Abstract
Ethics committees routinely require anonymisation of data based on the reasoning that masking all potentially identifiable details of participants determines ethical conduct. In this chapter I argue that the potential social benefit of research should instead be considered key to determining ethical conduct. I reflect on gaining ethics approval for my study of obstetric violence in South Africa and draw on research into public goods to demonstrate that social benefits of research are given limited attention during ethics review. I outline how public interest research may be especially restricted by bureaucratic barriers, conflicts of interest, and required anonymisation of data. I conclude that current ethics clearance models often restrict the potential social benefit of research and I show how such restrictions inevitably produce “powerless datasets”.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Last week I had a meeting with the entire night nurse staff…because the Maternity Obstetric Unit wasn’t taking some patients. In one week, we had three cases of stillbirth. That’s why we had to meet. [Secondary hospital] alerted me. …We don’t have accountability in the system. This has been happening all along. The CEO [Chief Executive Officer] didn’t meet with the Unit for the first five years on the job. That meeting you attended, that was the first meeting [the CEO] ever had about maternity things. …She’s [Unit Manager] also not monitoring. If you don’t pick it up personally, you won’t find out. Dr. Tlou Lekgoathi, Senior Family Physician, Public Day Hospital, Cape MetroFootnote 1
Scholarship widely acknowledges that violence against women and gender -based violence in South Africa have reached epidemic proportions (Coovadia, Jewkes, Barron, Sanders, & McIntyre, 2009; Gqola, 2015; Moffett, 2006). Recently, the range of adverse treatment pregnant women receive when seeking healthcare and particularly in maternity wards during childbirth has been labeled as violent (Chadwick, 2017; Jewkes & Penn-Kekana, 2015; Pickles, 2015). This includes slapping, sexual assault, humiliation, the denial of health services, coercive medical procedures that are either unnecessary and/or performed without consent including long-acting and permanent contraception (e.g., sterilisation), refusal of pain medication, denial of admission to health facilities, and the detention of women and newborns after childbirth for lack of payment (World Health Organisation, 2015). This ubiquitous problem has been described as ‘obstetric violence ’ and has become punishable by law in some countries (D’Gregorio, 2010). While this problem is found in both public and private health systems, my research focused on the public sector which is directly managed by public servants.
The excerpt above, from an interview for my doctoral research, shows an example of the systemically poor management that is adversely impacting on public services, and on pregnant women and their families . This narrative shows how the poor performance of health managers can create patterns of risk for those seeking maternal healthcare. To contextualise the urgency of the public health system ’s problems of oversight, it is useful to reflect on the task fulfilled by Maternity Obstetric Units (MOU) in the Cape Town Metro. Everyday, between four and eight women deliver in a primary care MOU. In other words, the creation of new life for six to eight families per day depends on care from these Units. Addressing patterns of violence and inadequate accountability where and when they occur to pregnant women is, thus, urgent, not only for the pregnant woman and her foetus or newborn but also for her and her partner’s families, and the communities from which they come.
Ensuring social benefit is especially important when research concerns public goods, for example, health system functioning or corruption in schools because such data and analysis is able to directly contribute to social benefit. Developing systems to monitor public goods is important for any polity and especially for states going through societal transition in which there is an attempt to replace former structures of inequity.
South Africa provides an example of such transition, as it has been shifting from centuries of colonial and apartheid regimes based on White-supremacist rule to a majoritarian democracy since 1994. During the early period of this political shift, the Truth and Reconciliation Commission ’s (TRC) investigation found health services to be a perpetrator and enabler of mass violence (TRC, 2003, p. 31). Recent research has suggested that Black pregnant women continue to face violence from the public health system (Farrell & Pattison, 2004; Kruger & Schoombee, 2010; Essack & Strode, 2012; Chadwick, 2017).Footnote 2 My research investigates why and how obstetric violence is caused and spread in South Africa’s public health system. By applying qualitative methods and a historical approach, I examine the socio-political drivers of this violence and what sustains abuses of power by public servants (health professionals, administrators, and policymakers) who are responsible for providing health services in the public interest. The majority of participants in my study are public servants, and includes those with limited visibility and power, for instance, Nurses and those with significant visibility and power, for instance, Chief Directors.
It is commonly argued that, given the potentially vulnerable position of participants, and the sensitivity of a research topic and its locations, conforming to informed consent , confidentiality , and anonymity requirements is essential (Garrard & Dawson, 2005). In addition, academic research in the social sciences is increasingly controlled by processes of ethics review which aim to certify compliance to these and other required methods (Haggerty, 2004). Certain of these requirements, however, can impose limitations on obtaining and using data, especially on topics of public interest. In this chapter I question the potential for the social benefit of academic research to be limited by bureaucratic barriers, conflicts of interest, and requirements of the blanket anonymisation of data.
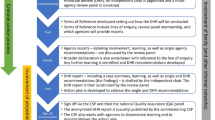
This chapter primarily draws on the regulation of my research by Ethics Committees , EC and the ways in which this has limited the contribution to social benefit that my dataset can make.Footnote 3 Firstly, my experience of gaining ethical approval illustrates the regulation of research through the imposition of bureaucratic barriers which have the overt objective of preventing unethical academic conduct. Secondly, institutions may have to negotiate several interests in fulfilling the responsibility of reviewing applications for ethical clearance. I highlight the potential for conflicts of interest in the Ethics Review model and how this may inhibit the potential for social benefit from research. Thirdly, ECs routinely require the methodological strategy of anonymisation for research involving people. By considering research concerning a public good, I analyse how anonymisation strategies necessitating the suppression of socially valuable information can produce what I call ‘powerless datasets’. In this way, the chapter questions the underlining reasoning of regulatory bodies who consider that informed consent and anonymity of research locations and participants is the best method of achieving utmost ethical conduct. To conclude, I raise several approaches to remedy these problems.
Background to This Public Interest Research
The presence of violence in maternity health services is not unique to South Africa. Pregnant women who are discriminated against because of their race , economic, and/or disease statuses, among other characteristics, are commonly subject to obstetric violence throughout the world (see Bowser & Hill, 2010; Pires, d’Oliveira, Diniz, & Schraiber, 2002 for literature reviews on this problem).
My research in South Africa has shown that the poor accountability and answerability, referred to in this chapter’s initial quote, enables obstetric violence . By way of example, in early 2010 a series of meetings to discuss obstetric violence was convened by a medical school professor with hospital CEOs and senior midwives from primary to tertiary levels of care. The result of these meetings was that ‘reports of abuse [by medical students] were reduced’.Footnote 4 However, the professor reported that by November of the same year, ‘every one of the twenty-four students… interviewed’ who had interned in maternity wards throughout the Cape Metro ‘reported a range of very distressing abuses committed against patients in labour’.Footnote 5 As a result, similar meetings were initiated over the following two years, which then included Directors of the Provincial Department of Health .Footnote 6 A year later, a senior physician described an example of how the absence of internal answerability sustains obstetric violence.
Two months ago there was a nurse who pulled a pregnant woman by the ear from the floor. I think she might have fallen because of pains…, she cried out to the nurse for help. The nurse went there already annoyed and pulled her by the ear… Do you know they delivered with the woman on the floor? They [nurses] made her deliver on the floor… I think she was a foreigner. …It was criminal. …They [medical students] took it up the channels but I won’t be surprised if it won’t just die. When I had to pull out the files I realised that they [midwives] didn’t even report that she gave birth on the floor. … I never see the results [of reports], that’s my issue with it. In the end there is no accountability .Footnote 7
As of 2017, medical students in Cape Town continue to report observingobstetric violence , especially in the form of ‘psychological and verbal abuse [which] is routine’, including the victimisation of especially discriminated against groups, for example, ‘HIV positive mothers’.Footnote 8 This summary of my findings demonstrates how, in the absence of functioning internal and external systems of accountability , major consultations, for example, those initiated by the Professor, are not sufficient to ensure the Provincial Department’s stated ‘zero tolerance’ for obstetric violence (Honikman, Fawcus, & Meintjes, 2015). My study demonstrates that the recent policy designed to curb obstetric violence in South Africa, referred to in Honikman et al. (2015) has been poorly developed and implemented. Moreover, the potential social value of research into obstetric violence, emerging from at least some reporting of major malpractice, appears to be dependent on the willingness of a university to agitate for accountability from administrators. This potential is lost, however, through EC barriers, conflicts of interest, and routine anonymisation, which I discuss in the following section.
The Loss of Social Benefits Due to Bureaucratic Barriers
In this section I analyse the increasing surveillance of research through ECs , specifically the constraints of the potential to design, implement, and apply public interest research. Applying for EC approval is an intensely bureaucratic process. Compounding bureaucratic barriers is that some research requires multiple institutional approvals. Regulators of academic research may represent governmental, non-profit institutions, as well as for-profit companies. For instance, my research required approvals from the University of Leeds (No. AREA 12-013) and the University of Cape Town UCT (No. HREC 290/2013) as well as additional approval from the Western Cape Department of Health (No. RP093/2013) . These approvals allowed me to present my final requests for access to the Chief Executive Officers and clinic managers at the various hospitals in the Cape Town Metro selected for the study. This summary of my multi-institutional ethics review process demonstrates the intense regulation of academic research.
Ethics Committees place little emphasis on evaluating and enabling the social benefit of research. In line with a bureaucratic process, applications entail completing forms which require extensive descriptions of the prospective research topic and methodological design, including questions concerning the safety of research participants. While these requirements result in increased scientific rigour, value, and justification for initiating research, they do not allow for consideration of the broader social contribution of research. For instance, not one question in my review process specifically enquired about the potential social benefit that would result from the research. The closest to this type of question came from my University of Leeds Application form under the heading ‘Risks of the Study’ which focused on the potential benefits and risks to research participants from engaging in the study (University of Leeds Research Ethics Committee Application Form, updated 17 January 2012).
These Ethics Committees ’ lack of enquiry into the broader social implications of research indicates that public interest is not a priority for them in determining sound ethical practice. My experience of ethical review is not unique. Some scholars find the consideration of social impact to be a common limitation of the EC model (Garrard & Dawson, 2005). Rather than assessing the potential social benefit and harm of research, in practice, ECs are primarily concerned with mitigating within a narrow view of individual harm. The Economic and Social Research Council, United Kingdom, for instance, defines harm as ‘substantive harm to participants (and others affected by the proposed research)’ (Economic and Social Research Council, 2016). Haggerty (2004), who is an EC board member at the University of Alberta, Canada, finds that ECs consider potentially harmful research to be that which may cause ‘damage’ to participants’ ‘reputation , finances, or relationships, [or that may] offend’ or subject participants to ‘trauma’ (p. 400).
Rather than agreeing with the EC ’s narrow interpretation that the social responsibility of research is to limit harm to participants, my position is closer to Buchanan’s and Miller’s (2006). They argue that institutions and researchers have a moral responsibility to develop methodological designs aimed to distribute fairly ‘the benefits and burdens’ arising from research across society (Buchanan & Miller, 2006, p. 729). As has been indicated, however, established EC procedures do not prioritise the potential to contribute social value in the public interest. The intensifying regulation of research combined with the lack of consideration for, and interest in, bolstering the social value of research may contribute to altering and/or preventing public interest research as early as the proposal/protocol stage.
Conflicts of Interest
In this section, I raise questions pertaining to conflicts of interest that may arise from applying for, or overseeing an EC process. Conflicts of interest arise when institutions or a person has incompatible interests with more than one party, for example, relationships through employment, consultative, or board membership. As a researcher, I was required to follow the EC processes which requested disclosure of any conflicts of interest. I posit here that there may be a greater chance of conflicts of interest for those overseeing ethics review processes when research proposals require multiple approvals , as described earlier. In addition, research concerning public interest, and studies relating to health systems in which institutions of higher education have a stake in those health systems, may entail greater risks of conflicts of interest.
These proposals, requiring multiple ECs approval which are located in interlocking systems, demand additional reviewers, but it is also likely for these systems to have overlapping interests and members, such as in, my case, those of health and higher education. The academic staff of universities’ health sciences often provide clinical oversight and management of public hospitals. In South Africa, these responsibilities are fulfilled through joint professional posts between universities and a provincial Department of Health. These responsibilities create dual institutional allegiances when academic institutions have vested interests in protecting the health facilities they manage clinically and use as resources for their teaching and for interning students. Moreover, such academic staff, who receive remuneration from both institutions, are likely to teach in public hospitals and regularly may advise government on policy and administrative matters. Such staff often administer and manage academic and health system resources, sometimes overseeing significant aspects of research grants and public health systems .
Conflicts of interest may arise when university health sciences academic staff have a seat on ECs . As was just outlined, these academic staff, their colleagues, and supervisors are commonly formally connected to public health systems . Thus, university departments who determine the initial approval and design of research proposals are likely to have vested interests in the public image of these important sites of research inquiry. Given the interests that follow these formal partnerships and joint responsibilities, determining approval of, for instance, proposals concerned with governance , corruption, management, or routine malpractice of public health resources may cause such conflicts.
Generally, once academic departmental approval is gained, researchers can apply for a necessary nationally accredited EC clearance. In South Africa, this can be obtained either through a university-based EC or an independent for-profitEC (Pharma-Ethics, 2017).Footnote 9 As noted in the previous section, studies involving participation at the facility level of services in South Africa require a secondary layer of official approval from a provincial Department of Health . Importantly, in South Africa, this required clearance is not framed as an ethics approval but rather an official ‘approval for health research ’. Nonetheless, the institution whose services and/or management and governance may be under scrutiny is required to provide further approval of research proposals thereby demonstrating a clear conflict of interest.
Another challenge to public interest research can be to obtain the generally required informed consent of local heads of public and private facilities that are locations of study. These administrators have the discretion to deny access to research studies even when all other approvals have been gained. This occurred in my experience. One of the seven institutions I approached for research declined access to me. Informally I was told my study was denied access out of the Executive’s interest to protect the institution from an examination of such a controversial topic. In another instance, I was afforded partial access, whereby the clinic manager agreed and encouraged the study, but the CEO refused to consider the request for informed consent and did not respond to my repeated inquiries; the clinic manager was told in a meeting that they would not approve the request. After the majority of fieldwork had taken place, this obstacle was overcome as a result of changes in management. Lastly, an acknowledged conflict of interest, similar to those discussed earlier, resulted in limiting my access to two of the remaining five facilities I had gained full approval to study.
My study of the governance and management of reproductive healthcare clearly tested the boundaries of conflict of interest. Although my critical protocol did achieve necessary approvals to conduct the research in the majorityof the hospitals to which I had applied, I suspect this was not a result of the absence of conflict of interest or a genuine openness and commitment to public interest research on the part of my Universities, the Department of Health, or the facilities where I did gain access . Rather, relevant to my gaining and maintaining what one health sciences Professor called ‘unprecedented access’, especially for someone foreign to the health system, was the institutional and political connections I developed and nurtured early on in the application process.Footnote 10 Without the support of key academics and policymakers of influence, my research protocol may have been amended at the stage of applying for academic departmental approval in South Africa. Research that involves issues of public interest such as malpractice and corruption make negotiating conflict of interest more difficult for both researchers and those overseeing ECs .
The Ethical Problems With Anonymising
When academic research involves people as participants, the study design is generally required to include the methodological strategy of blanket anonymity . Anonymisation is understood as ‘not disclosing the identity of a research participant, or the author of a particular view or opinion’ (Clark, 2006, p. 4) with a view to reducing potential harm .
In this section, I argue that requiring anonymisation to reduce harm equates to constraining the intended, and unintended, benefits of research. I question the reasoning underlying the consensus of regulatory bodies that blanket anonymity equates with ethical conduct. I ask whether, in fact, lack of public transparency —particularly when research concerns public goods—enables the least risk of harm when this is applied more broadly than to individual participants.
Instead of a singular interest in protecting individual participants and research locations from stigma or personal harms , I posit another foundation that may be involved in the current regulatory consensus to anonymise, thereby gaining access to research sites. Requiring researchers automatically to apply a methodological strategy of anonymisation involves a trade-off: on the one hand, to obtain access to locations and participants of interest, and, on the other hand, the ability of researchers to produce the greatest social benefits from their research. In order to facilitate the former, the latter is forfeited or it is greatly reduced. Through an analysis of two studies that have produced ‘less-powerful’ evidence of obstetric violence (my own, and a Human Sciences Research Council, HSRC study (Cloete, Simbayi, Zuma, Jooste, & Wabiri, 2015), I argue that this requirement can threaten the power of academic research to best contribute to public interest. In other words, requiring blanket anonymity can render a dataset powerless. While the initial EC regulating my application did not foreclose the proposal of an ethical strategy of disclosure of biographical participant and site details, this approach is legally restricted in the United Kingdom where the standard of anonymisation of captured data is routine.Footnote 11 Therefore, this ethical clearance (as well as the additional approvals I was later required to obtain) meant that my research design significantly encouraged my ‘complicity’ in incorporating ‘blanket anonymisation’ (Clark, 2006, p. 5). Methodologically for my study, this included anonymising research locations and ensuring confidentiality for all informants. Although confidentiality and anonymisation are different, their processes are connected in that confidentiality entails ‘not disclosing to other parties opinions or information gathered in the research process’ (Clark, 2006, p. 4). My experience corroborates findings that the EC model has expanded, and through this expansion provides little exception for the disclosure of participants’ identities and research locations (Clark, 2006; Haggerty, 2004).
By providing important evidence, academic research has the potential to contribute to the public interest of addressing gender -based violence , which, as was noted earlier, is understood to have an epidemic scope in South Africa (Coovadia et al., 2009; Gqola, 2015; Moffett, 2006). The routine application of anonymity strategies may cause datasets with evidence of violence to be powerless with regard to specific evidence in the public’s interest. For example, a nationwide ‘Stigma Index Survey’ conducted by the Human Sciences Research Council of South Africa (HSRC) revealed evidence of the forced sterilisation of women. The 2014 HSRC study assessed experiences of the stigma of people living with HIV . The study found that 498, that is 7.4% of respondents, ‘reported forced sterilization’, among other coercive reproductive health practices by the public health system (Cloete et al., 2015, p. 16). The HSRC could not, however, follow up on these serious findings. Professor Khangelani Zuma, Co-Principal investigator for the study, explained to the public the powerlessness of the research team when journalists pressed the issue: ‘all respondents to the survey were anonymous and cannot be traced, so action could not be taken against the Department of Health or hospitals at which sterilisations took place’ (Child, 2015, June 12, Non paginated). The Department of Health spokesperson, Popo Maja, stated similarly, ‘[i]t is extremely difficult to investigate the four hundred and ninety-eight cases because the survey was anonymous’ (Child, 2015, June 12, Non paginated). In this case the EC requirement of anonymising the research locations and participants deprived a nationally commissioned survey of the information necessary to act on a significant finding of egregious obstetric violence . This example bolsters Haggerty’s (2004) argument that academic research, which is constrained by agreements of anonymity, unlike journalistic investigations, can become void of ‘political weight’ and ‘critical’ contributions (p. 409).
Clark (2006) rightly asserts that the manner in which anonymisation is applied influences the degree of limitation for the data to be utilised for the public good. Characteristics often deemed relevant only for the background context may in fact be ‘crucial for analysis’ (Clark, 2006, p. 6). For example, the HSRC survey anonymised the names of hospitals and clinics but not of gender . After their results were made public, it became clear that both markers (hospital and clinic names) were critical for analysis, further research, and the dissemination to relevant institutions obliged to ensure the protection of those seeking healthcare services .
Similar to the weaknesses of the HSRC survey, the requirement of anonymisation for my study resulted in an inability to name the hospitals and professionals perpetrating direct obstetric violence, thereby allowing for the evasion of accountability . I have been unable to document and use specific information for a range of problems relating to obstetric violence and accountability, including routine neglect of services in terms of stock-outs of goods and equipment (e.g., the long-term, of over two years, stock outs of essential sterile equipment); several accusations and observations of likely corruption; numerous accounts of dysfunctional accountability mechanisms including sub-district Directors seemingly not following up on several reports of obstetric violence, including reports leading to foetal/neonatal mortalities; the disclosure of facilities where forms of direct obstetric violence have been observed routinely; and of public servants who have been identified by respondents to have repeatedly abused women during childbirth in primary and secondary facilities. A few examples of the forms of obstetric violence I am unable to report on with specifying information include: routine denial of pain medication during active labour; the administration of progesterone-only Depo-Provera contraceptives with lack of informed consent , and at times coercively;Footnote 12 egregious abuse of women during childbirth (e.g., unnecessary, and un-anesthetised episiotomies,Footnote 13 and those administered without sterile surgical sutures;Footnote 14 unnecessary repeated manual vaginal dilation during the second phase of labour, reported as ‘almost like sexually assaulting the patient’).Footnote 15 These practices during childbirth cause additional pain, restrict the power of women, and contribute to risks of maternal and neonatal health . Had blanket anonymity not been required, my study may have offered considerable data about where obstetric violence is taking place. Additionally, it could report to the various regulatory authorities about multiple levels of management responsible for the failure of oversight which, relates to the perpetuation of this particular for of gender-based violence.
Conclusion and Suggestions
This chapter concerns the limitations posed by Ethics Committees ’ narrow interpretation of ethical conduct. Ethics Review regulations reason that by suppressing or restricting the specific details of a study, the protection of participants and the achievement of the greatest ethical conduct is achieved. To question this thinking, and especially the lack of attention to the social value of research, I have drawn on the regulation of my research into the functioning of a public good, that is South Africa’s public health system .
The chapter draws on my experience of applying for, and gaining, the multi-institutional ethics and official approvals required for my study. I found the potential for research to contribute social value in the public interest is not a priority of the Ethics Review model. This, coupled with the expansion of bureaucratic barriers imposed by EC requirements, may contribute to altering the methodological design, and/or preventing public interest research as early as the protocol/proposal stage. Moreover, I found that when research concerns certain public goods, there may be significant opportunities for conflicting interests throughout the review process. I argued that this can lead to avoidable and/or biased decisions which can impact on the social benefits of research. Specifically, I highlighted that in health sciences, academics often have joint posts with public health systems and that this may raise incompatible interests both for members of ECs and within academic institutions. Importantly, while conflict of interests were found during the implementation of my study, my experience illustrates, at times these can be negotiated productively by researchers: by repeatedly providing strong evidence-based justifications for their research, taking an active role in their engagement with EC authorities, and revisiting access to sites that were initially made inaccessible by approvals.
Through an analysis of two studies that found evidence of obstetric violence , I argue that the standard Ethics Review requirement of anonymising identifying characteristics of participants and locations can weaken the contribution of academic research by producing what I call ‘powerless datasets’. I found that research can be made powerless through two processes. Firstly, conflicts of interest may limit the scope and intended benefit of a research project by constraining research design, for example, when authorities of a site of research refuse to consider applications for access . Secondly, required anonymity can constrain both intended, and unintended, research outcomes. By constraint, I mean the limiting of a dataset’s usefulness to further investigations, and an inability to report specific evidence to vested authorities, for example, to institutions who are legally bound to respond to corruption or violence against women.
Through this analysis I problematise the underlining reasoning that blanket anonymity equates to the strongest approach to ethical conduct. I conclude that perhaps the expansion of the Ethics Review model, and its routine anonymisation requirement, translates to a trade-off, thereby gaining access to locations and participants of interest through the forfeiture of greatest social benefit . And in this way there is often a minimised role academic research can have in the oversight of public goods. I argue this is a weakness as for example, while there are several regulatory bodies vested with the power to scrutinise South Africa’s health system, they have been ineffective. This is clear from the consensus that the system is in crisis due to poor governance and oversight (National Planning Commission, 2011; TAC, 19 February, 2015). I argue that academic research can play a critical role if given the chance by institutions and regulatory bodies to prioritise the public interest of research. This is particularly important in contexts, such as South Africa’s, where corruption, poor management capacity, and violence are endemic, for instance, in public institutions (von Hodlt & Webster, 2005). If research investments continue to produce powerless datasets, social benefits will continue to be weakened. Instead academic research needs to be acknowledged and used as the major public asset that it is.
While I am critical of the narrow form and application of the Ethics Review model, it is important to mention the reasons that I am grateful for its expansion to the social sciences and its global influence. Firstly, universities possess the power of enforcement to ensure the disclosure and ethical regulation of research. Additionally, the requirement of an Ethics Review process ensures a platform for all researchers to consider the ethical aspects and consequences of the social value of their work. Importantly, the imposition of a regulatory necessity presents an opportunity for the broad consideration of which approaches to ethical conduct best ensure the most commonly held benefit leading to the least individual and social harm . Academic research has brought about considerable critiques of its unethical conduct. This has established a plurality of operational models to which academic institutions and researchers adhere (for instance, see Smith Tuhiwai, 2012). It is telling that the institutionalisation of this variety of epistemic models has been developed by Indigenous and African peoples who have been subject to notoriously unethical research. This shows that the current globalising Ethics Review model, based on Eurocentric bureaucratic regulatory codes, has been found inadequate and in several cases has been replaced.
Given these findings, I recommend the following be considered to address the constraints raised by the current Ethics Review model. Firstly, further evaluation of the performance of the model in relation to intended and unintended outcomes of social benefit is needed. Secondly, the investigation of potential conflict of interest at the differing levels of ethics and officially required clearance should be instituted with each application.
I recommend that these steps are taken by universities and their communities to give broad consideration to which epistemic , cultural , and operational model is best suited to ensure the greatest ethical conduct in their locality. Interestingly, the University of Cape Town has taken steps towards such an approach. Their EC includes ‘social value’ as an ‘ethical requirement’ of research (Human Research Ethics Committee, 2013, p. 1). This is described as research ‘…worth doing. It must be relevant to broad health and development needs of South Africa and to the individual needs of those who suffer from the conditions under study. Ideally, the findings should translate into mechanisms for improving the health status of South Africans’ (Human Research Ethics Committee, 2013, p. 1, emphasis added). The plurality of epistemic models to consider ethical conduct provides a rich starting point for any researcher and EC to better enable their work to powerfully contribute the greatest social benefit .
Notes
- 1.
Personal interview, 27 October 2013. All names used for persons informing the study are pseudonyms that retain participants’ ethnicities.
- 2.
Black refers to all of those discriminated against under colonialism and apartheid, namely, South Africans categorised as coloured, Indian, and black African. African is used as an inclusive term referring to the people of South Africa or the continent.
- 3.
For ease of reading, I use ‘Ethics Committee ’ and ‘EC’ to refer to the committees to which I applied for ethical review, which used different names. University of Leeds uses Research Ethics Committee, REC ; the University of Cape Town uses Internal Review Board , IRB, and ethics committee for shorthand.
- 4.
Personal communication, Academic Head of Department, Professor Eleanor Grant to a Chief Director, WC Provincial Department of Health , David Claassen 23 November 2010.
- 5.
Ibid.
- 6.
Archive, Academic Head of Department, Professor Eleanor Grant ‘Aide Memoir of Meeting with [MOU] Staff’ and Hospital Administration 1 July 2011; Meeting Agenda, Attendees Senior Administrative and Professional Directors and Staff, 3 August 2012.
- 7.
Personal interview, Senior Family Physician, Public Day Hospital, Tlou Lekgoathi 27 October 2013.
- 8.
Interview, Academic Head of Department, Professor Eleanor Grant, 3 May 2017.
- 9.
Pharma-Ethics is an independent corporate EC operating in South Africa. It provides reviews of research proposals for fees ranging from 20,200 ZAR (1,500 USD) for clinical trials to 3,000 ZAR (230 USD) for student proposals.
- 10.
Personal communication, Professor Sophie Bunting, Health Sciences, 18 July 2013.
- 11.
In the UK, the Data Protection Act (1998) legally regulates the obligation of researchers and all other capturers of personal data specifically to anonymise data to ensure protection of personal information and participants’ identities (Clark, 2006, p. 4). While the Act encourages case-by-case discretion for the granting of exemptions, it does provide for ‘personal data that is processed only for research, statistical or historical purposes’ to be disclosed (Information Commissioners Office. Retrieved at https://ico.org.uk/for-organisations/guide-to-data-protection/exemptions/).
- 12.
Adding to concern about the coercive administration of contraception is that since at least 1991 scholars have argued that for a variety of reasons progesterone-only injectable contraceptives are risky (Sathyamala, 2000). Increasingly scientific evidence suggests that especially the three-month progestogen-only injectable contraception, commonly known as Depo-Provera, puts women at increased risk of being infected with HIV (Polis et al., 2014, 2016; Hapgood et al., 2018). For example, the results of a meta-analysis shows that women using Depo-Provera have a 40% higher risk of HIV infection compared to women not using a hormonal method of contraception (Polis et al., 2016). Though this scientific point is still under contestation, validation of the strength of these recent conclusions can be evidenced by the World Health Organisation’s (2017) shifting of progestogen-only methods to a ‘category two’ level of risk, which requires health professionals to advise women seeking these contraceptive methods of the potential for an increased risk of contracting HIV (p. 6). An open-label multi-year randomised control trial running predominantly in South Africa, the ‘ECHO study’ aims to determine conclusively the risk of progesterone-only injectable contraception, and will disclose the findings in 2019. For details, see http://echo-consortium.com.
- 13.
Personal interview, MOU Unit Manager, Midwife, Asanda Mlandu, 26 October 2016 conducted with the participation of the Operations Manager.
- 14.
Observation notes, MOU, 30 September, 7, 14 October 2013.
- 15.
Personal interview, medical student, secondary hospital internship, Thomas Russell, 30 November 2013.
References
Bowser, D., & Hill, K. (2010). Exploring evidence for disrespect and abuse in facility-based childbirth: Report of a landscape analysis. USAID-TRAction Project, Harvard School of Public Health University Research Co. Washington, District of Columbia: United States Agency for International Development.
Buchanan, D. R., & Miller, F. G. (2006). A public health perspective on research ethics. Journal of Medical Ethics, 32, 729–733. https://doi.org/10.1136/jme.2006.015891
Chadwick, R. (2017). Ambiguous subjects: Obstetric violence, assemblage and South African birth narratives. Feminism & Psychology. https://doi.org/10.1177/0959353517692607
Child, K. (2015, June 10). HIV positive women sterilised without consent. The Sowetan. Retrieved from www.sowetanlive.co.za/news/2015/06/10/hiv-positive-women-sterilised-without-consent
Clark, A. (2006). Anonymising Research Data ESRC National Centre for Research Methods. NCRM Working Paper Series (No. 7). Leeds: The University of Leeds.
Cloete, A., Simbayi, L., Zuma, K., Jooste, S., & Wabiri, N. (2015). The people living with HIV stigma index: South Africa 2014, Summary Report. HSRC, 05, 1–26.
Coovadia, H., Jewkes, R., Barron, P., Sanders, D., & McIntyre, D. (2009). The health and health system of South Africa: Historical roots of current public health challenges. The Lancet, 374, 817–834. https://doi.org/10.1016/S0140-6736(09)60951-X
D’Gregorio, R. P. (2010). Obstetric violence: A new legal term introduced in Venezuela. International Journal of Gynecology and Obstetrics, 111(3), 201–202. https://doi.org/10.1016/j.ijgo.2010.09.002
Economic and Social Research Council. (2016). Our Expectations of Ethics Review, Economic and Social Research Council, United Kingdom. Retrieved from www.esrc.ac.uk/funding/guidence-for-applicants/research-ethics/our-expectations-of-ethics-review
Essack, Z., & Strode, A. (2012). “I feel like half a woman all the time”: The impacts of coerced and forced sterilisations on HIV-positive women in South Africa. Agenda, 26(2), 24–34.
Farrell, E., & Pattison, R. C. (2004). Out of the Mouths of Babes–Innocent reporting of harmful labour ward practices. South African Medical Journal, 94(11), 896–897.
Garrard, E., & Dawson, A. (2005). What is the role of the research ethics committee? Paternalism, inducements, and harm in research ethics. Journal of Medical Ethics, 31, 419–423. https://doi.org/10.1136/jme.2004.010447
Gqola, P. D. (2015). Rape a South African nightmare. Johannesburg: MF Books.
Haggerty, K. (2004). Ethics creep: Governing social science research in the name of ethics. Qualitative Sociology, 27(4), 391–414. https://doi.org/10.1023/B:QUAS.0000049239.15922.a3
Hapgood, J. P., Kaushic, C., & Hel, Z. (2018). Hormonal contraception and HIV-1 acquisition: Biological mechanisms. Endocrine Reviews, 39(1), 36–78. https://doi.org/10.1210/er.2017-00103
von Hodlt, K., & Webster, E. (2005). Beyond the apartheid workplace: Studies in transition. Scottsville: University of KwaZulu-Natal Press.
Honikman, S., Fawcus, S., & Meintjes, I. (2015). Abuse in South African maternity settings is a disgrace: Potential solutions to the problem. South African Medical Journal, 105(4), 284–286. https://doi.org/10.7196/SAMJ.9582
Human Research Ethics Committee, Faculty of Health Sciences, University of Cape Town. (2013). Standard operating procedure ethical and regulatory requirements for human research. May.
Jewkes, R., & Penn-Kekana, L. (2015). Mistreatment of women in childbirth: Time for action on this important dimension of violence against women. PLOS Medicine, 12(6), 95–99. https://doi.org/10.1371/journal.pmed.1001849
Kruger, L., & Schoombee, C. (2010). The other side of caring: Abuse in a South African maternity ward. Journal of Reproductive and Infant Psychology, 28, 84–101.
Moffett, H. (2006). ‘These women, they force us to rape them’: Rape as narrative of social control in post-apartheid South Africa. Journal of Southern African Studies, 32, 129–144. https://doi.org/10.1080/03057070500493845
National Planning Commission (2011). Diagnostic overview, South African government. Retrieved from http://www.gov.za/sites/ www.gov.za/files/npc_diagnostic_overview.pdf
Pharma-Ethics (2017) Fees schedule: 1 January 2017. Retrieved from www.pharmaethics.co.za/fees.htm
Pickles, C. (2015). Eliminating abusive ‘care’: A Criminal law response to obstetric violence in South Africa. South African Crime Quarterly, 54, 5–16.
Pires, A. F., d’Oliveira, L., Diniz, S. G., & Schraiber, L. B. (2002). Violence against women in health-care institutions: An emerging problem. The Lancet, 359(9318), 1681–1685. https://doi.org/10.1016/S0140-6736(02)08592-6
Polis, C. B., Curtis, K. M., Hannaford, P. C., Phillips, S. J., Chipato, T., Kiarie, J. N., … Steyn, P. S. (2014). Hormonal contraceptive methods and risk of HIV acquisition in women: A systematic review of epidemiological evidence. Contraception, 90(4), 360–390. https://doi.org/10.1016/j.contraception.2014.07.009
Polis, C. B., Curtis, K. M., Hannaford, P. C., Phillips, S. J., Chipato, T., Kiarie, J. N., … Steyn, P. S. (2016). An updated systematic review of epidemiological evidence on hormonal contraceptive methods and HIV acquisition in women. AIDS, 30(17), 2665–2683. https://doi.org/10.1097/QAD.0000000000001228
Sathyamala, C., (2000). An epidemiological review of the injectable contraceptive, depo-provera. Pune and Mumbai: Medico Friend Circle and Forum for Women’s Health.
Smith Tuhiwai, L. (2012). Decolonizing Methodologies: Research and Indigenous Peoples (2nd ed.). Dunedin: University of Otago Press.
Treatment Action Campaign. (2015, February 19). TAC to continue to call for dismissal of MEC for health in free state. Cape Town: Treatment Action Campaign.
Truth and Reconciliation Commission of South Africa. (2003). Truth and reconciliation commission of South Africa report (Vol. 4). Cape Town: Truth and Reconciliation Commission.
World Health Organization. (2015). The prevention and elimination of disrespect and abuse during facility-based childbirth. WHO/RHR/14.23, Geneva: WHO.
World Health Organization. (2017). Hormonal contraceptive eligibility for women at high risk of HIV: Guidance Statement. Geneva: WHO.
Acknowledgements
I am the primary investigator of the research project upon which this chapter is based and thus solely responsible for the contents of the chapter. This research has been supported by funding from the Economic and Social Research Council, United Kingdom, and through the EUSAid program of the European Commission.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 The Author(s)
About this chapter
Cite this chapter
Rucell, J. (2018). Ethics Review and the Social Powerlessness of Data: Reflecting on a Study of Violence in South Africa’s Health System. In: Macleod, C., Marx, J., Mnyaka, P., Treharne, G. (eds) The Palgrave Handbook of Ethics in Critical Research. Palgrave Macmillan, Cham. https://doi.org/10.1007/978-3-319-74721-7_19
Download citation
DOI: https://doi.org/10.1007/978-3-319-74721-7_19
Published:
Publisher Name: Palgrave Macmillan, Cham
Print ISBN: 978-3-319-74720-0
Online ISBN: 978-3-319-74721-7
eBook Packages: Behavioral Science and PsychologyBehavioral Science and Psychology (R0)