Abstract
This chapter is addressed to the description of the forms of caudal herniation through the foramen magnum different from Chiari type I malformation, which is largely the most common variant of hindbrain herniation. Among the here-illustrated conditions, Chiari type II malformation is the most frequently encountered in the clinical practice, following the epidemiological distribution of the open spina bifida to which it is strictly related. Chiari II malformation provides diagnostic and management challenges because it is not a single malformation but a constellation of malformations involving either the neural (brain, cerebellum, spinal cord) and the bony structures (skull, spine). The clinical picture can vary significantly according to the age at onset and the severity of the brainstem dysfunction. On the other hand, the other variants are very rare, like Chiari type III malformation, or exceptional and nosographically still debated, like Chiari types IV and V malformations. These rare forms are quite often burdened by a dismal prognosis.
Access provided by Autonomous University of Puebla. Download reference work entry PDF
Similar content being viewed by others
Introduction
This chapter is addressed to the description of the forms of caudal herniation through the foramen magnum different from Chiari type I malformation, which is largely the most common variant of hindbrain herniation. Among the here-illustrated conditions, Chiari type II malformation is the most frequently encountered in the clinical practice, following the epidemiological distribution of the open spina bifida to which it is strictly related. Chiari II malformation provides diagnostic and management challenges because it is not a single malformation but a constellation of malformations involving either the neural (brain, cerebellum, spinal cord) and the bony structures (skull, spine). The clinical picture can vary significantly according to the age at onset and the severity of the brainstem dysfunction. On the other hand, the other variants are very rare, like Chiari type III malformation, or exceptional and nosographically still debated, like Chiari types IV and V malformations. These rare forms are quite often burdened by a dismal prognosis.
Definition and Classification
The eponym “Chiari malformation” is adopted to indicate a hindbrain herniation into the upper spinal canal in recognition of the pathologist Hans Chiari who carried out the first systematic analysis of the phenomenon (Chiari 1891). Sometimes, the term “Arnold-Chiari malformation” is still used to indicate this herniation in patients with open spina bifida (Chiari II malformation) as result of the first description of this condition by Julius Arnold (1894) and the eponym created by two of his pupils in honor of their mentor (Schwalbe and Gredig 1907).
In the last decades, several new entities (in particular, different subtypes of Chiari I malformation) have been described in addition to the “original” four variants of Chiari malformations. They are here briefly summarized for an overall classification and for a correct differentiation from the Chiari malformations illustrated in this chapter:
-
Chiari type I malformation (C-I): prolapse of the cerebellar tonsils 5 mm or more below the foramen magnum (basion-opisthion line), according to the universally used criteria by Ester and Chen (Elster and Chen 1992).
-
Borderline Chiari I malformation: 3–4 mm herniation of the cerebellar tonsils. A less than 3 mm prolapse is considered normal as well as a 6 mm ectopia in children during the first decade of life (Mikulis et al. 1992).
-
Chiari 0 malformation: symptomatic condition with hydromyelia and crowded foramen magnum but without tonsillar herniation (Isik et al. 2009).
-
Chiari 1.5 malformation: caudal displacement of the tonsils, brainstem, and IV ventricle without spina bifida (Iskandar and Oakes 1999).
-
Chiari type II malformation (C-II): complex malformation, almost invariably associated with myelomeningocele or other forms of open spina bifida (OSB), consisting of the herniation of the cerebellar vermis and tonsils, medulla oblongata, and IV ventricle (usually the inferior portion) below the foramen magnum. The use of the term “C-I” to indicate mild forms of hindbrain herniation in OSB is then incorrect.
-
Chiari type III malformation (C-III): severe ectopia of the cerebellum and the brainstem/IV ventricle coupled with an occipital or upper cervical encephalocele.
-
Chiari type IV malformation (C-IV): bilateral cerebellar hypoplasia, which is not a form of hindbrain herniation (“cerebellar hypoplasia without herniation of posterior fossa content into the spinal canal,” according to the original Chiari’s definition), plus occipital encephalocele (Chiari 1896).
-
Chiari type V malformation (C-V): quite recently introduced to describe the absence of the cerebellum and herniation of the occipital lobes through the foramen magnum (Tubbs et al. 2012).
Chiari Type II Malformation
Epidemiologic and Etiologic Aspects
The incidence of C-II necessarily corresponds to that of OSB, to which is strictly related. The incidence of the latter varies significantly in the different areas of the world because of the differences in ethnicity, economic levels, and health policies, e.g., folic acid prophylaxis and pregnancy termination. The incidence of OSB is traditionally estimated to be around 1/1000 live births (ranging from 0.2 to 2/1000) (Dias 1999). The highest rates were registered in the British Isles (2.4–3.8 up to 5/1000 live births and in the Irish population) (The EUROCAT Working Group 1987), while the incidence in the continental Europe (0.1–0.6/1000 live births) (The EUROCAT Working Group 1991) overlapped that of North America (0.3–0.4/1000 live births, with the higher figures recorded in the Hispanic population) (Josan and Morokoff 2008). Currently 300,000 new cases of myelomeningocele/year are expected in the world, with a significant reduction (up to 80%) in the Western countries compared with the developing ones (Aguilera et al. 2009). About one fourth of the pregnancies in Western countries are electively terminated following the intrauterine recognition of OSB (Velie and Shaw 1996). The incidence of C-II in subjects with OSB is about 98% (range, 90–100%), which further confirms its strict relationship with this specific form of dysraphism (McLone 1998). Even though the occurrence of C-II depends on the CSF loss during the intrauterine life secondary to OSB (as the results of its intrauterine repair unequivocally demonstrated), in the vast majority of the cases in the world, its epidemiology remains still associated to that of OSB: in other words, to the understanding of its complex interaction between environmental and genetic factors on the base of which prophylactic measures can be established. The folate deficiency resulting from an inadequate intake before the conception and during the pregnancy is the most important and well-established environmental risk factor (Ganesh et al. 2014; Meijer and de Walle 2005; MRC Vitamin Study Research Group 1991; Pitkin 2007; Ray et al. 2002). Other possible risk factors are represented by maternal obesity and hyperinsulinemic diabetes, maternal intake of antiepileptic drugs in the periconceptional period (in particular, carbamazepine and valproate), and febrile illness in the early pregnancy (Chambers et al. 1998; Melvin et al. 2000; Shaw et al. 1996). Many teratogens can induce OSB and C-II in animal models (Sim et al. 1996; Sim et al. 2013). Moreover, the serum deficiency of vitamin B12 has been suggested as possible specific risk factor for C-II (Verma and Pratiaraj 2012; Welsch et al. 2013). Other than by syndromes (trisomy 13 and 18, Fraser syndrome, Waardenburg syndrome) and by affected siblings (Papp et al. 1997), the risk of OSB is increased by genetic mutations involving the synthesis and metabolism of the folate and its metabolites (e.g., gene for the folate-homocysteine pathway enzymes) (Schwahn and Rozen 2001; Van der Linden et al. 2006) or the genes necessary for the metabolism of substances necessary for the embryonal development (e.g., Pax gene family) (Hol et al. 1996; Melvin et al. 2000). Among these genes, the methylene tetrahydrofolate dehydrogenase gene (MTHFD) is crucial in the folate metabolism pathway. Actually, MTHFD 1 G1958A gene polymorphism has been found as strongly related to OSB (Jiang et al. 2014).
Pathogenesis
OSD is universally accepted to originate from the morphogenetic movements occurring during the neurulation (see pertinent chapter in this book). In spite of the strict relationship between C-II and OSB, C-II is not observed during the embryonal life, but it appears only during the fetal life, thus suggesting that it is a secondary anomaly and not a primary one (Osaka et al. 1978). The first hypothesis to explain its occurrence was made by Chiari itself who postulated that the hindbrain prolapse was the consequence of the pressure from above exerted by the hydrocephalus (Chiari 1891). If this theory can be still partially accepted for some cases of C-I, it is not valid for C-II as the malformation in some cases is not associated to the presence of hydrocephalus and in many affected subjects, the hydrocephalus starts after the myelomeningocele repair. Moreover, the rostral herniation of the superior cerebellum cannot be justified by the hydrocephalus. Penfield and Coburn, on the other hand, proposed as pathogenetic mechanism of C-II a caudal traction exerted from below by the spinal cord anchored to the dysraphic spinal defect (Penfield and Coburn 1938). They based their theory on the case of a young woman with thoracic OSB whose cervical spinal roots had an oblique upward course rather than an horizontal one at autopsy. This mechanism, however, is currently discarded because the oblique course of the spinal cord roots is not constantly observed in OSB and because it does not produce hindbrain herniation in similar conditions with tethered cord (e.g., closed spina bifida). A tissue hyperplasia at the level of the foramen magnum was postulated by Barry and coworkers in 1957 (Barry et al. 1957). Although this hyperplasia has not been confirmed, the concept of a primary brain dysgenesis, firstly proposed by Cleland in 1883 (Cleland 1883), has been taken into account to explain the C-II associated anomalies and even the occurrence of C-I in subjects with other neurological diseases (e.g., epilepsy, autism) (Massimi et al. 2011a).
The “unified theory” proposed by McLone and Knepper in 1989 remains the most accepted one (McLone and Knepper 1989). Accordingly, C-II can be defined as a dysembriogenetic process resulting from the incomplete occlusion of the spinal neurocele with chronic escape of CSF from the neural tube at the myelomeningocele site causing the collapse/missed opening of the IV ventricle followed by low pressure on the surrounding mesenchyme: the subsequent undersized posterior cranial fossa (PCF) creates a mismatch between the PCF itself (too small) and its content (normal cerebellar and brainstem volume) with following caudal prolapse of the latter. Such a decompression of the cerebral vesicles and ventricles would result in the “pan-cerebral” and “pan-cranial” malformation that is found in OSB patients (McLone and Dias 2003). A similar CSF siphoning mechanism was propounded by Cameron in 1957 (Cameron 1957). The experimental surgical models of OSB clearly show that C-II is not a simply associated anomaly of OSB but the result of OSB (Paek et al. 2000; Sim et al. 2013; Weber-Guimaraes et al. 2005). The reversion of C-II after prenatal OSB repair observed after both experimental and clinical experiences (Adzick 2013; Bouchard et al. 2003; Sutton et al. 2003; von Koch et al. 2005a) further supports the hypothesis that the CSF leakage through the exposed central canal prevents the CSF hydrodynamics and the enlargement of PCF, resulting in hindbrain herniation (McLone and Naidich 1992). The unified theory also explains the typical decompensation of hydrocephalus after the myelomeningocele closure though it does not explain those cases of hydrocephalus and syringomyelia occurring already in the fetal life, unless considering them as an effect of the hindbrain herniation itself. According to the review on the “unifying hypothesis for hydrocephalus, Chiari malformation, syringomyelia, anencephaly and spina bifida” by Williams (2008), (1) PCF hypoplasia associated to C-II prevents the CSF exit from the spine to the head as the blood enters the central nervous system during the movements, causing syringomyelia and the spinal cord damage found in OSB; (2) in turn, these two conditions prevent the escape of CSF from the head to the spine favoring the occurrence of hydrocephalus and the brain injury found in anencephaly.
The presence of other brain (e.g., large massa intermedia, tectal beaking, or heterotopia) and membranous and bone covering malformations (e.g., meningeal and falx anomalies, craniolacunae, or short clivus) remains partially unexplained though suggesting a more complex anomaly involving both the neuroectoderm and the mesoderm (Massimi et al. 2011a). On these grounds, a multifactorial theory could be advocated to explain the origin of C-II in OSB, taking into account the unified theory and a dysgenesis of the neural and bone tissues. Indeed, a mesoderm deficiency, causing the hypoplasia of the PCF, has been induced in the experimental models of C-II and OSB (Di Rocco and Rende 1989; Marin-Padilla and Marin-Padilla 1981).
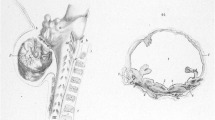
Pathological Findings
C-II is a group of malformations mainly consisting in an undersized PCF with partial caudal herniation of its content. The relationship with open dysraphisms must be emphasized since C-II occurs only in OSB, so that it is considered as part of OSB complex (Cama et al. 1995). Sometimes, C-II is poorly evident (viz., when the PCF volume is quite normal), but it is absent in OSB very rarely (Tortori-Donati et al. 2000).
Macroscopic Findings
The macroscopic picture of C-II is characterized by a rich and variegated number of pathological findings and associated anomalies as expression of a dysplasia of all the central nervous system (Gilbert et al. 1986; Iskandar and Oakes 1999; McLone and Dias 2003; Raybaud and Miller 2008; Van Roost et al. 1995). They can be summarized as follows (see also Table 1):
-
1.
As far as the PCF content is concerned, a significant elongation and dysplasia of the cerebellum are present, which are prolapsed into the upper spinal canal together with the IV ventricle and its choroid plexus and the medulla. All these structures are elongated and may be variously dysplastic. The herniating cerebellum, other than the hemispheres, tonsils, and vermis, often involves also the nodulus, pyramid, and uvula. The herniating tissue resembles a peg or a long tail, usually extending to C2–C3 level but often up to C4–C5 or more. The prolapsed cerebellum may cover the roof IV ventricle or may be intraventricular. In addition, the neural structures may present several anomalies, such as kinking of the cervico-medullary junction, upward herniation of the superior part of the cerebellar vermis through the tentorial notch (generally enlarged), stretching of the lower cranial nerves, forking or kinking of the Sylvian aqueduct, beaking of the quadrigeminal plate, and rhombencephalosynapsis (very rare condition with fusion of the cerebellar hemispheres and dentate nuclei because of agenesis of the vermis) (Sener and Dzelzite 2003). Based on the autoptic observations of Emery and MacKenzie in 300 children, the mildest forms of hindbrain herniation are characterized by IV ventricle in normal position and are revealed only by the upward angle at which the first couple of cervical roots exits the cord (Emery and MacKenzie 1973). The most severe forms, on the other hand, show displacement of the IV ventricle in the foramen magnum (with caudal cyst) and kinking of the medulla. According to these authors, the severity of C-II is directly proportional to the extension of the myelomeningocele and inversely to the length of the cervical dentate ligaments.
-
2.
Also the bones of the PCF and the dural envelopes are involved in the malformation process, being characterized by small volume of PCF (seldom, normal, or quite normal), which is counterbalanced by a wide enlargement of the foramen magnum, craniolacunae (thinning or complete erosion of the skull, especially involving the upper half of the skull), shortening of the clivus (often concave and thinned), scalloping of the petrous bone, tentorial hypoplasia, low attachment of the tentorium (the torcula often lying just above or in correspondence of the foramen magnum), hypoplasia, and/or fenestration of the cerebral falx.
-
3.
With regard to the supratentorial space, the most common associated anomaly is hydrocephalus (up to 90% of cases), with typical features such as colpocephaly, round and oblique frontal horns (pointing anteromedially), and thin third ventricle. A large mass intermedia is frequently encountered. Callosal hypoplasia or agenesis, polygyria, microgyria, and subcortical heterotopia may complete the picture. The most typical cortical pattern (about 50% of cases with C-II) is the so-called stenogyria (Gilbert et al. 1986). This term indicates a cortical overfolding with packed gyri (but with normal sulcation, differently from polymicrogyria), especially involving the posteromedial cortex.
-
4.
The spinal cord-associated malformations are represented by myelomeningocele in about all cases (and its possible related anomalies, e.g., dermoid cyst, diplomyelia, etc.) and syringomyelia in more than 50% of cases, ranging from 40% to 95% (and its consequences, like scoliosis).
Microscopic Findings
The histological analysis of the prolapsed tonsils and cerebellar tissue reveals atrophy and gliosis. The atrophy results from depletion of Purkinje and granule cells and absent/reduced myelination of the fibers composing the cerebellar folia (Sav 2008). In the brainstem, a distortion of tracts and nuclei is common as well as hypoplasia or dysgenesis/agenesis of cranial nerve and pontine nuclei (Gilbert et al. 1986). These findings can be primary or secondary to a compression damage. The extreme form of cerebellar damage, called vanishing cerebellum, is characterized by secondary cerebellar shrinkage coupled with brainstem atrophy and the other OSB brain findings (Boltshauser et al. 2002).
A dense arachnoid scarring is found around the embedded neural prolapsing structures.
In the brain hemisphere, areas of focal cortical dysplasia and gray matter heterotopia can be easily recognized within the white matter. The normal cortical cytoarchitecture is preserved in the polygyric pattern, while laminar abnormalities can be appreciated in case of polymicrogyria.
Clinical Picture
C-II per se remains asymptomatic or poorly symptomatic in most of the cases. This is because of the congenital distribution of the herniating hindbrain within the foramen magnum and the upper spinal canal, which consequently result enlarged to accommodate this excess of neural tissue. Actually, the C-II neurological deterioration is quite rarely seen as primary event, which usually affects neonates and infants (see below). More commonly, the deterioration results from the C-II associated malformations; of course, this aspect may complicate the clinical diagnosis. Frequently, the clinical worsening occurs after a raised ICP, mainly in infants with new-onset hydrocephalus, or decompensation of an already existing hydrocephalus (e.g., shunt malfunction in older children). Such a decompensation can cause clinical signs and symptoms by worsening the hindbrain structures’ prolapse and/or the possible associated syringomyelia. Syringobulbia and/or syringomyelia, as well as tethered cord, on the other hand, can worsen independently from the raised ICP and can produce signs/symptoms referable to C-II or that can worsen C-II itself (especially, compression on the bulbo-cervical junction by syringomyelia). Similarly, the clinical picture can be dominated by the neurological worsening resulting from the myelomeningocele (e.g., bladder and/or bowel dysfunction, late sensory-motor deterioration) or its associated spinal problems (especially, scoliosis). The problems related to myelomeningocele, syringomyelia, tethered cord, and spine usually occur in old children and adolescents rather than infants and young children.
Symptomatic C-II is revealed by bulbar, cerebellar, or spinal cord dysfunction as dyspnea, dysphagia, dysphonia, nystagmus, vertigo, ataxia, paresthesia, and spastic tetraparesis. The clinical picture varies substantially with the age.
Neonatal Period and Early Infancy
In newborns and infants, the brainstem dysfunction/compression is prevalent, presenting with stridor and/or high pitched cry (which are crucial signs revealing the vocal cords paralysis), central apnea, depressed gag reflex, swallowing disturbances, breath-holding spells (leading even to loss of consciousness), bradycardia, recurrent aspiration pneumonia, opisthotonus (other important, revealing sign of PCF neural compression), hypotonia, and tetraparesis (or variable weakness of upper and lower arms). These symptoms are estimated to occur in 5–10% of cases (Sgouros 2008). It is worth noting that the clinical onset can be insidious and not easy to be recognized in neonates. Indeed, they can show, as isolated or in combination, poor sucking and poor crying (because of dyspnea), poor feeding and vomiting (because of dysphagia), torticollis, unilateral facial palsy, and lower limb weakness, which may be overlooked or attributed to other causes.
The deterioration is more frequent in the first months of life when it can represent a life-threatening emergency because of the acute and sudden occurrence of apnea and aspiration pneumonia. Typically, however, these clinical signs are present already at birth and evolve after the closure of the myelomeningocele and/or after the appearance of hydrocephalus. The severe evolution is often progressing and not responsive to the surgical and/or medical management (because of the primary brainstem damage) leading to the death of the affected patient. The occurrence of congenital symptoms is explained by some authors by a granulomatous meningitis induced by the contamination of the CSF with the vernix caseosa (Stritzke et al. 2011).
Finally, C-II can be concomitant to several and variable pathological conditions or syndromes. Recently, for example, two rare associations have been described: C-II and achondroplasia, with the subsequent, challenging “double-hit” at level of the foramen magnum (Awad et al. 2014), and C-II and triple spinal dysraphism (myelomeningocele, lipomyelomeningocele, and split cord malformation type I), with the following pathogenetic puzzle (Dhandapani and Srinivasan 2016).
From Late Infancy to Adulthood
In older children and adolescents, the symptoms arising from the brainstem and lower cranial nerve dysfunction/compression/stretching are uncommon. Indeed, cerebellar and spinal signs and symptoms are prevalent, partially resembling those of patients with C-I. Occipital and cervical pain (sometimes, cough headache), syncopal episodes, weakness of the upper extremities (cervical myelopathy), increased tendon reflexes, spasticity, paresthesia, ataxia, scoliosis, worsening of the bladder function, strabismus, nystagmus, defects of pursuit and optokinetic movements, and convergence can be observed. The occurrence of episodes of aspiration pneumonia and the deterioration of the ambulation and/or the scoliosis can orientate the diagnosis. The clinical diagnosis, in fact, can be hard also in old children because of the signs and symptoms that can be referred to the various conditions associated with OSB. The aforementioned cortical anomalies may account for the occurrence of seizures (Shankar et al. 2016).
Sleep-disordered breathing is predictable, but being not explored routinely, it is probably underreported (Vinck et al. 2006). The analysis of 16 C-II children by Alsaadi et al. demonstrated a mean 6.3/h apnea-hypopnea index (AHI), with a ≥10/h AHI in about one fifth of cases (Alsaadi et al. 2012). As expected, the mean central AHI was substantially higher (5.9/h) than the mean obstructive AHI (0.4/h).
The cognitive development in C-II children follows that of OSB, being grossly normal in the patients without severe hydrocephalus or significant comorbidities (brain malformations, seizures, infection) (Mirzai et al. 1998; Soare and Ramondi 1977). However, the analysis of adult cohorts shows a certain cognitive impairment (especially, attention deficits) in the majority of patients, which can prevent an independent life other than the psychical disability (Jenkinson et al. 2011). The associated brain anomalies seem to be more relevant than the shunt malfunction or the hydrocephalus alone on the final cognitive outcome. The severity of the morphological findings (viz., degree of ventriculomegaly, site and extension of the myelomeningocele, and degree of hindbrain herniation) is found to correlate with the neurodevelopmental outcome (Barf et al. 2003; Coniglio et al. 1997) though this datum is not ever confirmed (Otera et al. 2014; van der Vossen et al. 2009). According to some authors, indeed, the best predictor of neurodevelopmental outcome (at least during infancy) is the fetal heart rate, the time spent in the quite phase being significantly higher among children with normal developmental quotient (DQ) than in those with impaired DQ (28% vs 11%) (Otera et al. 2014). The role of C-II on the cognitive outcome of OSB has not been well established yet. However, based on the comparison between 27 children with OSB with C-II and 19 children with OSB without C-II provided by Vinck et al., C-II was associated to lower VIQ and TIQ in the complete group (both retarded and not retarded children, high significance) and to lower PIQ and TIQ among non-retarded patients (lower significance) (Vinck et al. 2006). Patients with C-II showed impaired visual analysis and synthesis, verbal memory, and verbal fluency as a specific profile shared with hydrocephalus.
Mild psychiatric comorbidities, as anxiety and mood disorders, and cannabis abuse are not uncommon and may affect the functioning and the quality of life (Bakim et al. 2013). On the other hand, severe psychiatric complications, as psychosis and major neurocognitive disorder, are rare (Del Casale et al. 2012; Hoederath et al. 2014).
Radiological Diagnosis
Antenatal Diagnosis
The diagnosis of C-II is made prenatally in most of the cases. On ultrasounds, indeed, C-II represents an important indirect sign for the diagnosis of OSB. Ultrasounds clearly show the small size of PCF together with the obliteration of the cisterna magna and the dysplastic/dysmorphic appearance of the cerebellum with its abnormal anterior curvature (the so-called banana sign) (Fig. 1a) (Campbell et al. 1987). The ventriculomegaly and the following frontal bossing (responsible of the deformation of the skull also known as “lemon sign”) (Fig. 1b) are other important indirect signs associated to C-II in configuring the intracranial picture of OSB (Penso et al. 1987). Differently from the ventriculomegaly and the lemon sign, which may be absent (50% of cases) or may be missed at diagnosis or may appear late during the pregnancy (usually by 22–24 weeks), the effacement of the cisterna magna and the banana sign are constant and reliable findings that can be appreciated by 16 weeks of gestation or earlier (Sebire et al. 1997; Van den Hof et al. 1990). Thanks to these signs the antenatal diagnosis of OSB and C-II is correctly done in up to 90% of cases (the majority of them before the 24th week of gestation) (Garne et al. 2005). In particular, four accessory features have been found useful and reliable for the prenatal sonographic diagnosis of C-II: (1) the pointed shape of the occipital horn, which results visible especially after the 24th week of gestation and in fetuses without ventriculomegaly (Callen and Filly 2008); (2) the shorter distance from the posterior edge of the occipital horn to the occipital bone as compared with healthy fetuses (Filly et al. 2010); (3) beaking of the tectum, which is seen either before and after the 24th week and the frequency of which increases as the severity of PCF findings increases (Callen et al. 2009); and (4) interhemispheric cysts, which are unrelated to the other C-II features and are more frequent than in fetuses with other malformations (Wong et al. 2009).
Ultrasounds also show the direct signs of OSB, as the spinal dysraphism and the myelomeningocele, but it is worth emphasizing that they may be missed (because of the position of the fetus and the difficult recognition of the spinal defect) so that the diagnosis of OSB is mainly obtained through the analysis of the indirect signs as C-II (Ghi et al. 2006).
The elevated accuracy of ultrasounds limits the use of prenatal MRI for the diagnosis of both C-II and OSB. MRI findings, however, are useful for doubtful or difficult cases (e.g., unfavorable position of the fetus, maternal obesity, oligohydramnios), for the differential diagnosis with other dysraphisms (e.g., closed spina bifida), and for the preoperative planning in case of antenatal surgery. For these reasons and thanks to the high-resolution anatomical details provided, fetal MRI is more and more utilized as complimentary tool to the ultrasounds diagnosis (Righini et al. 2011; Simon 2004; Von Koch et al. 2005b). Abele et al. recently reported on the inter-observer review (senior resident radiologist and senior radiologist) of 37 C-II fetal MRI that they carried out to compare bSSFP (balanced steady-state free precession) and half-Fourier RARE (rapid acceleration with relaxation enhancement) MRI (Abele et al. 2013). Both types of MRI were judged equivalent in showing the foramen magnum characteristics, the entity of the tonsillar ectopia, and the extent of the open dysraphism, while the tonsils appeared more conspicuous on RARE and the intervertebral disks more conspicuous on bSSFP.
In utero MRI clearly shows the characteristics of the spina bifida, and though the vertebral level and extent of the malformation are demonstrated as well by ultrasounds, it offers a higher resolution of the imaging of the malformation itself, favoring the differential diagnosis between myelomeningocele and, for example, myelocystocele or lipomyelomeningocele (Aaronson et al. 2003; Bruner et al. 2004). Similarly, fetal MRI provides the same accuracy than ultrasounds on the diagnosis but a clearer definition of C-II and some of its related anomalies (e.g., subcortical heterotopia, commissural agenesis), thus giving more details for the prognosis (Mangels et al. 2000). The use of DWI (diffusion-weighted imaging) allowed Mignone Philpott et al. to detect a significant increase of ADC (apparent diffusion coefficient) values in the cerebellum of C-II fetuses compared with healthy fetuses, in spite of the expected decline of ADC during pregnancy and the expected lower values of the cerebellum compared with the brain (similar values were found in the pons) (Mignone Philpott et al. 2013). The authors attributed these increased values to the augmented extracellular water resulting from the impaired CSF dynamics in PCF of the affected fetuses. Similarly, the use of DTI (diffusion tensor imaging) in fetal MRI allows to differentiate between changes in C-II (midbrain increased fractional anisotropy (FA) and isolated hydrocephalus or ventriculomegaly (normal FA) (Woitek et al. 2016).
A further, important distinction favored by MRI is between hydrocephalus and dysgenetic ventriculomegaly. The main limitations of prenatal MRI are represented by the movements (fetus, maternal breathing), which can be limited by ultrafast T2 sequences, and the small size of the fetal brain that prevents a reliable analysis before 18–20 weeks of gestation.
Postnatal Diagnosis
Cranio-spinal MRI is the gold standard examination to provide the diagnosis of C-II and its associated malformations thanks to the high-resolution multiplanar display and the high sensitivity to tissue changes. Standard MRI can show the characteristics of the hindbrain herniation as well as all the associated intracranial and spinal cord abnormalities reported in Table 1. T1 and T2 sequences on the sagittal plane are optimal to show the small posterior fossa; the caudal dislocation of brainstem; IV ventricle and cerebellum, with large foramen magnum and cervical spinal canal; the short and scalloped clivus; the hypoplastic and down-attached tentorium; the elongation of the vein of Galen that joins a shortened straight sinus; and the low transverse sinuses lying close to the enlarged foramen magnum (Figs. 2, 3, and 4). High-definition 3D T2 acquisition and venography emphasize the details as well as the venous anatomy. These details can be summarized as follows (Raybaud and Miller 2008):
-
1.
Severe hindbrain herniation with the cerebellum compressing and indenting the medulla that, in turn, is dislocated behind the upper spinal cord. The spinal cord remains tethered by C1 dentate ligaments, resulting in the kinking of the brainstem within the spinal canal. Therefore, the upper spinal canal contains, from anterior to posterior, the spinal cord, the medulla, the IV ventricle, and the cerebellum. The ectopic cerebellar vermis is poorly differentiated from the remaining herniating cerebellum, even though some authors found it well evident along the midline and enlarged because of a squeezing effect (Salman et al. 2006).
-
2.
Rarely (2% of cases), the hindbrain herniation is mild to moderate with all the structures accommodated within the small posterior fossa or, at most, with caudal dislocation of a small portion of cerebellum and with a recognizable cisterna magna.
-
3.
Upward herniation of the cerebellum located behind pons and medulla and the pericerebellar cistern through the tentorial incisura. The herniated cerebellum, also called cerebellar towering or pseudotumor of the tentorium, is shaped by the incisura and is able to displace superiorly and laterally the temporo-occipital lobes (Fig. 3b). Moreover, the exuberant cerebellum goes around the brainstem occupying the peripontine and perimedullary cistern (triple-peaked appearance) (Fig. 2c). In severe cases, the cerebellum can encase the basilar artery and cover the cranial nerves (that emerge from the cerebellar folia).
-
4.
Overall, the cerebellum is normal sized or reduced in size because of the atrophy induced by the chronic compression due to the small PCF (Juranek et al. 2010). The “vanishing” cerebellum, on the other hand, is revealed by cerebellar edema at birth and atrophic involution with an abnormal PCF and PCF content (differently from the primary agenesis of the cerebellum where the PCF size, the brain, and the spine are normal) (Sener and Dzelzite 2003).
-
5.
Narrowing, elongation, and flattening of the pons, which is located across the foramen magnum with subsequent, possible effacement of the ponto-medullary sulcus.
-
6.
Flattening and inferior stretching of the IV ventricle, sometimes with the tela choroidea bulging inferiorly below the cerebellum and forming a cyst (as result of the failed opening of the roof of the IV ventricle). This cyst can be delimitated by the choroid plexus (best visualized after contrast medium administration).
-
7.
The cranial nerves show a course longer than normal because of the distance between the caudally displaced brainstem (and nuclei) and the normally positioned exit foramina.
-
8.
In spite of the possible clinical evolution and in spite of the possible radiological worsening resulting from hydrocephalus and/or syringomyelia and some anecdotic cases of “real” radiological worsening, the radiological picture of C-II generally remains stable, included the cerebellar atrophy (Salman 2011). A reduction of the hindbrain herniation (without changes of PCF volume), on the other hand, can be appreciated after the treatment of the hydrocephalus in infants with cerebellar ectopia lower than C1 (Hashiguchi et al. 2016).
Showing the MRI of a 5-year-old girl. (a): typical appearance of C-II with herniation of the cerebellum up to C3, dislocation of the lower part of the IV ventricle and the medulla below the enlarged foramen magnum, low attachment of the tentorium, beaking of the midbrain, large massa intermedia, hypoplasia of the corpus callosum, and stenogyria. Note the wrapping of the pons (b) and the medulla (c) by the cerebellum
Thanks to the rich and detailed radiological picture that nowadays can be obtained, C-II can be differentiated from other Chiari malformations easily. A synopsis of the differential diagnosis with C-I and C-III is reported on Table 2. At the same time, however, the interpretation of such a constellation of radiological signs may not be straightforward. According to the inter-observer blind and independent review (by one junior neurologist, one senior neurologist, and one senior radiologist) of 76 MRI reported by Geerdink et al., 23 morphological findings were judged as unreliable, while a general agreement was obtained only about 9 findings, 8 in the sagittal MRI plan (downward herniation of the cerebellum, downward herniation of the tonsils, downward displacement of the medulla, downward displacement of the fourth ventricle, medullary kinking, abnormal width of the fourth ventricle, hypoplastic tentorium, beaked tectum) and 1 in the axial plan (small fourth ventricle) (Geerdink et al. 2012). Therefore, taking into account the biases related to their statistical analysis, the authors proposed to base the diagnosis of C-II mainly on these nine features.
Morphometric and volumetric MRI analysis of PCF should be obtained for a correct diagnosis and surgical planning, although this aspect is less relevant than in C-I (Massimi et al. 2011b; Sgouros et al. 2006; Trigylidas et al. 2008). Phase-contrast cine MRI provides information on the CSF flow patterns during the cardiac cycle revealing dorsal and/or ventral obstruction/reduction/inversion of the CSF flow at the foramen magnum. It can be integrated by 3D reconstruction of the subarachnoid spaces (Roldan et al. 2009). Also this type of MRI plays a role in C-I rather than C-II.
CT scan (with 3D reconstructions) is required to deepen the diagnosis of C-II associated bony abnormalities or to obtain a quick diagnosis when, for example, a shunt malfunction/decompensated hydrocephalus is suspected. Head CT scan (and X-rays) reveals the typical dysplastic lacunae involving the inner and outer layers of the skull (the so-called Lückenschädel or “beaten copper”), which are present at birth in about 85% of cases and disappear later (Naidich et al. 1980). They are not a sign of raised intracranial pressure (and must not be confused with fingerprintings) but the expression of an intrinsic mesenchymal defect. On the contrary, during late childhood and adolescence, CT scan may reveal a significant thickening of the skull as result of early shunting in hydrocephalic patients. Further cranial anomalies well detected by CT scan are the following (Raybaud and Miller 2008): enlarged foramen magnum and upper cervical canal, short and scalloped clivus, the absence of basilar impression or invagination, scalloping of the petrous pyramids, shortening of the auditory canals, flattened and convex upward occipital squama, and incomplete neural arch of C1 (70% of cases) with intact C2. The inion is low as well as the attachment of the tentorium and the markings of the venous sinuses (important information for the surgical planning).
Plain X-rays are used to rule out instability of the cranio-cervical junction and to monitor the progression of the scoliosis or other associated orthopedic spinal (kyphosis, hyperlordosis) and non-spinal deformities (hip subluxation or dislocation, coxa valga, knee deformities, ankle and foot abnormalities). The latter is the most frequent and important application of X-rays, since they provide quick and useful information, limiting the use of CT scan. In particular, the monitoring of spinal deformities is crucial because they can be developmental or acquired during the late childhood and adolescence other than congenital or acquired early (Guille et al. 2006).
Ultrasounds maintain a role in neonates and infants with open bony acoustic windows. They are very useful for monitoring the ventriculomegaly and for detecting an incipient hydrocephalus (which, as mentioned, can worsen the associated C-II). C-II can be visualized through a favorable acoustic window (posterior or temporal fontanel rather than anterior fontanel), even though ultrasounds are not the best options to evaluate its extension or its possible evolution. The small PCF and the effaced IV ventricle (often not visualized because compressed and herniated) are quite clearly depicted as well as the corpus callosum and/or septum pellucidum agenesis/dysgenesis, the large massa intermedia, and the prominent interhemispheric fissure.
Other Diagnostic Tools
Polysomnography is complementary to neuroimaging for completing the diagnostic work-up in C-II. It allows to detect the presence and severity of sleep apnea and to differentiate between central and obstructive (peripheral) apnea syndrome. It also permits to identify possible epileptic seizures. Sleep apnea was present in 81% of the 52 patients analyzed by Patel et al., with a mild apnea in 50%, moderate in 19%, and severe in 12% (Patel et al. 2015). Several specific studies demonstrated that (Alsaadi et al. 2012; Filho and Pratesi 2009; Patel et al. 2015; Waters et al. 1998):
-
1.
Sleep-disordered breathing is highly prevalent in children with OSB/C-II, although it might be underreported.
-
2.
Both central and peripheral/obstructive apnea can occur. Central apnea is more specific, and usually, they are more frequent than obstructive one (though not in all series).
-
3.
The severity of apnea syndrome is increased by the presence of brainstem and pulmonary malformations, the level of the spinal defect (thoracic or thoracolumbar), and a previous PCF decompression (indicating a symptomatic C-II).
-
4.
PCF decompression does not seem to significantly improve the frequency of apnea (both central and obstructive) and the hypopnea/apnea index.
-
5.
There is a clear correlation between apnea syndrome and attention deficits, with subsequent poor quality of learning and cognitive deficits.
-
6.
Nocturnal pulse oximetry and possible oxygen supplementation are mandatory for a correct management. Adenotonsillectomy may be required to improve obstructive apnea.
Brainstem auditory evoked potentials (BAEPs) are the most sensitive neurophysiologic test to find out brainstem dysfunction. They can be successfully coupled with the study of brainstem reflexes (blink reflex, masseter reflex) (Massimi et al. 2011a). According to specific studies on C-II (Fujii et al. 1997; Nishimura and Mori 1996; Nishimura et al. 1991; Worley et al. 1994):
-
1.
The sensitivity of BAEPs is very high, more than 90% of children with brainstem dysfunction showing altered BAEPs even before the appearance of clinical signs. Abnormal BAEPs are found in up to 40% of patients without clinical signs.
-
2.
The brainstem dysfunction improves over the time, as result of neural maturation, as indicated by a progressive shortening of wave latency and I–III and III–IV inter-peak latency.
-
3.
The persistence and/or worsening of the BAEPs abnormalities may be helpful for the surgical indication.
-
4.
The blink reflex can complete the neurophysiological diagnosis of brainstem dysfunction by disclosing subclinical lesions not detected by BAEPs.
Special Considerations on Two Frequent Associated Diseases
Hydrocephalus and syringomyelia associated to C-II deserve a special mention because of some peculiarities in their clinic-radiological picture and management.
Hydrocephalus
Hydrocephalus occurs in about 80–90% of patients with OSB and C-II, without a clear correlation with the level and entity of the myelomeningocele and C-II (Januschek et al. 2016; Mirzai et al. 1998; Perez da Rosa et al. 2015). Typically, hydrocephalus is present only in a minority of cases at birth (15–25%), since it tends to develop after the closure of the myelomeningocele, usually during the first weeks of life (Chakraborty et al. 2008; Dias 1999; Drake 2008; Tude Melo et al. 2015). A second typical feature of C-II-related hydrocephalus is the clinical manifestation. An active hydrocephalus, indeed, may cause signs and symptoms of brainstem dysfunction (see above) before that the typical picture of raised ICP appears (macrocrania, bulging fontanel, sunset-rise eyes, bulging of the scalp vein, vomiting). This must be taken in consideration to avoid a missing diagnosis and severe complications (like respiratory arrest).
Also the radiological appearance of hydrocephalus is peculiar. Besides the aforementioned characteristics of the lateral and third ventricles and aqueduct, MRI or CT scan shows a large ventriculomegaly with raised ICP signs (bulging profile of the ventricles, CSF transependymal readsorption) only in one fifth/one fourth of the cases (Fig. 4), while often it is about a progressing but moderate ventriculomegaly (Van Roost et al. 1995). On the other hand, the colpocephaly should not be misinterpreted as an active hydrocephalus.
Active hydrocephalus is managed as soon as possible with shunt placement. It usually happens at birth or within the first weeks/months of life. As known, endoscopic third ventriculostomy is not effective in newborns/infants with OSB, but it can be successfully used in older children in case of shunt malfunction (O’Brien et al. 2005; Spennato et al. 2013). Mild to moderate ventriculomegaly can be followed up and treated in case of progression. The last peculiarity of hydrocephalus in C-II is the deterioration of the scoliosis as a possible sign of progression of an untreated ventriculomegaly: in this instance, the shunt insertion improves the scoliosis (Geiger et al. 1999; Hall et al. 1979). Indeed, it has been postulated that the hydrocephalus, by worsening the hindbrain herniation, increases the compression on the descending pathways at the cranio-cervical junction producing the muscular weakness necessary for the scoliosis to progress in a spine already compromised by the OSB.
Syringomyelia
Syringomyelia in C-II presents some differences with the most common form of syringomyelia, which is associated with C-I. The first difference, indeed, is just the frequency because C-I is the most common cause of syringomyelia while C-II accounts only for about 5% of all cases (Williams 1990). Of course, this difference results from the lower incidence of C-II compared with C-I.
The second difference concerns the pathogenesis, partially shared with C-I-related syringomyelia. The first observations on syringomyelia (which are used to explain C-I-related syringomyelia) were based on patients with C-II and spinal bifida. In his second publication on these malformations, indeed, Chiari advocates the duration of hydrocephalus and its communication with a patent central ependymal canal as possible cause of C-II and syringomyelia (Chiari 1896). Also the famous Gardner’s hydrodynamic theory resulted from observations on C-II patients (Gardner 1965): it postulates an occlusion of the IV ventricle foramina and the absence of communication between the spinal canal and the IV ventricle (currently, it is ascertained that the foramina and, sometimes, even the obex are patent in C-I patients and that a communication between IV ventricle and ependymal canal can be radiologically demonstrated in C-II patients) so that the choroid plexus pulsations redirect the CSF into the spinal canal causing syringomyelia. Similarly, the development of this theory by Williams (1975, 1990) and Oldfield et al. (1994), which postulates the hindbrain herniation and the collection of CSF inside the ependymal canal as result of a missed equilibrium between the endoventricular and the endospinal pressure during the Valsalva maneuver (this hypothesis is not valid for C-II which is present already during the fetal life and does not explain the small PCF and the upward ectopia of the cerebellum), was formulated considering patients with C-II and aqueduct stenosis.
Some pathological, clinical, and radiological differences between C-I and C-II support such a difference in the pathogenesis of their related syringomyelia:
-
1.
C-II is a more severe form of hindbrain herniation where the large amount of herniating tissue and the dense arachnoid adhesions do not permit evident pulsations and movement of these structures. In C-I, instead, the prolapsed cerebellar tonsils can follow the pulsation of the cardiac cycle, giving reason of the hypotheses based on their “piston” action on plugging the foramen magnum.
-
2.
Most of the patients with C-I and syringomyelia are symptomatic, while most of those with C-II and syringomyelia are not. As mentioned, C-II patients usually do not develop symptoms directly by the malformation but by decompensated hydrocephalus (which can decompensate also the syringomyelia).
-
3.
Syringomyelia develops progressively both in C-I and C-II. However, in many cases of C-I, the syringomyelia is already present at diagnosis, differently from C-II cases where it is rarely seen at birth and where it usually develops during the early-to-late childhood (La Marca et al. 1997; Milhorat et al. 1993). Of course, such a discrepancy may depend on the early diagnosis of C-II, which is known already during the prenatal period.
-
4.
The trend of C-II and its related syringomyelia strongly depends on the behavior of the associated hydrocephalus, which is present in 80–90% of cases. In C-I patients, hydrocephalus is present only in 7–10% of cases, and its relationship with the malformation and its related syringomyelia is still a matter of debate (Massimi et al. 2011b).
-
5.
Syringomyelia in C-II patients may be worsened (or originated) also by the myelomeningocele (viz., recurrent tethered cord) (Caldarelli et al. 2013).
-
6.
There is not a clear relationship between entity of the C-II hindbrain prolapse and occurrence or severity of syringomyelia, while a certain correlation between entity/crowding of C-I and frequency/severity of syringomyelia exists (Taylor et al. 2017).
-
7.
On MRI, differently from C-I, where syringomyelia is mainly cervical and seldom loculated, C-II-related syringomyelia is usually thoracic (frequently holocord, with syringobulbia) and not rarely multiloculated (Fig. 5). In C-II, the central ependymal canal is typically showed to communicate with the cerebral ventricles through the obex, thus justifying the aforementioned dependence of C-II and syringomyelia from the hydrocephalus (Raybaud and Miller 2008). The patency of the ependymal canal would result from the leakage of the ventricular CSF during the embryonal and fetal life. Chronic, long-lasting syringomyelia may produce a significant thinning of the spinal cord with enlargement of the spinal canal and thinning of the vertebral bodies and the neural arches.
Syringomyelia in C-II patients is often detected incidentally during the radiological follow-up. In the clinical practice, since this condition is well tolerated by the patients, no surgical treatment is proposed even in case of large syrinx with significant thinning of the spinal cord (Sgouros 2008). These patients are actually followed up and treated only if symptomatic because only a small proportion of them will require surgery (Caldarelli et al. 1998). However, once again, in OSB patients, it can be very hard to distinguish among signs/symptoms of hydrocephalus, C-II syringomyelia, and tethered cord. Based on the personal experience, which is in large part shared with the literature (Dias 2005; Piatt 2004; Tubbs and Oakes 2004), the following management protocol is adopted:
-
1.
First of all, if present, an active hydrocephalus/shunt malfunction is treated.
-
2.
Once hydrocephalus/shunt malfunction is ruled out, a differentiation between C-II and tethered cord is necessary. Urologic signs and urodynamic tests may be helpful in pointing out an active tethered cord, so that a surgical detethering is performed.
-
3.
When also a tethered cord has been excluded, a PCF decompression is realized for the indirect treatment of the syringomyelia.
-
4.
A direct surgical approach to the syringomyelia (syringo-subarachnoid shunt) is performed only if all the previous options failed. Indeed, syringo-arachnoid or syringo-pleural shunts do not provide good and long-lasting results in many cases, though better results in OSB patients are reported (Vernet et al. 1996).
Management
C-II in asymptomatic patients is managed by a long-term follow-up. In newborns and small infants, close clinical evaluations and cerebral ultrasounds are planned during the first year of life to check for the absence of specific symptoms and for the monitoring of the hydrocephalus. Serial controls are then carried out after the first year of life with clinical (at least once per year or more, according to the patient’s characteristics) and neuroradiological examinations. At our institution, based on a protocol for OSB patients, we perform a first brain and spinal cord MRI at birth, then during the second year of life, and then, if the clinical picture is stable, each 3–4 years up to the end of the psychophysical development. Polysomnography also is performed each 3–4 years in clinically stable patients.
When dealing with a symptomatic newborn or infant, the neonatal or the pediatric intensive care unit should be alerted in case of acute onset. Since the clinical picture may quickly deteriorate, an urgent CT or MRI has to be performed to rule out hydrocephalus and/or cervical syringomyelia/syringobulbia. Although more rarely, an acute deterioration may occur also in older children and adolescents where the management protocol is the same. More frequently, however, this subset of patients shows a progressive deterioration with a variable combination of symptoms like occipito-cervical pain, sleep apnea syndrome, limb weakness, ataxia, and paresthesia. In this instance, the pre-treatment work-up should include physical and neuroradiological examinations and polysomnography. It is worth stressing once more that, in these patients, the C-II symptoms often result from raised ICP due to shunt malfunction (but without the classic symptoms of shunt malfunction) and disappear after the shunt revision. We published elsewhere the case of a 6-year-old boy presenting C-II deterioration with severe OSAS (confirmed by polysomnography) (Luigetti et al. 2010). Brain MRI showed a stable picture within the PCF and the spinal canal but the enlargement of one of the several cystic components of the patient’s multiloculated hydrocephalus. Both the clinical picture and the polysomnography were normalized after the endoscopic cyst fenestration/shunt revision.
Once hydrocephalus or other causes of raised ICP have been excluded, the preoperative work-up is completed by angio-MRI for the correct planning of the PCF decompression. This exam is needed to check for the position of the torcula and to look for possible accessory and/or anomalous dural sinuses. In some instances, a CT scan of the occipito-cervical junction is required to rule out bony anomalies and/or instability of the junction. Neurophysiological exams are used to complete the preoperative work-up, especially in case of syringomyelia. Indeed, ABRs, MEPs, and SSEPs may be helpful in assessing the neurological deterioration in doubtful cases, that is, when a mismatch between clinical and radiological worsening exists.
Indications for Surgery
Patients with new-onset hydrocephalus or with shunt malfunction are managed according to the routinary surgical procedures required in such instances. It is worth reminding that a CSF shunt malfunction can be hard to be excluded especially in old children and adolescents with OSD because the signs/symptoms of raised ICP may be missing and may be replaced by misleading ones (Bianchi et al. 2016). Therefore, the shunt patency/functioning must be ascertained by careful neuroimaging analysis and, in doubtful cases, by shunt tapping or even surgical exploration. Among the 50 pediatric patients (mean age, 7.1 years) operated on for deteriorating C-II by Messing-Jünger and Röhrig, 38 cases needed shunt revision (76%), 13 surgery for scoliosis/kyphosis (26%), 17 myelolysis for tethered cord (34%), and “only” 14 a PCF decompression (28%) (Messing-Jünger and Röhrig 2013).
PCF decompression is performed in clearly symptomatic patients without other causes of C-II deterioration or in case of progressing syringomyelia. In the neonatal and early infancy period, the cranio-vertebral decompression should be carried out as soon as the hydrocephalus has been ruled out because an early decompression seems to ensure a better outcome (Pollack et al. 1996; Vandertop et al. 1992). Nevertheless, the matter about this indication is quite controversial (Sgouros 2008). Indeed, it has been observed that children undergoing a very early decompression (within the second month of life) do not show a clinical recovery and usually need tracheostomy and gastrostomy to be managed. This is because the symptoms of this subset of children would result from an intrinsic brainstem dysfunction more than a brainstem compression. Therefore, it could be speculated that, in this instance, the cranio-vertebral decompression could be even avoided. On the other hand, children undergoing surgery later (after the second month of life) show a significantly better outcome (especially if they do not have experienced a vocal cord paralysis yet) because their clinical picture is more likely to result from a brainstem compression.
Surgical Decompression
C-II requires both PCF and cervical spinal cord decompression. PCF decompression usually involves the occipital squama more than the foramen magnum, which is often enlarged by the early cerebellar/brainstem herniation. However, since the foramen magnum is already enlarged, the occipital squama is very small (the transverse sinuses are at almost level of the foramen magnum), and the cerebellum is located in part in the cervical canal and in part in the middle fossa; the decompression of PCF is usually very limited, and the real surgical decompression involves the upper cervical canal (Mc Lone 2011). Cervical laminectomy is carried out up to C3 or more, according to the cerebellar prolapse. Duraplasty is performed to improve the decompression, whereas, generally, the coagulation/removal of the cerebellar tonsils is not attempted because of their very dysmorphic appearance that increases the risk to damage the ectopic IV ventricle or the spinal cord.
Because of the peculiar anatomy of the PCF in OSB patients, some key points must be carefully considered for a correct cranio-vertebral decompression:
-
1.
Bone lacunae on the occipital squama. Care should be taken during the muscle dissection not to enter the dura (especially in infants, where the bone is thin).
-
2.
Lower position of the torcula and accessory dural sinuses. The dural incision should be accurately planned based on the preoperative neuroimaging because the injury of the venous sinuses can be a life-threatening complication (in particular, in neonates and infants). The anular sinus, located at the rim of the foramen magnum, is almost invariably encountered, and facing it may be the most dangerous part of the operation.
-
3.
Subverted “subarachnoid” anatomy, with the cerebellum, IV ventricle, and medulla within the upper cervical canal. Particular care should be paid during the opening of the dura to avoid injury of these underlying neural structures because they are significantly compressed and the subarachnoid spaces virtually absent (so that an evident herniation of the content of the spinal canal above the dural plane occurs after the dural decompression). Moreover, every attempt of manipulation of the parenchymal structures should be avoided unless they are clearly recognized. Indeed, although the parenchymal dissection might be useful to obtain a better decompression through the removal of the malformed herniating cerebellar tissue, this procedure is significantly complicated by the dense arachnoid adhesions and the hypervascularity of the parenchymal surface (Fig. 6). Differently from the intradural manipulation in C-I, however, the tonsils coagulation and the opening of the IV ventricle are not mandatory in C-II. Should a parenchymal decompression be necessary (e.g., in case of very large syringomyelia), a gentle subpial coagulation of the inferior vermis (only if recognizable) can be performed by keeping the IV ventricle opened in the subarachnoid spaces (Fig. 7).
-
4.
Lack of dural tissue for the closure (because of the parenchymal herniation). A capacious duraplasty is needed for an optimal decompression. It necessarily relies on the use of pericranium or dural substitutes, unless the dura is left opened (so-called pseudomeningocele technique). Some authors performed only a bony decompression of PCF and upper spinal canal (at most with external dural delamination) to avoid the complications of the dural opening with success (Akbari et al. 2013; Ogiwara and Morota 2013). Their preliminary results were encouraging (especially in young infants) and even better than those of children undergoing duraplasty (although the latter aspect may reflect a patients’ selection bias).
-
5.
Malformations of the cervical spine. The management of these malformations is treated in the specific chapters. They are mentioned here since they represent a further, important reason for an accurate preoperative planning.
Results and Prognosis
In the natural history of C-II, the neurological deterioration is expected in 9–18% of cases (Caldarelli et al. 1995; Hoffman et al. 1975). In the personal experience with about 800 OSB cases in the last 30 years, the rate of deterioration requiring surgery was 8%. Similarly, Talamonti and Zella reported on 228 subjects with C-II, 74 of which became symptomatic (31.5%) requiring surgical decompression in 26 cases (11.4%) (Talamonti and Zella 2011). In 12 out of those 26 patients, the first treatment concerned the hydrocephalus.
The results of the surgical decompression mainly depend on the preoperative status. A complete clinical resolution (or a substantial improvement) is expected in patients whose C-II signs/symptoms are caused by raised ICP or even in infants presenting with late stridor alone (Pollack et al. 1996). Similarly, a good outcome is found in patients operated on for scoliosis and/or syringomyelia resulting from C-II (once again, mainly late deterioration) (Messing-Jünger and Röhrig 2013). In the other instances, a stabilization or mild improvement of the clinical picture is more frequently obtained than a complete recovery, and a risk of mortality is recorded (Caldarelli and Di Rocco 2010; Pollack et al. 1992; Vandertop et al. 1992). Infants with early stridor and apneic spells show a functional recovery and a survival in 50% and 75% of cases, respectively. In more complicated pictures (stridor, apneic and cyanotic spells, dysphagia), the chance of survival drops to 40% with minimal functional recovery. Such a dismal prognosis results from the irreversible brainstem dysfunction and from the anatomical disarrangement of the PCF structures that do not benefit from any surgical procedure. The older experience by the Hospital for Sick Children of Toronto (1971–1981) on 85 cases with neurological deterioration showed newborns affected (45 cases, 53%) much more than infants (20%), toddlers/children (13%), and adolescents (14%) (Hoffman et al. 1975; Hoffman et al. 1983). Ten patients needed a tracheostomy (12%), which was realized after the surgical decompression in 8 out of 10 cases. The C-II-related mortality was as high as 33% (28/85 cases), occurring almost exclusively within the first year of life (26/28 cases). All the surviving patients experienced a complete recovery.
An updated experience by the same group carried out a decade later (1981–1991) on 17 children treated early (1 to 121 days from the clinical onset) showed the same outcome but with a significantly lower mortality rate (overall 12%; only 6% for sequelae from C-II) (Vandertop et al. 1992). The authors attributed this improvement to the early decompression and concluded that C-II deterioration results from the compressive injury rather than on the brainstem intrinsic dysfunction (which is advocated in children with symptoms at birth). This statement reflects the absence of a conclusive knowledge on this topic and the lack of guidelines on the management of C-II (Messing-Jünger and Röhrig 2013). The surgical decompression of PCF, indeed, seems to be able to normalize the CSF spaces within the PCF and, if performed very early, to reduce the occurrence of symptoms even though it does not prevent the cerebellar atrophy (Salman 2011). Nevertheless, the resulting discrepancy between decompressed PCF and persistent cerebellar atrophy should be emphasized (Vinchon 2011). Similarly, the spinal cord detethering seems to be able to improve C-II symptoms, but it cannot induce a complete clinical resolution, and as expected, it does not induce significant changes of the radiological picture; therefore, it can be proposed only for poorly symptomatic children (Mehta et al. 2011).
Symptomatic C-II accounts for the mortality among OSB patients together with renal failure due to neurogenic bladder dysfunction and shunt malfunction. The mortality rate, which was up to 47% according to old statistics (Center for Disease Control and Prevention 1995), is now less than 25% at long-term follow-up (Bowman et al. 2001). C-II is responsible for the early mortality, while the other two causes account for the late (and more frequent) mortality. The mortality rate among early symptomatic C-II patients is 15–35% (McLone 1992; Oakeshott and Hunt 2003).
The prognosis of C-II has improved since the introduction of prenatal surgery for OSB. Fetal surgery would produce this enhancement by stopping the CSF leakage from the myelomeningocele site, by protecting the exposed spinal cord and roots from the action of the amniotic fluid (“double-hit theory”), and, possibly, by reducing the risk of vernix caseosa meningitis (Dionigi et al. 2015a; Stritzke et al. 2011). Early fetal surgery (before 25–26 weeks) has been demonstrated to substantially improve the hindbrain herniation (Abd-El-Barr et al. 2014; Tulipan et al. 1999). The effects of the in utero repair of the myelomeningocele on C-II are so evident that the incidence of this condition can drop from 95–98% up to 38% and a complete reversion of the malformation can be often noticed after surgery (Bruner et al. 1999; Sutton et al. 2003). These results have been confirmed also experimentally. For example, the prenatal myelomeningocele repair was able to induce a reversion of the hindbrain herniation in fetal sheep within 3 weeks from surgery (Bouchard et al. 2003). Moreover, the simple trans-amniotic injection of stem cells (TRASCET) has proved to significantly reduce the C-II in rats with OSB (Dionigi et al. 2015b). Randomized trials, like the MOMS trial and the post-MOMS trials, confirmed the improvement of the hindbrain herniation following the prenatal repair of OSB together with the reduced rate of shunt insertion (Adzick et al. 2011; Tulipan et al. 2015). Yet the reduced occurrence of active hydrocephalus has a positive prognostic value for the natural history of C-II. It is worth reminding that, however, prenatal surgery cannot be considered as a complete treatment of OSB and C-II, highly specialized and qualified centers are needed to be realized, and the benefits should be balanced with the maternofetal risks (Adzick 2013; Meuli and Moehrlen 2014).
Chiari Type III Malformation
Definition and Epidemiology
C-III is defined by the combination of C-II findings with an occipital or cervical meningoencephalocele. This severe condition is very rare, accounting for less than 1% of Chiari malformations (Caldarelli and Di Rocco 2010), varying from 0.65% to 4.4% in large series (Cama et al. 1995; Isik et al. 2009). The estimated incidence of encephalocele is 1–2/5000 live births (about 75–90% of them being occipital) (Furtado et al. 2009; Kiymaz et al. 2010). According to the extensive review by Ivashchuk et al., from the first description by Chiari in 1891 to 2015, 57 subjects have been reported in literature, almost exclusively by case reports except for a couple of small series with 8–9 cases (Ivashchuk et al. 2015). Among these patients, the encephalocele was located in the low occipital/upper cervical region in 40% of cases, in the low occipital position in 30%, and in the upper cervical one in 14% (in 16% of cases, this information was not available).
Pathogenesis
The pathogenesis of C-III is still unclear. The main attempts to explain it are based on the theories used for C-I, C-II, and OSB. Actually, the following hypotheses have been propounded so far:
-
1.
C-III would result from a chronic escape of CSF at level of the occipito-cervical neural tube defect, inducing underdevelopment of the cerebral ventricle and PCF (McLone and Knepper 1989). The main limit of this theory, which remains the most advocated one, is the lack of an obvious CSF leakage in many cases.
-
2.
The distention of the embryonic ventricular system would be prevented by a primary neuroectodermal defect leading to an abnormal neurulation with following hypoplasia of PCF and herniation of its content (Cakirer 2003).
-
3.
PCF hypoplasia and bone defect would result from an insufficient endochondral bone development due to the poor induction by the neural tube defect (Ramdurg et al. 2013) or to a primary mesodermal defect (Kiymaz et al. 2010).
-
4.
The absence of C-III in animal models of surgically induced myeloschisis (Sim et al. 1996) suggests a predominant role of altered CSF dynamics rather than failed neurulation-induced or primary mesenchymal defect (Lee et al. 2002; Smith et al. 2007).
Pathological Anatomy
C-III shares with C-II some of its main pathological characteristics (see also Table 2) (Cesmebasi et al. 2015):
-
1.
Bony anomalies: small PCF, enlarged foramen magnum, scalloping of the clivus and the posterior petrous bones, Lückenshädel, and malformations of the upper spinal canal (like missed fusion of the posterior C1 arch) (Atlas 2009). Specific features of C-III are the possible hypoplasia of the parietal bones and the possible posterior cervical agenesis (missing posterior elements from C1 to C5) (Castillo et al. 1992).
-
2.
Intracranial/intraspinal anomalies: caudal displacement of the cerebellar tonsils, vermis, and IV ventricle, enlarged or lacking cerebellum, medullary kinking, tectal beaking, callosum dysgenesis, colpocephaly, hydrocephalus (up to 88% of cases), ectopic and/or aberrant venous sinuses, aplasia of the posterior falx, and syringomyelia (up to 70% of cases) (Atlas 2009; Cakirer 2003). The distinctive trait is represented by the herniation of the cerebellum through an occipital or upper cervical defect, which realizes a PCF encephalocele. In the most severe cases, the herniated tissue includes the brainstem, the occipital lobes and even the parietal ones, the dural venous sinuses, and the subarachnoid spaces (Castillo et al. 1992). Sometimes, the herniation is composed by an occipital encephalocele plus meningocele (Muzumdar et al. 2007).
The microscopic anatomy of the herniating tissues reveals abnormal and nonfunctioning neural tissue with necrosis, reactive astrocytosis and gray matter heterotopia, areas of gliosis, meningeal inflammation, portion of ventricles, and choroid plexus (Castillo et al. 1992; Isik et al. 2009).
Diagnosis
The diagnosis (or, at least, the strong suspect) of the disease is obtained during pregnancy by ultrasounds showing the evident malformation involving the posterior fossa (Aribal et al. 1996; Caldarelli et al. 2002). The earliest prenatal diagnosis by ultrasounds was done at 18 weeks and by MRI at 23 weeks (Ivashchuk et al. 2015). The prenatal diagnosis is mandatory for a correct planning of the delivery (cesarean section) and the postnatal management (Smith et al. 2007).
MRI (in utero and after the birth) demonstrates all the complexity of the condition, in particular the large encephalocele protruding through the bony defect extending from the occipital squama (lower aspect) to the upper spinal canal (posterior arch of the first cervical vertebrae), the small posterior fossa with hypoplastic cerebellum herniating into the malformation, the low attachment of the tentorium, the scalloping of the clivus, the dysgenetic corpus callosum, and the hydrocephalus (variable severity) (Rani et al. 2013) (Fig. 8).
The differential diagnosis of C-III is with other Chiari malformations (see also Table 2) and iniencephaly. Iniencephaly (or iniencephalus) is a rare congenital anomaly (0.1–10/10,000 pregnancies) characterized by large occipital defect with enlarged foramen magnum, spina bifida of the cervical vertebrae with absent neck, and fixed retroflexion of the head (Chikkannaiah et al. 2014; Erdincler et al. 1998; Kulkarni et al. 2011). The associated anomalies are numerous, concerning both the spine and chest (e.g., absent vertebrae, Klippel-Feil syndrome, Sprengel’s deformity, malformed thoracic vertebrae, nuchal tumors) and the brain (e.g., anencephaly, hydrocephaly, cyclopia, microcephaly, polymicrogyria, holoprosencephaly, and atresia of the ventricular system). It is classified as apertus (open) or clausus (closed) according to the presence of encephalocele (Fig. 9).
Clinical Picture
The clinical picture is dominated by symptoms and signs of encephalocele. Generally, there is a strict correlation between the severity of the PCF herniation and the severity of the clinical picture (Bulut et al. 2013; Sirikci et al. 2001).
At inspection, a large and soft occipital mass, usually covered by normal or dyschromic skin, is evident (Fig. 10a), while a skin defect is rarely observed. The most typical clinical findings are respiratory distress, aspiration pneumonia, stridor, dysphagia, nystagmus, hypotonia or spasticity, sensory loss, and ataxia (Cakirer 2003; Caldarelli et al. 2002; Isik et al. 2009; Muzumdar et al. 2007). In the most severe cases, a respiratory failure is present at birth. Several associated findings have been reported to complicate the clinical picture in rare cases, as cerebellar hematoma and congenital heart disease (Bulut et al. 2013), large diaphragmatic defect (De Reuck and Thienpont 1976), microcephaly and hypertelorism (Garg et al. 2008), syndactyly and polydactyly (De Chalain et al. 1994), proatlas anomaly (Garg et al. 2011), and scoliosis (Isik et al. 2009). On the other hand, Dandy-Walker malformation, Klippel-Feil syndrome, and split cord malformation are relatively common (Castillo et al. 1992; Erol et al. 2011).
It is worth noting that some asymptomatic cases have been described (Ramdurg et al. 2013; Sirikci et al. 2001). The diagnosis was obtained even at 14 years of life (Cakirer 2003).
Management
Children with C-III often require an initial admission in intensive care unit because of the young age (they often need treatment soon after the birth) and the possible, severe respiratory distress. Since the condition may be lethal if untreated, the management consists of the primary closure of the malformation. Occipital or cervical encephalocele is not necessarily burdened by a worst prognosis, and this is a further argument in favor of their repair.
The timing of surgery is debated. Indeed, some authors advocate an early repair to avoid long-lasting brainstem and spinal cord compression/dysfunction, whereas other authors suggest a late closure, to allow the patient to grow and undergo a safer operation, unless a skin defect is present (Garg et al. 2011; Isik et al. 2009; Jaggi and Premsagar 2007; Snyder et al. 1998). A preoperative shunt or external drainage has been used to favor the detention of the PCF content and/or to delay the closure of the encephalocele (Agrawal et al. 2011; Caldarelli et al. 2002; Snyder et al. 1998). As for other encephalocele, the repair consists of a resection of the nonfunctioning herniating tissue, trying to preserve as much as possible the neurological functions of the healthy neural tissues, careful dissection of the PCF structures and their accommodation in an enough large space to prevent the re-tethering, and dural reconstruction and watertight closure. Intraoperative neurophysiological monitoring can be helpful in driving the surgical dissection, although the chaotic anatomy and the patients’ young age may make it less sensitive than in other instances. MRI with DTI (diffuse tensor imaging) has been proposed for evaluating the position of the descending tracts preoperatively in order to better identify the resectable, herniating tissues (Zolal et al. 2010). In case of large bony defects, a cranioplasty and rotation of the surgical skin flap may be required (Furtado et al. 2009). The cranioplasty is necessary to prevent the occurrence of pseudomeningocele. The rotational skin flap is indicated when the dystrophic or the lacking skin does not ensure an adequate covering at site of the repair (Fig. 10b).
Prognosis
In spite of the prompt surgical treatment, the prognosis of C-III remains poor in several cases. Negative prognostic factors are represented by stridor at birth, poor neurological status before surgery, large encephalocele, and hydrocephalus (Agrawal et al. 2011; Kiymaz et al. 2010; Muzumdar et al. 2007). As expected, the amount of herniating brainstem is crucial, a better outcome being registered in case of ectopia less than 5 cm (Isik et al. 2009).
Apart from the high risk of spontaneous and surgical mortality (overall rate, 29%) (Cesmebasi et al. 2015; Kiymaz et al. 2010), the surviving children almost invariably show a developmental delay (variable severity), motor deficits with hypotonia or spasticity, lower cranial nerve deficits, epilepsy, and, sometimes, persistent respiratory distress needing tracheotomy (Caldarelli and Di Rocco 2010; Furtado et al. 2009). Once again, these sequelae are attributed to a primary brainstem dysfunction and/or to a secondary damage resulting from the distortion and traction of the brainstem by the malformation.
In the most favorable cases, on the other hand, the respiratory distress quickly improves in up to 80% of cases (Isik et al. 2009). Even patients with a normal life have been reported (Iskandar et al. 1998).
Chiari Type IV Malformation
The use of the term “C-IV” still generates some misunderstandings. According to the original Chiari’s description, C-IV is characterized by hypoplasia of the cerebellar hemispheres (not aplasia) and small PCF, without hindbrain herniation through the foramen magnum but with occipital encephalocele through a relatively small bony defect below the posterior fontanel (Chiari 1896; Tubbs et al. 2016). Other associated anomalies are small foramen magnum, split of the superior sagittal sinus around the encephalocele, narrowed tentorium, aplasia of the falx cerebelli, elongated inferior medullary velum, rolled inferior vermis, hydrocephalus, normal pons, and medulla oblongata. Chiari stressed the presence of occipital encephalocele with supratentorial content as the main feature of this malformation. On these grounds, only the cases of hypoplasia of PCF and its content with occipital encephalocele can be considered as C-IV.
The confusion on the Chiari’s description was probably induced by the misinterpretation of the Cruveilhier’s report on a specimen of cerebellar hypoplasia and funnel-shaped PCF (Tubbs et al. 2016). As a consequence, any form of cerebellar hypoplasia or aplasia (primary cerebellar agenesis (PCA), Dandy-Walker malformation complex, vanishing cerebellum) without hindbrain herniation was considered as C-IV in spite of the differences with the original Chiari’s description (Brownlee et al. 1997; Chaudhari et al. 2008; Raimondi 1972; Tekin et al. 2002). Such an improper classification was used not only in the absence of occipital encephalocele or hydrocephalus but also in the presence of pontine (or brainstem) anomalies or even C-III.
Currently, PCA is the condition more frequently referred as C-IV (Boltshauser et al. 2002; Sener and Dzelzite 2003; Tubbs et al. 2012). PCA is characterized by complete agenesis of the cerebellar tissue (except for possible remnants of the anterior quadrangular lobes), resulting from several congenital or acquired disorders, with a normal-sized PCF filled by CSF (Alkan et al. 2009; Titomanlio et al. 2005). Mild mental retardation and a variable degree of cerebellar dysfunction (usually ataxia, dysmetria, and nystagmus) are the clinical features. The most similar condition to PCA is represented by the vanishing cerebellum where, however, the cerebellar “agenesis” is subtotal and results from a mechanically induced ischemia, PCF is small, and all the intracranial signs of C-II are present.
The outcome of “original” C-IV depends on the encephalocele and the coordination deficits related to the cerebellar hypoplasia, thus configuring a better prognosis than that expected on the basis of some of the other “similar” conditions.
Chiari “Type V” Malformation
This entity has been presented by Tubbs et al. on 2012 (Tubbs et al. 2012). The reported case was characterized by sacral myelomeningocele, hydrocephalus, vanishing cerebellum, and herniation of the occipital lobes into the foramen magnum. The child was managed by myelomeningocele repair, shunt placement for associated hydrocephalus, and tracheostomy for stridor and was alive and in quite good clinical condition at 6 months follow-up (awake, mild delay, tracking with eyes, movements of upper and lower extremities). The herniation of the occipital lobes through the foramen magnum is exceptional. Previously, it has been reported as a feature of very severe C-II in a calf (Testoni et al. 2010). Also a temporal lobe herniation, with partial occipital herniation, in a human C-II has been described (Udayakumaran et al. 2010). On these grounds, it has been postulated that the occipital herniation could result from the combination of the C-II pathogenesis with a significant tentorial defect and a prenatal hydrocephalus, thus configuring a “C-II plus” (Udayakumaran 2012). However, the case presented by Tubbs and coworkers shows the unique combination of occipital herniation and the absence of the cerebellum, and no similar cases have been reported so far, so that the authors claimed for it the definition of “C-V” (Tubbs and Oakes 2012).
References
Aaronson OS, Hernanz-Schulman N, Bruner JP, Reed GW, Tulipan NB (2003) Myelomeningocele: prenatal evaluation – comparison between transabdominal US and MR imaging. Radiology 227:839–843
Abd-El-Barr MM, Strong CI, Groff MW (2014) Chiari malformations: diagnosis, treatments and failures. J Neurosurg Sci 58:215–221
Abele TA, Lee SL, Twickler DM (2013) MR imaging quantitative analysis of fetal Chiari II malformations and associated open neural tube defects: balanced SSFP versus half-Fourier RARE and interobserver reliability. J Magn Reson Imaging 38:786–793
Adzick NS (2013) Fetal surgery for spina bifida: past, present, future. Semin Pediatr Surg 22:10–17
Adzick NS, Thom EA, Spong CY, Brock JW 3rd, Burrows PK, Johnson MP, Howell LJ, Farrell JA, Dabrowiak ME, Sutton LN, Gupta N, Tulipan NB, D’Alton ME, Farmer DL, Investigators MOMS (2011) A randomized trial of prenatal versus postnatal repair of myelomeningocele. N Engl J Med 364:993–1004
Agrawal A, Mittal A, Kohali GB, Sampley S, Gupta A (2011) Chiari III malformation. Pediatr Neurosurg 47:309–310
Aguilera S, Soothill P, Denbow M, Pople I (2009) Prognosis of spina bifida in the era of prenatal diagnosis and termination of pregnancy. Fetal Diagn Ther 26:68–74
Akbari SH, Limbrick DD Jr, Kim DH, Narayan P, Leonard JR, Smyth MD, Park TS (2013) Surgical management of symptomatic Chiari II malformation in infants and children. Childs Nerv Syst 29:1143–1154
Alkan O, Kizilkilic O, Yildirim T (2009) Malformations of the midbrain and hindbrain: a retrospective study and review of the literature. Cerebellum 8:355–365
Alsaadi MM, Iqbal SM, Elgamal EA, Gozal D (2012) Sleep-disordered breathing in children with Chiari malformation type II and myelomeningocele. Pediatr Int 54:623–626
Aribal ME, Gurcan F, Aslan B (1996) Chiari III malformation: MRI. Neuroradiology 38:S184–S186
Arnold J (1894) Myelocyste, Transposition von Gewebskeimen und Sympodie. Beitr Path Anat 16:1–28
Atlas SW (2009) Magnetic resonance imaging of the brain and spine, vol. 2. Lippincott Williams & Wilkins, Philadelphia, p 233
Awad A-W, Aleck KA, Bhardwaj RD (2014) Concomitant achondroplasia and Chiari malformation: a double-hit at the cervicomedullary junction. World J Clin Cases 2:711–716
Bakim B, Goksan YB, Yilmaz A, Karamustafalioglu O, Akbiyik M, Yayla S, Yuce I, Alpak G, Tankaya O (2013) The quality of life and psychiatric morbidity in patients operated for Arnold- Chiari malformation type I. Int J Psychiatry Clin Pract 17:259–263
Barf HA, Verhoef M, Jennekens-Schinkel A, Post MW, Gooskens RH, Prevo AJ (2003) Cognitive status of young adults with spina bifida. Dev Med Child Neurol 45:813–820
Barry A, Bm P, Stewart BH (1957) Possible factors in the development of the Arnold Chiari malformation. J Neurosurg 14:285–301
Bianchi F, Frassanito P, Tamburrini G, Caldarelli M, Massimi L (2016) Shunt malfunction mimicking a cystic tumour. Br J Neurosurg 6:1–3
Boltshauser E, Schneider J, Kollias S, Waibel P, Weissert M (2002) Vanishing cerebellum in myelomeningocele. Eur J Paediatr Neurol 6:109–113
Bouchard S, Davey MG, Rintoul NE (2003) Correction of hindbrain herniation and anatomy of the vermis after in utero repair of myelomeningocele in sheep. J Pediatr Surg 38:451–458
Bowman RM, McLone DG, Grant JA, Tomita T, Ito JA (2001) Spina bifida outcome: a 25-year prospective. Pediatr Neurosurg 34:114–120
Brownlee R, Myles T, Hamilton MG (1997) The Chiari III and IV malformations. In: Anson JA, Benzel EC, Awad IA (eds) Syringomyelia and the Chiari malformations. AANS, Park Ridge, pp 88–89
Bruner JP, Tulipan N, Paschall R, Boehm FH, Walsh WF, Silva SR, Hernanz-Schulman M, Lowe LH, Reed GW (1999) Fetal surgery for myelomeningocele and the incidence of shunt-dependent hydrocephalus. JAMA 282:1819–1825
Bruner JP, Tulipan N, Drabowiak ME, Walsh DS, Rorke LB, Adzick NS (2004) Upper level of the spina bifida defect: how good are we? Ultrasound Obstet Gynecol 24:612–617
Bulut MD, Yavuz A, Bora A, Gulsen I, Ozkacmaz S, Sosuncu E (2013) Chiari III malformation with a giant encephalocele sac: case report and a review of the literature. Pediatr Neurosurg 49:316–319
Cakirer S (2003) Chiari III malformation varieties of MRI appearances in two patients. J Clin Imag 27:1–4
Caldarelli M, Di Rocco C (2010) Chiari malformations. In: Lumenta CB, Di Rocco C, Haase J, Mooij JJA (eds) Neurosurgery. Springer, Berlin/Heidelberg, pp 311–314
Caldarelli M, Di Rocco C, Colosimo C Jr, Fariello G, Di Gennaro M (1995) Surgical treatment of late neurological deterioration in children with myelodysplasia. Acta Neurochir 137:199–206
Caldarelli M, Di Rocco C, La Marca F (1998) Treatment of hydromyelia in spina bifida. Surg Neurol 50:411–420
Caldarelli M, Rea G, Cincu R, Di Rocco C (2002) Chiari type III malformation. Childs Nerv Syst 18:207–210
Caldarelli M, Boscarelli A, Massimi L (2013) Recurrent tethered cord: radiological investigation and management. Childs Nerv Syst 29:1601–1609
Callen AL, Filly RA (2008) Supratentorial abnormalities in the Chiari II malformation. I – the ventricular point. J Ultrasound Med 27:33–38
Callen AL, Stengel JW, Filly RA (2009) Supratentorial abnormalities in the Chiari II malformation. II – Tectal morphological changes. J Ultrasound Med 28:29–35
Cama A, Tortori-Donati P, Piatelli GL, Fondelli MP, Andreussi L (1995) Chiari complex in children. Neuroradiological diagnosis, neurosurgical treatment and proposal of a new classification (312 cases). Eur J Pediatr Surg 5(Suppl 1):35–38
Cameron AH (1957) The Arnold-Chiari and other neuroanatomical malformations associated with spina bifida. J Pathol 73:195–211
Campbell J, Gilbert WM, Nicolaides KH, Campbell S (1987) Ultrasound screening for spina bifida: cranial and cerebellar signs in a high-risk population. Obstet Gynecol 70:247–250
Castillo M, Quencer RM, Dominguez R (1992) Chiari III malformation: imaging features. Am J Neuroradiol 13:107–113
Center for Disease Control and Prevention-(1992) (1995) Economic costs of birth defects and cerebral palsy – United States. MMWR 44:694–699
Cesmebasi A, Loukas M, Hogan E, Kralovic S, Tubbs RS, Cohen-Gadol AA (2015) The Chiari malformations: a review with emphasis on anatomical traits. Clin Anat 28:184–194
Chakraborty A, Crimmins D, Hayward R, Thompson D (2008) Toward reducing shunt placement rates in patients with myelomeningocele. J Neurosurg Pediatr 1:361–365
Chambers CD, Johnson KA, Dick LM, Felix RJ, Jones KL (1998) Maternal fever and birth outcome: a prospective study. Teratology 58:251–257
Chaudhari IM, Karas CS, Baig MN, Elton SW (2008) Unique defect representing features of Chiari type III and IV malformations. Pediatr Neurosurg 44:513–514
Chiari H (1891) Uber Veränderungen des Kleinhirns infolge von Hydrocephalie des Grosshirns. Dtsch Med Wschr 17:1172–1175
Chiari H (1896) Uber die Veränderungen des Kleinhirns, der Pons und der Medulla oblongata in Folge von congenitaler Hydrocephalie des Grosshirns. Denkschr Akad Wissensch Math Nature 63:71–116
Chikkannaiah P, Srinivasamurthy V, Satish Prasad BS, Lalyanayak P, Shivaram DN (2014) Iniencephaly: radiological and pathological features of a series of three cases. J Neurosci Rural Pract 5:389–393
Cleland J (1883) Contribution to the study of spina bifida, encephalocele, and anencephalus. J Anat Physiol 17:257–292
Coniglio SJ, Anderson SM, Ferguson JE (1997) Developmental outcomes of children with myelomeningocele: prenatal predictors. Am J Obstet Gynecol 177:319–324
De Chalain T, Hudgins R, Burstein F, Armfield K (1994) Combination of unilateral polydactyly, syndactyly, and clinodactyly with occipitocervical encephalocele and vertebral fusion. Ann Plast Surg 44:86–89
De Reuck J, Thienpont L (1976) Fetal Chiari’s type III malformation. Childs Brain 2:85–91
Del Casale A, Serata D, Rapinesi C, Simonetti A, Tamorri SM, Comparelli A, De Carolis A, Savoja V, Kotzalidis GD, Sani G, Tatarelli R, Girardi P (2012) Psychosis risk syndrome comorbid with panic attack disorder in a cannabis abusing patient affected by Arnold-Chiari malformation type I. Gen Hosp Psychiatry 34:702–707
Dhandapani S, Srinivasan A (2016) Contiguous triple spinal dysraphism associated with Chiari malformation type II and hydrocephalus: an embryological conundrum between the unified theory of pang and the unified theory of McLone. J Neurosurg Pediatr 17:103–106
Di Rocco C, Rende M (1989) Neural tube defects: considerations on the pathogenesis and correlation with myelodysplasia in man. II. An experimental model. Fetal Ther 4:99–103
Dias MS (1999) Myelomeningocele. In: Choux M, Di Rocco C, Hockley A, Walker M (eds) Pediatric neurosurgery. Churchill Livingstone, London, pp 33–59
Dias MS (2005) Neurosurgical causes of scoliosis in patients with myelomeningocele: an evidence-based literature review. J Neurosurg 103(1 Suppl):24–35
Dionigi B, Ahmed A, Brazzo J 3rd, Connors JP, Zurakowski D, Fauza DO (2015a) Partial or complete coverage of experimental spina bifida by simple intra-amniotic injection of concentrated amniotic mesenchymal stem cells. J Pediatr Surg 50:69–73
Dionigi B, Brazzo JA III, Ahmed A, Feng C, Wu Y, Zurakowski D, Fauza DO (2015b) Trans-amniotic stem cells therapy (TRSCET) minimizes Chiari II malformation in experimental spina bifida. J Pediatr Surg 50:1037–1041
Drake JM (2008) The surgical management of pediatric hydrocephalus. Neurosurgery 62(Suppl 2):633–640
Elster AD, Chen MY (1992) Chiari I malformations: clinical and radiological reappraisal. Radiology 183:347–353
Emery JL, MacKenzie N (1973) Medullo-cervical dislocation deformity (Chiari II deformity) related to neurospinal dysraphism (myelomeningocele). Brain 96:155–162
Erdincler P, Kaynar MY, Canbaz B, Kocer N, Kuday C, Çiplak N (1998) Iniencephaly: neuroradiological and surgical features. J Neurosurg 89:317–320
Erol FS, Ucler N, Yakar H (2011) The association of Chiari type III malformation and Klippel-Feil syndrome with mirror movement: a case report. Turk Neurosurg 21:655–658
Filho PSAH, Pratesi R (2009) A possible cause of attention deficit in children and adolescents with Chiari malformation type II. Arq Neuropsiquiatr 67:29–34
Filly MR, Filly RA, Barkovich AJ, Goldstein RB (2010) Supratentorial abnormalities in the Chiari II malformation. IV – the too-far-back ventricle. J Ultrasound Med 29:243–248
Fujii M, Tomita T, McLone DG, Grant JA, Stack CV, Mori K (1997) Developmental normo-maturation of brainstem auditory evoked potentials in children with asymptomatic meningo-myelocele during the first year of life. Childs Nerv Syst 13:147–153
Furtado SV, Anantharam BA, Reddy K, Hegde A (2009) Repair of Chiari III malformation using cranioplasty and occipital rotation flap: technical note and review of literature. Surg Neurol 72:414–417
Ganesh D, Sagayaraj BM, Barua RK, Sharma N, Ranga U (2014) Arnold Chiari malformation with spina bifida: a lost opportunity of folic acid supplementation. J Clin Diagn Res 8:OD01–OD03
Gardner WJ (1965) Hydrodynamic mechanism of syringomyelia: its relationship to myelocele. J Neurol Neurosurg Psychiatry 28:247–259
Garg K, Malik N, Jaiswal AK, Behari S (2008) Chiari III malformation with hypertelorism and microcephaly in a neonate: case report and review of literature. J Pediatr Neurosci 3:169–171
Garg K, Tandon V, Mahapatra AK (2011) Chiari III malformation with proatlas abnormality. Pediatr Neurosurg 47:295–298
Garne E, Loane M, Dolk H, De Vigan C, Scarano G, Tucker D, Stoll C, Gener B, Pierini A, Nelen V, Rösch C, Gillerot Y, Feijoo M, Tincheva R, Queisser-Luft A, Addor MC, Mosquera C, Gatt M, Barisic I (2005) Prenatal diagnosis of severe structural congenital malformations in Europe. Ultrasound Obstet Gynecol 25:6–11
Geerdink N, van der Vliet T, Rotteveel JJ, Feuth T, Roeleveld N, Mullaart RA (2012) Essential features of Chiari II malformation in MR imaging: an interobserver reliability study – part 1. Childs Nerv Syst 28:977–985
Geiger F, Parsch D, Carstens C (1999) Complications of scoliosis surgery in children with myelomeningocele. Eur Spine J 8:22–26
Ghi T, Pilu GL, Falco P, Segata M, Carletti A, Cocchi G, Santini D, Bonasoni P, Tani G, Rizzo N (2006) Prenatal diagnosis of open and closed spina bifida. Ultrasound Obstet Gynecol 28:899–903
Gilbert JN, Jones KL, Rorke LB, Chernoff GF, James HE (1986) Central nervous system anomalies associated with meningomyelocele, hydrocephalus, and the Arnold-Chiari malformations: reappraisal of thesis regarding the pathogenesis of posterior neural tube closure defects. Neurosurgery 18:559–563
Guille JT, Starwark JF, Sherk HH, Kumar SJ (2006) Congenital and developmental deformities of the spine in children with myelomeningocele. J Am Acad Orthop Surg 14:294–302
Hall P, Lindseth R, Campbell R, Kalsbeck JE, Desousa A (1979) Scoliosis and hydrocephalus in myelocele patients. The effects of ventricular shunting. J Neurosurg 50:174–178
Hashiguchi K, Morioka T, Murakami N, Togao O, Hiwatashi A, Ochiai M, Eriguchi G, Kishimoto J, Iihara K (2016) Sequential morphological change of Chiari malformation type II following surgical repair of myelomeningocele. Childs Nerv Syst 32:1069–1078
Hoederath L, Jellestad L, Jenewein J, Boettger S (2014) Psychotic and major neurocognitive disorder secondary to Arnold-Chiari type II malformation. Psychiatr Danub 26:291–293
Hoffman HJ, Hendrick EB, Humphreys RP (1975) Manifestations and management of the Arnold-Chiari malformation in patients with myelomeningocele. Childs Brain 1:255–259
Hoffman HJ, Hendrick EB, Humphreys RP (1983) Manifestazioni e trattamento della malformazione di Arnold- Chiari nel bambino con mielomeningocele. In: Di Rocco C, Caldarelli M (eds) Mielomeningocele. Casa del Libro, Rome, pp 251–260
Hol FA, Geurds MP, Chatkupt S et al (1996) PAX genes and human neural tube defects: an amino acid substitution in PAX 1 in a patient with spina bifida. J Med Gen 33:655–660
Isik N, Elmaci I, Silva G, Celik M, Kalelioglu M (2009) Chiari malformation type III and results of surgery: a clinical study. Pediatr Neurosurg 45:19–28
Iskandar BJ, Oakes WJ (1999) Chiari malformations. In: Albright L, Pollack I, Adelson D (eds) Principles and practice of pediatric neurosurgery. Thieme, New York, pp 165–187
Iskandar BJ, Hedlund GL, Grabb PA, Oakes WJ (1998) The resolution of syringohydromyelia without hindbrain herniation after posterior fossa decompression. J Neurosurg 89:212–216
Ivashchuk G, Loukas M, Blount JP, Tubbs RS, Oakes WJ (2015) Chiari III malformation: a comprehensive review of this enigmatic anomaly. Childs Nerv Syst 31:2035–2040
Jaggi RS, Premsagar IC (2007) Chiari malformation type III treated with primary closure. Pediatr Neurosurg 43:424–427
Januschek E, Röhrig A, Kunze S, Fremerey C, Wiebe B, Messing-Jünger M (2016) Myelomeningocele – a single institute analysis of the years 2007 to 2015. Childs Nerv Syst 32(7):1281–1287. https://doi.org/10.1007/s00381-016-3079-1. Epub 2016 Apr 16
Jenkinson MD, Campbell S, Hayhurst C, Clark S, Kandasamy J, Lee MK, Flynn A, Murphy P, Mallucci CL (2011) Cognitive and functional outcome in spina bifida-Chiari II malformation. Childs Nerv Syst 27:967–974
Jiang J, Zhang Y, Wei L, Sun Z, Liu Z (2014) Association between MTHDI G1958A polymorphism and neural tube defects susceptibility: a meta-analysis. PLoS One 9:e1011169
Josan V, Morokoff MWJ (2008) Epidemiology and aetiological factors. In: Ozek MM, Cinalli G, Maixner WJ (eds) Spina bifida. Springer, Milan, pp 59–65
Juranek J, Dennis M, Cirino PT, El-Messidi L, Fletcher JM (2010) The cerebellum in children with spina bifida and Chiari II malformation: quantitative volumetrics by region. Cerebellum 9:240–248
Kiymaz N, Yilmaz N, Demir I, Keskin S (2010) Prognostic factors in patients with occipital encephalocele. Pediatr Neurosurg 46:6–11
Kulkarni PR, Rao RV, Alur MB, Joshi SK (2011) Iniencephaly clausus: a case report with review of literature. J Pediatr Neurosci 6:121–123
La Marca F, Herman R, Grant JA, McLone DG (1997) Presentation and management of hydromyelia in children with Chiari type II malformation. Pediatr Neurosurg 26:57–67
Lee R, Tay KS, Cheng PW, Lui WM, Chan FL (2002) Chiari III malformation: antenatal MRI diagnosis. Clin Radiol 57:759–767
Luigetti M, Losurdo A, Dittoni S, Testani E, Colicchio S, Gnoni V, Farina B, Scarano E, Zampino G, Mariotti P, Rendeli C, Di Rocco C, Massimi L, Della Marca G (2010) Improvement of obstructive sleep apneas caused by hydrocephalus associated with Chiari malformation type II following surgery. J Neurosurg Pediatrics 6:336–339
Mangels KJ, Tulipan N, Tsao LY (2000) Fetal MRI in the evaluation of intrauterine myelomeningocele. Pediatr Neurosurg 32:124–131
Marin-Padilla M, Marin-Padilla TM (1981) Morphogenesis of experimentally induced Arnold-Chiari malformation. J Neurol Sci 50:29–55
Massimi L, Novegno F, Di Rocco C (2011a) Chiari type I malformation in children. Advances and Technical Standards in Neurosurgery, Springer, Wien New York 37:143–211
Massimi L, Pravatà E, Tamburrini G, Gaudino S, Pettorini B, Novegno F, Colosimo C Jr, Di Rocco C (2011b) Management of Chiari I and related hydrocephalus: outcome and pathogenetic implications. Neurosurgery 68:950–956
Mc Lone DG (2011) Comment on Salman M: posterior fossa decompression and the cerebellum in Chiari type II malformation: a preliminary MRI study. Childs Nerv Syst 27:465
McLone DG (1992) Continuing concepts in the management of spina bifida. Pediatr Neurosurg 18:254–256
McLone DG (1998) Care of the neonate with myelomeningocele. Neurosurg Clin N Am 9:111–120
McLone DG, Dias MS (2003) The Chiari II malformation: cause and impact. Childs Nerv Syst 19:540–550
McLone DG, Knepper PA (1989) The cause of Chiari II malformation: a unified theory. Pediatr Neurosci 15:1–12
McLone DG, Naidich TP (1992) Developmental morphology of the subarachnoid space, brain vasculature and contiguous structures, and the cause of the Chiari II malformation. Am J Neuroradiol 13:463–482
Mehta VA, Bettegowda C, Amin A, El-Gassim M, Jallo G, Ahn ES (2011) Impact of tethered cord release on symptoms of Chiari II malformation in children born with a myelomeningocele. Childs Nerv Syst 27:975–978
Meijer WM, de Walle HE (2005) Differences in folic acid policy and the prevalence of neural-tube defects in Europe; recommendations for food fortification in a EUROCAT report. Ned Tijdschr Genneeskd 149:2561–2564 (article in Dutch)
Melvin EC, George TM, Worley G, Franklin A, Mackey J, Viles K, Shah N, Drake CR, Enterline DS, McLone D, Nye J, Oakes WJ, McLaughlin C, Walker ML, Peterson P, Brei T, Buran C, Aben J, Ohm B, Bermans I, Qumsiyeh M, Vance J, Pericak-Vance MA, Speer MC (2000) Genetic studies in neural tube defects. NTD collaborative group. Pediatr Neurosurg 32:1–9
Messing-Jünger M, Röhrig A (2013) Primary and secondary management of the Chiari II malformation in children with myelomeningocele. Childs Nerv Syst 29:1553–1562
Meuli M, Moehrlen U (2014) Fetal surgery for myelomeningocele is effective: a critical look at the whys. Pediatr Surg Int 30:689–697
Mignone Philpott C, Shannon P, Chitayat D, Ryan G, Raybaud CA, Blaser CI (2013) Diffusion-weighted imaging of the cerebellum in the fetus with Chiari II malformation. Am J Neuroradiol 34:1656–1660
Mikulis DJ, Diaz O, Egglin TK, Sanchez R (1992) Variance of the position of the cerebellar tonsils with age: preliminary report. Radiology 183:725–728
Milhorat TH, Miller JI, Johnson WD, Adler DE, Heger IM (1993) Anatomical basis of syringomyelia occurring with hindbrain lesions. Neurosurgery 32:748–754
Mirzai H, Ersahin Y, Mutluer S, Kayahan A (1998) Outcome of patients with myelomeningocele: the Ege University experience. Childs Nerv Syst 14:120–123
MRC Vitamin Study Research Group (1991) Prevention of neural tube defects: results of the Medical Research Council vitamin study. Lancet 338:131–137
Muzumdar D, Gandhi S, Fattepurkar S, Goel A (2007) Type III Chiari malformation presenting as intermittent respiratory stridor: a neurological image. Pediatr Neurosurg 43:446–448
Naidich TP, Pudlowski RM, Naidich JB, Gornish M, Rodriguez FJ (1980) Computed tomography signs of the Chiari II malformation. Part I: skull and dural positions. Radiology 134:65–71
Nishimura T, Mori K (1996) Blink reflex in meningomyelocele, with special reference to its usefulness in the evaluation of brainstem dysfunction. Childs Nerv Syst 12:2–12
Nishimura T, Mori K, Uchida Y, Ohira T, Tamura K (1991) Brain stem auditory-evoked potentials in meningomyelocele. Natural history of Chiari II malformations. Childs Nerv Syst 7:316–326
Oakeshott P, Hunt GM (2003) Long-term outcome in open spina bifida. Br J Gen Pract 53:632–636
O’Brien DF, Javadpour M, Collins DR, Spennato P, Mallucci CL (2005) Endoscopic third ventriculostomy: an outcome analysis of primary cases and procedures performed after ventriculoperitoneal shunt malfunction. J Neurosurg 103(5 Suppl):393–400
Ogiwara H, Morota N (2013) Surgical decompression without dural opening for symptomatic Chiari type II malformation in young infants. Childs Nerv Syst 29:1563–1567
Oldfield EH, Muraszko K, Shawker TH, Patronas NJ (1994) Pathophysiology of syringomyelia associated with Chiari I malformation of the cerebellar tonsils. Implications for diagnosis and treatment. J Neurosurg 80:3–15
Osaka K, Tanimura T, Hirayama A, Matsumoto S (1978) Myelomeningocele before birth. J Neurosurg 49:711–724
Otera Y, Morokuma S, Fukushima K, Anami A, Yumoto Y, Ito Y, Ochiai M, Hashiguchi K, Wake N, Sago H, Kato K (2014) Neurological outcomes in Chiari type II malformations and their correlation to morphological findings and fetal heart rate patterns: a retrospective study. BMC Res Notes 8:57
Paek BW, Farmer DL, Wilkinson CC, Albanese CT, Peacock W, Harrison MR, Jennings RW (2000) Hindbrain herniation develops in surgically created myelomeningocele but is absent after repair in fetal lambs. Am J Obstet Gynecol 183:1119–1123
Papp C, Adam Z, Toth-Pal E, Török O, Váradi V, Papp Z (1997) Risk of recurrence of craniospinal anomalies. J Matern Fetal Med 6:53–57
Patel DM, Rocque BG, Hopson B, Arynchyna A, Bishop ER, Lozano D, Blount JP (2015) Sleep-disordered breathing in patients with myelomeningocele. J Neurosurg Pediatr 16:30–35
Penfield W, Coburn DF (1938) Arnold-Chiari malformation and its operative treatment. Arch Neurol Psychiatr 40:328–336
Penso C, Redline RW, Benacerraf BR (1987) A sonographic sign which predicts which fetuses with hydrocephalus have an associated neural tube defect. J Ultrasound Med 6:307–311
Perez da Rosa S, Millward CP, Chiappa V, Martinez de Leon M, Ibáñez Botella G, Ros López B (2015) Endoscopic third Ventriculostomy in children with myelomeningocele: a case series. Pediatr Neurosurg 50:113–118
Piatt JH Jr (2004) Syringomyelia complicating myelomeningocele: review of the evidence. J Neurosurg 100(2 Suppl Pediatrics):101–109
Pitkin RM (2007) Folate and neural tube defects. Am J Clin Nutr 85:285S–288S
Pollack IF, Pang AD, Albright AL, Krieger D (1992) Outcome following hindbrain decompression of symptomatic Chiari malformations in children previously treated with myelomeningocele closure and shunts. J Neurosurg 77:881–888
Pollack IF, Kinnunen D, Albright LA (1996) The effect of early craniocervical decompression on functional outcome in neonates and young infants with myelodysplasia and symptomatic Chiari II malformations: results from a prospective series. Neurosurgery 38:703–710
Raimondi AJ (1972) Pediatric neurosurgery. Saunders, Philadelphia, pp 235–237, 339–343
Ramdurg SR, Solpure S, Dubey S, Gubbi S (2013) Asymptomatic Chiari III malformation with tectal beaking and holocord syrinx. J Pediatr Neurosci 8:254–256
Rani H, Kulkarni AV, Rao RV, Patil P (2013) Chiari III malformation: a rare case with review of literature. Fetal Pediatr Pathol 32:169–174
Ray JG, Meier C, Vermeulen MJ, Boss S, Wyatt PR, Cole DE (2002) Association of neural tube defects and folic acid fortification in Canada. Lancet 360:2047–2048
Raybaud C, Miller E (2008) Radiological evaluation of myelomeningocele-Chiari II malformation. In: Ozek MM, Cinalli G, Maixner WJ (eds) Spina bifida. Springer Verlag, Milan, pp 111–142
Righini A, Parazzini C, Doneda C, Arrigoni F, Rustico M, Re TJ, Triulzi F (2011) Fetal MRI features related to the Chiari malformations. Neurol Sci 32(Suppl 3):S279–S281
Roldan O, Wieben O, Haughton V, Osswald T, Chesler N (2009) Characterization of CSF hydrodynamics in the presence and absence of tonsillar ectopia by means of computational flow analysis. AJNR 30:941–946
Salman MS (2011) Posterior fossa decompression and the cerebellum in Chiari type II malformation: a preliminary MRI study. Childs Nerv Syst 27:457–462
Salman MS, Blaser SE, Sharpe JA, Dennis M (2006) Cerebellar vermis morphology in children with spina bifida and Chiari type II malformation. Childs Nerv Syst 22:385–393
Sav A (2008) Pathological anatomy of spina bifida. In: Ozek MM, Cinalli G, Maixner WJ (eds) Spina bifida. Springer, Milan, pp 43–57
Schwahn B, Rozen R (2001) Polymorphisms in the methylenetetrahydrofolate reductase gene: clinical consequences. Am J Pharmacogenomics 1:189–201
Schwalbe E, Gredig M (1907) Ueber Entwicklungstströrungen des Kleihirns, Hirnstamms und Halsmarks bei Spina bifida (Arnold’sche und Chiari’sche Missbildung). Beitr Path Anat 40:132–194
Sebire NJ, Noble PI, Thorpe-Beeston JG, Snijders RJ, Nicolaides KH (1997) Presence of the lemon sign in fetuses with spina bifida at the 12-14 week scan. Ultrasound Obstet Gynecol 10:403–407
Sener RN, Dzelzite S (2003) Rhombencephalosynapsis and a Chiari II malformation. J Comput Assist Tomogr 27:257–259
Sgouros S (2008) Chiari II malformation and syringomyelia. In: Ozek MM, Cinalli G, Maixner WJ (eds) Spina bifida. Springer, Milan, pp 237–248
Sgouros S, Kountouri M, Natarajan K (2006) Posterior fossa volume in children with Chiari malformation type I. J Neurosurg 105:101–106
Shankar P, Zamora C, Castillo M (2016) Congenital malformations of the brain and spine. Handb Clin Neurol 136:1121–1137
Shaw GM, Velie EM, Shaffer D (1996) Risk of neural tube defect-affected pregnancies among obese women. JAMA 275:1093–1096
Sim KB, Hong SK, Cho BK, Choi DY, Wang KC (1996) Experimentally induced Chiari-like malformation with myeloschisis in chick embryos. J Korean Med Sci 11:509–516
Sim K-B, Lee JY, Phi JH, Kim S-K, Wang KC (2013) Experimental models of spinal open neural tube defect and Chiari type II malformation. Childs Nerv Syst 29:1435–1449
Simon EM (2004) MRI of the fetal spine. Pediatr Radiol 34:712–719
Sirikci A, Bayazit YA, Bayram M (2001) The Chiari III malformation: an unusual and asymptomatic variant in an 11-year old child. Eur J Radiol 29:147–150
Smith AB, Gupta N, Otto C, Glenn OA (2007) Diagnosis of Chiari III malformation by second trimester fetal MRI with postnatal MRI and CT correlation. Pediatr Radiol 37:1035–1038
Snyder WE Jr, Luerssen TG, Boaz JC, Kalsbeck JE (1998) Chiari III malformation treated with CSF diversion and delayed surgical closure. Pediatr Neurosurg 29:117–120
Soare PL, Ramondi AJ (1977) Intellectual and perceptual-motor characteristics of treated myelomeningocele children. Am J Dis Child 131:199–204
Spennato P, Ruggiero C, Aliberti F, Nastro A, Mirone G, Cinalli G (2013) Third ventriculostomy in shunt malfunction. World Neurosurg 79(2 Suppl):e21–e26
Stritzke AI, Dunham CP, Smyth JA, Steinbok P (2011) Congenital stridor in the context of Chiari malformation type II: the etiological role of vernix caseosa granulomatous meningitis. J Neurosurg Pediatrics 8:372–376
Sutton L, Adzik NS, Johnson MP (2003) Fetal surgery of myelomeningocele. Childs Nerv Syst 19:587–591
Talamonti G, Zella S (2011) Surgical treatment of CM2 and syringomyelia in a series of 231 myelomeningocele patients. Neurol Sci 32(Suppl 3):S331–S333
Taylor DG, Mastorakos P, Jane JA Jr, Oldfield EH (2017) Two distinct populations of Chiari I malformation based on presence or absence of posterior fossa crowdedness on magnetic resonance imaging. J Neurosurg 126:1934–1940
Tekin D, Uysal S, Iyigun O (2002) Primary cerebellar agenesis – Chiari IV malformation. MOU Tip Dergisi 19:213–216
Testoni S, Pria AD, Gentile A (2010) Imaging diagnosis-cerebellar displacement and spina bifida in a calf. Vet Radiol Ultrasound 51:162–164
The EUROCAT Working Group (1987) Prevalence of neural tube defects in 16 regions of Europe, 1980–1983. Int J Epidemiol 16:246–251
The EUROCAT Working Group (1991) Prevalence of neural tube defects in 20 regions of Europe and the impact of prenatal diagnosis, 1980-1986. J Epidemiol Comm heatlh 45:52–58
Titomanlio L, Romano A, Del Giudice E (2005) Cerebellar agenesis. Neurology 64:E21
Tortori-Donati P, Rossi A, Cama A (2000) Spinal dysraphism: a review of neuroradiological features with embryological correlations and proposal for a new classification. Neuroradiology 42:471–491
Trigylidas T, Baronia B, Vassyliadi M, Ventureyra ECG (2008) Posterior fossa dimension and volume estimates in pediatric patients with Chiari I malformations. Childs Nerv Syst 24:329–336
Tubbs RS, Oakes WJ (2004) Treatment and management of the Chiari II malformation: an evidence-based review of the literature. Childs Nerv Syst 20:375–381
Tubbs RS, Oakes WJ (2012) The Chiari V malformation. Childs Nerv Syst 28:339
Tubbs RS, Muhleman M, Loukas M, Oakes WJ (2012) A new form of herniation: the Chiari V malformation. Childs Nerv Syst 28:305–307
Tubbs RS, Demerdash A, Vahedi P, Griessenauer CJ, Oakes WJ (2016) Chiari IV malformation: correcting an over one century long historical error. Childs Nerv Syst 32:1175–1179
Tude Melo JR, Pacheco P, Nunes de Melo E, Vasconcellos A, Klein Passos R (2015) Clinical and ultrasonographic criteria for using ventriculoperitoneal shunts in newborns with myelomeningocele. Arq Neuropsiquiatr 73:759–763
Tulipan N, Hernanz-Schulman M, Lowe LH, Bruner JP (1999) Intrauterine myelomeningocele repair reverses pre-existing hindbrain herniation. Pediatr Neurosurg 31:137–142
Tulipan N, Wellons JC 3rd, Thom EA, Gupta N, Sutton LN, Burrows PK, Farmer D, Walsh W, Johnson MP, Rand L, Tolivaisa S, D’alton ME, Adzick NS, MOMS Investigators (2015) Prenatal surgery for myelomeningocele and the need for cerebrospinal fluid shunt placement. J Neurosurg Pediatr 16:613–620
Udayakumaran S (2012) Chiari V or Chiari II plus? Childs Nerv Syst 28:337–338
Udayakumaran S, Ben Sira L, Constantini S (2010) Temporal lobe herniation of developmental origin: a novel radiological association with open spina bifida and Chiari II malformation. Childs Nerv Syst 26:277–278
Van den Hof MC, Nicolaides KH, Campbell J, Campbell S (1990) Evaluation of the lemon and banana signs in one hundred and thirty foetuses with open spina bifida. Am J Obstet Gynecol 162:322–327
Van der Linden IJ, Afman LA, Heil SG, Blom HJ (2006) Genetic variations in gene of folate metabolism and neural tube defect risk. Proc Nutr Soc 65:204–215
Van Der Vossen S, Pistorius LR, Mulder EJ, Platenkamp M, Stoutenbeek P, Visser GH, Gooskens RH (2009) Role of prenatal ultrasound in predicting survival and mental and motor functioning in children with spina bifida. Ultrasound Obstet Gynecol 34:253–258
Van Roost D, Solymosi L, Funke K (1995) A characteristic ventricular shape in myelomeningocele-associated hydrocephalus? A CT stereology study. Neuroradiology 37:412–417
Vandertop WP, Asai A, Hoffman HJ, Drake JM, Humphreys RP, Rutka JT, Becker LE (1992) Surgical decompression for symptomatic Chiari II malformation in neonates with myelomeningocele. J Neurosurg 77:541–544
Velie E, Shaw GM (1996) Impact of prenatal diagnosis and elective termination on prevalence and risks estimates of neural tube defects in California. 1989-1991. Am J Epidemiol 144:473–479
Verma R, Pratiaraj HN (2012) Unusual association of Arnold Chiari malformation and vitamin B12 deficiency. BMJ Case Rep Jul 9:2012
Vernet O, Farmer JP, Montes JL (1996) Comparison of syringopleural and syringosubarachnoid shunting in the treatment of syringomyelia in children. J Neurosurg 84:624–628
Vinchon M (2011) Comment on Salman M: posterior fossa decompression and the cerebellum in Chiari type II malformation: a preliminary MRI study. Childs Nerv Syst 27:463–464
Vinck A, Maassen B, Mullaart R, Rotteveel J (2006) Arnold-Chiari-II malformation and cognitive functioning in spina bifida. J Neurol Neurosurg Psychiatry 77:1083–1086
von Koch CS, Compagnone N, Hirose S, Yoder S, Harrison MR, Farmer DL (2005a) Myelomeningocele: characterization of a surgically induced sheep model and its central nervous system similarities and differences to the human disease. Am J Obstet Gynecol 193:1456–1462
Von Koch CS, Glenn OA, Goldstein RB, Barkovic AJ (2005b) Fetal magnetic resonance imaging enhances detection of spinal cord anomalies in patients with sonographically detected bony anomalies of the spine. J Ultrasound Med 24:781–789
Waters KA, Forbes P, Morielli A, Hum C, O’Gorman AM, Vernet O, Davis GM, Tewfik TL, Ducharme FM, Brouillette RT (1998) Sleep-disordered breathing in children with myelomeningocele. J Pediatr 132:672–881
Weber Guimarães Barreto M, Ferro MM, Guimarães Bittencourt D, Violin Pereira LA, Barini R, Sbragia L (2005) Arnold-Chiari in a fetal rat model of dysraphism. Fetal Diagn Ther 20:437–441
Welsch M, Antes S, Kiefer M, Meyer S, Eymann R (2013) Association of Chiari malformation and vitamin B12 deficiency in a family. Childs Nerv Syst 29:1193–1198
Williams B (1975) Cerebrospinal fluid pressure gradients in spina bifida cystica, with special reference to the Arnold-Chiari malformation and aqueductal stenosis. Dev Med Child Neurol 35:138–150
Williams B (1990) Syringomyelia. Neurosurg Clin North Am 1:653–685
Williams H (2008) A unifying hypothesis for hydrocephalus, Chiari malformation, syringomyelia, anencephaly and spina bifida. Cerebrospinal Fluid Res 5:7
Woitek R, Prayer D, Weber M, Amann G, Seidl R, Bettelheim D, Schöpf V, Brugger PC, Furtner J, Asenbaum U, Kasprian G (2016) Fetal diffusion tensor quantification of brainstem pathology in Chiari II malformation. Eur Radiol 26:1274–1283
Wong SK, Barkovich AJ, Callen AL, Filly RA (2009) Supratentorial abnormalities in the Chiari II malformation. III – the interhemispheric cyst. J Ultrasound Med 28:999–1006
Worley G, Erwin CW, Schuster JM, Park Y, Boyko OB, Griebel ML, Weidman ER, Radtke RA, Oakes WJ (1994) BAEPs in infants with myelomeningocele and later development of Chiari II malformation-related brainstem dysfunction. Dev Med Child Neurol 36:707–715
Zolal A, Vachata P, Hefcl A, Malucelli A, Bartos R, Sames M (2010) Identification of the large descending tracts using diffusion tensor imaging in Chiari III malformation. Childs Nerv Syst 26:867–870
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Section Editor information
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this entry
Cite this entry
Massimi, L., Caldarelli, M., Di Rocco, C. (2020). Chiari Malformations Types II, III, IV, and V. In: Di Rocco, C., Pang, D., Rutka, J. (eds) Textbook of Pediatric Neurosurgery. Springer, Cham. https://doi.org/10.1007/978-3-319-72168-2_9
Download citation
DOI: https://doi.org/10.1007/978-3-319-72168-2_9
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-72167-5
Online ISBN: 978-3-319-72168-2
eBook Packages: MedicineReference Module Medicine