Abstract
There are controversial suggestions in the literature about the routine measurement of calcitonin (Ct) in thyroid nodules. Barriers in front of measuring routine serum calcitonin are cost-effectiveness and the possibility of having elevated serum Ct in the absence of medullary thyroid carcinoma (MTC). Here we report a sporadic MTC patient with negative fine needle aspiration biopsy (FNAB) result whose diagnosis was made by preoperative calcitonin measurement. As we perform routine Ct measurement before surgery, the surgeon becomes aware of the MTC earlier, and this gives the opportunity of making an appropriate surgical procedure which is crucial for patients’ outcome.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Thyroid Nodules
- Fine-needle Aspiration Biopsy (FNAB)
- Medullary Thyroid Carcinoma (MTC)
- Controversial Suggestion
- Central Neck Lymph Node Dissection
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Case Presentation
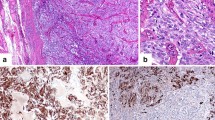
A 45-year-old woman admitted to endocrinology outpatient clinic with a 4-week history of palpable cervical mass. Physical examination revealed grade 1b palpable thyroid gland with 1 cm nodules on both lobes. Other physical examination findings and family history were unremarkable. Thyroid function tests were within the normal limit. Anti-TPO was 117.6 IU/ml (<9 IU/ml). Neck ultrasound (USG) revealed bilateral hypoechoic thyroid nodules with irregular margins and microcalcifications. Fine needle aspiration biopsy (FNAB) from left-sided nodule was benign, while right-sided nodule showed Hurthle cell metaplasia with benign findings. We measured calcitonin (Ct) according to our routine practice. The serum calcitonin level was 4049 pg/ml (0–11.5 pg/ml). Repeated Ct level at another center was >1636 pg/ml (<10 pg/ml) again. Twenty-four-hour urine estimation of catecholamines, normetanephrine and plasma normetanephrine, serum calcium, and parathyroid hormone (PTH) was determined to identify or exclude pheochromocytoma and hyperparathyroidism. All were within the normal limits. RET protooncogene testing was negative. The patient underwent total thyroidectomy and central compartment node clearance (level VI). Postoperative histopathology confirmed thyroid medullary carcinoma of 1.2 cm in the right lobe, papillary microcarcinoma of 0.5 cm at three different foci at the left lobe, and metastatic medullary thyroid carcinoma in the resected lymph nodes. After thyroid operation serum Ct level was 10.3 pg/ml (0–11.5 pg/ml).
2 Discussion
2.1 Evaluation and Diagnosis
The rate of MTC diagnosed only after thyroid operation is approximately 10–15% [1]. This delay in diagnosis can adversely affect the patient’s outcome. Initial surgery is an important modality in the treatment and course of MTC. Diagnosis of MTC before surgery also has significance for the diagnosis of MEN syndromes especially accompanying life-threatening pheochromocytoma in index cases. There are controversial suggestions in the literature about the routine measurement of Ct in thyroid nodules. “The American Thyroid Association (ATA) Guideline for Thyroid Nodule and Differentiated Thyroid Cancer” does not recommend either for or against routine measurement of serum Ct (Recommendation 4) [2], while “The American Association of Clinical Endocrinologists (AACE), Associazione Medici Endocrinologi (AME), and European Thyroid Association (ETA) Thyroid Nodule Guidelines” recommend measurement of basal serum Ct level as a useful test in the initial evaluation of thyroid nodules [3]. The reasons for ATA recommendation are unresolved issues of assay performance, lack of pentagastrin availability in the United States, and potential biases in the cost-effectivity analysis [2]. The ATA recommendation and evidence quality about Ct are insufficient. There are false-negative and false-positive results of basal Ct measurement that cause misdiagnosis. Technical problems, (hook effect, heterophilic antibodies), some drugs (omeprazole), chronic renal failure, pernicious anemia, and lymphocytic thyroiditis are some reasons of false-positive results, while nonsecretory medullary thyroid carcinoma is the false-negative result [4]. If basal calcitonin level is increased, the test should be repeated, and if confirmed in the absence of modifiers, a pentagastrin or calcium stimulation test will increase the diagnostic accuracy [3]. However, pentagastrin is not available in every country, and there are problems with calcium stimulation test like cutoff levels, cost, assay performance, sensitivity, and specificity [2]. The main rationale for the recommendation of AACE, AME, and ETA concerning Ct measurement in the thyroid nodule is its higher sensitivity compared to FNAB [5,6,7,8,9,10,11]. As it is in our case, FNAB was not able to diagnose the MTC of the patient. If routine calcitonin had not been measured, the patient could be misdiagnosed.
Another problem in the routine measurement of basal calcitonin for every thyroid nodule is the cost-effectiveness of this screening. There are studies from the United States and European countries demonstrating that it is valuable to measure calcitonin level [12,13,14]. However, the costs of finding one patient with abnormal results and MTC are quite reasonable for routine basal Ct measurement, compared with the potential costs of missing the diagnosis of this treatable malignant condition [15].
2.2 Management
One of the important benefits of knowing preoperative Ct is the tailoring of surgical treatment. Central neck lymph node dissection is an important and necessary treatment modality in the management of MTC. As we perform routine Ct measurement before surgery, the surgeon becomes aware of the MTC earlier, and the procedure is at least total thyroidectomy and central neck lymph node dissection as it was in our case. Also, preoperative Ct measurement is effective in the detection of clinically occult MTC [5,6,7,8]. In addition, screening thyroid nodules with serum Ct measurement allows the diagnosis and treatment of MTC at an earlier stage, resulting in a better outcome compared with MTC not detected by serum Ct measurement [13].
3 Follow-Up and Outcome
The patient has been under follow-up for 6 years. Her postoperative serum calcitonin level was 10.3 pg/ml (0–11.5 pg/ml).After 5 years of follow-up, last serum calcitonin level was 13.56 pg/ml (0–6.4 pg/ml). Neck USG revealed nothing pathologic. The patient is on L-thyroxin replacement therapy.
3.1 The Future
Barriers in front of measuring routine serum Ct are cost-effectiveness and the possibility of having elevated serum Ct in the absence of an MTC. Other different diagnostic modalities can help us in this regard. Recent small studies have shown improved sensitivity with Ct measurement in FNA washout fluid with as high as 100% accuracy [16]. Procalcitonin, the precursor of Ct, has been reported as a potential MTC marker and could be a good candidate for a first-line screening test to exclude MTC in patients with suspicious thyroid nodules [17].
What Can We Learn from This Case?
-
Ct measurement is an effective method for the diagnosis of MTC and is superior to FNAB concerning diagnosis of MTC.
-
Recognition of MTC by preoperative calcitonin measurement increases the chance of curative therapy by diagnosing MTC in the early stages and then performing the appropriate surgical procedure.
References
Ahmed SR, Ball DW. Incidentally discovered medullary thyroid cancer: diagnostic strategies and treatment. J Clin Endocrinol Metab. 2011;96:1237–45.
Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE, et al. 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American Thyroid Association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid. 2016;26:1–133.
Gharib H, Papini E, Paschke R, Duick DS, Valcavi R, Hegedus L, et al. American Association of Clinical Endocrinologists, Associazione Medici Endocrinologi, and European Thyroid Association medical guidelines for clinical practice for the diagnosis and management of thyroid nodules: executive summary of recommendations. J Endocrinol Investig. 2010;33(5 Suppl):51–6.
Elisei R, Romei C. Calcitonin estimation in patients with nodular goiter and its significance for early detection of MTC: European comments to the guidelines of the American Thyroid Association. Thyroid Res. 2013;6(Suppl 1):S2.
Pacini F, Fontanelli M, Fugazzola L, Elisei R, Romei C, Di Coscio G, et al. Routine measurement of serum calcitonin in nodular thyroid diseases allows the preoperative diagnosis of unsuspected sporadic medullary thyroid carcinoma. J Clin Endocrinol Metab. 1994;78:826–9.
Rieu M, Lame MC, Richard A, Lissak B, Sambort B, Vuong-Ngoc P, et al. Prevalence of sporadic medullary thyroid carcinoma: the importance of routine measurement of serum calcitonin in the diagnostic evaluation of thyroid nodules. Clin Endocrinol. 1995;42:453–60.
Niccoli P, Wion-Barbot N, Caron P, Henry JF, de Micco C, Saint Andre JP, et al. Interest of routine measurement of serum calcitonin: study in a large series of thyroidectomized patients. The French Medullary Study Group. J Clin Endocrinol Metab. 1997;82:338–41.
Vierhapper H, Raber W, Bieglmayer C, Kaserer K, Weinhäusl A, Niederle B. Routine measurement of plasma calcitonin in nodular thyroid diseases. J Clin Endocrinol Metab. 1997;82:1589–93.
Kaserer K, Scheuba C, Neuhold N, Weinhäusel A, Vierhapper H, Haas OA. C-cell hyperplasia and medullary thyroid carcinoma in patients routinely screened for serum calcitonin. Am J Surg Pathol. 1998;22:722–8.
Ozgen AG, Hamulu F, Bayraktar F, Yilmaz C, Tüzün M, Yetkin E, et al. Evaluation of routine basal serum calcitonin measurement forearly diagnosis of medullary thyroid carcinoma in seven hundred seventy-three patients with nodular goiter. Thyroid. 1999;9:579–82.
Hahm JR, Lee MS, Min YK, Lee MK, Kim KW, Nam SJ, et al. Routine measurement of serum calcitonin is useful for early detection of medullary thyroid carcinoma in patients with nodular thyroid diseases. Thyroid. 2001;11:73–80.
Verga U, Ferrero S, Vicentini L, Brambilla T, Cirello V, Muzza M, et al. Histopathological and molecular studies in patients with goiter and hypercalcitoninemia: reactive or neoplastic C-cell hyperplasia? Endocr Relat Cancer. 2007;14:393–403.
Elisei R, Bottici V, Luchetti F, Di Coscio G, Romei C, Grasso L, et al. Impact of routine measurement of serum calcitonin on the diagnosis and outcome of medullary thyroid cancer: experience in 10,864 patients with nodular thyroid disorders. J Clin Endocrinol Metab. 2004;89:163–8.
Cheung K, Roman SA, Wang TS, Walker HD, Sosa JA. Calcitonin measurement in the evaluation of thyroid nodules in the United States: a cost-effectiveness and decision analysis. J Clin Endocrinol Metab. 2008;93:2173–80.
Turk Y, Makay O, Ozdemir M, Ertunc G, Demir B, Icoz G, et al. Routine calcitonin measurement in nodular thyroid disease management: is it worthwhile? Ann Surg Treat Res. 2017;92:173–8.
Hu MI, Ying AK, Jimenez C. Update on medullary thyroid cancer. Endocrinol Metab Clin N Am. 2014;43:423–42.
Lim SK, Guéchot J, Vaubourdolle M. Negative predictive value of procalcitonin in medullary thyroid carcinoma. Ann Biol Clin. 2016;74:213–8.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Adaş, M., Adaş, G. (2019). Should Calcitonin Be Measured in Every Thyroid Nodule?. In: Özülker, T., Adaş, M., Günay, S. (eds) Thyroid and Parathyroid Diseases. Springer, Cham. https://doi.org/10.1007/978-3-319-78476-2_14
Download citation
DOI: https://doi.org/10.1007/978-3-319-78476-2_14
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-78475-5
Online ISBN: 978-3-319-78476-2
eBook Packages: MedicineMedicine (R0)