Abstract
The storage of excess body fat has profound effects on intermediary metabolism and endocrine function. Here, I review the effects of obesity on linear growth and bone maturation, thyroid function, sexual development, adrenal function, calcium homeostasis, and bone mineralization. Subsequent chapters in this volume discuss the implications of obesity for insulin production and action and the regulation of glucose tolerance, blood pressure, lipid metabolism, atherogenesis, sleep hygiene, and hepatic, renal, and neurologic function.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Childhood obesity
- Growth hormone
- Insulin-like growth factor (IGF)
- Thyroid hormone
- Adrenal function
- Cortisol
- Prolactin
- Pseudohypoparathyroidism
- Adrenarche
- Puberty
- Gynecomastia
- Vitamin D
- Bone mineralization
Introduction
The accumulation of excess body fat has profound effects on somatic development and endocrine function. Here I review the effects of obesity on linear growth and bone maturation, thyroid function, sexual development, adrenal function, calcium homeostasis, and bone mineralization.
Effects of Obesity on Linear Growth and Bone Maturation
Final adult height in otherwise normal obese children generally falls within two standard deviations of parental target height. However, rates of linear growth and bone maturation are often increased in obese pre- and peri-pubertal children despite marked reductions in basal and stimulated plasma growth hormone (GH) concentrations and a reduction in circulating GH half-life [1]. The reduction in GH secretion in obese children and adults has been ascribed to negative feedback by free fatty acids, a reduction in plasma ghrelin (a GH secretagogue produced by the stomach), and nutrient-stimulated increases in IGF-1 production. Total IGF-1 and IGF binding protein (BP)-3 concentrations in obese subjects are typically normal or mildly elevated; this may reflect in part the production of IGF-1 and IGFBP-3 by white adipose tissue [2, 3] and/or an increase in hepatic GH sensitivity, resulting from induction of hepatic GH receptors by hyperinsulinemia (Fig. 20.1). Induction of GH receptor expression in obesity is suggested by an increase in levels of GH binding protein [4], the circulating form of the extracellular GH receptor domain, and by heightened production of IGF-1 following a single dose of GH [5].
Total IGF-2 concentrations were elevated in obese adults in two studies but were normal in a study of obese adolescents [6]. Many investigations have found reductions in serum IGF binding proteins 1 and 2 (IGFBP-1 and BP-2) , which correlate inversely with plasma insulin concentrations and liver fat content [7,8,9,10,11,12]. The decreases in IGFBPs 1 and 2 are postulated to increase the bioavailability of IGF-1, which may maintain or increase linear growth in obesity despite diminished GH secretion [13,14,15] (Fig. 20.1). “Free” IGF-1 levels have been found to be elevated in some, but not all, studies of obese adults [13, 14]. Interestingly, increased rates of linear growth and reductions in fat mass have been observed in mouse models engineered to make endogenous IGF-1 incapable of binding to IGF binding proteins [16].
Reductions in plasma IGFBP-1 or IGFBP-2 concentrations in insulin-resistant obese subjects may facilitate weight gain because overexpression of IGFBP-1 or IGFBP-2 in transgenic mice reduces adipogenesis and prevents diet-induced obesity. Interestingly BP-1 excess reduces insulin sensitivity but BP-2 excess improves glucose tolerance [8, 17, 18].
Growth and bone maturation in obesity may be potentiated by increases in adrenal androgen production (Fig. 20.1 and below) (see also Fig. 20.3); bone age may be advanced as much as 1–2 years in children with precocious adrenarche, which is more common in obese children. The hyperleptinemia of obesity also appears to play a role (Fig. 20.1). Circulating leptin levels rise in proportion to body (particularly subcutaneous) fat stores and are higher in girls than in boys. Leptin stimulates proliferation of isolated mouse and rat osteoblasts and increases the width of the chondroprogenitor zone of the mouse mandible in vivo. Conversely, leptin deficiency in ob/ob mice reduces cortical bone mass but increases trabecular mass [19]; leptin treatment increases femoral length, bone area, and bone mineral content [20] and may promote the differentiation of osteoblasts from bone marrow stem cells [19]. The effects of leptin may be exerted in concert with IGF-1 because leptin increases IGF-1 receptor expression in mouse chondrocytes [21]. Nevertheless, linear growth is normal in patients with congenital deficiencies of leptin or the leptin receptor [22, 23].
Effects of Obesity on Thyroid Function
Free T4 levels generally fall within the normal range in obese subjects but thyroid-stimulating hormone (TSH) and triiodothyronine (T3) concentrations are mildly, and variably, elevated. The increase in T3 reflects its peripheral conversion from circulating T4 [1, 24] (Fig. 20.2). Higher levels of T3 increase thermogenesis and energy expenditure [25, 26] and may thereby limit further weight gain; see also Chap. 7 on Brown Adipose Tissue. Conversely, caloric restriction and weight loss decrease T3 levels, reducing energy expenditure and thereby facilitating weight regain.
The effects of caloric excess and deprivation on thyroid hormone levels are mediated in part by leptin-dependent effects on hypothalamic TRH production (Fig. 20.2). Thyroid hormone levels are variably low in leptin receptor-deficient humans and are reduced in leptin receptor-deficient db/db mice. Leptin treatment reverses the loss of TSH pulsatility that accompanies short-term fasting and normalizes thyroid hormone levels following longer-term caloric restriction. These actions are mediated by direct effects of leptin/STAT3 signaling on TRH transcription and indirect effects on TRH production mediated by increases in ∝MSH and reductions in agouti-related peptide (AgRP) and neuropeptide Y [27, 28]. By increasing sympathetic nervous system activity and deiodinase expression, hyperleptinemia may also promote peripheral T4 to T3 conversion [29, 30].
Some clinicians consider a mild elevation of TSH (typically in the range of 4.5–7 uIU/mL) in an obese child with normal free T4 to represent a state of subclinical hypothyroidism. However, the elevation of TSH may reflect hyperleptinemia rather than thyroid dysfunction. The author would consider thyroid hormone replacement in a child with elevated TSH if (a) there is a goiter, (b) the child is seropositive for thyroid antibodies, (c) the TSH exceeds 8–10 uIU/mL), (d) the T3 is not markedly elevated, and/or (e) the child’s symptoms or physical findings (other than obesity) suggest a true hypothyroid state.
Effects of Obesity on Gonadal Function and Pubertal Development
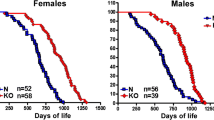
Recent studies show that obesity in early childhood (age 36–54 months) and excessive weight gain between 3–9 years of age increase the risks of precocious thelarche in girls and reduce by ~6–9 months the age of menarche [31]. Since leptin promotes gonadotropin secretion and rises transiently before the onset of puberty in normal weight children, it is possible that the hyperleptinemia of obesity promotes early sexual maturation, at least in girls.
More commonly, obese girls and boys develop precocious adrenarche without true puberty, and obese adolescent females are prone to ovarian hyperandrogenism with mild hirsutism, acne, anovulation, and menstrual irregularity. The pathogenesis of precocious adrenarche and ovarian hyperandrogenism in obesity remains poorly understood (Fig. 20.3). However, insulin and IGF-1 in excess act in synergy with adrenocorticotrophic hormone (ACTH) and luteinizing hormone (LH) to stimulate the production of androgens from adrenocortical cells and ovarian theca cells, respectively. These effects are mediated through induction of P450c17α hydroxylase activity. The biologic availability of ovarian and adrenal androgens is increased because insulin suppresses hepatic sex hormone-binding globulin (SHBG) expression and reduces plasma SHBG concentrations. In obese girls with polycystic ovary syndrome, the free androgens (and, possibly, hyperinsulinemia) increase the frequency of LH pulses [32, 33] and the ratio of LH to follicle-stimulating hormone (FSH), thereby exacerbating thecal androgen production. The increase in free androgens can cause precocious adrenarche in prepubertal girls and boys and anovulation, hirsutism, and acne in adolescent girls and young women. Thus, obesity may mimic and clearly exacerbates the reproductive phenotype of the polycystic ovary syndrome [34,35,36] (Fig. 20.3); see also Chap. 36 by Dr. Barber and colleagues.
Free and total testosterone levels are generally normal in boys with mild to moderate obesity but decline with dramatic weight gain in association with normal or low gonadotropin levels. Among a group of obese teenage boys [37] aged 14–20 years, free testosterone levels were inversely related to BMI and measures of insulin resistance (HOMA-IR). LH, FSH, and estradiol levels were normal or low, suggesting suppression of the hypothalamic-pituitary-gonadal axis.
The mechanisms driving the fall in testosterone in obese adolescents (and adults) are unclear (Fig. 20.4); potential mediators include hypothalamic resistance to insulin and leptin and increases in circulating proinflammatory cytokines, which in concert reduce gonadotropin releasing-hormone (GnRH) secretion and LH pulse amplitude [38]. In addition, resistance to insulin action in bone may reduce circulating levels of osteocalcin (see below), an osteoblast hormone that in mice promotes Leydig cell testosterone production [39]. Testosterone levels in obese boys and men can be restored with weight loss.
Obesity is now the most common cause of gynecomastia in teenage boys. Aromatization of androgens by adipose tissue likely increases local estrogen concentrations (Fig. 20.4), causing true breast enlargement (commonly superimposed upon adipomastia). In rare cases, gynecomastia in obese boys and ovarian hyperandrogenism in obese teenage girls are caused by hyperprolactinemia. Prolactin levels are typically normal or low in obese children [40]. However, hyperprolactinemia in children with pituitary tumors may be associated with weight gain in children as well as adults [41, 42]. Studies in rodents suggest that prolactin-dependent weight gain derives from increases in food intake and white adipogenesis [43,44,45,46,47,48,49]; alternatively, hyperprolactinemia may cause weight gain and fat deposition in pubertal and postpubescent boys and girls by suppressing sex steroid production [50].
Effects of Obesity on Glucocorticoid Production and Turnover
The abdominal weight gain, striae, hirsutism, and menstrual irregularity that may accompany obesity are often confused with Cushing’s syndrome . In contrast to “exogenous” obesity, Cushing’s syndrome is typically associated with linear growth failure and delayed bone maturation (unless a primary adrenal tumor produces excess androgens as well as glucocorticoids) as well as broad (>1 cm diameter), atrophic, and/or hemorrhagic/violaceous striae, rather than thin (<1 cm diameter) pink striae. Basal plasma, salivary, and urinary free cortisol concentrations and basal ACTH levels in obese, non-Cushingoid children generally fall within the normal range, and diurnal variation and the response to dexamethasone are maintained [51]. However, body fat mass correlates with total excretion of glucocorticoid metabolites, suggesting that obesity is accompanied by increased cortisol secretion and turnover.
Polymorphisms in the glucocorticoid receptor have been associated with obesity, hypertension, and insulin resistance in some studies in adults. However, in contrast to the mineralocorticoid receptor (which binds cortisol with very high affinity), the glucocorticoid receptor is not overexpressed in white adipose tissue of obese adults [52]. Regulation of tissue glucocorticoid metabolism, rather than circulating cortisol levels per se, may be a critical determinant of fat distribution and peripheral insulin sensitivity in non-Cushingoid obese subjects [53]. Many investigations find overexpression of 11βHSD-1 in visceral adipose tissue of obese adults. In theory, the resulting overproduction of cortisol may either cause or aggravate pre-existing visceral adiposity and insulin resistance. On the other hand, some studies find lower expression of 11βHSD-1 in preadipocytes of obese, nondiabetic adults [54]; the expected reduction in tissue cortisol concentrations is postulated to reduce adipogenesis, stabilize or reverse pre-existing weight gain, and increase insulin sensitivity. Conversely, an increase in 11βHSD-1 expression after weight loss might in theory facilitate adipose cortisol production, adipogenesis, and weight rebound.
Effects of Obesity on Calcium Homeostasis, Bone Mineralization, and Fractures
25-OH Vitamin D, Parathyroid Hormone (PTH), and Vitamin D Binding Protein in Obesity
Adolescents and adults with severe obesity, particularly those with dark skin, often have subnormal circulating levels of 25-hydroxyvitamin D (25-OHD). One study [55] found that 25-OHD levels were less than 20 ng/mL in 78.4% of markedly obese (BMI 43.3) African American teenage girls (mean age 14 years). Reductions in 25-OHD are less frequent in obese white than in black or Hispanic children [56]: in a total of 127 obese adolescents (mean age 13 years, BMI 36.4), low levels of 25-OHD were noted in 43.6% of Hispanics and 48.7% of African Americans but only 10.2% of Caucasians. In that study, levels of 25-OHD correlated inversely with serum parathyroid hormone (PTH) . A more recent investigation [57] showed that 17 of 58 obese adolescents (mean 14.9 years, BMI 36, 66% female, 14% black) had 25-OHD levels below 20 ng/mL; however, none had elevated (>65 ng/mL) PTH levels, and bone mineral content and density fell within the normal range.
In theory, the reductions in 25-OHD levels in obese children may be explained by decreased intake of vitamin D-containing dairy products, decreased cutaneous synthesis of vitamin D3 (in persons of color), and/or reduced bioavailability of vitamin D3 owing to sequestration in adipose tissue [58]. However, recent investigations suggest that rates of “vitamin D deficiency” in obese subjects may be drastically overestimated by standard measurements of 25-OHD, which encompass the fraction bound with high affinity to vitamin D binding protein (85–90% of total circulating 25-OHD), the fraction bound with low affinity to albumin (10–15% of total), and the unbound or “free” 25-OHD (<1% of total). A number of investigators consider free and albumin-bound 25-OHD to be “bioavailable” and therefore biologically active. Studies in Italian and American adolescents [59] and American adults [60] found normal levels of “bioavailable” 25-OHD and PTH in obese subjects with low total 25-OHD; moreover, unlike total 25-OHD, the levels of bioavailable 25-OHD did not correlate with either BMIz or the metabolic syndrome. The differences between total and bioavailable 25-OHD in obesity were explained by downregulation of vitamin D binding protein. Interestingly, vitamin D binding protein levels were ~50% lower in African American than in Caucasian teenage girls and, in contrast to bioavailable 25-OHD, correlated inversely with plasma insulin and HOMA-IR [61]. These findings suggest that levels of biologically active 25-OHD are maintained in obesity and insulin resistance through reductions in vitamin D binding protein. Given that vitamin D treatment neither prevents nor reverses weight gain or insulin resistance in obese subjects [62,63,64], the widespread treatment of obese children of color with mild reductions of (total) 25-OHD should be reconsidered pending development of standard assays for vitamin D binding protein and bioavailable 25OH D.
Bone Density and Fracture Rates in Obese Children
Bone quality depends on sex, age, pubertal development, and nutritional status and is modulated by hormones, growth factors, cytokines, and a variety of genetic and environmental factors including vitamin and micronutrient intake, sun exposure, weight bearing, and physical activity, which promote bone accrual and strength. In general, bone density is more closely related to lean body mass than to fat mass [65]; the increases in lean as well as fat mass in obesity are associated with increased bone mass in boys and with increased bone density and bone mass in girls [66]. Nevertheless, the literature is inconsistent and its findings are highly variable. Some studies show mild reductions in bone mineral content in obese subjects; others find that overweight and obese children have normal or increased bone mass compared with lean controls. One investigative group finds that bone mineral content, bone density, and bone mass are reduced in obese children with insulin resistance or prediabetes but not in otherwise healthy obese children [67].
It is likely that hormones and cytokines produced by adipose tissue and infiltrating immune cells mediate effects of obesity on bone development [65]. High levels of leptin and inflammatory cytokines (including TNF-α and interleukin 6) and low levels of adiponectin and ghrelin in obese subjects with insulin resistance and glucose intolerance act in concert to promote bone resorption and reduce bone density. Resistance to insulin in bone reduces both bone formation and osteoclast differentiation and impedes the release of osteocalcin (see below). These effects are countered by sex steroids, which inhibit bone resorption and promote bone growth by recruiting osteoblast precursors from a common osteoadipogenic stem cell and by inhibiting the trans-differentiation of osteogenic to adipogenic precursors [65]. The effects of sex steroids in males as well as females are mediated by estrogen receptor signaling.
It is unclear if changes in bone density or mass in obesity alter current or future fracture risk. A retrospective review of medical records of more than 900,000 children [68] found that obesity was associated with a modest increase in fracture risk (odds ratio 1.23–1.42). In contrast, a prospective cross-sectional study of 2213 otherwise healthy children [69] found that obesity reduced fracture risk (OR 0.75). Experiments in mice suggest that high-fat feeding increases bone density but reduces bone strength, bending stiffness, and fracture resistance [70].
Osteopontin, Osteocalcin, and the Complications of Obesity
Bone cells produce a number of proteins that appear to play important roles in the pathogenesis of obesity and its metabolic complications. The osteoclast matrix glycoprotein osteopontin is markedly upregulated in adipose tissue of obese humans and mice [71]. It reduces insulin sensitivity in adipocytes and hepatocytes through recruitment of tissue monocytes and macrophages and local production of inflammatory cytokines [72, 73]. Plasma levels are increased in adults with obesity, insulin resistance, and type 2 diabetes [74, 75]. In contrast, serum osteopontin was not increased in a single study of obese adolescents [76]. It should be noted, however, that circulating osteopontin levels vary widely in the normal population and decline sharply during and after puberty, making comparisons among varying age groups difficult.
Like osteopontin, the plasma levels of the osteoblast protein osteocalcin decline with age [77]. Plasma osteocalcin is downregulated by leptin and the glucocorticoids; levels are reduced in children as well as adults with obesity, diabetes, and other insulin-resistant states [65, 78,79,80].
The carboxylated form of osteocalcin is stored in bone matrix; in response to bone resorption induced by insulin or parathyroid hormone, the protein is decarboxylated and released into the circulation, where it boosts energy expenditure through induction of BAT thermogenesis, reduces white adipose mass, increases insulin sensitivity, and improves glucose tolerance [80, 81]. A knockout of osteocalcin or its receptor in mice [80, 81] reduces energy expenditure, increases abdominal fat mass, reduces pancreatic beta cell mass and insulin production, decreases insulin sensitivity, impairs glucose tolerance, and reduces Leydig cell testosterone production. The fall in plasma osteocalcin in obese children and adults would therefore be expected to exacerbate the metabolic and reproductive phenotypes associated with obesity. Potential adaptive benefits of low osteocalcin in obesity might include a reduction in insulin-dependent bone resorption; this would implicate a functional axis with feedback loops involving the bone, pancreas, gonad, and adipose tissue.
References
Douyon L, Schteingart DE. Effect of obesity and starvation on thyroid hormone, growth hormone and cortisol secretion. Endocrinol Metab Clin N Am. 2002;31:173–89.
Wabitsch M, Heinze E, Debatin KM, Blum WF. IGF-I- and IGFBP-3-expression in cultured human preadipocytes and adipocytes. Horm Metab Res. 2000;32:555–9.
Peter MA, Winterhalter KH, Boni-Schnetzler M, Froesch ER, Zapf J. Regulation of insulin-like growth factor-I (IGF-I) and IGF-binding proteins by growth hormone in rat white adipose tissue. Endocrinology. 1993;133:2624–31.
Kratzsch J, Dehmel B, Pulzer F, et al. Increased serum GHBP levels in obese pubertal children and adolescents: relationship to body composition, leptin and indicators of metabolic disturbances. Int J Obes. 1997;21:1130–6.
Gleeson HK, Lissett CA, Shalet SM. Insulin-like growth factor-I response to a single bolus of growth hormone is increased in obesity. J Clin Endocrinol Metab. 2005;90:1061–7.
Wabitsch M, Blum WF, Muche R, Heinze E, Haug C, Mayer H, Teller W. Insulin-like growth factors and their binding proteins before and after weight loss and their associations with hormonal and metabolic parameters in obese adolescent girls. Int J Obes Relat Metab Disord. 1996;20(12):1073–80.
Wheatcroft SB, Kearney MT. IGF-dependent and IGF-independent actions of IGF-binding protein-1 and -2: implications for metabolic homeostasis. Trends Endocrinol Metab. 2009;20:153–62.
Nam SY, Lee EJ, Kim KR, Cha BS, Song YD, Lim SK, Lee HC, Huh KB. Effect of obesity on total and free insulin-like growth factor (IGF)-1, and their relationship to IGF-binding protein (BP)-1, IGFBP-2, IGFBP-3, insulin, and growth hormone. Int J Obes Relat Metab Disord. 1997;21(5):355–9.
Saitoh H, Kamoda T, Nakahara S, Hirano T, Nakamura N. Serum concentrations of insulin, insulin-like growth factor(IGF)-I, IGF binding protein (IGFBP)-1 and -3 and growth hormone binding protein in obese children: fasting IGFBP-1 is suppressed in normoinsulinaemic obese children. Clin Endocrinol. 1998;48(4):487–92.
Kotronen A, Lewitt M, Hall K, Brismar K, Yki-Jarvinen H. Insulin-like growth factor binding protein 1 as a novel specific marker of hepatic insulin sensitivity. J Clin Endocrinol Metab. 2008;93:4867–72.
Ballerini MG, Ropelato MG, Domené HM, Pennisi P, Heinrich JJ, Jasper HG. Differential impact of simple childhood obesity on the components of the growth hormone-insulin-like growth factor (IGF)-IGF binding proteins axis. J Pediatr Endocrinol Metab. 2004;17(5):749–57.
Hoeflich A, Russo VC. Physiology and pathophysiology of IGFBP-1 and IGFBP-2 - consensus and dissent on metabolic control and malignant potential. Best Pract Res Clin Endocrinol Metab. 2015;29(5):685–700.
Frystyk J, Skjaerbaek C, Vestbo E, Fisker S, Orskov H. Circulating levels of free insulin-like growth factors in obese subjects: the impact of type 2 diabetes. Diabetes Metab Res Rev. 1999;15:314–22.
Rasmussen MH, Juul A, Kjems LL, Hilsted J. Effects of short-term caloric restriction on circulating free IGF-I, acid-labile subunit, IGF-binding proteins (IGFBPs)-1-4, and IGFBPs-1-3 protease activity in obese subjects. Eur J Endocrinol. 2006;155(4):575–81.
Frystyk J, Brick DJ, Gerweck AV, Utz AL, Miller KK. Bioactive insulin-liike growth factor-1 in obesity. J Clin Endocrinol Metab. 2009;94:3093–7.
Elis S, Wu Y, Courtland HW, Cannata D, Sun H, Beth-On M, Liu C, Jasper H, Domené H, Karabatas L, Guida C, Basta-Pljakic J, Cardoso L, Rosen CJ, Frystyk J, Yakar S. Unbound (bioavailable) IGF1 enhances somatic growth. Dis Model Mech. 2011;4(5):649–58.
Rajkumar K, Modric T, Murphy LJ. Impaired adipogenesis in insulin-like growth factor binding protein-1 transgenic mice. J Endocrinol. 1999;162(3):457–65.
Wheatcroft SB, Kearney MT, Shah AM, Ezzat VA, Miell JR, Modo M, Williams SC, Cawthorn WP, Medina-Gomez G, Vidal-Puig A, Sethi JK, Crossey PA. IGF-binding protein-2 protects against the development of obesity and insulin resistance. Diabetes. 2007;56(2):285–94.
Cirmanova V, Bayer M, Starka L, Zajickova K. The effect of leptin on bone: an evolving concept of action. Physiol Res. 2008;57(Suppl 1):S143–51.
Steppan CM, Crawford DT, Chidsey-Frink KL, Ke H, Swick AG. Leptin is a potent stimulator of bone growth in ob/ob mice. Regul Pept. 2000;92:73–8.
Maor G, Rochwerger M, Segev Y, Phillip M. Leptin acts as a growth factor on the chondrocytes of skeletal growth centers. J Bone Miner Res. 2002;17:1034–43.
Montague CT, Farooqi IS, Whitehead JP, Soos MA, Rau H, Wareham NJ, Sewter CP, Digby JE, Mohammed SN, Hurst JA, Cheetham CH, Earley AR, Barnett AH, Prins JB, O’Rahilly S. Congenital leptin deficiency is associated with severe early-onset obesity in humans. Nature. 1997;387(6636):903–8.
Farooqi IS, Wangensteen T, Collins S, Kimber W, Matarese G, Keogh JM, Lank E, Bottomley B, Lopez-Fernandez J, Ferraz-Amaro I, Dattani MT, Ercan O, Myhre AG, Retterstol L, Stanhope R, Edge JA, McKenzie S, Lessan N, Ghodsi M, De Rosa V, Perna F, Fontana S, Barroso I, Undlien DE, O’Rahilly S. Clinical and molecular genetic spectrum of congenital deficiency of the leptin receptor. N Engl J Med. 2007;356(3):237–47.
Taylor PN, Richmond R, Davies N, Sayers A, Stevenson K, Woltersdorf W, Taylor A, Groom A, Northstone K, Ring S, Okosieme O, Rees A, Nitsch D, Williams GR, Smith GD, Gregory JW, Timpson NJ, Tobias JH, Dayan CM. Paradoxical relationship between body mass index and thyroid hormone levels: a study using mendelian randomization. J Clin Endocrinol Metab. 2016;101(2):730–8.
Santini F, Marzullo P, Rotondi M, Ceccarini G, Pagano L, Ippolito S, Chiovato L, Biondi B. Mechanisms in endocrinology: the crosstalk between thyroid gland and adipose tissue: signal integration in health and disease. Eur J Endocrinol. 2014;171(4):R137–52.
Lombardi A, Moreno M, de Lange P, Iossa S, Busiello RA, Goglia F. Regulation of skeletal muscle mitochondrial activity by thyroid hormones: focus on the “old” triiodothyronine and the “emerging” 3,5-diiodothyronine. Front Physiol. 2015;6:237.
Feldt-Rasmussen U. Thyroid and leptin. Thyroid. 2007;17(5):413–9.
Hollenberg AN. The role of the thyrotropin-releasing hormone (TRH) neuron as a metabolic sensor. Thyroid. 2008;18:131–8.
Ortega FJ, Jílková ZM, Moreno-Navarrete JM, Pavelka S, Rodriguez-Hermosa JI, Kopeck Ygrave J, Fernández-Real JM. Type I iodothyronine 5′-deiodinase mRNA and activity is increased in adipose tissue of obese subjects. Int J Obes. 2012;36(2):320–4.
Boelen A, van Beeren M, Vos X, Surovtseva O, Belegri E, Saaltink DJ, Vreugdenhil E, Kalsbeek A, Kwakkel J, Fliers E. Leptin administration restores the fasting-induced increase of hepatic type 3 deiodinase expression in mice. Thyroid. 2012;22(2):192–9.
Lee JM, Appugliese D, Kaciroti N, Corwyn RF, Bradley RH, Lumeng JC. Weight status in young girls and the onset of puberty. Pediatrics. 2007;119:e624–30.
Roelfsema F, Kok P, Veldhuis JD, Pijl H. Altered multihormone synchrony in obese patients with polycystic ovary syndrome. Metabolism. 2011;60(9):1227–33.
Witchel SF, Tena-Sempere M. The Kiss1 system and polycystic ovary syndrome: lessons from physiology and putative pathophysiologic implications. Fertil Steril. 2013;100(1):12–22.
Sam S, Dunaif A. Polycystic ovary syndrome: syndrome XX? Trends Endocrinol Metab. 2003;14:365–70.
Chang RJ. The reproductive phenotype in polycystic ovary syndrome. Nat Clin Pract Endocrinol Metab. 2007;3(10):688–95.
Freemark M. Management of adolescents with polycystic ovary syndrome. J Clin Endocrinol Metab. 2011;96(11):3354–6.
Mogri M, Dhindsa S, Quattrin T, Ghanim H, Dandona P. Testosterone concentrations in young pubertal and post-pubertal obese males. Clin Endocrinol. 2013;78(4):593–9.
Kelly DM, Jones TH. Testosterone and obesity. Obes Rev. 2015;16(7):581–606.
Oury F, Sumara G, Sumara O, Ferron M, Chang H, Smith CE, Hermo L, Suarez S, Roth BL, Ducy P, Karsenty G. Endocrine regulation of male fertility by the skeleton. Cell. 2011;144(5):796–809.
Chirico V, Cannavò S, Lacquaniti A, Salpietro V, Mandolfino M, Romeo PD, Cotta O, Munafò C, Giorgianni G, Salpietro C, Arrigo T. Prolactin in obese children: a bridge between inflammation and metabolic-endocrine dysfunction. Clin Endocrinol. 2013;79(4):537–44.
Colao A, Sarno AD, Cappabianca P, Briganti F, Pivonello R, Somma CD, Faggiano A, Biondi B, Lombardi G. Gender differences in the prevalence, clinical features and response to cabergoline in hyperprolactinemia. Eur J Endocrinol. 2003;148(3):325–31.
Gillam MP, Molitch ME, Lombardi G, Colao A. Advances in the treatment of prolactinomas. Endocr Rev. 2006;27:485–534.
Nanbu-Wakao R, Fujitani Y, Masuho Y, Muramatu M, Wakao H. Prolactin enhances CCAAT enhancer-binding protein-beta (C/EBP beta) and peroxisome proliferator-activated receptor gamma (PPAR gamma) messenger RNA expression and stimulates adipogenic conversion of NIH-3T3 cells. Mol Endocrinol. 2000;14(2):307–16.
Fleenor D, Arumugam R, Freemark M. Growth hormone and prolactin receptors in adipogenesis: STAT-5 activation, suppressors of cytokine signaling, and regulation of insulin-like growth factor I. Horm Res. 2006;66(3):101–10.
Ben-Jonathan N, Hugo E. Prolactin (PRL) in adipose tissue: regulation and functions. Adv Exp Med Biol. 2015;846:1–35.
Perez Millan MI, Luque Guillermina M, Ramirez MC, Noain D, Ornstein AM, Rubinstein M, Becu-Villalobos D. Selective disruption of dopamine D2 receptors in pituitary lactotropes 2 increases body weight and adiposity in female mice. Endocrinology. 2014;155:829–39.
García MC, López M, Gualillo O, Seoane LM, Diéguez C, Señarís RM. Hypothalamic levels of NPY, MCH, and prepro-orexin mRNA during pregnancy and lactation in the rat: role of prolactin. FASEB J. 2003;17:1392–400.
Augustine RA, Grattan DR. Induction of central leptin resistance in hyperphagic pseudopregnant rats by chronic prolactin infusion. Endocrinology. 2008;149(3):1049–55.
Nagaishi VS, Cardinali LI, Zampieri TT, Furigo IC, Metzger M, Donato J Jr. Possible crosstalk between leptin and prolactin during pregnancy. Neuroscience. 2014;259:71–83.
Sonigo C, Bouilly J, Carré N, Tolle V, Caraty A, Tello J, Simony-Conesa FJ, Millar R, Young J, Binart N. Hyperprolactinemia-induced ovarian acyclicity is reversed by kisspeptin administration. J Clin Invest. 2012;122(10):3791–5.
Artz E, Haqq A, Freemark M. Hormonal and metabolic consequences of childhood obesity. Endocrinol Metab Clin N Am. 2005;34(3):643–58.
Lee MJ, Pramyothin P, Karastergiou K, Fried SK. Deconstructing the roles of glucocorticoids in adipose tissue biology and the development of central obesity. Biochim Biophys Acta. 2014;1842(3):473–81.
Wake DJ, Rask E, Livingstone DEW, Soderberg S, Olsson T, Walker BR. Local and systemic impact of transcriptional up-regulation of 11β-hydroxysteroid dehydrogenase type 1 in adipose tissue in human obesity. J Clin Endocrinol Metab. 2003;88(8):3983.
Tomlinson JW, Moore JS, Clark PM, Holder G, Shakespeare L, Stewart PM. Weight loss increases 11β-hydroxysteroid dehydrogenase type 1 expression in human adipose tissue. J Clin Endocrinol Metab. 2004;89:2711–6.
Ashraf A, Alvarez J, Saenz K, Gower B, McCormick K, Franklin F. Threshold for effects of vitamin D deficiency on glucose metabolism in obese female African-American adolescents. J Clin Endocrinol Metab. 2009;94:3200–6.
Alemzadeh R, Kichler J, Babar G, Calhoun M. Hypovitaminosis D in obese children and adolescents: relationship with adiposity, insulin sensitivity, ethnicity, and season. Metabolism. 2008;57:183–91.
Lenders CM, Feldman HA, Von Scheven E, et al. Relation of body fat indexes to vitamin D status and deficiency among obese adolescents. Am J Clin Nutr. 2009;90:459–67.
Wortsman J, Matsuoka LY, Chen TC, Lu Z, Holick MF. Decreased bioavailability of vitamin D in obesity. Am J Clin Nutr. 2000;72(3):690–3.
Miraglia del Giudice E, Grandone A, Cirillo G, Capristo C, Marzuillo P, Di Sessa A, Umano GR, Ruggiero L, Perrone L. Bioavailable vitamin D in obese children: the role of insulin resistance. J Clin Endocrinol Metab. 2015;100(10):3949–55.
Powe CE, Evans MK, Wenger J, Zonderman AB, Berg AH, Nalls M, Tamez H, Zhang D, Bhan I, Karumanchi SA, Powe NR, Thadhani R. Vitamin D-binding protein and vitamin D status of black Americans and white Americans. N Engl J Med. 2013;369(21):1991–2000.
Ashraf AP, Huisingh C, Alvarez JA, Wang X, Gower BA. Insulin resistance indices are inversely associated with vitamin D binding protein concentrations. J Clin Endocrinol Metab. 2014;99(1):178–83.
Jamka M, Woźniewicz M, Jeszka J, Mardas M, Bogdański P, Stelmach-Mardas M. The effect of vitamin D supplementation on insulin and glucose metabolism in overweight and obese individuals: systematic review with meta-analysis. Sci Rep. 2015;5:16142.
Chandler PD, Wang L, Zhang X, Sesso HD, Moorthy MV, Obi O, Lewis J, Prince RL, Danik JS, Manson JE, LeBoff MS, Song Y. Effect of vitamin D supplementation alone or with calcium on adiposity measures: a systematic review and meta-analysis of randomized controlled trials. Nutr Rev. 2015;73(9):577–93.
Pathak K, Soares MJ, Calton EK, Zhao Y, Hallett J. Vitamin D supplementation and body weight status: a systematic review and meta-analysis of randomized controlled trials. Obes Rev. 2014;15(6):528–37.
Greco EA, Lenzi A, Migliaccio S. The obesity of bone. Ther Adv Endocrinol Metab. 2015;6(6):273–86.
Pollock NK. Childhood obesity, bone development, and cardiometabolic risk factors. Mol Cell Endocrinol. 2015;410:52–63.
Pollock NK, Bernard PJ, Wenger K, Misra S, Gower BA, Allison JD, Zhu H, Davis CL. Lower bone mass in prepubertal overweight children with prediabetes. J Bone Miner Res. 2010;25(12):2760–9.
Kessler J, Koebnick C, Smith N, Adams A. Childhood obesity is associated with increased risk of most lower extremity fractures. Clin Orthop Relat Res. 2013;471(4):1199–207.
Sabhaney V, Boutis K, Yang G, Barra L, Tripathi R, Tran TT, Doan Q. Bone fractures in children: is there an association with obesity? J Pediatr. 2014;165(2):313–8.
Ionova-Martin SS, Do SH, Barth HD, et al. Reduced size-independent mechanical properties of cortical bone in high fat diet-induced obesity. Bone. 2010;46(1):217–25.
Zeyda M, Gollinger K, Todoric J, Kiefer FW, Keck M, Aszmann O, Prager G, Zlabinger GJ, Petzelbauer P, Stulnig TM. Osteopontin is an activator of human adipose tissue macrophages and directly affects adipocyte function. Endocrinology. 2011;152(6):2219–27.
Aouadi M, Tencerova M, Vangala P, Yawe JC, Nicoloro SM, Amano SU, Cohen JL, Czech MP. Gene silencing in adipose tissue macrophages regulates whole-body metabolism in obese mice. Proc Natl Acad Sci U S A. 2013;110(20):8278–83.
Kahles F, Findeisen HM, Bruemmer D. Osteopontin: a novel regulator at the cross roads of inflammation, obesity and diabetes. Mol Metab. 2014;3(4):384–93.
Nomiyama T, Perez-Tilve D, Ogawa D, Gizard F, Zhao Y, Heywood EB, Jones KL, Kawamori R, Cassis LA, Tschöp MH, Bruemmer D. Osteopontin mediates obesity-induced adipose tissue macrophage infiltration and insulin resistance in mice. J Clin Invest. 2007;117(10):2877–88.
Gómez-Ambrosi J, Catalán V, Ramírez B, Rodríguez A, Colina I, Silva C, Rotellar F, Mugueta C, Gil MJ, Cienfuegos JA, Salvador J, Frühbeck G. Plasma osteopontin levels and expression in adipose tissue are increased in obesity. J Clin Endocrinol Metab. 2007;92(9):3719–27.
Schreier M, Schwartze JT, Landgraf K, Scheuermann K, Erbs S, Herberth G, Pospisilik JA, Kratzsch J, Kiess W, Körner A. Osteopontin is BMI-independently related to early endothelial dysfunction in children. J Clin Endocrinol Metab. 2016;101(11):4161–9.
Boucher-Berry C, Speiser PW, Carey DE, Shelov SP, Accacha S, Fennoy I, Rapaport R, Espinal Y, Rosenbaum M. Vitamin D, osteocalcin, and risk for adiposity as comorbidities in middle school children. J Bone Miner Res. 2012;27(2):283–93.
Reinehr T, Roth CL. A new link between skeleton, obesity and insulin resistance: relationships between osteocalcin, leptin and insulin resistance in obese children before and after weight loss. Int J Obes. 2010;34(5):852–8.
Lenders CM, Lee PD, Feldman HA, Wilson DM, Abrams SH, Gitelman SE, Klish WJ, Wertz MS, Taylor GA, Alongi RT, Chen TC, Holick MF, Elisabeth Glaser Pediatric Research Network Obesity Study Group. A cross-sectional study of osteocalcin and body fat measures among obese adolescents. Obesity (Silver Spring). 2013;21(4):808–14.
Ferron M, Lacombe J. Regulation of energy metabolism by the skeleton: osteocalcin and beyond. Arch Biochem Biophys. 2014;561:137–46.
Lee NK, Sowa H, Hinoi E, Ferron M, Ahn JD, Confavreux C, Dacquin R, Mee PJ, McKee MD, Jung DY, Zhang Z, Kim JK, Mauvais-Jarvis F, Ducy P, Karsenty G. Endocrine regulation of energy metabolism by the skeleton. Cell. 2007;130:456–69.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG
About this chapter
Cite this chapter
Freemark, M. (2018). Obesity and the Endocrine System, Part II: The Effects of Childhood Obesity on Growth and Bone Maturation, Thyroid and Adrenal Function, Sexual Development, and Bone Mineralization. In: Freemark, M. (eds) Pediatric Obesity. Contemporary Endocrinology. Humana Press, Cham. https://doi.org/10.1007/978-3-319-68192-4_20
Download citation
DOI: https://doi.org/10.1007/978-3-319-68192-4_20
Published:
Publisher Name: Humana Press, Cham
Print ISBN: 978-3-319-68191-7
Online ISBN: 978-3-319-68192-4
eBook Packages: MedicineMedicine (R0)