Abstract
A considerable body of pre-clinical and clinical research data support a pivotal role played by immune-inflammatory responses in atherosclerosis formation and development. Recent clinical trial results confirm the feasibility of targeting immune pathways for the therapeutic control of the pathology. In this chapter, we discuss the key immune-inflammatory mechanisms involved in atherosclerosis development and progression and plaque destabilization. We discuss the anti-inflammatory pleiotropic effects of lipid-lowering drugs and potential therapeutic strategies for the direct control of vascular inflammation. Finally, we discuss vaccination approaches in atherosclerosis and critical questions that should be addressed in future investigations.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
1 Atherosclerosis
Atherosclerosis and related cardiovascular diseases (CVDs ) are the principal cause of death worldwide [1]. The atherosclerotic lesion, known as atheroma, consists of the accumulation of cells, debris, lipids and extracellular matrix (ECM) components in the inner layer of the artery, inducing a thickening of the intima in small and medium sized arteries. Symptomatic pathologies occur when the atheroma rupture occludes the blood flow through the arteries and, depending on the location of the obstruction, the blood cessation can lead to more severe complications such as myocardial infarction and death [2].
At first, atherosclerosis had been considered exclusively as an arterial occlusive disease in which the accumulation of cells, mainly smooth muscle cells (SMCs) and macrophages, in conjunction with lipids represents the central mechanism in the formation of the stenosis. For decades, the degree of the stenosis, combined with the manifestation of symptoms represented the only tools available for the assessment of atherosclerosis [2].
The cholesterol hypothesis is the most accredited pathophysiological theory for the development of atherosclerosis. It postulates that hypercholesterolemia is the causal factor in disease development. Indeed, elevated blood cholesterol levels, in particular low-density lipoprotein (LDL) are directly correlated to adverse cardiovascular events (ACEs) and denote an incontrovertible risk factor. Most importantly, normalising circulating cholesterol levels significantly reduces the burden of disease and its clinical consequences [3]. In addition to actively lowering modifiable risk factors, the identification of multiple molecular pathways that regulate cholesterol metabolism has led to the development of effective drug therapies. Statins are the main class of lipid-lowering drugs developed to reduce circulating levels of LDL and are effective in treating CVDs. More recently, the Food and Drug Administration (FDA) and the European Medicines Agency (EMA) approved monoclonal antibodies that inactivate proprotein convertase subtilisin/kexin type 9 (PCSK9) as new drugs to reduce circulating LDL. Despite these substantial advances in controlling circulating LDL levels, the recurrent rate of ACEs is approximately 20% within 3 years [4], with many individuals who experience myocardial infarction having cholesterol concentrations at currently mandated targets.
1.1 The Immune-Inflammatory Nature of Atherosclerosis
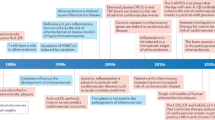
There is currently a wide acceptance that atherosclerosis consists not only of accumulation of lipids in the arterial wall but that a local chronic inflammatory response, consisting of both innate and adaptive immunity , represents a critical factor in the development and progression of the pathology (Fig. 1).
Inflammation and immune cells are crucially involved in atherosclerosis progression and plaque destabilization. (A, B) Circulating LDL diffuse and accumulate in the sub endothelial layer of medium and large sized arteries, undergoing a process of oxidation. (C) OxLDL are an inflammatory trigger dictating the recruitment of monocytes/macrophages into the vessel wall. (D) The activated monocytes differentiate intro macrophages, which are deputed to phagocyte and remove arterial debris. Sustained phagocytosis of LDL by macrophages creates cholesterol ester-laden foam cells. (E) The local production of inflammatory mediators induces the intensification of endothelial cell activation . The subsequent expression of other adhesion molecules facilitates the recruitment of multiple subtypes of leukocytes. (F) In advanced atheroma, the reactivation and local proliferation of detrimental T cells subtypes is well documented, as is the accumulation of immune cells in the adventitial space and the formation of tertiary lymphoid organs, known as ATLOs. (G, H) On the other hand, the inflammatory mediators are strong activators of smooth muscle cells . Once activated, they are able to migrate from the media and proliferate in the intimal layer of the vessel producing a protective coating known as fibrous cap. This is an essential feature of the stable plaque phenotype. (I) During acute local immune-inflammatory activation , the production of digesting enzymes, e.g. metalloproteinases, critically degrades the protective layer with the subsequent formation of thrombi
The generation of radical oxygen species (ROS) is a key event in the vessel wall disease. ROS are produced as part of the physiological respiration or pathological processes and participate in the formation of a microenvironment suitable to oxidation. Inflammation is closely interconnected with the production of ROS. In fact, the local production of ROS is able per se to induce an inflammatory state [5, 6].
The increase in circulating cholesterol facilitates the deposition of LDL in the subendothelial layer of the artery wall. The local accumulation of lipids is an inflammatory trigger, dictating the recruitment of monocytes/macrophages, the cells deputed to phagocytose and remove arterial oxidative lipids. This process amplifies the production of local ROS formation and the subsequent oxidation of LDL (ox-LDL) . In particular, the oxidation of LDL results in the modification of apolipoproteins (apo), such as apoB-100. Interestingly, it has been previously demonstrated that the modification of apoB-100 activates in vitro the scavenger receptor mediated uptake of lipid particles by macrophages [7,8,9].
The ox-LDL particles are a strong activator of endothelial cells (ECs), inducing the expression of adhesion molecules such as intracellular adhesion molecule-1 (ICAM-1) , which facilitates the subsequent recruitment of monocytes in concert with enhanced local chemokine release. Following differentiation, macrophages display elevated expression of scavenger receptors on their surface (i.e. SR-A, LOX-1, CXCL16 and CD36) [10]. The continuous cycle of LDL deposition, oxidation and endothelial dysfunction mediated by the local inflammatory process leads to the recruitment of a large number of macrophages. The sustained phagocytosis of LDL by-products creates cholesterol ester-laden foam cells. The accumulation of foam cells and lipids within the intima (termed ‘fatty-streak lesion’) is the first step in the development of a more complex atherosclerotic lesion. In parallel, macrophages can proliferate and secrete several inflammatory mediators, most notably interleukin (IL)-1β, which function to sustain and amplify the inflammatory response. Depletion of monocytes from the circulation in hypercholesterolemic rabbits significantly reduced plaque formation, implying a major role for monocytes in atherosclerosis [11].
In the 1980s, the first clear documentation of T lymphocytes in human atherosclerotic plaque was published, which consisted of histological identification of adaptive immune cells located within a human atherosclerotic plaque [12]. Subsequently, the identification of major histocompatibility complex (MHC) class II expression in multiple cell types within the plaque supported the evidence of an active local adaptive immune response [13].
Amongst CD4+ T cell subtypes, Th1 T cells are mainly responsible for driving atherogenesis [14]. Indeed, in advanced human lesions, Th1 markers correlate with ACEs [15] and the plaque microenvironment contains several Th1 pro-inflammatory cytokines, such as IFN-γ and TNF-α [2]. Dendritic cells (DCs) are the most effective antigen presenting cells (APCs) and are located in the intimal and adventitial space of healthy arteries. The number of DCs increases in the aorta of atherosclerotic mice and in human atherosclerotic lesions. During atherosclerosis progression, other APCs display a parallel increase in number, including B cells and macrophages [16].
T cells recruited to the atherosclerotic lesion can locally recognise antigens presented as peptides on MHC-II by APCs and undergo reactivation. In fact, human lesional CD4+ T cells can be reactivated in vitro by plaque antigens [17].
The detrimental role of Th1 T cells is counterbalanced by regulatory T cells (Treg) producing anti-atherogenic TGF-β and IL-10 [17]. We have recently provided strong evidence for a functional local adaptive immune response in the advanced stages of atherosclerosis in hyperlipidemic apolipoprotein-E (apoE)−/− mice in which the formation of artery tertiary lymphoid organs (ATLOs) occurs in the adventitia, adjacent to underlying plaques. These lymphoid structures are organized into well-defined immune cell compartments, including T cell areas, activated B cell follicles and zones with plasma cells. They are characterised by a high content in Tregs and are capable of controlling vascular T cell responses leading to a reduction in plaque size [18].
Of note, a broad range of innate and adaptive immune cells are also present in healthy vessels [18, 19].
1.2 Plaque Progression and Destabilization
In response to multiple inflammatory stimuli secreted by macrophages and ECs, SMCs migrate from the tunica media to the intimal space where they start to proliferate, creating a protective layer, known as the fibrous cap. SMCs are the primary cells responsible for the production of the ECM that further stabilises the fibrous cap. These processes cause the lesion to evolve into a fibrotic plaque that encapsulates the lipid and necrotic core. The rupture of the plaque cap is the most important mechanism underlying the sudden thrombotic occlusion of the vessel lumen, responsible for clinical events.
In the generation of the fibrous protective layer, the role of growth factors such as platelet derived growth factor (PDGF)-BB, cytokines such as tumour necrosis factor (TNF)-α and chemokines such as chemokine (C-C motif) ligands (CCL)-2 are required for the induction, migration and proliferation of the SMCs [20,21,22].
On the other hand, pro-inflammatory cytokines and chemokines modulate a number of detrimental steps in the control of plaque stability and rupture. A balance between the expression of matrix metalloproteinases (MMPs) and their inhibitors (TIMPs, tissue inhibitor of metalloproteinases) regulates the degradation and synthesis of the ECM. The expression and activity of MMPs and TIMPs are directly regulated by cytokines and chemokines [23]. Moreover, cytokines such as IFN-γ, TNF-α and IL-1β may promote apoptosis of macrophages and SMCs leading to the enlargement of the necrotic core and the thinning of the fibrous cap [24].
The direct involvement of immune cells in modulating plaque stability has also been evaluated. Adoptive transfer of CD4+ T cells from human plaques into immunodeficient mice engrafted with human atherosclerotic vessels resulted in apoptosis of SMCs in a TNF-related apoptosis-inducing ligand (TRAIL)-dependent manner, inducing fibrous cap thinning and plaque destabilization [25]. Interestingly, Klingenberg et al. [26] showed the considerable increase of Th1 cells in vulnerable plaques and the detrimental effect of Treg depletion on plaque stability in mouse models. This effect could, at least in part, be justified by the reduction in the local level of TGF-β, a cytokine produced by Treg with direct fibrogenic action on SMCs and fibroblasts.
2 A Lesson from Anti-atherosclerotic Drugs
2.1 Statins
Since their introduction, more than 25 years ago, as the first line therapeutic for lipid lowering, statins are a proven class of drugs for effective prevention of CVDs but with benefits beyond those predicted solely by their actions in reducing plasma LDL cholesterol [27].
Indeed, statins have an undefined pleiotropic anti-inflammatory action and are able to reduce plaque formation in hypercholesterolemic mice, without affecting lipid levels [28]. Recently, by injecting simvastatin-loaded reconstituted high-density lipoprotein nanoparticles in apoE−/− mice, Duivenvoorden et al. [29] revealed a selective uptake into the vessel wall with associated local anti-inflammatory activity, sufficient to inhibit plaque progression without any systemic effect on lipid concentrations.
Statins are inhibitors of 3-hydroxy 3-methyl glutaryl coenzyme A (HMG-CoA) reductase and therefore of the synthesis of cholesterol, resulting in reduction of circulating LDL levels. Interestingly, as part of their mechanism of action, statins inhibit biosynthetic intermediates of cholesterol synthesis and their precursors such as geranyl-geranylpyrophosphate (GGPP) [30]. GGPP is a lipidic attachment for Rho-GTPase and its inhibition reduces Rho-GTPase related activity. This is one of the mechanisms that can explain the pleiotropic effect of statins [27, 30]. In fact, the production of nitric oxide (NO) by the endothelium via nitric oxide synthase (eNOS) regulates the homeostasis of the vessel. Indeed, atherosclerotic lesions develop faster and grow larger in hypertensive eNOS/apoE double knockout mice when compared to control apoE−/− mice [31]. Statins stimulate NO production by ECs via eNOS. Indeed, pravastatin and simvastatin induce vasorelaxation in mouse aortic rings and NO production by cultured bovine aortic ECs [32]. The direct inhibition of RhoA or GGPP leads to increased expression of eNOS, suggesting that the effect of statins on eNOS is cholesterol-lowering independent [27]. Laufs et al. [33] reported that statins increased eNOS mRNA half-life in ECs. Finally, Scalia et al. [34] demonstrated that an acute treatment with simvastatin in apoE−/− mice is able to increase NO production in the aorta via eNOS, without the reduction of circulating cholesterol levels.
Statins also exert canonical anti-inflammatory effects. Simvastatin showed anti-inflammatory activity, similar to that of indomethacin, in a model of acute inflammation in normocholesterolemic mice, the carrageenan paw oedema [28]. The potent anti-inflammatory activity of statins is only partially explained by their action on NO production by the endothelial layer. Reduction in the transendothelial migration of leukocytes to inflammatory sites is one of the most coherent effects of statins. Atorvastatin, simvastatin and cerivastatin inhibit the expression of adhesion molecules on human ECs and peripheral blood mononuclear cells, reducing binding to ECs in vitro [35]. Statins reduce the production of chemokine CCL-2 in vitro in human ECs exposed to IL-1 and in vivo in a mouse model of air-pouch [36]. Statins also reduce in vitro CCL-2-induced migration of a human continuous monocyte/macrophages cell line (THP-1) and the secretion of MMP-9 [37], a metalloprotease important for the migration/invasion of leukocytes. Taken together, these data suggest that statins reduce the transendothelial migration by reducing adhesion molecule expression, recruitment signals, migration to and entry into the subendothelial space.
In addition to suppressing cell infiltration into sites of injury, statins also exert direct effects on immune cells. Activation of T cells is mediated by the interaction with MHC-II and costimulatory molecules. Kwak et al. [38] demonstrated that statins inhibit MHC-II-mediated T cell activation. Statins are able to inhibit the expression of CD40 in human ECs, SMCs, macrophages and fibroblasts affecting NOS and peroxisome proliferator-activated receptor (PPAR) signalling pathways [39]. Moreover, treatment of LPS-stimulated human monocyte-derived DCs from healthy patients with simvastatin and atorvastatin reduced the expression of CD83, CD86 and human leukocyte antigen-DR. Statins also reduced the production of IL-6, IL-8, IL-12, and TNF-α by DCs and suppressed their ability to induce T cell proliferation, activation and Th1 differentiation [40]. Statins have pronounced effects on T cell activation and proliferation through modulation of the Rho-GTPase pathway [41], and atorvastatin in particular has been shown to promote differentiation of T cells into a Th2 subtype with concomitant suppression of the secretion of Th1 cytokines [42]. Finally, lovastatin increases Treg cell recruitment into inflamed sites in a chemokine (C-C motif) ligand 1 (CCL1)-dependent manner. This effect, is in fact, abrogated in CCL1-deficient mice [43].
The atheroprotective effect of statins is exerted not only by reducing plaque development but also stabilizing vulnerable plaques. Atorvastatin inhibits the development of an unstable plaque phenotype in hypercholesterolemic mice, lowering the level of chemokines and chemokine receptors [44]. Intriguingly, rosuvastatin reduces nuclear factor (NF)-κB activation induced by CD40L in human aortic SMCs thus regulating plaque ECM production [45]. Rosuvastatin also reduces the expression of MMP-9 by macrophages [37], a metalloproteinase able to induce acute plaque disruption in apoE−/− mice [46].
Main pleiotropic targets of statins are listed in Table 1.
2.2 PCSK9 Inhibitors
PCSK9 is an enzyme ubiquitously expressed by many cell types. PCSK9 binds the LDL receptor (LDLr), which is primarily expressed in the liver and is a signal for inducing the degradation of the receptor such that is no longer recycled back to the cell membrane surface [47]. Consequently, increased levels of PCSK9 can inhibit LDLr expression on hepatocyte cell membranes and therefore increase LDL levels in the bloodstream. Chang et al. [48] reported for the first time the possibility to neutralize the PCSK9 using a monoclonal antibody, termed mAb1, in mouse and non-human primates (Fig. 2). Interestingly, they demonstrated that a single subcutaneous injection in cynomolgus monkeys of the neutralizing antibody led to rapid and significant LDL lowering, 8 h after injection, reaching a maximum of 80% below pre-dose levels by day 10.
Proprotein convertase subtilisin/kexin type 9 serine protease (PCSK9) regulates LDL receptor degradation. (A) During hypercholesterolemia, the circulating levels of PCSK9 increase and are free to bind LDLr on the hepatocyte surface. The PCSK9-LDLr complex is a signal for degradation via lysosome. (B) Binding of circulating PCSK9 by specific monoclonal antibodies results in recirculation of the LDLr and accelerated clearance of circulating LDL
In 2015, two PCSK9 inhibitors: the monoclonal antibodies alirocumab and evolocumab, have been approved by FDA and subsequently by EMA for lowering circulating LDL levels. They are used as a second line treatment for atherosclerotic patients who are resistant to statins or affected by familial hypercholesterolemia. Across all clinical trials performed, the use of alirocumab and evolocumab in association with the prescribed statin regimen, reduced the level of LDL (<70 mg/dL) in 90% and 82% of patients respectively [47].
In early 2017, results from the Further Cardiovascular Outcomes Research with PCSK9 Inhibition in Subjects with Elevated Risk (FOURIER) study have been revealed. The study analysed 27,564 patients with CVD and who were receiving a moderate- to high-intensity statin regimen with a LDL cholesterol level between 70 and 100 mg/dL. Researchers randomly assigned patients (1:1) to receive, in association with the canonical statin treatment, a subcutaneous injection of evolocumab or placebo . Relative to placebo, the circulating LDL level reduced by 59%, from a median baseline value of 92 mg/dl to 30 mg/dl. After 2 years of observation, the group treated with the anti-PCSK9 therapy showed a statistically significant 27% and 21% reduction in heart attack and stroke respectively when compared with placebo [49].
The efficacy of these inhibitors is now clearly corroborated by clinical trial data, demonstrating the potency of these new agents in greatly reducing circulating cholesterol levels yet the reduction in cardiovascular risk is only partially identified. Interestingly, experimental studies have suggested also a pro-inflammatory role for the PCSK9 protein, promoting atherosclerosis with a LDL-independent mechanism. PCSK9 reduces the expression of LDLr in human macrophages [50] while modulating expression of stress response and inflammatory genes in liver cells, independent of its effects on cholesterol uptake [51], suggesting a direct role for PCSK9 in foam cell formation and inflammation. Cheng et al. [52], correlated PCSK9 serum levels with the size of necrotic core tissue in coronary atherosclerosis evaluated by IVUS-VH imaging on 581 patients, showing that serum PCSK9 linearly correlates with coronary plaque inflammation, independently of serum LDL cholesterol levels and statin usage. To investigate the direct effects of PCSK9 on vascular inflammation, Tang et al. [53] silenced PCSK9 with the lentivirus-mediated PCSK9 shRNA (LV-PCSK9 shRNA) vector in apoE−/− mice. PCSK9 gene interference decreased atherosclerosis formation by directly reducing vascular inflammation and inhibiting the TLR4/NF-κB signalling. Furthermore, the neutralization of PCSK9 in hypercholesterolemic mice using alirocumab decreased monocyte recruitment, leading to a more stable plaque phenotype [54]. Finally, silencing of PCSK9 inhibited in vitro ox-LDL induced human APC maturation and T cell activation [55].
3 Old and New Agents to Target Immune Mechanisms in Atherosclerosis
The establishment that atherosclerosis is a chronic inflammatory disease identifies multiple targets in the molecules sustaining inflammation in the plaque microenvironment. Therefore, known multi-target anti-inflammatory and immunomodulating drugs may find a novel application in the control of atherosclerosis. In parallel, the development of biologics targeting specific components of traditional and emerging immune-inflammatory pathways may greatly enhance selective treatment opportunities.
3.1 Methotrexate
Methotrexate , developed as an antifolate drug for inhibiting cell division in the treatment of cancer, is actually used in the therapy of rheumatoid arthritis although its anti-inflammatory effects are not well characterized. Some of the proposed mechanism of actions are independent from the antifolate activity and include alterations of the cellular redox state, the inhibition of polyamine formation and the increase of extracellular release of the anti-inflammatory adenosine [56]. Treatment with methotrexate downregulated in vitro the expression of pro-inflammatory genes including TNF-α, IL-1β, chemokine (C-X-C motif) ligand 2 (CXCL2) and TLR2 while upregulating the anti-inflammatory TGF-β1 gene in TNF-α-stimulated human ECs [57]. Moreover, methotrexate promotes reverse cholesterol transport, reducing foam cell formation in lipid-loaded THP-1 macrophages [58]. Methotrexate reduces levels of TNF-α and increases the expression of IL-10 in thioglycollate-induced peritoneal exudates in mice [59]. This effect was further confirmed in high-fat diet induced obesity in mice. Methotrexate administration reduced TNF-α, IL-6 and leptin production from the adipose tissue of these mice leading to increased production of anti-inflammatory molecules such as adiponectin and IL-10 [60]. In addition, methotrexate reduces circulating levels of the pro-inflammatory cytokine IL-6 in psoriatic patients [61] and adhesion molecule expression in biopsies of human inflammatory tissue from oral bullous pemphigoid [62]. Finally, methotrexate inhibits antigen-induced T cell proliferation in mice [63].
All these actions support the possibility of using methotrexate in atherosclerosis treatment. Indeed, methotrexate reduces atherosclerotic lesion areas in cholesterol fed rabbits leading to a reduction in plaque macrophage content and the presence of apoptotic cells [57] in addition to reductions of MMP-9 and pro-inflammatory cytokines [64, 65].
A randomised clinical trial: the Cardiovascular Inflammation Reduction Trial (CIRT; https://clinicaltrials.gov/ct2/show/NCT01594333), is actually ongoing. The rationale is the use of low-dose methotrexate to reduce heart attacks, stroke, or death in people with type 2 diabetes, metabolic syndrome and heart attack or multiple coronary occlusions. The primary completion date for CIRT will be the end of 2018.
3.2 The IL-1 Pathway
IL-1 is a major mediator of inflammation and immune diseases [66]. IL-1α and IL-1β bind to the same receptor (IL-1R) and share the same downstream pathway. An endogenous inhibitor of the IL-1 signal is the receptor antagonist (IL-1RA) that serves as decoy receptor. Both IL-1α and IL-1β precursors are activated following enzymatic cleavage [67]. Their different properties are primarily related to the cellular location and to the method of activation. Despite the IL-1β precursor being inactive, the IL-1α precursor is active and functions as alarmin, inducing the expression of other cytokines and chemokines [66]. IL-1α mediates the early phases of sterile inflammation [68]. Alternatively, IL-1β is produced as an inactive precursor and is activated by caspase-1, a process controlled upstream by the NLRP3 inflammasome [66, 67].
The IL-1 pathway is unequivocally involved in atherosclerosis. IL-1 induces adhesion molecule expression in human umbilical vein endothelial cells [69], increasing leukocytes adhesion [70]. Mice deficient in IL-1RA developed foam cell lesions once fed a high fat diet supplemented with cholate. While mice genetically deficient in LDLr overexpressing a murine sIL-1RA showed reduced atherosclerosis formation compared to LDLr−/− control mice [71]. Finally, treatment of apoE−/− mice with human recombinant IL-1RA reduced lesion area [72].
Cholesterol crystals and ox-LDL accumulated in the lesions activate the NLRP3 inflammasome, inducing the secretion of the active form of IL-1β by macrophages in the plaque [73, 74]. On the other side, it has been demonstrated that IL-1α-driven vascular inflammation induced by fatty-acids through mitochondrial uncoupling is independent from IL-1β [75].
The blocking of IL-1β represents an interesting target to treat atherosclerosis inflammation. IL-1β is a potent tissutal pro-inflammatory mediator, inducing local vasodilatation and recruitment of leukocytes [76]. Moreover, during inflammation, IL-1β has been linked to the activation of several T cells subtypes, which suggest IL-1β as a link between the innate and the adaptive immunity [76]. To confirm its role in atherosclerosis, IL-1β deficiency [77] or IL-1β neutralization [78] inhibited atherosclerosis development in apoE−/− mice.
Different strategies have been followed to develop biologics able to inhibit the IL-1 pathway. The anakinra is a recombinant version of the human IL1-RA and is approved for the treatment of rheumatoid arthritis. In 2009, the FDA approved canakinumab , a human monoclonal antibody targeted at interleukin-1β, for the treatment of cryopyrin-associated periodic syndrome, a group of rare and heterogeneous autoinflammatory diseases mediated by IL-1. Currently, canakinumab is used clinically as a second line treatment in rheumatoid diseases and is also approved for TNF receptor associated periodic syndrome and familial Mediterranean fever.
3.3 Canakinumab Anti-inflammatory Thrombosis Outcomes Study (CANTOS)
The CANTOS is a randomised, double-blinded, placebo-controlled trial on secondary prevention in more than 10,000 patients previously affected by myocardial infarction. The enrolled patients, with elevated levels of the inflammatory marker C-reactive protein (CRP), were randomised and treated with canakinumab at three different doses or placebo, as control. About 90% of the enrolled patients had cholesterol levels under control by statins [79]. Canakinumab significantly reduced rate of recurrent cardiovascular events without reducing all-cause mortality.
Despite the modest cardiovascular benefit CANTOS results finally convey to basic and clinical researchers the demonstration of a theory: that immune-inflammatory responses not only represent a pathophysiological mechanism but also a valid target for the development of new and selective therapies in atherosclerosis [80].
4 Vaccination Strategies
Systemic treatment with immunosuppressant drugs may lead to several side effects and cannot be suggested for primary prevention. In this regard, modulation of antigen-specific adaptive immune responses via vaccination strategies may be a preferable approach.
Several potential antigens have been found in the atherosclerotic plaque. They include endogenous LDL , in particular apoB-100, ox-LDL and heat shock protein 65 (HSP65) or exogenous antigens like Chlamydia pneumoniae and periodontal pathogens.
During the 1990s, several publications reported the efficacy of an active immunization against ox-LDL in reducing atherosclerosis severity in rabbits [81, 82]. The better identification of the peptides comprising the protein components of LDL and their modified forms in ox-LDL makes more definitive immunological studies possible.
The immunisation with specific apoB-100 sequences reduced plaque formation by 60% in apoE−/− mice [83]. Scanning the apoB-100 protein aminoacid sequence, Tse et al. [84], identified the portions predicted to bind to the mouse MHC-II molecule I-Ab. Two fragments: ApoB3501–3516 and ApoB978–993 were used to immunise the mice and resulted in reduced atherosclerosis development in apoE−/− mice via increased IL-10 production. Generating T cell hybridomas from human apoB-100 transgenic (huB100(tg)) mice immunised with human apoB-100, Hermansson et al. [85] identified an MHC-II-restricted apoB-100-responding CD4+ T cells hybridoma expressing a T cell receptor variable (V) beta chain, TRBV31. The immunization of hypercholesterolemic mice with a TRBV31-derived peptide reduced atherosclerosis by 65%. Finally, the apoB-100 peptide sequence, named p210, also represents an interesting antigen in vaccine formulations due to its consistent atheroprotective effect [86]. The immunization of mice with p210 is effective in atherosclerosis reduction by the systemic induction of the CD4+IL-10+ [87] and CD4+CD25+FoxP3+ cells [88], suppressing the immune response, with minor effects on the other T cell subtypes [86].
PCSK9 also represents an interesting target for immunisation. As previously described, the injection of a human monoclonal antibody against this enzyme, effectively reduced LDL circulating levels and cardiovascular risk in humans [49]. Active immunisation against this target could achieve similar results with long-term biological effects. Recently the effect of an anti-PCSK9 vaccine , named AT04A, has been evaluated in hypercholesterolemic mice. AT04A was able to induce persistently high antibody levels against PCSK9 with a reduction of LDL. Interestingly, AT04A reduced atherosclerosis formation by 64%, data correlated to the systemic and local reduction in inflammatory markers [89].
5 Conclusions and Perspectives
This chapter highlights the importance of immune-inflammatory mechanisms in the pathogenesis of atherosclerosis and related clinical manifestations. Conventional lipid-lowering treatments exert pleiotropic anti-inflammatory effects and recent results from the CANTOS trial have shown that targeting inflammation may be beneficial in secondary prevention. However, several key questions still need to be addressed before considering widespread use of anti-inflammatory drugs in the prevention and treatment of CVDs.
Atherosclerosis is a life-long pathology, identified mainly as a vascular rather than a systemic immune disorder. As such, it is unlikely that the current generation of biologics will ever be used for primary prevention in atherosclerosis given the high risks associated with chronic systemic immunosuppression. Different immune pathways play may different roles at different stages of the disease development and progression. We may therefore hypothesize that different immunomodulatory options may be required to selectively affect disease onset, progression, and/or plaque stabilization. Finally, the development of better diagnostic tools for the direct evaluation of vascular inflammation is required for better patient stratification and the design of future clinical trials. In summary, treatment of vascular inflammation is still in its infancy, but exciting developments lie ahead this rapidly expanding research field.
References
Welsh P, Grassia G, Botha S, Sattar N, Maffia P (2017) Targeting inflammation to reduce cardiovascular disease risk: a realistic clinical prospect? Br J Pharmacol 174(22):3898–3913
Packard RR, Libby P (2008) Inflammation in atherosclerosis: from vascular biology to biomarker discovery and risk prediction. Clin Chem 54(1):24–38
Nicholls SJ, Ballantyne CM, Barter PJ, Chapman MJ, Erbel RM, Libby P, Raichlen JS, Uno K, Borgman M, Wolski K, Nissen SE (2011) Effect of two intensive statin regimens on progression of coronary disease. N Engl J Med 365(22):2078–2087
Linden F, Domschke G, Erbel C, Akhavanpoor M, Katus HA, Gleissner CA (2014) Inflammatory therapeutic targets in coronary atherosclerosis-from molecular biology to clinical application. Front Physiol 5:455
Cuzzocrea S, Riley DP, Caputi AP, Salvemini D (2001) Antioxidant therapy: a new pharmacological approach in shock, inflammation, and ischemia/reperfusion injury. Pharmacol Rev 53(1):135–159
Touyz RM (2005) Molecular and cellular mechanisms in vascular injury in hypertension: role of angiotensin II. Curr Opin Nephrol Hypertens 14(2):125–131
Han J, Hajjar DP, Febbraio M, Nicholson AC (1997) Native and modified low density lipoproteins increase the functional expression of the macrophage class B scavenger receptor, CD36. J Biol Chem 272(34):21654–21659
Keidar S, Brook GJ, Rosenblat M, Fuhrman B, Dankner G, Aviram M (1992) Involvement of the macrophage low density lipoprotein receptor-binding domains in the uptake of oxidized low-density lipoprotein. Arterioscler Thromb 12(4):484–493
Kleinman Y, Krul ES, Burnes M, Aronson W, Pfleger B, Schonfeld G (1988) Lipolysis of LDL with phospholipase A2 alters the expression of selected apoB-100 epitopes and the interaction of LDL with cells. J Lipid Res 29(6):729–743
Ley K, Miller YI, Hedrick CC (2011) Monocyte and macrophage dynamics during atherogenesis. Arterioscler Thromb Vasc Biol 31(7):1506–1516
Ylitalo R, Oksala O, Yla-Herttuala S, Ylitalo P (1994) Effects of clodronate (dichloromethylene bisphosphonate) on the development of experimental atherosclerosis in rabbits. J Lab Clin Med 123:769–776
Jonasson L, Holm J, Skalli O, Bondjers G, Hansson GK (1986) Regional accumulations of T cells, macrophages, and smooth muscle cells in the human atherosclerotic plaque. Arteriosclerosis 6(2):131–138
Hansson GK, Jonasson L, Holm J, Claesson-Welsh L (1986) Class II MHC antigen expression in the atherosclerotic plaque: smooth muscle cells express HLA-DR, HLA-DQ and the invariant gamma chain. Clin Exp Immunol 64(2):261–268
Lahoute C, Herbin O, Mallat Z, Tedgui A (2011) Adaptive immunity in atherosclerosis: mechanisms and future therapeutic targets. Nat Rev Cardiol 8:348–358
Erbel C, Sato K, Meyer FB, Kopecky SL, Frye RL, Goronzy JJ, Weyand CM (2007) Functional profile of activated dendritic cells in unstable atherosclerotic plaque. Basic Res Cardiol 102:123–132
Galkina E, Ley K (2009) Immune and inflammatory mechanisms of atherosclerosis. Annu Rev Immunol 27:165–197
Robertson AK, Hansson GK (2006) T cells in atherogenesis: for better or for worse? Arterioscler Thromb Vasc Biol 26(11):2421–2432
Hu D, Mohanta SK, Yin C, Peng L, Ma Z, Srikakulapu P, Grassia G, MacRitchie N, Dever G, Gordon P, Burton FL, Ialenti A, Sabir SR, McInnes IB, Brewer JM, Garside P, Weber C, Lehmann T, Teupser D, Habenicht L, Beer M, Grabner R, Maffia P, Weih F, Habenicht AJ (2015) Artery tertiary lymphoid organs control aorta immunity and protect against atherosclerosis via vascular smooth muscle cell lymphotoxin β receptors. Immunity 42(6):1100–1115
Grassia G, MacRitchie N, Platt AM, Brewer JM, Garside P, Maffia P (2013) Plasmacytoid dendritic cells: biomarkers or potential therapeutic targets in atherosclerosis? Pharmacol Ther 137(2):172–182
Grassia G, Maddaluno M, Guglielmotti A, Mangano G, Biondi G, Maffia P, Ialenti A (2009) The anti-inflammatory agent bindarit inhibits neointima formation in both rats and hyperlipidaemic mice. Cardiovasc Res 84(3):485–493
Grassia G, Maddaluno M, Musilli C, De Stefano D, Carnuccio R, Di Lauro MV, Parratt CA, Kennedy S, Di Meglio P, Ianaro A, Maffia P, Parenti A, Ialenti A (2010) The I{kappa}B kinase inhibitor nuclear factor-{kappa}B essential modulator-binding domain peptide for inhibition of injury-induced neointimal formation. Arterioscler Thromb Vasc Biol 30(12):2458–2466
Maddaluno M, Grassia G, Di Lauro MV, Parisi A, Maione F, Cicala C, De Filippis D, Iuvone T, Guglielmotti A, Maffia P, Mascolo N, Ialenti A (2012) Bindarit inhibits human coronary artery smooth muscle cell proliferation, migration and phenotypic switching. PLoS One 7(10):e47464
Khokha R, Murthy A, Weiss A (2013) Metalloproteinases and their natural inhibitors in inflammation and immunity. Nat Rev Immunol 13(9):649–665
Maiuri MC, Grassia G, Platt AM, Carnuccio R, Ialenti A, Maffia P (2013) Macrophage autophagy in atherosclerosis. Mediat Inflamm 2013:584715
Sato K, Niessner A, Kopecky SL, Frye RL, Goronzy JJ, Weyand CM (2006) TRAIL-expressing T cells induce apoptosis of vascular smooth muscle cells in the atherosclerotic plaque. J Exp Med 203(1):239–250
Klingenberg R, Gerdes N, Badeau RM, Gisterå A, Strodthoff D, Ketelhuth DF, Lundberg AM, Rudling M, Nilsson SK, Olivecrona G, Zoller S, Lohmann C, Lüscher TF, Jauhiainen M, Sparwasser T, Hansson GK (2013) Depletion of FOXP3+ regulatory T cells promotes hypercholesterolemia and atherosclerosis. J Clin Invest 123(3):1323–1334
Liao JK, Laufs U (2005) Pleiotropic effects of statins. Annu Rev Pharmacol Toxicol 45:89–118
Sparrow CP, Burton CA, Hernandez M, Mundt S, Hassing H, Patel S, Rosa R, Hermanowski-Vosatka A, Wang PR, Zhang D, Peterson L, Detmers PA, Chao YS, Wright SD (2001) Simvastatin has anti-inflammatory and antiatherosclerotic activities independent of plasma cholesterol lowering. Arterioscler Thromb Vasc Biol 21(1):115–121
Duivenvoorden R, Tang J, Cormode DP, Mieszawska AJ, Izquierdo-Garcia D, Ozcan C, Otten MJ, Zaidi N, Lobatto ME, van Rijs SM, Priem B, Kuan EL, Martel C, Hewing B, Sager H, Nahrendorf M, Randolph GJ, Stroes ES, Fuster V, Fisher EA, Fayad ZA, Mulder WJ (2014) A statin-loaded reconstituted high-density lipoprotein nanoparticle inhibits atherosclerotic plaque inflammation. Nat Commun 5:3065
Cai A, Zhou Y, Li L (2015) Rho-GTPase and Atherosclerosis: Pleiotropic Effects of Statins. J Am Heart Assoc 4(7):pii: e002113
Chen J, Kuhlencordt PJ, Astern J, Gyurko R, Huang PL (2001) Hypertension does not account for the accelerated atherosclerosis and development of aneurysms in male apolipoprotein e/endothelial nitric oxide synthase double knockout mice. Circulation 104(20):2391–2394
Kaesemeyer WH, Caldwell RB, Huang J, Caldwell RW (1999) Pravastatin sodium activates endothelial nitric oxide synthase independent of its cholesterol-lowering actions. J Am Coll Cardiol 33(1):234–241
Laufs U, La Fata V, Plutzky J, Liao JK (1998) Upregulation of endothelial nitric oxide synthase by HMG CoA reductase inhibitors. Circulation 97(12):1129–1135
Scalia R, Gooszen ME, Jones SP, Hoffmeyer M, Rimmer DM 3rd, Trocha SD, Huang PL, Smith MB, Lefer AM, Lefer DJ (2001) Simvastatin exerts both anti-inflammatory and cardioprotective effects in apolipoprotein E-deficient mice. Circulation 103(21):2598–2603
Rezaie-Majd A, Prager GW, Bucek RA, Schernthaner GH, Maca T, Kress HG, Valent P, Binder BR, Minar E, Baghestanian M (2003) Simvastatin reduces the expression of adhesion molecules in circulating monocytes from hypercholesterolemic patients. Arterioscler Thromb Vasc Biol 23(3):397–403
Romano M, Diomede L, Sironi M, Massimiliano L, Sottocorno M, Polentarutti N, Guglielmotti A, Albani D, Bruno A, Fruscella P, Salmona M, Vecchi A, Pinza M, Mantovani A (2000) Inhibition of monocyte chemotactic protein-1 synthesis by statins. Lab Investig 80(7):1095–1100
Wong B, Lumma WC, Smith AM, Sisko JT, Wright SD, Cai TQ (2001) Statins suppress THP-1 cell migration and secretion of matrix metalloproteinase 9 by inhibiting geranylgeranylation. J Leukoc Biol 69(6):959–962
Kwak B, Mulhaupt F, Myit S, Mach F (2000) Statins as a newly recognized type of immunomodulator. Nat Med 6(12):1399–1402
Mulhaupt F, Matter CM, Kwak BR, Pelli G, Veillard NR, Burger F, Graber P, Lüscher TF, Mach F (2003) Statins (HMG-CoA reductase inhibitors) reduce CD40 expression in human vascular cells. Cardiovasc Res 59(3):755–766
Yilmaz A, Reiss C, Weng A, Cicha I, Stumpf C, Steinkasserer A, Daniel WG, Garlichs CD (2006) Differential effects of statins on relevant functions of human monocyte-derived dendritic cells. J Leukoc Biol 79(3):529–538
Ghittoni R, Patrussi L, Pirozzi K, Pellegrini M, Lazzerini PE, Capecchi PL, Pasini FL, Baldari CT (2005) Simvastatin inhibits T-cell activation by selectively impairing the function of Ras superfamily GTPases. FASEB J 19(6):605–607
Youssef S, Stüve O, Patarroyo JC, Ruiz PJ, Radosevich JL, Hur EM, Bravo M, Mitchell DJ, Sobel RA, Steinman L, Zamvil SS (2002) The HMG-CoA reductase inhibitor, atorvastatin, promotes a Th2 bias and reverses paralysis in central nervous system autoimmune disease. Nature 420(6911):78–84
Mira E, León B, Barber DF, Jiménez-Baranda S, Goya I, Almonacid L, Márquez G, Zaballos A, Martínez-A C, Stein JV, Ardavín C, Mañes S (2008) Statins induce regulatory T cell recruitment via a CCL1 dependent pathway. J Immunol 181(5):3524–3534
Nie P, Li D, Hu L, Jin S, Yu Y, Cai Z, Shao Q, Shen J, Yi J, Xiao H, Shen L, He B (2014) Atorvastatin improves plaque stability in ApoE-knockout mice by regulating chemokines and chemokine receptors. PLoS One 9(5):e97009
Wang XL, Zhou YL, Sun W, Li L (2016) Rosuvastatin attenuates CD40L-induced downregulation of extracellular matrix production in human aortic smooth muscle cells via TRAF6-JNK-NF-κB pathway. PLoS One 11(4):e0153919
Gough PJ, Gomez IG, Wille PT, Raines EW (2006) Macrophage expression of active MMP-9 induces acute plaque disruption in apoE-deficient mice. J Clin Invest 116(1):59–69
He NY, Li Q, Wu CY, Ren Z, Gao Y, Pan LH, Wang MM, Wen HY, Jiang ZS, Tang ZH, Liu LS (2017) Lowering serum lipids via PCSK9-targeting drugs: current advances and future perspectives. Acta Pharmacol Sin 38(3):301–311
Chan JC, Piper DE, Cao Q, Liu D, King C, Wang W, Tang J, Liu Q, Higbee J, Xia Z, Di Y, Shetterly S, Arimura Z, Salomonis H, Romanow WG, Thibault ST, Zhang R, Cao P, Yang XP, Yu T, Lu M, Retter MW, Kwon G, Henne K, Pan O, Tsai MM, Fuchslocher B, Yang E, Zhou L, Lee KJ, Daris M, Sheng J, Wang Y, Shen WD, Yeh WC, Emery M, Walker NP, Shan B, Schwarz M, Jackson SM (2009) A proprotein convertase subtilisin/kexin type 9 neutralizing antibody reduces serum cholesterol in mice and nonhuman primates. Proc Natl Acad Sci U S A 106(24):9820–9825
Sabatine MS, Giugliano RP, Keech AC, Honarpour N, Wiviott SD, Murphy SA, Kuder JF, Wang H, Liu T, Wasserman SM, Sever PS, Pedersen TR, FOURIER Steering Committee and Investigators (2017) Evolocumab and clinical outcomes in patients with cardiovascular disease. N Engl J Med 376(18):1713–1722
Ferri N, Tibolla G, Pirillo A, Cipollone F, Mezzetti A, Pacia S, Corsini A, Catapano AL (2012) Proprotein convertase subtilisin kexin type 9 (PCSK9) secreted by cultured smooth muscle cells reduces macrophages LDLR levels. Atherosclerosis 220(2):381–386
Lan H, Pang L, Smith MM, Levitan D, Ding W, Liu L, Shan L, Shah VV, Laverty M, Arreaza G, Zhang Q, Murgolo NJ, Hernandez M, Greene JR, Gustafson EL, Bayne ML, Davis HR, Hedrick JA (2010) Proprotein convertase subtilisin/kexin type 9 (PCSK9) affects gene expression pathways beyond cholesterol metabolism in liver cells. J Cell Physiol 224(1):273–281
Cheng JM, Oemrawsingh RM, Garcia-Garcia HM, Boersma E, van Geuns RJ, Serruys PW, Kardys I, Akkerhuis KM (2016) PCSK9 in relation to coronary plaque inflammation: results of the ATHEROREMO-IVUS study. Atherosclerosis 248:117–122
Tang ZH, Peng J, Ren Z, Yang J, Li TT, Li TH, Wang Z, Wei DH, Liu LS, Zheng XL, Jiang ZS (2017) New role of PCSK9 in atherosclerotic inflammation promotion involving the TLR4/NF-κB pathway. Atherosclerosis 262:113–122
Kühnast S, van der Hoorn JW, Pieterman EJ, van den Hoek AM, Sasiela WJ, Gusarova V, Peyman A, Schäfer HL, Schwahn U, Jukema JW, Princen HM (2014) Alirocumab inhibits atherosclerosis, improves the plaque morphology, and enhances the effects of a statin. J Lipid Res 55(10):2103–2112
Frostegard J, Liu A (2017) PCSK9 plays a novel immunological role in Oxidized LDL-induced dendritic cell maturation and T cell activation from human blood and atherosclerotic plaque. European Heart Journal 38(suppl 1):ehx504.3856
Cronstein BN (2005) Low-dose methotrexate: a mainstay in the treatment of rheumatoid arthritis. Pharmacol Rev 57(2):163–172
Bulgarelli A, Martins Dias AA, Caramelli B, Maranhão RC (2012) Treatment with methotrexate inhibits atherogenesis in cholesterol-fed rabbits. J Cardiovasc Pharmacol 59(4):308–314
Reiss AB, Carsons SE, Anwar K, Rao S, Edelman SD, Zhang H, Fernandez P, Cronstein BN, Chan ES (2008) Atheroprotective effects of methotrexate on reverse cholesterol transport proteins and foam cell transformation in human THP-1 monocyte/macrophages. Arthritis Rheum 58(12):3675–3683
Montesinos MC, Desai A, Cronstein BN (2006) Suppression of inflammation by low-dose methotrexate is mediated by adenosine A2A receptor but not A3 receptor activation in thioglycollate-induced peritonitis. Arthritis Res Ther 8(2):R53
DeOliveira CC, Acedo SC, Gotardo EM, Carvalho Pde O, Rocha T, Pedrazzoli J Jr, Gambero A (2012) Effects of methotrexate on inflammatory alterations induced by obesity: an in vivo and in vitro study. Mol Cell Endocrinol 361(1–2):92–98
Elango T, Dayalan H, Subramanian S, Gnanaraj P, Malligarjunan H (2012) Serum interleukin-6 levels in response to methotrexate treatment in psoriatic patients. Clin Chim Acta 413(19–20):1652–1656
Dahlman-Ghozlan K, Ortonne JP, Heilborn JD, Stephansson E (2004) Altered tissue expression pattern of cell adhesion molecules, ICAM-1, E-selectin and VCAM-1, in bullous pemphigoid during methotrexate therapy. Exp Dermatol 13(2):65–69
Yamaki K, Uchida H, Harada Y, Li X, Yanagisawa R, Takano H, Hayashi H, Taneda S, Mori Y, Yoshino S (2003) Effect of methotrexate on Th1 and Th2 immune responses in mice. J Pharm Pharmacol 55(12):1661–1666
Bulgarelli A, Leite AC Jr, Dias AA, Maranhão RC (2013) Anti-atherogenic effects of methotrexate carried by a lipid nanoemulsion that binds to LDL receptors in cholesterol-fed rabbits. Cardiovasc Drugs Ther 27(6):531–539
Leite AC Jr, Solano TV, Tavares ER, Maranhão RC (2015) Use of combined chemotherapy with etoposide and methotrexate, both associated to lipid nanoemulsions for atherosclerosis treatment in cholesterol-fed rabbits. Cardiovasc Drugs Ther 29(1):15–22
Garlanda C, Dinarello CA, Mantovani A (2013) The interleukin-1 family: back to the future. Immunity 39(6):1003–1018
Dinarello CA (2011) Interleukin-1 in the pathogenesis and treatment of inflammatory diseases. Blood 117(14):3720–3732
Hoffman HM, Mueller JL, Broide DH, Wanderer AA, Kolodner RD (2001) Mutation of a new gene encoding a putative pyrin-like protein causes familial cold autoinflammatory syndrome and Muckle-Wells syndrome. Nat Genet 29(3):301–305
Aziz KE, Wakefield D (1996) Modulation of endothelial cell expression of ICAM-1, E-selectin, and VCAM-1 by beta-estradiol, progesterone, and dexamethasone. Cell Immunol 167(1):79–85
Bevilacqua MP, Pober JS, Wheeler ME, Cotran RS (1985) Gimbrone MA Jr. Interleukin-1 activation of vascular endothelium. Effects on procoagulant activity and leukocyte adhesion. Am J Pathol 121(3):394–403
Devlin CM, Kuriakose G, Hirsch E, Tabas I (2002) Genetic alterations of IL-1 receptor antagonist in mice affect plasma cholesterol level and foam cell lesion size. Proc Natl Acad Sci U S A 99(9):6280–6285
Elhage R, Maret A, Pieraggi MT, Thiers JC, Arnal JF, Bayard F (1998) Differential effects of interleukin-1 receptor antagonist and tumor necrosis factor binding protein on fatty-streak formation in apolipoprotein E-deficient mice. Circulation 97(3):242–244
Duewell P, Kono H, Rayner KJ, Sirois CM, Vladimer G, Bauernfeind FG, Abela GS, Franchi L, Nuñez G, Schnurr M, Espevik T, Lien E, Fitzgerald KA, Rock KL, Moore KJ, Wright SD, Hornung V, Latz E (2010) NLRP3 inflammasomes are required for atherogenesis and activated by cholesterol crystals. Nature 464(7293):1357–1361
Rajamäki K, Lappalainen J, Oörni K, Välimäki E, Matikainen S, Kovanen PT, Eklund KK (2010) Cholesterol crystals activate the NLRP3 inflammasome in human macrophages: a novel link between cholesterol metabolism and inflammation. PLoS One 5(7):e11765
Freigang S, Ampenberger F, Weiss A, Kanneganti TD, Iwakura Y, Hersberger M, Kopf M (2013) Fatty acid-induced mitochondrial uncoupling elicits inflammasome-independent IL-1α and sterile vascular inflammation in atherosclerosis. Nat Immunol 14(10):1045–1053
Schett G, Dayer JM, Manger B (2016) Interleukin-1 function and role in rheumatic disease. Nat Rev Rheumatol 12(1):14–24
Kirii H, Niwa T, Yamada Y, Wada H, Saito K, Iwakura Y, Asano M, Moriwaki H, Seishima M (2003) Lack of interleukin-1beta decreases the severity of atherosclerosis in ApoE-deficient mice. Arterioscler Thromb Vasc Biol 23(4):656–660
Bhaskar V, Yin J, Mirza AM, Phan D, Vanegas S, Issafras H, Michelson K, Hunter JJ, Kantak SS (2011) Monoclonal antibodies targeting IL-1 beta reduce biomarkers of atherosclerosis in vitro and inhibit atherosclerotic plaque formation in apolipoprotein E-deficient mice. Atherosclerosis 216(2):313–320
Ridker PM, Everett BM, Thuren T, MacFadyen JG, Chang WH, Ballantyne C, Fonseca F, Nicolau J, Koenig W, Anker SD, Kastelein JJP, Cornel JH, Pais P, Pella D, Genest J, Cifkova R, Lorenzatti A, Forster T, Kobalava Z, Vida-Simiti L, Flather M, Shimokawa H, Ogawa H, Dellborg M, Rossi PRF, Troquay RPT, Libby P, Glynn RJ, CANTOS Trial Group (2017) Antiinflammatory therapy with canakinumab for atherosclerotic disease. N Engl J Med 377(12):1119–1131
Hansson GK (2017) Inflammation and atherosclerosis: the end of a controversy. Circulation 136(20):1875–1877
Ameli S, Hultgårdh-Nilsson A, Regnström J, Calara F, Yano J, Cercek B, Shah PK, Nilsson J (1996) Effect of immunization with homologous LDL and oxidized LDL on early atherosclerosis in hypercholesterolemic rabbits. Arterioscler Thromb Vasc Biol 16(8):1074–1079
Palinski W, Miller E, Witztum JL (1995) Immunization of low density lipoprotein (LDL) receptor-deficient rabbits with homologous malondialdehyde-modified LDL reduces atherogenesis. Proc Natl Acad Sci U S A 92(3):821–825
Fredrikson GN, Söderberg I, Lindholm M, Dimayuga P, Chyu KY, Shah PK, Nilsson J (2003) Inhibition of atherosclerosis in apoE-null mice by immunization with apoB-100 peptide sequences. Arterioscler Thromb Vasc Biol 23(5):879–884
Tse K, Gonen A, Sidney J, Ouyang H, Witztum JL, Sette A, Tse H, Ley K (2013) Atheroprotective vaccination with MHC-II restricted peptides from ApoB-100. Front Immunol 4:493
Hermansson A, Ketelhuth DF, Strodthoff D, Wurm M, Hansson EM, Nicoletti A, Paulsson-Berne G, Hansson GK (2010) Inhibition of T cell response to native low-density lipoprotein reduces atherosclerosis. J Exp Med 207(5):1081–1093
Chyu K-Y, Dimayuga PC, Shah PK (2017) Vaccine against arteriosclerosis: an update. Therapeutic Advances in Vaccines 5(2):39–47
Klingenberg R, Lebens M, Hermansson A, Fredrikson GN, Strodthoff D, Rudling M, Ketelhuth DF, Gerdes N, Holmgren J, Nilsson J, Hansson GK (2010) Intranasal immunization with an apolipoprotein B-100 fusion protein induces antigen-specific regulatory T cells and reduces atherosclerosis. Arterioscler Thromb Vasc Biol 30(5):946–952
Wigren M, Kolbus D, Dunér P, Ljungcrantz I, Söderberg I, Björkbacka H, Fredrikson GN, Nilsson J (2011) Evidence for a role of regulatory T cells in mediating the atheroprotective effect of apolipoprotein B peptide vaccine. J Intern Med 269(5):546–556
Landlinger C, Pouwer MG, Juno C, van der Hoorn JWA, Pieterman EJ, Jukema JW, Staffler G, Princen HMG, Galabova G (2017) The AT04A vaccine against proprotein convertase subtilisin/kexin type 9 reduces total cholesterol, vascular inflammation, and atherosclerosis in APOE*3Leiden.CETP mice. Eur Heart J 38(32):2499–2507
Acknowledgements
Our work was funded by the British Heart Foundation grants PG/12/81/29897 and RE/13/5/30177; the European Commission Marie Skłodowska-Curie Individual Fellowships 661,369; the Engineering and Physical Sciences Research Council (EPSRC) grant EP/L014165/1; and the Tenovus Scotland PROJECT S15/24.
Author information
Authors and Affiliations
Corresponding authors
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Grassia, G., MacRitchie, N., Maffia, P. (2018). Immune Mechanisms in Atherosclerosis and Potential for Immunomodulatory Therapies. In: Riccardi, C., Levi-Schaffer, F., Tiligada, E. (eds) Immunopharmacology and Inflammation. Springer, Cham. https://doi.org/10.1007/978-3-319-77658-3_9
Download citation
DOI: https://doi.org/10.1007/978-3-319-77658-3_9
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-77657-6
Online ISBN: 978-3-319-77658-3
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)