Abstract
According to the European Association of Urology (EAU), urinary sepsis (urosepsis) corresponds to a urinary tract infection (UTI) with signs and symptoms of systemic inflammatory response. Alternatively, urosepsis is defined by the presence of bacteraemia with a urinary tract focus.
Compared to the epidemiology of uncomplicated UTIs, community-acquired and healthcare-associated (nosocomial) urosepsis most likely occurs in elderly males and in patients with risk factors for complicated UTIs. Although decreasing with improved standards of care, the morbidity and mortality of urosepsis remain substantial.
The aim of cross-sectional imaging in severe UTIs include (a) to detect urological complications requiring directed treatment; (b) document congenital, acquired or postsurgical anatomical situations predisposing to infection; and (c) confirm sepsis from urological source over other potential causes.
Multidetector CT (including intravenous contrast enhancement unless contraindicated) provides comprehensive, reliable investigation of urinary sepsis, resulting in major abnormal findings in almost one-third of patients, which require directed intervention in approximately one-half of cases. Furthermore, CT detects signs of haematogenous septic dissemination in other organs and provides consistent follow-up of severe or complicated UTIs after medical or interventional therapy.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Although extremely common, urinary tract infections (UTI) encompass a wide range of conditions which range from asymptomatic bacteriuria and simple cystitis causing local symptoms to potentially life-threatening conditions. Generally, urinary sepsis or urosepsis is defined by the presence of bacteraemia with a urinary tract infectious focus [1].
The incidence of sepsis is reportedly increasing, in both community-acquired and healthcare-associated (nosocomial) UTIs. Patients with the RENUC risk factors (as listed in Table 1.1 in the introductory chapter of this book) are much more likely to develop urosepsis, such as diabetics, immunosuppressed and transplant recipients, those treated with corticosteroid or chemotherapy, those with urolithiasis, obstructed urinary tract, neurogenic bladder and congenital abnormalities, or following recent instrumentation. Although associated with a better prognosis compared to other systemic infections, urosepsis remains a critical situation, particularly in the elderly and immunocompromised. The associated mortality is estimated to fall in the range between 20 and 40% and is probably declining due to improvements in patient care. However, mortality remains considerable in severe sepsis (defined by the development of organ dysfunction) and in septic shock with persistent hypotension despite fluid resuscitation [1, 2].
2 Role of Imaging in Urosepsis
Suspected urosepsis requires early diagnosis and timely treatment, particularly in those patients with risk factors for complicated UTI. The role of imaging includes:
-
(a)
To detect urological complications requiring directed treatment, such as abscess and pyonephrosis
-
(b)
To document congenital, acquired or postsurgical anatomical situations which predispose to infection
-
(c)
To confirm urological cause of sepsis while excluding other potential sources in the body
The ultimate aim is to prevent renal function deterioration and to decrease morbidity and mortality [1, 3].
As well known, first-line ultrasound readily allows detecting urinary obstruction and pyonephrosis requiring prompt drainage without use of ionizing radiation and intravenous contrast medium. However, as extensively discussed in other chapters of this book, multidetector CT (including intravenous contrast enhancement unless contraindicated) is superior to ultrasound in the detection of infection and abscesses and by far represents the ideal modality to comprehensively investigate severe UTI and possible complications [4,5,6,7,8,9,10].
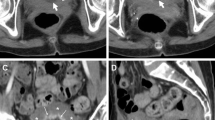
Figures 17.1, 17.2, and 17.3 present three clinical examples of cross-sectional imaging investigation of urinary sepsis. In our experience, the use of CT is particularly useful in the postoperative setting after urological instrumentation and surgery [9, 11,12,13].
A 71-year-old female with a congenital solitary kidney was hospitalized for voiding difficulty and high fever unresponsive to empirical antibiotics. Urgent unenhanced (a) and post-contrast (b–d) multidetector CT revealed mild hydronephrosis with preserved renal function. The dilated renal pelvis (*) showed minimal, enhancing mural thickening (thin arrows in b) which was even more pronounced along the ureter (thin arrow in c) and in the bladder (thin arrow in d; note Foley catheter indicated by thick arrow). Findings were consistent with diagnosis of urosepsis which required prolonged in-hospital treatment. Four months after discharge, repeated CT (e, f) showed decreased hydronephrosis, normalized mural thickening and disappearance of urothelial hyperenhancement. Note absent left kidney
A 41-year-old female immigrant from the Middle East had history of renal colic 2 years ago. Currently attended at emergency department for abdominal and right flank pain associated with shivers, high fever and dysuria. Laboratory tests revealed leukocytosis and increased acute phase reactants. Urgent contrast-enhanced CT (a, b) showed mild, hyperenhancing thickening of the renal pelvis (thin arrows), calyceal dilatation (arrow) at the upper renal third, two wedge-shaped hypoperfused parenchymal areas (*), consistent with right acute pyelitis and pyelonephritis. Transferred to intensive care unit, she progressively improved with medical therapy. Urine cultures diagnosed Escherichia coli infection. Before discharge, repeated CT (c, d) showed resolution of parenchymal changes and persistence of calyceal dilatation (arrow) and of pelvic urothelial enhancement (thin arrows). Distant follow-up CT (e, f) showed resolved hydronephrosis and urothelial enhancement and persistent upper calyceal dilatation (arrows) with focal thinning of the overlying parenchyma consistent with chronic “scarring”
A 61-year-old male with recent radical cystectomy for bladder carcinoma and orthotopic neobladder (§) reconstruction, as documented by postoperative multidetector CT urography. Note right-sided hydronephrosis (*) with delayed contrast excretion. A year later, he was hospitalized for sepsis and acute renal failure. Unenhanced CT (b) showed stable dilatation of the right renal pelvis (*) with appearance of peripelvic and perirenal “fat stranding” (+) and of ipsilateral fascial thickening (thin arrows). Pyonephrosis was relieved by ureteral stenting (thick arrows) as seen on repeated unenhanced CT (c, d) with resolution of perirenal inflammation and persistently thickened posterior renal fascia (thin arrow in d). With resolution of urosepsis and improved renal function, follow-up contrast-enhanced CT (e, f) showed resolution of infectious changes, preserved nephrographic effect, stable hydronephrosis (*) compared to (a) and well-distended neobladder (§)
In a large study including 221 adult patients experiencing first-time urosepsis, the use of CT discovered major findings in almost one-third (32%) of patients, particularly hydro- or pyonephrosis (17%) and urolithiasis (7.6%). Other findings in descending order or frequency included tumours, renal abscesses, ureteral dilatation, calyceal dilatation, duplex kidney, ureteral structure, infected polycystic kidney, emphysematous pyelonephritis and displaced nephrostomy. Clinical predictors of major abnormalities include increased serum creatinine, type 2 diabetes, diabetic complications, known renal disease or urological abnormality. Interestingly, abnormal CT findings led to urological intervention in approximately one-half of cases, such as positioning or replacement of nephrostomy or ureteral stent, sometimes cyst drainage, catheter replacement, stone removal and occasionally even nephrectomy [3].
Furthermore, multidetector CT provides panoramic body exploration, thus allowing to detect infectious changes resulting from haematogenous dissemination in other anatomical regions, which are most usually found in the lungs, the brain, the liver and spleen and the iliopsoas muscles [14]. Finally, as exemplified in Figs. 17.1, 17.2, and 17.3, cross-sectional CT imaging is highly valuable to provide consistent follow-up of severe or complicated UTIs during medical or interventional therapy, in order to document resolution of infectious changes or long-term sequelae [5,6,7,8].
References
Grabe M, Bartoletti R, Bjerklund-Johansen TE et al (2014) Guidelines on urological infections. European Association of Urology, The Netherlands. Available at: http://uroweb.org/wp-content/uploads/19-Urological-infections_LR2.pdf
Foxman B (2003) Epidemiology of urinary tract infections: incidence, morbidity, and economic costs. Dis Mon 49:53–70
Sorensen SM, Schonheyder HC, Nielsen H (2013) The role of imaging of the urinary tract in patients with urosepsis. Int J Infect Dis 17:e299–e303
van Nieuwkoop C, Hoppe BP, Bonten TN et al (2010) Predicting the need for radiologic imaging in adults with febrile urinary tract infection. Clin Infect Dis 51:1266–1272
Ifergan J, Pommier R, Brion MC et al (2012) Imaging in upper urinary tract infections. Diagn Interv Imaging 93:509–519
Craig WD, Wagner BJ, Travis MD (2008) Pyelonephritis: radiologic-pathologic review. Radiographics 28:255–277. quiz 327–258
Demertzis J, Menias CO (2007) State of the art: imaging of renal infections. Emerg Radiol 14:13–22
Browne RF, Zwirewich C, Torreggiani WC (2004) Imaging of urinary tract infection in the adult. Eur Radiol 14(Suppl 3):E168–E183
Tonolini M, Ippolito S (2016) Cross-sectional imaging of complicated urinary infections affecting the lower tract and male genital organs. Insights Imaging 7(5):689–711
Lee MJ (2002) Non-traumatic abdominal emergencies: imaging and intervention in sepsis. Eur Radiol 12:2172–2179
Tonolini M, Ierardi AM, Varca V et al (2015) Multidetector CT imaging of complications after laparoscopic nephron-sparing surgery. Insights Imaging 6:465–478
Tonolini M, Villa F, Ippolito S et al (2014) Cross-sectional imaging of iatrogenic complications after extracorporeal and endourological treatment of urolithiasis. Insights Imaging 5:677–689
Tonolini M, Villa F, Bianco R (2013) Multidetector CT imaging of post-robot-assisted laparoscopic radical prostatectomy complications. Insights Imaging 4:711–721
Tonolini M, Campari A, Bianco R (2012) Common and unusual diseases involving the iliopsoas muscle compartment: spectrum of cross-sectional imaging findings. Abdom Imaging 37:118–139
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG
About this chapter
Cite this chapter
Tonolini, M. (2018). Cross-Sectional Imaging of Urosepsis. In: Tonolini, M. (eds) Imaging and Intervention in Urinary Tract Infections and Urosepsis. Springer, Cham. https://doi.org/10.1007/978-3-319-68276-1_17
Download citation
DOI: https://doi.org/10.1007/978-3-319-68276-1_17
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-68275-4
Online ISBN: 978-3-319-68276-1
eBook Packages: MedicineMedicine (R0)