Abstract
Phenotypic sex differences in coronary artery disease (CAD) and its risk factors have been apparent for many decades in basic and clinical research; however, whether these are also present at the gene level and thus influence genome-wide association and genetic risk prediction studies has often been ignored. From fundamental and medical standpoints, this is critically important to assess in order to fully understand the underlying genetic architecture that predisposes to CAD and better predict disease outcomes based on the interaction between genes, sex effects, and environment. In this chapter we aimed to (1) integrate the history and latest research from genome-wide association studies for CAD and clinical and genetic risk scores for prediction of CAD, (2) highlight sex-specific differences in these areas of research, and (3) discuss reasons why sex differences have often not been considered and, where present, why sex differences exist at genetic and phenotypic levels and how important they are for consideration in future research. While we find interesting examples of sex differences in effects of genetic variants on CAD, genome-wide association and genetic risk studies have typically not tested for sex-specific effects despite mounting evidence from diverse fields that these are likely very important to consider at both the genetic and phenotypic levels. In-depth testing for sex effects in large-scale genome-wide association studies that include autosomal and often excluded sex chromosomes alongside parallel improvements in resolution of sex-specific differences for risk factors and disease outcomes for CAD has the potential to substantially improve clinical and genetic risk prediction studies. Developing sex-tailored genetic risk scores as has been done recently for other disorders might be also warranted for CAD. In the era of precision medicine, this level of accuracy is essential for such a common and costly disease.
 GWAS and risk scores. Art work by Piet Michiels, Leuven, Belgium
GWAS and risk scores. Art work by Piet Michiels, Leuven, Belgium
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- GWAS
- Coronary risk factors
- Single nucleotide polymorphism
- Sex-specific analysis
- Genetic risk score
- Women’s Genome Health Study
History, Utility, and Sex Biases in Clinical Risk Scores for CAD
Historically, cardiovascular disease (CVD) risk assessment was initiated during the middle of the twentieth century spurred on by the spike in deaths in the USA due to coronary artery disease (CAD) that rose from ~10% of all deaths in 1900 to ~40% by 1960 [1]. This disease epidemic resulted in the Framingham Heart Study (FHS) being founded in 1947 by the US National Heart Institute in order to study and uncover causes of CVD in a relatively stable and well-defined community of mostly European ancestry [1]. Over a decade later in 1960, results from the FHS resulted in the initial concept of coronary risk factors (CRFs, see Fig. 38.1 for a comparison of their predictive performance in Framingham males and females), including, for example, high blood pressure, high cholesterol, history of smoking, type 2 diabetes (T2D), age, and sex that are observable in the preclinical phase before the disease occurs and are predictive of future CVD outcomes. After this initial success in providing some basic translational disease indicators, research over the following 20 years provided deeper understanding of the multiplicative nature of CRFs and the development of a cardiovascular risk prediction algorithm called the Framingham risk score (FRS) pioneered again by Framingham investigators. The first Framingham risk prediction algorithm to predict CAD (FRS-CAD) was designed in 1998 to combine individual patient’s risk factor information and produce a 10-year absolute risk score for angina, myocardial infarction (MI) , or death due to CAD in order to help clinicians decide whether therapy should be initiated [2]. In 2001, the Third Report from the Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) recommended a modified 10-year Framingham risk score for CAD (ATP III-FRS-CAD) combined with a web-based calculator for use in patients exhibiting two or more risk factors to decide on thresholds for treatment of low-density lipoprotein (LDL) cholesterol [3, 4]. It was estimated that the use of these risk prediction scores increased the average life expectancy of CAD patients by 3 years in the USA [5].
Variation in lifetime coronary artery disease (CAD) risk depending on coronary risk factors (CRFs) in Framingham men and women. Each CRF was divided into quintiles (only highest, medium, lowest shown in Kaplan-Meier plots). Dashed lines are 95% CIs. Values shown in plots: Harrell’s C-index difference (ΔC) and significance test (assessed using a correlated jackknife test) between two models (with/without each CRF); net reclassification improvement (NRI) and associated p-value. SBP systolic blood pressure, TC total cholesterol; HDL, high-density lipoprotein cholesterol; T2D, type 2 diabetes. p-values: *p < 0.05, **p < 0.01, ***p < 0.001
While the FRS has often been the standard against which other subsequently developed CAD risk prediction tools are measured [2, 6,7,8,9], the general applicability of Framingham risk equations to modern populations has been debated over the last 10–15 years. This was partly because the FRSs are based on an ethnically and geographically limited, male-dominated sample when cardiovascular risk profiles were less well developed and also because many recent studies in diverse populations suggest that the FRS poorly classifies risk, particularly in women [10,11,12,13,14,15]. This is likely partly due to sex differences in progression and outcomes of CAD. For example, approximately 20% of all coronary events in women occur in the absence of major CRFs [16], and many women with CRFs do not experience coronary events [17]. As a consequence, the Reynolds Risk Score (RRS) for women was developed in 2007 that included C-reactive protein and parental history of premature CAD [18], and a revised Framingham risk score (FRS-CVD) that included increasingly common atherosclerotic cardiovascular disease (ASCVD ) events (i.e., stroke) was developed in 2008 [13]. The RRS for women [18] tested 35 potential risk factors on 24,558 initially healthy US women, and the resulting accuracy of the clinical risk score was greatly improved demonstrating the benefits of a sex-specific algorithm. This was further supported by a study in 2008 where the RRS for men was tested and optimized in 10,724 US men, which also significantly improved global cardiovascular risk prediction [19]. While we largely discuss US-based risk scores here, other non-US-based consortia have also developed other risk prediction algorithms (all simply include sex as a covariate) including, for example, the German Prospective Cardiovascular Munster Heart Study (PROCAM ) [20], the European Systematic Coronary Risk Evaluation (SCORE ) system [21], and QRISK2 [22].
Most recently, the American Heart Association (AHA) and the American College of Cardiology (ACC) developed a new ASCVD risk score (AHA-ACC-ASCVD) in 2013 (see Fig. 38.2 below for an indication of its performance in Framingham males and females) derived from four (including FHS data) racially and geographically diverse prospective cohort studies [23,24,25,26] that utilize the same traditional CRFs as the original FRSs while offering tailored equations for white and African-American men and women in order to improve and guide ASCVD risk-reducing therapy [26]. However, problems still reside in this most contemporary risk score as it overestimates risk in independent cohorts [27, 28]. Moreover, there is a certain level of misclassification of most clinical risk scores developed to date depending on sex. For example, DeFilippis et al. [29] compared performance of the AHA-ACC-ASCVD risk score with four other risk prediction equations (FRS-CAD, FRS-CVD, ATP III-FRS-CAD, RRS) utilizing the Multi-Ethnic Study of Atherosclerosis (MESA ) study, which is a community-based, sex-balanced, multiethnic cohort consisting of 54% women, 42% European, 26% African-American, 20% Hispanic, and 12% Chinese. The authors found that the performance of the five risk scores to discriminate between those who did or did not have an ASCVD or CAD event was fairly similar. However, the FRS-CAD, FRS-CVD, ATP III-FRS-CAD, and AHA-ACC-ASCVD overestimated CAD and ASCVD risk by 37–154% in men. In comparison, the RRS estimated ASCVD and revascularization events in men relatively accurately (9% discordance). In women, the FRS-CVD accurately estimated risk (8% discordance), while the FRS-CAD, ATP III-FRS-CAD, and AHA-ACC-ASCVD overestimated risk (46–67% discordance) and the RRS underestimated (−21% discordance) the rate of events [29].
Lifetime risk of coronary artery disease (CAD) depending on individual variation in the AHA-ACC-ASCVD clinical risk score in Framingham men and women. AHA-ACC-ASCVD scores were divided into quintiles (highest, medium, lowest shown in Kaplan-Meier plots). Dashed lines are 95% CIs. For Framingham males, integration of the AHA-ACC-ASCVD score into a simple CAD risk prediction model (first five principal components on genotypes) improved 10-year risk prediction (Harrell’s C-index, C-index difference (ΔC) between two models assessed using a correlated jackknife test) by 3.4% (p < 0.001) with a net reclassification improvement (NRI) score of 0.45 (p < 0.001). For females, addition of the same score did not significantly improve 10-year C-index but did significantly improve the NRI (0.43, p < 0.001). P-values: *p < 0.05, **p < 0.01, ***p < 0.001
In summary, none of the most well-known ASCVD and CAD clinical risk prediction scores in the USA are highly accurate for both men and women [29]. More generally, CRFs underlying clinical risk scores provide only modest discrimination and cannot fully capture underlying risk [30]. This has clinical relevance for the current 10-year predicted risk threshold of 7.5% in the USA: over- or underestimation is likely to result in individuals with lower or higher risk receiving or not reaching the cutoff value for preventative treatment (statins), respectively [31,32,33]. Further testing and refinement of clinical risk scores, tailored to distinct populations and sex, is needed. While the RRS and AHA-ACC-ASCVD developed between 2007 and 2013 offer sex-specific clinical risk prediction algorithms, we now know that many more sex differences exist in the progression of CRFs and cardiovascular outcomes between men and women [34,35,36,37] (discussed below) that need to be accounted for in order to improve prediction of CAD and broader CVD. With the ever-increasing availability of large clinical and biobank-scale data as well as inclusion of genetic risk predictors (discussed below), these will lead to new more powerful clinical risk prediction equations.
GWAS and Sex-Specific Genetic Effects on CAD
Typical of common diseases, individual risk for CAD is modulated by the interplay between lifestyle and genetic factors [38]. Some of the first evidence that CAD had a genetic component was through early clinical observations [39], twin [40, 41] and cohort [42, 43] studies, which found increased CAD risk depending on whether there was direct or indirect family history of the disease and also estimated the heritability of CAD as ~50%. Genome-wide methods estimate CAD heritability between 40% and 50% [44]. Collectively these seminal studies laid the groundwork that helped drive the development of modern genetic tools to better define the underlying genetic architecture of CAD and begin to translate these findings into practice.
Historically, linkage analysis studies on families with a predisposition to early-onset CAD provided some initial insights into Mendelian or monogenic-like drivers of CAD. Linkage analysis can be an effective means of utilizing large multigenerational families to identify highly penetrant variants responsible for disease. Familial hypercholesterolemia defined by a heritable pattern of increased cholesterol and premature CAD was first described in 1938 [45], and in 1985 a deletion in the LDLR gene was found to be causative [46] demonstrating that a discrete mutation in a single gene predisposed to CAD. Subsequent family-based studies have identified further mutations in APOB, PCSK9, and ABCG5/ABCG8 [47,48,49,50] that contribute to familial hypercholesterolemia, but beyond this condition that predisposes to CAD, the use of family studies to identify drivers of CAD has been limited. This was especially clear in linkage studies performed on families with more common presentations of CAD that failed to detect any susceptibility loci [51, 52]. Therefore, despite the tendency to cluster in families, these earlier studies highlighted the complex polygenic nature of CAD.
After the sequencing of the human genome in the late 1990s and early 2000s, which resulted in ~1.5 million single nucleotide polymorphisms (SNPs), researchers used small-scale candidate gene studies (i.e., using previously identified potentially causative variants) to identify genes involved in disease; however, this underpowered approach with small sample sizes often resulted in false-positive findings [53, 54]. Many of the larger-scale candidate gene studies on CAD (or stroke) performed in the mid-late 2000s pooled data on both sexes and added sex as a covariate [55,56,57,58,59,60] without consideration for potential sex-specific effects. However, in 2002, a Japanese case-control study that tested variants predictive for MI found differences in the significance of those between males and females when they were analyzed separately [61], supporting the presence of sex-specific genetic risk factors for CAD. In 2008, a case-control study of over 14,000 Finnish individuals where authors tested for sex-specific effects on 46 candidate genes for CAD and CVD found that while some variants conferred risk in both sexes, others showed significant effects only in males (e.g., rs2069840 in IL6 for CVD) and females (e.g., SNPs in SELENOS for stroke) with a larger number of sex-specific effects for women than men [62]. These studies showed some of the first evidence for sex differences in the effects of known variants in genes underlying CAD and CVD.
Subsequent further sequencing with the availability of cheaper genotyping chips (designed to capture common variation in populations) and careful documentation by the International HapMap Consortium of ~3.1 million SNPs in 270 individuals from four ethnic backgrounds in 2007 [63, 64] provided the necessary resources for initial genome-wide association studies (GWAS ). The first CAD GWAS was published in 2007, and during that time, three independent groups reported variants at the 9p21 locus with the risk allele significantly increasing risk of CAD in European populations by approximately 30% [65,66,67]. Following those initial discoveries, progressively larger sample sizes have been used to define many variants with relatively small effects that contribute significantly to CAD. Over the last 5 years, large international consortia have utilized massive sample sizes from mixed ethnic backgrounds in GWAS meta-analyses for CAD and have identified ~60 distinct genetic loci significantly linked to CAD [68,69,70,71,72,73]. Six more common variant loci were identified in 2017 [74], and rare variant (captured with whole exome/genome sequencing, i.e., not included on genotyping chips) association studies have identified at least nine genes in which mutations significantly alter CAD risk [75].
The majority of common CAD variants identified to date have a minor allele frequency of >5% in most worldwide populations, are located in nonprotein-coding regions of the genome highlighting their impact on CAD risk through gene regulation [73, 76], only cause modest increases in CAD risk (i.e., typically <20% change in risk per allele), collectively explain ~30–40% of CAD heritability [72, 73], and just under half (~40%) modulate CAD risk by influencing CRFs such as cholesterol, T2D, and hypertension [68, 72, 77] suggesting that the mechanisms whereby a majority of these loci mediate CAD risk remain unknown.
Since the first CAD GWAS was performed a decade ago (including previous candidate gene studies), researchers to date have typically not tested for sex-specific effects despite earlier findings (particularly in candidate gene studies) that these exist. Most studies have pooled men and women (adjusting for sex as a covariate) and typically account for population structure by including the first 5–10 principal components derived on genotypes from the sample. For example, one of the most recent GWAS meta-analyses of CAD [73] that used 60,801 CAD cases and 123,504 controls from a mix of males and females from different ancestral backgrounds (77% European, South (13% India and Pakistan) and East (6% China and Korea) Asian, Hispanic and African-American ~4%) included sex as a covariate. However, a slightly earlier study [72] published by the same consortium with a similar sample performed subgroup analyses by sex, and while they observed no higher risk trends for males vs females for any of the 46 genome-wide significant CAD risk loci identified in the main analysis (with sex added as a covariate), they did find one new locus (rs16986953 in gene desert, 1.3 Mb away from APOB) that reached genome-wide significance in males [72] but not females. Other non-CAD large-scale GWAS studies have revealed significant sex differences in contributing genetic variants [78,79,80] demonstrating that these are present in many polygenic traits and diseases.
A small subset of genome-wide CAD studies focusing on women exist but have often been limited by sample sizes with insufficient power to test for association [81]. For example, in 2012 Orozco et al. [82] tested for sex-specific associations in the Wellcome Trust Case Control Consortium of 399/1527 cases and 1492/1446 controls, for women and men, respectively, and found no CAD variants (previously identified from GWAS ) were significant in women or men. More recent studies with larger sample sizes have found some convincing sex-specific genetic effects on CAD. Goodarzynejad et al. [83] in a sex-stratified study discovered a SNP in SCARB1 (plasma membrane receptor for HDL) was associated with CAD in women but not men. A SNP in CPS1 has also been found significantly associated with CAD in women but not men [84]. Liu et al. [78] found a SNP on 9p21 that showed a large (p = 1.38 × 10–8) male-specific association with CAD, but not females (p = 0.167). Taylor et al. [80] found sex-specific SNPs associated with risk factors (HDL, LDL) for CAD. This supports earlier findings from candidate gene studies that uncovered sex-specific genetic effects on CAD. Other recent GWAS have found autosomal variants contributing to complex traits in a sex-specific manner (e.g., adiposity [85]). Therefore, the investigation of sex-specific effects on CAD with larger better-powered studies is warranted. Resolving the full complement of shared and sex-specific CAD genetic loci will help provide a better understanding of the pathological pathways in progression and thus improve individually tailored treatments for this disease.
Notably, GWAS to date have almost exclusively focused on autosomal variation [86], even though the X chromosome is included on all current microarrays, and as a result, the role the X chromosome plays in CAD (and most complex diseases) remains largely unknown. This is mainly due to difficulty in accounting for analytical problems arising from the X’s unique mode of inheritance and expression (i.e., dosage compensation in females), but recent analytical tools to perform XWAS [87] could begin to resolve this. The Y chromosome might also bring further understanding of sex-based differences in CVD development and outcomes [37]. For example, significant associations between Y chromosome variants and blood pressure have been found in different populations [88, 89], and some studies have suggested that blood pressure in men is largely determined by paternal (and not maternal) blood pressure status [90]. In males, the Sry locus of the Y chromosome contributes to hypertension through regulation of tyrosine hydroxylase, whereas in women, estrogen modulates the activity of this enzyme [36]. Therefore, modification of blood pressure, a key risk factor for CAD, is partly regulated by different genetic loci interacting with environmental stimuli that vary between males and females (i.e., changes in estrogen with pregnancy and menopause, discussed below). For an in-depth discussion of sex-specific differences in CVD related to the sex chromosomes, see Sampson et al. [37], Kling et al. [36], and Regitz-Zagrosek and Kararigas [35]. A recent study has also shown CVD is more prevalent among patients with pathogenic mtDNA mutations [91]. Given the seemingly incomplete autosomal nuclear genetic picture of CAD, variation in sex chromosomes and mtDNA could represent part of the missing heritability of CAD.
Genetic and Genomic Risk Prediction in CAD
While many genetic loci for CAD have now been identified, individually these are not clinically useful. For example, based on the most recent meta-analysis [73], the 9p21 locus remains the strongest genetic risk factor for CAD boasting an impressive significance of p = 2.29 × 10−98; however, the odds ratio (OR) for the effect allele is a modest 1.21 [92]. This represents the basis for recently developed genetic risk scores (GRS) that aim to improve CAD risk prediction. By combining GRS with or without CRFs (often referred to as modifiable risk factors because of the large environmental component to their variation), this should provide more accurate risk stratification of individuals [33, 93]. GRS are calculated essentially by counting the number of risk alleles (adjusted for effect size) inherited for each individual in a given population and provide a quantitative measure of genetic risk [94]. While family history might naturally serve as a substitute for genetic risk, individual risk loci and GRS predict CAD independent of family history, and the association between family history and CAD tends not to be attenuated after the inclusion of GRS [95]. This suggests that the proportion of heritability captured by current GRS is not currently high enough to erode the predictive power of family history and that family history of CAD partially reflects common environment effects.
The first attempt to include genetic markers for CVD prediction was in 2008 where variants associated with cholesterol were used to predict cardiovascular events [96] and extended later with nine significant independent risk variants for CAD [68]. These initial studies showed that individuals in the top GRS quintile had a twofold increased risk of CAD compared to those in the lowest GRS quintile [68] and paved the way for the exploration of various GRS based on different combinations of genetic loci for CAD in different populations [96,97,98,99,100,101,102,103,104,105]. For example, Mega et al. [106] utilized a GRS based on 27 CAD genetic risk variants (GRS27) and showed that genetic risk is independent of CRFs. Shortly after, Tada et al. [95] incorporated these same 27 with additional 23 CAD risk variants to form a 50-variant GRS (GRS50) and tested its performance on 23,595 individuals from the Malmo Diet and Cancer Study. They found their GRS50 further significantly improved CAD discrimination (i.e., C-index: measures how well a model discriminates individuals with(out) the outcome of interest; values range from 0.5 (performs no better than random) to 1.0 (perfectly distinguishes outcomes)) and reclassification (estimates improvement in performance of risk prediction model after additional risk variable is included). A recent study in 2016 by Abraham et al. [107] advanced the GRS by taking account of 49,310 small-effect SNPs predicted to underlie polygenic CAD to construct a genomic risk score (GRS49k), and tested this on 12,676 Finnish men and women (Cox regression stratified by sex). The GRS49k confirmed the increased predictive value of including a large number of SNPs, by improving CAD risk prediction largely independently of CRFs (including family history) and significantly improved 10-year CAD risk prediction when it was combined with the ATP III-FRS-CAD or AHA-ACC-ASCVD clinical risk scores.
These studies show risk stratification provided by GRS is superior to clinical risk scores and the inclusion of many genetic risk variants significantly improves prediction of CAD outcomes. This could be particularly important in asymptomatic individuals without major risk factors. Because DNA is essentially stable across the lifetime of individuals, genetic risk can be obtained at birth. GRS could therefore be particularly useful for very early (i.e., young adults) intervention, which is especially important for a disease like CAD that begins to develop very early in life and is a result of lifetime modifiable exposures (diet, smoking, exercise) interacting on a background of low to high genomic risk. Adherence to a healthy lifestyle will be particularly important for young individuals with a high CAD GRS. For example, a recent analysis of high GRS individuals found a 46% attenuation of CAD risk in those with a favorable versus unfavorable lifestyle [38], and in another study a 50% reduction in CAD risk was achieved through statin therapy in those with high GRS [106]. Another recent study importantly showed the ability of GRS not only to predict incident CAD but also recurrent CAD independent of all CRFs and family history [106]. This shows that GRS hold great potential to improve both primary and secondary prevention strategies for CAD.
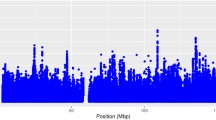
While the performance of GRS for CAD prediction is now being tested on less well-studied populations [98, 108,109,110,111], almost all GRS studies to date have not examined sex-specific effects in GRS. Of the few studies that have, the predictive performance and ability of GRS to stratify high- and low-risk individuals for CAD tends to perform much more poorly in women. For example, Paynter et al. [101] used a 101 SNP GRS based on GWAS loci significantly associated with CVD (or intermediate phenotypes) and found the GRS hazard ratio was initially weak (1.02, p = 0.006) but then not significantly associated with incident CVD in multivariable models in the Women’s Genome Health Study (WGHS ). Compare this to some of the most recent GRS predicting CAD, where hazard ratios for GRS are typically highly significant ranging from 1.27 to 1.74 [102, 103, 107] in multivariable models. A recent study demonstrated that the ability of the GRS49k and CRFs to stratify high- and low-risk individuals for CAD performed much better in males than females (e.g., see Fig. 38.3 and Fig. S11–S13 in Abraham et al. [107]). This is also supported statistically by subsequent analyses on these cohorts that highlight male-female differences for key risk prediction performance indicators (see Fig. 38.3 for estimates).
Differences in the ability of the genomic risk score (GRS49k) to stratify men and women into high and low coronary artery disease (CAD) risk groups. Plots show Kaplan-Meier estimates for cumulative risk up to age 75 in 12,676 FINRISK and 3406 Framingham Heart Study (FHS) men and women. GRS were grouped into quintiles (only 0–20, 40–60, 80–100% shown), with vertical bars showing the age at which each group attained a cumulative CAD risk of 10%. Dashed lines are 95% CIs (Sourced from Abraham et al. [107]). For Framingham males, integration of the GRS with a simple CAD risk prediction model (first five principal components on genotypes) or complex model (first five PCs, total and HDL cholesterol, systolic blood pressure, T2D, smoking, treatment for high blood pressure, family history of CAD) improved 10-year risk prediction (Harrel’s C-index, C-index difference between two models assessed using a correlated jackknife test) by 2.5% (p = 0.02) to 1.6% (p = 0.05), respectively. For Framingham females, integration of the GRS with simple and complex CAD risk prediction models did not improve 10-year risk prediction with C-index changing by 0.2% (p = 0.78) to 0.03% (p = 0.86), respectively. The same sample and methods as described in Abraham et al. [107] were used to obtain these estimates
Less successful prediction and stratification in females is perhaps not surprising in these studies given the combination of genetic and phenotypic biases that currently exist in CAD research. Current GRS are based on variants from GWAS that insufficiently capture sex-specific genetic effects on CVD and CAD (particularly females, discussed above), and clinical definitions for CAD outcomes (i.e., progression, presentation, age at onset) are male-dominated, resulting in lower specificity and accuracy of CAD outcomes captured and predicted in females. Testing a sex-specific GRS for CAD might be appropriate. Sex-tailored GRS have been constructed in other fields for conditions and diseases other than CAD. For example, female-specific GRS have been tested in relation to natural menopause [112], polycystic ovary syndrome (PCOS ) [113], multiple sclerosis [114], and breast cancer [115], and a male-specific GRS has been tested for prostate cancer [116]. Indeed, developing sex-specific GRS can be useful when there are known differential sex differences in clinical phenotypes [117]. For CAD, the success of this will depend on better annotation of sex-specific variants identified in large GWAS that specifically search for sex-specific effects.
Improvement of Future Clinical and Genetic Risk Scores for CAD Through More Precise Definitions of Sex-Specific Effects
As is the case for many common human diseases, improving our understanding of the genetic architecture underlying CAD, which is essential for enhancing predictive performance of GRS, must also involve parallel improvements in the definitions of sex-specific differences in phenotypic presentations of CAD, which will reduce case/control misclassification and improve precision and risk stratification of males and females. The performance of clinical risk scores will also benefit from more refined CRFs that account for sex differences in their progression and interactions with environmental stimuli. As we discuss below, using exactly the same CAD and CRF definitions for males and females is not optimal in the era of precision medicine.
Firstly, because pathophysiology of CAD in men and women is quite different, grouping males and females and simply including sex as a covariate will reduce trait specificity and cause a level of bias in GWAS [118] from sex-based misclassification of CAD cases/controls. This bias is likely further compounded (especially for rarer genetic variants or variants with weaker yet significant effects) with the disproportionate ratio of men and women when they are pooled in GWAS . In general, analyzing sex differences in genetic associations for CAD risk is complicated because the age at onset is sex-dependent. For example, mortality from CAD tends to appear more commonly [119] and much earlier in males than females [120, 121]. Various factors have been proposed (e.g., psychological stressors, access and utilization for health care, inappropriate surveillance, and treatment guidelines for women) to contribute toward this mortality difference [36].
Progression of CAD shows some distinct differences by sex. For example, more severe structural/functional abnormalities in epicardial coronary arteries typify CAD progression in men, while more abnormal coronary reactivity, microvascular dysfunction, and plaque erosion/distal microembolism typify CAD progression in women [122]. This has led to the recent suggestion that the definition of ischemic heart disease (IHD) might be more appropriate for women than CAD [81]. Heart failure in women is often more associated with preserved ejection fraction (HFpEF), and if women suffer from left ventricular hypertrophy, they have a higher mortality risk compared to men [123]. Compared to women, men also present with more severe atherosclerosis in their coronary arteries. Correspondingly, MI typically occurs 10 years earlier in men [35]. Some recent studies suggest that most newly identified CAD GWAS loci mainly predict atherosclerosis [124]. Given that the pathophysiology of CAD can be roughly divided into three major processes (plaque formation (atherosclerosis), plaque rupture, thrombotic response to plague rupture [125]) and atherosclerosis tends to be more typical of male CAD progression [125], this suggests many newly identified CAD loci might be more predictive in males. This corresponds with differences of GRS to stratify high- and low-risk males and females for CAD outcomes [107] discussed in Sect. “Genetic and Genomic Risk Prediction in CAD” above.
Risk factors for CAD (i.e., cholesterol, BP, T2D) also show distinct differences between men and women [126,127,128,129,130,131,132] that often vary with age (see Fig. 38.4 for examples in Framingham males and females). For example, even though men often present with systemic hypertension at an earlier age, the incidence of pulmonary hypertension is greater in women than men [133,134,135]. Further, hypertension and T2D can be triggered by pregnancy and menopause [36]. For example, mothers experiencing pregnancy disorders such as preeclampsia and gestational diabetes subsequently have a much higher risk of hypertension and T2D [136,137,138,139,140,141,142]. Menopause also involves significant changes in estrogen levels, and estrogen modulates tyrosine hydroxylase, which is a key enzyme in the development of hypertension [36]. Correspondingly, premenopausal women have a reduced risk for hypertension and IHD compared to men, but this reverses after menopause [143, 144]. There is some evidence that women may be more protected from atherosclerosis before menopause [35], which is supported by the observation that women who have hormonal (estrogen) disturbances due to PCOS develop atherosclerosis and subsequent MI earlier in life [145, 146]. Men with a mutation in the estrogen receptor gene (ESR1) also have earlier CAD [147, 148].
Variation in coronary risk factors (CRFs) between the ages of 20 and 80, 1955–2005, for males and females in the Framingham Heart Study. Note the very different lifetime profiles of cholesterol for males and females. At around 60 years of age, total cholesterol (TC) tends to be much higher in females compared to males, and high-density lipoprotein (HDL) cholesterol levels in females tend to be generally higher in females compared to males. Plots show the 3-D surface accurately derived from many repeated individual measures (total cholesterol measured 37,317 times in 6605 males, 44,798 times in 7518 females; systolic blood pressure (SBP) measured 45,990 times in 6626 males, 58,690 in 7546 females; HDL cholesterol measured 17,207 times in 5334 males, 20,095 times in 6210 females) in a generalized additive model. Each plot shows example of individual repeated measures from three randomly chosen individuals
In summary, more accurate classification of phenotypic sex differences in CAD risk factors, environmental stimuli that interact with these differently by sex, and sex differences in clinical presentations of CAD will in turn allow for further and more accurate identification of genes in female-focused and male-focused studies [149] and better predictive models that utilize GRS and CRFs . This will become increasingly important as we move further into the era of precision medicine.
References
Wong ND, Levy D. Legacy of the Framingham heart study: rationale, design, initial findings, and implications. Glob Heart. 2013;8:3–9.
Wilson PW, D’Agostino RB, Levy D, Belanger AM, Silbershatz H, et al. Prediction of coronary heart disease using risk factor categories. Circulation. 1998;97:1837–47.
National Cholesterol Education Program Expert Panel on Detection E, Treatment of High Blood Cholesterol in A. Third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III) final report. Circulation. 2002;106:3143–421.
Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive summary of the third report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection. Evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III). JAMA. 2001;285(19):2486–97.
Lenfant C. Shattuck lecture – clinical research to clinical practice – lost in translation? N Engl J Med. 2003;349:868–74.
Fletcher B, Berra K, Ades P, Braun LT, Burke LE, et al. Managing abnormal blood lipids: a collaborative approach. Circulation. 2005;112:3184–209.
Goldstein LB, Bushnell CD, Adams RJ, Appel LJ, Braun LT, et al. Guidelines for the primary prevention of stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2011;42:517–84.
Mosca L, Benjamin EJ, Berra K, Bezanson JL, Dolor RJ, et al. Effectiveness-based guidelines for the prevention of cardiovascular disease in women – 2011 update: a guideline from the American Heart Association. Circulation. 2011;123:1243–62.
Pletcher MJ, Moran AE. Cardiovascular risk assessment. Med Clin North Am. 2017;101:673–88.
Bastuji-Garin S, Deverly A, Moyse D, Castaigne A, Mancia G, et al. The Framingham prediction rule is not valid in a European population of treated hypertensive patients. J Hypertens. 2002;20:1973–80.
Brindle P, Emberson J, Lampe F, Walker M, Whincup P, et al. Predictive accuracy of the Framingham coronary risk score in British men: prospective cohort study. BMJ. 2003;327:1267.
Cook NR, Paynter NP, Eaton CB, Manson JE, Martin LW, et al. Comparison of the Framingham and Reynolds risk scores for global cardiovascular risk prediction in the multiethnic Women’s Health Initiative. Circulation. 2012;125:1748–56. S1741–1711.
D’Agostino RB Sr, Vasan RS, Pencina MJ, Wolf PA, Cobain M, et al. General cardiovascular risk profile for use in primary care: the Framingham heart study. Circulation. 2008;117:743–53.
Liu J, Hong Y, D’Agostino RB Sr, Wu Z, Wang W, et al. Predictive value for the Chinese population of the Framingham CHD risk assessment tool compared with the Chinese multi-provincial cohort study. JAMA. 2004;291:2591–9.
Ridker PM, Cook NR. Statins: new American guidelines for prevention of cardiovascular disease. Lancet. 2013;382:1762–5.
Khot UN, Khot MB, Bajzer CT, Sapp SK, Ohman EM, et al. Prevalence of conventional risk factors in patients with coronary heart disease. JAMA. 2003;290:898–904.
Greenland P, Knoll MD, Stamler J, Neaton JD, Dyer AR, et al. Major risk factors as antecedents of fatal and nonfatal coronary heart disease events. JAMA. 2003;290:891–7.
Ridker PM, Buring JE, Rifai N, Cook NR. Development and validation of improved algorithms for the assessment of global cardiovascular risk in women: the Reynolds risk score. JAMA. 2007;297:611–9.
Ridker PM, Paynter NP, Rifai N, Gaziano JM, Cook NR. C-reactive protein and parental history improve global cardiovascular risk prediction: the Reynolds Risk Score for men. Circulation. 2008;118:2243–51. 2244p following 2251.
Assmann G, Cullen P, Schulte H. Simple scoring scheme for calculating the risk of acute coronary events based on the 10-year follow-up of the prospective cardiovascular Munster (PROCAM) study. Circulation. 2002;105:310–5.
Conroy RM, Pyorala K, Fitzgerald AP, Sans S, Menotti A, et al. Estimation of ten-year risk of fatal cardiovascular disease in Europe: the SCORE project. Eur Heart J. 2003;24:987–1003.
Hippisley-Cox J, Coupland C, Vinogradova Y, Robson J, Minhas R, et al. Predicting cardiovascular risk in England and Wales: prospective derivation and validation of QRISK2. BMJ. 2008;336:1475–82.
The Atherosclerosis Risk in Communities (ARIC) Study: design and objectives. The ARIC investigators. Am J Epidemiol. 1989;129:687–702.
Fried LP, Borhani NO, Enright P, Furberg CD, Gardin JM, et al. The cardiovascular health study: design and rationale. Ann Epidemiol. 1991;1:263–76.
Friedman GD, Cutter GR, Donahue RP, Hughes GH, Hulley SB, et al. CARDIA: study design, recruitment, and some characteristics of the examined subjects. J Clin Epidemiol. 1988;41:1105–16.
Goff DC Jr, Lloyd-Jones DM, Bennett G, Coady S, D’Agostino RB, et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association task force on practice guidelines. Circulation. 2014;129:S49–73.
Kavousi M, Leening MJ, Nanchen D, Greenland P, Graham IM, et al. Comparison of application of the ACC/AHA guidelines, adult treatment panel III guidelines, and European Society of Cardiology guidelines for cardiovascular disease prevention in a European cohort. JAMA. 2014;311:1416–23.
Muntner P, Colantonio LD, Cushman M, Goff DC Jr, Howard G, et al. Validation of the atherosclerotic cardiovascular disease pooled cohort risk equations. JAMA. 2014;311:1406–15.
DeFilippis AP, Young R, Carrubba CJ, McEvoy JW, Budoff MJ, et al. An analysis of calibration and discrimination among multiple cardiovascular risk scores in a modern multiethnic cohort. Ann Intern Med. 2015;162:266–75.
Wang TJ, Gona P, Larson MG, Tofler GH, Levy D, et al. Multiple biomarkers for the prediction of first major cardiovascular events and death. N Engl J Med. 2006;355:2631–9.
Brindle P, Beswick A, Fahey T, Ebrahim S. Accuracy and impact of risk assessment in the primary prevention of cardiovascular disease: a systematic review. Heart. 2006;92:1752–9.
Stone NJ, Robinson JG, Lichtenstein AH, Bairey Merz CN, Blum CB, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association task force on practice guidelines. Circulation. 2014;129:S1–45.
Thanassoulis G, Vasan RS. Genetic cardiovascular risk prediction: will we get there? Circulation. 2010;122:2323–34.
Arain FA, Kuniyoshi FH, Abdalrhim AD, Miller VM. Sex/gender medicine. The biological basis for personalized care in cardiovascular medicine. Circ J. 2009;73:1774–82.
Regitz-Zagrosek V, Kararigas G. Mechanistic pathways of sex differences in cardiovascular disease. Physiol Rev. 2017;97:1–37.
Kling JM, Miller VM, Mulvagh SL. Transitions across a lifetime: unique cardiovascular physiology of women and relationship to cardiovascular disease risk. In: Spangenburg EE, editor. Integrative biology of Women’s health. New York: Springer; 2013. p. 141–56.
Sampson AK, Jennings GL, Chin-Dusting JP. Y are males so difficult to understand?: a case where “X” does not mark the spot. Hypertension. 2012;59:525–31.
Khera AV, Emdin CA, Drake I, Natarajan P, Bick AG, et al. Genetic risk, adherence to a healthy lifestyle, and coronary disease. N Engl J Med. 2016;375:2349–58.
Gertler MM, Garn SM, White PD. Young candidates for coronary heart disease. J Am Med Assoc. 1951;147:621–5.
Marenberg ME, Risch N, Berkman LF, Floderus B, de Faire U. Genetic susceptibility to death from coronary heart disease in a study of twins. N Engl J Med. 1994;330:1041–6.
Zdravkovic S, Wienke A, Pedersen NL, Marenberg ME, Yashin AI, et al. Heritability of death from coronary heart disease: a 36-year follow-up of 20 966 Swedish twins. J Intern Med. 2002;252:247–54.
Lloyd-Jones DM, Nam BH, D’Agostino RB Sr, Levy D, Murabito JM, et al. Parental cardiovascular disease as a risk factor for cardiovascular disease in middle-aged adults: a prospective study of parents and offspring. JAMA. 2004;291:2204–11.
Murabito JM, Pencina MJ, Nam BH, D’Agostino RB Sr, Wang TJ, et al. Sibling cardiovascular disease as a risk factor for cardiovascular disease in middle-aged adults. JAMA. 2005;294:3117–23.
Won HH, Natarajan P, Dobbyn A, Jordan DM, Roussos P, et al. Disproportionate contributions of select genomic compartments and cell types to genetic risk for coronary artery disease. PLoS Genet. 2015;11:e1005622.
Müller C. Xanthomata, hypercholesterolemia, angina pectoris. J Intern Med. 1938;89:75–84.
Lehrman MA, Schneider WJ, Sudhof TC, Brown MS, Goldstein JL, et al. Mutation in LDL receptor: Alu-Alu recombination deletes exons encoding transmembrane and cytoplasmic domains. Science. 1985;227:140–6.
Abifadel M, Varret M, Rabes JP, Allard D, Ouguerram K, et al. Mutations in PCSK9 cause autosomal dominant hypercholesterolemia. Nat Genet. 2003;34:154–6.
Soria LF, Ludwig EH, Clarke HR, Vega GL, Grundy SM, et al. Association between a specific apolipoprotein B mutation and familial defective apolipoprotein B-100. Proc Natl Acad Sci USA. 1989;86:587–91.
Garcia CK, Wilund K, Arca M, Zuliani G, Fellin R, et al. Autosomal recessive hypercholesterolemia caused by mutations in a putative LDL receptor adaptor protein. Science. 2001;292:1394–8.
Berge KE, Tian H, Graf GA, Yu L, Grishin NV, et al. Accumulation of dietary cholesterol in sitosterolemia caused by mutations in adjacent ABC transporters. Science. 2000;290:1771–5.
Musunuru K, Kathiresan S. Genetics of coronary artery disease. Annu Rev Genomics Hum Genet. 2010;11:91–108.
Risch NJ. Searching for genetic determinants in the new millennium. Nature. 2000;405:847–56.
Tabor HK, Risch NJ, Myers RM. Candidate-gene approaches for studying complex genetic traits: practical considerations. Nat Rev Genet. 2002;3:391–7.
Wacholder S, Chanock S, Garcia-Closas M, El Ghormli L, Rothman N. Assessing the probability that a positive report is false: an approach for molecular epidemiology studies. J Natl Cancer Inst. 2004;96:434–42.
McCarthy JJ, Parker A, Salem R, Moliterno DJ, Wang Q, et al. Large scale association analysis for identification of genes underlying premature coronary heart disease: cumulative perspective from analysis of 111 candidate genes. J Med Genet. 2004;41:334–41.
Ozaki K, Ohnishi Y, Iida A, Sekine A, Yamada R, et al. Functional SNPs in the lymphotoxin-alpha gene that are associated with susceptibility to myocardial infarction. Nat Genet. 2002;32:650–4.
Pare G, Serre D, Brisson D, Anand SS, Montpetit A, et al. Genetic analysis of 103 candidate genes for coronary artery disease and associated phenotypes in a founder population reveals a new association between endothelin-1 and high-density lipoprotein cholesterol. Am J Hum Genet. 2007;80:673–82.
Topol EJ, McCarthy J, Gabriel S, Moliterno DJ, Rogers WJ, et al. Single nucleotide polymorphisms in multiple novel thrombospondin genes may be associated with familial premature myocardial infarction. Circulation. 2001;104:2641–4.
Yamada Y, Matsuo H, Segawa T, Watanabe S, Kato K, et al. Assessment of genetic risk for myocardial infarction. Thromb Haemost. 2006;96:220–7.
Yamada Y, Metoki N, Yoshida H, Satoh K, Ichihara S, et al. Genetic risk for ischemic and hemorrhagic stroke. Arterioscler Thromb Vasc Biol. 2006;26:1920–5.
Yamada Y, Izawa H, Ichihara S, Takatsu F, Ishihara H, et al. Prediction of the risk of myocardial infarction from polymorphisms in candidate genes. N Engl J Med. 2002;347:1916–23.
Silander K, Alanne M, Kristiansson K, Saarela O, Ripatti S, et al. Gender differences in genetic risk profiles for cardiovascular disease. PLoS One. 2008;3:e3615.
International HapMap C. The international HapMap Project. Nature. 2003;426:789–96.
International HapMap C, Frazer KA, Ballinger DG, Cox DR, Hinds DA, et al. A second generation human haplotype map of over 3.1 million SNPs. Nature. 2007;449:851–61.
Samani NJ, Erdmann J, Hall AS, Hengstenberg C, Mangino M, et al. Genomewide association analysis of coronary artery disease. N Engl J Med. 2007;357:443–53.
Helgadottir A, Thorleifsson G, Manolescu A, Gretarsdottir S, Blondal T, et al. A common variant on chromosome 9p21 affects the risk of myocardial infarction. Science. 2007;316:1491–3.
McPherson R, Pertsemlidis A, Kavaslar N, Stewart A, Roberts R, et al. A common allele on chromosome 9 associated with coronary heart disease. Science. 2007;316:1488–91.
Myocardial Infarction Genetics C, Kathiresan S, Voight BF, Purcell S, Musunuru K, et al. Genome-wide association of early-onset myocardial infarction with single nucleotide polymorphisms and copy number variants. Nat Genet. 2009;41:334–41.
Erdmann J, Grosshennig A, Braund PS, Konig IR, Hengstenberg C, et al. New susceptibility locus for coronary artery disease on chromosome 3q22.3. Nat Genet. 2009;41:280–2.
Coronary Artery Disease Genetics C. A genome-wide association study in Europeans and south Asians identifies five new loci for coronary artery disease. Nat Genet. 2011;43:339–44.
Consortium IKC. Large-scale gene-centric analysis identifies novel variants for coronary artery disease. PLoS Genet. 2011;7:e1002260.
Consortium CD, Deloukas P, Kanoni S, Willenborg C, Farrall M, et al. Large-scale association analysis identifies new risk loci for coronary artery disease. Nat Genet. 2013;45:25–33.
Nikpay M, Goel A, Won HH, Hall LM, Willenborg C, et al. A comprehensive 1,000 genomes-based genome-wide association meta-analysis of coronary artery disease. Nat Genet. 2015;47:1121–30.
Webb TR, Erdmann J, Stirrups KE, Stitziel NO, Masca NG, et al. Systematic evaluation of pleiotropy identifies 6 further loci associated with coronary artery disease. J Am Coll Cardiol. 2017;69:823–36.
Do R, Stitziel NO, Won HH, Jorgensen AB, Duga S, et al. Exome sequencing identifies rare LDLR and APOA5 alleles conferring risk for myocardial infarction. Nature. 2015;518:102–6.
Maurano MT, Humbert R, Rynes E, Thurman RE, Haugen E, et al. Systematic localization of common disease-associated variation in regulatory DNA. Science. 2012;337:1190–5.
Schunkert H, Konig IR, Kathiresan S, Reilly MP, Assimes TL, et al. Large-scale association analysis identifies 13 new susceptibility loci for coronary artery disease. Nat Genet. 2011;43:333–8.
Liu LY, Schaub MA, Sirota M, Butte AJ. Sex differences in disease risk from reported genome-wide association study findings. Hum Genet. 2012;131:353–64.
Morris AP, Voight BF, Teslovich TM, Ferreira T, Segre AV, et al. Large-scale association analysis provides insights into the genetic architecture and pathophysiology of type 2 diabetes. Nat Genet. 2012;44:981–90.
Taylor KC, Carty CL, Dumitrescu L, Buzkova P, Cole SA, et al. Investigation of gene-by-sex interactions for lipid traits in diverse populations from the population architecture using genomics and epidemiology study. BMC Genet. 2013;14:33.
Kavousi M, Bielak LF, Peyser PA. Genetic research and Women’s heart disease: a primer. Curr Atheroscler Rep. 2016;18:67.
Orozco G, Ioannidis JP, Morris A, Zeggini E, Consortium D. Sex-specific differences in effect size estimates at established complex trait loci. Int J Epidemiol. 2012;41:1376–82.
Goodarzynejad H, Boroumand M, Behmanesh M, Ziaee S, Jalali A. The rs5888 single nucleotide polymorphism in scavenger receptor class B type 1 (SCARB1) gene and the risk of premature coronary artery disease: a case-control study. Lipids Health Dis. 2016;15:7.
Hartiala JA, Tang WH, Wang Z, Crow AL, Stewart AF, et al. Genome-wide association study and targeted metabolomics identifies sex-specific association of CPS1 with coronary artery disease. Nat Commun. 2016;7:10558.
Shungin D, Winkler TW, Croteau-Chonka DC, Ferreira T, Locke AE, et al. New genetic loci link adipose and insulin biology to body fat distribution. Nature. 2015;518:187–96.
Wise AL, Gyi L, Manolio TA. eXclusion: toward integrating the X chromosome in genome-wide association analyses. Am J Hum Genet. 2013;92:643–7.
Gao F, Chang D, Biddanda A, Ma L, Guo Y, et al. XWAS: a software toolset for genetic data analysis and association studies of the X chromosome. J Hered. 2015;106:666–71.
Charchar FJ, Tomaszewski M, Padmanabhan S, Lacka B, Upton MN, et al. The Y chromosome effect on blood pressure in two European populations. Hypertension. 2002;39:353–6.
Ellis JA, Stebbing M, Harrap SB. Association of the human Y chromosome with high blood pressure in the general population. Hypertension. 2000;36:731–3.
Uehara Y, Shin WS, Watanabe T, Osanai T, Miyazaki M, et al. A hypertensive father, but not hypertensive mother, determines blood pressure in normotensive male offspring through body mass index. J Hum Hypertens. 1998;12:441–5.
Bray AW, Ballinger SW. Mitochondrial DNA mutations and cardiovascular disease. Curr Opin Cardiol. 2017. https://doi.org/10.1097/HCO.0000000000000383.
Assimes TL, Roberts R. Genetics: implications for prevention and Management of Coronary Artery Disease. J Am Coll Cardiol. 2016;68:2797–818.
Manolio TA. Genomewide association studies and assessment of the risk of disease. N Engl J Med. 2010;363:166–76.
Chatterjee N, Shi J, Garcia-Closas M. Developing and evaluating polygenic risk prediction models for stratified disease prevention. Nat Rev Genet. 2016;17:392–406.
Tada H, Melander O, Louie JZ, Catanese JJ, Rowland CM, et al. Risk prediction by genetic risk scores for coronary heart disease is independent of self-reported family history. Eur Heart J. 2016;37:561–7.
Kathiresan S, Melander O, Anevski D, Guiducci C, Burtt NP, et al. Polymorphisms associated with cholesterol and risk of cardiovascular events. N Engl J Med. 2008;358:1240–9.
Anderson JL, Horne BD, Camp NJ, Muhlestein JB, Hopkins PN, et al. Joint effects of common genetic variants from multiple genes and pathways on the risk of premature coronary artery disease. Am Heart J. 2010;160:250–6. e253.
Qi L, Ma J, Qi Q, Hartiala J, Allayee H, et al. Genetic risk score and risk of myocardial infarction in Hispanics. Circulation. 2011;123:374–80.
Ripatti S, Tikkanen E, Orho-Melander M, Havulinna AS, Silander K, et al. A multilocus genetic risk score for coronary heart disease: case-control and prospective cohort analyses. Lancet. 2010;376:1393–400.
Thanassoulis G, Peloso GM, Pencina MJ, Hoffmann U, Fox CS, et al. A genetic risk score is associated with incident cardiovascular disease and coronary artery calcium: the Framingham heart study. Circ Cardiovasc Genet. 2012;5:113–21.
Paynter NP, Chasman DI, Pare G, Buring JE, Cook NR, et al. Association between a literature-based genetic risk score and cardiovascular events in women. JAMA. 2010;303:631–7.
Tikkanen E, Havulinna AS, Palotie A, Salomaa V, Ripatti S. Genetic risk prediction and a 2-stage risk screening strategy for coronary heart disease. Arterioscler Thromb Vasc Biol. 2013;33:2261–6.
Ganna A, Magnusson PK, Pedersen NL, de Faire U, Reilly M, et al. Multilocus genetic risk scores for coronary heart disease prediction. Arterioscler Thromb Vasc Biol. 2013;33:2267–72.
Hughes MF, Saarela O, Stritzke J, Kee F, Silander K, et al. Genetic markers enhance coronary risk prediction in men: the MORGAM prospective cohorts. PLoS One. 2012;7:e40922.
Weijmans M, de Bakker PI, van der Graaf Y, Asselbergs FW, Algra A, et al. Incremental value of a genetic risk score for the prediction of new vascular events in patients with clinically manifest vascular disease. Atherosclerosis. 2015;239:451–8.
Mega JL, Stitziel NO, Smith JG, Chasman DI, Caulfield MJ, et al. Genetic risk, coronary heart disease events, and the clinical benefit of statin therapy: an analysis of primary and secondary prevention trials. Lancet. 2015;385:2264–71.
Abraham G, Havulinna AS, Bhalala OG, Byars SG, De Livera AM, et al. Genomic prediction of coronary heart disease. Eur Heart J. 2016;37:3267–78.
Shahid SU, Shabana, Cooper JA, Beaney KE, Li K, et al. Genetic risk analysis of coronary artery disease in Pakistani subjects using a genetic risk score of 21 variants. Atherosclerosis. 2017;258:1–7.
Joseph PG, Pare G, Asma S, Engert JC, Yusuf S, et al. Impact of a genetic risk score on myocardial infarction risk across different ethnic populations. Can J Cardiol. 2016;32:1440–6.
Shanker J, Arvind P, Jambunathan S, Nair J, Kakkar V. Genetic analysis of the 9p21.3 CAD risk locus in Asian Indians. Thromb Haemost. 2014;111:960–9.
Sotos-Prieto M, Baylin A, Campos H, Qi L, Mattei J. Lifestyle cardiovascular risk score, genetic risk score, and myocardial infarction in Hispanic/Latino adults living in Costa Rica. J Am Heart Assoc. 2016;5(12):e004067.
Pasquale LR, Aschard H, Kang JH, Bailey JN, Lindstrom S, et al. Age at natural menopause genetic risk score in relation to age at natural menopause and primary open-angle glaucoma in a US-based sample. Menopause. 2017;24:150–6.
Lee H, Oh JY, Sung YA, Chung HW. A genetic risk score is associated with polycystic ovary syndrome-related traits. Hum Reprod. 2016;31:209–15.
Xia Z, Steele SU, Bakshi A, Clarkson SR, White CC, et al. Assessment of early evidence of multiple sclerosis in a prospective study of asymptomatic high-risk family members. JAMA Neurol. 2017;74:293–300.
Vachon CM, Pankratz VS, Scott CG, Haeberle L, Ziv E, et al. The contributions of breast density and common genetic variation to breast cancer risk. J Natl Cancer Inst. 2015;107:dju397.
Helfand BT, Kearns J, Conran C, Xu J. Clinical validity and utility of genetic risk scores in prostate cancer. Asian J Androl. 2016;18:509–14.
Carayol J, Schellenberg GD, Dombroski B, Genin E, Rousseau F, et al. Autism risk assessment in siblings of affected children using sex-specific genetic scores. Mol Autism. 2011;2:17.
Thornton-Wells TA, Moore JH, Haines JL. Dissecting trait heterogeneity: a comparison of three clustering methods applied to genotypic data. BMC Bioinformatics. 2006;7:204.
Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, et al. Heart disease and stroke statistics – 2013 update: a report from the American Heart Association. Circulation. 2013;127:e6–e245.
Leening MJ, Ferket BS, Steyerberg EW, Kavousi M, Deckers JW, et al. Sex differences in lifetime risk and first manifestation of cardiovascular disease: prospective population based cohort study. BMJ. 2014;349:g5992.
Mosca L, Barrett-Connor E, Wenger NK. Sex/gender differences in cardiovascular disease prevention: what a difference a decade makes. Circulation. 2011;124:2145–54.
Bairey Merz CN, Shaw LJ, Reis SE, Bittner V, Kelsey SF, et al. Insights from the NHLBI-sponsored Women's ischemia syndrome evaluation (WISE) study: part II: gender differences in presentation, diagnosis, and outcome with regard to gender-based pathophysiology of atherosclerosis and macrovascular and microvascular coronary disease. J Am Coll Cardiol. 2006;47:S21–9.
Regitz-Zagrosek V, Lehmkuhl E. Heart failure and its treatment in women. Role of hypertension, diabetes, and estrogen. Herz. 2005;30:356–67.
Salfati E, Nandkeolyar S, Fortmann SP, Sidney S, Hlatky MA, et al. Susceptibility loci for clinical coronary artery disease and subclinical coronary atherosclerosis throughout the life-course. Circ Cardiovasc Genet. 2015;8:803–11.
Assimes TL, Salfati EL, Del Gobbo LC. Leveraging information from genetic risk scores of coronary atherosclerosis. Curr Opin Lipidol. 2017;28:104–12.
Barrett-Connor E. Sex differences in coronary heart disease. Why are women so superior? The 1995 Ancel keys lecture. Circulation. 1997;95:252–64.
Jousilahti P, Vartiainen E, Tuomilehto J, Puska P. Sex, age, cardiovascular risk factors, and coronary heart disease: a prospective follow-up study of 14 786 middle-aged men and women in Finland. Circulation. 1999;99:1165–72.
Pilote L, Dasgupta K, Guru V, Humphries KH, McGrath J, et al. A comprehensive view of sex-specific issues related to cardiovascular disease. CMAJ. 2007;176:S1–44.
Tunstall-Pedoe H, Kuulasmaa K, Amouyel P, Arveiler D, Rajakangas AM, et al. Myocardial infarction and coronary deaths in the World Health Organization MONICA project. Registration procedures, event rates, and case-fatality rates in 38 populations from 21 countries in four continents. Circulation. 1994;90:583–612.
Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364:937–52.
Carroll MD, Lacher DA, Sorlie PD, Cleeman JI, Gordon DJ, et al. Trends in serum lipids and lipoproteins of adults, 1960-2002. JAMA. 2005;294:1773–81.
Mittendorfer B. Sexual dimorphism in human lipid metabolism. J Nutr. 2005;135:681–6.
Roger VL, Go AS, Lloyd-Jones DM, Benjamin EJ, Berry JD, et al. Heart disease and stroke statistics – 2012 update: a report from the American Heart Association. Circulation. 2012;125:e2–e220.
Townsend EA, Miller VM, Prakash YS. Sex differences and sex steroids in lung health and disease. Endocr Rev. 2012;33:1–47.
Nauser TD, Stites SW. Diagnosis and treatment of pulmonary hypertension. Am Fam Physician. 2001;63:1789–98.
Lykke JA, Langhoff-Roos J, Sibai BM, Funai EF, Triche EW, et al. Hypertensive pregnancy disorders and subsequent cardiovascular morbidity and type 2 diabetes mellitus in the mother. Hypertension. 2009;53:944–51.
Wu P, Haththotuwa R, Kwok CS, Babu A, Kotronias RA, et al. Preeclampsia and future cardiovascular health: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes. 2017;10
Garovic VD, Bailey KR, Boerwinkle E, Hunt SC, Weder AB, et al. Hypertension in pregnancy as a risk factor for cardiovascular disease later in life. J Hypertens. 2010;28:826–33.
Funai EF, Friedlander Y, Paltiel O, Tiram E, Xue X, et al. Long-term mortality after preeclampsia. Epidemiology. 2005;16:206–15.
Brown DW, Dueker N, Jamieson DJ, Cole JW, Wozniak MA, et al. Preeclampsia and the risk of ischemic stroke among young women: results from the stroke prevention in young women study. Stroke. 2006;37:1055–9.
Vikse BE, Irgens LM, Leivestad T, Skjaerven R, Iversen BM. Preeclampsia and the risk of end-stage renal disease. N Engl J Med. 2008;359:800–9.
Kuklina EV, Ayala C, Callaghan WM. Hypertensive disorders and severe obstetric morbidity in the United States. Obstet Gynecol. 2009;113:1299–306.
Ostadal B, Ostadal P. Sex-based differences in cardiac ischaemic injury and protection: therapeutic implications. Br J Pharmacol. 2014;171:541–54.
Nwankwo TYS, Burt V, Gu Q. Hypertension among adults in the United States: National Health and nutrition examination survey, 2011–2012. NCHS Data Brief. 2013;133:1–8.
Legro RS. Polycystic ovary syndrome and cardiovascular disease: a premature association? Endocr Rev. 2003;24:302–12.
Vryonidou A, Papatheodorou A, Tavridou A, Terzi T, Loi V, et al. Association of hyperandrogenemic and metabolic phenotype with carotid intima-media thickness in young women with polycystic ovary syndrome. J Clin Endocrinol Metab. 2005;90:2740–6.
Puzianowska-Kuznicka M. ESR1 in myocardial infarction. Clin Chim Acta. 2012;413:81–7.
Sudhir K, Chou TM, Chatterjee K, Smith EP, Williams TC, et al. Premature coronary artery disease associated with a disruptive mutation in the estrogen receptor gene in a man. Circulation. 1997;96:3774–7.
Shaw LJ, Bugiardini R, Merz CN. Women and ischemic heart disease: evolving knowledge. J Am Coll Cardiol. 2009;54:1561–75.
Acknowledgments
The Framingham Heart Study (FHS) dataset was obtained from dbGaP (phs000007), approved by the University of Melbourne Health Sciences Human Ethics Sub-Committee (HREC 1442186). The FHS is conducted and supported by the National Heart, Lung, and Blood Institute (NHLBI) in collaboration with Boston University (Contract No. N01-HC-25195 and HHSN268201500001I). This chapter was not prepared in collaboration with investigators of the Framingham Heart Study and does not necessarily reflect the opinions or views of the Framingham Heart Study, Boston University, or NHLBI. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the chapter.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Byars, S.G., Inouye, M. (2018). Genome-Wide Association Studies and Risk Scores for Coronary Artery Disease: Sex Biases. In: Kerkhof, P., Miller, V. (eds) Sex-Specific Analysis of Cardiovascular Function. Advances in Experimental Medicine and Biology, vol 1065. Springer, Cham. https://doi.org/10.1007/978-3-319-77932-4_38
Download citation
DOI: https://doi.org/10.1007/978-3-319-77932-4_38
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-77931-7
Online ISBN: 978-3-319-77932-4
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)