Abstract
Neoplastic patterns in a gastric biopsy may be subtle, and differentiating from non-neoplastic mimics may be challenging. Once a neoplastic lesion is diagnosed, further issues include identifying the key features that determine further management. They include subtyping, distinguishing invasive and noninvasive lesions and grading and phenotyping of various types of noninvasive lesions. In particular some patterns of well-differentiated gastric carcinomas are unique to the gastric mucosa. This chapter on neoplastic gastric lesions offers clues to identifying such unique patterns as well as common patterns that should not be missed with several detailed illustrations. A series of short stories will further strengthen neoplastic patterns of gastric mucosa. A practical guide of HER2 testing for gastric carcinomas is also presented.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Neoplastic lesions
- Tumour-like lesions
- Dysplastic pattern
- Glandular proliferation
- Site-specific patterns
- Non-epithelial pattern
- Biomarker testing
- Molecular testing
The most common neoplastic pattern encountered in a gastric biopsy is the “epithelial pattern” as adenocarcinomas are the most common tumours in the stomach. Lymphomas account for 5–10% of gastric malignancies. Mesenchymal tumours account for <1% of gastric tumours. However, 60–70% of gastrointestinal stromal tumours arise in the stomach. Neuroendocrine neoplasm (NENs) account for approximately 1% of gastric tumours.
The patterns related to common neoplasms are further discussed here and uncommon patterns are listed in Chap. 2.
Considering the prevalence of gastric neoplasms, the most common low-power, dominant “neoplastic pattern” on a gastric biopsy is characterised by architectural abnormalities and cytonuclear atypia (“epithelial pattern”). A standard diagnostic algorithm of biopsy interpretation is shown in Fig. 5.1. In parallel additional secondary patterns that may give clues to rare types and variants of primary gastric tumours as well as metastatic tumours should be noted (i.e. diffuse round cells, pink cell, clear cell, spindle cell, biphasic patterns).
If invasion can be definitely identified with the epithelial pattern, a diagnosis of adenocarcinoma will be established. Alternatively, in a biopsy featuring “neoplastic epithelial pattern” with no evidence of invasion, the diagnostic clues that are immediately recognised and then confirmed at higher magnification are abrupt transition, lack of surface maturation and stromal change such as inflammation. When marked cytological or architectural atypia are present, making a diagnosis of high-grade dysplasia/adenoma or even adenocarcinoma is possible. However, at times, marked epithelial atypia may be seen in non-neoplastic conditions such as a regenerative process or epithelial injury induced by chemotherapy and irradiation.
Epithelial Pattern with No Stromal Invasion
When an endoscopic biopsy of the stomach presents the glandular proliferative pattern, the approach is similar to the rest of the GIT to differentiate a non-neoplastic glandular proliferation from neoplasms. Inflammatory and hyperplastic polyps and polypoid mucosal lesions constitute the main non-neoplastic lesions. Most of these are discussed in the preceding sections in this chapter under polypoid and hyperplastic pattern.
Hamartomatous lesions introduced in Chap. 2 may involve the stomach. Polyps of Peutz-Jeghers syndrome and Cronkhite-Canada syndrome may present in endoscopic biopsies. Confirmative diagnosis may be difficult on a gastric biopsy alone. When a glandular proliferation pattern without atypia is noted in an endoscopic biopsy, endoscopic appearance should always be correlated as some syndromes may show important clues. Pancreatic heterotopia presenting as a proliferation of benign acinar structure may be recognised in biopsies.
Epithelial Pattern with Cellular Atypia: No Stromal Invasion (Intraepithelial Neoplasia)
The dysplastic glandular pattern comprises a glandular proliferation characterised by architectural abnormality of glands coupled with cytological atypia with lack of surface maturation and abrupt transition with the adjacent epithelium. Most lesions retain the glandular pattern. These lesions are called “dysplasia” (or “adenoma” if it is a polyp or nodule) or intraepithelial neoplasia (IEN) and divided into low- and high-grade categories throughout the GIT [1, 2].
Abrupt transition, lack of surface maturation and stromal change such as inflammation and absence of desmoplasia are important diagnostic clues that are immediately recognised on low-power examination and then confirmed at higher magnification.
Abrupt Transition
Abrupt transition in a biopsy fragment is a highly valuable finding for a diagnosis of gastric neoplasia. This feature is considered to represent clonal nature of the epithelium. In general, neoplastic glands are morphologically sharply demarcated from non-neoplastic gastric pits or glands, and constitutive cells are often more atypical and monomorphic compared to adjacent non-neoplastic epithelium (Fig. 5.2). This contrasts with reactive changes, which are less uniform, are not sharply demarcated and gradually transit to unremarkable neighbouring mucosa. However, it should be noted that a sharp transition can also be seen between metaplastic and non-metaplastic epithelium.
Surface Maturation
The presence of surface maturation in a biopsy is a feature that would help pathologists exclude a diagnosis of dysplasia, because dysplasia most frequently involves surface epithelium (Fig. 5.3a). In normal or most reactive processes, as the epithelium moves towards the luminal surface, the nuclei become smaller and the cytoplasm becomes larger (“maturation ”) (Fig. 5.3b). However, lack of surface maturation is not a specific feature to dysplasia, because it can also be caused by inflammation and regeneration (Fig. 5.3c). In addition, several studies reported intestinal metaplasia with basal gland atypia, which showed cytological atypia consistent with dysplasia, without surface involvement (“pit dysplasia ”) [3]. These observations suggest that early dysplastic change in chronic gastritis may be limited to the basal pit epithelium. Furthermore, some neoplastic polyps are frequently covered with non-neoplastic foveolar epithelium (i.e. oxyntic gland adenoma/polyp) [4].
Surface maturation : (a) Low-grade dysplasia/adenoma. Neoplastic cells involve the entire gland uniformly without surface maturation. (b) Reactive mucosa with intestinal metaplasia featuring surface maturation. Metaplastic glandular epithelium shows nuclear elongation in the bottom part resembling an adenoma but has smaller nuclei with a lower N/C ratio towards the surface. (c) Regenerative mucosa without surface maturation. Note that nuclear enlargement and prominent nucleoli can be seen even in the surface epithelium in early phase of regenerative process
Stromal Changes
Stromal changes , such as increased inflammatory cells, fibrosis, healed granulation tissue or haemorrhage, should also be included into consideration because these may suggest reactive aetiology. However, myxoid transformation can represent early desmoplastic changes
Dysplastic Sub-patterns
On the basis of cellular phenotype, gastric intraepithelial neoplasia can be divided into five categories forming unique patterns (Table 5.1). They are intestinal, foveolar, pyloric, oxyntic (and chief cell) and signet ring patterns. Gastric intraepithelial neoplastic lesions are intestinal-type (type I, adenomatous) dysplasia/adenoma which resemble colonic adenoma (Fig. 5.4a, b; Box 5.1), gastric phenotype including foveolar-type (type II) dysplasia/adenoma (Fig. 5.5a, b; Box 5.2) and pyloric gland adenoma (Figs. 5.6a, b and 5.7) [5, 6]. Intraepithelial neoplasia of pyloric gland type is always polypoid and therefore called pyloric gland “adenoma” (Fig. 5.7), whereas those of intestinal type and foveolar type may be polypoid or flat (or even slightly depressed). Some of these sub-patterns share similarities with those in the setting of Barrett’s neoplasia (Chap. 3).
Case 1: An 88-year-old lady presenting with constipation, bloating and recurrent iron deficiency anaemia. Abdominal CT was by her primary care practitioner revealing a mid-gastric body mass along the anterior gastric wall. Referral was made for further endoscopic evaluation. A gastroscopy note was made of a benign appearing 40 mm gastric polyp within the mid-gastric body greater curve on a short stalk (Paris Ip) (a). The polyp was resected in multiple pieces and retrieved for histopathology. The diagnosis is a pyloric gland adenoma (b)
Box 5.1 Dysplastic Intestinal Pattern (See Fig. 5.4)
-
Proliferated of intestinal (colonic)-type glands with typical pencillate hyperchromatic nuclei
-
Identical to colonic adenomas
-
MUC 2 and CDX2, always positive; MUC5AC, may be weakly and focally positive, accentuated on the surface and superficial glands; MUC6, negative
Box 5.2 Dysplastic Foveolar Pattern (See Fig. 5.5a, b)
-
Often villiform and glands featuring a frayed border with apical mucin cap, nuclei are oval or rounded and basal.
-
Resembles the foveolar epithelium closely. Resemblance is more in low-grade lesions.
-
MUC5AC, always positive; MUC 6 and MUC 2 and CDX2, variable.
Rarer neoplastic lesions of oxyntic mucosa have been recognised recently. Recent studies have recognised novel low-grade neoplastic lesions differentiating to oxyntic glandular epithelium, predominantly of chief cell type (Figs. 5.8 and 5.9; Box 5.3). This entity was first reported as “adenocarcinoma of fundic gland type” on the basis of the significant glandular architectural abnormality and frequent submucosal involvement, but subsequent studies suggested a term “oxyntic gland polyp/adenoma ” and “chief cell predominant adenoma ” for this entity because of its benign clinical nature as well as a lack of unequivocal invasion [4, 7, 8]. Another emerging dysplastic lesion associated with expansion of oxyntic compartment has been documented in the newly described genetic syndrome known as GAPPS syndrome (Fig. 5.10a) [9]. Fundic gland-type polyps with hyper-proliferative aberrant pits (HPAPs—Fig. 5.10a) progressing to dysplasia (Fig. 5.10b) and to carcinoma are described. In addition, although very rare, “signet ring cell carcinoma in situ” is considered to be a precursor of signet ring cell carcinoma, and this is usually seen in the setting of hereditary diffuse-type gastric carcinoma.
Case 2: “Oxyntic gland polyp/adenoma ” and “chief cell predominant adenoma ”. (a) This biopsy is from a small elevated lesion (about 1 cm) at the gastric body. (b) At high-power magnification, the lesion is composed of oxyntic-type glands. Looking at this for the first time, it may be difficult to interpret it as neoplastic. However, there is mild glandular architectural disarray, while cytological atypia is minimal. This is a typical example of adenocarcinoma of fundic gland-type or oxyntic gland polyp/adenoma, which has been recently recognised. (c) Endoscopic resection was performed and demonstrated the tumour showed pushing growth into the submucosa, a finding frequently seen in this type of tumour (d) Compared to normal oxyntic mucosa (right), neoplastic mucosa (left) shows a higher nuclear density and a mild nuclear enlargement of oxyntic and chief cells
Box 5.3 Oxyntic (Chief Cell Predominant) Pattern (See Figs. 5.8 and 5.9)
-
Closely packed mixture of parietal and chief cells.
-
A range of architectural patterns: clustered and or solid glands with or without well-defined lumina, anastomosing cords, dilated glands with or without infoldings, complex glands with multiple layers of cells and cribriform glands.
-
MUC6 and MUC5AC, positive; CDX2 and MUC2, negative; pepsinogen-I, positive; H-K-ATPase, variable.
-
Rarely extends to submucosa (“invasion”)—metastases have not been reported to date.
-
Terminology is controversial—reported as adenocarcinoma of fundic gland-type by Japanese authors.
Grading of Dysplasia
Low-grade dysplasia (or low-grade adenoma/IEN) has mild architectural abnormality and cytological atypia, whereas high-grade dysplasia (or high-grade adenoma/IEN) is characterised by marked cytological atypia or architectural complexity. Altered nuclear features are nuclear enlargement, elongation, stratification, loss of polarity, hyperchromasia, prominent nucleoli, increased nuclear-to-cytoplasmic ratio, increased mitoses and atypical mitoses. Architectural abnormalities may include branching, crowding, irregular shapes, villiform or papillary structures. However, if pronounced these changes in addition of budding and cribriforming become diagnostic of intramucosal adenocarcinoma. Of note, phenotypic characteristics of dysplastic sub-patterns get blurred in higher-grade lesions.
The distinction between low grade and high grade in a gastric biopsy is important, because the management will be different. Higher-grade lesions usually need treatment by endoscopic mucosal resection or submucosal endoscopic dissection, while low-grade lesions can be followed by endoscopy and biopsies. Unfortunately, grading is not a perfect marker for the risk of progression to adenocarcinoma due to lack of uniform diagnostic criteria resulting in interobserver disagreement. There is also limited data of natural history of dysplastic lesions. Tumour heterogeneity plays a role too [10, 11].
There are differences between Japan and Western countries in the interpretation of biopsies of intraepithelial neoplasia [12]. Invasion into the lamina propria and architectural complexity (irrespective of invasiveness) are the essential features of intramucosal adenocarcinoma according to Western criteria, but cytonuclear atypia is considered of paramount importance for the diagnosis of adenocarcinoma in Japan. Consequently, intraepithelial neoplasia with high-grade cytonuclear atypia is diagnosed as “adenocarcinoma” in Japan, while similar lesions are diagnosed as “high-grade dysplasia” in most Western countries (Fig. 5.11). However, this disagreement may not be of great importance, because both intramucosal adenocarcinoma and high-grade dysplasia are usually treated with conservative approach through endoscopic resection. In addition, among many Japanese pathologists, a diagnosis of “adenoma” is reserved only for a low-grade pyloric gland adenoma or typical example of low-grade intestinal-type adenoma, which is small (usually 1 cm or less).
When marked cytological or architectural atypia is present, making a diagnosis of high-grade dysplasia/adenoma is not difficult. At times, marked epithelial atypia may be seen in non-neoplastic condition such as regenerative process or epithelial injury by chemotherapy and irradiation. As mentioned earlier, characteristic features of phenotypic sub-patterns as well as immunohistochemical features become less distinctive as the neoplastic processes progress to high-grade and ultimately to invasive carcinoma.
Epithelial Pattern with Mild to Moderate Atypia “Noninvasive Atypical Epithelium”
A major problem in gastric biopsy interpretation includes differentiating neoplastic conditions from reactive or regenerative changes. Abrupt transitions, surface maturation and stromal changes in addition to the degree of architectural and cytological abnormalities are key features to be focused.
On the basis of these core features in combination, distinction between neoplastic and non-neoplastic lesion can be made in most biopsies. A diagnosis of “indefinite for neoplasia/dysplasia” is reserved for biopsies in which a reliable differentiation between neoplastic and non-neoplastic is not possible. Such a diagnosis should not be ignored since some of these changes are either genuine neoplastic lesions or flag bearers of more sinister lesions [13, 14].
Reasons for a diagnosis of “indefinite for neoplasia” are diverse and include technical problems, such as too little amount of atypical epithelium for concern, marked cautery or crushed artefacts, poor orientation, tangential cutting, denuded surface epithelium, etc. In such cases, cutting deeper level sections or obtaining additional biopsies may solve the diagnostic dilemma.
A useful rule in such a situation is to describe the reason for the diagnosis of “indefinite for neoplasia” and the degree of concern. This approach is valuable for clinical management.
Correlation with the endoscopic appearance and review of previous biopsies (if any) and a dialogue with the clinician can reveal important information such as medication history may resolve the uncertainty to a great extent (Fig. 4.31). Other clinical information such as past medication history may facilitate further follow-up and investigations.
Epithelial Pattern (Glandular Proliferations) with Stromal Invasion (“Invasive Pattern”)
This pattern signifies invasive carcinoma acknowledging the criteria used by Japanese pathologists described above. This category includes adenocarcinoma, excluding intraepithelial adenocarcinoma in Japanese criteria and in situ signet ring cell carcinoma.
In addition to cytoarchitectural disturbances described above, features of stromal invasion are present represented by single-cell/small cluster infiltration, angulated/abortive glands, sheetlike growth, never-ending/anastomosing gland pattern, highly complex cribriform arrangement of glands and stromal desmoplasia. Again, there are similarities to adenocarcinomas in Barrett’s setting (Chap. 3) (Box 5.4).
Box 5.4 Invasive Patterns in Gastric Adenocarcinoma
Recognition of the wide morphologic spectrum (sub-patterns) within the established histological types is important not to miss early GAC in a biopsy.
-
Tubular, papillary, mucinous, poorly cohesive, and mixed (five main WHO histologic types)
-
Sub-patterns/types
-
“Very well-differentiated adenocarcinoma” pattern (WHO tubular)
-
Micropapillary
-
Mixed neuroendocrine carcinomas (MANEC/MiNEN)
-
AFP-positive adenocarcinoma
-
EBV-positive adenocarcinoma
-
Although many schemes have been proposed for gastric cancer classification, two major classification schemes internationally used in pathology practice are WHO classification and Laurén classification (Table 5.2) [13, 15]. The WHO classification system recognises five main histological types, namely, tubular adenocarcinoma, papillary adenocarcinoma, mucinous adenocarcinoma, poorly cohesive carcinoma (including signet ring cell carcinoma and other variants) and mixed carcinoma. A molecular classification of GAC with four molecular subtypes has been proposed recently. They are EBV-positive, microsatellite-unstable (MSI), genomically stable tumours and tumours with chromosomal instability (CIN)
However, gastric adenocarcinoma is characterised by a wide morphologic spectrum with respect to cellular differentiation, architecture and growth pattern and shows heterogeneity (Fig. 5.12). Thus, it is important to recognise these sub-patterns within the spectrum of the invasive pattern in an endoscopic biopsy to accurately diagnose early gastric carcinoma.
Case 3: Heterogeneity of gastric carcinoma . (a) Endoscopic resection was performed for an elevated lesion of the stomach. (b) Peripheral area of the lesion is composed of low-grade intestinal-type dysplasia (smaller square of A). (c) At the centre (larger square of A), submucosal invasive adenocarcinoma is noted. It is important to know that gastric neoplasm often shows heterogeneity within a lesion like this case and to take multiple biopsies if the endoscopic appearance is heterogeneous
Tubular Pattern
Tubular adenocarcinoma is composed of irregularly distended, fused or branching tubules of various sizes, often with intraluminal mucin or debris (Fig. 5.13). Acinar structures or cribriform pattern may also be present. Tumour with solid pattern is considered as a poorly differentiated form of this type. Of note, rare cases of tubular adenocarcinoma have minimal architectural abnormality as well as subtle cytological atypia, for which a term “very well-differentiated adenocarcinoma” may be used.
Papillary Pattern
Papillary adenocarcinoma is characterised by epithelial fingerlike projections with central fibrovascular cores (Fig. 5.14a). Some tumours show tubulopapillary architectures. Micropapillary pattern can be present in a rare tumour (Fig. 5.14b) [16].
Mucinous Pattern
Mucinous adenocarcinoma is characterised by extracellular mucinous pools, which constitute at least 50% of tumour volume. The tumour cells form glandular structures, irregular cell clusters or scattered signet ring cells floating in the mucin pools (Fig. 5.15).
Poorly Cohesive Pattern
Poorly cohesive carcinoma includes signet ring cell carcinoma and other variants and is often composed of a mixture of both of them. Signet ring cell is characterised by abundant mucin-filled cytoplasm and eccentrically placed nucleus (Fig. 5.16a). Poorly cohesive non-signet ring carcinoma cells are those that morphologically resemble histiocytes, lymphocytes, plasma cells and even spindle fibroblast-like cells. Those tumour cells can form irregular micro-trabeculae or lacelike abortive glands. This type of tumour is often accompanied by marked stromal desmoplasia in the submucosal or deeper invasive area, whereas intramucosal component consists of dense aggregation of signet ring cells with minimal stromal change (Fig. 5.16b). Histiocytes, xanthoma cells (Fig. 5.16c), plasma cells with abundant brightly eosinophilic cytoplasm of plasma cells in Russell body gastritis (Fig. 5.16d) and small dilated vessels filled with eosinophilic plasma constituents (Fig. 5.16e) may mimic signet ring cells in small biopsies raising concern.
Mixed Pattern
In the Laurén classification, tumours are classified into intestinal and diffuse types. Intestinal type essentially corresponds to tubular and papillary adenocarcinoma in WHO scheme, whereas diffuse type falls into the poorly cohesive carcinoma category. Tumours containing both of intestinal and diffuse components are termed mixed type . Undifferentiated tumours are classified as indeterminate.
“Invasive Epithelial Pattern”: Others
Other patterns include EBV-positive adenocarcinoma, AFP-producing carcinoma, rarer sub-patterns of well-differentiated adenocarcinoma and those with the neuroendocrine sub-pattern.
AFP-producing carcinoma is characterised by the AFP expression by neoplastic cells, which is usually demonstrated by positive AFP immunostaining or increased serum AFP level. Histologically, AFP-producing carcinoma has two major histological types: adenocarcinoma with enteroblastic differentiation, a tubular or papillary adenocarcinoma composed of columnar neoplastic cells with glycogen-rich clear cytoplasm resembling foetal gut epithelium at early gestation (Fig. 5.17a), and hepatoid adenocarcinoma, which consists of polygonal eosinophilic neoplastic cells similar to hepatocellular carcinoma (Fig. 5.17b). Yolk-sac tumour-like carcinoma can be less frequently noted in a component of AFP-producing carcinoma. It may be important to recognise this entity because it is associated with highly aggressive phenotype with frequent liver metastasis and serum AFP levels can be used as a sensitive tumour marker.
EBV-positive adenocarcinoma is a carcinoma with EBV positivity in almost all neoplastic cells. This tumour has distinct clinicopathological and molecular features, which reflect peculiar viral carcinogenesis [17, 18]. The presence of EBV in tumour cells is confirmed by in situ hybridisation targeting an EBV-encoded small RNA (EBER-ISH) , whereas immunohistochemistry of LMP1 or EBNA2 is always negative in this tumour. EBV-positive adenocarcinoma typically shows a pushing tumour border and is usually composed of moderately to poorly differentiated tubular adenocarcinoma accompanied by lymphoid stroma (Fig. 5.18). Cases with prominent lymphoid infiltrates are called “gastric carcinoma with lymphoid stroma ” (also reported as “lymphoepithelioma-like carcinoma ”). More than 80% of gastric carcinomas with lymphoid stroma are EBV positive. Clinical features of EBV-positive gastric cancer include male predominance, a proximal location, low rate of nodal metastasis in early cancer and a relatively favourable prognosis.
Cases with very rare histological types, such as adenosquamous/squamous cell carcinoma, yolk-sac tumour-like carcinoma, choriocarcinoma, carcinosarcoma, malignant undifferentiated/rhabdoid carcinoma, mucoepidermoid carcinoma, parietal cell carcinoma, pancreatic-type acinar/mixed acinar and endocrine carcinoma, and gastroblastoma have been reported.
Rare Differentiated Patterns of GAC
In general, because most gastric carcinomas have significant architectural abnormality and cytological atypia as well as invasive features, a diagnosis of adenocarcinoma is straightforward in adequate biopsies. Exceptionally, rare gastric adenocarcinomas show minimal cytological and/or architectural abnormalities even though they are clearly invasive (Figs. 5.19a, b and 5.20). Biopsy diagnosis for such a lesion is often difficult and can be misinterpreted. In addition, metastatic carcinoma needs to be considered in the differential diagnoses.
Very well-differentiated adenocarcinoma . (a) Very well-differentiated adenocarcinoma of intestinal type closely mimicking intestinal metaplasia. Cellular atypia is minimal, but neoplastic glands show characteristic “hand-in-hand”-type anastomoses. (b) Very well-differentiated adenocarcinoma of gastric type resembling hyperplastic foveolar epithelium. (c) Very well-differentiated adenocarcinoma of gastric type with transformation into signet ring cell carcinoma
Case 4: Very well-differentiated adenocarcinoma . (a) This biopsy is from a slightly elevated lesion measuring 2 cm in size. This looks like a reactive gastropathy with mild architectural disarray. It may be very difficult to make a diagnosis of cancer for this biopsy. (b) This lesion is actually an advanced cancer invading into the muscularis propria composed of very well-differentiated adenocarcinoma of intestinal type. (c) Neoplastic glands show mild distortion and mild nuclear enlargement. (d) The deeply invasive area also consists of glandular proliferation with minimal cytological atypia
Gastric adenocarcinoma with low-grade atypia include a several subtypes, including very well-differentiated adenocarcinoma of intestinal type which resembles intestinal metaplasia and that of gastric type mimicking foveolar epithelium (Fig. 5.19a, b) [19]. These lesions are rare and exhibit minimal cytological atypia, and therefore recognising architectural abnormalities is important for a diagnosis. Characteristic architectural features of gastric adenocarcinoma with low-grade atypia include pit and glandular anastomosis, spiky glands, distended glands, discohesive cells, abortive glands and budding. A subset of this tumour may transform into poorly cohesive carcinoma and behave aggressively (Fig. 5.19c).
Neuroendocrine Pattern
The characteristic pattern consists of relatively uniform round cells with variable amounts of eosinophilic cytoplasm and central nuclei with granular, speckled (“salt and pepper”) chromatin (Figs. 5.21 and 5.22a, b). Nucleoli are inconspicuous. Well-differentiated neuroendocrine neoplasms (NENs) or neuroendocrine carcinomas (NECs) uncommonly may present with the “epithelial pattern” especially those exhibiting pseudo glandular formations. Additional sub-patterns of insular (nested), trabecular and solid patterns are often noted. As neuroendocrine neoplasm often show the epithelial pattern in endoscopic biopsies, they can be mistaken for GAC. The cells may appear blue or pink and also show other cellular patterns in an endoscopic biopsy (see Table 5.4). In general, the neuroendocrine nature is appreciated on H&E sections and confirmed by neuroendocrine markers.
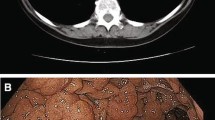
Case 5: Well-differentiated (WHO Grade 1) neuroendocrine neoplasm in the setting of AIG (Type 1). A 72-year-old man referred for evaluation of macrocytic anaemia with B12 deficiency. Gastroscopy revealed atrophic appearing corpus gastric mucosa with antral sparing suggesting likely autoimmune atrophic gastritis. In addition to this, there was a 9 mm nodule noted on the mid-gastric body greater curve (a, b featuring retroflexion view). The nodule was resected and sent for histopathology. Diagnosis was a well-differentiated (Grade 1) neuroendocrine neoplasm (c)
Neuroendocrine carcinoma (NECs), in particular poorly differentiated tumours, may show the epithelial pattern but with more cytological variability, nuclear hyperchromasia, frequent mitoses and prominent nucleoli together with necrosis and may be of small-cell (Fig. 5.22c) or large-cell type (Fig. 5.22d). Cytological features of small-cell type include a small size, a round-to-fusiform shape, scant cytoplasm, finely granular nuclear chromatin, absent or inconspicuous nucleoli and a high mitotic ratio (>20 mitoses per 10 HPF). Large-cell type shows more vesicular nuclei with more prominent nucleoli as well as larger cell size and lower nuclear-cytoplasmic ratios than small-cell type. The cells are usually positive for neuroendocrine markers but may be patchy.
A tumour with both neuroendocrine carcinoma and adenocarcinoma components (with each component exceeding 30%) is referred to as a “mixed adenoneuroendocrine carcinoma”, MANEC, now called MiNEN in the new WHO 2017 endocrine tumour classification.
Confirmation of Neuroendocrine Nature
The most useful confirmative immunostains include chromogranin, synaptophysin and CD56 although routine immunohistochemical stains may not be necessary to identify the neuroendocrine pattern but are used for confirmation in particular in NECs and mixed neoplasms. Immunostains for neuropeptide hormones are not routinely performed.
Grading of NENs
Once a diagnosis of a neuroendocrine neoplasm or neuroendocrine carcinoma is confirmed, mitotic count and proliferation index (PI) determined nuclear staining by Ki-67 immunohistochemistry are performed. Manual counting (2000 cells per ENETS), “eyeballed” estimate and digital image analysis are methods used for assessment of proliferation index. Readers are advised to refer to texts that would detail recommendations and discuss controversies of grading criteria of NENs. In spite of heterogeneity reported in NENs and NECs, grading of NENs/NECs should be performed on endoscopic biopsies. This is important for therapeutic decisions in patients with inoperable and/or high-grade NENs and NECs in which the only diagnostic material available may be endoscopic biopsies. NECs by definition are high grade and proliferation index is often irrelevant.
An endoscopic biopsy report of a confirmed neuroendocrine neoplasm/carcinoma should include any relevant associated pathology such as autoimmune gastritis considering the clinical setting in view of their tendency for recurrences yet good prognosis. A common pitfall is crushed neuroendocrine cells in small biopsies that could be easily missed especially those found in random endoscopic biopsies. A comment on the margin status may be required for those tumours that present as small polyps and subject to polypectomy.
Gastric NENs are of three types with important prognostic and clinical differences. Type I tumours arise in the setting of autoimmune gastritis (70–80%). Type II tumours are associated with MEN1-Zollinger-Ellison syndrome and account for 5–10% of NENs. Type III tumours are sporadic, are nearly always solitary and are generally aggressive (Fig. 5.22b). Type 1 tumours (Fig. 5.22a) show indolent behaviour, whereas the biology of type II tumours is intermediate.
In the stomach if the tumour is confined to the mucosa measuring more than 500 μm (0.5 mm) or invades the submucosa, the lesion is considered NEN. The WHO defined these nodules that are < 0.5mm (500μm) as micro carcinoids. The lesions measuring 150–500 μm are termed neuroendocrine dysplasia. Those <150 μm are classified as hyperplasia. However, the size may be an arbitrary criterion and inadequate to determine the clinical significance.
Long-standing hypergastrinaemia is consistently associated with endocrine cell (enterochromaffin-like cells) hyperplasia. Corpus predominant chronic AIG is the most common cause. Less commonly AIG may supervene over chronic Helicobacter pylori gastritis. In a minority of cases, corpus predominant Helicobacter pylori gastritis may be responsible. Less commonly unrelated causes may be responsible for ECL oncogenesis (i.e. MEN syndrome) [20,21,22,23,24,25,26,27].
Non-epithelial Pattern
This category includes many neoplastic entities common to the entire GI tract, and a general introduction is given in Chap. 2. On the basis of morphologic pattern, non-epithelial patterns in a gastric mucosa biopsy are with diffuse round cell (or epithelioid-like) pattern (Table 5.4), spindle cell pattern (Table 5.3) and an admixture, biphasic pattern (Table 5.5). Epithelial tumours when differentiated may assume a diffuse architectural pattern with sparse or no glandular differentiation. When rounded epithelioid growth patterns are noted, non-glandular epithelial neoplasms, in particular squamous cell and neuroendocrine neoplasm, as well as lymphoma, melanoma and epithelioid mesenchymal tumours should be considered. Dominant cytoplasmic tinctorial quality (blue cell, pink cell or clear cell) on the H&E stain can give a clue to the diagnosis. Tumours that develop specifically in the stomach include plexiform fibromyxoma and gastroblastoma, a diagnosis unlikely to be made in a gastric biopsy.
Diffuse Round Cell Pattern
The most common neoplasm that presents with “diffuse round small blue cell pattern” in a gastric biopsy is MALT lymphoma characterised by a monotonous infiltrate of monocytoid B cells that expand and replace the normal structures of the lamina propria (Fig. 5.23a). Infiltration of the gastric glands by neoplastic lymphoid cells in the form of lymphoepithelial lesions is a characteristic feature. Presence of larger blue cells should raise the possibility of transformation to diffuse large B-cell lymphoma. Genuine diffuse large B-cell lymphomas (DLBCL) show large blue cell pattern (Fig. 5.23b) and are more likely to present with macroscopic lesions compared MALT lymphomas that often present in mucosal biopsies. Florid H. pylori gastritis with a diffuse lymphoplasmacytic infiltrate can be alarming. In fact, distinction may be very difficult. B-cell clonality studies by advanced polymerase chain reaction technology (using Wotherspoon criteria) may be helpful in the distinction. Other neoplasms that may present as small round blue pattern are listed in Table 5.4.
The stomach is one of the most common sites of gastrointestinal MALT lymphomas. Approximately 50% of MALT lymphomas occur in the GI tract, and about 85% of these occur in the stomach. Around 50% of gastric lymphomas are MALT lymphomas. Helicobacter pylori is the major cause of gastric MALT lymphoma and is present in 75–90% of cases. Eradication of H. pylori with antibiotics results in complete histological remission in about 70% cases. Histological response can be scored on endoscopic biopsies according to GELA recommendations.
Eradication of H. pylori with antibiotics induces complete histological remission in about 70% of gastric MALT lymphoma (GML) cases, and time to achieve remission may last up to 24 months [28,29,30].
Blue Cell Pattern
Blue cell pattern in a gastric biopsy can mimic a lymphoma. Lymphomatoid gastropathy (or NK-cell enteropathy) is a rare NK-cell proliferation in the gastrointestinal mucosa [31, 32]. This is essentially a benign lesion and usually self-limited disease, but unfortunately overdiagnoses and overtreatment frequently occur because of its close resemblance to malignant lymphoma. Endoscopically, lymphomatoid gastropathy shows slightly elevated haemorrhagic appearance and is always small (around 1 cm) and localised or has multiple lesions. Mucosal biopsy shows expansion of the lamina propria by confluent infiltrates of medium to large-sized atypical lymphoid cells with abundant clear or slightly eosinophilic cytoplasm (Fig. 5.24a, b). Mitoses or apoptosis are not prominent. Characteristically, eosinophilic granules are often observed in the cytoplasm (Fig. 5.24b). In immunohistochemistry, lymphomatoid gastropathy shows NK-cell phenotype, i.e. cytoplasmic CD3+, CD7+, CD56+, and cytotoxic molecules +. T-cell markers (surface CD3, CD4, CD5, TCRαβ), B-cell markers (CD20) and EBV infection (EBER-ISH) are negative. Ki-67 positive ratio is about 10–30%.
Lymphomatoid gastropathy . (a) A biopsy shows diffuse cellular infiltration in the lamina propria with haemorrhage and erosion. (b) Medium-sized atypical lymphoid cells with abundant clear or slightly eosinophilic cytoplasm diffusely infiltrate the lamina propria. Some of them have eosinophilic granules in their cytoplasm (arrow). These atypical lymphoid cells are positive for CD56 immunostaining (inset)
Spindle Cell Pattern
Spindle cell pattern in a gastric biopsy is characteristic of gastrointestinal stromal tumour (GIST) although rare epithelial tumour cells may be spindle-shaped, such as poorly differentiated carcinoma and sarcomatoid carcinoma (or sarcomatous component of carcinosarcoma). The vast majority of mesenchymal tumours within the GI tract are GIST, and in this section the major emphasis is on this neoplasm. GISTs must be distinguished from other spindle cell proliferations in the GI tract (Table 5.3) (Fig. 5.25a, b).
Gastrointestinal stromal tumour (GIST) . (a) Tissue sample of this gastric submucosal tumour was taken by endoscopic ultrasound-guided fine-needle aspiration. Tumour is a spindle cell GIST composed of uniform spindle cells with perinuclear vacuoles and nuclear palisading. (b) Endoscopic biopsy of a GIST. (c, d). Spidle and myxoid areas (highlighted in b in high power) (e) Epithelioid GIST composed of epithelioid cells with moderate nuclear pleomorphism. (f) CD117 and (g) DOG-1 stain with immunohistochemistry in case shown in (b)
Many have overlapping histologic features, and their accurate diagnosis can be challenging in the setting of limited endoscopic biopsy material. Because most of these lesions develop as a submucosal mass, mucosal biopsy often fails to obtain tissues sufficient for a diagnosis, although several approaches such as boring biopsy (tunnel biopsy) and endoscopic ultrasound/fine-needle aspiration (EUS-FNA) biopsy are currently used. In this setting, a panel of immunohistochemistry (and molecular testing) is often needed to make a definitive diagnosis (Table 5.3). The histomorphology of GIST has a wide spectrum, but most GISTs show spindle cell tumours, and a minority (20–25%) has epithelioid, mixed spindle and epithelioid or rarely pleomorphic histology. Spindle cell GISTs are composed of uniform elongated cells arranged in intersecting fascicles. Perinuclear vacuoles are frequently present in gastric GISTs (Fig. 5.25a). Nuclear palisading, resembling Antoni A areas of a schwannoma, is occasionally encountered. The stroma may show myxoid change (Fig. 5.25c, d), hyalinisation or calcification. Nearly one half of small intestinal GISTs contain oval or elongated eosinophilic aggregates of extracellular collagen fibres, so-called skeinoid fibres. Epithelioid GISTs are characterised by rounded cells arranged in nests or sheets, with variably eosinophilic to clear cytoplasm and vesicular nuclei (Fig. 5.25e). Pleomorphic morphology is unusual in GISTs but can be seen especially in a rare example of dedifferentiated GIST, in which a transition from a conventional KIT-positive spindle cell pattern to an anaplastic or pleomorphic morphology with frequent loss of KIT immunoreactivity is noted [33]. Tumour size and mitotic activity are key parameters in assessing the biologic potential and should be reported when enough tissue samples are biopsied [34]. In immunohistochemistry, the key feature of GIST is positivity for the Kit (CD117; Fig. 5.25f); it is expressed in more than 95% of GISTs. DOG1 antibody is an equally sensitive and specific marker for GISTs (Fig. 5.25g). CD34 is also commonly expressed in about 70% of GISTs but less specific than Kit and DOG1. A minority of GISTs are variably positive for smooth muscle actin (20–30%), S100 (5%) and keratin (CK18) or Desmin (1–2%). Since a subset of malignant melanomas express KIT, melanoma should be excluded by performing a panel of melanocytic markers in a case with significant atypia and mitotic activity. SDH-deficient GISTs, which especially include paediatric GISTs and those associated with Carney triad or Carney-Stratakis syndromes, are identified by immunohistochemical loss of SDHB.
Metastatic Patterns
The characteristic metastatic pattern is submucosal tumour-like appearance, lack of intraepithelial neoplastic component (i.e. precursor lesion of dysplasia/adenoma), distribution predominantly involving deep mucosal or submucosal layer rather than mucosal surface and invasion between non-neoplastic glands, although none of them are specific to metastatic diseases.
A diagnosis of metastatic carcinoma is usually established by confirming the morphologic similarity between the gastric biopsy and the primary tumour. Even if the histology of primary tumour is not available for review, the diagnosis is often possible based on the characteristic morphology and immunophenotype specific to tumours of each primary site. When the presence of extra-gastric lesion or past medical history of cancer is not recognised clinically, the diagnosis can be challenging. Common primary sites developing gastric metastases include lung cancer, breast cancer, oesophageal cancer and malignant melanoma. Table 5.6 summarises markers of these tumours that are useful for differential diagnosis. Other primary tumours from the kidney, pancreas, testis, cervix, colon, liver, etc. have been reported as well. Notably, stomach metastasis from the breast lobular carcinoma may mimic primary poorly cohesive carcinoma histologically and endoscopically, because it may show morphology of signet ring cell carcinoma and extensive infiltration involving stomach wall similar to scirrhous-type gastric cancer (Fig. 5.26).
Metastatic lobular carcinoma of the breast. (a) This patient has a past medical history of breast cancer 5 years ago. Upper endoscopic examination shows diffuse mucosal erythema and thickened folds, worrisome feature for scirrhous carcinoma. (b) Mucosal biopsy shows diffuse infiltration of discohesive neoplastic cells, consistent with primary diffuse-type gastric cancer. Immunohistochemistry of oestrogen receptor was performed to rule out metastatic breast cancer and revealed the neoplastic cells were diffusely positive. This is a typical example of metastatic lobular carcinoma of the breast. It is important to know that metastatic lobular carcinoma often mimics poorly cohesive carcinoma endoscopically and histologically
HER2 (Human Epidermal Growth Factor Receptor 2 ) and Gastric Carcinomas
Recent advances in targeted therapy have identified HER2 as an important target for anticancer therapy of gastric and gastroesophageal junctional adenocarcinomas. The ToGA study showed clinically and statistically significant benefit in response rates, median progression-free survival and overall survival with the addition of the anti-HER2 biological agent, trastuzumab, to standard chemotherapeutic regimens in advanced and metastatic G/GOJ carcinoma [35, 36]. Amplification of the human epidermal growth factor receptor 2 (HER2) gene resulting in overexpression of the protein products has been identified in 10–20% of G/GOJ carcinomas. The reported frequency of HER2 overexpression ranges from 8.2% to 53.4% in gastric carcinoma. Therefore, HER2 testing in G/GOJ carcinomas should be routinely performed to identify those who will benefit from trastuzumab-based therapy.
When a G/GOJ carcinoma is diagnosed in an endoscopic biopsy, there are a few important factors to consider with regard to routine HER2 testing.
Selection of the Correct Patient for Targeted Therapy
HER2 positivity determines the eligibility for HER2 targeted therapy. HER2 status can be determined by estimation of protein expression by immunohistochemistry (IHC) or assessment of HER2 amplification by in situ hybridisation (ISH). Accurate testing is dependent on several pre-analytical and analytical factors including sample selection, laboratory techniques and accurate interpretation of HER2 test results.
Material Suitable for Testing?
As most patients with G/GOJ carcinoma present with advanced disease, endoscopic biopsy may be the only material available for diagnosis and biomarker testing. Samples that could be tested are endoscopic biopsies, resection specimens and metastatic tumours including cytology samples. Formalin-fixed paraffin-embedded tissue is ideal for HER2 testing by any method. Cold ischaemic time and duration of fixation are important pre-analytical issues that may influence test results. Archival material may be used for testing; however, freshly cut sections should be used for testing.
Testing Methods Employed
Gene amplification is tested by in situ hybridisation (ISH) and protein expression by IHC methods. ISH can be performed by bright-field (chromogen (CISH) or silver (SISH)) and dark-field {fluorescence (FISH)} techniques. Bright-field method is preferred for HER2 testing.
Who Should Be Interpreting and Reporting Results?
Interpretation of both IHC and ISH requires specific expertise on the subject. Centralised testing has shown to give more reliable testing. Ideally gastrointestinal pathologists who have been specially trained to deal with pre-analytical, analytical and post-analytical issues should be dealing with HER2 interpretation and reporting. It is of paramount importance that invasive carcinoma cells are assessed separating them from preinvasive lesions and indeed reactive epithelial and stromal cells. Diagnostic problems of invasive carcinoma, in particular signet ring cell and poorly cohesive carcinomas, and problems of differentiating dysplasia, reactive changes and invasion are discussed above. HER2 assessment is essentially a manual exercise that needs to be coupled with in-depth understanding of diagnostic issues of endoscopic biopsies and knowledge of technical issues. The optimum number of tumour fragments for accurate result is 5 or more due to heterogeneity of HER2 expression in G/GOJ carcinomas.
Standardised reporting with documentation of specimen adequacy, methods employed, interpretation and final test result are mandatory items.
Testing Algorithm
Hoffman et al. validated IHC scoring for HER2 protein expression before the landmark ToGA trial. Scoring criteria and adequacy criteria for biopsies (and resections) were recommended (Fig. 5.27). The main differences from assessing HER2/neu in breast cancer are that gastric cancers often do not show complete membranous staining (i.e. staining is often basolateral) and that only five cells in a biopsy specimen are required to show immunoreactivity to be considered for a positive. Heterogeneity of the overexpression/amplification of HER2 in gastric cancer is more prevalent up to 40% in GC. The recent ASCO/CAP guidelines recommend ISH confirmation for IHC 2+ cases only. The cut-offs for HER2 ISH positivity have been defined as ratio >2 or CN >6 even in the presence of a ratio. Others recommend ISH confirmation for IHC3+ cases to avoid false-positive results [37,38,39,40,41,42,43,44].
References
Rugge M, Correa P, Dixon MF, et al. Gastric dysplasia: the Padova international classification. Am J Surg Pathol. 2000;24:167–76.
Raftopoulos SC, Kumarasinghe P, de Boer B, Iacobelli J, Kontorinis N, Fermoyle S, Olynyk J, Forrest C, Ee HC, Yusoff IF. Gastric intraepithelial neoplasia in a Western population. Eur J Gastroenterol Hepatol. 2012;24:48–54.
Shin N, Jo HJ, Kim WK, et al. Gastric pit dysplasia in adjacent gastric mucosa in 414 gastric cancers: prevalence and characteristics. Am J Surg Pathol. 2011;35:1021–9.
Ueyama H, Yao T, Nakashima Y, et al. Gastric adenocarcinoma of fundic gland type (chief cell predominant type): proposal for a new entity of gastric adenocarcinoma. Am J Surg Pathol. 2010;34:609–19.
Park DY, Srivastava A, Kim GH, et al. Adenomatous and foveolar gastric dysplasia: distinct patterns of mucin expression and background intestinal metaplasia. Am J Surg Pathol. 2008;32:524–33.
Vieth M, Kushima R, Borchard F, et al. Pyloric gland adenoma: a clinico-pathological analysis of 90 cases. Virchows Arch. 2003;442:317–21.
Singhi AD, Lazenby AJ, Montgomery EA. Gastric adenocarcinoma with chief cell differentiation: a proposal for reclassification as oxyntic gland polyp/adenoma. Am J Surg Pathol. 2012;36:1030–5.
Chan K, Brown IS, Kyle T, Lauwers GY, Kumarasinghe MP. Chief cell-predominant gastric polyps: a series of 12 cases with literature review. Histopathology. 2016;68(6):825–33.
Priyanthi Kumarasinghe W, Bastiaan de Boer M, Hooi E. Neoplasia in gastric adenocarcinoma and proximal polyposis syndrome (GAPPS): gastric rather than intestinal phenotype. Pathology. 2016;48(Suppl 1):S1–S164.
Cho SJ, Choi IJ, Kim CG, et al. Risk of high-grade dysplasia or carcinoma in gastric biopsy-proven low-grade dysplasia: an analysis using the Vienna classification. Endoscopy. 2011;43:465–71.
Yamada H, Ikegami M, Shimoda T, et al. Long-term follow-up study of gastric adenoma/dysplasia. Endoscopy. 2004;36:390–6.
Lauwers GY, Shimizu M, Correa P, et al. Evaluation of gastric biopsies for neoplasia: differences between Japanese and Western pathologists. Am J Surg Pathol. 1999;23:511–8.
WHO. WHO classification of tumours of the digestive system. Lyon: IARC; 2010.
Shepherd NA, Warren BF, Williams GT, Greenson JK, Lauwers GY, editors. Morson and Dawson’s gastrointestinal pathology. 5th ed. New York, NY: John Wiley and Sons; 2013.
Lauren P. The two histological main types of gastric carcinoma: diffuse and so-called intestinal-type carcinoma. An attempt at a histo-clinical classification. Acta Pathol Microbiol Scand. 1965;64:31–49.
Ushiku T, Matsusaka K, Iwasaki Y, et al. Gastric carcinoma with invasive micropapillary pattern and its association with lymph node metastasis. Histopathology. 2011;59:1081–9.
Shinozaki-Ushiku A, Kunita A, Fukayama M. Update on Epstein-Barr virus and gastric cancer (review). Int J Oncol. 2015;46:1421–34.
Min BH, Tae CH, Ahn SM, et al. Epstein-Barr virus infection serves as an independent predictor of survival in patients with lymphoepithelioma-like gastric carcinoma. Gastric Cancer. 2016;19:852–9.
Ushiku T, Arnason T, Ban S, et al. Very well-differentiated gastric carcinoma of intestinal type: analysis of diagnostic criteria. Mod Pathol. 2013;26:1620–31.
Modlin IM, Lye KD, Kidd M. A 5-decade analysis of 13,715 carcinoid tumours. Cancer. 2003;97(4):934–59.
Modlin IM, Shapiro MD, Kidd M. An analysis of rare carcinoid tumours: clarifying these clinical conundrums. World J Surg. 2005;29:92–101.
Rindi G, Petrone G, Inzani F. The 2010 WHO classification of digestive neuroendocrine neoplasms: four years after its introduction. Endocr Pathol. 2014;25:186–92.
Tang LH, Gonen M, Hadvat C, Modlin IM, Klimstra DS. Objective quantification of the Ki67 proliferative index in neuroendocrine tumours of the gastroenteropancreatic system: a comparison of digital image analysis with manual methods. Am J Surg Pathol. 2012;36:1761–70.
Yang Z, Tang LT, Klimstra DS. Effect of tumour heterogeneity on the assessment of Ki67 labeling index in well-differentiated neuroendocrine tumours metastatic to the liver: implications for prognostic stratification. Am J Surg Pathol. 2011;35:853–60.
Abraham SC, Carney JA, Ooi A, et al. Achlorhydria, parietal cell hyperplasia, and multiple gastric carcinoids. A new disorder. Am J Surg Pathol. 2005;29:969–75.
Borch K, Ahren B, Ahlman H, Falkmer S, Granerus G, Grimelius L. Gastric carcinoids: biologic behaviour and prognosis after differentiated treatment in relation to type. Ann Surg. 2005;242:64–73.
Ishida M, Sekine S, Fukagawa T, et al. Neuroendocrine carcinoma of the stomach: morphologic and immunohistochemical characteristics and prognosis. Am J Surg Pathol. 2013;37:949–59.
Ruskone-Fourmestraux A, Fischbach W, Aleman BMP, et al. EGILs consensus report: gastric extranodal marginal zone B-cell lymphoma of MALT. Gut. 2011;60:747–58.
Nakamura S, Sugiyama T, Matsumoto T, et al. Long-term clinical outcome of gastric MALT lymphoma after eradication of Helicobacter pylori: a multicentre cohort follow-up study of 420 patients in Japan. Gut. 2012;61:507–13.
Copie-Bergman C, Wotherspoon AC, Capella C, Motta T, Pedrinis E, Piler SA, Berton F, Concon A, Zucca E, Ponzoni M, Ferreri AJM. Gela histological scoring system for post-treatment biopsies of patients with gastric MALT lymphoma is feasible and reliable in routine practice. Br J Haematol. 2012;160:47–52.
Mansoor A, Pittaluga S, Beck PL, et al. NK-cell enteropathy: a benign NK-cell lymphoproliferative disease mimicking intestinal lymphoma: clinicopathologic features and follow-up in a unique case series. Blood. 2011;117:1447–52.
Takeuchi K, Yokoyama M, Ishizawa S, et al. Lymphomatoid gastropathy: a distinct clinicopathologic entity of self-limited pseudomalignant NK-cell proliferation. Blood. 2010;116:5631–7.
Antonescu CR, Romeo S, Zhang L, et al. Dedifferentiation in gastrointestinal stromal tumour to an anaplastic KIT-negative phenotype: a diagnostic pitfall: morphologic and molecular characterization of 8 cases occurring either de novo or after imatinib therapy. Am J Surg Pathol. 2013;37:385–92.
Miettinen M, Lasota J. Gastrointestinal stromal tumours: pathology and prognosis at different sites. Semin Diagn Pathol. 2006;23:70–8.
Bang YJ, Van Cutsem E, Feyereislova A, Chung HC, Shen L, Sawaki A, Lordick F, Ohtsu A, Omuro Y, Satoh T, Aprile G, Kulikov E, Hill J, Lehle M, Rüschoff J, Kang YK. Trastuzumab in combination with chemotherapy versus chemotherapy alone for treatment of HER2-positive advanced gastric or gastro-oesophageal junction cancer (ToGA): a phase 3, openlabel, randomised controlled trial. Lancet. 2010;376:687–97.
Jørgensen JT. Targeted HER2 treatment in advanced gastric cancer. Oncology. 2010;78:26–33. https://doi.org/10.1159/000288295. PMID: 20185938.
Kim KC, Koh YW, Chang HM, Kim TH, Yook JH, Kim BS, Jang SJ, Park YS. Evaluation of HER2 protein expression in gastric carcinomas: comparative analysis of 1,414 cases of whole-tissue sections and 595 cases of tissue microarrays. Ann Surg Oncol. 2011;18:2833–40. https://doi.org/10.1245/s10434-011-1695-2. PMID: 21468783.
Wong DD, Kumarasinghe MP, Platten MA, de Boer WB. Concordance of HER2 expression in paired primary and metastatic sites of gastric and gastro-oesophageal junction cancers. Pathology. 2015;47:641–6.
Fox SB, Kumarasinghe MP, Armes JE, et al. Gastric HER2 Testing Study (GaTHER): an evaluation of gastric/gastroesophageal junction cancer testing accuracy in Australia. Am J Surg Pathol. 2012;36:577–82.
Hofmann M, Stoss O, Shi D, Büttner R, van de Vijver M, Kim W, Ochiai A, Rüschoff J, Henkel T. Assessment of a HER2 scoring system for gastric cancer: results from a validation study. Histopathology. 2008;52:797–805.
Wang T, Hsieh ET, Henry P, Hanna W, Streutker CJ, Grin A. Matched biopsy and resection specimens of gastric and gastroesophageal adenocarcinoma show high concordance in HER2 status. Hum Pathol. 2014;45:970–5.
Bartley AN, Washington MK, Colasacco C, et al. HER2 testing and clinical decision making in gastroesophageal adenocarcinoma: guideline from the College of American Pathologists, American Society for Clinical Pathology, and the American Society of Clinical Oncology. J Clin Oncol. 2017;35:446–64.
Lee S, de Boer WB, Fermoyle S, Platten M, Kumarasinghe MP. Human epidermal growth factor receptor 2 testing in gastric carcinoma: issues related to heterogeneity in biopsies and resections. Histopathology. 2011;59:832–40.
Priyanthi Kumarasinghe M, Morey A, Bilous M, Farshid G, Francis G, Lampe G, McCue G, Von Neumann-Cosel V, Fox SB. HER2 testing in advanced gastric and gastro-oesophageal cancer; analysis of an Australia-wide testing program. Pathology. 2017;49:575–81.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Ushiku, T., Raftopoulos, S.C., Lauwers, G.Y., Kumarasinghe, M.P. (2019). Stomach: Neoplastic Patterns and Mimics. In: Kumarasinghe, M., Brown, I. (eds) Endoscopic Biopsy Interpretation. Springer, Cham. https://doi.org/10.1007/978-3-319-79117-3_5
Download citation
DOI: https://doi.org/10.1007/978-3-319-79117-3_5
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-79116-6
Online ISBN: 978-3-319-79117-3
eBook Packages: MedicineMedicine (R0)