Abstract
Until now, chemotherapy has been the main line of defense against Leishmania infections. However, drug use and abuse have resulted in the selection and development of resistance mechanisms which strongly limit the number of antiprotozoal agents that are effective for the treatment of this disease. The emergence and spread of resistance to drugs currently in use and available for leishmaniasis emphasize that new compounds need to be identified and developed and that novel chemotherapeutic targets must be characterized. Mechanisms of drug resistance are often associated with decreased uptake of the drug into the parasite, poor drug activation, physiological alterations in the drug target, and overexpression of drug transporter proteins. One mechanism of resistance to antimony in Leishmania involves a decrease in its accumulation by either reduced uptake or increased efflux, mediated by P-glycoprotein (Pgp)-like transporters, which belong to the ATP-binding cassette (ABC) superfamily of proteins. The inhibition of the function of these proteins represents an attractive way to control drug resistance in clinical environments. New natural or synthetic sesquiterpenes, flavonoids, acridonecarboxamide derivative modulators of human Pgp (zosuquidar and elacridar), statins, pyridine analogs, 8-aminoquinolines, or phenothiazines revert in Leishmania the resistance phenotype to antimony, pentamidine, sodium stibogluconate, and miltefosine by modulating intracellular drug concentrations. In this chapter, we review some concepts concerning the reversal mechanism of multidrug resistance by the use chemosensitizers which alter the capacity of Pgp.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Leishmania
- P-glycoprotein
- ATP-binding cassette
- Multidrug-resistant protein
- Antileishmanial drug
- Chemosensitizer
1 Introduction
Arsenic- and antimony-containing drugs are still the first line of treatment for leishmaniasis. Pentavalent antimonial compounds (SbV) remain the choice of treatment for all forms of leishmaniasis, ranging from cutaneous lesions to fatal visceral infections. The emergence and spread of resistance to currently used antileishmanial drugs emphasize the fact that new compounds need to be identified and developed. Resistance to antimonial drugs is everyday more frequently reported [1,2,3].
A large amount of scientific effort is spent on elucidating the mechanisms underlying this resistance with the hope of restoring/improving the efficacy of existing drugs and of developing new drugs that can bypass resistance mechanisms.
Among the various drug resistance mechanisms identified, those based on drug movement through the membranes appear to play an important role by decreasing the drug concentration at the target sites. The transport proteins of the ATP-binding cassette (ABC) superfamily provide the basis of multidrug resistance in mammalian cancer cells and in pathogenic yeasts, fungi, parasites, and bacteria [4,5,6,7,8]. ABC proteins were also identified in resistance to antileishmanial drugs (see Table 14.1). The ABC transporters are described in Chap. 11.
But all of the ABC families are not associated with antileishmanial drug resistance, such as the ABCA family [9].
The ABCB family includes the multidrug-resistant protein 1 (MDR1) or ABCB4 protein and the multidrug-resistant protein 2 (MDR2) or ABCB2 protein, whose overexpression confers resistance to vinblastine and structurally non-related hydrophobic compounds such as puromycin, adriamycin, doxorubicin, and daunomycin [10,11,12,13,14,15,16]. LeMDR1 (LeABCB4) can also affect pentamidine resistance [17]. Additionally, LgMDR1 and LaMDR1 are increased in antimony-resistant strains of L. (V.) guyanensis or L. (L.) amazonensis [18]. The subcellular location of LeABCB4 and LaABCB2 (LaMDR2) in the tubular structure, a compartment that may correspond to a multivesicular tubule lysosome, suggests that mechanisms of resistance in Leishmania are different from those acting in the conventional mammalian efflux pump Pgp MDR1.
The ABCC family includes the multidrug-resistant protein A (MRPA) or P-glycoprotein A (PGPA) or ABCC3; the P-glycoprotein E (PGPE) or ABCC4, associated with resistance to arsenite and antimonial drugs; and the pentamidine resistance protein 1 (PRP1) or ABCC7. ABCC3 and ABCC4 are involved in the resistance of Leishmania toward arsenic and antimony compounds [19,20,21,22]. Overexpression of ABCC4 and ABCC5 can also confer resistance to antimonial drugs in L. (S.) tarentolae [23]. Additionally, field-resistant isolates to antimony exhibit upregulation in ABCC3 (MRPA or PGPA) transcript levels in L. (L.) donovani, L. (V.) braziliensis, L. (V.) guyanensis, L. (L.) amazonensis, or L. (L.) major (>1.5) [18, 24, 25]. ABCC7 is shown to confer pentamidine resistance in the promastigote and amastigote form of L. (L.) major and is cross-resistant to trivalent antimonial drugs when overexpressed [26,27,28].
The ABCG family includes the ABCG4 and ABCG6 proteins. ABCG4, localized mainly to the parasite plasma membrane, reduced the accumulation of phosphatidylcholine analogs and conferred resistance to alkyl-phospholipids (miltefosine (MIL), edelfosine, and perifosine) when overexpressed. The second ABCG reported, ABCG6, also localized mainly to the parasite plasma membrane, confers resistance to MIL and sitamaquine when overexpressed in L. (L.) infantum [29]. ABCG6 confers also resistance to camptothecin and arsenite [30].
The inhibition of the activity of ABC proteins represents an interesting way to control drug resistance. This concept of inhibiting ABC transporters is well studied for malaria [31,32,33]. Leishmania parasites overexpressing ABCG2 are resistant to antimony, as they demonstrate a reduced accumulation of SbIII due to an increase in drug efflux [34].
2 Transporter Inhibitors and Modulators of Multidrug Resistance
A number of compounds, e.g., calcium channel blockers, calmodulin antagonists, hydrophobic peptides, protein kinase inhibitors, antibiotics, hormone derivatives, and flavonoids, have been previously described to reverse in vitro multidrug resistance in mammalian cells [35]. They are called modulators or chemosensitizers; those that reverse the multidrug-resistant phenotype in Leishmania spp. are listed in Table 14.2.
2.1 Calcium Channel Blockers: Verapamil
Some of these compounds, like the L-type voltage-gated channel blocker verapamil, are known to efficiently overcome multidrug-resistant phenotype in vitro, not only in mammalian cells [54,55,56] but also in some bacteria such as Mycobacterium spp. [57, 58] or Enterococcus spp. [59] and in parasites such as nematodes like Haemonchus contortus [60,61,62] and protozoa like Entamoeba histolytica [63,64,65] or Plasmodium falciparum [66,67,68]. Verapamil is an inhibitor of the human Pgp (ABCB1) [69].
Previous studies have demonstrated that verapamil increases the in vitro antimony activity on L. (L.) donovani [36]. Verapamil shows efficacy in reversing several P-glycoprotein and MRP overexpression-mediated arsenite resistance phenotype in L. (S.) tarentolae or L. (L.) donovani [30, 38]. The reversion of in vitro drug resistance by verapamil is confirmed in L. (L.) donovani clinical isolates resistant to sodium stibogluconate [70]. This drug partially reverses the resistance in vinblastine-resistant L. (L.) amazonensis, which show cross-resistance to adriamycin [13]. The energy-dependent efflux of pirarubicin, an anthracycline derivative, is inhibited by verapamil in L. (V.) braziliensis, L. (V.) guyanensis, L. (L.) mexicana, L. (V.) peruviana, and L. (V.) panamensis [39]. However, verapamil cannot revert the resistance to camptothecin, a cytotoxic quinoline alkaloid which inhibits the DNA enzyme topoisomerase-I [30]. Various studies in cancer cell lines reveal that development of resistance to topoisomerase inhibitors is a multifactorial event including altered transport, modified drug metabolism and detoxification, and change in drug-target interaction. Amino acid substitutions in topoisomerase-I confer camptothecin resistance in L. (L.) donovani [71]. The apparent wide substrate specificity of the Leishmania transport system suggests that it could be responsible for the intrinsic resistance of parasite promastigotes to drugs. Its physiological relevance is supported by the fact that it was described in at least five different Leishmania species. It seems that verapamil regulates drug susceptibility by downregulating Pgp expression in arsenical-resistant Leishmania spp. [72]. In tumor cells, the ability of verapamil to modulate multidrug resistance protein 1 (MRP1 or ABCC1)-mediated resistance seems to be link to its effect on the reduced glutathione (GSH) status [73]. In addition to stimulate MRP1-mediated GSH transport, verapamil modulates MRP1-mediated leukotriene C4 transport [74].
Verapamil also enhances pentamidine uptake into resistant L. (L.) mexicana and also partially reverses the drug resistance phenotype in promastigotes [37], but not in axenic amastigotes [75]. In addition, using nontoxic concentrations of verapamil, a dose-dependent reversion of pentamidine is observed in resistant parasites when compared with those not treated with verapamil in L. (L.) amazonensis [27]. However, verapamil has any impact either in drug uptake or drug resistance in L. (L.) donovani [76]. This suggests that Pgp-mediated efflux of pentamidine is not operative in L. (L.) donovani as it is in L. (L.) mexicana or L. (L.) amazonensis. PRP1 (ABCC7) is shown to confer pentamidine resistance in the promastigote and amastigote form of L. (L.) major and in L. (L.) infantum when overexpressed [26, 28], but not in L. (L.) amazonensis [27]. No difference in PRP1 transcript levels is observed between susceptible and resistant L. (L.) donovani parasites to SbV [77].
The specific Pgp inhibitor cyclosporin-A does not interfere with calcein cell retention (efflux measurement) in L. (L.) amazonensis, while verapamil does [78]. These results demonstrate that the drug transport systems expressed in Leishmania are susceptible to MRP (ABCC) inhibitors like verapamil, but not to the Pgp (ABCB) inhibitor like cyclosporin-A.
In addition, it seems that verapamil is ineffective in reverting ABCG6 overexpression-mediated resistance in Leishmania [30].
2.2 Calmodulin Inhibitors: Phenothiazine Derivatives
Phenothiazines and reserpine can also reverse drug resistance in mammalian cells, bacteria, and parasites [79,80,81,82]. Phenothiazine drugs, of which chlorpromazine is the leading molecule, are widely used for their antipsychotic, antianxiety, and antiemetic effects. In addition, they also possess protozoacidal activity against amastigotes and promastigotes of L. (L.) donovani and L. (L.) chagasi in vitro as well as in vivo [83,84,85]. Chlorpromazine is also an inhibitor of the human Pgp (ABCB1) [69].
Chlorpromazine, trifluoropromazine, thioridazine, trifluoperazine, and prochlorperazine are reported to inhibit the energy-dependent efflux of pirarubicin, an anthracycline derivative, in L. (V.) braziliensis, L. (V.) guyanensis, and L. (L.) mexicana [39]. A synergistic effect between chlorpromazine and N-meglumine antimoniate is observed in multidrug-resistant L. (L.) donovani and L. (L.) major cells in vitro [40]. The effect of phenothiazine derivatives on Leishmania drug transport may be explained by their ability to inhibit the activity of trypanothione reductase [86, 87]. Indeed, if we consider that the reduced form of trypanothione is an important co-factor for the function of the Leishmania drug transporter, in the same way as reduced glutathione is required for the MRP1 function [74, 88], phenothiazines may inhibit transport activity by decreasing the intracellular level of reduced trypanothione [39]. However, no significant effect is observed in vivo against amastigotes of L. (L.) major and L. (L.) mexicana, in cutaneous lesions in mice [40]. The toxic effects reported with the most frequently studied phenothiazine, which is chlorpromazine, have impaired the investigation of other phenothiazines as potential clinical agents.
Prochlorperazine and trifluoperazine enhance pentamidine uptake into resistant L. (L.) mexicana and also partially reverse the drug resistance phenotype [37]. However, these drugs have any impact either in drug uptake or drug resistance in L. (L.) donovani [76]. This indicates that Pgp-mediated efflux of pentamidine is not operative in L. (L.) donovani as it is in L. (L.) mexicana, like for verapamil.
2.3 Flavonoids
The flavonoid class is constituted by flavones, flavonols, isoflavones, flavanones, and chacones [89]. More than 6500 different flavonoids have been identified from plant sources.
Flavonoids have shown promise to reverse multidrug-resistant phenotypes in L. (L.) tropica [41, 42, 90, 91]. Flavonoids constitute a well-known class of natural inhibitors of different proteins [92] with contradictory results concerning their modulation effects on different multidrug-resistant cells [93,94,95]. They bind to the two cytosolic NBSs of the ABC transporters. The flavanolignan silybin and its hemisynthetic derivatives exhibit good affinity to NBD2 [96]. The flavonoid interactions with the ATP-binding site and a vicinal hydrophobic region [41, 91, 97] cause the inhibition of drug efflux and reverse the resistance to daunomycin in L. (L.) tropica. Only flavonoids which bind with high affinity to the cytosolic domain NBD2 are able to both increase daunomycin accumulation in a L. (L.) tropica line overexpressing MDR1 (LtrABCB4) and inhibit the parasite growth in the presence of the drug [41]. In addition, flavonoids, such as quercetin a flavone, may modulate the multidrug transporter by decreasing Pgp synthesis and inhibiting the transcriptional activation of the mdr gene involved in the susceptibility to daunomycin [53, 98]. Quercetin is a human Pgp (ABCB1), MRP2 (ABCC2), and BCRP (ABCG2) transporter inhibitor [69, 99]. Quercetin reverts the resistance to camptothecin in L. (L.) donovani that overexpresses LdABCG6 involved in resistance to camptothecin and arsenite [30] and is associated with reduction of accumulation of alkyl-phospholipid drugs such as MIL in Leishmania [29]. Synthetic flavonoid dimmers exhibit a significant reversing activity on pentamidine and sodium stibogluconate resistance in L. (S.) enriettii and L. (L.) donovani [42]. This modulatory effect is dose-dependent and due to the bivalent nature of the flavonoid compounds. Compared to other MDR inhibitors such as verapamil, reserpine, quinine, quinacrine, and quinidine, these compounds are the only agents that can reverse sodium stibogluconate resistance in L. (S.) enriettii. These modulators exhibit reversal activity on pentamidine resistance, comparable to that of reserpine and quinacrine but whatever the level of overexpression of Lemdr1 gene suggesting that these modulators are not specific to LeABCB4 (LeMDR1). Recently, new compounds derived from aurone, flavones, isoflavones, xanthone, chalcones, and trolox were evaluated against antimony-resistant strains of L. (L.) major [43]. Two trolox carboxamides induce reversion of antimony resistance in the promastigote form of L. (L.) major. These two compounds are specific reversal agents targeting the Leishmania ABCI4 transporter. This transporter belongs to an unclassified group of proteins in the ABC family with no known homology with other eukaryotic ABC proteins but with orthologues in Trypanosoma brucei and Trypanosoma cruzi [100]. ABCI4 is a protein located in the plasma membrane and mitochondria of the parasite and efflux antimony. Overexpression of ABCI4 confers resistance to antimony.
2.4 Sesquiterpenes
Agarofuran sesquiterpenes, e.g., natural compounds isolated from Maytenus cuzcoina [101, 102], M. chubutensis [91], M. macroparta [103], M. magellanica [91], M. apurimacensis, [104] and Crossopetalum tonduzii [105], are new promising reversal agents that overcome the multidrug-resistant phenotype in Leishmania, including the resistance to anthracyclines (daunomycin) and alkyl-lysophospholipids (MIL and edelfosine). In L. (L.) tropica, dihydro-β-agarofuran sesquiterpenes enhance accumulation of calcein, a Pgp substrate, probably due to Pgp-like transporter inhibition [91]. These compounds bind to the NBD2 C-terminal of L. (L.) tropica Pgp-like transporter, LtrMDR1 (LtrABCB4) [105]. A series of dihydro-β-agarofuran sesquiterpenes isolated from the leaves of Maytenus cuzcoina or semisynthetic derivatives have been tested on L. (L.) tropica parasites overexpressing Pgp [101]. Three-dimensional quantitative structure-activity relationship using the comparative molecular similarity indices analysis (3D-QSAR/CoMSIA) is employed to characterize the steric, electrostatic, lipophilic, and hydrogen-bond-donor and hydrogen-bond-acceptor requirements of these sesquiterpenes as modulators at Pgp-like transporter. The most salient features of requirements are the H-bond interaction between the substituents at the C-2 and C-6 positions with the receptor. The structure-activity relationship (SAR) suggests that a substituent at the C-2 position seems to be essential for reversal activity in the MDR Leishmania line by acting as a H-bond acceptor. The furan ring at the C-6 position seems to form a hydrogen bond with the receptor. The introduction of a carbonyl group, capable of acting as a H-bond acceptor in the H-bond with the receptor, produces a tenfold higher chemosensitization. This suggests a direct interaction with the receptor. These results would be used to design and synthesize more effective and specific new Pgp inhibitors.
Sesquiterpene C-3 remarkably sensitizes multidrug-resistant parasites to MIL and edelfosine by increasing alkyl-lysophospholipid accumulation [53]. Moreover, mdr1 gene transfections can alter membrane fluidity in mammalian cells and change alkyl-lysophospholipid effects [106, 107].
Nortriterpene, extracted from Maytenus chubutensis and M. magellanica (Celastraceae family), shows only moderate MDR1 reversal activity in a L. (L.) tropica strain overexpressing LtrMDR1, involved in daunomycin resistance [64].
Glycyrrhizic acid, a triterpenoid saponin isolated from the root of the liquorice plant, limits infection with sodium antimony gluconate (SAG)-resistant L. (L.) donovani in combination with SAG treatment [45]. Glycyrrhizic acid enhances antimony retention by inhibition of MRP1 and Pgp expression levels in splenic macrophages from infected mice. Glycyrrhizic acid acts by modulation of host ABC transporters. Glycyrrhizic acid suppresses cell surface expression of MRP1 and Pgp in host macrophages.
2.5 Statins: Lovastatin
Statins, 3-hydroxy-3-methylglutaryl-coenzyme A (HMG-CoA) reductase inhibitors, belong to a family of lipid-lowering drugs that are currently used for the control of hyperlipidemia and are considered useful for protection from cardiovascular events. Apart from the cholesterol-lowering activity of statins, the immunomodulatory and pleiotropic effects of statins may significantly impact infection-related survival [108, 109]. Statins interfered with the growth of protozoan parasites in the Trypanosomatidae family, such as Trypanosoma cruzi and various Leishmania species [110,111,112].
Statins are also inhibitors of Pgp in cancer cells [66, 113, 114]. Additionally, in Plasmodium falciparum, atorvastatin has synergistic effects in combination with antimalarial drugs such as dihydroartemisinin, quinine, or mefloquine [115,116,117]. atorvastatin acts probably by inhibition of MDR-like proteins, which are involved in malaria resistance.. In Leishmania, the combination of the antifungal drug miconazole and lovastatin is synergic in terms of inhibition of promastigote proliferation, macrophage infection, and amastigote number [118]. In promastigote cultures, the effect is more marked in L. (L.) amazonensis parasites than L. (L.) donovani. But it seems that this effect is due to inhibition of sterol biosynthesis by both lovastatin and miconazole. More recently, lovastatin, which can inhibit both Pgp and MRP1 (ABCC1), allows the accumulation of sodium antimony gluconate in resistant L. (L.) donovani and reversion of antimony resistance [46]. Lovastatin can induce not only the retention of antimony compounds but also that of an unrelated chemotherapeutic agent such as doxorubicin in cancer cells.
2.6 Pyridine Analog: PAK-104P
A pyridine analog, PAK-104P, was demonstrated in vitro as well as in vivo to inhibit Pgp-mediated multidrug resistance to vincristine, adriamycin, doxorubicin, paclitaxel, and antimonial and arsenical drugs [119,120,121,122,123,124]. PAK-104P partially reverses the resistance and increases the arsenite accumulation in cancer cells that overexpress MRP1 (ABCC1) [125]. PAK-104P can inhibit both Pgp and MRP [123]. PAK-104P also blocks the energy-dependent efflux of pirarubicin in L. (V.) braziliensis, L. (V.) guyanensis, and L. (L.) mexicana [39]. This compound probably alters the activity of trypanothione reductase and the transport activity by decreasing the intracellular level of reduced trypanothione.
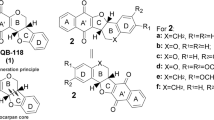
Oxazolo[3,2-α]pyridine derivatives produce a significant reversion of resistance to both MIL and daunomycin in a MDR1 overexpressing L. (L.) tropica strain [47].
2.7 Sulfonylurea: Glibenclamide
Glibenclamide is a sulfonylurea that inhibits ABC proteins such as Pgp (ABCB1) [69, 126] and MRP1 (ABCC1) of cancer cells [127].
Glibenclamide increases calcein accumulation in L. (L.) amazonensis-resistant line, like verapamil [78]. Cyclosporin-A, which is a specific inhibitor of Pgp, doesn’t increase calcein accumulation. These results demonstrate that the drug transport systems expressed in L. (L.) amazonensis are susceptible to MRP (ABCC) inhibitors like glibenclamide or verapamil, but not to the Pgp (ABCB) inhibitor like cyclosporin-A. The increased expression of MRP1 (ABCC1) at the plasma membrane of the protoplast of Arabidopsis thaliana is associated with an increase in the resistance of Arabidopsis to SbIII and a decrease of SbIII accumulation in protoplast [128]. The simultaneous administration in vitro of glibenclamide, a human MRP1 (ABCC1) inhibitor, increases the efficacy of Glucantime and decreases the infection rate of infected macrophages by L. (L.) major [49]. A fixed concentration of 50 μM glibenclamide in combination with various concentration of Glucantime caused an inhibition of 80–90% in cell growth. The administration of glibenclamide in experimental in vivo settings increases the potency of Glucantime when administered simultaneously and reduces the size of lesions in mice infected with drug-susceptible and drug-resistant Leishmania [48]. The Glucantime-glibenclamide combination could represent a novel strategy to fight against Leishmania infection.
2.8 Acridonecarboxamide Derivatives: Elacridar and Zosuquidar
Acridonecarboxamide derivatives, elacridar (LY335979) and zosuquidar (GF120918), modulators of human P-glycoprotein [129, 130], can overcome Pgp (LtrMDR1 or LtrABCB4)-mediated Leishmania MIL resistance by increasing intracellular MIL accumulation [131]. Overexpression of LtrABCB4 is involved in MIL resistance [59]. In addition, ABCG4, localized mainly to the parasite plasma membrane, reduced the accumulation of phosphatidylcholine analogs and conferred resistance to alkyl-phospholipids (MIL, edelfosine, and perifosine) when overexpressed [132]. The second ABCG reported, ABCG6, also localized mainly to the parasite plasma membrane, conferred resistance to MIL and sitamaquine when overexpressed in L. (L.) infantum [29]. Overexpression of ABCG6 is associated with reduction of accumulation of alkyl-phospholipid drugs into Leishmania.
2.9 Dithiocarbamate: Disulfiram
Disulfiram (Antabuse) is used as an adjunct in the treatment of chronic alcoholism. Disulfiram is able to potentiate the antimalarial action of subcurative doses of chloroquine and amodiaquine in Plasmodium berghei- and P. vinckei petteri-infected mice [133]. Disulfiram inhibits P-glycoproteins by covalently modifying one or more endogenous cysteine residues (Cys1074) in NBD2 [134]. Modification of only one of the Walker A cysteines is sufficient to inactive Pgp [135]. This drug could be effective in combination with Glucantime [136].
2.10 Benzoquinones
Bis-pyranobenzoquinones inhibit the activity of Pgp of mammalian cells but not MRP1 (ABCC1) [50]. In addition, these compounds increase the activity of daunorubicin in resistant L. tropica line. Bis-pyrano-1,4-benzoquinones are the best modulators in MDR human cancer cells, while bis-pyrano-1,2-benzoquinones exhibit the higher toxicity in combination with daunorubicin in MDR L. (L.) tropica line.
2.11 Quinacrine
Quinacrine is an acridine derivative with antimalarial, antileishmanial, and antitrypanosomal activities [137,138,139].
Quinacrine can have a synergistic effect in combination with pentamidine in L. (M.) enriettii and in L. (L.) donovani [42, 51]. Moreover, quinacrine is only effective in the pentamidine-resistant Leishmania, not in the sodium stibogluconate-resistant or vinblastine-resistant parasites [42]. Surprisingly, quinacrine not only restores the susceptibility of resistant parasites to pentamidine but also increases the susceptibility of susceptible parasites. This result suggests that the quinacrine target remains unaltered in susceptible and resistant parasites to pentamidine. Whatever the quinacrine target might be, it cannot be an ABC transporter in Leishmania.
2.12 8-Aminoquinolines: Sitamaquine
Sitamaquine (WR6026), an 8-aminoquinoline analog, overcomes the MDR1-mediated resistance to MIL by increasing intracellular MIL accumulation in a L. (L.) tropica strain overexpressing MDR1 and resistant to MIL [52]. Additionally, sitamaquine also modulates the activity of MRPA, involved in antimony resistance, in resistant L. (L.) tropica strain. Sitamaquine reverses MRPA-mediated resistance to antimony.
3 Conclusion and Future Trends
Efflux transporters play a key role in the emergence and dissemination of resistant parasites and in the acquisition of additional mechanisms of drug resistance caused by a decrease in intracellular drug concentration. Despite their noticeable divergence in structure and membrane topology, the major efflux systems share a dependence on specific key parameters including (1) the functional assembly of a membrane transporter, (2) the energy required (e.g., ATP, ion antiport, or membrane potential) for active transport, and (3) the presence of affinity sites inside the transporter that are involved in substrate recognition and transport.
The identification of functional domains and the characterization of various interactions with the transported drug may elucidate key parameters that govern efflux activity. At present, some 3D structures have been solved for bacterial drug transporters, and these have allowed the proposal of dynamic and mechanical models for drug transport [140]. The same approach must be used for Leishmania infection. Drug-transporter interactions have recently been shown to be an important part of multidrug resistance. In silico modeling is a powerful tool often employed to predict drug properties prior to in vitro and in vivo studies. Modeling efforts are currently being undertaken using both ligand- and transporter-based methods such as structure-activity relationship (SAR) studies, quantitative-SAR (QSAR) studies, hologram QSAR (HQSAR), comparative molecular field analysis (CoMFA) and comparative molecular similarity index analysis (CoMSIA) studies, pharmacophore modeling, homology modeling, and molecular dynamics studies. The most common approaches to discover human ABC substrates and inhibitors are development of QSAR models and SAR. This approach has been carried out in the case of human ATP-transporter multidrug resistance-associated protein 2 (MRP2 or ABCC2) [141]. The goal of QSAR modeling is to construct a mathematical relationship between descriptors and pharmacological activities of compounds. The model can then be used to predict the activity for an untested compound. The goal of SAR is usually to discern the structural features or side groups that directly lead to the desired activity under investigation. In order to use these in silico modeling techniques, compounds need to be screened to find the degree of substrate binding to inhibition. Until now, there are no or very few inhibitors or substrate datasets available for ABC transporters in Leishmania in literature. Some compounds with inhibitory effects toward human ABCB1 (Pgp) and ABCC1 (MRP1) transporters were studied by pharmacophore modeling, docking, and 3D QSAR to described the binding preferences of these proteins [142]. Docking of selective inhibitors into the Pgp binding cavity by the use of a structural model based on the recently resolved Pgp structure confirms the Pgp pharmacophore features identified and reveals the interactions of some functional groups and atoms in the structures with particular protein residues. However, due to the complex nature of the applied methods, useful interpretation of the models that can be directly translated into chemical structures by the medicinal chemist is rather difficult.
The aim of these efforts is to decipher the molecular basis of drug transport, to explain how differences in chemical structures modify interactions with the transporter, or to elucidate how the transporter functions in general. In addition, original molecules have been demonstrated to restore the antileishmanial activity of drugs that are pump substrates, and these studies make it possible to identify pharmacophoric groups that are involved in efflux inhibition.
These data are crucial for the design of (1) new antileishmanial molecules that are devoid of efflux-substrate characteristics and can reach a normal intracellular accumulation level and (2) new compounds that have strong efflux pump affinity associated with a high inhibitor capability and block the pump, restoring the intracellular concentration of antileishmanial drugs.
The most prevalent mechanisms of resistance in Leishmania are mutations of proteins involved in the drug transport (uptake or efflux) and amplification of transporter genes. The role of ABC transporters in drug resistance in Leishmania is well established. Several modulators have been described to reverse multidrug resistance in vitro in Leishmania. Most of these drugs remain to be evaluated in vivo. Hence, clinical evaluation of therapeutic regimens is now required to validate the efficacy of these promising compounds or combinations for the treatment of leishmaniasis.
Another perspective is to modulate proteins which participate to the regulation of the expression of the level of MDR1 in Leishmania. Silent information regulator 2 (Sir2) is involved in Leishmania survival by preventing programmed cell death [143]. Sir2 plays a role in regulating the expression of MDR1 and thereby amphotericin-B (AMB) efflux from the resistant L. (L.) donovani [144]. Inhibition or deletion of Sir2 allele shows decreased expression levels of MDR1 and lower efflux of AMB in resistant parasites. In contrast, Sir2 overexpression in susceptible parasites leads to resistant phenotype associated with reduced activity of AMB, increased drug efflux, and increased mRNA level of MDR1. Sir2 will be used as a potent drug target for Leishmania treatment.
References
Faraut-Gambarelli F, Piarroux R, Deniau M, Giusiano B, et al. In vitro and in vivo resistance of Leishmania infantum to meglumine antimoniate: a study of 37 strains collected from patients with visceral Leishmaniasis. Antimicrob Agents Chemother. 1997;41:827–30.
Jackson JE, Tally JD, Ellis WY, Mebrahtu YB, et al. Quantitative in vitro drug potency and drug susceptibility evaluation of Leishmania spp. from patients unresponsive to pentavalent antimony therapy. Am J Trop Med Hyg. 1990;43:464–80.
Sundar S, More DK, Singh MK, Singh VP, et al. Failure of pentavalent antimony in visceral Leishmaniasis in India: report from the center of the Indian epidemic. Clin Infect Dis. 2000;31:1104–7.
Ambudkar SV, Rosen BP, Gottesman MM. Workshop on ABC transporters and human diseases. Drug Resist Update. 2000;3:51–4.
Lage H. ABC-transporters: implications on drug resistance from microorganisms to human cancers. Int J Antimicrob Ag. 2003;22:188–99.
Rubio JP, Cowman AF. The ATP-binding cassette (ABC) gene family of Plasmodium falciparum. Parasitol Today. 1996;12:135–40.
Schuetzer-Muehlbauer M, Willinger B, Egner R, Ecker G, et al. Reversal of antifungal resistance mediated by ABC efflux pumps from Candida albicans functionally expressed in yeast. Int J Antimicrob Ag. 2003;22:291–300.
Sparreboom A, Danesi R, Ando Y, Chan J, et al. Pharmacogenomics of ABC transporters and its role in cancer chemotherapy. Drug Resist Update. 2003;6:71–84.
Araujo-Santos JM, Parodi-Talice A, Castanys S, Gamarro F. The overexpression of an intracellular ABCA-like transporter alters phospholipid trafficking in Leishmania. Biochem Biophys Res Commun. 2005;330:349–55.
Chiquero MJ, Perez-Victoria JM, O’Valle F, Gonzales-Ros JM, et al. Altered drug membrane permeability in a multidrug-resistant Leishmania tropica line. Biochem Pharmacol. 1998;55:131–9.
Chow LM, Wong AK, Ullman B, Wirth DF. Cloning and functional analysis of an extrachromosomally amplified multidrug resistance-like gene in Leishmania enriettii. Mol Biochem Parasitol. 1993;60:195–208.
Gamarro F, Chiquero MJ, Amador MV, Lagare D, et al. P-glycoprotein overexpression in methotrexate-resistant Leishmania tropica. Biochem Pharmacol. 1994;47:1939–47.
Gueiros-Filho FJ, Viola JPB, Gomes FCA, Farina M, et al. Leishmania amazonensis: multidrug resistance in vinblastine-resistant promastigotes is associated with rhodamine 123 efflux, DNA amplification, and RNA overexpression of a Leishmania mdr1 gene. Exp Parasitol. 1995;81:480–90.
Henderson DM, Sifri CD, Rodgers M, Wirth DF, et al. Multidrug resistance in Leishmania donovani is conferred by amplification of a gene homologous to the mammalian mdr1 gene. Mol Cell Biol. 1992;12:2855–65.
Katakura K, Iwanami M, Ohtomo H, Fujise H, et al. Structural and functional analysis of the LaMDR1 multidrug resistance gene in Leishmania amazonensis. Biochem Biophys Res Commun. 1999;255:289–94.
Mary C, Faraut F, Deniau M, Dereure J, et al. Frequency of drug resistance gene amplification in clinical Leishmania strains. Int J Microbiol. 2010;2010:819060.
Wong ILK, Chow LMC. The role of Leishmania enriettii multidrug resistance protein 1 (LeMDR1) in mediating drug resistance is iron-dependent. Mol Biochem Parasitol. 2006;150:278–87.
Moreira DS, Monte Neto RL, Andrade JM, Santi AMM, et al. Molecular characterization of the MRPA transporter and antimony uptake in four new world Leishmania spp. susceptible and resistant to antimony. Int J Parasitol Drugs Drugs Resist. 2013;3:143–53.
Borst P, Ouellette M. New mechanisms of drug resistance in parasitic protozoa. Annu Rev Microbiol. 1995;49:427–60.
Chow LMC, Volkman K. Plasmodium and Leishmania: the role of mdr genes in mediating drug resistance. Exp Parasitol. 1998;90:135–41.
El Fadili K, Messier N, Leprohon P, Roy G, et al. Role of the ABC transporter MRPA (PGPA) in antimony resistance in Leishmania infantum axenic and intracellular amastigotes. Antimicrob Agents Chemother. 2005;49:1988–93.
Ouellette M, Legare D, Papadopoulou B. Multidrug resistance and ABC transporters in parasitic protozoan. J Mol Microbiol Biotechnol. 2001;3:201–6.
Leprohon P, Legare D, Ouellette M. Intracellular localization of the ABCC proteins of Leishmania and their role in resistance to antimonials. Antimicrob Agents Chemother. 2009;53:2646–9.
Rai S, Goel SK, Dwivedi UN, Sundar S, et al. Role of efflux pumps and intracellular thiols in natural antimony resistant isolates of Leishmania donovani. PLoS One. 2013;8:74862.
Soleimanifard S, Arjmand R, Saberi S, Khamesipour A, et al. P-glycoprotein a gene expression in glucantime-resistant and sensitive Leishmania major (MRHO/IR/75/ER). Iranian. J Parasitol. 2014;9:423–8.
Coelho AC, Beverley SM, Cotrim PC. Functional genetic identification of PRP1, an ABC transporter superfamily member conferring pentamidine resistance in Leishmania major. Mol Biochem Parasitol. 2003;130:83–90.
Coelho AC, Gentil LG, Franco da Silveira J, Cotrim PC. Characterization of Leishmania (Leishmania) amazonensis promastigotes resistant to pentamidine. Exp Parasitol. 2008;120:98–102.
Coelho AC, Messier N, Ouellette M, Cotrim PC. Role of the ABC transporter PRP1 (ABCC7) in pentamidine resistance in Leishmania amastigotes. Antimicrob Agents Chemother. 2007;51:3030–2.
Castanys-Munoz E, Perez-Victoria JM, Gamarro F, Castanys S. Characterization of an ABCG-like transporter from the protozoan parasite Leishmania with a role in drug resistance and transbilayer lipid movement. Antimicrob Agents Chemother. 2008;52:3573–9.
Bose Dasgupta S, Ganguly A, Roy A, Mukherjee T, et al. A novel ATP-binding cassette transporter, ABCG6 is involved in chemoresistance in Leishmania. Mol Biochem Parasitol. 2008;158:176–88.
Alibert-Franco S, Pradines B, Mahamoud A, Davin-Regli A, et al. Efflux mechanism, an attractive target to combat Plasmodium falciparum and Pseudomonas aeruginosa. Curr Med Chem. 2009;16:301–17.
Henry M, Alibert S, Orlandi-Pradines E, Bogreau H, et al. Chloroquine resistance reversal agents as promising antimalarial drugs. Curr Drug Targets. 2006;7:935–48.
Henry M, Alibert S, Rogier C, Barbe J, et al. Inhibition of efflux of quinolines as new therapic strategy in malaria. Curr Top Med Chem. 2008;8:563–78.
Perea A, Manzano JI, Castanys S, Gamarro F. The LABCG2 transporter from the protozoan parasite Leishmania is involved in antimony resistance. Antimicrob Agents Chemother. 2016;60:3489–96.
Stein WD. Reversers of the multidrug resistance transporter P-glycoprotein. Curr Opin Investig Drugs. 2002;3:812–7.
Neal RA, van Bueren J, McCoy NG, Iwobi M. Reversal of drug resistance in Trypanosoma cruzi and Leishmania donovani by verapamil. Trans R Soc Trop Med Hyg. 1989;83:197–8.
Basselin M, Denise H, Coombs GH, Barrett MP. Resistance to pentamidine in Leishmania mexicana involves exclusion of the drug from the mitochondrion. Antimicrob Agents Chemother. 2002;46:3731–8.
Dey S, Papadopoulou B, Haimeur A, Roy G, et al. High level arsenite resistance in Leishmania tarentolae is mediated by an active extrusion system. Mol Biochem Parasitol. 1994;67:49–57.
Essodaïgui M, Frézard F, Moreira ESA, Dagger F, et al. Energy-dependent efflux from Leishmania promastigotes of substrates of the mammalian multidrug resistance pumps. Mol Biochem Parasitol. 1999;100:73–84.
el-On J, Rubinstein N, Kernbaum S, Schnur LF. In vitro and in vivo anti-leishmanial activity of chlorpromazine alone and combined with N-meglumine antimonate. Ann Trop Med Parasitol. 1986;80:509–17.
Perez-Victoria JM, Chiquero MJ, Conseil G, Dayan G, et al. Correlation between the affinity of flavonoids binding to the cytosolic site of Leishmania tropica multidrug transporter and their efficiency to revert parasite resistance to daunomycin. Biochemistry. 1999;38:1736–43.
Wong ILK, Chan KF, Burkett BA, Zhao Y, et al. Flavonoid dimmers as bivalent modulators for pentamidine and sodium stibogluconate resistance in Leishmania. Antimicrob Agent Chemother. 2007;51:930–40.
Manzano JI, Lecerf-Schmidt F, Lespinasse MA, Di Pietro A, et al. Identification of specific reversal agents for Leishmania ABCI4-mediated antimony resistance by flavonoid and trolox derivatives screening. J Antimicrob Agents. 2014;69:664–72.
Kennedy ML, Lianos GG, Castanys S, Gamarro F, et al. Terpenoids from Maytenus species and assessment of their reversal activity against a multidrug-resistant Leishmania tropica line. Chem Biodivers. 2011;8:2291–8.
Bhattacharjee A, Majumder S, Majumdar SB, Choudhuri SK, et al. Co-administration of glycyrrhizic acid with the antileishmanial drug sodium antimony gluconate (SAG) cures SAG-resistant visceral leishmaniasis. Int J Antimicrob Agents. 2015;45:268–77.
Mookerjee Basu J, Mookerjee A, Banerjee R, Saha M, et al. Inhibition of ABC transporters abolished antimony resistance in Leishmania infection. Antimicrob Agents Chemother. 2008;52:1080–93.
Caballero E, Manzano JI, Puebla P, Castanys S, et al. Oxazolo[3,2-]pyridine. A new structural scaffold for the reversal of multi-drug resistance in Leishmania. Bioorg Med Chem Lett. 2012;22:6272–5.
Serrano-Martin X, Payares G, Mendoza-Leon A. Glibenclamide, a blocker of K+ATP channels, shows antilesihmanial activity in experimental murine cutaneous leishmaniasis. Antimicrob Agents Chemother. 2006;50:4214–6.
Padron-Nieves M, Diaz E, Machuca C, Romero A, et al. Glibenclamide modulates glucantime activity and disposition in Leishmania major. Exp Parasitol. 2009;121:331–7.
Jimenez-Alonso S, Perez-Lomas AL, Estevez-Braun A, Munoz Martinez F, et al. Bis-pyranobenzoquinones as a new family of reversal agents of the multidrug resistance phenotype mediated by P-glycoprotein in mammalian cells and the protozoan parasite Leishmania. J Med Chem. 2008;51:7132–43.
Wong ILK, Chan KF, Zhao Y, Hang Chan T, et al. Quinacrine and a novel apigenin dimmer can synergistically increase the pentamidine susceptibility of the protozoan parasite Leishmania. J Antimicrob Chemother. 2009;63:1179–90.
Perez-Victoria JM, Bavchvarov BI, Torrecillas IR, Martinez-Garcia M, et al. Sitamaquine overcomes ABC-mediated resistance to miltefosine and antimony in Leishmania. Antimicrob Agents Chemother. 2011;55:3838–44.
Perez-Victoria JM, Perez-Victoria FJ, Parodi-Talice A, Jimenez IA, et al. Alkyl-lysophospholipid resistance in multidrug-resistant Leishmania tropica and chemosensitization by a novel P-glycoprotein-like transporter modulator. Antimicrob Agents Chemother. 2001;45:2468–74.
Tsuruo T, Iida H, Tsukagoshi S, Sakurai Y. Overcoming of vincristine resistance in P388 leukemia in vivo and in vitro through enhanced cytotoxicity of vincristine and vinblastine by verapamil. Cancer Res. 1981;41:1967–72.
Tsuruo T, Iida H, Tsukagoshi S, Sakurai Y. Potentiation of vincristine and adriamycin effects in human hemopoietic tumor cell lines by calcium antagonists and calmodulin inhibitors. Cancer Res. 1983;43:2267–72.
Twentyman PR, Fox NE, Bleehen NM. Drug resistance in human lung cancer cell lines: cross-resistance studies and effects of the calcium transport blocker, verapamil. J Radiat Oncol Biol Phys. 1986;12:1355–8.
Banerjee SK, Bhatt K, Rana S, Misra P, et al. Involvement of an efflux system in mediating high level of fluoroquinolone resistance in Mycobacterium smegmatis. Biochem Biophys Res Commun. 1996;226:362–8.
Choudhuri BS, Bahkta S, Barik R, Basu J, et al. Overexpression and functional characterization of an ABC (ATP-binding cassette) transporter encoded by the genes drrA and drrB of Mycobacterium tuberculosis. Biochem J. 2002;367:279–85.
Jonas BM, Murray BE, Weinstock GM. Characterization of emeA, a NorA homolog and multidrug resistance efflux pump, in Enterococcus faecalis. Antimicrob Agents Chemother. 2001;45:3574–9.
Beugnet F, Gauthey M, Kerboeuf D. Partial in vitro reversal of benzimidazole resistance by the free-living stages of Haemonchus contortus with verapamil. Vet Rec. 1997;141:575–6.
Kerboeuf D, Blackhall W, Kaminsky R, von Samson-Himmelstjerna G. P-glycoprotein in helminths: function and perspectives for antihelminthic treatment and reversal of resistance. Int J Antimicrob Agents. 2003;22:332–46.
Kerboeuf D, Chambrier P, Le Vern Y, Aycardi J. Flow cytometry analysis of drug transport mechanisms in Haemonchus contortus susceptible or resistant to antihelminthics. Parasitol Res. 1999;85:118–23.
Ayala P, Samuelson J, Wirth D, Orozco E. Entamoeba histolytica: physiology of multidrug resistance. Exp Parasitol. 1990;71:169–75.
Banuelos C, Orozco E, Gomez C, Gonzales A, et al. Cellular location and function of the P-glycoprotein (EhPgp) in Entamoeba histolytica multidrug-resistant trophozoites. Microb Drug Resist. 2002;8:291–300.
Orozco E, Lopez C, Gomez C, Perez DG, et al. Multidrug resistance in the protozoan parasite Entamoeba histolytica. Parasitol Int. 2002;51:353–9.
Holtzman CW, Wiggings BS, Spinler SA. Role of P-glycoprotein in statin drug interaction. Pharmacotherapy. 2006;26:1601–7.
Millet J, Torrentino-Madamet M, Alibert S, Rogier C, et al. Dihydroethanoanthracene derivatives as in vitro malarial chloroquine resistance reversal agents. Antimicrob Agents Chemother. 2004;48:2753–6.
Pradines B, Alibert-Franco S, Houdoin C, Mosnier J, et al. In vitro reversal of chloroquine resistance in Plasmodium falciparum with dihydroethanoanthracene derivatives. Am J Trop Med Hyg. 2002;66:661–6.
Matsson P, Pedersen JM, Norinder U, Bergstrom CAS, et al. Identification of novel specific and general inhibitors of the three major human ATP-binding cassette transporters, P-gp, BCRP and MRP2 among registered drugs. Pharm Res. 2009;26:1816–31.
Valiathan R, Dubey ML, Mahajan RC, Malla N. Leishmania donovani: effect of verapamil on in vitro susceptibility of promastigote and amastigote stages of Indian clinical isolates to sodium stibogluconate. Exp Parasitol. 2006;114:103–8.
Marquis JF, Hardy I, Olivier M. Topoisomerase I amino acid substitutions, Gly185Arg and Asp325Glu, confer camptothecin resistance in Leishmania donovani. Antimicrob Agents Chemother. 2005;49:1441–6.
Kaur J, Dey CS. Putative P-glycoprotein expression in arsenite-resistant Leishmania donovani down-regulated by verapamil. Biochem Biophys Res Commun. 2000;271:615–9.
Loe DW, Deeley RG, Cole SPC. Verapamil stimulates glutathione transport by the 190-kDa multidrug resistance protein 1 (MRP1). J Pharmacol Exp Ther. 2000;293:530–8.
Loe DW, Oleschuk CJ, Deeley RG, Cole SPC. Structure-activity studies of verapamil analogs that modulate transport of Leukotriene C4 and reduced glutathione by multidrug resistance protein MRP1. Biochem Biophys Res Commun. 2000;275:795–803.
Sereno D, Lemesre JL. In vitro life cycle of pentamidine-resistant amastigotes: stability of the chemoresistant phenotypes is dependent on the level of resistance induced. Antimicrob Agents Chemother. 1997;41:1898–903.
Mukherjee A, Padmanabhan PK, Sahani MH, Barrett MP, et al. Roles for mitochondria in pentamidine susceptibility and resistance in Leishmania donovani. Mol Biochem Parasitol. 2006;145:1–10.
Decuypere S, Rijal S, Yardley V, De Doncker S, et al. Gene expression analysis of the mechanism of natural Sb(V) resistance in Leishmania donovani isolates from Nepal. Antimicrob Agents Chemother. 2005;49:4616–21.
Machuca C, Rodriguez A, Herrera M, Silva S, et al. Leishmania amazonensis: metabolic adaptations induced by resistance to an ABC transporter blocker. Exp Parasitol. 2006;114:1–9.
Ford JM, Prozialeck WC, Hait WN. Structural features determining activity of phenothiazines and related drugs for inhibition of cell growth and reversal of multidrug resistance. Mol Pharmacol. 1989;35:105–15.
Henry M, Alibert S, Baragatti M, Mosnier J, et al. Dihydroethanoanthracene derivatives reverse in vitro quinoline resistance in Plasmodium falciparum malaria. Med Chem. 2008;4:426–37.
Molnar J, Hever A, Falka I, Ocsovski I, et al. Inhibition of the transport function of membrane proteins by some substituted phenothiazines in E. coli and multidrug resistant tumor cells. Anticancer Res. 1997;17:481–6.
Pearce HL, Safa AR, Bac NJ, Winter MA, et al. Essential features of the P-glycoprotein pharmacophore as defined by a series of reserpine analogs that modulate multidrug resistance. Proc Natl Acad Sci U S A. 1989;86:5128–32.
Pearson RD, Manian AA, Hall D, Harcus JL, et al. Antileishmanial activity of chlorpromazine. Antimicrob Agents Chemother. 1984;25:571–4.
Pearson RD, Manian AA, Harcus JL, Hall D, et al. Lethal effect of phenothiazine neuroleptics on the pathogenic protozoan Leishmania donovani. Science. 1982;217:369–71.
Werbovetz KA, Lehnert EK, MacDonald TL, Pearson RD. Cytotoxicity of acridine compounds for Leishmania promastigotes in vitro. Antimicrob Agents Chemother. 1992;36:495–7.
Chan C, Yin H, Garforth J, McKie JH, et al. Phenothiazines inhibitors of trypanothione reductase as potential antitrypanosomal and antileishmanial drugs. J Med Chem. 1998;41:148–56.
Khan MO, Austin SE, Chan C, Yin H, et al. Use of an additional hydrophobic binding site, the Z site, in the rational design of a new class of stronger trypanothione reductase inhibitor, quaternary alkylammonium phenothiazines. J Med Chem. 2000;43:3148–56.
Loe DW, Stewart RK, Massey TE, Deeley RG, et al. ATP-dependent transport of aflatoxin B1, and its glutathione conjugates by the product of the multidrug resistance protein (MRP) gene. Mol Pharmacol. 1997;51:1034–41.
di Pietro A, Conseil G, Perez-Victoria JM, Dayan G, et al. Modulation by flavonoids of cell multidrug resistance mediated by P-glycoprotein and related ABC transporters. Cell Mol Life Sci. 2002;59:307–22.
Kennedy ML, Cortes F, Pinero JE, Castanys S, et al. Leishmanicidal and reversal multidrug resistance constituents from Aeonium lindleyi. Planta Med. 2011;77:77–80.
Kennedy ML, Cortés-Selva F, Perez-Victoria JM, Jimenez IA, et al. Chemosensitization of a multidrug-resistant Leishmania tropica line by new sesquiterpenes from Maytenus magellanica and Maytenus chubutensis. J Med Chem. 2001;44:4668–76.
Shapiro AB, Ling V. Effect of quercetin on Hoechst 33342 transport by purified and reconstituted P-glycoprotein. Biochem Pharmacol. 1997;53:587–96.
Critchfield JW, Welsh CJ, Phang JM, Yeh GC. Modulation of adriamycin accumulation and efflux by flavonoids in HCT-15 colon cells. Activation of P-glycoprotein as a putative mechanism. Biochem Pharmacol. 1994;48:1437–45.
Ferté J, Kühnel JM, Chapuis G, Rolland Y, et al. Flavonoid-related modulators of multidrug resistance: synthesis, pharmacological activity, and structure-activity relationships. J Med Chem. 1999;42:478–89.
Shapiro AB, Ling V. Positively cooperative sites for drug transport by P-glycoprotein with distinct drug specificities. Eur J Biochem. 1997;250:130–7.
Maitrejean M, Comte G, Barron D, El Kirat K, et al. The flavanolignan silybin and its hemisynthetic derivatives, a novel series of potential modulators of P-glycoprotein. Bioorg Med Chem Lett. 2000;10:157–60.
Conseil G, Baubichon-Cortay H, Dayan G, Jault JM, et al. Flavonoids: a class of modulators with bifunctional interactions at vicinal ATP- and steroid-binding sites on mouse P-glycoprotein. Proc Natl Acad Sci U S A. 1998;95:9831–6.
Kioka N, Hosokawa N, Komano T, Hirayoshi K, et al. Quercetin, a bioflavonoid, inhibits the increase of human multidrug resistance gene (MDR1) expression caused by arsenite. FEBS Lett. 1992;301:307–9.
Yoshikawa M, Ikegami Y, Sano K. Transport of SN-38 by the wild type of human ABC transporter ABCG2 and its inhibition by quercetin, a natural flavonoid. J Exp Ther Oncol. 2004;4:25–35.
Manzano JI, Garcia-Hernandez R, Castanys S, Gamarro F. A new ABC half-transporter in Leishmania is involved in resistance to antimony. Antimicrob Agents Chemother. 2013;57:3719–30.
Cortes-Selva F, Campillo M, Reyes CP, Jimenez IA, et al. SAR studies of dihydro-beta-agarofuran sesquiterpenes as inhibitors of the multidrug-resistance phenotype in a Leishmania tropica line overexpressing a P-glycoprotein-like transporter. J Med Chem. 2004;47:576–87.
Cortes-Selva F, Munoz-Martinez F, Ilias A, Jimenez IA, et al. Functional expression of a multidrug P-glycoprotein transporter of Leishmania. Biochem Biophys Res Commun. 2005;329:502–7.
Cortes-Selva F, Jimenez IA, Munoz-Martinez F, Campillo M, et al. Dihydro-beta-agarofuran sesquiterpenes: a new class of reversal agents of the multidrug resistance phenotype mediated by P-glycoprotein in the protozoan parasite Leishmania. Curr Pharm Des. 2005;11:3125–39.
Delgado-Mendez P, Herrera N, Chavez H, Estevez-Braun A, et al. New terpenoids from Maytenus apurimacensis as MDR reversal agents in the parasite Leishmania. Bioorg Med Chem. 2008;16:1425–30.
Perez-Victoria JM, Tincusi BM, Jimanez IA, Bazzocchi IL, et al. New natural sesquiterpenes as modulators of daunomycin resistance in a multidrug-resistant Leishmania tropica line. J. Med Chem. 1999;42:4388–93.
Callaghan R, van Gorkom LC, Epand RM. A comparison of membrane properties and composition between cell lines selected and transfected for multi-drug resistance. Br J Cancer. 1992;66:781–6.
Storme GA, Berdel WE, van Blitterswijk WJ, Bruyneel EA, et al. Antiinvasive effect of racemic 1-O-octadecyl-2-O-methylglycero-phosphocholine on MO4 mouse fibrosarcoma cells in vitro. Cancer Res. 1985;45:351–7.
Greenwood J, Mason JC. Statins and the vascular endothelial inflammatory response. Trends Immunol. 2007;28:88–98.
Terblanche M, Almog Y, Rosenson RS, Smith TS, et al. Statins: panacea for sepsis? Lancet Infect Dis. 2006;6:242–8.
Montalvetti A, Pena-Diaz J, Hurtado R, Ruiz-Perez LM, et al. Characterization and regulation of Leishmania major 3-hydroxy-methyl-glutaryl—CoA reductase. Biochem J. 2000;349:27–34.
Urbina JA, Lazardi K, Marchan E, Visbal G, et al. Mevinolin (lovastatin) potentiates the antiproliferative effects of ketoconazole and terbinafine against Trypanosoma (Schizotrypanum) cruzi: in vitro and in vivo studies. Antimicrob Agents Chemother. 1993;37:580–91.
Yokoyama K, Trobridge P, Buckner FS, Scholten J, et al. The effects of protein farnesyltransferase inhibitors on trypanosomatids: inhibition of protein farnesylation and cell growth. Mol Biochem Parasitol. 1998;94:87–97.
Wang E, Casciano CN, Clement RP, Johnson WW. HMG-CoA reductase inhibitors (statins) characterized as direct inhibitors of P-glycoprotein. Pharm Res. 2001;18:800–6.
Wu X, Whitfield I, Stewart BH. Atorvastatin transport in the Caco-2 cell model: contributions of P-glycoprotein and the proton-monocarboxylic acid co-transporter. Pharm Res. 2000;17:209–15.
Parquet V, Henry M, Wurtz N, Dormoi J, et al. Atorvastatin as a potential anti-malarial drug: in vitro synergy in combinational therapy with quinine against Plasmodium falciparum. Malar J. 2010;9:139.
Savini H, Souraud JB, Briolant S, Baret E, et al. Atorvastatin as a potential antimalarial drug: in vitro synergy in combinational therapy with dihydroartemisinin. Antimicrob Agents Chemother. 2010;54:966–7.
Wurtz N, Briolant S, Gil M, Parquet V, et al. Synergy of mefloquine activity with atorvastatin, but not chloroquine and monodesethylamodiaquine, and association with the pfmdr1 gene. J Antimicrob Chemother. 2010;65:1387–94.
Haughan PA, Chance ML, Goad LJ. Synergism in vitro of lovastatin and miconazole as anti-leishmanial agents. Biochem Pharmacol. 1992;44:2199–206.
Chen ZS, Mutoh M, Sumizawa T, Furukawa T, et al. Reversal of heavy metal resistance in multidrug-resistant human KB carcinoma cells. Biochem Biophys Res Commun. 1997;236:586–90.
Chuman Y, Chen ZS, Seto K, Sumizawa T, et al. Reversal of MRP-mediated vincristine resistance in KB cells by buthionine sulfoximine in combination with PAK-104P. Cancer Lett. 1998;129:69–76.
Kitasono M, Okumura H, Ikeda R, Sumizawa T, et al. Reversal of LRP-associated drug resistance in colon carcinoma SW-620 cells. Int J Cancer. 2001;91:126–31.
Shudo N, Mizoguchi T, Kiyosue T, Arita M, et al. Two pyridine analogues with more effective ability to reverse multidrug resistance and with lower calcium blocking activity than their dihydropyridine counterparts. Cancer Res. 1990;50:3055–61.
Sumizawa T, Chen ZS, Chuman Y, Seto K, et al. Reversal of multidrug resistance-associated protein-mediated drug resistance by the pyridine analog PAK-104P. Mol Pharmacol. 1997;51:399–405.
Vanhoefer U, Cao S, Minderman H, Toth K, et al. PAK-104P, a pyridine analogue, reverses paclitaxel and doxorubicin resistance in cell lines and nude mice bearing xenografts that overexpress the multidrug resistance protein. Clin Cancer Res. 1996;2:369–77.
Tachiwada T, Chen ZS, Che XF, Matsumoto M, et al. Isolation and characterization of arsenite-resistant human epidermoid carcinoma KB cells. Oncol Rep. 2007;18:721–7.
Golstein PE, Boom A, van geffel J, Jacobs P, et al. P-glycoprotein inhibition by glibenclamide and related compounds. Pflugers Arch. 1999;437:652–60.
Conseil G, Deeley RG, Cole SPC. Role of two adjancent cytoplasmic tyrosine residues in MRP1 (ABCC1) transport activity and sensitivity to sulfonylureas. Biochem Pharmacol. 2005;69:451–61.
Gayet L, Picault N, Cazalé AC, Beyly A, et al. Transport of antimony salts by Arabidopsis thaliana protoplasts over-expressing the human multidrug resistance-associated protein 1 (MRP1/ABCC1). FEBS Lett. 2006;580:6891–7.
Dantzig AH, Law KL, Cao J, Starling JJ. Reversal of multidrug resistance by the P-glycoprotein modulator, LY335979, from the bench to the clinic. Curr Med Chem. 2001;8:39–50.
Hyafil F, Vergely C, Du Vignaud P, Grand-Perret T. In vitro and in vivo reversal of multidrug resistance by GF120918, an acridonecarboxamide derivative. Cancer Res. 1993;53:4595–602.
Perez-Victoria JM, Cortes-Selva F, Parodi-Talice A, Bavchvarov BI, et al. Combination of suboptimal doses of inhibitors targeting different domains of LtrMDR1 efficiently overcomes resistance of Leishmania spp. to miltefosine by inhibiting drug efflux. Antimicrob Agent Chemother. 2006;50:3102–10.
Castanys-Munoz E, Alder-Baerens N, Pomorski T, Gamarro F, et al. A novel ATP-binding cassette transporter from Leishmania is involved in transport of phosphatidylcholine analogues and resistance to alkyl-phospholipids. Mol Microbiol. 2007;64:1141–53.
Deharo E, Barkan D, Krugliak M, Golenser J, et al. Potentialization of the antimalarial action of chloroquine in rodent malaria by drugs known to reduce cellular glutathione levels. Biochem Pharmacol. 2003;66:809–17.
Loo TW, Bartlett MC, Clarke DM. Disulfiram metabolites permanently inactivate the human multidrug resistance P-glycoprotein. Mol Pharm. 2004;1:426–33.
Loo TW, Clarke DM. Blockage of drug resistance in vitro by disulfiram, a drug used to treat alcoholism. J Natl Cancer Inst. 2000;92:898–902.
Namazi MR. Potential utility of disulfiram against leishmaniasis. Indian J Med Res. 2008;127:193–4.
Gamage SA, Figgitt DP, Wojcik SJ, Ralph RK, et al. Structure-activity relationships for the antileishmanial and trypanosomal activities of 1′-substituted 9-anilinoacridines. J Med Chem. 1997;40:2634–42.
Gamage SA, Tepsiri N, Wilairat P, Wojcik SJ, et al. Synthesis and in vitro evaluation of 9-anilino-3,6-diaminoacridines active against a multidrug-resistant strain of the malaria parasite Plasmodium falciparum. J Med Chem. 1994;37:1486–94.
Girault S, Grellier P, Berecibar A, Maes L, et al. Antimalarial, antitrypanosomal, and antileishmanial activities and cytotoxicity of bis(9-amino-6-chloro-2-methoxyacridines): influence of the linker. J Med Chem. 2000;43:2646–54.
Seeger MA, Schiefner A, Eicher T, Verrey F. Structural asymmetry of AcrB trimer suggests a peristaltic pump mechanism. Science. 2006;313:1295–8.
Pedersen JM, Matsson P, Bergstrom CA, Norinder U, et al. Prediction and identification of drug interactions with the human ATP-binding cassette transporter multidrug-resistance associated protein 2 (MRP2; ABCC2). J Med Chem. 2008;51:3275–87.
Pajeva IK, Globisch C, Wiese M. Combined pharmacophore modeling, docking, and 3D QSAR studies of ABCB1 and ABCC1 transporter inhibitors. Chem Med Chem. 2009;4:1883–96.
Vergnes B, Sereno D, Madjidian-Sereno N, Lesmesre JL, Ouaissi A. Cytoplasmic SIR2 homologue overexpression promotes survival of Leishmania parasites by preventing programmed cell death. Gene. 2002;296:139–50.
Purkait B, Singh R, Wasnik K, Das S, et al. Up-regulation of silent information regulator 2 (Sir2) is associated with amphotericin B resistance in clinical isolates of Leishmania donovani. J Antimicrob Agents. 2015;70:1343–56.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Pradines, B. (2018). P-Glycoprotein-Like Transporters in Leishmania: A Search for Reversal Agents. In: Ponte-Sucre, A., Padrón-Nieves, M. (eds) Drug Resistance in Leishmania Parasites. Springer, Cham. https://doi.org/10.1007/978-3-319-74186-4_14
Download citation
DOI: https://doi.org/10.1007/978-3-319-74186-4_14
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-74185-7
Online ISBN: 978-3-319-74186-4
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)