic body radiotherapy with integrated boost for clinically localized prostate cancer (RAD1203). 2013. http://clinicaltrials.gov/ct2/show/NCT01856855.
Jereczek-Fossa BO, Orecchia R. Short-term high precision radiotherapy for early prostate cancer with concomitant boost on the dominant lesion. 2013. http://clinicaltrials.gov/ct2/show/NCT01913717.
Timon G, Ciardo D, Bazani A, Garioni M, Maestri D, De Lorenzo D, et al. Rationale and protocol of AIRC IG-13218, short-term radiotherapy for early prostate cancer with concomitant boost to the dominant lesion. Tumori. 2016;102(5):536–40.
Zelefsky M. Radiotherapy to the prostate and dominant intra-prostatic lesion (DIL). 2017. http://clinicaltrials.gov/ct2/show/NCT03269422.
Ritter MA. Stereotactic body radiation therapy with boost using urethral-sparing intensity-modulated radiation therapy planning in treating patients with prostate cancer. 2015. http://clinicaltrials.gov/ct2/show/NCT02470897.
Morris BA, Bayliss RAB, Anger N, Morris ZS, Ritter MA. A phase 1/2 trial of stereotactic body radiation therapy for prostate cancer with a simultaneous integrated boost to MRI-identified regions of high tumor volume (NCT02470897). Int J Radiat Oncol Biol Phys. 2017;99(2, Suppl):E255.
Fuller DB, Mardirossian G. CyberKnife radiosurgery for low and intermediate risk prostate cancer: emulating HDR brachytherapy dosimetry. 2008. http://clinicaltrials.gov/ct2/show/NCT00643617.
Fuller DB, Kane BL, Medbery CA, Underhill K, Gray JR, Peddada A, et al. 5-year outcomes from a prospective multi-institutional trial of heterogeneous dosing stereotactic body radiotherapy (SBRT) for low- and intermediate-risk prostate cancer. J Clin Oncol. 2017;35(Suppl 6):35.
Fuller DB, Mardirossian G, Wong D, McKellar H. Prospective evaluation of stereotactic radiotherapy for low and intermediate risk prostate cancer: emulating HDR brachytherapy dose distribution. Int J Radiat Oncol Biol Phys. 2010;78(3):S358–S9.
Fuller D. CyberKnife radiosurgery for localized prostatic cancer. 2010. http://clinicaltrials.gov/ct2/show/NCT01045148.
Fuller DB, Naitoh J, Mardirossian G. Virtual HDR cyberknife SBRT for localized prostatic carcinoma: 5-year disease-free survival and toxicity observations. Front Oncol. 2014;4:321.
Loblaw A. Two StereoTactic ablative adaptive radiotherapy treatments for localized prostate cancer (2STAR). 2014. http://clinicaltrials.gov/ct2/show/NCT02031328.
Nicolae A, Davidson M, Easton H, Helou J, Musunuru H, Loblaw A, et al. Clinical evaluation of an endorectal immobilization system for use in prostate hypofractionated stereotactic ablative body radiotherapy (SABR). Radiat Oncol. 2015;10:122.
Sanguineti G. A phase I-II on stereotactic body radiotherapy in 3 fractions for low/intermediate risk prostate cancer (eHYPO). 2015. http://clinicaltrials.gov/ct2/show/NCT02623647.
Zilli T. ONE-SHOT trial – Ultra-fractionated single-dose SBRT for prostate cancer. 2017. http://clinicaltrials.gov/ct2/show/NCT03294889.
Mantz C. Phase II trial of SBRT+ or -IMRT in treatment of patients with clinically confined prostate adenocarcinoma. 2015. http://clinicaltrials.gov/ct2/show/NCT02339948.
Lartigau E. Hypofractionated stereotactic boost in prostate cancer (CKNO-PRO). 2012. http://clinicaltrials.gov/ct2/show/NCT01596816.
Pasquier D, Nickers P, Peiffert D, Maingon P, Pommier P, Lacornerie T, et al. Hypofractionated stereotactic boost in intermediate risk prostate carcinoma: Preliminary results of a multicenter phase II trial (CKNO-PRO). PLoS One. 2017;12(11):e0187794.
Stephans K. High-dose stereotactic radiation for prostate cancer. 2012. http://clinicaltrials.gov/ct2/show/NCT01664130.
Kotecha R, Djemil T, Tendulkar RD, Reddy CA, Thousand RA, Vassil A, et al. Dose-escalated stereotactic body radiation therapy for patients with intermediate- and high-risk prostate cancer: initial dosimetry analysis and patient outcomes. Int J Radiat Oncol Biol Phys. 2016;95(3):960–4.
Stephans KL, Thousand R, Reddy CA, Magnelli A, Qi P, Zhuang T, et al. Heterogeneous dose-escalated prostate stereotactic body radiation therapy for all risk prostate cancer: an institutional phase 2 study. Int J Radiat Oncol Biol Phys. 2016;96(2):E243.
Meier R. Stereotactic body radiotherapy for stage I-III prostate cancer. 2015. http://clinicaltrials.gov/ct2/show/NCT02334579.
Nickers P. CyberKnife for prostate cancer patients aged 70 y or more (ProRobot). 2017. http://clinicaltrials.gov/ct2/show/NCT03235557.
Bauman GS. Fairly brief androgen suppression and stereotactic radiotherapy for high risk prostate cancer – protocol 2 (FASTR-2). 2014. http://clinicaltrials.gov/ct2/show/NCT02229734.
Loblaw A, Suneil J. Safety and efficacy study of hypofractionated radiotherapy and androgen deprivation therapy for prostate cancer (pHART8). 2012. http://clinicaltrials.gov/ct2/show/NCT01505075.
Ong A. Functional MR-guided stereotactic body radiation therapy of prostate cancer. 2013. http://clinicaltrials.gov/ct2/show/NCT01976962.
van As N. The SPARC trial: stereotactic prostate ablative radiotherapy using CyberKnife (SPARC). 2014. http://clinicaltrials.gov/ct2/show/NCT02145494.
Herrera F. A phase I-II dose escalation study of stereotactic body radiation therapy in patients with localized prostate cancer. 2014. http://clinicaltrials.gov/ct2/show/NCT02254746.
King CR. Stereotactic body radiation therapy in treating patients with localized high-risk prostate cancer. 2014. http://clinicaltrials.gov/ct2/show/NCT002296229.
Kishan AU, Fuller DB, Steinberg ML, Ramirez V, Agazaryan N, Ruan D, et al. Stereotactic body radiotherapy for high-risk prostate cancer (5 treatment days): toxicity results of a phase II trial. J Clin Oncol. 2017;35(Suppl 6):46.
Kishan AU, Fuller DB, Steinberg ML, Ramirez V, Ostendorf E, Tsai SH, et al. Stereotactic body radiotherapy for high-risk prostate cancer: preliminary toxicity results of a phase 2 trial. Int J Radiat Oncol Biol Phys. 2017;99(2):E248.
Bauman G, Rodrigues G. FASTR: fairly brief androgen suppression and stereotactic radiotherapy for high risk prostate cancer (FASTR). 2011. http://clinicaltrials.gov/ct2/show/NCT01439542.
Bauman G, Ferguson M, Lock M, Chen J, Ahmad B, Venkatesan VM, et al. A Phase 1/2 trial of brief androgen suppression and stereotactic radiation therapy (FASTR) for high-risk prostate cancer. Int J Radiat Oncol Biol Phys. 2015;92(4):856–62.
Loblaw A. SABR including regional lymph node irradiation for patients with high risk prostate cancer (SATURN). 2013. http://clinicaltrials.gov/ct2/show/NCT01953055.
Musunuru HB, D’Alimonte L, Davidson M, Ho L, Cheung P, Vesprini D, et al. Phase I/II study of stereotactic ablative radiotherapy including regional lymph node irradiation for patients with high-risk prostate cancer (SATURN): early results. J Clin Oncol. 2016;34(Suppl 2):264.
Hannan R. Stereotactic ablative radiotherapy (SABR) of pelvis and prostate targets for high risk prostate cancer. 2015. http://clinicaltrials.gov/ct2/show/NCT02353819.
Mc Bride SM. AASUR in high risk prostate cancer. 2016. http://clinicaltrials.gov/ct2/show/NCT02772588.
Hirsch A. CyberKnife as monotherapy or boost SBRT for intermediate or high risk localized prostate cancer. 2013. http://clinicaltrials.gov/ct2/show/NCT01985828.
Harsolia A, Muniruzzamon M. Evaluation of CyberKnife stereotactic radiotherapy in prostate cancer. 2013. http://clinicaltrials.gov/ct2/show/NCT02016248.
Eade T. Early investigation of high precision radiotherapy prior to commencing radiotherapy for prostate cancer (BOOSTER). 2013. http://clinicaltrials.gov/ct2/show/NCT02004223.
Lagerwaard F, Bruynzeel A, Tetar S, Oei SS, Haasbeek C, Slotman BJ, et al. Stereotactic MR-guided adaptive radiation therapy (SMART) for prostate cancer. Int J Radiat Oncol Biol Phys. 2017;99(2_supplement):E681–E2.
Dearnaley D, Syndikus I, Mossop H, Khoo V, Birtle A, Bloomfield D, et al. Conventional versus hypofractionated high-dose intensity-modulated radiotherapy for prostate cancer: 5-year outcomes of the randomised, non-inferiority, phase 3 CHHiP trial. Lancet Oncol. 2016;17(8):1047–60.
Widmark A, Gunnlaugsson A, Beckman L, Thellenberg-Karlsson C, Hoyer M, Lagerlund M, et al. Extreme hypofractionation versus conventionally fractionated radiotherapy for intermediate risk prostate cancer: early toxicity results from the Scandinavian Randomized Phase III Trial (HYPO-RT-PC). Int J Radiat Oncol Biol Phys. 2016;96(5):938–9.
Mohler JA, Bahnson RR. NCCN clinical practice guidelines in oncology: prostate cancer. J Natl Compr Canc Netw. 2016;14(1):19–30.
King CR, Freeman D, Kaplan I, Fuller D, Bolzicco G, Collins S, et al. Stereotactic body radiotherapy for localized prostate cancer: pooled analysis from a multi-institutional consortium of prospective phase II trials. Radiothe Oncol. 2013;109(2):217–21.
Dearnaley DP, Sydes MR, Graham JD, Aird EG, Bottomley D, Cowan RA, et al. Escalated-dose versus standard-dose conformal radiotherapy in prostate cancer: first results from the MRC RT01 randomised controlled trial. Lancet Oncol. 2007;8(6):475–87.
Kuban DA, Tucker SL, Dong L, Starkschall G, Huang EH, Cheung MR, et al. Long-term results of the M. D. Anderson randomized dose-escalation trial for prostate cancer. Int J Radiat Oncol Biol Phys. 2008;70(1):67–74.
Zelefsky MJ, Yamada Y, Fuks Z, Zhang Z, Hunt M, Cahlon O, et al. Long-term results of conformal radiotherapy for prostate cancer: impact of dose escalation on biochemical tumor control and distant metastases-free survival outcomes. Int J Radiat Oncol Biol Phys. 2008;71(4):1028–33.
Pollack A, Zagars GK, Starkschall G, Antolak JA, Lee JJ, Huang E, et al. Prostate cancer radiation dose response: results of the M. D. Anderson phase III randomized trial. Int J Radiat Oncol Biol Phys. 2002;53(5):1097–105.
Miralbell R, Roberts SA, Zubizarreta E, Hendry JH. Dose-fractionation sensitivity of prostate cancer deduced from radiotherapy outcomes of 5,969 patients in seven international institutional datasets: alpha/beta = 1.4 (0.9–2.2) Gy. Int J Radiat Oncol Biol Phys. 2012;82(1):e17–24.
Proust-Lima C, Taylor J, Secher S, Sandler H, Kestin L, Pickles T, et al. Confirmation of a low alpha/beta ratio for prostate cancer treated by external beam radiation therapy alone using a post-treatment repeated-measures model for PSA dynamics. Int J Radiat Oncol Biol Phys. 2011;79(1):195–201.
Vogelius IR, Bentzen SM. Meta-analysis of the alpha/beta ratio for prostate cancer in the presence of an overall time factor: bad news, good news, or no news? Int J Radiat Oncol Biol Phys. 2013;85(1):89–94.
Hannan R, Tumati V, Xie XJ, Cho LC, Kavanagh BD, Timmerman R, et al. Stereotactic body radiation therapy for low and intermediate risk prostate cancer – results from a multi-institutional clinic trial. Eur J Cancer. 2016;59:142–51.
Kim DWN, Straka C, Cho LC, Timmerman RD. Stereotactic body radiation therapy for prostate cancer: review of experience of a multicenter phase I/II dose-escalation study. Front Oncol. 2014;4:319.
Pucar D, Hricak H, Shukla-Dave A, Kuroiwa K, Drobnjak M, Eastham J, et al. Clinically significant prostate cancer local recurrence after radiation therapy occurs at the site of primary tumor: magnetic resonance imaging and step-section pathology evidence. Int J Radiat Oncol Biol Phys. 2007;69(1):62–9.
Arrayeh E, Westphalen AC, Kurhanewicz J, Roach M, Jung AJ, Carroll PR, et al. Does local recurrence of prostate cancer after radiation therapy occur at the site of primary tumor? Results of a longitudinal MRI and MRSI study. Int J Radiat Oncol Biol Phys. 2012;82(5):e787–e93.
Monninkhof EM, van Loon JWL, van Vulpen M, Kerkmeijer LGW, Pos FJ, Haustermans K, et al. Standard whole prostate gland radiotherapy with and without lesion boost in prostate cancer: toxicity in the FLAME randomized controlled trial. Radiother Oncol. 2018;127(1):74–80.
Aluwini S, van Rooij P, Hoogeman M, Kirkels W, Kolkman-Deurloo I-K, Bangma C. Stereotactic body radiotherapy with a focal boost to the MRI-visible tumor as monotherapy for low- and intermediate-risk prostate cancer: early results. Radiat Oncol. 2013;8:84.
Jabbari S, Weinberg VK, Kaprealian T, Hsu IC, Ma L, Chuang C, et al. Stereotactic body radiotherapy as monotherapy or post-external beam radiotherapy boost for prostate cancer: technique, early toxicity, and PSA response. Int J Radiat Oncol Biol Phys. 2012;82:228–34.
Hoskin P, Rojas A, Ostler P, Hughes R, Alonzi R, Lowe G, et al. High-dose-rate brachytherapy with two or three fractions as monotherapy in the treatment of locally advanced prostate cancer. Radiother Oncol. 2014;112(1):63–7.
Hoskin P, Rojas A, Ostler P, Hughes R, Alonzi R, Lowe G, et al. High-dose-rate brachytherapy alone given as two or one fraction to patients for locally advanced prostate cancer: acute toxicity. Radiother Oncol. 2014;110(2):268–71.
Hoskin PJ, Rojas AM, Bownes PJ, Lowe GJ, Ostler PJ, Bryant L. Randomised trial of external beam radiotherapy alone or combined with high-dose-rate brachytherapy boost for localised prostate cancer. Radiother Oncol. 2012;103(2):217–22.
Reis Ferreira M, Khan A, Thomas K, Truelove L, McNair H, Gao A, et al. Phase 1/2 dose-escalation study of the use of intensity modulated radiation therapy to treat the prostate and pelvic nodes in patients with prostate cancer. Int J Radiat Oncol Biol Phys. 2017;99(5):1234–42.
Roach M 3rd, Lu J, Pilepich M, Asbell S, Mohiuddin M, Terry R, et al. Predicting long-term survival, and the need for hormonal therapy: a meta-analysis of RTOG prostate cancer trials. Int J Radiat Oncol Biol Phys. 2000;47(3):617–27.
Valicenti RK, Bae K, Michalski J, Sandler H, Shipley W, Lin A, et al. Does hormone therapy reduce disease recurrence in prostate cancer patients receiving dose-escalated radiation therapy? An analysis of radiation therapy oncology group 94-06. Int J Radiat Oncol Biol Phys. 2011;79(5):1323–9.
Zapatero A, Guerrero A, Maldonado X, Alvarez A, Segundo CGS, Rodríguez MAC, et al. High-dose radiotherapy with short-term or long-term androgen deprivation in localised prostate cancer (DART01/05 GICOR): a randomised, controlled, phase 3 trial. Lancet Oncol. 2015;16(3):320–7.
Ryan CJ, Smith MR, Fizazi K, Saad F, Mulders PF, Sternberg CN, et al. Abiraterone acetate plus prednisone versus placebo plus prednisone in chemotherapy-naive men with metastatic castration-resistant prostate cancer (COU-AA-302): final overall survival analysis of a randomised, double-blind, placebo-controlled phase 3 study. Lancet Oncol. 2015;16(2):152–60.
Beer TM, Armstrong AJ, Rathkopf D, Loriot Y, Sternberg CN, Higano CS, et al. Enzalutamide in men with chemotherapy-naive metastatic castration-resistant prostate cancer: extended analysis of the phase 3 PREVAIL study. Eur Urol. 2017;71(2):151–4.
James ND, de Bono JS, Spears MR, Clarke NW, Mason MD, Dearnaley DP, et al. Abiraterone for Prostate Cancer Not Previously Treated with Hormone Therapy. N Engl J Med. 2017;377(4):338–51.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Morrison, K., van As, N. (2019). Summary of Ongoing Prospective Trials Using SBRT for Prostate Cancer. In: Zelefsky, M. (eds) Stereotactic Radiosurgery for Prostate Cancer. Springer, Cham. https://doi.org/10.1007/978-3-319-92453-3_14
Download citation
DOI: https://doi.org/10.1007/978-3-319-92453-3_14
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-92452-6
Online ISBN: 978-3-319-92453-3
eBook Packages: MedicineMedicine (R0)