Abstract
The use of nanoparticles (NPs) in commercially available products and as biomedicinal materials could lead to increasing contact of human blood vessels with NPs, and it is necessary to assess the potential adverse effects of NPs to cells lining blood vessels. Of them, endothelial cells (ECs) are of particular relevance as they play a crucial role in the regulation of function of blood vessels. In this book chapter, I discussed studies that used human ECs to study the toxicity and mechanisms of NPs. It has been shown that exposure of human ECs to NPs could lead to cytotoxicity, genotoxicity, endothelial activation and impaired NO signaling. Oxidative stress and inflammation induced by NPs have been suggested as the mechanisms associated with the toxicity of NPs to ECs, and a three-tier model has been proposed to explain the association between NP induced oxidative stress and toxicity. In recent years, dysfunction of autophagy (excessive autophagy induction) has also been suggested as one of the mechanisms associated with the toxicity of NPs to human ECs. In the future, it is necessary to use human ECs to assess the toxicity of NPs to better understand the potential adverse effects of NPs entering circulation.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
4.1 Introduction
Nanoparticles (NPs) are defined as ‘natural, incidental or manufactured material containing particles, in an unbound state or as an aggregate or as an agglomerate and where, for 50% or more of the particles in the number size distribution, one or more external dimensions is in the size range 1 nm–100 nm’ by the European Commission in 2011. In specific cases, the threshold between 1% and 50% for the number size distribution may also be used instead of 50% [1]. Nano-sized particles could be generated through combustion, and combustion-derived NPs have been convincingly shown to induce adverse health effects to blood vessels [2, 3]. In recent years, the rapid development of nanotechnologies also leads to increasing use of engineered NPs in many commercial products, marking engineered NPs as one of the major sources for particle exposure in modern society. According to a recent survey, a total of 1814 commercial products sold in global markets contain at least one type of NPs, which can lead to human exposure to NPs in daily life via three major routes, namely dermal (count for 58% of products evaluated), inhalational (25%) and oral (16%) exposure [4]. By the analog with combustion-derived NPs, it has been suggested that engineered NPs added in commercial products may also induce adverse health effects [2, 3].
Besides intended use in commercial products, NPs may also have potential use in medicine. For example, carbon nanotubes (CNTs), including single-walled carbon nanotubes (SWCNTs) and multi-walled carbon nanotubes (MWCNTs), could be used as nanocarriers for drug delivery [5]. Ag NPs are potential anticancer therapeutic agents that could be used in the treatment of a number of cancer, such as leukemia, breast cancer and lung cancer [6]. Metal-based NPs including Ag and ZnO NPs are also effective alternative antimicrobial agents for the treatment of infectious diseases [7]. Iron oxide NPs (IONPs) could be applied as contrast agents in magnetic resonance imaging (MRI) as well as for the treatment of iron deficiency [8]. However, despite the enthusiasm for the development of NPs for medicinal purposes, progress into clinics is relatively slow. One of the concerns is the adverse health effects of NPs, especially to the vasculature, because intravenous injection of NPs in nanomedicine could lead to increasing contact of vasculature to NPs [9]. Thus, it is necessary to evaluate the potential effects of NPs to cells lining blood vessels.
Human blood vessels are covered by a thin layer of endothelial cells (ECs), which act as the first contact and barrier for NPs entering circulation. Moreover, ECs play a crucial role in the regulation of blood vessel tone, thrombogenicity, homeostasis and monocytes recruitment [10]. In normal vascular physiology, the ECs generate NO by endothelial NOS (eNOS), which plays a key role to maintain the quiescent state of the endothelium by inhibition of inflammation, cellular proliferation and thrombosis, and the monocytes adhere poorly onto the endothelium under normal conditions [11]. With the development of cardiovascular diseases, persistent inflammation in blood vessels activates ECs, which in turn express excessive adhesion molecules such as selectins, ICAM-1 and VCAM-1 to recruit monocytes. Monocytes adhere to the activated ECs, migrate through the endothelium to the intima, accumulate lipids and transform to lipid laden foam cells, which result in the earliest visible atherosclerotic lesions as fatty streaks [12]. Meanwhile, the development of cardiovascular diseases was also associated with a gradual loss of NO bioactivity due to the uncoupling of eNOS (eNOS uncoupling; Fig. 4.1). Given the importance of ECs in maintaining the proper function of blood vessels, it is necessary to evaluate the toxicity of NPs to ECs in order to better understand the potential effects of NPs in vivo [9].
Key events associated with the early development of atherosclerosis. In normal endothelial cells (ECs), endothelial NOS (eNOS) generate NO to maintain the quiescent state of the endothelium, and the monocytes adhere poorly onto the endothelium. With the development of cardiovascular diseases, ECs are activated to express excessive adhesion molecules, and monocytes subsequently adhere to the activated ECs, migrate through the endothelium to the intima, accumulate lipids and transform to lipid laden foam cells to form the earliest visible atherosclerotic lesions. Meanwhile, there is also a gradual loss of NO bioactivity due to eNOS uncoupling
In this book chapter, I will discuss about the toxicity of NPs to ECs as well as the possible mechanisms. The discussion will be limited to studies using human ECs, rather than animal ECs, as the results are easier to be extrapolated to human endothelium in vivo. I hope this book chapter will help future studies which consider to evaluate the adverse effects of NPs to endothelium.
4.2 Toxicity of NPs to Human Endothelial Cells
4.2.1 Cytotoxicity
A number of NPs has been shown to induce cytotoxicity to human ECs. Of them, the soluble metal based NPs appear to be the most cytotoxic due to the dissolution of NPs to release metal ions. For example, ZnO NPs are partially soluble to release Zn ions, which has been convincingly shown as one of the mechanisms for ZnO NP induced toxicity to mammalian cells [13]. A pilot study by Sun et al. [14] showed that 24 h exposure to ZnO NPs (primary size 45.3 nm) was associated with significantly decreased mitochondrial activity in human cardiac microvascular endothelial cells (HCMECs), with a threshold as low as 5 μg/mL. Liang et al. [15] showed that 24 h exposure to ZnO NPs (primary size 70 nm) at the concentrations ≥15 μg/mL significantly induced cytotoxicity in human aortic endothelial cells (HAECs) as decreased mitochondrial activity, lactate dehydrogenase (LDH) release and apoptosis. We have also recently shown that 24 h exposure to 32 μg/mL ZnO NPs (primary size 100 nm) induced cytotoxicity in human umbilical vein endothelial cells (HUVECs) as decreased mitochondrial activity, LDH release and lysosomal damages, which was associated with increased intracellular Zn ions [16, 17]. Ag NPs, which may lead to the accumulation of Ag ions, were also cytotoxic to endothelial cells. Guo et al. [18] showed that 24 h incubation of HUVECs with citrated-coated Ag NPs (10, 75, and 110 nm) from 1 to 40 μg/mL significantly induced cytotoxicity associated with increased accumulation of intracellular Ag, with 110 nm Ag NPs being most effective. Meanwhile, AgNO3 at the same concentrations was more cytotoxic compared with Ag NPs, which indicated that AgNO3 induced cells death through a mechanism different from Ag NPs. A comparative study by Danielsen et al. [19] also showed that Ag NPs (<20 nm) induced cytotoxicity in HUVECs, but the threshold of Ag NPs (64 μg/mL) was higher than that of ZnO NPs (32 μg/mL). Another example is Cd based quantum dot (QD), which can release the highly toxic Cd ions. Yan et al. [20] showed that CdTe QD (mercaptosuccinic acid coated; primary size ~4 nm) induced cytotoxicity in HUVECs, with a threshold as low as 0.1 μg/mL. At 10 μg/mL, 24 h incubation of HUVECs with CdTe QD reduced cellular viability to about 50% of control and induced apoptosis about five times higher over control.
Some of the insoluble NPs may also induce cytotoxicity to human ECs. For example, Yang et al. [21] showed that 24 h exposure of HUVECs to 20 μg/mL silica NPs (primary size 56.8 nm) significantly induced cytotoxicity as about 50% decrease of viability and about 6.6 times higher LDH release. Similarly, Guo et al. [22] also showed that 24 h or 48 h exposure of HUVECs to amorphous silica NPs (average diameter 57.66 nm) from 12.5 to 100 μg/mL significantly induced cytotoxicity. Walker et al. [23] compared the effects of single-walled carbon nanotube (SWCNT; surface area 641 m2/g) and multi-walled carbon nanotube (MWCNT; 56 m2/g), and results showed that 24 h exposure to both types of CNT (10, 50, 100 μg/106 cells) induced cytotoxicity in human aortic endothelial cells (HAEC) to a similar extent, which indicated that surface area is not important in influencing the cytotoxicity of CNT to ECs. Orecna et al. [24] showed that exposure to 100 μg/mL pristine and carboxylated MWCNT (average diameter 60 nm) induced similar effects in mitochondrial viability and LDH release in HUVECs, but the carboxylated MWCNT was associated with higher apoptosis. Ge et al. [25] showed that 6 h and 12 h exposure to 30 μg/mL SWCNT (primary size not provided; with ion impurities) caused over 50% decrease in HUVEC viability, which was attenuated by the presence of proteins due to the formation of protein corona.
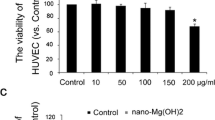
In contrast, organic NPs generally showed little to no cytotoxicity. For example, Matuszak et al. [26] showed that exposure to up to 100 μg/mL lipid NPs (50, 80, 120 nm) or liposomes (109, 139 nm) did not significantly affect HUVEC viability (indicated as cell index by real-time measurement), whereas 100 μg/mL micelles (145, 227 nm) significantly decreased the viability. Menard et al. [27] showed that micelles based on diglutamic acid (linked to lithocholic, arachidonic or linoleic acid) did not significantly induce LDH release in HUVECs, and the EC50 to reduce mitochondrial viability was larger than 250 μg/mL. Our recent study also showed that up to 200 μg/mL micelles based on MPEG-PLA (hydrodynamic size ~20 nm) did not significantly induce cytotoxicity in HUVECs [28]. Indeed, coating with organics could be a strategy to improve the biocompatibility of toxic NPs. For example, Su et al. [29] coated Ag NPs with polyurethane micelles with MPEG brush, and the nanocomposite showed relatively low cytotoxicity to HUVECs (viability approximate 72% after 24 h exposure to 20 μg/mL NPs) while efficiently inhibited the growth of bacteria. All of these studies in combination suggested that NPs could induce cytotoxicity to human ECs in vitro, and the cytotoxic potential is probably dependent on the physicochemical properties of NPs.
4.2.2 Genotoxicity
Comet assay, also known as the single cell gel electrophoresis assay, is one of the most popular assays used in particle toxicology studies to detect DNA damage, i.e., DNA strand breaks and oxidative DNA damage [30]. By using this method, it has been shown that exposure of human ECs to TiO2 NP, silica NP, carbon black (CB) NPs and micelles based on polyethylenimine (PEI) was associated with DNA damage [31,32,33,34,35]. Another popular method is to measure the formation of γH2AX foci, which has been applied to indicate the DNA damage in human ECs induced by MWCNT, multiwall carbon nano-onion (MWCNO) and CdSe/ZnS QD [36,37,38]. Duan et al. [32] further showed that silica NP (average size 62 nm; concentrations >25 μg/mL) induced DNA damage was associated with G2/M cell cycle checkpoint activation and inhibition of proliferation, which suggested that NP exposure could induce the downstream events associated with DNA damage.
Based on available reports, there appears to be no strong correlation between NP induced DNA damage and cytotoxicity in human ECs. For example, Bayat et al. [31] showed that 24 h exposure to 10 μg/mL TiO2 NPs (primary size 1–3 nm and 30 nm) significantly induced DNA strand damage without an effect on LDH release in human dermal microvascular endothelial cells (HDMVCs). Guo et al. [38] showed that cytotoxicity was significantly induced in HUVECs after 24 h exposure to 10 μg/mL MWCNT (average diameter 30 nm, length <1 μm), whereas DNA damage was induced after incubation with MWCNT as low as 0.5 μg/mL. Xu et al. [36] showed that the EC50 for MWCNO (hydrodynamic size 31.2 nm) induced cytotoxicity was 44.12 μg/mL, whereas γH2AX foci formation was observed in HUVECs after 6 h, 12 h and 24 h incubation with 5 μg/mL MWCNO. These studies indicated that DNA damage could be used as a sensitive marker to reflect NP induced toxicity.
Cowie et al. [35] compared DNA damage induced by TiO2 NPs (20 nm), iron oxide NPs (8 nm, with or without oleic acid coating), silica NPs (25 nm and 50 nm; rhodamine-labeled) and polylactic glycolic acid polyethylene oxide polymeric NPs in a number of different cell lines, namely human lymphoblastoid TK6 cells, human kidney HEK293, monkey kidney COS-1 cells, human cerebral endothelial cells (HCECs), bronchial 16HBE14o cells and human BeWo b30 placental cells. The results showed that HCECs were as effective as other types of cells to identify genotoxic and non-genotoxic NPs, however, the TK6 cells, BeWo b30 and kidney cells seem to be the most reliable for detecting a dose-response.
4.2.3 Endothelial Activation
It has been shown that direct exposure of human ECs to different types of NPs could induce endothelial activation in vitro, i.e., expression of adhesion molecules, release of inflammatory markers and monocyte adhesion. For example, Zhu et al. [39] showed that exposure of HAECs to iron oxide NPs (22 nm and 43 nm) at 2, 20, 100 μg/mL significantly promoted the expression of interleukin 8 (IL-8) and ICAM-1 as well as adhesion of U937 to ECs. Montiel-Davalos et al. [40] reported that TiO2 NPs (average size <50 nm) from 5 to 40 μg/cm2 induced the expression of adhesion molecules (i.e., E-selectin, P-selectin, ICAM-1, VCAM-1 and PECAM-1) as well as adhesion of U937 cells to HUVECs. Li et al. [41] found that exposure of HUVECs to 0.1, 1 and 10 μg/mL ZnO NPs (50 nm), but not the microparticles (>100 nm), was associated with increased expression of ICAM-1 and monocyte adhesion. Meanwhile, elevated expression of ICAM-1 and foam cell formation were also observed in ZnO NP exposed mice. Shi et al. [42] showed that Ag NPs (hydrodynamic size 65 nm) from 0.5 to 2.0 μg/mL induced the expression of inflammatory cytokines (i.e., IL-6, IL-8 and MCP-1) and adhesion molecules (ICAM-1, VCAM-1 and P-selectin). For carbonaceous NPs, Cao et al. [43] showed that 24 h exposure of HUVECs to MWCNT (primary size 700–3000 nm in length × 5–35 nm in diameter, and 400–4000 nm in length × 6–20 nm in diameter) significantly induced expression of ICAM-1 and VCAM-1 at concentrations from 16 to 64 μg/mL as well as monocyte adhesion at 64 μg/mL, whereas CB NPs (primary size 14 nm) only induced significantly increased expression of ICAM-1 and VCAM-1 without an effect on monocyte adhesion at the concentrations of 50 and 100 μg/mL [44].
Meanwhile, by using co-culture models, it has been shown that NPs may also activate ECs without direct contact with ECs. For example, Napierska et al. [45] incubated EA.hy 926 cells (an immortalized EC cell line) with A549 and THP-1 co-cultures that had been exposed to silica NPs (2 and 60 nm) for 12 h, and found increased release of IL-6, IL-8 and MIP-1 in indirectly exposed endothelial monolayer. Snyder-Talkington et al. [46] showed that apical exposure of human small airway epithelial cells (SAEC) to 1.2 μg/mL MWCNT (length 3.86 μm × diameter 49 nm) for 24 h induced the release of VEGFA, sICAM-1 and sVCAM-1 in human microvascular endothelial cells (HMVEC) cultured in basolateral chamber. In a later study, the same group further showed that 24 h incubation of SAEC with 0.5 and 1.0 μg/mL printer-emitted NPs (aerodynamic diameters ranged from 39 to 122 nm) promoted the release of cytokines and chemokines without the internalization of NPs into HMVEC by using the same model [47]. Cao et al. [48] showed that exposure of A549 and THP-1 cells with 8 μg/mL MWCNT (primary size 700–3000 nm in length × 5–35 nm in diameter, and 400–4000 nm in length × 6–20 nm in diameter) for 24 h modestly promoted the release of IL-6 and IL-8 as well as monocyte adhesion in HUVEC monolayer in basolateral chamber. In combination, it is possible that exposure to NPs could lead to endothelial activation in vitro, either due to the direct effect of NPs or an indirect effect by inflammatory mediators.
4.2.4 Dysfunction of NOS and Impaired NO Signaling
The proper function of blood vessels requires the endothelium to release NO, and dysfunction of NO, particularly diminished NO bioactivity due to eNOS uncoupling, has been implicated in the development of cardiovascular diseases [11]. Some of the NPs have been shown to induce eNOS uncoupling and/or decreased NO production. For example, Duan et al. [49] showed that exposure to silica NPs (diameter 62 nm) dose-dependently (25–100 μg/mL) decreased the NO production and activity of eNOS and NOS but increased the activity of iNOS in HUVECs. Similarly, decreased activity of eNOS and NO production have been observed in human ECs after exposure to magnetic ferroferric oxide NPs (diameter ranges from 10 to 15 nm) [50] and superparamagnetic iron oxide (size ranges from 5 to 75 nm) [51]. A decreased NO/peroxynitrite ratio has been observed in HUVECs after exposure to silica NPs with different sizes (10, 50, 150 and 500 nm), especially 10 nm silica NPs [52]. Exposure to detonation diamond NPs (size grains 2–5 nm) [53] or TiO2 NPs (1–3 nm) [31] was also associated with decreased NO production. Although these studies did not attempt measuring the activity of NOS, the decreased NO production could be due to decreased activity of NOS, particularly eNOS uncoupling.
In contrast, exposure to NPs may also promote NOS activity and NO over-production. For example, Zhu et al. [39] showed that iron oxide NPs (22 nm and 43 nm) at 2, 20, 100 μg/mL promoted NO over-production due to elevated NOS activity. Similarly, Su et al. [54] showed that magnetic NPs (diameter 15–20 nm) at 400 μg/mL significantly induced NO production and eNOS activity. Furthermore, an increase of serum NO was also observed in mice after 3 days exposure to 20 mg/kg magnetic NPs. Han et al. [55] showed that exposure to 200 μg/mL ZnS nanoarchitectures was associated with increased NO production and NOS activity in HUVECs, whereas exposure to 5 mg/kg and 10 mg/kg ZnS nanoarchitectures promoted NO in serum and damages to endothelium in aortic root of normal mice. NO over-production was also observed in human ECs after exposure to TiO2 NPs (average size <50 nm) [40] and ZnO NPs (diameter 20 nm; not significantly affected by ZnO NPs with diameter of 90–210 nm) [56], although the NOS activity was not further measured. In combination, exposure of human ECs to NPs could lead to impaired NO signaling, showing as diminished NO bioactivity due to eNOS uncoupling or NO over-production due to increased NOS activity.
4.3 Mechanisms
4.3.1 Oxidative Stress
It well known that exposure to NPs could lead to oxidative stress and inflammation, which could be the mechanisms associated with cardiovascular toxicity of NPs [57, 58]. To explain NP induced oxidative stress and toxicity, a three-tier model has been proposed [59, 60]. This model suggested that at low amount of oxidative stress (tier-1 level), NPs could lead to the antioxidant responses mediated by Nrf-2 signaling pathway. At intermediate amount of oxidative stress (tier-2 level), NPs could induced inflammatory responses due to the activation of NF-κB cascades. At high amount of oxidative stress, NPs could result in oxidative damage and eventually apoptosis and necrosis [59, 60]. Over-production of reactive oxygen species (ROS) or NO has been observed in human ECs after exposure to different kinds of NPs, e.g., Ag NPs, silica NPs, TiO2 NPs and carbonaceous NPs, which may further mediate the oxidative damage of bio-molecules and inhibit the function of antioxidant systems [32, 42,43,44, 52, 61]. Activation of Nrf-2 signaling pathway has also been observed in human ECs after NP exposure. For example, Lai et al. [62] showed that Au NPs enhanced the level and nuclear translocation of the Nrf-2 protein and Bach1 export/tyrosine phosphorylation, leading to the expression of heme oxygenase-1 (HO-1) protein in HUVECs. Guo et al. [63] also found increased protein expression of Nrf-2 and HO-1 in silica NP exposed HUVECs. Interestingly, it has been shown that the presence of antioxidant may prevent NP induced toxicity in human ECs. For instance, Shi et al. [42] showed that Ag NP induced cytotoxicity, intracellular ROS and inflammatory responses in HUVECs were inhibited by the presence of antioxidant N-acetylcysteine (NAC). Similarly, Guo et al. [22] also found that silica NP induced cytotoxicity and oxidative damage was restored by NAC. In another study, Liang et al. [15] showed that exposure of HAECs to ZnO NPs induced cytotoxicity associated with ROS mediated mitochondria membrane potential decrease, cytochrome C release, activation of caspases 3 and caspases 9 and increase of Bax/Bcl-2 ratio. Moreover, these effects were partially or completely inhibited by the treatment of α-lipoic acid (LA). All of these studies suggested that oxidative stress could be the mechanism associated with the toxicity of NPs to ECs, which is in agreement with the three-tier model [59, 60].
4.3.2 Inflammation
As suggested by the three-tier model, intermediate amount of oxidative stress induced by NP exposure could lead to inflammation due to the activation of NF-κB cascades [59, 60]. Activation of NF-κB cascades has also been observed in NP exposed human ECs. For example, Corbalan et al. [52] showed that exposure of HUVECs to silica NPs was associated with increased NF-κB DNA binding activity as well as up-regulation of a number of inflammatory genes. In addition, suppression of NF-κB activity by proteasome inhibitor significantly prevented the up-regulation of ICAM-1, VCAM-1, SELE, F3, and IL-8 induced by silica NPs. In a later study, Guo et al. [63] also showed that exposure of HUVECs to silica NPs was associated with activation of NF-κB and increased expression of a number of inflammatory markers, including IL-1β, IL-6, IL-8, TNFα, ICAM-1, VCAM-1, and MCP-1. Shi et al. [42] found that exposure of HUVECs to Ag NPs increased the phosphorylation of IKKα/β and IκBα (two key proteins of NF-κB), p65 subunit and the formation of the NF-κB nuclear protein-DNA complex, associated with increased expression of inflammatory cytokines and adhesion molecules. Moreover, all of these effects could be prevented by the treatment of antioxidant NAC, which indicated a role of oxidative stress in mediating NP induced NF-κB cascades. Liu and Sun [64] found increased NF-κB activity as well as expression of inflammatory cytokines and adhesion molecules in hydroxyapatite NP exposed HUVEC+THP-1 co-cultures, but not the HUVEC mono-culture. TiO2 NPs have also been shown to induce the translocation of NF-κB and IκBα degradation, which could be responsible for NP induced expression of adhesion molecules and U937 adhesion to HUVECs [40]. All of these studies in combination indicated that exposure to NPs could lead to endothelial dysfunction due to the activation of NF-κB cascades, which is in agreement of the three-tier model.
4.3.3 Dysfunction of Autophagy
Autophagy is a process where cytoplasmic components are sequestered in double-membrane vesicles for degradation into lysosomes, and dysfunction of autophagy has been implicated in endothelial dysfunction and development of cardiovascular diseases [65, 66]. In recent years, it has been suggested that exposure to NPs may lead to autophagy dysfunction (defined as excessive autophagy induction) as the mechanism for NP induced toxicity [67]. In human ECs, it has been shown that a number of NPs, such as iron oxide NPs, TiO2 NPs, Ag NPs and silica NPs, could lead to induction of autophagy [49, 61, 68, 69]. In addition, inhibition of autophagy dysfunction has been shown to attenuate NP induced toxicity to ECs. For example, it has been shown that exposure of HUVECs to Fe3O4 NPs promoted endothelial dysfunction (eNOS uncoupling, inflammatory responses) associated with an induction of autophagy, and suppression of autophagy induction or stimulation of autophagic flux partially attenuated the toxic effects of NPs [50]. Similarly, exposure of HUVECs to carboxylated MWCNT was also shown to be associated with the profound accumulation of autophagosomes due to blockade of the autophagic flux, and stimulation of the autophagic flux attenuated the cytotoxicity of NPs associated with the extracellular release of NPs in autophagic microvesicles [24]. In another study, it was shown that the presence of antioxidant NAC attenuated silica NP induced endothelial toxicity partially through the inhibition of autophagy [22]. All of these studies suggested that excessive autophagy induced by NPs could be one of the mechanisms responsible for NP induced endothelial toxicity.
4.4 Conclusions
Once entering circulation, it is likely that NPs will interact with the endothelium, and it is necessary to assess the toxicity of NPs to ECs to better understand the potential adverse effects of NPs in vivo [9]. By using human ECs, including primary ECs or immortalized EC cell lines, it has been shown that NPs could induce cytotoxicity, genotoxicity, endothelial activation and impairment of NO signaling (Fig. 4.2). Oxidative stress and inflammatory response induced by NPs have been suggested as the mechanisms, as revealed by the three-tier model (Fig. 4.3). In recent years, dysfunction of autophagy (excessive autophagy induction) has also been suggested as one of the mechanisms responsible for NP induced toxicity to ECs. In the future, it is still necessary to use ECs to assess the potential toxic effects of NPs and to study the mechanisms.
The three-tier model to explain NP induced oxidative stress and toxicity. At low amount of oxidative stress (tier-1 level), NPs could lead to the antioxidant responses mediated by Nrf-2 signaling pathway. At intermediate amount of oxidative stress (tier-2 level), NPs could induced inflammatory responses due to the activation of NF-κB cascades. At high amount of oxidative stress, NPs could result in oxidative damage and eventually apoptosis and necrosis. The presence of antioxidant may prevent NP induced toxicity (Originally proposed by Nel et al. [59])
References
European Commission Commission recommendation of 18 October 2011 on the definition of nanomaterial text with EEA relevance. http://eur-lex.europa.eu/legal-content/EN/TXT/?uri=CELEX:32011H0696. Accessed 18 Dec 2011
Donaldson K, Tran L, Jimenez LA et al (2005) Combustion-derived nanoparticles: a review of their toxicology following inhalation exposure. Part Fibre Toxicol 2:10
Donaldson K, Duffin R, Langrish JP et al (2013) Nanoparticles and the cardiovascular system: a critical review. Nanomedicine (Lond) 8:403–423
Vance ME, Kuiken T, Vejerano EP et al (2015) Nanotechnology in the real world: redeveloping the nanomaterial consumer products inventory. Beilstein J Nanotechnol 6:1769–1780
Wong BS, Yoong SL, Jagusiak A et al (2013) Carbon nanotubes for delivery of small molecule drugs. Adv Drug Deliv Rev 65:1964–2015
Wei L, Lu J, Xu H et al (2015) Silver nanoparticles: synthesis, properties, and therapeutic applications. Drug Discov Today 20:595–601
Khan ST, Musarrat J, Al-Khedhairy AA (2016) Countering drug resistance, infectious diseases, and sepsis using metal and metal oxides nanoparticles: current status. Colloids Surf B: Biointerfaces 146:70–83
Soenen SJ, Parak WJ, Rejman J et al (2015) (Intra)cellular stability of inorganic nanoparticles: effects on cytotoxicity, particle functionality, and biomedical applications. Chem Rev 115:2109–2135
Setyawati MI, Tay CY, Docter D et al (2015) Understanding and exploiting nanoparticles’ intimacy with the blood vessel and blood. Chem Soc Rev 44:8174–8199
Libby P (2012) Inflammation in atherosclerosis. Arterioscler Thromb Vasc Biol 32:2045–2051
Karbach S, Wenzel P, Waisman A et al (2014) eNOS uncoupling in cardiovascular diseases – the role of oxidative stress and inflammation. Curr Pharm Des 20:3579–3594
Gimbrone MA Jr, Garcia-Cardena G (2016) Endothelial cell dysfunction and the pathobiology of atherosclerosis. Circ Res 118:620–636
Saptarshi SR, Duschl A, Lopata AL (2015) Biological reactivity of zinc oxide nanoparticles with mammalian test systems: an overview. Nanomedicine (Lond) 10:2075–2092
Sun J, Wang S, Zhao D et al (2011) Cytotoxicity, permeability, and inflammation of metal oxide nanoparticles in human cardiac microvascular endothelial cells: cytotoxicity, permeability, and inflammation of metal oxide nanoparticles. Cell Biol Toxicol 27:333–342
Liang S, Sun K, Wang Y et al (2016) Role of Cyt-C/caspases-9,3, Bax/Bcl-2 and the FAS death receptor pathway in apoptosis induced by zinc oxide nanoparticles in human aortic endothelial cells and the protective effect by alpha-lipoic acid. Chem Biol Interact 258:40–51
Gong Y, Ji Y, Liu F et al (2017) Cytotoxicity, oxidative stress and inflammation induced by ZnO nanoparticles in endothelial cells: interaction with palmitate or lipopolysaccharide. J Appl Toxicol 87:895–901
Gu Y, Cheng S, Chen G et al (2017) The effects of endoplasmic reticulum stress inducer thapsigargin on the toxicity of ZnO or TiO2 nanoparticles to human endothelial cells. Toxicol Mech Methods 27:191–200
Guo H, Zhang J, Boudreau M et al (2016) Intravenous administration of silver nanoparticles causes organ toxicity through intracellular ROS-related loss of inter-endothelial junction. Part Fibre Toxicol 13:21
Danielsen PH, Cao Y, Roursgaard M et al (2015) Endothelial cell activation, oxidative stress and inflammation induced by a panel of metal-based nanomaterials. Nanotoxicology 9:813–824
Yan M, Zhang Y, Xu K et al (2011) An in vitro study of vascular endothelial toxicity of CdTe quantum dots. Toxicology 282:94–103
Yang L, Yan Q, Zhao J et al (2013) The role of potassium channel in silica nanoparticle-induced inflammatory effect in human vascular endothelial cells in vitro. Toxicol Lett 223:16–24
Guo C, Yang M, Jing L et al (2016) Amorphous silica nanoparticles trigger vascular endothelial cell injury through apoptosis and autophagy via reactive oxygen species-mediated MAPK/Bcl-2 and PI3K/Akt/mTOR signaling. Int J Nanomedicine 11:5257–5276
Walker VG, Li Z, Hulderman T et al (2009) Potential in vitro effects of carbon nanotubes on human aortic endothelial cells. Toxicol Appl Pharmacol 236:319–328
Orecna M, De Paoli SH, Janouskova O et al (2014) Toxicity of carboxylated carbon nanotubes in endothelial cells is attenuated by stimulation of the autophagic flux with the release of nanomaterial in autophagic vesicles. Nanomedicine 10:939–948
Ge C, Du J, Zhao L et al (2011) Binding of blood proteins to carbon nanotubes reduces cytotoxicity. Proc Natl Acad Sci U S A 108:16968–16973
Matuszak J, Baumgartner J, Zaloga J et al (2016) Nanoparticles for intravascular applications: physicochemical characterization and cytotoxicity testing. Nanomedicine (Lond) 11:597–616
Menard N, Tsapis N, Poirier C et al (2012) Novel surfactants with diglutamic acid polar head group: drug solubilization and toxicity studies. Pharm Res 29:1882–1896
Liu F, Huang H, Gong Y et al (2017) Evaluation of in vitro toxicity of polymeric micelles to human endothelial cells under different conditions. Chem Biol Interact 263:46–54
Su Y, Zhao L, Meng F et al (2017) Silver nanoparticles decorated lipase-sensitive polyurethane micelles for on-demand release of silver nanoparticles. Colloids Surf B: Biointerfaces 152:238–244
Moller P, Hemmingsen JG, Jensen DM et al (2015) Applications of the comet assay in particle toxicology: air pollution and engineered nanomaterials exposure. Mutagenesis 30:67–83
Bayat N, Lopes VR, Scholermann J et al (2015) Vascular toxicity of ultra-small TiO2 nanoparticles and single walled carbon nanotubes in vitro and in vivo. Biomaterials 63:1–13
Duan J, Yu Y, Li Y et al (2013) Toxic effect of silica nanoparticles on endothelial cells through DNA damage response via Chk1-dependent G2/M checkpoint. PLoS One 8:e62087
Frikke-Schmidt H, Roursgaard M, Lykkesfeldt J et al (2011) Effect of vitamin C and iron chelation on diesel exhaust particle and carbon black induced oxidative damage and cell adhesion molecule expression in human endothelial cells. Toxicol Lett 203:181–189
Calarco A, Bosetti M, Margarucci S et al (2013) The genotoxicity of PEI-based nanoparticles is reduced by acetylation of polyethylenimine amines in human primary cells. Toxicol Lett 218:10–17
Cowie H, Magdolenova Z, Saunders M et al (2015) Suitability of human and mammalian cells of different origin for the assessment of genotoxicity of metal and polymeric engineered nanoparticles. Nanotoxicology 9(1):57–65
Xu Y, Wang SY, Yang J et al (2013) Multiwall carbon nano-onions induce DNA damage and apoptosis in human umbilical vein endothelial cells. Environ Toxicol 28:442–450
Soenen SJ, Montenegro JM, Abdelmonem AM et al (2014) The effect of nanoparticle degradation on amphiphilic polymer-coated quantum dot toxicity: the importance of particle functionality assessment in toxicology [corrected]. Acta Biomater 10:732–741
Guo YY, Zhang J, Zheng YF et al (2011) Cytotoxic and genotoxic effects of multi-wall carbon nanotubes on human umbilical vein endothelial cells in vitro. Mutat Res 721:184–191
Zhu MT, Wang B, Wang Y et al (2011) Endothelial dysfunction and inflammation induced by iron oxide nanoparticle exposure: risk factors for early atherosclerosis. Toxicol Lett 203:162–171
Montiel-Davalos A, Ventura-Gallegos JL, Alfaro-Moreno E et al (2012) TiO(2) nanoparticles induce dysfunction and activation of human endothelial cells. Chem Res Toxicol 25:920–930
Li CH, Liao PL, Shyu MK et al (2012) Zinc oxide nanoparticles-induced intercellular adhesion molecule 1 expression requires Rac1/Cdc42, mixed lineage kinase 3, and c-Jun N-terminal kinase activation in endothelial cells. Toxicol Sci 126:162–172
Shi J, Sun X, Lin Y et al (2014) Endothelial cell injury and dysfunction induced by silver nanoparticles through oxidative stress via IKK/NF-kappaB pathways. Biomaterials 35:6657–6666
Cao Y, Jacobsen NR, Danielsen PH et al (2014) Vascular effects of multiwalled carbon nanotubes in dyslipidemic ApoE−/− mice and cultured endothelial cells. Toxicol Sci 138:104–116
Cao Y, Roursgaard M, Danielsen PH et al (2014) Carbon black nanoparticles promote endothelial activation and lipid accumulation in macrophages independently of intracellular ROS production. PLoS One 9:e106711
Napierska D, Thomassen LC, Vanaudenaerde B et al (2012) Cytokine production by co-cultures exposed to monodisperse amorphous silica nanoparticles: the role of size and surface area. Toxicol Lett 211:98–104
Snyder-Talkington BN, Schwegler-Berry D, Castranova V et al (2013) Multi-walled carbon nanotubes induce human microvascular endothelial cellular effects in an alveolar-capillary co-culture with small airway epithelial cells. Part Fibre Toxicol 10:35
Sisler JD, Pirela SV, Friend S et al (2015) Small airway epithelial cells exposure to printer-emitted engineered nanoparticles induces cellular effects on human microvascular endothelial cells in an alveolar-capillary co-culture model. Nanotoxicology 9:769–779
Cao Y, Roursgaard M, Jacobsen NR et al (2016) Monocyte adhesion induced by multi-walled carbon nanotubes and palmitic acid in endothelial cells and alveolar-endothelial co-cultures. Nanotoxicology 10:235–244
Duan J, Yu Y, Yu Y et al (2014) Silica nanoparticles induce autophagy and endothelial dysfunction via the PI3K/Akt/mTOR signaling pathway. Int J Nanomedicine 9:5131–5141
Zhang L, Wang X, Miao Y et al (2016) Magnetic ferroferric oxide nanoparticles induce vascular endothelial cell dysfunction and inflammation by disturbing autophagy. J Hazard Mater 304:186–195
Astanina K, Simon Y, Cavelius C et al (2014) Superparamagnetic iron oxide nanoparticles impair endothelial integrity and inhibit nitric oxide production. Acta Biomater 10:4896–4911
Corbalan JJ, Medina C, Jacoby A et al (2011) Amorphous silica nanoparticles trigger nitric oxide/peroxynitrite imbalance in human endothelial cells: inflammatory and cytotoxic effects. Int J Nanomedicine 6:2821–2835
Solarska-Sciuk K, Gajewska A, Skolimowski J et al (2013) Stimulation of production of reactive oxygen and nitrogen species in endothelial cells by unmodified and Fenton-modified ultradisperse detonation diamond. Biotechnol Appl Biochem 60:259–265
Su L, Han L, Ge F et al (2012) The effect of novel magnetic nanoparticles on vascular endothelial cell function in vitro and in vivo. J Hazard Mater 235–236:316–325
Han L, Su L, Chen D et al (2015) ZnS nanoarchitectures induced dysfunction of vascular endothelial cells in vitro and in vivo. Environ Toxicol 30:755–768
Chuang KJ, Lee KY, Pan CH et al (2016) Effects of zinc oxide nanoparticles on human coronary artery endothelial cells. Food Chem Toxicol 93:138–144
Moller P, Christophersen DV, Jacobsen NR et al (2016) Atherosclerosis and vasomotor dysfunction in arteries of animals after exposure to combustion-derived particulate matter or nanomaterials. Crit Rev Toxicol 46:437–476
Cao Y, Long J, Ji Y et al (2016) Foam cell formation by particulate matter (PM) exposure: a review. Inhal Toxicol 28:583–590
Nel A, Xia T, Madler L et al (2006) Toxic potential of materials at the nanolevel. Science 311:622–627
Nel A, Xia T, Meng H et al (2013) Nanomaterial toxicity testing in the 21st century: use of a predictive toxicological approach and high-throughput screening. Acc Chem Res 46:607–621
Halamoda KB, Chapuis BC, Guney-Ayra S et al (2012) Induction of oxidative stress, lysosome activation and autophagy by nanoparticles in human brain-derived endothelial cells. Biochem J 441:813–821
Lai TH, Shieh JM, Tsou CJ et al (2015) Gold nanoparticles induce heme oxygenase-1 expression through Nrf2 activation and Bach1 export in human vascular endothelial cells. Int J Nanomedicine 10:5925–5939
Guo C, Xia Y, Niu P et al (2015) Silica nanoparticles induce oxidative stress, inflammation, and endothelial dysfunction in vitro via activation of the MAPK/Nrf2 pathway and nuclear factor-kappaB signaling. Int J Nanomedicine 10:1463–1477
Liu X, Sun J (2014) Potential proinflammatory effects of hydroxyapatite nanoparticles on endothelial cells in a monocyte-endothelial cell coculture model. Int J Nanomedicine 9:1261–1273
Jiang F (2016) Autophagy in vascular endothelial cells. Clin Exp Pharmacol Physiol 43:1021–1028
Gatica D, Chiong M, Lavandero S et al (2015) Molecular mechanisms of autophagy in the cardiovascular system. Circ Res 116:456–467
Stern ST, Adiseshaiah PP, Crist RM (2012) Autophagy and lysosomal dysfunction as emerging mechanisms of nanomaterial toxicity. Part Fibre Toxicol 9:20
Manshian BB, Pfeiffer C, Pelaz B et al (2015) High-content imaging and gene expression approaches to unravel the effect of surface functionality on cellular interactions of silver nanoparticles. ACS Nano 9:10431–10444
Yang FY, Yu MX, Zhou Q et al (2012) Effects of iron oxide nanoparticle labeling on human endothelial cells. Cell Transplant 21:1805–1820
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 The Author(s)
About this chapter
Cite this chapter
Cao, Y. (2018). The Toxicity of Nanoparticles to Human Endothelial Cells. In: Saquib, Q., Faisal, M., Al-Khedhairy, A., Alatar, A. (eds) Cellular and Molecular Toxicology of Nanoparticles. Advances in Experimental Medicine and Biology, vol 1048. Springer, Cham. https://doi.org/10.1007/978-3-319-72041-8_4
Download citation
DOI: https://doi.org/10.1007/978-3-319-72041-8_4
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-72040-1
Online ISBN: 978-3-319-72041-8
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)