Abstract
Individuals with cerebral palsy often have functional deficits in their feet that adversely affect their gait. In order to effectively treat these deficits, an accurate description of the function of the individual’s foot function is necessary. The foot is a complex structure with many intrinsic components. Traditionally, the foot’s function has been measured through physical exams, pedobarographs, force plates, and a single-segment approximation in motion analysis. With improvements in technology, it has become clinically practical to measure the kinematics of the foot using multiple segments. These models provide the clinician with information and insight into the function of intrinsic structures of the foot, while the foot performs an actual task. This chapter will explore the limitations of non-motion analysis measurement techniques, and the traditional single foot model. The multisegmented foot model will be introduced with a discussion of its limitations. Finally, the advantages and utility of the multisegmented foot model will be demonstrated through normative and clinical examples.
Access provided by Autonomous University of Puebla. Download reference work entry PDF
Similar content being viewed by others
Keywords
Introduction
The bipedal foot is a complex structure of 26 bones, 33 joints, and hundreds of ligaments tendons and muscles (these values differ slightly depending on the reference). Major joints of the foot and ankle are the talocrural (ankle joint), talocalcaneal (subtalar), transverse tarsal (midtarsal), and metatarsophalangeal. The ankle and subtalar joints together comprise a mechanism of two joints, which are linked in motion (Close et al. 1967; Wong et al. 2005). The subtalar and multiple other joints participate in the clinically significant combined motions of supination, inversion, and adduction and the corresponding opposite motion of pronation, eversion, and abduction. The axes of rotation and range of motion of the ankle, subtalar, and midfoot joints have been studied in cadavers, and elegant models of foot function have been described (Chen et al. 1988; Mann and Coughlin 1992a, b; Ouzounanian and Shereff 1989; Scott and Winter 1991; Siegler et al. 1988). These structures serve as a firm foundation for support, as a flexible and malleable mechanism for shock absorption and adaptation to uneven surfaces, and as a rigid lever for propulsion. The details of these functions vary with task, structure, environment, and motor control. For example, the method that the foot uses to accomplish shock absorption is different for running than it is for walking (task dependence). The technique used by the foot to propel the body is different if the foot is forced to turn out due to tibial torsion than the technique used if the foot is inline (structural dependence). The action of the foot will vary between hard and soft surfaces, level and tilted, smooth and uneven surfaces, and shod and unshod conditions (environmental dependence). The foot performs differently for a person with an equinus contracture than it does for a person with a heel toe pattern gait (motor control dependence). Because of these types of differences, it is crucially important to study and analyze the foot as it functions in performing the task of interest. This point was supported by the work of Cavanagh et al. (1997) who demonstrated that very few relationships exist between static foot structure such as that gained from radiological examination or physical exam and dynamic foot function as characterized by motion analysis. They concluded from their work that only dynamic study during activity allows clinicians to distinguish between normal and pathological foot function, to discriminate between the various levels of impairment, and to quantitatively assess clinical outcomes. While radiological imaging can provide insight into the structure of the foot and physical exam can explore the potential and limitations of a foot’s capabilities by probing the limits of range of motion and strength, a foot may not actually perform up to these potentials during ambulation. Conversely it is difficult for examiners to match the external forces of a task like walking in magnitude, direction, and timing; thus, the foot may not perform up to its capabilities during the examination.
Measurement Other than Motion Analysis
Insight into the function of the foot can be gained through the use of force plates and pressure platforms (Miller 2005; Chang et al. 2002; Church et al. 2008). These devices measure the interaction of the foot with the ground. Ground reaction forces and moments are typically measured using force plates. A force plate is simply a very accurate scale that has six outputs: the force in each of the three directions (Fx, Fy, Fz), the location of the center of the application of the force (also called the Center of Pressure CoPx and CoPy), and the amount of twist that is applied to the surface (the free moment designated as Mz). While very accurate sensitive and fast, force plates only provide the net result of the body’s interaction with the ground. That is, if two feet are pushing on the plate at the same time as might occur during double support, the force plate reports the net result of the feet and not the independent contributions of each foot. Even in the case of single foot contact, the plate only reports a single force and moment regardless of how the force is distributed underneath the foot. While it is true that one can get more information by mapping the path of the CoP under the foot and infer varus and valgus or equinus patterns, one still has no detailed information of the foot’s function.
This is solved through the use of pressure platforms, which divide the surface into small squares and measure the corresponding force in each region. They provide a more detailed picture of the ground-foot interaction. There are many methods for detecting the force ranging from piezoelectric sensor arrays to light refraction, but the ultimate result is a three-dimensional array of data (force at each x, y location and time). The spatial and temporal resolution of the images generated by commercial pedobarographic systems range from approximately 3 to 10 mm and 25 to 500 Hz. Thus, a typical resolution can result in a contact area of approximately 500 sensors (given a typical adult human foot surface is approximately 100 cm2). The force is converted to an average pressure over the given area of an individual sensor.
To aid in interpretation, the maximum value at each location is color coded (six maps at the top of Fig. 1). While the values at each time point can be displayed, this is not typically done as the amount of data would simply overwhelm the clinician in a typical circumstance. Instead the foot is subdivided into anatomical or functional regions, and the summated pressure in each region is presented along with normative bands (six graphs at the bottom of Fig. 1). The method of subdividing the foot differs with pressure system, software, and institution. We have found, at the AI duPont Hospital for Children, that five functional subdivisions, heel, medial midfoot, lateral midfoot, medial forefoot, and lateral forefoot, create a good practical balance between detail, repeatability, and processing time. In this manner the pedobarograph is very useful for monitoring diabetic foot ulceration and for quantifying varus/valgus and heel contact positions. The test can be used as a yearly follow-up tool for children with foot deformities, and it is especially useful to assess planovalgus feet in young children as Chap. 95, “Pedobarograph Foot Evaluations in Children with Cerebral Palsy”. The drawbacks of the pedobarograph are that only normal forces are measured (no sheer or moment), the speed and dynamic response of pedobarographs are less than force plates, and they are not as accurate as force plates.
While the aforementioned techniques provide insight into task-specific foot function, they are limited to the ground-foot interactions. Three-dimensional motion analysis does not have this limitation. Three-dimensional motion analysis has developed into a major component of orthopedic medicine. By modeling the body as a group of rigid body segments, it is possible to calculate the kinematics and kinetics at any articulation (Chap. 93, “Kinematics and Kinetics: Technique and Mechanical Models”). It is frequently used for presurgical planning, postsurgical follow-up, and numerous research studies.
Motion Analysis: Single-Segment Foot Model
Unfortunately, when clinical motion analysis was being developed in the late 1980s and early 1990s, technical capabilities and practical considerations limited the modeling of a foot to a simple single rigid segment composed of everything distal to the ankle or talocrural and the talocalcaneal (subtalar) joints. Such a model allows identification of movement, forces, moments, and powers generated about the ankle (Winter 2005). As shown in Fig. 2, the traditional single-segment foot model is based on a vector that passes from a marker placed on the rear medial/lateral bisection of the calcaneus to a “toe” marker that is placed just proximal to the space between the second and third metatarsal heads. The height of the calcaneal marker is adjusted up or down so that the vector is parallel to the plantar surface of the foot.
As a vector, this model cannot provide any information about the rotation about the foot’s longitudinal axis (varus/valgus); however, sometimes, the ankle joint center is utilized as a third point to define the midsagittal plane of the foot to measure motion in three dimensions. This can be an unreliable reference. For example, with a collapsed foot (midfoot break), the ankle joint center, toe, and calcaneal markers may be nearly collinear or form a plane that poorly corresponds with the midsagittal plane of the foot. The primary assumption of the single-segment foot model is that the foot segment is relatively rigid between the heel and the toe markers and the structure of the foot is relatively normal with no static or dynamic deficits. This assumption combined with the placement of the markers means that the measured ankle motion is actually a combination of all the joints of the foot. These joints include the proximal and distal tibiofibular joints, the talocrural or ankle joint, the talocalcaneal or subtalar joint, the talonavicular and the calcaneal cuboid joints, the five tarsometatarsal joints, five metatarsophalangeal joints, and the interphalangeal joints. If the bones of the foot are well aligned and stable, this assumption may be reasonable, and the ankle motion measured by the single-segment foot represents the combined action of the talocrural (tibiotalar) and subtalar (talocalcaneal) joints. This compound joint can be considered to function as a universal joint consisting of two successive, nonparallel hinge joints. While there are methods that attempt to distinguish and separate the actions of the two joints (Lewis et al. 2006, 2007), it is beyond the scope of this chapter. For the remainder of this chapter, the term “ankle” will be used to refer to the combined structure and function of the talocrural and subtalar joints. The effects of the inferior tibiofibular joint are assumed to be inconsequential.
If there are static deformities in the foot, then the foot vector will be mal-aligned resulting in a fixed offset in the ankle angle. For example, in a foot with metatarsus adductus, the measured ankle position will be internal relative to what it should be. One method of addressing this issue is to place the “toe” marker proximal to the deformity. This will correct the ankle measurement at the expense of ignoring the function and position of the distal foot. The situation is even more problematic if there is dynamic instability in the foot. When this happens the rigid body assumption will be jeopardized, and the measurement of ankle joint kinematics will reflect the net effect of all the joints spanned by the calcaneal and toe markers. That is, the measured ankle joint motion includes the effects of the midfoot (Chopart) (navicular and cuboid) movement relative to the hindfoot (talus and calcaneus) and the forefoot (cuneiforms, metatarsals, and phalanges) motion relative to the midfoot (Lisfranc) in addition to the talocrural and subtalar motion. As an illustration of how intrinsic foot joints affect the measured ankle motion, one study using three markers on the calcaneus measured the motion of the hindfoot to be generally smaller than that measured by the traditional single-segment foot model (Lui et al. 1997).
Motion Analysis: Multisegment Foot Model
Many of the shortcomings of the single-segment foot can be addressed by utilizing a multisegmented foot model. Fortunately, computers and cameras used for motion analysis systems have evolved and improved to make this a practical possibility. Specifically, cameras with >12 megapixel resolution of sufficient sensitivity and the corresponding computer power to process this volume of data in a timely manner allow one to cover large enough volumes for full body gait analysis that includes small closely spaced markers needed to subdivide the foot into multiple segments. While the ideal foot model would consider the function of all the bones and joints in the foot, it is obviously impossible to account for every aspect of the foot’s skeletal anatomy by monitoring the motion of markers placed on the skin. Consequently, concessions have to be made regarding how the foot is modeled and how marker locations are defined to enable measurement of the model’s components. That is, multisegmental foot models still need to cluster groups of bones together to form segments. Because of the complexity of the foot, the substantial number of models that can be imagined to represent the foot, and the number of laboratories working independently on this problem, many different multiple segment foot models have been proposed. The differences between multisegment foot models include number and selection of segments, landmarks used, type of marker/clusters used, definition of the anatomical frames, neutral reference posture, and offsets. Most models divide the foot into three or four segments, namely, the hindfoot (rearfoot), midfoot, forefoot, and hallux. A majority of the models use three non-co-linear markers to represent each segment; however, some markers are shared between two adjacent segments. Thus some segments have a full six degrees of freedom; however, relative segmental displacements are rarely measured or documented. The shank as the rigid combination of the tibia and fibula was considered as the proximal segment that the ankle motion is based upon. In a majority of the models, the calcaneus and the talus were modeled as a single segment, or conversely, the motion of the talus was simply ignored, and only the relative movement of the calcaneus and the shank were reported. In either case, the hindfoot segment is represented by markers placed on the calcaneus. The number and placement of markers varies with each model as does the determination of hindfoot anatomical axes. As is true for the hindfoot, some investigators model the midfoot as a rigid segment, while others consider it to be part of the joint between the hind- and forefoot. Bones included in the midfoot section, marker placement, and coordinate axes vary considerably with each specific model. The forefoot can be defined as one rigid segment that includes the five metatarsal bones or split into medial and lateral segments. The tendency is to group the first and second metatarsals to form the medial forefoot and group metatarsals three to five to comprise the lateral forefoot, but this is not universal. The hallux is included in a majority of the models as a segment with one, two, or three degrees of freedom. If only one degree of freedom is considered, it is typically flexion/extension. Abduction or adduction is added for two degrees of freedom. These motions only require the use of one marker on the hallux and a shared marker on the forefoot. For the third degree of freedom, internal/external rotation, one needs a marker or cluster on a wand. There are instances where the lateral toes are modeled, but this is rare. Most models use a Cardan/Euler angle or Joint Coordinate System (Grood and Suntay 1983) to describe the orientation of adjacent segments. A deviation from the standard approach is seen in the Heidelberg foot measurement method (Simon et al. 2006) which uses projections that may not necessarily coincide with standard planes of reference. Additionally, several authors have also modeled some clinical or functional parameters that are of clinical interest such as the medial longitudinal arch index as represented by the ratio of the arch height to its length. These issues represent problems of choice, in that clinicians will eventually have to choose a model with defined structural and mathematical properties that best suits their needs. More details regarding specific models can be found in review articles by Rankine et al. (2008), Deschamps et al. (2011), and Novak et al. (2014). Rankine et al. (2008) analyzed 25 papers to classify foot models in terms of number of segments and joint rotations. Deschamps et al. (2011) looked at 15 models in relationship to the number of markers, the number of modeled segments, the method of 3D angle calculations, the methodological studies, and subsequent clinical studies. Novak et al. (2014) presents an in-depth review of five foot models.
All of these differences in foot models make it difficult to compare and contrast results from different studies. To make it even more difficult, each investigator typically utilizes populations that vary in size, age gender, and diagnosis or particular deformity. Two studies have examined this issue by placing an amalgamation of markers from multiple models on a single subject. The first by Mahaffey et al. (2013) combined marker sets of the Oxford model (Stebbins et al. 2006; Curtis et al. 2009), the Leardini model (Leardini et al. 1999, 2007), and the MacWilliams model (MacWilliams et al. 2003). Another paper by Nicholson et al. (2018) examined the unification of the Oxford (Stebbins et al. 2006; Curtis et al. 2009), the Leardini (Leardini et al. 1999, 2007), the duPont (Henley et al. 2004, 2008), Utah (Saraswat et al. 2012), and Heidelberg (Simon et al. 2006) models. In summary, while the measured patterns of movement produced by each model were similar, fixed or dc offsets were often present. Additionally, there were differences in repeatability in the models that may have been due to differences in therapist’s familiarity with the models as opposed to an intrinsic model attribute.
As markers are placed in proximity to other markers, the precision of marker placement becomes more critical to the validity of the results. More to the point, as markers are placed closer together, small errors in placement have larger effects on the orientation of the segments defined by the markers (Brown et al. 2009). For example, if two markers were placed on the shank with a center-to-center distance of 400 mm (typical adult tibial length or distance between ankle and knee markers), and one marker had a lateral displacement error (displacement orthogonal to the vector formed by the two markers) of 3 mm, the resulting error in orientation of the vector formed by the two markers would be 0.43° of orientation error. Now, consider two markers placed on the back of the calcaneus with a center-to-center distance of 18 mm. In this situation, the same 3 mm lateral displacement for one marker will yield a 9.5° of orientation error. Laterally misplacing both markers in different directions would amplify the orientation error.
Errors in marker placements can occur for a number of reasons, most of which are associated with one’s abilities to visualize or palpate anatomical landmarks and place the markers on the exact points of identification. The ability to visualize or palpate anatomical landmarks is complicated by the fact that most landmarks are covered by skin, fat tissue, muscle, and/or tendon. It would be convenient if all subjects had freckles or birthmarks at the precise locations where we desire to place the markers; instead, landmarks consist of flat surfaces, depressions, or points (such as an epicondyle or a tubercle), and each of these has its own unique issues. The flat surface identifies an area for marker placement but provides no precise point. Consequently, the clinician is faced with the decision of determining the exact location for placement of the marker center within the area, and this is open to interpretation on the part of the clinician. Pointed surfaces present both a palpation/visualization problem and a marker attachment problem. For example, the shape of the medial malleolus resembles a ridge more than a point, and the clinician is again faced with determining the location on the ridge where the marker should be placed. The lateral malleolus, on the other hand, resembles more of a point and provides a more precise landmark. However, attachment of the marker over the lateral malleolus is more difficult because of the fact that it resembles a point and because the peroneal tendons which move beneath the marker and result in unwanted marker motion. More subtle landmarks that are found in the foot (i.e., the navicular or cuboid surfaces) are difficult to palpate and almost impossible to visualize in many subjects. Given that anatomical structures are not clean, simple geometric shapes that exhibit variability even bilaterally within an individual (i.e., the left and right feet of an individual are not mirror images of one another), precise marker placement is not an easy accomplishment. Tendons, fat pads, veins, and interference from other structures such as the opposing limb may alter the appropriateness of specific landmarks and require that markers be placed in other locations. Additionally, the presentation of these structures may be altered as a result of therapeutic interventions such as surgery.
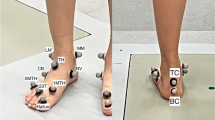
To better understand these limitations, a study to determine the reliability associated with placing markers on specific anatomical landmarks about the foot and the ankle was conducted in the gait laboratory at AI duPont Hospital for Children. Marker reliability measures were obtained using 14 adult feet (mean, 30 ± 7.8 years; average foot length, 246.26 ± 22.11 mm) and 8 pediatric feet (mean, 6.5 ± 2.6 years; mean foot length, 196.38 ± 28.80 mm). Three clinicians with extensive experience in gait analysis identified anatomical landmarks on the foot necessary to produce the desired four-segment foot model. The model used was one developed and used in the gait laboratory at AI duPont Hospital for Children since 2002 (Henley et al. 2004, 2008) which developed out of a model used at the Richmond children’s hospital (Henley et al. 2001).
The foot model intrinsic segments consist of the hindfoot, forefoot, medial forefoot, lateral forefoot, and hallux. The “ankle joint” is defined by the relative orientation of the hindfoot and the lower leg. The forefoot, medial forefoot, and lateral forefoot “joints” are defined by the orientation of the respective segments with the hindfoot and the hallux with respect to the forefoot.
The hindfoot anatomical coordinate system is created from the two posterior calcaneal markers and the ankle joint center, which was simply defined as the bisection of the medial and lateral malleolus markers. The Z-axis of the hindfoot anatomical system was the unit cross product of the vector from the bottom calcaneus marker to the ankle joint center with the vector from the bottom calcaneus marker to the top calcaneus marker pointing right. The anatomical Y-axis of the hindfoot was the unit vector parallel to the cross product of the global Z-axis and the Z hindfoot anatomical axis. This was determined with the patient standing in weight bearing and the foot flat on the ground. The anatomical X-axis of the hindfoot was formed from the unit cross product of the Y and the Z hindfoot anatomical axes. Thus the Z-axis points to the right of both feet, the Y-axis points anteriorly, and the X-axis points toward the plantar surface.
By utilizing the global vertical when the foot is flat on the ground, the calcaneal markers define the eversion/inversion attitude of the hindfoot. The plantar/dorsiflexion attitude of the hindfoot is defined to parallel to the floor when the foot is flat. The internal/external rotation attitude of the hindfoot was defined by the plane formed by the calcaneal markers and the ankle joint center.
The Y-axis of the forefoot followed line segment between the bisection of the navicular and the cuboid and the bisection of the first and fifth metatarsal markers. The X-axis was the resulting cross product of the vector from the first metatarsal to the fifth metatarsal and the Y-axis. The Z-axis of the forefoot was the cross of the X- and Y-axes. The medial forefoot segment Y-axis is the vector from the navicular to the first metatarsal. The X-axis is the cross of the navicular to the 2/3 metatarsal with the Y-axis. The Z-axis is the result of the cross of the X- and Y-axes. The lateral forefoot segment Y-axis is the vector from the cuboid to the fifth metatarsal. The X-axis is the result of the cross of the cuboid to the 2/3 metatarsal with the Y-axis. The Z-axis is the cross of the X- and Y-axes. The height of the arch was calculated as the height of the navicular with respect to the bottom of the foot, and the arch index was the ratio of this height to the distance between the bottom calcaneus and the first metatarsal markers (Fig. 3).
Data collection consisted of two parts. First, a method to insure that the subjects’ feet could be positioned in the exact location and orientation within the camera volume was tested. The method consisted of creating plaster of Paris molds that formed a cast around the sole of each subjects’ feet. The molds were formed directly on the laboratory floor and were immovable. The ability of a subject to place their feet in the exact same position and orientation in the calibrated volume was tested by having one clinician place the markers on the feet of each subject. The subjects then placed their feet in their molds, and the positions of the markers were recorded using an eight-camera motion analysis system for 0.5 s at 60 Hz in a 3 m by 7 m volume. The subjects removed their feet from their molds, walked around the perimeter of the laboratory, and then repositioned their feet in the molds without disturbing the original marker placement. A second measurement was taken with the motion analysis system. The positions of each marker on each subjects’ feet were then compared between trials.
The second part of data collection had two goals: (1) to measure the ability of a single clinician to repeatedly place markers on the same landmarks on each subject’s feet and (2) to determine the agreement between different clinicians placing markers on the same landmarks on each subject’s feet. Three clinicians placed the marker set on each subject’s feet twice. Clinicians and trials were randomized for each subject. Following marker placement by an individual clinician, the subject stepped into the plaster casts, and the marker positions were recorded. The subject then stepped out of the casts, and the markers were removed. A second clinician would then apply the markers, and the measurement process was repeated.
Comparison of Fig. 4a–c provides a sense of the additional of variability when multiple clinicians place the markers. Note that each series of figures was performed on the same individual ten times.
(a) Ten trials of a single subject after stepping in and out of the mold without having markers removed and replaced between trials. (b) Ten trials of a single subject after having markers removed and replaced between trials by a single clinician. (c) Ten trials of a single subject after having markers removed and replaced between trials by a three clinicians
The variability in marker placement in turn produced variability in the orientation of the foot model segments. Table 1 lists the resulting errors in hindfoot orientation.
Although the specific numerical results are applicable only to our model, our lab and camera system, and our clinicians, it is safe to generalize these trends to all multisegment foot models. That is, the higher within-clinician reliability and lower between-clinician reliability suggest that measures of multisegment foot kinematics are related to the clinician’s sense of the foot anatomy and their preferences in placing markers on irregular surfaces. In light of the work by Gorton et al. (2009), in looking at a laboratory’s ability to utilize full body marker sets, foot marker sets are not unique. However, due to the close proximity of the markers utilized in multisegment marker sets, the variability associated with placing markers has a more detrimental effect. Researchers need to be aware of this issue and not rely on reports of motion analysis system accuracy and marker tracking ability as the sole limitations in the accuracy of data. At this juncture, the accuracy of marker placement is likely to have a more profound effect.
In addition to placement error, markers mounted on the skin surface will move relative to bone when the foot moves. This can be eliminated using intercortical bone pins or external fixators instrumented with markers or through the use of radiopaque beads in radiostereometric analysis (Reinschmidt et al. 1997; Leardini et al. 2005; Wrbaskić and Dowling 2007; Shultz et al. 2011). While the invasive nature of these procedures makes their clinical use impractical, these studies provide insight into the limitations of foot models, and they can serve as a reference for other studies. The measures found in general that the relative motion of markers and bone to be small (Tranberg and Karlsson 1998) and less than that typically found for markers on the shank or thigh (Leardini et al. 2005) and therefore good enough for foot bone tracking even though artifacts as large as 16 mm in the hindfoot and midfoot were observed at toe-off. In vitro robotic manipulation of cadaver specimens has shown that skin- and bone-based systems produce similar foot joint kinematic patterns (Whittaker et al. 2011; Peeters et al. 2013; Nester et al. 2007a; Westblad et al. 2002). In vivo bone pin experiments (Nester et al. 2007a, b, 2010; Arndt et al. 2007; Lundgren et al. 2008; Wolf et al. 2008; Okita et al. 2009) revealed that the motion of major intrinsic foot to be complex and that the motion of small joints to be larger than expected (e.g., the talonavicular has a range of 10° in three dimensions). Nester et al. (2007a) disagreed slightly in that they believed that markers will not be able to accurately capture the precise kinematics of individual foot structures. However, the modes are likely to continue to be of value in identifying subjects with gross pathology. Wolf et al. (2008) used their results to define segments as grouping of structures that had the most movement harmony. They concluded gait analysis should consist of the following four segments: calcaneus, navicular-cuboid, medial cuneiform-first metatarsal, and fifth metatarsal. They also used their later results (Nester et al. 2010) from pins to prose a functional model consisting of a reported three segment mid- and forefoot model: (1) navicular and cuboid; (2) cuneiforms and metatarsals 1, 2, and 3; and (3) metatarsals 4 and 5. They acknowledged that while this makes kinematic since it may not be the best grouping of segments depending on the clinical issue and the problem being examined.
Perhaps the greatest source of confusion regarding foot models is defining the anatomical axes for each segment (Arndt et al. 2007). For large segments of the body, this poses little problem, and there are generally agreed standards for the anatomical axes (e.g., ISB recommendations: Wu et al. 2002). For example, the thigh is usually defined as having the Y-axis follow the line joining the midpoint between the medial and lateral femoral epicondyles and the hip joint center, the Z-axis perpendicular to the Y-axis and in the plane defined by the hip joint center, and the two femoral epicondyles pointing to the right. The X-axis is the line perpendicular to both the Y- and Z-axis pointing anteriorly (Cappozzo et al. 1995). With the exception of the metatarsal bones, most of the bones are small irregular bones that do not have an obvious anatomical axis. Additionally, while the motions of the foot and ankle are defined in terms of cardinal planes, the axes of motion are not perpendicular to the cardinal planes (Root et al. 1977). Because of the orientation of these joints, axes of motion pass through all three of the cardinal planes. Therefore, motion which occurs at these joint occurs in all three planes. The geometry of the situation requires that if motion occurs in one plane, it must also occur in the other two. The amount of motion occurring in each plane depends entirely on the direction and magnitude that the rotational axis differs from the planes perpendicular. Pronation and supination are the terms that historically have been used to describe the triplanar motions in the foot and ankle. These two motions are pure rotation about an oblique axis resulting in the end position as three separate rotations in the cardinal planes (Oatis 1988). The issue is even more confusing when open chain (OC) and closed chain (CC) foot/ankle motions are considered. OC pronation produces dorsiflexion, eversion, and abduction, while CC pronation produces internal rotation of the tibia, adduction and plantarflexion of the talus, and eversion of the calcaneus. CC pronation will cause a lowering of the medial longitudinal arch height. Pronation is a normal motion that begins at the time of initial contact and continues until the time of foot flat in mid-stance. Pronation facilitates the ability of the foot to adapt to uneven walking surfaces by unlocking the joints of the foot to make it flexible. It also facilitates flexion of the knee allowing the lower extremity to function as a shock absorber. In contrast while OC supination produces plantarflexion, inversion, and adduction, CC supination produces external rotation of the tibia, abduction and dorsiflexion of the talus, and inversion of the calcaneus. Therefore CC supination will increase the height of the medial longitudinal arch. Supination of the foot begins in mid-stance and peaks just prior to toe-off and creates a stable, rigid lever for push-off. This difference in open and closed chain motion also makes evaluation of foot function difficult to achieve through physical examination.
Normal Multisegment Foot Model Kinematics
The hindfoot as reference to the tibia starts neutral at initial contact and then rapidly moves into plantar flexion as the first rocker occurs and the foot achieves foot flat. Additionally, during this initial stance phase, the hindfoot experiences a period of rapid pronation and slight external rotation. This is consistent with subtalar motion and with increasing foot loading. During foot flat, the tibia continues to rotate over the foot producing a relative hindfoot dorsiflexon (second rocker). The hindfoot continues its relative pronation and internal rotation position. At toe-off (third rocker), the sagittal plane motion reversed, and the hindfoot plantarflexes under the forceful influence of the gastroc-soleus contraction and supinates. During the swing phase, the hindfoot quickly dorsiflexes to prepare for heel strike. In the coronal plane, during the initial period of stance, the hindfoot everts and externally rotates. This is consistent with motion through the subtalar joint to accept loading. The measured range of eversion is about 4° on average. Inversion occurs in late stance and proceeds through push-off. There is a single cycle of eversion and inversion which occurs during swing phase as the ankle recovers dorsiflexion and prepares for heel strike (Fig. 5).
The forefoot and lateral forefoot demonstrate similarly patterned kinematics starting with sharp dorsiflexion at initial stance as the weight of the body is supported. This is followed by little movement during the middle of the stance phase. At toe-off, the forefoot plantar flexes as the muscles contract and the foot turns into a lever for propulsion. During swing the foot relaxes and prepares for initial contact. The difference between the medial and lateral components of the forefoot relates to the offsets provided by the medial longitudinal arch. The forefoot starts supinated with a healthy arch; and as the path of the Center of Pressure (COP) follows the lateral border of the foot with weight acceptance, the COP moves medially across the metatarsal heads, and the longitudinal arch diminishes leading to a pronation of the forefoot. At toe-off, the shock absorption and weight acceptance mechanisms are released, and the forefoot segment supinates in preparation for initial contact.
The kinematics of the medial forefoot are reflected in the motion of the arch. With weight acceptance, the arch height decreases and the arch length increases, thus decreasing the arch index. The index peaks at toe-off after which the elastic properties and residual muscular action draw the foot back. Just prior to initial contact, the arch decreases in height leading to a decrease in the index.
Note that this model only measures flexion/extension and abduction/adduction of the hallux relative to the forefoot. The hallux starts in slight dorsiflexion relative to the forefoot and gradually increases throughout stance as the foot flattens. Dorsiflexion of the hallux continues at terminal stance during the push-off as the foot pivots on the ball of the foot (third rocker). After toe-off, the elastic structures and continued muscle flexion act to snap the hallux into plantarflexion which it maintains until initial contact. With respect to the transverse plane, the hallux is neutral at initial contact and moves into abduction through stance. It experiences a short adduction at toe-off and returns to neutral during swing phase.
Clinical Examples
The following are three example cases to illustrate the insight that can be derived from using a multisegment foot model. The first is of an individual with a midfoot break, the second is of an individual with a forefoot adduction, and the third is of an individual with a cavovarus foot deformity.
Midfoot break (MFB) is a deformity where there is excessive motion at the midfoot. It is most common in children with cerebral palsy (CP) (Gage et al. 2009), but may also be seen in children with other disorders such as spina bifida (Maurer et al. 2013). The MFB develops because the gastroc-soleus muscles are tight and pull the hindfoot into equinus resulting in a stiff ankle. This results in a breakdown of intrinsic foot joints, resulting in excessive midfoot motion, a collapse of the longitudinal arch of the foot, and an inefficient lever arm. The foot becomes ineffective at push-off, and this may result in painful calluses over the navicular and or talus. Surgical intervention is sometimes necessary to establish a plantigrade foot whereby both the hindfoot and forefoot are on the ground during standing (Mosca 2010). The long-term morbidity following surgical treatment of MFB can be serious; thus early diagnosis and preventative treatments for MFB are critical. A clinical diagnosis of MFB can be made by keeping the ankle joint fixed and manipulating the forefoot. Motion at the forefoot is a positive sign for MFB as a typical foot should present with little bending at the midfoot. This can be confirmed with a radiograph of the standing foot and measuring the talonavicular angle on both the AP and lateral views (Davids et al. 2005). However, this is just a static measure, and as stated before, radiographs provide no information about the dynamic function of the body.
Figure 6 illustrates that a single-segment foot model (blue ankle graph line) shows the foot to have a fairly normal sagittal plane motion. However, the multisegmented foot shows that the hindfoot has a normal initial contact and first rocker, yet it fails to dorsiflex with respect to the lower leg. That is, with the lower leg rotating forward during stance, the hindfoot rotates with it. This motion is accommodated as the forefoot dorsiflexes with respect to the hindfoot as seen in the bottom graph of Fig. 6.
Sagittal plane motion of a foot with a midfoot break. Top graph. Hindfoot: relative motion of the hindfoot and the lower leg. Ankle: relative motion of the whole foot as modeled as a single segment. Bottom graph. Forefoot: motion of the forefoot relative to the hindfoot as modeled by a multisegmented foot
Based on the information provided by the single-segment foot model, one might conclude, in this case, that while there was a slight reduction in ankle motion, the range was quite reasonable. However, the information from the multisegment model indicates that the ankle motion is quite restricted with considerable abnormal movement in the midfoot. Given this additional information about the true muscle tightness across the ankle, clinical management would differ greatly, and surgical treatment options would likely be considered to prevent progression of the midfoot break. This is confirmed in a lateral photograph (Fig. 7) of the subject that clearly shows the midfoot break and the relative motion of the fore- and hindfoot segments.
The following (Fig. 8) illustration shows how the multisegment foot model views the intrinsic motion of the foot. In the figure, the hindfoot is fixed in place and the other parts of the foot move relative to it. The red lines represent the foot just after initial contact when it first reaches foot flat, and the blue lines represent the foot at terminal stance or push-off.
Next is an example of an individual with an adducted forefoot (Fig. 9).
Note (Fig. 10) how the single segment (ankle) portrays a neutral presentation, while the multisegment foot has the hindfoot external and the forefoot adducted. That is, the rear of the foot externally rotated and the front of the foot pointing inward in adduction for a net neutral presentation in a non-neutral foot.
Finally, here is an example (Fig. 11) of an individual with cavovarus foot deformity where the relatively strong peroneus longus and tibialis posterior muscles cause a hindfoot varus and forefoot valgus (pronated) position.
With a single-segment foot model, we get no information in this plane, while the multisegmented foot model (Fig. 12) shows the torsional situation very clearly along with a larger than normal arch. Note that the torsion in this case is relatively rigid and constant over the gait cycle.
Summary
The foot is a complex structure with many individual parts that play a key role in one’s ability to walk. Thus understanding its function is crucial. While there are many tools and methods used to measure a foot’s function, it is vital to make the measurements during the task of interest. Therefore, while physical exam and radiographic studies provide useful information, they fall short because the information gained can only be extrapolated to what occurs in functional tasks such as walking. While functional measurements can be made using motion analysis, traditional single-segment foot models were the only practical option in the past. Improvements in computer and camera technology have allowed clinicians to develop more sophisticated multisegmented models that can be used clinically. The ideal measurement of each individual bone is probably impossible due to the small size and proximity of individual bones. Additionally, markers have to be attached to the supple skin covering which generates an unwanted relative motion. However, the foot can be divided into functional units that can be measured in a practical manner. The one caveat is that there are many multisegmented foot models each with a unique manner of segmenting and marking the foot. Thus, each model makes its measurement from a different perspective. While this is an inconvenience, it is not unsurmountable. If one understands the limitations and assumptions of the model used, one can still gain tremendous insight into the function of healthy and pathological feet as was illustrated in the examples above. More accurate measurement of foot motion through the use of a multisegmented foot model will enable physicians and physical therapists to more accurately identify and classify deformities, plan more specific and effective management techniques, and improve evaluation of treatment outcomes.
References
Arndt A, Wolf P, Liu A, Nester C, Stacoff A, Jones R, Lundgren P, Lundberg A (2007) Intrinsic foot kinematics measured in vivo during the stance phase of slow running. J Biomech 40(12):2672–2678
Brown KM, Bursey DE, Arneson LJ, Andrews CA, Ludwig PM, Glasoe WM (2009) Consideration of digitization precision when building local coordinate axes for a foot model. J Biomech 42:1263–1269
Cappozzo A, Catani F, Della Croce U, Leardini A (1995) Position and orientation of bones during movement: anatomical frame definition and determination. Clin Biomech 10:171–178
Cavanagh PR, Morag E, Boulton AJM, Young MJ, Deffner KT, Pammer SE (1997) The relationship of static foot structure to dynamic foot function. J Biomech 30:243–250
Chang CH, Miller F, Schuyler J (2002) Dynamic pedobarograph in evaluation of varus and valgus foot deformities. J Pediatr Orthop 22:813
Chen J, Siegler S, Schneck CD (1988) The three dimensional kinematics and flexibility characteristics of the human ankle and subtalar joint – part II: flexibility characteristics. J Biomech Eng 110(4):374–385
Church C, Lennon, N, Coleman S, Henley J, Nagai M, Miller F (2008) Dynamic foot pressure in the early evolution of foot deformities in children with spastic cerebral palsy. In: Harris GF, Smith PA, Marks RM (eds) Foot and ankle motion analysis: clinical treatment and technology. CRC Press, Boca Raton pp 93–103. https://books.google.com/books/about/Foot_and_Ankle_Motion_Analysis.html?id=EQGnLP_mKHcC&printsec=frontcover&source=kp_read_button#v=onepage&q&f=false
Close JR, Inman VT, Poor PM, Todd FN (1967) The function of the subtalar joint. Clin Orthop Relat Res 50:159–179
Curtis DJ, Bencke J, Stebbins JA, Stansfield B (2009) Intra-rater repeatability of the oxford foot model in healthy children in different stages of the foot roll over process during gait. Gait Posture 30(1):118–121
Davids JR, Gibson TW, Pugh LI (2005) Quantitative segmental analysis of weight bearing radiographs of the foot and ankle for children: normal alignment. J Pediatr Orthop 25:769–776
Deschamps K, Staes F, Roosen P, Nobels F, Desloovere K, Bruyninckx H, Matricali GA (2011) Body of evidence supporting the clinical use of 3D multi-segment foot models: a systematic review. Gait Posture 33(3):338–349
Gage JR, Schwartz MH, Koop SE, Novacheck TF (2009) The identification and treatment of gait problems in cerebral palsy (clinics in developmental medicine). Mac Keith Press, London
Gorton GE, Herbert DA, Gannotti ME (2009) Assessment of the kinematic variability among 12 motion analysis laboratories Gait and Posture 29:398–402. https://www.ncbi.nlm.nih.gov/pubmed/19056271
Grood ES, Suntay WJ (1983) A joint coordinate system for the clinical description of three-dimensional motions: application to the knee. J Biomech Eng 105:136–144
Henley J, Wesdock K, Masiello G, Nogi J (2001) A new three-segment foot model for gait analysis in children and adults. GCMA conference. Sacramento, 26–28 Apr
Henley J, Richards J, Hudson D, Church C, Coleman S, Kerstetter L, Miller F (2004) Reliability of a clinically practical multi-segment foot marker set/model. Abstracts of Ninth Annual Gait and Clinical Movement Analysis Society Lexington KY, 21–24 Apr
Henley J, Richards J, Hudson D, Church C, Coleman S, Kerstetter L, Miller F (2008) Reliability of a clinically practical multi-segment foot marker set/model. In: Harris G, Smith P, Marks R (eds) Foot and ankle motion analysis clinical treatment and technology. CRC Press, Boca Raton, pp 445–463. https://books.google.com/books/about/Foot_and_Ankle_Motion_Analysis.html?id=EQGnLP_mKHcC&printsec=frontcover&source=kp_read_button#v=onepage&q&f=false
Leardini A, Cappozzo A, Catani F, Toksvig-Larsen S, Petitto A, Sforza V, Cassanelli G, Gianini S (1999) Validation of a functional method for the estimation of the hip joint centre location. J Biomech 32:99–103
Leardini A, Chiari L, Della Croce U, Cappozzo A (2005) Human movement analysis using stereophotogrammetry. Part 3. Soft tissue artifact assessment and compensation. Gait Posture 21(2):212–225
Leardini A, Benedetti MG, Berti L, Bettinelli D, Nativo R, Giannini S (2007) Rear-foot, mid-foot and fore-foot motion during the stance phase of gait. Gait Posture 25(3):455
Lewis GS, Sommer HJ, Piazza SJ (2006) In vitro assessment of a motion-based optimization method for locating the talocrural and subtalar joint axes. J Biomech Eng 128(4):596–603
Lewis GS, Kirby KA, Piazza SJ (2007) Determination of subtalar joint axis location by restriction of talocrural joint motion. Gait Posture 25(1):63–69
Lui W, Siegler S, Hillstrom H, Whitney K (1997) Three-dimensional, six-degrees-of-freedom kinematics of the human hindfoot during the stance phase of level walking. Hum Mov Sci 16:283–289
Lundgren P, Nester C, Liu A, Arndt A, Jones R, Stacoff A, Wolf P, Lundberg A (2008) Invasive in vivo measurement of rear-, mid- and forefoot motion during walking. Gait Posture 28(1):93–100
MacWilliams BA, Cowley M, Nicholson DE (2003) Foot kinematics and kinetics during adolescent gait. Gait Posture 17(3):214–224
Mahaffey R, Morrison SC, Drechsler WI, Cramp MC (2013) Evaluation of multi-segment kinematic modeling in the pediatric foot models. J Foot Ankle Res 6:43
Mann RA, Coughlin MJ (1992a) Surgery of the foot and ankle, vol 1. Mosby, St. Louis
Mann RA, Coughlin MJ (1992b) Surgery of the foot and ankle, vol 2. Mosby, St. Louis
Maurer JD et al (2013) A kinematic description of dynamic midfoot break in children using a multi-segment foot model. Gait Posture 38:287–292
Miller F (2005) Cerebral Palsy. Springer Science – Business Media. Singapore https://www.springer.com/us/book/9780387204376
Mosca V (2010) Flexible flatfoot in children and adolescents. J Child Orthop 4:107–121
Nester C, Jones RK, Liu A, Howard D, Lundberg A, Arndt A, Lundgren P, Stacoff A, Wolf P (2007a) Foot kinematics during walking measured using bone and surface mounted markers. J Biomech 40(15):3412–3423
Nester CJ, Liu AM, Ward E, Howard D, Cocheba J, Derrick T, Patterson P (2007b) In vitro study of foot kinematics using a dynamic walking cadaver model. J Biomech 40(9):1927–1937
Nester CJ, Liu AM, Ward E, Howard D, Cocheba J, Derrick T (2010) Error in the description of foot kinematics due to violation of rigid body assumptions. J Biomech 43(4):666–672
Nicholson KF, Church C, Takata C, Niiler T, Chen BP, Lennon N, Sees JP, Henley J, Miller F (2018) Comparison of three-dimensional multi-segmental foot models used in clinical gait laboratories. Gait Posture 63:236–241
Novak AC, Mayich DJ, Perry SD, Daniels TR, Brodsky JW (2014) Gait analysis for foot and ankle surgeons – topical review, part 2: approaches to multi-segment modeling of the foot. Foot Ankle Int 35(2):178–191
Oatis C (1988) Biomechanics of the foot and ankle under static conditions. Phys Ther 68:1815
Okita N, Meyers SA, Challis JH, Sharkey NA (2009) An objective evaluation of a segmented foot model. Gait Posture 30(1):27–34
Ouzounanian TJ, Shereff MJ (1989) In vitro determination of midfoot motion. Foot Ankle 10(3):140–146
Peeters K, Natsakis T, Burg J, Spaepen P, Jonkers I, Dereymaeker G, Vander Sloten J (2013) An in vitro approach to the evaluation of foot-ankle kinematics: performance evaluation of a custom-built gait simulator. Proc Inst Mech Eng H 227(9):955–967
Rankine L, Long J, Canseco K, Harris GF (2008) Multisegmental foot modeling: a review. Crit Rev Biomed Eng 36(2–3):127–181
Reinschmidt C, van Den Bogert AJ, Murphy N, Lundberg A, Nigg BM (1997) Tibiocalcaneal motion during running, measured with external and bone markers. Clin Biomech 12(1):8–16
Root ML, Orien WP, Weed JH (1977) Clinical biomechanics: normal and abnormal function of the foot. Clinical Biomechanics Corp, Los Angeles
Saraswat P, MacWilliams BA, Davis RB (2012) A multi-segment foot model based on anatomically registered technical coordinate systems: method repeatability in pediatric feet. Gait Posture 35:547–555
Scott SH, Winter DA (1991) Talocrural and talocalcaneal joint kinematics and kinetics during the stance phase of walking. J Biomech 24(8):743–752
Shultz R, Kedgley AE, Jenkyn TR (2011) Quantifying skin motion artifact error of the hindfoot and forefoot marker clusters with the optical tracking of a multi-segment foot model using single-plane fluoroscopy. Gait Posture 34(1):44–48
Siegler S, Chen J, Schneck CD (1988) The three-dimensional kinematics and flexibility characteristics of the human ankle and subtalar joints – part 1: kinematics. J Biomech Eng 110(4):364–373
Simon J, Doederlein L, McIntosh AS, Metaxiotis D, Bock HG, Wolf SI (2006) The Heidelberg foot measurement method: development, description and assessment. Gait Posture 23:411–424
Stebbins J, Harrington M, Thompson N, Zavatsky A, Theologis T (2006) Repeatability of a model for measuring multi-segment foot kinematics in children. Gait Posture 23(4):401–410
Tranberg R, Karlsson D (1998) The relative skin movement of the foot: a 2-D roentgen photogrammetry study. Clin Biomech (Bristol Avon) 13(1):71–76
Westblad P, Hashimoto T, Winson I, Lundberg A, Arndt A (2002) Differences in ankle-joint complex motion during the stance phase of walking as measured by superficial and bone anchored markers. Foot Ankle Int 23(9):856–863
Whittaker EC, Aubin PM, Ledoux WR (2011) Foot bone kinematics as measured in a cadaveric robotic gait simulator. Gait Posture 33(4):645–650
Winter DA (2005) Biomechanics and motor control of human movement, 3rd edn. Wiley, New York
Wolf P, Stacoff A, Liu A, Nester C, Arndt A, Lundberg A, Stuessi E (2008) Functional units of the human foot. Gait Posture 28(3):434–441
Wong Y, Kim W, Ying N (2005) Passive motion characteristics of the talocrural and the subtalar joint by dual Eular angles. J Pediatr Orthop 38(12):2480–2485
Wrbaskić N, Dowling JJ (2007) An investigation into the deformable characteristics of the human foot using fluoroscopic imaging. Clin Biomech 22(2):230–238
Wu G, Siegler S, Allard P, Kirtley C, Leardini A, Rosenbaum D, Whittle M, D’Lima DD, Cristofolini L, Witte H, Schmid O, Stokes I (2002) Standardization and Terminology Committee of the International Society of Biomechanics. ISB recommendation on definitions of joint coordinate system of various joints for the reporting of human joint motion–part I: ankle, hip, and spine. International Society of Biomechanics. J Biomech 35(4):543–8. https://www.ncbi.nlm.nih.gov/pubmed/11934426
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Section Editor information
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this entry
Cite this entry
Henley, J. (2020). Foot Kinematics: Models Used to Study Feet in Children with Cerebral Palsy. In: Miller, F., Bachrach, S., Lennon, N., O'Neil, M.E. (eds) Cerebral Palsy. Springer, Cham. https://doi.org/10.1007/978-3-319-74558-9_95
Download citation
DOI: https://doi.org/10.1007/978-3-319-74558-9_95
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-74557-2
Online ISBN: 978-3-319-74558-9
eBook Packages: MedicineReference Module Medicine