Abstract
The percentage of the world’s population aged over 65 is growing at unprecedented rates. Many countries face the challenge of supporting an aging population despite increasing healthcare costs, and an insufficient number of caregivers. Emerging technologies, like the Internet of Things (IoT) and Artificial Intelligence (AI), can help. Activities of daily living (ADLs) are a good indicator of healthy aging and provide a baseline for detecting an elder’s changes in physical and cognitive state. Monitoring and accurately classifying elders’ activities helps prevent and mitigate some common risks faced by elders when they age-in-place. In our study, we partnered with a senior care provider to add sensors to five apartments in an independent living facility and provided the requisite 24/7 monitoring. Ambient sensors were deployed in each of the apartments and collected high-density IoT sensor data for six months for each of the study participants, who were all over the age of 70. While we successfully created a model to classify ADLs through the recognition and observation of patterns based on high-density ambient sensor placement, sensor data and semantics, and characteristics of activities, we discovered challenges in capturing every ADL for each participant. Often, the ADLs captured for each participant offered unique and personalized indicators of healthy aging. This paper explores the challenges of deploying consumer-grade, IoT, sensors, and the application of AI technology to learn and model elders’ ADLs. We also share results of our exploration to classify ADLs in the data using manual crowd-sourcing, rule-based reasoning and machine learned analytics.
You have full access to this open access chapter, Download conference paper PDF
Similar content being viewed by others
1 Introduction
The percentage of the world population aged over 65 is growing at unprecedented rates [14]. For the first time in history, older adults outnumber children under the age of five. By 2050, 1.6 billion people will be 65 or older; in some countries, including Japan and Singapore, individuals older than 65 will constitute over forty percent of the population. According to a U.S. Census Bureau report [10], nearly 40% of older adults develop disabilities, and an even greater percentage suffer from chronic physical and mental diseases that require intensive monitoring and care.
Unfortunately, many countries face the challenge of supporting an aging population – with rising healthcare costs and a declining number of caregivers [18]. Even when considering non-professional caregivers – typically, family members – there is an insufficient number of caregivers available. Further, caring for elderly relatives is an exhausting task. According to an article published in the American Journal of Nursing [20], family caregivers have higher rates of depression, greater financial challenges, and shorter average life spans than the general population. This is a long-term societal issue with far-reaching implications that transcend industries and borders.
Emerging technologies, such as the Internet of Things (IoT) and Artificial Intelligence (AI), can enable improved care for the elderly, at a lower cost and with reduced human effort. In this paper we describe a study we conducted, partnering with a senior care provider, that explored how IoT and AI technology can be effectively applied to achieve this goal. In particular, we evaluated whether and how we can use data collected from ambient IoT sensors to learn and model individual patterns of behavior, and identify connections between, and changes in, behavioral patterns and an elder’s risk for developing cognitive or physical illnesses.
Our approach explored the use of a high-density deployment of ambient sensors in an elder’s apartment to support unobtrusive, continuous monitoring of the elder’s activities. We used AI technology over the ambient sensor data to identify the elder’s behavior patterns—and any statistically significant deviations from those patterns—and use them to prevent or mitigate some common risks faced by elders who are aging in place [16]. To minimize invasiveness and participants’ privacy concerns, this study did not include any direct observations, interviews, surveys, audio or video. This paper provides reflections on the effectiveness of a high-density deployment of ambient sensors for monitoring Healthy Aging.
1.1 Background
According to a research report by the National Conference of State Legislatures and the AARP Public Policy Institute [1], nearly 90% of people over age 65 prefer to live in their homes for as long as possible. Even as individuals begin to require day-to-day assistance or ongoing health care, 82% prefer to remain in their homes. Interestingly, the majority of Americans aim to live to be at least the age of 100 [21]. Helping people live an entire century will depend heavily on enabling this demographic to better manage life-vital decisions – health, wealth, lifestyle, and safety – as their physical and cognitive abilities naturally decline.
A common life trajectory begins with elders living unassisted in their own home or apartment. As their needs and abilities change, they may transition into an independent living (“IL”) facility. IL is defined by freedom, choice, amenities, and convenient assistance for a range of needs. There are hundreds of communities across the nation that have been specially designed to cater to retirees who are active and in good health but may require access to varying levels of senior-centered healthcare programs, assistance with home care, and a range of comforts. Residents of IL facilities typically live in independent apartments but share a common area with the other IL members. Common areas may be used for social gatherings and community activities.
Throughout the transition of living arrangements, friends and family can regularly engage with the elder, providing ongoing assistance and interaction to support prolonged quality of life. As an elder’s physical and cognitive capabilities diminish, friends, family and even the elders themselves worry about increasing risks of serious or catastrophic events. These concerns often lead elders to transition to higher levels of care.
1.2 Indicators of Healthy Aging
In the 1950s, Katz [12] developed the Index of Independence of Activities for Daily Living (ADLs) which measures an individual’s ability to live independently. ADLs are basic self-care tasks such as toileting, bathing, and transfer. Instrumental ADLs (IADLs) are complex skills required to enable an individual to successfully live independently such as shopping, food preparation, and housekeeping. Katz’s work has been widely cited and refined over the years. Today, both ADLs and IADLs have been widely adopted by the eldercare industry as key metrics for assessing changes in an elder’s physical and cognitive status over time. Medical practitioners often use ADLs and IADLs to provide a functional assessment of the individual. In fact, in the United States, ADL assessments are included in the Long Term Care Minimum Data Set (MDS) form [5] which is part of the U.S. federally-mandated process for clinical assessment of all residents in Medicare or Medicaid certified skilled nursing facilities.
1.3 Study
This study combines two streams of research. The first stream begins with Katz’s foundational research into ADLs and IADLs, which has demonstrated that activities of daily living are key to understanding how well an elder is managing aging-in-place and determining the level of care required. The second stream includes the rapidly expanding use of IoT sensors everywhere, including in the home. The sensors presence provides a previously inaccessible view into activities occurring within the home.
Specifically, the study examines various aspects of a high-density deployment of ambient sensors in residences. In particular, the ambient sensors are deployed in an independent living (IL) environment and the sensor readings are analyzed to identify ADL and IADL behavioral patterns. These patterns are then used to assess the well-being of individuals in their living environments. The ADLs behavioral patterns provide a baseline of indicators of an individual’s health that may be monitored through the aggregation of data from multiple sensors and types of sensors. The analysis sought to identify from that data the following ADLs and IADLs: (a) toileting, (b) bathing, (c) sleeping, (d) dressing, (e) mobility (transferring), and (f) cooking (kitchen activity). The insights gained ultimately might be shared with family members and care providers to proactively monitor the health and well-being of elder residents.
1.4 Study Partner
To conduct this study, IBM partnered with The Avamere Family of Companies [3]. Avamere operates nearly 50 Independent Living, Assisted Living, Transitional Care and Skilled Nursing facilities, as well as multiple ancillary healthcare companies that provide services including inpatient and outpatient rehabilitation, home care, home health, hospice, palliative care, and primary care. The Avamere facility that participated in this study comprised of 105 units of which 93 are independent living apartments and the remaining 12 are assisted living units.
1.5 Study Participants
Participation in this research study was optional. To solicit participation, residents of the Avamere IL facility met with the IL facility manager and an IBM researcher in a town hall-style meeting. In this meeting, the objective of the study was explained and any questions were answered. The majority of the questions addressed topics such as the value of the study, the data that was being collected, how the participants might benefit from this study, and privacy assurances.
Participant consent was required before any participant was included in the study. Following comprehensive explanations of the study, residents of six IL apartments opted to participate in the study. All of the participants were over 70 years old. Four of the six consenting IL apartments had a single resident; two of these apartments housed females and two were home to males. One apartment was home to two residents – a husband and wife. The sixth apartment also had two residents but this apartment dropped out of the study before any sensors were deployed for reasons unrelated to the study.
The five IL apartments that participated in the study varied in size and configuration. The smallest apartment was a 452-ft\(^2\) studio; the largest was an 1104-ft\(^2\), two-bed and one-and-a-half bath apartment. Table 1 provides details on each of the IL apartments included in the study: number of occupants, number and type of rooms, apartment size, and the number of sensors deployed.
2 Sensor System
One of the main objectives of the study was to measure the effectiveness of monitoring ADL behaviors from consumer-grade IoT sensors. The creation and deployment of the ambient sensor system at the Avamere IL facility included the following tasks: (a) evaluating the sensor ecosystems to define selection criteria, (b) exploring sensor placement for ADLs detection, (c) gathering and analyzing the streaming sensor data, and (d) installing the sensors in the IL apartments.
2.1 Sensor Evaluation Criteria
The criteria used to evaluate sensors reflect the need to gather data to detect ADLs. Specifically, sensor evaluation criteria were: (a) type of sensor data (e.g. motion, temperature, etc.), (b) programmatic access to data streams, (c) ease of configuration, (d) commercial availability, and (e) cost.
Each sensor ecosystem has a unique processing infrastructure and network connections to allow for remote access and monitoring capabilities. Each sensor connects to its ecosystem-specific cloud-hosted servers. The sensors were evaluated via test deployments conducted in the IBM Research aging-in-place environment lab in Austin, TX [13]. These test deployments provided insight into each of specified sensor evaluation criteria. The test deployments involved installation of several types of sensors from different vendor ecosystems; this allowed the team to evaluate the effectiveness of each sensor type and placement as well as differences between the various vendor ecosystems.
2.2 Sensor Placement Evaluation
An understanding of sensor performance and optimal sensor placement in the apartment is critical to the ability to detect an elder’s activities of daily living. The power of observation comes not from a single sensor signal, but from identifying ADL patterns based on modeling the aggregate of readings from multiple sensors installed in the apartment (see Sect. 4.1). Toward this end, different sensor types and placements were evaluated to determine an environment-specific placement that is effective for detecting ADLs.
In addition to the comprehensive evaluations conducted at the IBM Research aging-in-place laboratory, a three month pilot study involving 48 sensors deployed throughout the home of an 87 year old female was conducted. The environment included bedroom, bathroom, long hallway and efficiency kitchen. For this pilot study, each sensor from the different ecosystems was placed in the environment with the objective of detecting transferring, toileting and cooking ADLs.
As an example, two types of motion sensors were deployed in the pilot study: the D-Link [8] Wi-Fi motion sensor and the Samsung SmartThings [22] motion sensor. The D-Link motion sensor must be plugged into an electrical outlet, limiting its placement to the locations of existing outlets. The SmartThings motion sensor is installed by securing the sensor with adhesive tape or screws, allowing for greater flexibility of placement within the home. The D-Links were placed in the hallway outlet approximately 12 in. above the ground and the kitchen outlet approximately 4.5 ft above the ground. The SmartThings motion sensors were placed about six feet high on the bathroom walls and approximately four feet high on the walls of the bedroom and hallway. One of the discoveries from the analysis of the sensor readings was that if a motion sensor eyelet is obstructed by any object, the sensor reading becomes invalid. Greater flexibility of placement to avoid obstruction and to maintain reliable sensor readings proved valuable for detecting ADLs.
Another interesting finding from the pilot study came from the effort to detect the toileting ADL. Several sensor placements were tested, including an accelerometer fastened to the toilet flush handle, a motion sensor mounted on the bathroom wall, and the use of various sensored toilet seats. The analysis of sensor readings for the different placements revealed that not every toileting event was accompanied by a toilet flush. It was further identified that motion sensors placed on bathroom walls captured general bathroom activity but not specifically the activity of toileting.
The results of this pilot study informed both the final selection and placement of sensors in the Avamere study. Analysis of the pilot data informed sensor selection and placement and also guided optimal modification of the motion sensors to support a more accurate range of detection. For example, to overcome the potential obstruction of the sensor and enable a more accurate scanning range, it was decided to place SmartThings motion sensors on the ceiling. The SmartThings motion sensor uses passive infrared, which measures infrared light radiating from warm objects in its field of view. It has a fixed range of 10–20 ft and does not offer the ability to adjust the sensing region. However, for optimal detection, restricting motion detection to a constrained region is preferred. Consequently, it was possible to limit the sensor’s sensing region by masking all but the center most part of the sensor’s eyelet with electrical tape. (Shown on the left of Fig. 4.) Using tape to mask off the eyelet enabled a 3 ft \(\times \) 3 ft detection area when the sensor was placed on an 8ft-high ceiling. Placing the masked motion sensors on the ceiling directly above the toilet and above the center of the bed enabled better monitoring of toileting and sleeping ADLs.
2.3 Sensor Selection
The results of the test deployments identified two sensor ecosystems that met the sensor evaluation criteria and placement requirements. Both were selected to be included in the Avamere study: Samsung SmartThings [22] and Netatmo Weather Stations [15].
Samsung SmartThings. Samsung SmartThings is a smart home platform that enables sensors and other devices to help automate tasks and secure the home. SmartThings Motion sensors may be attached to fixtures such as walls and ceilings to monitor motion and temperature. They send a {motion: true} signal immediately when motion is detected and a {motion: false} signal 10 s after motion ceases. Ambient temperature is reported whenever a change of \(1^\circ \) is detected.
SmartThings Multipurpose sensors are attached to fixtures such as doors to monitor opening/closing, ambient room temperature, orientation, and acceleration. They support a magnetic contact sensor using a remote magnet often connected to a door frame opposite the sensor itself. Contact sensors send a {open: true} or {open: false} signal immediately upon sensing a change in the proximity of the remote magnet. They also detect motion via an accelerometer. Once a sensor detects motion, it sends a {acceleration: true}. It then sends one or more readings of the acceleration along each of three spatial axes (X, Y, and Z), which range from −2400 to +2400 units (32/1000 ft/sec\(^2\)). Once no acceleration has been detected for at least 10 s, an {acceleration: false} signal is sent. Ambient temperature is reported whenever a change of \(1^\circ \) is detected.
SmartThings Outlets are plugged into wall outlets to monitor and control lights, electronics, and small appliances. Once installed, the device to be controlled is plugged into an outlet provided by the SmartThings device itself. The sensor reports on/off status as well as power consumption in amperes.
SmartThings Hub wirelessly connects a wide range of wireless sensors to the internet. Users can monitor and control the connected devices through an iPhone or Android SmartThings app. SmartThings Outlets and Hub plug into an electrical outlet while all other sensors run on battery.
Netatmo. The Netatmo sensors measure various attributes of climate. Different sensors are designed for indoor or outdoor use. Netatmo Indoor Module measures temperature, humidity, pressure, carbon dioxide, and sound levels. Netatmo Outdoor Modules measure temperature, humidity, and pressure. Netatmo Indoor Module base station plugs into an electrical outlet while remote modules run on battery. Netamo modules send readings approximately every 10 min.
2.4 Sensor Installation
Prior to installing sensors into each IL apartment that elected to participate in the study, a detailed sensor deployment schematic was developed (as shown in Fig. 1) using floor plans provided by the IL facility manager. The deployment schematic served as a reference for (a) sensor procurement (b) organization for sensor preparation, (c) mapping of the sensor to install location and (d) quick reference for maintenance.
For each sensor, the deployment schematic specifies a unique short code (e.g., M1, A4, C1) and the location and range of detection within the apartment. The short code is a quick reference to an expanded code that includes specific details regarding the sensor, including the apartment in which it is deployed, the sensor ecosystem, the sensor type, location within the apartment, and more. A label sticker with the short and expanded codes was affixed to each sensor, enabling quick identification and replacement of any misplaced (e.g., fallen) sensors. The expanded label was also useful to speed the analysis of the data collected, by enabling easy organization of sensor data streams on the back-end data systems.
A home visit with each elder was scheduled prior to installation, to validate the deployment schematic and ensure that the candidate sensor locations took into consideration the resident’s home decor, furniture configuration, fire sprinklers, air vents, and other built-in infrastructure. The schematic was updated as needed. A workspace was set up to prepare the sensor for installation, which included unpacking, organizing, labeling, masking and pairing to hub or base station. The actual sensor installation took approximately 2 h per apartment.
3 Data Architecture
A data architecture is required to collect and curate data flowing across a distributed system, starting with sensor readings collected in a resident’s apartment and ending with data analytics in the cloud. The data architecture must be designed to efficiently handle the large volumes of data generated by all of the sensors. The data must be properly stored, cleaned and processed. Data visualization tools were needed to help focus the analytic on time frames of interest in the large volume of sensor data.
3.1 Data Flow
The data flow manages large volumes of data collected from sensors installed in the IL apartments. The sensors include the Samsung SmartThings sensors for measuring motion, acceleration, contact closure, and power consumption, as well as the Netatmo indoor weather sensors that measure attributes including temperature, pressure, CO\(_2\), humidity and noise levels.
As shown in Fig. 2, data flows across a distributed system. Each sensor wirelessly sends its readings to its paired Hub. Communication may also pass through one or more repeaters (e.g., SmartThings Outlets), which expand the feasible sensor-to-hub distance.Footnote 1 Samsung sensors communicate with their hub using Zigbee and ZWave; Netatmo sensors communicate using Wi-Fi. Each Hub sends all the sensor data to accounts in its ecosystem cloud managed by Avamere. The sensor data are then collected via a Node-RED application running in an Avamere account on IBM’s Cloud. Given that some sensor vendors (Samsung) “push”? sensor readings to a provided Web service, while other vendors (Netatmo) provide a “pull”? API for a service to call, there are different Node-RED scripts or “flows”? to collect all sensor data. The data are converted to a common form and stored in a database on the IBM Cloud. Then, locally written programs transfer sensor readings from both SmartThings and Netatmo clouds to a local, Microsoft SQL Server database on Avamere’s premises, where the sensor data is de-identified by another locally written, bulk “scrubber” program and finally written to a different database. After Avamere de-identified the dataset to comply with HIPAA requirements, batches of data are bulk transmitted to systems for analysis (not shown).
3.2 Data Volume
The large volume of sensor readings collected across all five apartments comprises a dataset contains 2.3 million readings and requires 2.3 GB of storage. Table 2 shows the number of sensor readings per sensor type as well as each sensor type’s representative percentage within the whole dataset. Motion sensor readings account for the bulk of the readings at approximately 47%. Temperature readings comprise approximately 29%. Accelerometer readings comprise approximately 15%.
3.3 Data Processing
Data processing cleans, aggregates and manipulates the data, producing meaningful information. The data must be cleaned including the ability to easily identify lost data readings (e.g., walked into bathroom but didn’t walk out), and to handle noisy data.
Basic descriptive statistics of the sensor data were computed, including the distribution of values, basic counts by various dimensions (e.g., by resident, by room, by sensor type, by day, by hour, by minute, etc.), sensor “on” durations, length of patient stay, daily and weekly patterns, etc.
The data for each IL apartment and each sensor are aggregated into time windows, including by minute, by hour and by day. For sensors that fire based on activity (as opposed to sensors that automatically fire at regular time intervals), the number of sensor firings were analyzed per time increment in each IL apartment to measure activity across all sensors. The heat map visualization shown in Fig. 3 provides an immediate visual summary of information. Lighter colored cells indicate fewer firings and darker colored cells indicate larger numbers of firings. For example, Fig. 3 shows a heat map of sensor firings for resident BBB. Residents’ behavior can vary day to day. This resident was quite active on some days (e.g., May 1st, May 2nd and May 5th) but was much less active on others (e.g. April 30th). Some sensors fire frequently (e.g., M1, M3 and M4) and are likely to be valuable for further analysis. Whereas, some sensors fire rarely (e.g. C2, C7, P1 and P3) and are not valuable for further analysis due to the insignificant number of readings.
3.4 Data Visualization
Visualization of the sensor activities became an essential requirement due to the large volume and variety of data collected. For this study, severals tools were developed to visualize the activities of each resident and to enable efficient analysis of the large volumes of data and locating time windows of interesting activity for analysis. One particularly valuable tool that was developed is the Topview tool (shown on the right of Fig. 4).
Topview overlays color-coded “sensing regions” on top of a background image of the IL apartment’s floor plan. It then replays streams of recorded sensor-reading events, allowing users to adjust the replay speed from 1X to 10000X. When a motion sensor turns on or off, Topview displays or hides the sensing region shape. The user sees the apartment’s floor plan, overlaid with sensor regions flashing on and off. Topview represents each sensor type using a unique letter, color and shape. Visualizing sensors streams—particularly at high speed—makes it much easier to “see” activities in the apartment than it is by looking at a spreadsheet of lifeless on/off events.
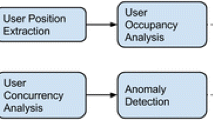
4 ADL Analytics
Activities of daily living provide useful information in the context of healthy aging. Both ADLs and IADLs are used by clinicians as good indicators of an elder’s changes in physical and cognitive status [12]. In the study, the ambient sensor data is analyzed to classify ADLs and IADLs. Models to identify patterns over time in the ADLs and IADLs were created, with the objective of identifying normal behavior and detecting any behavioral anomalies. This study focuses on six specific activities of daily living patterns: (a) toileting, (b) bathing, (c) transferring, (d) sleeping, (e) dressing, and (f) cooking.
4.1 Data Models
The data models define how ADLs, IADLs and sensor signals relate to each other and how they are classified and analyzed. The goal is to recognize and observe patterns of daily living based on ambient sensor data, sensor placement, semantics and characteristics of activities. The models are based on the practical knowledge of activities and their basic properties.
One approach to data modeling classifies ADLs and IADLs by identifying sensors as (a) highly relevant, (b) corroborating, or (c) conflicting. A highly relevant sensor is one that is required to detect the activity. A corroborating sensor strengthens confidence that the activity occurred. A conflicting sensor reduces confidence that the activity occurred. As an example, consider classifying the toileting ADL based on the IL BBB sensor deployment in Fig. 1. The ceiling sensor M8 is highly relevant to toileting because any person using the toilet will be within it’s 3ft by 3ft region of detection. The adjacent sensors R1, C9, M7, M9, and W2 in the bathroom corroborate toileting because any person using entering the bathroom will likely trigger these sensors. Lastly, the motion sensors M10, above the bed and A4, above the living room chair, are conflicting because a person is highly unlikely to simultaneously generate readings during toileting. The TV power sensor P3 is irrelevant because it may or may not be active during toileting.
4.2 Classify ADLs
Classifying ADLs is done through close examination of sensor data in the context of sensors placement in the environment. The goal is to convert sensor reading data into ADL classes. The sensor data is aggregated into time windows and a single ADL class is assigned to each time window.
Three different methods were adopted to classify ADLs: manual sensor data classification via crowd sourcing, rule-based reasoning using ADL classification model, and machine learning using Latent Dirichlet Allocation (LDA) model.
Crowd Sourcing. Similar to the deployment of sensors at Avamere prior to receiving the IL sensor dataset, a manual process was tested as the starting point for classifying sensor data from the pilot study. Human annotators assigned a single ADL class to each one minute time window, based solely on examining sensor firings in that time window. Correlation coefficients measure the degree to which each pair of annotators agreed on ADL assignments. Table 3 shows the correlation coefficients between annotator pairs from three human annotators, referred to as A, B and C. These relatively high scores provide a measure of confidence that the manual annotations are reasonably correct.
Rule-Based. Rule-based reasoning creates rules that define relationships between sensor firings and ADL classes using the classification model in Sect. 4.1. Six rules were written that correspond to the six ADLs of focus in the Avamere study. A rule begins by defining the set of conditions required for the activity, and validating the condition with corroborating and conflicting evidence. Reasonable durations of the conditions must also be satisfied. For example, the activity of bathing may have a minimum duration time set to 8 min. If all rule conditions are satisfied, the ADL class is inferred. Figure 5 shows the results of detecting the activity of bathing using rule-based method.
Latent Dirichlet Allocation. Latent Dirichlet Allocation (LDA) was originally used by the Natural Language Processing community to automatically infer a set of topics for the set of words in a given set of documents. Similar to [11, 17], LDA was applied to infer ADLs for a set of sensor readings in time windows. Each LDA identified topic (cluster) is then manually assigned to an activity based on the topic’s most frequent sensor readings.
An important input to LDA is the assumed number of topics (activities). This parameter was set to seven assuming the data contained six ADLS (toileting, bathing, transferring, grooming, dressing and eating/cooking) plus one additional “watching TV” activity. LDA detected that front door contact sensor firings were frequently concurrent with toilet ceiling motion sensor firings. It was assumed the resident often uses the toilet before leaving, and after returning to, the apartment.
While results are preliminary, six of the seven topics clearly correspond to identifiable activities; one LDA topic was not easily assignable to any activity.
4.3 ADL Pattern Detection
Discovering activities is nontrivial. ADL pattern detection is based on a set of features that measure characteristics of the ADL under observation such as the calculating activity duration, frequency, interval between, variance and outliers.
As an example, for IL BBB resident whose sensored apartment is shown in Fig. 1, the model was run over three different granularities of time in the month of May to identify ADL patterns from the classified dataset: (a) weeks in the month, (b) days of the week, (c) hours in a day.
Weeks in the Month. For IL BBB resident, a consistent ADL pattern emerged within the first few weeks of capturing sensor data; this pattern remained consistent throughout the study. This pattern is visualized in the stacked bar chart in Fig. 6.
For IL BBB resident, the activity of dressing was more challenging to detect as shown by the minimal occurrence counts. This may be due in part to the particular layout of the studio apartment and it’s lack of a designated dressing closet. Ultimately, this is a sensor placements issue as the location of the sensors or lack of sensors made it difficult to distinguish dressing from the other activities.
Days of the Week. Over the same month, the resident’s total count of each type of ADL activity is also consistent across each day of the week – including weekends; these findings are visualized in the pie charts in Fig. 7. The weekend and weekdays do not show any significant change in routine - contrary to what one may have anticipated.
Hours in the Day. The data was analyzed at the hour of the day level to understand daily activity patterns. Analyzing the data at the hourly view, daily patterns become evident – especially for specific activities such as bathing. Over the month of May, the IL BBB resident bathed every day except on 2 days, May 10th and 26th. Bathing consistently occurred between the hours of 8–9am with only two days where bathing occurred at 1pm and 4pm (Shown in Fig. 5), respectively. Over the course of May, the average duration is approximately 11 min, with a minimum of approximately 8 min and a maximum of approximately 16 min. It is evident through this analysis that the concentration of activities of daily living happen between the hours of 8–9am and 11–12pm. The model at an hourly granularity provides insight on the correlation between activities of daily living and begins to touch upon daily routines.
5 Results
ADL detection using ambient sensor data is challenging for reasons such as variation in each individual’s daily habits, sensor placement within the residence, and community amenities (e.g., using the meal plan to eat outside the apartment). We were able to successfully use ambient sensor data collected from the Avamere study participants to identify patterns – as well as anomolies – in activities of daily living. Activities of daily living are critical indicators of healthy aging. The data provides a baseline for detecting an elder’s changes in physical and cognitive state. Each resident has a unique set of strong signals – the bathing ADL pattern may be strong for one individual while sleeping ADL may be a strong pattern for a different individual. In other instances, the analysis of the correlations between several ADL patterns provides healthy aging insights.
5.1 Healthy Aging Insights
The activities of daily living patterns are key to understanding how well an elder is aging-in-place and guides the appropriate level of required care. Specifically, monitoring healthy aging requires measuring the activities of daily living against known physician or caregiver recommendations. Preliminary analysis of the data gathered from the study has shown that ADLs provide a baseline for evaluating the well-being of an elder in the context of healthy aging.
Toileting is fundamental to survival and a key indicator of an individual’s health. A consistent bathing and toileting routine is important for preventing Urinary Tract Infections (UTI) and is an indication of possible Urinary Incontinence (UI). UTI is a common cause of mortality for people over 70 years old and is often undetected [7]. Undetected UTIs can be expensive; severe infections, in which the kidneys become involved and hospitalization is required, costs can reach up to $20,000 per episode depending on the severity of the infection and length of stay [6].
By modeling bathing and toileting, it is possible to monitor an elder to ensure she is following the simple doctor recommendations of emptying her bladder every 2–3 h and bathing once a day [23]. Following these doctor recommendations can dramatically reduce the risk of a UTI, reduce the cost of care that comes from the UTI treatment and improve the quality of the elder’s life. The hourly toileting pattern for IL BBB resident is not as consistent as the daily bathing activity. For each day, the gaps in toileting tend to fall midday to early evening. However, as discussed in Sect. 4.3, the resident BBB consistently showers each day between 8am–9am, with few outliers. By monitoring these toileting and bathing patterns, a care provider can be notified of any significant changes in behavior.
Sleep is essential for cognitive performance, especially memory consolidation. People who sleep less than seven hours per night usually experience a decline in cognitive performance and changes in mood [2]. Using ambient sensors, it is possible to track sleep duration and patterns. For IL BBB resident, the high frequency sensor activity detected around 11pm indicates significant movement which may indicate that the resident is in bed but not asleep. The low sensor frequency activity in the early mornings, as detected around 4am–6am, may indicate normal sleep movement. The duration of sleep start and finish time is approximately 12am to 8am; approximately 8 h. Based on current recommendation for healthy sleeping, this meets the recommended sleep duration of greater than seven hours.
By monitoring transferring (movement), it is possible to track trends in mobility over time. A decrease in mobility is correlated with an increase fall risk. In the United States, every 11 s an Elder is treated in an emergency room for injuries associated with falling, at a cost of $31 billion a year [4]. In addition, greater sedentary time, more than 3 h, was related to an increased risk mortality in the older adults [19]. For IL BBB resident, hourly mobility was detected, with only a few days having large gaps of sedentary behavior as well as clear traversal of pathways.
Along with fall and dementia risk, a drastic decline in transferring and an increase in sedentary behavior over extended period of time is an indication of concern such as illness. Over the course of the study, the IL CCC resident had a change in ADL patterns over the first two weeks in May compared to the last two weeks as shown in Fig. 8. Bedding and transferring are similar in both ranges but the last two weeks show a substantial decrease in transferring activity. The reason for this change is unknown. However, the change in bedding and transferring activity can be used to trigger a notification to the care provider.
5.2 Future Work
Preliminary results have uncovered many obvious and exciting areas for follow-on research such as exploring new sensors and placement, classification algorithms and expanding the study to include sensor and electronic medical records from participants in a skilled nursing facility.
In the area of new sensors and placement, follow-on research will include an EarlySense [9] bed sensor that can sense heart rate, respiration rate, sleep stages, stress levels as well as movement. The sensor can be placed unobtrusively under the bed mattress.
In the area of classification algorithms, the study showed that manual classification of ADL instances is onerous and time consuming yet valuable because it forces the researcher to examine all the data– leading to new insights. Rule-based classification is faster and more efficient because it exploits tools but it is critically dependent on good rules. Machine learning methods, like LDA, can find obscure correlations that humans might miss. Follow-on research will expand the existing LDA analysis with variations in data preparation, different numbers of topics, and a rigorous comparison with the other classification methods as well as explore alternative machine learning algorithms to identify activity patterns. Also, future research will explore the application of gamification for crowd sourcing ADL classification using a visualization tool like Topview (Sect. 3.4) to reduce ADL classification costs.
Lastly, in the area of fusing sensor data with electronic medical records, follow-on research will study patients in 20 skilled nursing rooms at the Avamere facility to identify early signs for hospital readmission. This will include exploring better ways to detect ADLs such as with transferring ADL measurement capturing in traversal pace (velocity) over time.
6 Conclusion
Important insights into activities of daily living do not come from a single sensor but come from identifying patterns based on aggregation of readings from multiple sensors. These patterns describe when an elder sleeps, cooks, exercises, bathes, toilets and how often she connects with family and friends. The ability to differentiate between “normal” and “abnormal” behaviors, per unique individual, in real time, will enable profound changes in eldercare. Anomalies will trigger alerts to caregivers, and might provide early detection of problems. The Avamere study dataset has provided us with valuable input to future research studies to document evidence between certain behaviors and successful healthy aging. And based on those studies, monitoring of anomalous activity patterns can lead to early detection of afflictions, and trigger alerts to caregivers for further investigation into the elders’ well-being. This ability will certainly generate new insights that reduce risk, reduce cost of care and significantly improve the quality of life of elders.
Notes
- 1.
Repeaters increase the demand on wireless bandwidth since they receive the sensor’s inbound packet and then rebroadcast that packet a second time. The demand on wireless bandwidth must be carefully monitored and managed as the number of sensors deployed to the environment increases to prevent network congestion.
References
AARP: Aging in place: a state survey of livability policies and practices. Brief 190, AARP (2011). https://assets.aarp.org/rgcenter/ppi/liv-com/ib190.pdf
Alhola, P., Polo-Kantola, P.: Sleep deprivation: impact on cognitive performance. Neuropsychiatric Dis. Treat 3, 553–567 (2007)
Avamere, February 2016. https://www.avamere.com
Burns, E.B., Stevens, J.A., Lee, R.: The direct costs of fatal and non-fatal falls among older adults-united states. J. Safety Res. 58, 99–103 (2016)
Centers for Medicare and Medicaid Services: Minimum data set 3.0 public reports. Technical report, Centers for Medicare and Medicaid Services. https://www.cms.gov/Research-Statistics-Data-and-Systems/Computer-Data-and-Systems/Minimum-Data-Set-3-0-Public-Reports/index.html
Costhelper, February 2018. http://health.costhelper.com/uti.html
Cove-Smith, A., Almond, M.: Management of urinary tract infections in the elderly (2007)
D-link connected home, February 2018. http://shop.us.dlink.com/connected-home
Earlysense, February 2018. https://www.earlysense.com/digital-health/product/sleep-tracker
He, W., Goodkind, D., Kowale, P.: An aging world: 2015. Technical report P95–16-1, United States Census Bureau, March 2016. https://www.census.gov/library/publications/2016/demo/P95-16-1.html
Ihianle, I., Naeem, U., Islam, S.: Ontology-driven activity recognition from patterns of object use, pp. 654–657, November 2017
Katz, S., Ford, A.B., Moskowitz, R.W., Jackson, B.A., Jaffe, M.W.: Studies of illness in the aged. the index of ADL: A standardized measure of biological and psychosocial function (1963)
Keohane, S.M.: Tour the IBM “Aging in Place” Environment, December 2016. https://www.ibm.com/blogs/age-and-ability/2016/12/08/tour-the-ibm-aging-in-place-environment
Nations, U.: World population prospects: the 2017 revision. Technical report, United Nations (2017). https://esa.un.org/unpd/wpp/Publications/Files/WPP2017_KeyFindings.pdf
Netatmo, February 2018. https://www.netatmo.com
Norlander, L.: Creating healthy communities for an aging population, May 2006
Ordonez, F.J., de Toledo, P., Sanchis, A.: Activity recognition using hybrid generative/discriminative models on home environments using binary sensors. Sensors 13(5), 5460–5477 (2013). http://www.mdpi.com/1424-8220/13/5/5460
Population Reference Bureau: Aging and the health care workforce. Today’s Research on Aging, vol. 19, June 2010. http://www.prb.org/pdf10/TodaysResearchAging19.pdf
de Rezende, L., Rey-López, J., Matsudo, V., do Carmo Luiz, O.: Sedentary behavior and health outcomes among older adults: a systematic review (2014)
Schulz, R., Sherwood, P.R.: Physical and mental health effects of family caregiving, vol. 108, pp. 23–27, September 2008. https://journals.lww.com/ajnonline/fulltext/2008/09001/Physical_and_Mental_Health_Effects_of_Family.9.aspx
Sifferlin, A.: Most americans want to live to 100: Survey. Time, February 2016
Smartthings, February 2018. https://www.smartthings.com
Wegerer, J.: The connection between UTIs and dementia, July 2017. https://www.alzheimers.net/2014-04-03/connection-between-utis-and-dementia
Acknowledgments
Thanks to the Avamere Family of Companies [3] for all of their insights, hard work and valuable data throughout this project.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG, part of Springer Nature
About this paper
Cite this paper
Keohane, S.M., Gerard, S.N., Heching, A., Adams, S.S., Tarr, P. (2018). Reflections on the Effectiveness of a High Density Ambient Sensor Deployment for Monitoring Healthy Aging. In: Zhou, J., Salvendy, G. (eds) Human Aspects of IT for the Aged Population. Applications in Health, Assistance, and Entertainment. ITAP 2018. Lecture Notes in Computer Science(), vol 10927. Springer, Cham. https://doi.org/10.1007/978-3-319-92037-5_24
Download citation
DOI: https://doi.org/10.1007/978-3-319-92037-5_24
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-92036-8
Online ISBN: 978-3-319-92037-5
eBook Packages: Computer ScienceComputer Science (R0)