Abstract
The most common metastatic sites of differentiated thyroid cancer (DTC) are the lung and bone after lymph nodes. A newly defined type of occult DTC is consistent with metastatic disease without an identified primary malignancy in the thyroid gland after total resection. We present a patient with multiple lung metastases of occult DTC showing mild 18F-fluorodeoxyglucose (FDG) uptake and intense radioiodine uptake without a primary lesion in the thyroid gland.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Case Presentation
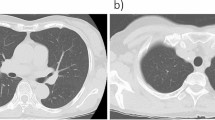
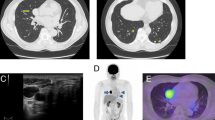
A 68-year-old woman presented with cough and chest pain. Thorax computerized tomography (CT) examination revealed multiple non-calcified nodular lesions suspected of metastases. The patient underwent 18F-fluorodeoxyglucose positron emission tomography/computerized tomography (FDG PET/CT) for metabolic characterization of nodules and localization of a possible primary malignancy (Fig. 30.1). Mild FDG uptake was observed in lung nodules (SUVmax = 1.9) and reported as nonspecific/inflammatory lesions. There was a peripherally calcified nodular lesion in the posterior region of the right thyroid lobe approximately 2 cm in diameter having FDG uptake at background levels. A wedge resection from the lung demonstrated metastasis of follicular variant of papillary thyroid carcinoma. Bilateral total thyroidectomy operation was performed upon this finding. The histopathological examination showed adenomatous hyperplasia in both thyroid lobes and no finding of malignancy. The patient was treated with 200 mCi I-131 for lung metastases. The whole-body scan after therapy showed intense radioiodine uptake in lung nodules and mediastinum (Fig. 30.2). The thyroglobulin (Tg) level was 2462 ng/mL before radioiodine therapy. Three months after the therapy, Tg level decreased to 17.6 ng/mL. The patient was under l-thyroxine therapy with suppressed TSH levels. A control 18F-FDG PET/CT scan was performed after 9 months of therapy (Fig. 30.3). Most of the lung nodules that were detected in first PET/CT study were regressed both in size and FDG uptake, and some of them were not visualized anymore. At this time, Tg level was 2.56 ng/mL, and second cure of radioiodine therapy was administered. The whole-body scan after 200 mCi I-131 administration did not show any pathologic uptake in the thyroid region, lungs, and other parts of the body, and the patient was ablated (Fig. 30.4). After 2 months of radioiodine therapy, Tg level was 0.06 ng/mL under TSH suppression.
2 Discussion
Differentiated thyroid cancer (DTC) referring to papillary and follicular carcinoma is usually characterized by good prognosis. The incidence of the distant metastatic disease has been reported to be 7–23% after initial treatment and 1–9% at first presentation before any treatment [1]. The lung and bone are the most common metastatic sites of DTC after lymph nodes [2]. A retrospective study with 49 patients having distant metastases at the presentation of thyroid carcinoma revealed 3-year and 5-year survival rates of 69% and 50%, respectively. The 3-year survival rates were better for patients aged ≤45, with lung-only versus bone-only metastasis, having papillary versus follicular carcinoma and iodine-avid disease versus non-avid [1].
Occult thyroid carcinoma (OTC) is usually considered as similar to papillary microcarcinoma. The tumor is either detected incidentally after total thyroidectomy for benign disease or at autopsy. In some cases, the patient is presented with apparent metastases of thyroid carcinoma, and the malign lesion is detected in the pathological examination of total thyroidectomy material. Liu et al. have defined a new group of OTC that presented with metastases of thyroid carcinoma at cervical lymph nodes or distant sites; however, the primary malign lesion is not detected in total thyroidectomy specimen. They reported a patient with lymph node metastasis of thyroid carcinoma and no malignity found in the thyroid gland after total thyroidectomy [3]. Our patient seems to be belonging to this group with lung metastases of thyroid carcinoma having no primary at thyroid gland. Borsò et al. also reported a case with disseminating bone metastases of DTC; however, primary malign focus was not detected in thyroidectomy [4]. Xu et al. have recently reported seven cases with this phenomenon having cervical lymph node metastases from thyroid cancer without an identifiable malign lesion in the thyroid gland. A papillary carcinoma phenotype was found in all cases, and most of them were BRAFV600E-positive tumors [5].
The lung is a common organ for metastasis from various tumor types. Pulmonary metastases of thyroid carcinoma are often seen as micronodular or miliary spread throughout both lungs. However, solitary nodular metastasis from thyroid cancer is also reported [6]. In a retrospective study with 75 patients having pulmonary metastases from DTC in different patterns like nodular, diffuse, or combined, it was reported that the treatment responses were not significantly different between patients with varying types of metastasis. However, there was a significant difference between patients with different types of tumor, papillary versus follicular thyroid carcinoma [7]. The initial size of the lung metastasis was also reported to be a significant prognostic factor revealing that patients having macronodular metastases (≥1 cm) had significantly poor treatment responses and disease progression irrespective of radioiodine avidity [8].
The first-line therapy for patients having pulmonary metastases from DTC should be I-131 therapy, as long as the metastases are iodine-avid [9,10,11]. Song et al. reported the therapy responses and prognostic factors in 372 patients with pulmonary metastases from DTC that received radioiodine therapy. Among patients with iodine-avid pulmonary metastases (68.8%), 60.9% showed a significant decrease in serum Tg levels after I-131 therapy and 60.3% showed a reduction in the size of pulmonary metastases on CT. In only 24.2% of patients, a complete cure was achieved. The significant independent variables between the groups of iodine-avid and non-avid groups were age, the presence of multiple distant metastases, and pulmonary metastatic nodule size; the patients under 40 years old with lung-only metastatic disease and micronodular or miliary metastases seemed to have favorable outcomes [9]. In another recent study with eight patients, the overall effective rate of radioiodine therapy for lung metastases of DTC was 72.5%. This study showed that gender, pulmonary nodule size, the absence or presence of extrapulmonary distant metastases, age, and Tg level at diagnosis were significantly associated with I-131 therapy efficacy; older patients with higher Tg levels at diagnosis and extrapulmonary distant metastases more likely showed poor prognosis. The optimal cutoffs for age and Tg level to predict therapy efficacy were reported to be 46 years old and 55.50 ng/mL, respectively [10].
The contribution of PET/CT with different radiolabelled agents to staging and follow-up of thyroid cancer has been reported in many studies up-to-date. 18F-FDG PET/CT is routinely used in patients of DTC presenting with high Tg levels and negative iodine scintigraphy (TENIS), and in medullary thyroid carcinoma with elevated tumor markers (calcitonin and carcinoembryonic antigen) detected after thyroidectomy. Another application of PET/CT in thyroid cancer is the use of somatostatin analogs labeled with 68Ga-DOTA compounds for evaluation of peptide receptor radionuclide therapy for patients having non-iodine-avid metastatic disease or considering the heterogeneous behavior of metastatic lesions. PET/CT with iodine-124 has also been reported to be used for dosimetric studies to achieve an individualized therapy [12]. As in many other tumor types, intense uptake of 18F-FDG in primary lesion or metastases of DTC indicates a rapidly dividing and dedifferentiated tumor and poor prognosis [13]. In a study comparing the efficacy of 18F-FDG PET/CT and PET/MRI in patients with dedifferentiated thyroid cancer, PET/CT was found to be superior to PET/MRI to detect the pulmonary metastases, while for cervical status, they were equal when PET/CT is performed with contrast enhancement [14]. The pathologic uptake in the thyroid gland or metastases associated with thyroid carcinoma may be found incidentally in a 18F-FDG PET/CT scan made for another known malignancy in other parts of the body [15]. In our patient, the pulmonary metastatic nodules had shown mild 18F-FDG uptake not reaching levels of malignancy, however, intense radioiodine uptake revealing the good differentiation of the tumor and a favorable outcome after radioiodine therapy.
What Can We Learn from This Case?
-
Occult thyroid carcinoma may present with distant metastases without a primary lesion detected on total thyroidectomy.
-
Well-differentiated thyroid cancer metastases may show low 18F-FDG uptake while they are intensely iodine-avid.
-
I-131 therapy is the preferred therapy for metastatic DTC as long as the metastases show iodine uptake.
References
Sampson E, Brierley JD, Le LW, Rotstein L, Tsang RW. Clinical management and outcome of papillary and follicular (differentiated) thyroid cancer presenting with distant metastasis at diagnosis. Cancer. 2007;110:1451–6.
Kalra R, Pawar R, Hasija S, Chandna A, Sankla M, Malhotra C. Frontal bone metastasis from an occult follicular thyroid carcinoma: diagnosed by FNAC. J Cytol. 2017;34:59–61.
Liu H, Lv L, Yang K. Occult thyroid carcinoma: a rare case report and review of literature. Int J Clin Exp Pathol. 2014;7:5210–4.
Borsò E, Boni G, Mazzarri S, Cocciaro A, Gambacciani C, Traino AC, et al. Disseminated bone metastases from occult thyroid cancer effectively treated with debulking surgery and a single dosimetry-guided administration of radioiodine. Rev Esp Med Nucl Imagen Mol. 2015;34:111–5.
Xu B, Scognamiglio T, Cohen PR, Prasad ML, Hasanovic A, Michael Tuttle R, et al. Metastatic thyroid carcinoma without identifiable primary tumor within the thyroid gland: a retrospective study of a rare phenomenon. Hum Pathol. 2017;65:133–9.
Kaseda K, Watanabe K, Sakamaki H, Kazama A. Solitary pulmonary metastasis from occult papillary thyroid carcinoma. Thorac Cancer. 2016;7:261–3.
Qutbi M, Shafeie B, Amoui M, Tabeie F, Azizmohammadi Z, Mahmoud-Pashazadeh A, et al. Evaluation of prognostic factors associated with differentiated thyroid carcinoma with pulmonary metastasis. Clin Nucl Med. 2016;41:917–21.
Kim M, Kim WG, Park S, Kwon H, Jeon MJ, Lee JJ, et al. Initial size of metastatic lesions is best prognostic factor in patients with metastatic differentiated thyroid carcinoma confined to the lung. Thyroid. 2017;27:49–58.
Song HJ, Qiu ZL, Shen CT, Wei WJ, Luo QY. Pulmonary metastases in differentiated thyroid cancer: efficacy of radioiodine therapy and prognostic factors. Eur J Endocrinol. 2015;173:399–408.
Wang R, Zhang Y, Tan J, Zhang G, Zhang R, Zheng W, et al. Analysis of radioiodine therapy and prognostic factors of differentiated thyroid cancer patients with pulmonary metastasis: an 8-year retrospective study. Medicine (Baltimore). 2017;96:e6809. https://doi.org/10.1097/MD.0000000000006809.
Biko J, Reiners C, Kreissl MC, Verburg FA, Demidchik Y, Drozd V. Favourable course of disease after incomplete remission on (131)I therapy in children with pulmonary metastases of papillary thyroid carcinoma: 10 years follow-up. Eur J Nucl Med Mol Imaging. 2011;38:651–5.
Basu S, Parghane RV. Designing and developing PET-based precision model in thyroid carcinoma: the potential avenues for a personalized clinical care. PET Clin. 2017;12:27–37.
Giraudet AL, Taïeb D. PET imaging for thyroid cancers: current status and future directions. Ann Endocrinol. 2017;78:38–42.
Vrachimis A, Burg MC, Wenning C, Allkemper T, Weckesser M, Schäfers M. [(18)F]FDG PET/CT outperforms [(18)F]FDG PET/MRI in differentiated thyroid cancer. Eur J Nucl Med Mol Imaging. 2016;43:212–20.
Kim MS, Sim YS, Lee SY, Jeon DG. Occult thyroid carcinoma detected by FDG-PET scan in elderly osteosarcoma patients: report of two cases. Ann Nucl Med. 2007;21:529–32.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Çermik, T.F., Ergül, N. (2019). A Patient Presented with Extensive Lung Metastases of Papillary Thyroid Carcinoma Without Any Primary Focus Detected on Total Thyroidectomy. In: Özülker, T., Adaş, M., Günay, S. (eds) Thyroid and Parathyroid Diseases. Springer, Cham. https://doi.org/10.1007/978-3-319-78476-2_30
Download citation
DOI: https://doi.org/10.1007/978-3-319-78476-2_30
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-78475-5
Online ISBN: 978-3-319-78476-2
eBook Packages: MedicineMedicine (R0)