Abstract
Antimicrobial peptides (AMPs) are small proteins synthesized predominantly by leukocytes. Although discovered about a century ago, interest in AMPs has only recently burgeoned, largely fueled by the need for alternative therapeutics against drug-resistant infections. AMPs are widely distributed; they are found intracellularly, in body fluids and at mucosal surfaces. Although their primary physiological function is considered protection against infections, it is increasingly evident that the role of AMPs may also extend to wound healing and immunomodulation. Several studies have associated dysregulation of AMPs with predisposition to infectious diseases and immune disorders, although causality remains to be established. Naturally occurring and synthetic AMPs have been developed for treatment of infections. However, as with antibiotics, pathogens acquire resistance to AMPs, which have posed an obstacle to their clinical development. The current review provides a brief overview of this complex and evolving field.
This work was supported by grants from the National Institutes of Health/National Institutes of Allergy and Infectious Diseases, AI111728, AI118161, AI119327, and AI114790.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
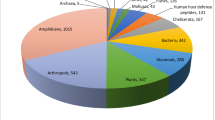
In 1922, Alexander Fleming isolated lysozyme, the first identified antimicrobial peptide from nasal mucus. Subsequently, several antimicrobial proteins and peptides have been identified in organisms from each of the six kingdoms of life. Interest in antimicrobial proteins and peptides surged in the 1960s when antibiotic-resistant bacteria began to emerge. These antimicrobial molecules vary greatly in size and structure. In some instances, antimicrobial functions have been discovered for molecules that have traditionally been associated with other physiological functions – examples include laminin and histones. A comprehensive catalog of over 2600 naturally occurring antimicrobial molecules, including 112 human host defense peptides, can be found on the antimicrobial peptide database (http://aps.unmc.edu/AP/main.php; [1]).
This review focuses mainly on antimicrobial peptides (AMPs), which are small (in most instances, fewer than 50 amino acids) soluble peptides with effector functions similar to the complement proteins. Like complement proteins, most AMPs are activated posttranslationally from precursor peptides on specific surfaces (most commonly of microbial origin), and neutralize their targets. Similar to membrane attack complex, the terminal pore-forming step of the complement cascade, some AMPs form barrel-stave pores on their target membranes. Other functions shared by complement and antimicrobial peptides include phagocyte chemotaxis, induction of chemokines and cytokines, and regulation of inflammation [2].
In addition to protecting the host against a broad spectrum of microbial pathogens , AMPs maintain the normal microbiome, modulate innate and adaptive immune responses, and may participate in tissue remodeling. Most AMPs are amphipathic or cationic, although anionic peptides have also been described. AMPs are usually synthesized as precursor peptides, which include a signal sequence, and subsequently undergo post-translational modifications such as proteolytic cleavage, glycosylation, C-terminal amidation, amino acid isomerization, or cyclization [3,4,5,6].
It is believed that AMPs have evolved separately on multiple occasions. Thus, it has been difficult to study their evolution even within the same gene families. For example, in humans a cluster of three β-defensin genes can exist in copy numbers of 2–12 per haploid genome because of duplication events [7]. It is believed that gene duplication followed by adaptive evolution could yield peptides with enhanced antimicrobial properties, or in some instances novel functions, while still retaining the function of the original peptide [5].
Synthesis of Human AMPs
Most canonical AMPs are synthesized by leukocytes, which transport them to sites of infection, or by epithelial cells and then released into the interstitial milieu [3]. For instance, cathelicidin, the precursor form of LL-37, is expressed in the epithelial cells of the eye, skin, and gastrointestinal, genitourinary, and respiratory tracts and also by neutrophils, natural killer, and mast cells [8]. Histatin (Hst) 1 is synthesized by the ocular epithelium, while Hst5 is produced by epithelial surfaces in the oral cavity. Human α-defensins like human neutrophil peptides (HNPs) 1, 3, 4 and human defensin (HD) 6 were originally described in neutrophils but are also found in Paneth cells, tracheal epithelium, oral mucosa, and salivary glands. HD5 is found at female reproductive mucosal surfaces and airway and digestive epithelium and in neutrophils. Human β-defensins (HBDs) 1, 2, 3, and 4 are secreted at gastrointestinal surfaces (small intestine, colon), pancreas, parotid glands, mammary glands, thymus, both male and female reproductive tracts (prostate, vagina, cervix, uterus, oviduct, and placenta), tracheobronchial epithelium, keratinocytes, skin, as well as by leukocytes such as macrophages and neutrophils [3]. Bactericidal/permeability-increasing protein (BPI), which bears structural homology with lipopolysaccharide (LPS)-binding protein (LBP) , is expressed in neutrophils and eosinophils and by some epithelial cells. Certain proteins with physiological “noninfective” functions, which upon processing may assume AMP-like properties, are more widely distributed. For example, the matrix protein laminin is widely distributed in the musculoskeletal, vascular, nervous, endocrine, respiratory, and reproductive systems [9]. Histone H2A is synthesized in excess of what is required for DNA packaging at the gastric mucosa and is stored in the secretory vesicles of cells at the site [3].
Functions of AMPs
Although AMPs have traditionally been construed as antimicrobial defense effectors, it is now evident that they participate in diverse processes, such as wound healing, distinguishing self from nonself, and maintenance of a healthy and normal microbiome. HBDs and the cathelicidin LL-37 facilitate tissue remodeling and wound healing through EGFR-mediated chemotaxis of epithelial cells and production of metalloproteinases [10]. TGF-β and insulin-like growth factor 1 (IGF-1) in wounds lead to LL-37 production, which stimulates angiogenesis and granulation tissue formation by activating fibroblasts. HNP1 upregulates procollagen mRNA transcripts and protein from fibroblasts, while HBD-1, 2, and 3 cause keratinocyte proliferation [11]. LL-37 also regulates genes responsible for autophagy, apoptosis, and pyroptosis in neutrophils and macrophages, thereby controlling inflammation [10].
Dysregulation of AMP homeostasis has been associated with autoimmune disorders. AMPs may also contribute to inflammation and the pathogenesis of autoimmune diseases [12]. For example, LL-37 can bind to self-DNA and self-RNA, facilitating their recognition by Toll-like receptors (TLR) 9 and 7 or 8, respectively. Enhanced stimulation of TLR9 on plasmacytoid dendritic cells leading to upregulation of IFN-α (type I IFN) may lead to autoimmune T-cell activation and exacerbation of the skin lesions of psoriasis [13]. LL-37 may also modulate activation of TLR4 by LPS [14, 15]. Downregulation of LL-37 and HBDs 2 and 3 that is observed in atopic dermatitis can predispose such individuals to infections with Staphylococcus aureus [6]. Enhanced proteolysis of cathelicidin to LL-37 by cutaneous serine proteases is thought to contribute to the pathology of rosacea [16]; direct inhibition of serine proteases by topical azelaic acid reduced cathelicidin levels and alleviated symptoms [8]. Dysregulation of AMPs has also been associated with inflammatory bowel disease. Significantly diminished mRNA levels of α-defensins (HDs 5 and 6) were seen in Paneth cells of patients with ileal Crohn’s disease [17]. On the other hand, these patients had elevated levels of β-defensins (HBDs 2 and 3) in their serum and terminal ileum, respectively [12].Therefore, while AMP-mediated innate immune signaling cascades can on the one hand control infection and inflammation, on the other hand they can also precipitate immune dysregulation [6].
Thus, given their diverse mechanisms of action, and increasing repertoire of functions, AMPs are now being evaluated for potential therapeutic applications not only in control of infections but also in wound healing and immune regulation and for treatment of cancer.
Classification of AMPs
AMPs are diverse in structure, function, and origin, and thus there is no clear consensus on their classification scheme. They may be classified based on their biological source (e.g., bacterial, plant, animal), function (e.g., antibacterial, antiviral, insecticidal, chemotactic), peptide properties (charge or hydrophobicity), molecular targets (cell surface targeting properties or intracellular targeting peptides), and covalent bonding pattern (also called the universal classification (UC) scheme, proposed by Wang) [18]. Some authors have proposed the classification of AMPs based on their structure (Fig. 5.1), which is discussed below.
Classification of antimicrobial peptides based on their structure. Structures of representative molecules are shown: α-helical peptides, LL-37 (https://doi.org/10.2210/pdb2k6o/pdb); β-sheet peptides, human neutrophil peptide (HNP) 1 (https://doi.org/10.2210/pdb3hjd/pdb), human beta-defensin (HBD) 1 (https://doi.org/10.2210/pdb1iju/pdb), and rhesus theta defensin-1 (https://doi.org/10.2210/pdb2lyf/pdb); extended structure AMPs, indolicidin (https://doi.org/10.2210/pdb1g8c/pdb)
α-Helical AMPs
Linear α-helical peptides are the most widely studied class of AMPs. Notable examples of this class of AMPs include the cathelicidin LL-37 and magainin-2 (pexiganan). Cathelicidins share a highly conserved N-terminal “cathelin” domain, but highly variable antimicrobial sequences, ranging from proline- and arginine-rich peptides to helical peptides to disulfide-linked peptides [19]. LL-37 is released following cleavage of the cathelin domain from the only known human cathelicidin, hCAP-18 (human cationic peptide of 18 kDa). The term cathelicidin was originally used to refer to the entire precursor protein but now is often used interchangeably to refer to the antimicrobial peptide. α-Helical AMPs are amphipathic and often 30–40 amino acids in length, and some are rich in lysine and arginine residues. A few peptides in this class have a kink or a bend at the center, which is essential for their ability to disrupt membranes. While some of these peptides might be disordered in solution, all of them undergo an α-helical conformation when inserted into biological membranes [20, 21].
β-Sheet AMPs
A second class of AMPs comprise β-sheets. Gramicidins, hepcidins, and α- and β-defensins belong to this class of peptides. Some of these AMPs have two or more antiparallel β-sheets stabilized by disulfide bridges, while others such as the human hepcidins contain β-sheets with smaller intervening α-helices [4, 6, 20, 22].
All defensins are cationic and have six conserved cysteine residues linked by three intramolecular disulfide bridges; coupling of the Cys residues defines the three subfamilies, α, β, and θ (Fig. 5.1) [23, 24]. θ-Defensins are macrocyclic peptides with 18 amino acid residues formed by head-to-tail splicing of two separate 9-mer precursors linked by three intramolecular disulfide bridges. These are not found in humans because of a premature stop codon in sequence of one of the precursors. They are however abundant in rhesus macaques and one of them called retrocyclin-1 inhibits cellular entry of HIV-1, HSV, and influenza A virus and protects against Bacillus anthracis spores. Their unique characteristics make them attractive therapeutic candidates [24].
Extended AMPs
These peptides contain an abundance of amino acids such as proline, glycine, histidine, arginine, and tryptophan, which prevent formation of specific structural motifs. Unlike other AMPs, the structures they assume do not result from inter-residue hydrogen bonds but occur through hydrogen bonds and van der Waals interactions with membrane lipids. Human histatins are representative of this class of AMPs [4, 6].
Mechanisms of Action
While some AMPs exert direct bactericidal effects, others may kill microorganisms and cause damage to eukaryotic cells through modulation of the immune system. In this light, it is reasonable to conclude that their functions cannot be generalized, but are contextual and specific to the infection or the inflammatory process in question. AMPs may target extracellular membranes or intracellular processes to mediate microbial or cellular damage. Table 5.1 summarizes their mechanisms of action.
Extracellular Targets of AMPs
Membrane Damage by Pore Formation
The initial interaction between the negatively charged microbial membrane and AMPs is driven by electrostatic forces. Thus membrane-active AMPs are often cationic or complexed to a metal cation, such as zinc. Subsequent to initial membrane targeting, α-helical peptides, which are relatively disordered in solution, undergo a phase transition. Upon interaction with phospholipid bilayers and LPS or lipid A, they quickly assume an amphipathic α-helical structure. β-Sheets which are more structured in solution may undergo multimer disassembly and form quaternary structures. Once the concentration of AMPs on the membrane reaches a critical threshold, the peptides undergo an amphipathicity-dependent second structural reorganization that leads to formation of pores in membranes. Their hydrophobicity enables these peptides to partition into the membrane lipid bilayer. Additionally, membrane damage is often brought about either by cationic AMPs or anionic AMPs complexed with a metal cation like zinc, which enables them to target anionic microbial membranes. Upon formation of pores, critical cellular functions such as maintenance of electrochemical gradients, selective permeability, respiration, and scaffolding of essential microbial proteins are perturbed, leading to rapid cell death [21, 25]. Multiple models of pore formation have been proposed (Fig. 5.2) and are discussed below.
Mechanisms of membrane damage by AMPs. AMPs are attracted to biological membranes by electrostatic interactions. When a critical peptide to lipid ratio is reached, peptides are inserted and oriented along membranes to form pores. Barrel-stave model: peptides are inserted into membrane parallel to each other to form a pore lined only with peptides. Toroidal model: peptides create a strain on the membrane causing it to thin progressively until the strain creates a water pore lined by both peptide as well as lipid head groups. Carpet model: AMPs cover the membrane in a carpet like fashion, causing strain. The membrane bends over and peptides line the cytoplasmic leaflet as well. Micelles are formed from intervening lipid bilayers. Ion channel: formed by AMPs which have no distinct structure in solution, but when they come in contact with bacterial membrane they form an α-helical structure and multiple peptides are stabilized by cations such Zn2+ to form ion channels that cause membrane depolarization
-
A.
Barrel-Stave Model
Alamethicin and gramicidin S are examples of AMPs that form barrel-stave pores in microbial membranes [26]. Upon reaching a critical lipid/peptide ratio, the AMPs oligomerize and insert perpendicularly into the microbial membrane, forming a transmembrane pore (internal and external diameters of 1.8 nm and 4 nm, respectively), akin to the staves that form a barrel. The hydrophobic regions of the peptide associate with lipid head groups, while the hydrophilic regions form the lumen. About 3–11 peptides are usually required to form barrel-stave pores [4, 21].
-
B.
Toroidal/Disordered Toroidal Pore Model
Peptides such as magainin and protegrin form toroidal pores. Toroidal pores are distinctive from barrel-stave pores in that the lumen of the pore facing the water core is lined by polar lipid head groups even when peptides are perpendicularly inserted into the membrane. Peptides bind to the membrane, causing strain such that it leads to progressive membrane thinning until the lamellar normal finally gives way and peptides get inserted perpendicularly and on the inner aspect of the membrane, such that a continuous peptide lined hole is formed. Such pores are usually larger than barrel-stave pores, with an internal diameter of 3–5 nm and an external diameter of 7–8.4 nm. These pores comprise 4–7 peptide monomers and about 90 lipid head groups. In this model, while most of the peptides line the external opening and a few line the internal leaflet, all are parallel to the membrane normal. Only a single peptide tilting inward is usually observed in the water core [21, 27, 28].
-
C.
Carpet Model
At very high concentrations, cationic peptides lie in-plane with the anionic microbial membranes covering it like a carpet and finally forming micelles in a detergent-like fashion. This leads to increases in membrane permeability without actually forming pores and is considered an extreme form of the toroidal pore. Cercopin derivatives, such as HB-50, HP-107, and LL-37, are thought to function via this model [4, 21, 25, 27].
-
D.
Formation of Ion Channels and Membrane Depolarization
The anionic antimicrobial peptide found in human sweat, dermacidin, is a broad-spectrum antimicrobial that is active against gram-positives such as Staphylococcus aureus, S. epidermidis, Enterococcus faecalis, and Listeria monocytogenes; gram-negatives such as Pseudomonas putida, Salmonella typhimurium, and Escherichia coli; and fungi such as Candida albicans. The protein is a random coil stabilized by the low pH and Zn2+ ions. However, when in proximity to an anionic microbial membrane, the cationic N-terminus of the protein interacts electrostatically with the membrane, assumes an α-helical secondary structure, and oligomerizes and inserts into the membrane via its C-terminus, forming an ion channel stabilized by the Zn2+ ions at its N-terminus. Loss of ions through this channel ultimately leads to disruption of membrane potential and cell death [29].
Inhibition of Peptidoglycan Cell Wall Synthesis
HBD-3 secreted by epithelial cells and neutrophils inhibits penicillin-binding protein 2-mediated transglycosylation of the monomeric lipid II pentapeptide molecules into the polymeric murein sacculus of S. aureus [30]. Human neutrophil defensin (HNP) 1 also interacts with lipid II of S. aureus to inhibit peptidoglycan synthesis [31].
Disruption of Membrane Integrity
Human ribonuclease 7 (hRNAse 7) is a 128 amino acid cationic protein which is abundant in epithelial tissues, skin, and respiratory and urogenital tracts. It is active against gram-positive as well as gram-negative bacteria such as Proteus mirabilis, P. aeruginosa, E. coli, Klebsiella pneumoniae, S. saprophyticus, and E. faecalis. Bacteria exposed to this CAMP showed extensive membrane splitting and blebbing ultimately leading to cell death [32]. Although the exact mechanism of action of this AMP has not been elucidated, evidence suggests that this AMP probably interacts with proteins tethering the bacterial cell membrane to underlying structures, thereby causing membrane release. For example, it disrupts the outer membrane protein (Opr) I (a homolog of Braun’s lipoprotein found in other gram-negatives such as E. coli and Klebsiella spp.) in Pseudomonas which tethers the outer membrane to the murein sacculus [33].
Neutralization of Extracellular Virulence Factors
Recent work demonstrated that cationic histone proteins H2A and H2B are expressed in cytosolic compartments, at cell surfaces, as well as in the extracellular milieu in the human placenta. In fact, the bactericidal effects of the amniotic fluid stems from the ability of H2A and H2B to bind strongly to the anionic lipid A and core oligosaccharides of gram-negative pathogens. Although not directly microbicidal, binding of these histone proteins to lipid A prevents lipid A signaling through TLR4, thereby limiting production of IL-1, IL-6, and TNF-α, all of which contribute to septic shock [34].
Human α- and β-defensins protect against herpes simplex virus (HSV) infections by inhibiting the virus from attaching to its cell receptor and entering cells. Several HNPs and HDs bind to various viral glycoproteins as well as to heparan sulfate (the cell surface receptor for HSV), thereby preventing viral penetration into host cells [35].
Intracellular Targets of AMPs
Disruption of Protein Synthesis and Function
Hst-5 is a strongly basic α-helical peptide which has been demonstrated to be effective against fungi such as Candida as well as parasites such as Leishmania. This AMP disrupts mitochondrial membrane integrity, resulting in malformation of cristae and dissipation of membrane potential, thereby abrogating ATP synthesis and cellular energetics [36, 37]. While this AMP undergoes receptor-mediated endocytosis to gain entry into Candida, the mechanism of its entry into Leishmania remains unclear [38]. Although not as conclusively documented as with Hst-5, there is some evidence that human bactericidal/permeability-increasing protein (BPI) also interferes with the bacterial NADH, ubiquinone oxidoreductase system in E. coli and Salmonella, thereby interfering with bacterial respiration and energy production [39]. HNP1 and thrombin-induced platelet microbicidal protein-1 (tPMP-1) are believed to inhibit translation by binding to staphylococcal 30s and 50s ribosomal subunits [40].
Inhibition of DNA Function
Laminins are a group of matrix proteins found throughout the human body that comprise three chains (α, β, and γ) linked by disulfide bridges. The globular C-terminus of the α-chain has 5 laminin G (LG) domain-like modules, two of which (LG4 and LG5) are secreted into the fluid phase following proteolytic cleavage, and can then bind to the DNA of S. aureus and E. coli and inhibit bacterial growth [9].
Immunological Functions of AMP
Chemotactic Function
AMPs are among the multiple chemotactic signals responsible for the influx of immune effector cells to the site of inflammation following tissue injury or infection. Defensins such as HNP1 and HNP2 that are released from neutrophil azurophilic granules cause the influx of monocytes and macrophages [41]. Human α- and β- defensins serve as chemoattractants for T cells and immature dendritic cells [42]; α-defensins attract CD45RA+ naïve T cells, while β-defensins attract CD45RO+ memory T cells and immature dendritic cells. The human cathelicidin LL-37 induces Ca2+ mobilization that is required for vesicle fusion and other cellular functions and also attracts neutrophils, monocytes, and T cells through the formyl peptide receptor-like 1 (FPRL1) [43].
Cytokine and Chemokine Induction
AMPs have also been implicated in chemokine and cytokine induction which lead to cellular influx and pro-inflammatory processes. For example, HNP1 and HNP4 cause mast cell degranulation and histamine release [44]. HNPs 1, 2, and 3 stimulate production of IL-8 by the bronchial epithelium and release of TNF-α, and IL-1 by monocytes, while simultaneously suppressing anti-inflammatory cytokines such as IL-10 [45]. HBD-3 can upregulate expression of co-stimulatory molecules such as CD80, CD86, and CD40 on monocytes and myeloid dendritic cells in a TLR 1- and TLR 2-dependent fashion that also involves downstream MyD88 and signaling IRAK-1 phosphorylation [46]. HBDs 2, 3, and 4 and LL-37 also induce the production of IL-18, IL-20, and IL-8 from human keratinocytes; these pro-inflammatory cytokines have been implicated in the pathogenesis of skin diseases such as psoriasis. HNPs 1, 2, and 3 stimulate IL-1, IL-4, IL-6, TNF-α, and IFN-γ from monocytes, and chemokines such as MCP-1 and MIP-2 from pulmonary epithelial cells, while the cathelicidin LL-37 induces IL-8, MCP-1, and MCP-3 production from monocytes and airway epithelium [47]. Such cytokine induction may subsequently trigger cascades where other immune cells like T, B, and NK cells are also activated to produce chemokines [42].
Defensins may also modulate activity of the complement system, although their role remains controversial. HNPs 1–3 immobilized to microtiter wells bind C1q and activate the classical pathway [48]. Although the C1q binding motif on defensins has not been localized, they possess structural and sequence homology with HIV gp41, which also binds C1q. Both gp41 and defensins contain charged amino acids arranged in a loop-like structure similar to the C1q binding motif in IgG (ExKxK) [48]. By contrast, Groeneveld and colleagues showed that HNP-1 binds to the collagen stalk regions of C1q and MBL in a Ca2+-independent manner and blocked activation of the classical and lectin pathways, respectively [49]. The authors posited that defensins may limit excessive complement activation at sites of tissue injury.
Resistance to Antimicrobial Peptides
Successful establishment of infection requires the pathogen to evade host defenses. While widespread resistance to currently available antibiotics has generated considerable interest in AMPs as possible alternatives in the management of infectious diseases, it is not surprising that resistance to these agents have been documented in several pathogens (summarized in Table 5.2).
Alteration of Cell Surface Properties
Cationic AMPs attack the negatively charged bacterial outer membrane. Bacteria have evolved mechanisms to decrease the affinity of their interaction with AMPs by making their cell surfaces less electronegative, either by adding positively charged residues or by removing negatively charged moieties. For instance, members of the Burkholderia cepacia complex, S. enterica serovar typhimurium, and Proteus mirabilis add a 4-amino-4-deoxy-T-arabinose group to the lipid A moiety of LPS that imparts a positive charge that neutralizes the negative charge of the phosphate group, thereby conferring resistance to polymyxin B. Similarly, the addition of phosphoethanolamine (PEtn) residues to the lipid A of Neisserial lipooligosaccharides renders them resistant to polymyxin, LL-37, and protegrin [50, 51]. While the classical biotype of Vibrio cholerae is susceptible to polymyxin, the O1 El Tor biotype is resistant to this AMP because it possesses glycine and diglycine residues in its lipid A [50]. Gram-positive bacteria like S. aureus, group B streptococci, and Listeria monocytogenes all possess a four-gene operon dltABCD, the products of which add D-alanine to the negatively charged polyanionic teichoic acid backbone. However, some authors suggest that D-alanylation-mediated AMP resistance is not because of decreased negative charge of the surface, but the result of enhanced cell wall density, which inhibits the interaction with AMPs. The addition of L-lysine to the anionic phosphatidylglycerol by the product of mprF of S. aureus renders it resistant to neutrophil defensins [50]. Francisella novicida and Helicobacter pylori resist polymyxin B by reducing the negative charge of their lipid A through lipid A phosphatase-mediated elimination of the 4′ phosphate [51].
Decoy Targets and Trapping of AMPs
Several bacteria and fungi elaborate capsules or glycocalyces or other exopolysaccharides that act as decoy targets or matrices for AMPs and sequester them such that they cannot reach their target membranes. A notable example is the anionic alginic acid capsule of Pseudomonas aeruginosa, which traps cationic AMPs before they can traverse to the membrane, thereby rendering the organism resistant to their bactericidal activity. Capsules and slime layers of most pathogens bear a negative charge and can be hypothesized to confer resistance against AMPs in a similar fashion [52]. Resistance of serogroup B Neisseria meningitidis to polymyxin B, α- and β-defensins, cathelicidin, and mCRAMP has been attributed to its capsular polysaccharide [51]. Other pathogens such as Klebsiella pneumoniae, Haemophilus influenzae, Legionella pneumophila, Streptococcus pneumoniae, and Bacillus anthracis may also employ similar AMP defense mechanisms [52]. Staphylokinase released by S. aureus forms complexes with α-defensins such as HNP1 and HNP2 and protects bacteria from their bactericidal effects [53]. Another protein, streptococcal inhibitor of complement (SIC) , that is produced in copious amounts by Streptococcus pyogenes binds to and neutralizes the activities of HNP1 and LL-37 [54].
Active Efflux
Efflux pumps are energy-dependent protein complexes that extrude a variety of toxic molecules that may traverse the outer membrane, including AMPs. The resistance-nodulation-cell division (RND) pumps are driven by proton-motive force and anti-port H+ ions into the cell while expelling AMPs from the intracellular compartment [55]. For example, the MtrCDE pump (encoded by multiple transferable resistance genes mtrC, D, and E) in Neisseria gonorrhoeae confers resistance to LL-37 and protegrin-1. Similarly, deleting mtrC in Haemophilus ducreyi enhances sensitivity to LL-37 and β-defensins [51]. The plasmid-encoded quaternary ammonium compounds A (QacA) multidrug efflux pump, a member of the major facilitator superfamily (MFS) of pumps, found in S. aureus as well as coagulase-negative Staphylococci anti-ports an AMP called thrombin-induced platelet microbicidal protein (tPMP-1) in exchange for H+ ions [56]. Others suggest that QacA-dependent alterations in the cytoplasmic membrane confer AMP resistance [57]. RosA/B, a potassium anti-porter efflux pump of the MFS family driven by proton-motive force in Yersinia spp. confers resistance to CAMPs such as polymyxin B [58]. Similarly, genetic deletion of the AcrAB efflux pump in Klebsiella pneumoniae significantly decreased bacterial survival in the presence of AMPs including polymyxin B, HNP1, HBD-1, and HBD-2 when compared to the wild-type strains [59]. The ATP-binding cassette (ABC) transporters utilize energy from ATP hydrolysis to scavenge and extrude AMPs from the periplasmic space [60]. Mutations of the ATP-binding domains of the ABC transporter encoded by yejABCDEF in S. typhimurium render it more sensitive to protamine, polymyxin B, melittin, HBD-1, and HBD-2 [61]. The action of efflux pumps appears to be AMP and bacteria specific because ectopic expression of such pumps in other bacteria does not confer resistance to AMPs. Further, overexpression of pumps that are responsible for resistance against particular AMPs in one genus may not confer resistance against the same AMPs in other genera [57].
Proteolytic Degradation
A number of pathogenic bacteria proteolytically degrade and inactivate AMPs. For instance, P. aeruginosa isolated from cutaneous ulcers expresses an elastase that proteolytically degrades LL-37, which allows the pathogen to survive in the presence of high concentrations of the AMP [62]. Burkholderia cepacia produces two zinc metalloproteases ZmpA and ZmpB, which degrade LL-37 and protamine, and HBD-1, respectively [63]. Aureolysin , a metalloproteinase expressed by S. aureus, cleaves LL-37 at multiple sites within its antibacterial C-terminal region. Bacterial survival in the presence of LL-37 correlated inversely with the amount of aureolysin expressed [64].The periodontal pathogen, Porphyromonas gingivalis elaborates proteases called gingipains, which degrade AMPs such as HBD-3 [65]. Omptins , a class of β-barrel membrane spanning aspartate proteases that hydrolyze proteins, are conserved across multiple genera within the Enterobacteriaceae family. They have five extracellular loops that determine substrate specificity. Both enterohemorrhagic and enteropathogenic E. coli (EHEC and EPEC, respectively) have an outer membrane omptin family protease, OmpT that cleaves α-helical AMPs such as LL-37 and C18G. The rate of cleavage is more rapid with EHEC OmpT than with EPEC OmpT [66]. PgtE which is a functional homolog of OmpT in Salmonella enterica cleaves the AMP C18G [67, 68].
Regulation of Host AMP Production and Activity
Stimulation of pattern recognition receptors (PRRs) such as TLRs by pathogen-associated molecular patterns (PAMPs) including LPS and teichoic acids results in activation of NF-κB, which upregulates host AMP production. The process is further amplified by chemokines and cytokines such as IL-1, IL-6, and TNF-α [50]. However, many pathogens have evolved to limit AMP production. For example, Streptococcus pyogenes is a poor inducer of HBD-2 production in terminally differentiated human epidermal keratinocytes [69]. RNA analysis from tissue biopsies from infected individuals and from epithelial and monocyte cell lines infected in vitro revealed that Shigella dysenteriae type I and S. flexneri actively suppress LL-37 and HBD-1 production during early phases of infection through a plasmid DNA-mediated process [70]. Cholera toxin from the Vibrio cholera O139 Bengal strain and labile toxin from enterotoxigenic E. coli (ETEC) transcriptionally repress the production of LL-37 and HBD-1 by activating several intracellular signaling pathways [71]. N. gonorrhoeae actively represses the production of LL-37 by epithelial cells [72]. P. aeruginosa that often colonizes the airways of individuals with cystic fibrosis upregulates the production of host cysteine proteases including cathepsins B, L, and S, which in turn degrade AMPs such as HBD-2 and HBD-3 [73].
Genetic Regulation of AMP Resistance
Bacterial genes that mediate AMP resistance are often transcribed only when the bacterium senses AMPs using two-component signaling systems (TCSSs) . TCSSs comprise a homodimeric membrane-bound periplasmic sensory protein that contains a histidine kinase (HK) domain and a cytoplasmic transcriptional response regulator (RR) protein, also organized as a homodimer. Upon stimulation, the HK domain catalyzes the ATP-dependent autophosphorylation of a conserved His residue within the HK dimerization region. The RR domain then catalyzes a phosphorelay whereby phosphate from the phospho-His in the HK domain is transferred to a conserved Asp residue in the RR. This event is followed by downstream activation of transcriptional regulators [74, 75].
In the PhoP/Q TCSS of Salmonella, PhoQ (the HK) senses low concentrations of divalent cations such as Mg2+ and Ca2+, or acidic pH within phagolysosomes, and phosphorylates PhoP (the RR), which in turn upregulates expression of pagP that palmitoylates lipid A. The resulting hepta-acylated lipid A alters membrane fluidity by enhancing hydrophobic interactions and renders it impermeable to α-helical AMPs [76, 77]. Phosphorylation of PhoP also upregulates PgtE, a membrane protease in Salmonella that cleaves α-helical AMPs such as C18G [77]. The HK of another Salmonella TCSS, PmrB, senses acidic pH and phosphorylates PmrA (the RR), which in turn regulates the pmrE/pmrF operon that adds positively charged moieties such as PEtn and aminoarabinose to LPS, thereby decreasing its negative charge and conferring resistance to polymyxin B as discussed above [77]. A TCSS homologous to the PmrA/PmrB is also present in P. aeruginosa, which upon stimulation adds aminoarabinose to the LPS and makes the organism polymyxin B resistant [78]. Additionally, P aeruginosa has two TCSSs called CprRS and ParRS that directly sense CAMPs such as CP28, indolicidin , and polymyxin B and activate the arnBCADTEF operon, which adds positively charged aminoarabinose to LPS, rendering the organism AMP resistant [79].
Clinical Use of Host Antimicrobial Peptides
Because of the widespread emergence of resistance to conventional antibiotics, AMPs may constitute an attractive alternative for the treatment of infectious diseases. They are effective against a broad spectrum of microorganisms, have a rapid onset of activity, and are relatively protected against development of resistance. Currently, only few AMPs, including polymyxin B, bacitracin, gramicidin, and glycopeptides such as vancomycin and teicoplanin, are licensed for clinical use. Some of the AMPs that have undergone or are currently undergoing clinical trials are discussed below.
Neuprex
Neuprex or rBPI21 is a 21 kDa recombinant form of the first 193 amino acid residues of N-terminal region of the 55 kDa bactericidal/permeability-increasing protein (BPI), where the cysteine at position 132 is replaced by alanine. BPI binds to LPS with high affinity, which forms the basis for its activity against gram-negative bacteria. Upon interaction with negatively charged membranes, rBPI21 induces aggregation and causes leakage through pores through hemifusion of inner and outer membranes enriched in phosphatidylglycerol [80, 81]. A phase 3 clinical trial assessed the efficacy of rBPI21 as adjunctive treatment of children with meningococcemia. The 60-day mortality among the 190 children who received rBPI21 and the 203 children who received placebo was 7.4% and 9.9%, respectively [82]. The lower than expected mortality in the placebo group led to the study being underpowered to obtain the desired improvement in survival with rBPI21. Among subjects who survived to receive the complete infusion of the study drug, mortality was 6.2% in the placebo group versus 2.2% in the rBPI21 group (P = 0.07). There were trends toward reduced requirement for renal replacement therapy, decreased need for blood products, and shorter time on ventilators in children who received rBPI21. Administration of rBPI21 was not associated with any major adverse effects. rBPI21 was also used in conjunction with conventional antibiotics in intra-abdominal infections and lung infection in persons with cystic fibrosis because this peptide may render otherwise drug-resistant organisms more sensitive to antibiotics. In a phase 2 trial in patients with hemorrhagic trauma, patients on Neuprex showed significantly better outcomes versus those on placebo [83].
Omiganan
Omiganan is a 12-amino acid peptide analog of indolicidin, an AMP found naturally in bovine neutrophil granules, with microbicidal activity against gram-positive and gram-negative bacteria, as well as fungi. Although its mechanism of action remains unclear, omiganan is hypothesized to cause cell death primarily by membrane depolarization and disintegration. It may also interact with DNA, thereby inhibiting the activity of DNA-binding enzymes and cause filamentation of genetic material [27]. Clinical trials suggest that topical omiganan gel may be effective for the prevention of intravascular catheter-related infections and the treatment of papulopustular rosacea. A study of topical omiganan for treatment of acne vulgaris is underway.
Pexiganan/MSI-78
Pexiganan is a synthetic derivative of the magainin-2, a naturally occurring AMP in the frog Xenopus laevis that has broad-spectrum (including anaerobes) bactericidal properties by forming toroidal pores in membranes [84]. Topical pexiganan is being evaluated for treatment of diabetic foot ulcers.
Iseganan/IB-367
Iseganan is derived from porcine protegrin-1 and also functions by forming pores in bacterial and fungal membranes [85]. Although topical iseganan reduced microbial colonization of the oropharynx, it failed to decrease the incidence of ventilator-associated pneumonia [86]. The drug is being evaluated to reduce the severity of oral mucositis in patients undergoing radiotherapy for head and neck cancer.
hLF1-11
Human lactoferrin-derived peptide , hLF1-11, is a synthetic peptide comprising the first 11 N-terminal residues of the native protein. It has activity against methicillin-resistant S. aureus, K. pneumoniae, L. monocytogenes, A. baumannii, and fluconazole-resistant C. albicans [87]. This peptide has direct microbicidal as well as immunomodulatory modes of action. It associates with anionic membranes through its positively charged N-terminal region and enhances membrane permeability [88, 89]. Upon stimulation with hLF1-11, monocyte differentiation was directed toward a subset of macrophages with a TLR 4-, 5-, and 7-mediated pro-inflammatory cytokine profile and enhanced effector functions against S. aureus and C. albicans [90, 91]. The peptide is currently being evaluated in hematopoietic stem cell transplant recipients to treat bacterial and fungal infections [92].
CZEN-002/8-mer α-Melanocyte-Stimulating Hormone (α-MSH) Derivative
This α-MSH derivative causes cAMP accumulation in C. albicans, thereby disrupting signaling pathways. CZEN-002 is also anti-inflammatory and suppresses TNF-α production [87]. CZEN-002 is currently in phase 2 trials for treatment of vulvovaginal candidiasis [92]. The peptide is also effective against C. krusei and C. glabrata, which are becoming increasingly drug-resistant.
PAC-113/Histatin 5 Derivative
PAC-113 is a derivative of the human salivary α-helical peptide histatin 5 (Hst-5) and has been granted an Investigational New Drug (IND) status by the FDA for treatment of oral candidiasis [87, 92]. It is active against several species of Candida such as C. albicans, C. glabrata, C. parapsilosis, and C. tropicalis, including drug-resistant isolates [87]. The mechanism of action of Hst-5 is dichotomous. On the one hand, Hst-5 can bind to the candidial membrane-bound heat shock protein (Ssa1/2), undergo receptor-mediated endocytosis, and subsequently target the mitochondria and intracellular plasma membranes. Alternatively, it can also function as a classical α-helical cationic AMP and interact with anionic membranes, causing membrane damage and cell death [38].
Several other antibacterial peptides are either in clinical development or in early stage clinical trials. The reader is referred to more detailed reviews on this subject [92,93,94].
Despite their broad spectrum of antimicrobial activity, often greater microbicidal efficacy on a molar basis when compared with conventional antibiotics, and limited evidence of development of acquired resistance, there are several considerations which have slowed development of these peptides as anti-infectives. Most AMPs are labile and susceptible to pH changes and proteolytic degradation within the host [87, 92]. This necessitates their use at high concentrations at which point they lose specificity for microbial membranes and often damage host cell membranes [95]. Toxicity following systemic administration often restricts their use to topical formulations. Moreover, effective drug delivery to locations where drug penetration is characteristically poor, or to intracellular sites, is another practical hurdle that hinders widespread use of these compounds. Finally, the costs of production of AMPs are often prohibitive, although engineering shorter peptides may help alleviate this problem [87, 92]. To overcome some of these obstacles, synthetic compounds called “peptidomimetics” are being developed. These molecules retain the function of AMPs but lack some of the drawbacks of AMPs listed above [94, 96].
Dysregulation of AMPs in Human Disease
The role of AMPs in human physiology is becoming increasingly appreciated. While causality between dysregulated AMP production and disease mechanisms is yet to be firmly established, associations between certain infections and diseases with presumed immunological origins and altered AMP levels have been documented. For instance, patients with atopic dermatitis (AD) have lower levels of dermicidin (DCD)-derived peptides in their sweat compared to healthy volunteers. Moreover, AD patients with histories of recurrent bacterial and viral skin infections had less DCD and DCD-1L in their sweat in comparison to AD patients with no prior history of infectious complications [97]. Skin biopsies of AD patients also revealed lower amounts of the cathelicidin LL-37 and human β-defensin 2 (HBD-2) compared to patients with psoriasis. These observations may account for the predisposition of AD patients to S. aureus infections [98]. On the other hand, enhanced inflammation as suggested by increased levels of LL-37 and HBD-2 may play a role in the pathogenesis of psoriasis [98] and rosacea [16]. Low levels of HBD-2, HBD-3, and LL-37 are also associated with atopic eczema [99]. The amount of HBD-2 in the intestinal mucosa correlates with copy number of the HBD-2. While normal hosts and individuals with ulcerative colitis or ileal Crohn’s disease (CD) possess four copies of the HBD-2 gene, the median copy number of the HBD-2 gene in patients with colonic CD is three (the difference was statistically significant), which led the authors to conclude that low HBD-2 production might be a predisposing factor for colonic CD [100].
Single-nucleotide polymorphisms (SNPs) in the DEFB1 gene that encodes for HBD-1 are associated with higher levels of oral carriage of Candida albicans [101]. Two independent studies have also associated SNPs in the DEFB1 gene with enhanced risk of perinatal acquisition of HIV-1 infections [102, 103].
Recurrent oral bacterial infections, especially periodontal infections associated with overgrowth of Actinobacillus actinomycetemcomitans, are a common feature of patients with Kostmann syndrome (severe congenital neutropenia). The neutrophils of these patients lack LL-37 and have diminished levels of HNPs 1–3. These individuals also lack LL-37 in their saliva and plasma. A patient in this cohort who underwent bone marrow transplantation, which restored normal plasma levels of LL-37, did not suffer from periodontal infections. These data suggest that LL-37 and HNPs 1–3 protect against periodontal infections [104]. Inadequate LL-37 activity may exacerbate the pathology of cystic fibrosis (CF). Under high salt concentrations seen in the alveolar surface fluid of persons with CF, LL-37 that is present at subinhibitory concentrations crosses the cell walls of P. aeruginosa, forms complexes with its DNA, and promotes mutations in the mucA gene, which controls alginate capsule production. These events culminate in the conversion of P. aeruginosa to a mucoid phenotype that produces high amounts of alginate, which promotes resistance to killing by LL-37 and correlates with a poor prognosis [105]. Other conditions associated with dysregulation of neutrophil AMP contents that lead to frequent severe bacterial infections are specific granule deficiency (SGD) and Chediak-Higashi syndrome (CHS) . SGD patients have normal levels of cathepsins and elastase, but lack defensins, while the converse occurs in CHS [106]. In a study conducted in Zambia, intestinal biopsy specimens from adults who had recently suffered from diarrhea but were disease-free for a month had tenfold lower mRNA transcripts of α-defensins (HD5 and HD6) compared to patients with no history of diarrhea. While the authors suggested that decreased α-defensins may predispose to diarrhea, it should be noted that the intestinal microbiome itself regulates AMP production, which could confound interpretation of the results [107]. The examples listed above only associate dysregulation of AMPs and disease; further research is required to establish causality.
Concluding Remarks
The widespread emergence of antibiotic resistance has led the scientific community to look for newer therapies, which has led to renewed interest in AMPs. The role of AMPs in physiology is becoming more clearly elucidated. While the prevailing view is that AMPs have an important role in antimicrobial defenses, some argue that this hypothesis is supported mostly by in vitro experiments that have used supraphysiologic concentrations of AMPs. They suggest that physiologic concentrations AMPs may play important roles in immunomodulation and processes such as wound healing. Studies have associated dysregulation of AMPs with immune-mediated disorders, normal physiology, and infections. While further research is needed to establish firm causality between defects in AMPs and diseases, the information harnessed so far has provided the foundation for development of AMP-based therapies. Although AMP-based therapies have not yet met with much clinical success, increasing knowledge in the field, coupled with advances in protein engineering, could witness successful AMP-based therapies in the near future.
References
Wang G, Li X, Wang Z. APD3: the antimicrobial peptide database as a tool for research and education. Nucleic Acids Res. 2016;44(D1):D1087–93.
Zimmer J, Hobkirk J, Mohamed F, Browning M, Stover CM. On the functional overlap between complement and antimicrobial peptides. Front Immunol. 2015;5
Zasloff M. Antimicrobial peptides of multicellular organisms. Nature. 2002;415(6870):389–95.
Park Y, Hahm KS. Antimicrobial peptides (AMPs): peptide structure and mode of action. J Biochem Mol Biol. 2005;38(5):507–16.
Tennessen JA. Molecular evolution of animal antimicrobial peptides: widespread moderate positive selection. J Evol Biol. 2005;18(6):1387–94.
Zhang LJ, Gallo RL. Antimicrobial peptides. Curr Biol. 2016;26(1):R14–9.
Hollox EJ, Armour JA, Barber JC. Extensive normal copy number variation of a beta-defensin antimicrobial-gene cluster. Am J Hum Genet. 2003;73(3):591–600.
Coda AB, et al. Cathelicidin, kallikrein 5, and serine protease activity is inhibited during treatment of rosacea with azelaic acid 15% gel. J Am Acad Dermatol. 2013;69(4):570–7.
Senyurek I, Klein G, Kalbacher H, Deeg M, Schittek B. Peptides derived from the human laminin alpha 4 and alpha 5 chains exhibit antimicrobial activity. Peptides. 2010;31(8):1468–72.
Mansour SC, Pena OM, Hancock REW. Host defense peptides: front-line immunomodulators. Trends Immunol. 2014;35(9):443–50.
Steinstraesser L, Kraneburg U, Jacobsen F, Al-Benna S. Host defense peptides and their antimicrobial-immunomodulatory duality. Immunobiology. 2011;216(3):322–33.
Meisch JP, et al. Human beta-defensin 3 peptide is increased and redistributed in Crohn’s ileitis. Inflamm Bowel Dis. 2013;19(5):942–53.
Lande R, et al. Plasmacytoid dendritic cells sense self-DNA coupled with antimicrobial peptide. Nature. 2007;449(7162):564–9.
Scott MG, Davidson DJ, Gold MR, Bowdish D, Hancock RE. The human antimicrobial peptide LL-37 is a multifunctional modulator of innate immune responses. J Immunol. 2002;169(7):3883–91.
Rosenfeld Y, Papo N, Shai Y. Endotoxin (lipopolysaccharide) neutralization by innate immunity host-defense peptides. Peptide properties and plausible modes of action. J Biol Chem. 2006;281(3):1636–43.
Yamasaki K, et al. Increased serine protease activity and cathelicidin promotes skin inflammation in rosacea. Nat Med. 2007;13(8):975–80.
Courth LF, et al. Crohn's disease-derived monocytes fail to induce Paneth cell defensins. Proc Natl Acad Sci U S A. 2015;112(45):14000–5.
Wang G. Improved methods for classification, prediction, and design of antimicrobial peptides. Methods Mol Biol. 2015;1268:43–66.
Zanetti M. Cathelicidins, multifunctional peptides of the innate immunity. J Leukoc Biol. 2004;75(1):39–48.
Bulet P, Stocklin R, Menin L. Anti-microbial peptides: from invertebrates to vertebrates. Immunol Rev. 2004;198:169–84.
Brogden KA. Antimicrobial peptides: pore formers or metabolic inhibitors in bacteria? Nat Rev Microbiol. 2005;3(3):238–50.
Ahmad A, et al. Identification and design of antimicrobial peptides for therapeutic applications. Curr Protein Pept Sci. 2012;13(3):211–23.
White SH, Wimley WC, Selsted ME. Structure, function, and membrane integration of defensins. Curr Opin Struct Biol. 1995;5(4):521–7.
Lehrer RI, Cole AM, Selsted ME. θ-Defensins: cyclic peptides with endless potential. J Biol Chem. 2012;287(32):27014–9.
Yount NY, Yeaman MR. Immunocontinuum: perspectives in antimicrobial peptide mechanisms of action and resistance. Protein Pept Lett. 2005;12(1):49–67.
Shah P, Hsiao FS, Ho YH, Chen CS. The proteome targets of intracellular targeting antimicrobial peptides. Proteomics. 2015.
Nguyen LT, Haney EF, Vogel HJ. The expanding scope of antimicrobial peptide structures and their modes of action. Trends Biotechnol. 2011;29(9):464–72.
Cho J, et al. The novel biological action of antimicrobial peptides via apoptosis induction. J Microbiol Biotechnol. 2012;22(11):1457–66.
Burian M, Schittek B. The secrets of dermcidin action. Int J Med Microbiol. 2015;305(2):283–6.
Sass V, et al. Human beta-defensin 3 inhibits cell wall biosynthesis in Staphylococci. Infect Immun. 2010;78(6):2793–800.
de Leeuw E, et al. Functional interaction of human neutrophil peptide-1 with the cell wall precursor lipid II. FEBS Lett. 2010;584(8):1543–8.
Spencer JD, et al. Ribonuclease 7, an antimicrobial peptide upregulated during infection, contributes to microbial defense of the human urinary tract. Kidney Int. 2013;83(4):615–25.
Lin YM, et al. Outer membrane protein I of Pseudomonas aeruginosa is a target of cationic antimicrobial peptide/protein. J Biol Chem. 2010;285(12):8985–94.
Kim HS, et al. Endotoxin-neutralizing antimicrobial proteins of the human placenta. J Immunol. 2002;168(5):2356–64.
Hazrati E, et al. Human α- and β-Defensins block multiple steps in herpes simplex virus infection. J Immunol. 2006;177(12):8658–66.
Helmerhorst EJ, et al. The cellular target of histatin 5 on Candida albicans is the energized mitochondrion. J Biol Chem. 1999;274(11):7286–91.
Luque-Ortega JR, van’t Hof W, Veerman EC, Saugar JM, Rivas L. Human antimicrobial peptide histatin 5 is a cell-penetrating peptide targeting mitochondrial ATP synthesis in Leishmania. FASEB J. 2008;22(6):1817–28.
Mochon AB, Liu H. The antimicrobial peptide histatin-5 causes a spatially restricted disruption on the Candida albicans surface, allowing rapid entry of the peptide into the cytoplasm. PLoS Pathog. 2008;4(10):e1000190.
Barker HC, Kinsella N, Jaspe A, Friedrich T, O’Connor CD. Formate protects stationary-phase Escherichia coli and Salmonella cells from killing by a cationic antimicrobial peptide. Mol Microbiol. 2000;35(6):1518–29.
Backo M, Gaenger E, Burkart A, Chai YL, Bayer AS. Treatment of experimental staphylococcal endocarditis due to a strain with reduced susceptibility in vitro to vancomycin: efficacy of ampicillin-sulbactam. Antimicrob Agents Chemother. 1999;43(10):2565–8.
Territo MC, Ganz T, Selsted ME, Lehrer R. Monocyte-chemotactic activity of defensins from human neutrophils. J Clin Invest. 1989;84(6):2017–20.
Lai Y, Gallo RL. AMPed up immunity: how antimicrobial peptides have multiple roles in immune defense. Trends Immunol. 2009;30(3):131–41.
De Y, et al. LL-37, the neutrophil granule- and epithelial cell-derived cathelicidin, utilizes formyl peptide receptor-like 1 (FPRL1) as a receptor to chemoattract human peripheral blood neutrophils, monocytes, and T cells. J Exp Med. 2000;192(7):1069–74.
Befus AD, et al. Neutrophil defensins induce histamine secretion from mast cells: mechanisms of action. J Immunol. 1999;163(2):947–53.
Yang D, Biragyn A, Kwak LW, Oppenheim JJ. Mammalian defensins in immunity: more than just microbicidal. Trends Immunol. 2002;23(6):291–6.
Funderburg N, et al. Human -defensin-3 activates professional antigen-presenting cells via Toll-like receptors 1 and 2. Proc Natl Acad Sci U S A. 2007;104(47):18631–5.
Niyonsaba F, Ushio H, Nagaoka I, Okumura K, Ogawa H. The human beta-defensins (-1, -2, -3, -4) and cathelicidin LL-37 induce IL-18 secretion through p38 and ERK MAPK activation in primary human keratinocytes. J Immunol. 2005;175(3):1776–84.
Prohaszka Z, et al. Defensins purified from human granulocytes bind C1q and activate the classical complement pathway like the transmembrane glycoprotein gp41 of HIV-1. Mol Immunol. 1997;34(11):809–16.
Groeneveld TW, et al. Human neutrophil peptide-1 inhibits both the classical and the lectin pathway of complement activation. Mol Immunol. 2007;44(14):3608–14.
Nizet V. Antimicrobial peptide resistance mechanisms of human bacterial pathogens. Curr Issues Mol Biol. 2006;8:11–26.
Gruenheid S, Le Moual H. Resistance to antimicrobial peptides in Gram-negative bacteria. FEMS Microbiol Lett. 2012;330(2):81–9.
Yeaman MR, Yount NY. Mechanisms of antimicrobial peptide action and resistance. Pharmacol Rev. 2003;55(1):27–55.
Jin T, et al. Staphylococcus aureus resists human defensins by production of staphylokinase, a novel bacterial evasion mechanism. J Immunol. 2004;172(2):1169–76.
Frick IM, Akesson P, Rasmussen M, Schmidtchen A, Bjorck L. SIC, a secreted protein of Streptococcus pyogenes that inactivates antibacterial peptides. J Biol Chem. 2003;278(19):16561–6.
Paulsen IT, Brown MH, Skurray RA. Proton-dependent multidrug efflux systems. Microbiol Rev. 1996;60(4):575–608.
Xu Z, O’Rourke BA, Skurray RA, Brown MH. Role of transmembrane segment 10 in efflux mediated by the staphylococcal multidrug transport protein QacA. J Biol Chem. 2006;281(2):792–9.
Guilhelmelli F, et al. Antibiotic development challenges: the various mechanisms of action of antimicrobial peptides and of bacterial resistance. Front Microbiol. 2013;4:353.
Bengoechea JA, Skurnik M. Temperature-regulated efflux pump/potassium antiporter system mediates resistance to cationic antimicrobial peptides in Yersinia. Mol Microbiol. 2000;37(1):67–80.
Padilla E, et al. Klebsiella pneumoniae AcrAB efflux pump contributes to antimicrobial resistance and virulence. Antimicrob Agents Chemother. 2010;54(1):177–83.
Nikaido H, Hall JA. Overview of bacterial ABC transporters. Methods Enzymol. 1998;292:3–20.
Eswarappa SM, Panguluri KK, Hensel M, Chakravortty D. The yejABEF operon of Salmonella confers resistance to antimicrobial peptides and contributes to its virulence. Microbiology. 2008;154(Pt 2):666–78.
Schmidtchen A, Frick IM, Andersson E, Tapper H, Bjorck L. Proteinases of common pathogenic bacteria degrade and inactivate the antibacterial peptide LL-37. Mol Microbiol. 2002;46(1):157–68.
Kooi C, Sokol PA. Burkholderia cenocepacia zinc metalloproteases influence resistance to antimicrobial peptides. Microbiology. 2009;155(Pt 9):2818–25.
Sieprawska-Lupa M, et al. Degradation of human antimicrobial peptide LL-37 by Staphylococcus aureus-derived proteinases. Antimicrob Agents Chemother. 2004;48(12):4673–9.
Maisetta G, Brancatisano FL, Esin S, Campa M, Batoni G. Gingipains produced by Porphyromonas gingivalis ATCC49417 degrade human-beta-defensin 3 and affect peptide’s antibacterial activity in vitro. Peptides. 2011;32(5):1073–7.
Thomassin JL, Brannon JR, Gibbs BF, Gruenheid S, Le Moual H. OmpT outer membrane proteases of enterohemorrhagic and enteropathogenic Escherichia coli contribute differently to the degradation of human LL-37. Infect Immun. 2012;80(2):483–92.
Grodberg J, Dunn JJ. Comparison of Escherichia coli K-12 outer membrane protease OmpT and Salmonella typhimurium E protein. J Bacteriol. 1989;171(5):2903–5.
Guina T, Yi EC, Wang H, Hackett M, Miller SI. A PhoP-regulated outer membrane protease of Salmonella enterica serovar typhimurium promotes resistance to alpha-helical antimicrobial peptides. J Bacteriol. 2000;182(14):4077–86.
Dinulos JG, Mentele L, Fredericks LP, Dale BA, Darmstadt GL. Keratinocyte expression of human beta defensin 2 following bacterial infection: role in cutaneous host defense. Clin Diagn Lab Immunol. 2003;10(1):161–6.
Islam D, et al. Downregulation of bactericidal peptides in enteric infections: a novel immune escape mechanism with bacterial DNA as a potential regulator. Nat Med. 2001;7(2):180–5.
Chakraborty K, et al. Bacterial exotoxins downregulate cathelicidin (hCAP-18/LL-37) and human beta-defensin 1 (HBD-1) expression in the intestinal epithelial cells. Cell Microbiol. 2008;10(12):2520–37.
Bergman P, et al. Neisseria gonorrhoeae downregulates expression of the human antimicrobial peptide LL-37. Cell Microbiol. 2005;7(7):1009–17.
Taggart CC, et al. Inactivation of human beta-defensins 2 and 3 by elastolytic cathepsins. J Immunol. 2003;171(2):931–7.
West AH, Stock AM. Histidine kinases and response regulator proteins in two-component signaling systems. Trends Biochem Sci. 2001;26(6):369–76.
Beier D, Gross R. Regulation of bacterial virulence by two-component systems. Curr Opin Microbiol. 2006;9(2):143–52.
Guo L, et al. Lipid A acylation and bacterial resistance against vertebrate antimicrobial peptides. Cell. 1998;95(2):189–98.
Ernst RK, Guina T, Miller SI. Salmonella typhimurium outer membrane remodeling: role in resistance to host innate immunity. Microbes Infect. 2001;3(14–15):1327–34.
Moskowitz SM, Ernst RK, Miller SI. PmrAB, a two-component regulatory system of Pseudomonas aeruginosa that modulates resistance to cationic antimicrobial peptides and addition of aminoarabinose to lipid A. J Bacteriol. 2004;186(2):575–9.
Fernandez L, et al. The two-component system CprRS senses cationic peptides and triggers adaptive resistance in Pseudomonas aeruginosa independently of ParRS. Antimicrob Agents Chemother. 2012;56(12):6212–22.
Domingues MM, Castanho MA, Santos NC. rBPI(21) promotes lipopolysaccharide aggregation and exerts its antimicrobial effects by (hemi)fusion of PG-containing membranes. PLoS One. 2009;4(12):e8385.
Domingues MM, Lopes SC, Santos NC, Quintas A, Castanho MA. Fold-unfold transitions in the selectivity and mechanism of action of the N-terminal fragment of the bactericidal/permeability-increasing protein (rBPI(21)). Biophys J. 2009;96(3):987–96.
Levin M, et al. Recombinant bactericidal/permeability-increasing protein (rBPI21) as adjunctive treatment for children with severe meningococcal sepsis: a randomised trial. rBPI21 Meningococcal Sepsis Study Group. Lancet. 2000;356(9234):961–7.
Mackin WM. Neuprex XOMA Corp. IDrugs. 1998;1(6):715–23.
Gottler LM, Ramamoorthy A. Structure, membrane orientation, mechanism, and function of pexiganan – a highly potent antimicrobial peptide designed from magainin. Biochim Biophys Acta. 2009;1788(8):1680–6.
Bolintineanu DS, Vivcharuk V, Kaznessis YN. Multiscale models of the antimicrobial peptide protegrin-1 on Gram-negative bacteria membranes. Int J Mol Sci. 2012;13(9):11000–11.
Jerse AE, et al. Multiple gonococcal opacity proteins are expressed during experimental urethral infection in the male. J Exp Med. 1994;179(3):911–20.
Seo MD, Won HS, Kim JH, Mishig-Ochir T, Lee BJ. Antimicrobial peptides for therapeutic applications: a review. Molecules. 2012;17(10):12276–86.
Nibbering PH, et al. Human lactoferrin and peptides derived from its N terminus are highly effective against infections with antibiotic-resistant bacteria. Infect Immun. 2001;69(3):1469–76.
Lupetti A, et al. Human lactoferrin-derived peptide’s antifungal activities against disseminated Candida albicans infection. J Infect Dis. 2007;196(9):1416–24.
van der Does AM, et al. The human lactoferrin-derived peptide hLF1-11 primes monocytes for an enhanced TLR-mediated immune response. Biometals. 2010;23(3):493–505.
van der Does AM, et al. Antimicrobial peptide hLF1-11 directs granulocyte-macrophage colony-stimulating factor-driven monocyte differentiation toward macrophages with enhanced recognition and clearance of pathogens. Antimicrob Agents Chemother. 2010;54(2):811–6.
Hancock RE, Sahl HG. Antimicrobial and host-defense peptides as new anti-infective therapeutic strategies. Nat Biotechnol. 2006;24(12):1551–7.
Fjell CD, Hiss JA, Hancock RE, Schneider G. Designing antimicrobial peptides: form follows function. Nat Rev Drug Discov. 2012;11(1):37–51.
Mendez-Samperio P. Peptidomimetics as a new generation of antimicrobial agents: current progress. Infect Drug Resist. 2014;7:229–37.
Aoki W, Kuroda K, Ueda M. Next generation of antimicrobial peptides as molecular targeted medicines. J Biosci Bioeng. 2012;114(4):365–70.
Mojsoska B, Jenssen H. Peptides and Peptidomimetics for antimicrobial drug design. Pharmaceuticals (Basel). 2015;8(3):366–415.
Rieg S, et al. Deficiency of dermcidin-derived antimicrobial peptides in sweat of patients with atopic dermatitis correlates with an impaired innate defense of human skin in vivo. J Immunol. 2005;174(12):8003–10.
Ong PY, et al. Endogenous antimicrobial peptides and skin infections in atopic dermatitis. N Engl J Med. 2002;347(15):1151–60.
Rivas-Santiago B, Serrano CJ, Enciso-Moreno JA. Susceptibility to infectious diseases based on antimicrobial peptide production. Infect Immun. 2009;77(11):4690–5.
Fellermann K, et al. A chromosome 8 gene-cluster polymorphism with low human beta-defensin 2 gene copy number predisposes to Crohn disease of the colon. Am J Hum Genet. 2006;79(3):439–48.
Jurevic RJ, Bai M, Chadwick RB, White TC, Dale BA. Single-nucleotide polymorphisms (SNPs) in human beta-defensin 1: high-throughput SNP assays and association with Candida carriage in type I diabetics and nondiabetic controls. J Clin Microbiol. 2003;41(1):90–6.
Segat L, et al. DEFB-1 genetic polymorphism screening in HIV-1 positive pregnant women and their children. J Matern Fetal Neonatal Med. 2006;19(1):13–6.
Milanese M, et al. DEFB1 gene polymorphisms and increased risk of HIV-1 infection in Brazilian children. AIDS. 2006;20(12):1673–5.
Pütsep K, Carlsson G, Boman HG, Andersson M. Deficiency of antibacterial peptides in patients with morbus Kostmann: an observation study. Lancet. 2002;360(9340):1144–9.
Limoli DH, et al. Cationic antimicrobial peptides promote microbial mutagenesis and pathoadaptation in chronic infections. PLoS Pathog. 2014;10(4):e1004083.
Ganz T, Metcalf JA, Gallin JI, Boxer LA, Lehrer RI. Microbicidal/cytotoxic proteins of neutrophils are deficient in two disorders: Chediak-Higashi syndrome and “specific” granule deficiency. J Clin Invest. 1988;82(2):552–6.
Kelly P, et al. Reduced gene expression of intestinal alpha-defensins predicts diarrhea in a cohort of African adults. J Infect Dis. 2006;193(10):1464–70.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Chakraborti, S., Ram, S. (2018). Antimicrobial Peptides. In: Segal, B. (eds) Management of Infections in the Immunocompromised Host. Springer, Cham. https://doi.org/10.1007/978-3-319-77674-3_5
Download citation
DOI: https://doi.org/10.1007/978-3-319-77674-3_5
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-77672-9
Online ISBN: 978-3-319-77674-3
eBook Packages: MedicineMedicine (R0)