Abstract
Economic burden of foodborne illness estimates is an important measure for setting policy priorities and assessing the efficacy of potential interventions. This chapter presents estimates for the health-related cost of foodborne illness in the United States. Updated models and data are used to examine illness costs across a number of dimensions. Specifically, two alternative economic models (similar to alternative approaches used by major regulatory agencies in the United States) are employed to assess total cost and cost per case estimates at the national, state, and pathogen levels.
Similar to previous studies, the approach used here integrates a replication of CDC’s illnesses model with the economic models to produce estimates that reflect uncertainty in both illness model and economic model parameters. Monte Carlo analysis is used to incorporate parameter distributions across the combined model.
I estimate aggregate economic costs for all foodborne illnesses in the United States to be $60.9 billion (90% CI, $37.2–$90.8 billion) or $90.2 billion (90% CI, $34.2–$161.8 billion), depending on model used. The corresponding cost per case estimates are $1275 (90% CI, $805–$1970) and $1887 (90% CI, $720–$3492), respectively. These costs vary substantially across pathogens and states.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
A number of methods for estimating the cost of foodborne illness have been employed both inside and outside the United States. In Chap. 6, many of these methods are described. In this chapter I present cost-of-illness estimates based on the methods employed by Scharff (2012, 2015). The Scharff approach integrates CDC estimates for incidence of illness (Scallan et al. 2011a, b) with estimates from alternative cost-of-illness models to illustrate the annual economic burden from foodborne illness in the United States. These measures are useful as metrics for prioritizing risk mitigation efforts, assessing whether given interventions are economically justified, and communicating the importance of the problem to the public.
Figure 8.1 illustrates the general approach used to estimate economic costs associated with foodborne illnesses. Essentially, a full replication of the CDC illness model (preserving all measures of uncertainty) is combined with an updated version of the economic model developed by Scharff (2012, 2015) to produce economic burden of illness estimates. The illness model provides measures for illness incidence and likelihood of disease severity. The economic model provides values for the cost of illness associated with each disease endpoint, including costs associated with secondary conditions/complications.
Below I present the basic models, describe how the models are integrated with CDC illness estimates, reveal updated estimates, and discuss the usefulness and limitations of the estimates given.
2 Cost-of-Illness Modeling
The economic cost of a case of foodborne illness theoretically includes both monetary costs and utility losses to those directly impacted by the illness and, when the illness is part of an outbreak, to others (including industry and public health entities). Though industry and public health costs are not inconsequential, the approach used here follows other cost-of-illness studies by focusing on health-related costs.
For each identified pathogen, disease outcome trees are used to determine probabilistic illness outcomes (see Chap. 6). Disease outcomes vary by illness severity, requiring different levels of medical attention and implicating different types of secondary conditions/complications that may arise as a result of the initial acute illness. For example, one person made ill due to salmonellosis may have a routine self-limiting gastrointestinal illness that resolves in 3 or 4 days, while another is hospitalized for a week and is afflicted with reactive arthritis for months following the resolution of the initial acute illness. Costs are assessed for each end node of the tree and are aggregated based on probabilistic assessments of the likelihood of each outcome.
To make the model tractable, a limited number of outcomes and secondary conditions are evaluated. For acute conditions, potential outcomes are did not seek medical care, sought medical care/saw doctor, was hospitalized, and died. For secondary conditions/complications that arise, condition-specific outcome trees are employed. Specifically, costs are assessed for Guillain-Barré syndrome (Campylobacter spp. ), hemolytic-uremic syndrome (Escherichia coli [STEC]), developmental disabilities (Listeria monocytogenes), and reactive arthritis (Campylobacter spp., Salmonella spp., Shigella spp., and Yersinia enterocolitica).
Potential measurable health-related costs from foodborne illnesses include medical costs (hospitalizations, physician services, and pharmaceuticals), lost productivity (for the person made ill or their caregiver), lost life expectancy, and lost quality of life. Though each of these cost categories is theoretically justified, many researchers have avoided using quality-of-life losses because the methods used to quantify them are controversial. For this reason, following Scharff (2012, 2015), I present two sets of estimates: one including quality-of-life losses and one excluding these losses. The first set of estimates is labeled as being from the “basic” model. The second set is from the “enhanced” model.
The basic cost-of-illness model measures the cost of a representative illness from pathogen p and is defined as
where, Hospitalp is hospitalization costs, Physicianp is physician costs (including lab fees), Pharmap is pharmaceutical costs, Prodp is productivity losses for the ill person, CProdp is caregiver productivity losses (for parents of ill children), and VSLp is costs due to premature death (using the value of a statistical life).
The enhanced model adds a monetized value for quality-of-life losses:
where QALYp is quality-of-life losses. Note that productivity losses for ill persons are not in this model. This reflects the fact that QALY losses include lost utility due to functional limitations, which likely also reflects productivity losses. By omitting Prodp the potential for double counting is eliminated.
3 Methods for Estimating Costs
The methods for estimating costs for the models displayed in Eqs. (8.1) and (8.2) are described in this section. More detailed descriptions can be found in Scharff (2012, 2015) and linked appendices. All costs have been updated to reflect January 2017 dollars and are derived for 30 identified pathogens and the broader category of unspecified agents.
Medical costs are incurred when an individual sees a doctor, is hospitalized, or buys pharmaceuticals to treat their illness. Though the existence of private and public insurance means that only portion of these costs are paid directly by consumers, ultimately all of these costs fall on consumers due to a resulting rise insurance premiums and taxes (or deficits) to fund the expenses. As a result, all medical costs are included in the analysis. Estimates for these values are obtained from several sources.
Hospital costs are a combination of hospital services and inpatient physician services. Hospital service costs are taken from the Healthcare Cost and Utilization Project’s National Inpatient Sample (NIS) (AHRQ 2016). Pathogen-specific costs are assessed by ICD-9 codes most closely related to the pathogen of interest. For example, ICD-9 code 003 specifically identifies hospitalizations due to Salmonella infections, allowing for direct assessment of salmonellosis hospitalization costs, while rarer hospitalizations resulting from infection with Clostridium perfringens are assumed to be captured by ICD-9 code 005.9 (food poisoning not otherwise specified). Costs are based on the most recent 5-year period of available data (generally 2009–2014) and are assumed to be uniformly distributed between the cost to the hospital (an underestimate of costs borne by patients/insurance) and hospital charges (an overestimate given that these charges are often negotiated down by insurance companies). Costs are updated to reflect January 2017 prices using the hospital services CPI (BLS 2017a).
Physician service costs are assessed for outpatient visits as well as emergency room and hospital inpatient visits. NIS data is used to determine the average length of hospital stays and the proportion of hospitalizations that utilize emergency room services (AHRQ 2016). Costs for each category of physician services (including lab work) are based on costs reported in a large annual physician survey (PMIC2017). Prescription drug costs reported in Scharff (2015) are updated to January 2017 prices using the prescription drug CPI (BLS 2017a).
When people become ill as a result of an infection with a foodborne illness, they are often unable to work. Productivity suffers as a result, and either wages are not paid or wages are paid to an absent employee. Either way, there is a cost to society. Costs associated with lost productivity are evaluated for workers who become ill and working parents of ill children aged 14 and younger. Following Scharff (2012, 2015) productivity losses are incurred when an adult misses work as a result of an illness and are equal to the cost of compensation for days of work missed (assuming that adults work on all weekdays except for 10 federal holidays and 10 vacation days). The percentage of adults employed reflects the most recent Bureau of Labor Statistics estimates, and the hourly cost of compensation is based on December 2016 estimates (BLS 2016, 2017b). The proportion of illnesses attributable to adults and children are based on the most recent FoodNet (through 2015) and National Disease Surveillance system (NNDSS) (through 2014) data (CDC 2015, 2016, 2017).
When people die as a result of a foodborne illness, there is a utility loss for the person who dies. To measure this loss, an age-invariant value of statistical life (VSL) measure is used. This revealed preference measure is widely used and is derived from the trade-off between mortality risk and wages (Viscusi and Aldy 2003). Estimates from Scharff (2015) are revised to include nominal income growth from 2013 to 2015 and inflation experienced between 2015 and January 2017 (BLS 2017a, Census Bureau 2016).
Quality-of-life losses not associated with death are also experienced by those who become ill as a result of foodborne illness. These are legitimate economic costs but, because markets for these losses do not exist, are more difficult to place values on. The Food and Drug Administration (FDA) provides estimates for these losses by monetizing quality-adjusted life year (QALY) losses using value of statistical life year estimates, derived from the VSL (Minor et al. 2015). Though this method is controversial, it is also more complete than more standard cost-of-illness studies, as reflected by Eq. (8.1). In the enhanced model (Eq. 8.2), economic values for quality-of-life losses are included. Scharff (2015) QALY estimates are replaced in this analysis with more recent FDA pathogen-specific estimates (Minor et al. 2015), and VSLY estimates are revised to reflect updated VSL estimates, as described above.
For several pathogens, secondary conditions or complications (sequelae) may occur as a result of the initial acute illness. These conditions may be time-limited or chronic. Though many conditions have been examined by researchers, only a few are generally accepted as being definitively tied to foodborne illness. Sequelae for which costs are derived include Guillain-Barré syndrome (Campylobacter spp.), hemolytic-uremic syndrome (STEC), developmental disabilities (Listeria monocytogenes), and reactive arthritis (Campylobacter spp., Salmonella spp., Shigella spp., and Yersinia enterocolitica). Generally, Scharff (2012) estimates are used, with cost categories updated as described above for acute illnesses.
Estimates for the economic burden of illness have also been derived at the state level (Scharff 2015). Costs, at the state level, vary due to differences in illness incidence, medical costs, employment rates, and wages (which affect both productivity losses and VSL—through the effect of income on demand for risk reduction). Consequently, state-based estimates are valuable for local policymakers who are best served by making decisions based on local information. State-specific illness incidence is estimated for illnesses caused by several pathogens (Brucella spp., Cryptosporidium spp., Cyclospora cayetanensis, Giardia intestinalis, hepatitis A virus, L. monocytogenes, Salmonella spp., STEC, Shigella spp., and Vibrio spp.) based on illnesses reported to the CDC through the NNDSS by state health departments (CDC 2015, 2016). State-specific differences for physician services, hospitalizations, employment rates, wages, and household income are assessed for all pathogens.
The Scharff (2015) state cost model is updated here in the following ways. State medical costs are updated using the most recent published geographic adjustment factors (PMIC 2017). Productivity costs are updated by using the most recent state estimates for employment and wages (BLS 2016). Finally, VSL estimates are updated using the latest state estimates for household income (Census Bureau 2016).
Uncertainty is incorporated into the model by using @Risk 7.5 to perform a Monte Carlo analysis that incorporates hundreds of measures of uncertainty; described more fully in Scharff (2012, 2015).
4 Integration with the CDC Illness Model
The economic costs for each category of illness outcomes, as described above, are of little use without knowing how likely these events are when an illness occurs. Similarly, cost estimates in the absence of illness incidence rates are of limited usefulness. Fortunately, the CDC illness model generates these estimates for each of the 30 pathogens examined in this study and a separate, larger, category for illnesses from unspecified agents (Scallan et al. 2011a, b). As illustrated in Fig. 8.1, the integration of the illness model with the economic model provides all of the elements needed to produce economic cost estimates at both per case and national levels.
To preserve the uncertainty measures in the CDC model, a full replication of the model is conducted using data and methods provided in Scallan et al. (2011a, b) (and the papers’ four technical appendices). Though this study uses @Risk 7.5 (to be compatible with the economic model), while Scallan used SAS for the empirical analyses; the resulting illness estimates are nearly identical.
CDC estimates of annual incidence of foodborne illness (generated through model replication and, where needed, adjusted to match CDC estimates) are presented in Table 8.1. More than half of all illnesses linked to a pathogen are caused by norovirus, followed by non-typhoidal Salmonella and C. perfringens . The presence of C. perfringens (a source of generally mild illnesses) near the top of the list of the most frequent sources of illness illustrates the value of economics as a means of providing severity weighted burden of illness estimates. As the results below demonstrate, the large number of C. perfringens illnesses are associated with a relatively modest economic cost. Severity differences are also apparent when illnesses are viewed in conjunction with hospitalizations and deaths. Though Salmonella is responsible for less than one fifth the number of illnesses associated with norovirus, Salmonella causes more hospitalizations and deaths than norovirus.
Significantly, of the almost 48 million foodborne illnesses that occur in the United States each year, most (over 38 million) are caused by unspecified agents. While most economic analyses have avoided placing costs on unspecified illnesses because of the difficulty in characterizing these illnesses (e.g., Hoffmann et al. 2012), the analysis used here includes values for these illnesses because failure to do so would lead to a gross mischaracterization of the health-related burden of foodborne illness in the United States. The cost estimates for these illnesses are based on the symptoms of the gastrointestinal illnesses identified through the FoodNet Population Survey, which is the basis for the unspecified illness estimates in Scallan (2011b).
Probabilities for each of the four potential acute illness outcomes (did not seek medical care, sought medical care/saw doctor, was hospitalized, and died) are assigned using data from Scallan. Probabilities for secondary conditions or complications (sequelae) are obtained from other sources, as described in Scharff (2012). In many cases, more than one outcome occurs (e.g., hospitalization followed by death) leading the sum of probabilities to exceed one. The combination of outcome probabilities with outcome costs allows for the cost of a representative case to be assessed (cost per case).
Incidence estimates from Scallan are used to estimate the total economic burden of foodborne illness. For most pathogens, incidence values can be determined using the approach shown in Fig. 8.1; inflating reported illnesses to account for underdiagnosis and underreporting. Underdiagnosis occurs because many who are made ill do not visit a doctor, many of those who seek care do not submit a sample for testing, and some samples are false positives. Underreporting occurs when a patient is correctly determined to have an infection caused by a specific pathogen, but the case is not reported to the state health department or the CDC. Underreporting is generally lowest when active surveillance is used (ten pathogens), is higher in passive surveillance systems (ten pathogens), and is highest where outbreaks are the only source of data (five pathogens) (Scallan et al. 2011a). Five pathogens (including Toxoplasma gondii and four viral agents) are not covered by any form of surveillance. Various sources of data are used to produce estimates using top-down methods (Scallan et al. 2011a). A similar method is employed for unspecified agents (Scallan et al. 2011b).
It should be noted that the Scallan estimates for illness incidence have not been updated in this analysis despite the fact that up to 7 years of new data is available for many pathogens in many data categories, including reported illnesses. Though, in many cases, observed changes in reported illnesses may reflect actual changes in the incidence rate, these changes may also reflect, at least in part, changes in underdiagnosis and/or underreporting rates. Without evidence detailing how these rates have changed, any update to incidence rates would be speculative. As a result, the analysis here is based on dated, but defensible incidence estimates combined with updated cost estimates.
5 The Cost of Foodborne Illness in the United States
The cost per case of foodborne illness for a given pathogen is the product of costs associated with specific outcomes (e.g., hospitalization) and the probabilities that each outcome occurs. The resulting expected costs for each outcome are summed across all component categories to determine the total expected cost of a typical illness. In Table 8.2, expected costs for each major outcome are illustrated for each pathogen. There is substantial variability in costs for pathogens across all categories. As expected, mild illnesses, such as those from C. perfringens , are associated with minimal costs, while more serious illnesses, such as botulism, have high costs across all categories.
The total economic cost of foodborne illness for each pathogen is derived by combining the expected cost per case with number of illnesses for each pathogen. Total costs from all foodborne illnesses are the sum of costs for all 30 specified pathogens and the larger category of unspecified illnesses.
Means and 90% credible intervals for cost per case and total cost estimates are provided for the basic model in Table 8.3. The expected cost per case (which includes medical costs, productivity losses, and mortality costs) ranges from $183 for a typical illness resulting from Bacillus cereus to $3.4 million for the (often deadly) illnesses caused by Vibrio vulnificus . Across all pathogens (and unspecified agents), the average cost of an illness is $1275, though the cost is higher ($2175) for illnesses from identified pathogens.
Aggregated across all pathogens and other unspecified agents, the basic model estimates an annual economic cost from foodborne illness of $60.9 billion. Two thirds of these costs are attributable to unspecified agents. Of identified pathogens, Salmonella has the highest social cost ($5.4 billion) due to a large number of illnesses, a relatively lengthy illness duration (affecting productivity losses), and relatively high hospitalization and death rates. Despite causing five times as many illnesses, the cost of norovirus is lower ($3.4 billion) due to shorter illnesses and a lower probability of hospitalization or death. C. perfringens, with nearly as many illnesses as Salmonella, leads to costs more than an order of magnitude smaller than Salmonella ($0.4 billion) because of very low probabilities of costly outcomes.
Cost estimates derived using the enhanced model are presented in Table 8.4. The inclusion of a measure for quality of life increases average cost per case to $1887. The largest relative increase in costs resulted from the inclusion of a cost measure for quality-of-life losses due to reactive arthritis. Consequently, Campylobacter , Salmonella , Shigella , and Yersinia costs all are substantially larger when the enhanced model is used. Conversely, the cost per case for illnesses caused by unspecified agents is only marginally higher when the enhanced model is used, increasing by only $109 (compared to a $2666 increase in the cost per case for identified pathogens). Total cost estimates mirror these effects. Inclusion of quality-of-life losses increases the economic burden of illness by almost half, to $90.2 billion.
The relative effects of different measures of burden of illness are more clearly illustrated in Figs. 8.2 and 8.3. The contributions of specified disease-causing agents (and categories of agents) vary considerably depending on which metric of burden of illness is used.
As panel A of Fig. 8.2 illustrates, the largest category of costs in the basic model are generated by unspecified agents (66%), followed by bacterial (21%), parasitic (7%), and viral (6%) pathogens. Though bacterial pathogens represent a much larger portion of costs in the enhanced model (39%), the largest cost category is still unspecified agents. Note that, due to a lower cost per case, unspecified agents make up a larger share of illnesses (80%) than costs for both the basic (66%) and enhanced (50%) models.
When illnesses of interest are limited to those from identified pathogens (panel B), norovirus makes up the bulk (52%) of illnesses, though not the bulk of the costs. In the basic economic model Salmonella is responsible for the highest proportion of costs (26%), followed by Toxoplasma gondii (18%) and norovirus (17%). In the enhanced model, the valuation of quality-of-life losses from reactive arthritis increases the share of costs associated with illnesses from Salmonella (34%) and Campylobacter (24%).
In most cases the 90% credible intervals for cost estimates have wide distributions, reflecting a large amount of uncertainty for several important model parameters. The largest single source of uncertainty in the economic model is the estimate for the value of statistical life (VSL) which is responsible for mortality costs of $27.6 billion (90% CI, $5.5–$55.0 billion). The VSL plays a large role in driving uncertainty, both because it is the source of a large portion of costs (used both in death cost and quality-of-life estimates) and because the credible interval for VSL is large, with each statistical death valued at $8.9 million (90% CI, $1.8–$16.1 million). VSL is especially influential because it is assumed that there is one true value for the parameter that, if discovered, would be applied uniformly across all pathogens. At the pathogen level, the number of illnesses is also highly variable for several sources of illness including STEC O157 (63,153; 90% CI, 17,587–149,631), Campylobacter (845,024; 90% CI, 337,031–1,611,083), and Shigella (13,254; 90% CI, 24,511–374,789) (Scallan et al. 2011a). Though these sources of uncertainty affect cost distributions for individual pathogens, the effect on the total cost of illness is muted by the fact that these distributions are independent from each other (e.g., it is less likely that high values in multiple distributions will be selected concurrently).
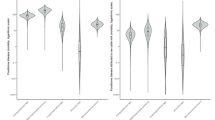
The relative role of uncertainty in the total cost estimates derived using the basic and enhanced models, respectively, is illustrated in Fig. 8.3. In panel A, the basic model total cost distribution that results from a Monte Carlo analysis of hundreds of uncertain parameter estimates is relatively narrow, with 90% of generated total cost estimates between $37.2 and $90.8 billion. For the enhanced model, in panel B, greater reliance on uncertain VSL numbers (though the use of VSLY to monetize QALYs) leads to a wider distribution of cost estimates, with 90% of estimates between $34.2 and $161.8 billion.
Efforts have also been made to evaluate costs at the state level (Scharff 2015). These estimates account for differences in incidence of illness due to differences in consumption patterns, regulatory regimes, and environmental conditions. Cost differences are also reflected in state-based figures. Tables 8.5 and 8.6 present state-specific cost-of-illness estimates using the basic and enhanced models, respectively. These updated estimates demonstrate that costs vary significantly across the states. Under the basic (enhanced) model, the average cost per case ranges from $933 ($1370) in West Virginia to $1981 ($2527) in Washington D.C. The average cost per case across all states is $1293 ($1917). Consequently, the estimates for total burden of foodborne illness are also higher when costs are first aggregated at the state level. Recognition of these cost differences allows states to tailor illness response efforts toward the needs of their residents.
Table 8.7 provides a sensitivity analysis for national burden of illness estimates. The primary approach, labeled as the “national” estimate is described in detail above. In addition, estimates based on initial aggregation at the state level (“state-based”) are provided. These have the advantage of not assuming uniform costs across the states. These are more difficult to derive, however, without having a large effect on aggregate costs. The final set of estimates (“population-adjusted”) is based on a relaxation of the assumption that illness estimates in Scallan et al. (2011a, b) are still true today. Instead, this scenario assumes that incidence rates, not illness numbers have remained steady in the decade following the data collection for the CDC study. Consequently, illnesses are assumed to grow proportionately with the US population, yielding estimates of aggregate cost that are $5 billion to $7 billion greater than “national” estimates.
6 The Use of Cost-of-Illness Estimates
Estimates of the economic cost of foodborne illness can be used in efforts to mitigate harms from foods contaminated with pathogens and other harmful agents. Risk managers seeking to improve social welfare can use these measures to help prioritize food safety efforts, evaluate interventions, and educate consumers. Essentially, cost estimates provide valuable information in an atmosphere where information is often scarce.
All food safety risk managers must make choices about where to employ their limited resources. This is true whether the manager is a decision-maker at a regulatory agency, an educator in an extension program, or a food safety manager in industry. As an aid in these efforts, managers often rely on burden of illness measures to assess where harms are greatest. This, presumably, provides some insight about where mitigation efforts are likely to have the biggest impact. In the absence of information about economic costs, burden of illness estimates are difficult to compare. For example, how might a manager compare the risk posed by C. perfringens (causing 965,958 illnesses, 438 hospitalizations, and 26 deaths) with Listeria m. (causing 1591 illnesses, 1455 hospitalizations, and 255 deaths)? Though it might appear that C. perfringens poses the larger threat due to the sheer number of illnesses, economic cost estimates suggest the opposite. The 1591 illnesses due to Listeria m. impose costs of $2.5 billion, compared to only $0.4 billion in costs from C. perfringens . Essentially, economics provides an objective means of completing the difficult task of weighting burdens based on illness severity.
The role that these estimates play in prioritizing resources is also apparent at higher levels. Legislators, department heads, and industry leaders all must decide what levels of resources to target toward food safety, as opposed to other goals. The finding that foodborne illnesses impose health-related social costs of up to $90 billion is powerful evidence that resources should be directed toward the mitigation of food safety risks. Nevertheless, it is important not to overstate the value of these estimates. While aggregate economic burden of illness estimates are useful as a means of highlighting the importance of the problem, they provide little guidance regarding whether a particular intervention is justified.
Though burden of illness estimates are insufficient as a means of evaluating intervention effectiveness, the cost per case estimates provided here can play an important role. Specifically, these estimates are used in benefit cost analyses to determine whether the costs of an intervention (or set of interventions) are justified by corresponding benefits. The estimates generated here can help improve benefit cost analyses that are often poorly calculated for major federal rules (Hahn and Dudley 2007).
A risk manager attempting to maximize social welfare would try to solve the following problem:
Essentially, the manager will choose a set of interventions with the goal of maximizing net benefits for the mix of interventions (i) used to reduce illnesses from pathogen (p). Benefits from the intervention are estimated to be the cost per case for the pathogen (CostperCasep) times the expected number of illnesses averted by the set of interventions (AvertedIllip). As long as these benefits exceed the costs of the intervention, it will improve social welfare, though, from an economist’s perspective, society will be best off when the difference between benefits and costs is greatest. In practice, the simultaneous evaluation of all potential interventions is impossible. Instead, policymakers will often be interested in knowing benefit cost ratios \( \left(\frac{{\mathrm{CostperCase}}_{\mathrm{p}}\times {\mathrm{AvertedIll}}_{\mathrm{ip}}\;}{{\mathrm{InterventionCost}}_{\mathrm{ip}}}\right) \) for a single intervention (or set of interventions) as a rough metric of return on investment. See Chap. 4 for an example of benefit cost analysis related to HACCP requirements for meat and poultry.
Economic cost estimates can also be used to educate consumers. In their roles as household risk managers, information about the economic burden of foodborne illness may influence consumers to take more care to prepare foods safely and buy foods from trusted sources. In their roles as voters, they can use the information to decide whether they support elected officials’ food safety efforts.
7 Conclusion
Foodborne illness imposes a substantial burden on the American public. Under alternative models and scenarios, the health-related cost of foodborne illness ranges from $60.9 billion to $97.4 billion or $1275 to $1917 per case. Cost per case and total cost estimates vary significantly, however, based on the pathogen causing the illness and the population affected. Total cost estimates are useful as a means of describing the burden of illness, which can be used to prioritize scarce resources. The cost per case estimates can be used as a tool for evaluating specific interventions. Nevertheless, some caution is advised when using these numbers. First, not all economic consequences are included. Costs to public health authorities and industry are omitted. Second, the illness model used is based on data that is more than a decade old. It is unclear how the incidence of foodborne illness has changed in intervening years. Third, the method used to measure quality-of-life losses (for the enhanced model) is controversial. This model is included because these types of losses are an important and theoretically justified, but the measurement technique is not universally accepted. Finally, modeling of uncertainty leads to large credible intervals for most estimates. This can lead to difficult decisions for risk managers who have to decide whether to adopt interventions that lead to potentially large, but uncertain, benefits or interventions leading to more modest, but certain, benefits. Future research aimed at ameliorating these issues would be of great value.
Abbreviations
- CDC:
-
Centers for Disease Control Research and Prevention/US
- COI:
-
Cost of illness
- CPI:
-
Consumer Price Index
- FDA:
-
Food and Drug Administration/US
- ICD-9:
-
The International Classification of Diseases, Ninth Revision
- NIS:
-
National Inpatient Sample
- NDSS:
-
National Notifiable Diseases Surveillance System
- NORS:
-
National Outbreak Reporting System
- PFGE:
-
Pulsed-field gel electrophoresis
- PulseNet:
-
National Molecular Subtyping Network for Foodborne Disease Surveillance
- QALY:
-
Quality-adjusted life year
- STEC:
-
Shiga-toxin E. coli
- VSL:
-
Value of a statistical life
References
Agency for Healthcare Research and Quality (AHRQ). HCUPnet, Healthcare Cost and Utilization Project, Rockville. 2016. https://hcupnet.ahrq.gov. Accessed 15 Feb 2017.
Bureau of Labor Statistics (BLS). May 2015 National occupational employment and wage estimates: United States, Washington. 2016. https://www.bls.gov/cpi. Accessed 17 Feb 2017.
Bureau of Labor Statistics (BLS). Consumer Price Index—all urban consumers, Washington. 2017a. http://www.bls.gov/cpi. Accessed 24 Mar 2017.
Bureau of Labor Statistics (BLS). Employer costs for employee compensation news release, Washington. 2017b. https://www.bls.gov/news.release/ecec.nr0.htm. Accessed 24 Mar 2017.
Census Bureau (Census). Current population survey, annual social and economic supplements, Washington. 2016. https://www.census.gov/did/www/saipe/data/model/info/cpsasec.html. Accessed 24 Mar 2017.
Centers for Disease Control and Prevention. (CDC). MMWR: Summary of Notifiable Diseases, Atlanta. 2015. https://www.cdc.gov/mmwr/mmwr_nd/index.html. Accessed on 12 February 2017.
Centers for Disease Control and Prevention (CDC). MMWR: Summary of notifiable diseases, Atlanta. 2016. https://www.cdc.gov/mmwr/mmwr_nd/index.html. Accessed 12 Feb 2017.
Centers for Disease Control and Prevention (CDC). FoodNet 2015 Surveillance Report (Final Data), Atlanta. 2017. https://www.cdc.gov/foodnet/reports/annual-reports-2015.html. Accessed 10 Mar 2017.
Hahn RW, Dudley PM. How well does the US government do benefit-cost analysis? Rev Environ Econ Pol. 2007;1(2):192–211.
Hoffmann S, Batz MB, Morris JG Jr. Annual cost of illness and quality-adjusted life year losses in the United States due to 14 foodborne pathogens. J Food Prot. 2012;75(7):1292–302.
Minor T, Lasher A, Klontz K, Brown B, Nardinelli C, Zorn D. The per case and total annual costs of foodborne illness in the United States. Risk Anal. 2015;35(6):1125–39.
Practice Management Information Corporation (PMIC). Medical fees 2017. Los Angeles: PMIC; 2017.
Scallan E, Hoekstra RM, Angulo FJ, Tauxe RV, Widdowson MA, Roy SL, Jones JL, Griffin PM. Foodborne illness acquired in the United States—major pathogens. Emerg Infect Dis. 2011a;17(1):7–15.
Scallan E, Griffin PM, Angulo FJ, Tauxe RV, Hoekstra RM. Foodborne illness acquired in the United States—unspecified agents. Emerg Infect Dis. 2011b;17(1):16.
Scharff RL. Economic burden from health losses due to foodborne illness in the United States. J Food Prot. 2012;75(1):123–31.
Scharff RL. State estimates for the annual cost of foodborne illness. J Food Prot. 2015;78(6):1064–71.
Viscusi WK, Aldy JE. The value of a statistical life: a critical review of market estimates throughout the world. J Risk Uncertain. 2003;27(1):5–76.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Scharff, R.L. (2018). The Economic Burden of Foodborne Illness in the United States. In: Roberts, T. (eds) Food Safety Economics. Food Microbiology and Food Safety(). Springer, Cham. https://doi.org/10.1007/978-3-319-92138-9_8
Download citation
DOI: https://doi.org/10.1007/978-3-319-92138-9_8
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-92137-2
Online ISBN: 978-3-319-92138-9
eBook Packages: Chemistry and Materials ScienceChemistry and Material Science (R0)