Abstract
The health-care and patient care outcomes for poly chronic conditions can be improved through the integration of multiple domains of the population health management approach and comprehensive coordination across multiple levels utilizing interdisciplinary care teams and appropriate applications of health information technology. Patient identification and risk stratification enable health-care providers to focus the appropriate resources on the patients with the greatest needs. By preventing acute events and worsening health status in higher-risk patients and providing preventative and wellness services for lower-risk patients, care management efforts can achieve optimal impact on health outcomes and cost-effectiveness. This chapter highlights the need for integrating contextual (macrolevel) and individual personalized care (microlevel) approaches to population health in solving multimorbidities.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
The challenges and inefficiencies stemming from the fragmentation and lack of coordination in the complex US health-care system are well documented. For patients with poly chronic conditions , the inadequacies of the health-care system are particularly problematic given the distinct needs and characteristics of these patients, as well the high service utilization patterns and costs associated with their care. Integration and coordination of care are fundamental in an improved health-care delivery system that functions to reach targeted populations, provide them with quality care , and reduce costs. Identifying the care and treatment patterns associated with higher risks and costs, and developing strategies and interventions to improve the health outcomes for these patients, requires the involvement of patients, caregivers, providers, community entities, and other stakeholders.
The term “care coordination” has been defined numerous ways. The Agency for Health Research and Quality (AHRQ) notes that it is important to consider care coordination from the perspective of the patient/family, health-care professionals, and system representatives, as these groups may have differing views. Defined broadly, care coordination is “the deliberate organization of patient care activities between two or more participants (including the patient) involved in a patient’s care to facilitate the appropriate delivery of health care services. Organizing care involves the marshaling of personnel and other resources needed to carry out all required patient care activities, and is often managed by the exchange of information among participants responsible for different aspects of care” (McDonald et al. 2014, p. 6). Lack of integration can result in patients with poly chronic conditions having unmet health-care needs, not receiving appropriate and/or high-quality care , and utilizing health services that could have been avoided, such as emergency room visits and hospital readmissions. Each year, Medicare beneficiaries see an average of two primary care practitioners and five specialists, and primary care practices consisting of 30% of Medicare patients with multiple chronic conditions (four or more) need to coordinate with 86 other providers in 36 practices (Tinetti et al. 2016). As the population health management (PHM) approach provides the opportunity to improve accessibility , quality, outcomes, and spending through the identification of groups of patients based on similar characteristics, it is important to understand the various elements involved with its implementation.
Recognizing the multiple domains or principles of the PHM approach and the ways in which components integrate is particularly important for the care of patients with poly chronic conditions , given the complexities of this population. In order to reach and care for patients with poly chronic conditions who would benefit from better coordinated care involving health services and social services, it is necessary to consider contextual aspects for identification and assessment of patient populations and the resources needed to care for them, as well as individual aspects for patient-centered care. Contextual elements pertain to population attributes, organizational structures of communities and health-care systems, and the geographic area. Individual personalized care elements include patient-centered needs across the health continuum and targeted interventions to effectively and efficiently address such needs. Technology is a critical component across all elements of the PHM approach. Meaningful and appropriate use of health information and enhanced communication with patients, providers, and other stakeholders help to facilitate actions and activities in the contextual and patient-centered domains, as well as impact evaluation and improvement components of the process.
Understanding how certain chronic conditions cluster based on clinical, financial, or social attributes and identifying homogeneous subgroups in the complex population of patients with multiple chronic conditions are important to integrating care effectively and efficiently. Patients, caregivers, providers, health plans, and other stakeholders can better transition from the traditional condition-based approach to a patient-centered approach by using information regarding these clusters and the ways in which chronic conditions group into common pairs or sets. Furthermore, identifying patterns in high-risk, high-cost patients with multiple chronic illnesses enhances the ability to predict vital patient characteristics, such as patients who are most likely to show significantly improved outcomes, have high future costs, and respond best to care management interventions (Kronick et al. 2007, pp. 35–37). A more precise depiction of the characteristics, variabilities, and potential challenges surrounding patients with multiple chronic conditions then makes it possible to develop and implement targeted interventions at multiple levels for these patients.
1 Contextual Domains or Ecological Parameters: Macrolevel Factors Influencing Population Health
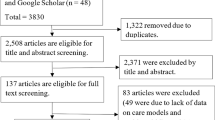
The process of employing PHM strategies requires efforts to address contextual and ecological components to ensure an adequate understanding of the population attributes and accessibility of resources. The ecological parameters, which Otis Duncan called an ecological complex, include population (P), organization (O), environment (E), and technology (T). Population health is influenced by the dynamic interplay of POET components. The POET model is shown in Fig. 3.1 (Wan 2014).
1.1 Population Identification, Risk Assessment , and Segmentation : The First Parameter
The first parameter (P) involves identification, assessment, and segmentation of the patient population health status and risk stratification to determine the specific population needs and the availability of resources required to provide care. Steps taken to identify meaningful population subgroups, classified by demographic, social, and economic characteristics of the population, and ascertain the level of care needed for patients enable health-care providers to recognize gaps in the delivery system and develop appropriate, patient-centered interventions that are tailored to individual needs and communities.
The prevalence of poly chronic conditions and utilization of health services by patients who have them may vary due to social, demographic, or geographic factors. Variations in the prevalence of multiple chronic conditions among Medicare beneficiaries have been shown to be associated with certain demographic factors, including age, gender, and race /ethnicity . Based on an analysis of administrative claims data for 2010, multiple chronic conditions were more prevalent as age increased and in the population of beneficiaries dually eligible for Medicaid and Medicare . Across all age groups, the prevalence of two or more and four or more chronic conditions was higher in women, particularly non-Hispanic black and Hispanic women. Analysis of men age 65 or older showed greater prevalence of multiple chronic conditions in non-Hispanic whites ; however, the rate of four or more chronic conditions was higher in non-Hispanic black men (Lochner and Cox 2013).
Patterns have been identified in the ways in which conditions group into pairs (dyads) or sets (triads) of diagnoses in populations of patients with multiple chronic conditions . Analyses of disabled Medicaid patients identified several specific conditions prevalent in dyads or triads among the 5% of highest-cost beneficiaries, including cardiovascular disease, central nervous system disorders, psychiatric illness, and pulmonary disease (Kronick et al. 2009, p. 12). Additionally, correlations between certain conditions have been identified, with the highest correlation being between diabetes and cardiovascular disease, followed by cardiovascular disease with pulmonary disease, skeletal and connective disease, and gastrointestinal disease (Kronick et al. 2007, p. 27).
While information concerning the grouping of diseases in population subsets is useful for identifying those considered to be high risk and determining the level of care needed, factors that are not disease specific must also be considered. The accessibility and coordination of health care for patients with multiple chronic conditions becomes even more challenging when there are social barriers (Miller et al. 2013, p. S17). Thus, a comprehensive assessment of the population health and risk stratification (segmentation ) to group patients according to the type of care required entail incorporating information pertaining to the setting and societal characteristics. An analytical technique, such as predictor tree analysis or automatic interaction detector analysis (Wan 2002), could be used to identify relatively homogeneous subgroups of the population at risk so that subgroup-specific interventions could be implemented and evaluated.
1.2 Organizational Resource Identification and Allocation : The Second Parameter
The second parameter refers to organizational capacity and resource availability for achieving optimal health. PHM efforts are influenced by factors such as the availability of resources, the presence of collaborations and partnerships , and other characteristics of the health-care delivery system. These area-level factors can have an impact on patients with poly chronic conditions . For example, patterns of state-level variations have been identified in prevalence, health services utilization, and spending among Medicare patients with six or more chronic conditions. In 2011, states in the Northeast and South regions of the United States had a higher prevalence of Medicare beneficiaries with six or more chronic conditions, with prevalence approximately 30% higher than the national average in Florida and New Jersey. In Washington, D.C., hospital readmissions, emergency room visits, and Medicare spending were found to be at least 15% higher than the national average. While additional research is needed to determine the specific factors influencing such patterns, the supply of health-care resources has been associated with observed regional variations in care given that the likelihood of conditions being identified can increase when the availability of health-care resources is greater. Therefore, state-level variability in the prevalence of poly chronic conditions among Medicare beneficiaries may be partially associated with the state health-care resources (Lochner et al. 2013, pp. E13–E15).
Community coalitions may form in response to challenges, opportunities, or threats identified by local stakeholders. The coordination of efforts by community partners has the potential to bring about meaningful changes; however, there is still the possibility for overlap of programs and services if there is no mechanism for individual coalitions formed around specific health issues to streamline efforts across multiple health issues and segments of the community (Janosky et al. 2013, p. 247). The availability and strength of these types of partnerships have the potential to greatly impact patients with poly chronic conditions by ensuring that the necessary health services and social services are accessible.
The risk stratification process assists health-care providers in focusing the appropriate resources on patient population groups with the greatest need (Care Continuum Alliance 2012, p. 10). Understanding the level of care that patients require and the types of providers that will be needed to serve these patients can help health service delivery and resource use be more targeted and efficient. Communication and a shared approach across community collaborators can facilitate greater consistency in comprehensively addressing health issues and, thus, improve impact and resource use (Janosky et al. 2013, p. 247). Actions and activities undertaken in the contextual domains of the PHM approach inform the development of the appropriate interventions to manage care in a coordinated, patient-centered fashion. The scarcity of resources may trigger the need to prioritize or segment resources to target the services for those who will most likely benefit from the program or intervention .
1.3 Environment or Geographical Milieu: The Third Parameter
The third parameter pertains to environmental or geographic factors that could potentially impact population health. Unique characteristics of the physical space can provide a better understanding of the distribution of health needs and possible threats to health and well-being. This is a highly important part of the PHM approach for patients with poly chronic conditions given the complex health and care needs of these individuals and the lack of research that has generated comprehensive knowledge concerning optimal treatments and practices. By assessing the geospatial clustering of health needs and factors that may hinder healthy environments, efforts can become more focused in the development of targeted interventions for individuals with poly chronic conditions .
According to Rocca et al. (2014), “the characterization of multimorbidity patterns in a geographically defined population allows comparisons with other localized populations in the United States or worldwide to investigate geographic similarities or differences. In addition, these findings can be used to guide decisions for clinical practice or public health in the local community” (p. 1337). Analysis of state-level variations across the United States using 2011 Medicare administrative data reported differences in the prevalence and utilization of health services in patients with multiple chronic conditions . Analysis also highlighted the need for future research in order to understand the specific factors associated with the patterns of state differences, such as variances in the distributions of underlying risk factors , combinations and types of conditions, and the quantity and delivery of available health-care resources (Lochner et al. 2013, pp. E14–E15).
Geospatial methodologies have been used to assess local-level distributions of multiple chronic conditions . A single-state analysis uncovered spatially distinct areas in which the prevalence of combinations of multiple chronic conditions was considered to be high in comparison to what would be expected given the frequencies of these conditions in the total state population. To better understand the factors contributing to the differential patterns of spatial association, it is suggested that future research explore the role of individual behaviors such as smoking, occupational exposures such as to particulates, and environmental conditions such as air quality and proximity to major highways (Cromley et al. 2016, pp. 18–21). Thus, examination of smaller area variations in the prevalence of specific multiple chronic conditions allows for incorporation of information concerning community resources, cultural differences, industrial impact, and other environmental characteristics that may influence health behaviors, status, or care delivery.
Environmental hazards such as pollution may play a role when considering health and health care for poly chronic conditions . A longitudinal analysis of the impact of air quality on health among patients with chronic conditions reported increased use of health services with higher levels of exposure to air pollution (To et al. 2015, p. 1). Although various environmental pollutants may contribute to chronic disease and adverse outcomes, the relationships between chemical exposures and health are diverse and complicated. In a review of environmental determinants of chronic disease and medical approaches, Sears and Genuis (2012) concluded that “addressing environmental health and contributors to chronic disease has broad implications for society, with large potential benefits from improved health and productivity,” with risk recognition, chemical assessment, exposure reduction, remediation, monitoring, and avoidance identified as possible public health initiatives (Sears and Genuis 2012, pp. 1–2).
While additional research is needed to elucidate many of the causal factors impacting the patterns and variabilities in environmental and geographic components of the PHM approach, the opportunity remains for health-care providers to consider existing empirical evidence and the available information from individual patients when developing patient-centered interventions for poly chronic conditions . An awareness of the distinct environmental and geographic characteristics of the physical space in which patients with poly chronic conditions live and/or receive care can be a vital step in ensuring that interventions entail the appropriate types of care, care providers, and other resources to account for health needs and possible threats to health and well-being.
1.4 Technological Innovation and Use: The Fourth Parameter
The contextual domains of the PHM approach are heavily impacted by technology. The availability of information and the ability for data from multiple sources to be combined and analyzed in a meaningful way are critical components for patient assessment (Care Continuum Alliance 2012, p. 10). Patient data can be used to assess health status, progress, service utilization, and delivery system gaps or deficiencies. Predictive analyses using current patient medical information provide an opportunity to improve the coordination of treatment, costs, and inefficiencies (Miller et al. 2013, p. S18). The use of predictive modeling enables health-care providers to identify patients who are likely to become high risk in the future and intervene in ways to prevent these individuals from having an acute event and to maintain their health (Healthcare Informatics 2016, p. 8). Thus, the availability of useful patient health information and innovative technological resources provide the opportunity for a better understanding of the population health status and those who have the greatest need for care.
Variations in the availability and sophistication of technology resources influence the ways in which PHM components are delivered. Rural areas, for example, may implement PHM differently due to limited technological capabilities (Care Continuum Alliance 2012, p. 13). Furthermore, without appropriate health information technology tools, health-care providers that do have the capacity to identify patients with the highest level of need or gaps in care still may be limited in their ability to serve these patients. To be more effective, information technology solutions need to facilitate adequate planning for the staff resources and scheduling opportunities available to care for patients (Healthcare Informatics 2016, p. 11). Distinct contextual characteristics and resources play an influential role when considering health information technology strategies to achieve patient care objectives.
The influence of factors associated with local setting when implementing health information technology programs is highlighted in the reported experiences of communities participating in the Beacon Community Cooperative Agreement Program. This program was created by the Office of the National Coordinator for Health Information Technology following the Health Information Technology for Economic and Clinical Health (HITECH) Act of 2010 to help communities build and strengthen their health information technology infrastructure. Due to variations associated with factors pertaining to the local context across these communities, their strategies for utilizing health information technology to support care management programs differed. However, three specific steps were identified as fundamental components for the design of these programs: (1) community needs assessment, (2) engagement of local and regional partners, and (3) assessment of available resources and infrastructure (Allen et al. 2014, pp. 150–152).
2 Individual Personalized Care Domains: Microlevel Factors Influencing Population Health
Individual personalized care elements are key components in the process of PHM. The most appropriate and effective methods to engage and communicate with patients can vary based on personal preferences, capabilities, resource availability, and level of need. Variations in the level of need for patients with poly chronic conditions may be rather complicated given that multiple illnesses must be considered in complex disease management efforts as well as lower-risk efforts such as prevention and wellness. The development of patient-centered interventions entails selecting delivery methods and treatment programs that are tailored to individuals’ needs across the health continuum. Ideally, information obtained by health-care providers’ contextual domain activities will facilitate meaningful conversations with patients. By integrating these domains, clinicians can better understand patients’ circumstances and preferences and develop care plans that will be more effective in attaining improved outcomes and costs.
2.1 Engagement and Communication
Patients must be involved and informed throughout the process of care delivery. Engagement has been described as “a psychological state which manifests in positive behavior change” and consists of “self-determined participation in intervention -directed activities in alignment with patient goals to which the patient is dedicated” (Care Continuum Alliance 2012, p. 21). Patient health is influenced by patients, their caregivers, and providers in the health system, with the patient being the most influential of these factors. Healthy behaviors and adherence to care plans, such as medication compliance among patients with poly chronic conditions , can be improved by effectively engaging patients. These improvements, in turn, lead to increased quality and reduced costs (Proctor et al. 2016, p. 13). Thus, patient engagement is a critical component of the PHM approach.
Increased communication with patients and the incorporation of their input into care plans can lead to increased treatment adherence, greater patient satisfaction , and improved outcomes. Seeking to develop patient priority-directed care, an advisory group composed of patients, caregivers, clinicians, health information technology experts, health system leaders, and other stakeholders elected to address three potentially modifiable factors contributing to fragmentation, burdensome care, and poor outcomes for older adults with multiple chronic conditions . These included (1) focus on diseases not patients for decision-making and care; (2) lack of clearly defined roles, responsibilities, and accountability among clinicians; and (3) insufficient attention to the health outcome goals and care preferences that matter most to patients and caregivers. A proposed strategy for addressing these factors was for the care of all clinicians to be aligned around the same outcome based on the individualized goals and preferences of patients (Tinetti et al. 2016, pp. 263–264).
Self-management support has been defined as “the systematic provision of education and supportive interventions by health care staff to increase patients’ skills and confidence in managing their health problems, including regular assessment of progress and problems, goal setting, and problem-solving support” (Suter et al. 2011, p. 88). Activities to support self-management goals in order to achieve coordinated care involve education and support for patients and their caregivers through information, training, or coaching that is tailored to patient preferences and capacity and facilitates patient capabilities for self-care to encourage improvements in behavior change, navigation of care transitions, and self-efficacy (AHRQ 2014, p. 24).
The role of families and other caregivers involved with the management of patients with poly chronic conditions must be carefully considered. The ability to perform self-care, which is critical for managing risk factors associated with declining health or the development of additional chronic conditions , may be limited among patients who are severely ill due to the existence of multiple chronic conditions (HHS 2010, p. 9). Patients living with chronic conditions must have confidence in their abilities to perform the tasks needed to live well. Self-efficacy is an important precondition for behavioral change, as individuals who believe in their ability to carry out tasks that will facilitate desired outcomes are driven to adopt the necessary behaviors. Thus, confidence in one’s ability to perform certain behaviors influences actual behaviors (Suter et al. 2011, pp. 88–89). While person-centered care that empowers patients in care management is an important element for successful care coordination (HHS 2010, p. 7), engaging patients’ family members and immediate caregivers in the process of designing and delivering care management plans may be a fundamental component of effective interventions for patients with poly chronic conditions .
2.2 Patient-Centered Interventions
For some patients with poly chronic conditions , the existing disease guidelines may not be applicable, as randomized clinical trials often exclude older adults with complex conditions. Given the lack of evidence, the benefits of the treatments these patients are receiving may be unclear (Tinetti et al. 2016, p. 262). The US Department of Health and Human Services has outlined several strategies to address the need for guidelines that account for multiple chronic conditions. These strategies include guideline developers adding information pertaining to common comorbidity clusters with a chronic condition, risk factor management to prevent additional conditions, and ensuring that chronic disease guideline repositories support the promotion of guidelines that include information on patients with multiple chronic conditions (HHS 2010, p. 13). The lack of guidelines based on empirical evidence makes it even more important for health-care providers to communicate with patients to comprehensively understand their treatment needs and preferences, as the information derived from such interactions can be critical for determining the most effective interventions .
It has been reported that only 10–12 percent of overall health is determined by health-care services and treatments, while behavioral and socioeconomic factors account for approximately 57% (Proctor et al. 2016, p. 5). To improve the health of patients with poly chronic conditions , there must be increased coordination of complex medical and longitudinal psychosocial care, with patients having access to community and other public health services, in addition to better coordination of medical care (HHS 2010, p. 6). Thus, it is crucial that care plans for patients with poly chronic conditions are developed with consideration for unique patient needs beyond medical care, as the multitude of various types of support services can have a profound impact on health status and outcomes.
Furthermore, there is an increased likelihood of reaching goals aimed at engaging patients and supporting self-management for improved health outcomes when intervention modalities are matched to patient preferences. In-person visits may be most appropriate for some patients, while others would prefer information and education delivered online or through the mail (Care Continuum Alliance 2012, pp. 10–11). Along with patient preference, risk level must also be considered, particularly among patients with poly chronic conditions , given the complexity of medical problems that are likely to exist. Identifying the health and needs of populations and utilizing resources to intervene appropriately can improve outcomes and costs. For example, hospital readmission rates among Medicare beneficiaries have been shown to increase in direct relation to the number of chronic conditions a patient has (Lochner et al. 2013, p. E8). Among patients with multiple chronic conditions , the inclusion of an in-person home visit by a nurse case manager to the transitional care management following hospital discharge has been shown to significantly reduce readmissions and lower the total costs of care (Jackson et al. 2016, p. 167).
A 2017 data brief published by the US Centers for Disease Control and Prevention National Center for Health Statistics reported that an increasing number of individuals with two or more chronic conditions had experienced barriers to health care. From 2012 to 2015, the percentage of patients aged 65 or older who delayed or did not obtain needed medical care for any reason in the past 12 months increased from 13.5% to 15%. Among patients aged 18–64, the percentage of those who delayed needed medical care due only to a non-cost reason increased from 12.4% in 2012 to 14.6% in 2015. Non-cost reasons include factors such as lack of transportation, inability to reach providers through the telephone or obtain an appointment soon enough, or health-care provider offices not being open during times that the patients were able to get there (Ward 2017, pp. 5–6). The implications of disparities in access to necessary medical care, social services, and other community resources can be even more severe for patients with poly chronic conditions given the complexity of their health status and needs and the importance of trying to maintain or reduce the risk level of these individuals by preventing new conditions from developing and mitigating the adverse effects of existing conditions.
Understanding the unique needs and circumstances of individuals is fundamental to ensuring that patient-centered interventions are tailored to address the types of care and appropriate service providers required. Through increased coordination and integration of medical and social services to provide patient-centered interventions for individuals with poly chronic conditions , the utilization of unnecessary or avoidable services can be reduced, and barriers to needed care can be alleviated. There are obvious challenges concerning communication and coordination across multiple medical care providers and others involved with the care for patients with poly chronic conditions . However, the PHM approach and adoption of innovative health information technology provide the opportunity to overcome such challenges and offer tangible improvements in the effectiveness and efficiency of health care and outcomes.
2.3 Technology Adoption and Use Behavior
Complex medical problems can be monitored and assessed through the use of technology for chronic disease management. Coordination of care can be improved through the integration of communication across institutions and organizations by utilizing health information technology . For patients with chronic conditions , problems occurring during care transitions, in long-term care management, and when acute intervention is needed for clinical episodes could be alleviated. Yet still, health-care access, outcomes, and value are compromised by the inefficiencies and wasted resources associated with the lack of widespread adoption and use of health information technology (Clarke et al. 2016, p. 24).
Clinicians, patients, families, and delivery systems all benefit from interoperable health information technology that improves the coordination of care and provision of uniform information to health-care providers involved with the care of individuals with poly chronic conditions . The implementation and effective use of health information technology to improve the care for patients with poly chronic conditions can be facilitated through strategies that support meaningful use of electronic and personal health records , patient portals, and registries, utilize secure information exchange platforms such as telemedicine and remote monitoring, and employ health information technology as a public health tool to monitor the health of the population and performance measures (HHS 2010, p. 8).
Telehealth technology provides the opportunity not only to identify disease exacerbation and provide timely interventions for chronically ill patients but also to improve patient self-efficacy for disease management through the inclusion of education and self-confidence building tools. However, issues such as those pertaining to reimbursement for remote patient-monitoring equipment and telemonitoring visits and the financial ability for some health-care providers to purchase monitoring units have created barriers in the widespread adoption of telehealth (Suter et al. 2011, pp. 91–92). Thus, while patient-centered approaches utilizing telehealth can help facilitate greater improvements in patient outcomes and costs, various obstacles may have to be overcome to increase the accessibility and utilization of such technology.
3 Outcome Evaluation and Improvement
The use and impact of interventions for patients with poly chronic conditions can be improved through monitoring and providing ongoing feedback (HHS 2010, p. 9). A process must be in place for evaluating the impact of interventions and applying evaluation information to make improvements as needed. Quality, cost-effectiveness, and significance are three broad areas that can be assessed to evaluate the overall impact of interventions in order for health-care providers to determine the value of their efforts and identify areas for improvement (Care Continuum Alliance 2012, p. 23). Outcome evaluation and improvement efforts should consider the multiple relevant levels involved given the importance of developing patient-centered interventions that incorporate medical and social services to comprehensively care for patients with poly chronic conditions.
Efforts to improve coordinated care for patients with poly chronic conditions are complemented by delivery system and provider payment changes accompanied by quality and performance metrics, as well as an increased degree of involvement of the public health system (HHS 2010, p. 7). Recognizing distinct community characteristics is essential when involving various types of care providers across multiple levels of the public health system in evaluation and improvement efforts. Health outcomes can be improved through increased communication and awareness across local stakeholders and the adoption of a context-specific approach to account for the distinct challenges and resources impacting health issues and mediating the effectiveness of health interventions in communities (Janosky et al. 2013, p. 248). When developing improvement plans and identifying the performance measures associated with such plans, various aspects of the community must be taken into consideration. Factors such as the population’s health needs, the availability of resources, and the accountability that health-care providers, organizations, and other involved entities are willing to accept for specific actions or contributions should be identified to ensure that strategies appropriately fit the communities in which they will be implemented (Stoto 2013, p. 4).
The opportunity exists for more widespread implementation of the PHM approach as recent changes to the US Medicare system encourage greater quality. The Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) ended the Medicare Part B Sustainable Growth Rate formula and replaced it with the Quality Payment Program, a value-based reimbursement system intended to improve Medicare through enhanced focus on quality care for patients. Through the Quality Payment Program, participating Medicare Part B providers can choose from two tracks: the Advanced Alternative Payment Models (APMs) , which entails earning an incentive payment for participation in an innovative payment model, or the Merit-based Incentive Payment System (MIPS) , which involves earning a performance-based payment adjustment. The first performance period is from January 1 to December 31 of 2017. During this performance period, providers must record quality data and note how technology was used to support their practice and then submit this data in 2018. Medicare will offer feedback to providers based on the data submitted, and for 2019 providers may potentially earn a positive payment adjustment under MIPS, or a 5% incentive payment for participation in an Advanced APM (Center for Medicare and Medicaid Services 2017).
The complex care needs of patients with poly chronic conditions often require various categories of providers and for providers to spend additional time with patients. Financial incentives can encourage care models to improve the health status and outcomes for patients with multiple chronic conditions (HHS 2010, p. 8). In a 2007 report developed to provide a greater understanding of the care needs of Medicaid beneficiaries who have multiple chronic conditions and are substantially driving costs, integration and coordination of care, performance measurement, financing, and evaluation were identified as key issues that must be addressed to improve the quality and cost of care for these patients (Kronick et al. 2007, p. 36). Reform efforts such as the Quality Performance Program hold the potential to comprehensively address these key issues by offering health-care providers tools and resources to a greater extent than in the past.
4 Integration and Coordination of Care
Patients with poly chronic conditions have complex, distinct needs for health and social services. Efforts to improve population health should include interventions that account for contextual and social factors, as well as individual factors. The balance of these types of interventions should be based on the distinct needs of patients and the communities in which they are being implemented in order to efficiently utilize resources and avoid gaps in the availability and accessibility of programs and services. Community coalitions of diverse members focused on a common goal provide the opportunity for complex health issues to be addressed at the local level by leveraging and increasing access to resources, coordinating services, reducing duplicative efforts, and garnering public support (Janosky et al. 2013, p. 246). Although measurement of the factors influencing population health outcomes may be arduous, a set of measures that operationally define population health dimensions is important for the various entities that must work cooperatively to improve the health of a population to monitor progress (Stoto 2013, p. 3).
The Health Impact Pyramid has been presented as a conceptual framework to depict the varying population impact levels of health interventions using a five-tier pyramid that incorporates both biomedical and social determinants of health. According to this framework, health interventions that accommodate socioeconomic factors and contextual/environmental factors require the least amount of individual-level behavior change and may have the greatest potential for impacting population health. Interventions involving the most individual effort and affecting the least change in population health are those focused on counseling, education , and clinical care. Protective interventions , including screenings and immunizations, which take place at a limited point in time and have the potential for long-term health impacts are depicted in middle-level of the pyramid. By coordinating interventions at each level of the pyramid, communities may achieve the maximum population health impact (Janosky et al. 2013, pp. 247–248).
In 2010, the US Department of Health and Human Services (HHS) developed a strategic framework intended to inspire a shift toward a multiple chronic conditions approach as opposed to the traditional approach of focusing on individual chronic illnesses. Four specific goals were outlined based on the HHS vision of “Optimum Health and Quality of Life for Individuals with Multiple Chronic Conditions.” These goals are “(1) Foster health care and public health system changes to improve the health of individuals with multiple chronic conditions , (2) Maximize the use of proven self-care management and other services by individuals with multiple chronic conditions, (3) Provide better tools and information to health care, public health, and social services workers who deliver care to individuals with multiple chronic conditions, and (4) Facilitate research to fill knowledge gaps about, and interventions and systems to benefit, individuals with multiple chronic conditions” (HHS 2010, p.6). In this organizing structure developed by HHS, health care management, interventions , and research are needed to address multiple chronic conditions (Lochner and Cox 2013, p. 1). Given that numerous federal programs related to chronic disease prevention and management are administered by HHS, the adoption of this framework holds the potential for widespread progress toward improving the health care and outcomes for patients with poly chronic conditions.
PHM efforts require new appropriate care processes and support for care processes using care managers and health information technology solutions that complement electronic health record capabilities. Also required are the right people to serve patients, with team-based care accepted as being essential (Healthcare Informatics 2016, p. 19). An interdisciplinary team with specialization in managing care transitions, the ability to be accessed on demand, and consistent communication across all stakeholders have been identified as essential components of solutions to effectively improve transitions of care, provide long-term care management, and reduce unplanned episodes of care (Clarke et al. 2016, p. 26).
The central goal of care coordination is to meet the needs and preferences of patients in the delivery of high-quality, high-value care (McDonald et al. 2014, p. 16). To that end, innovative approaches to effectively deliver comprehensive and appropriate health care continue to be explored. For example, the mobile integrated health-care model , which leverages EMS systems, has been introduced as a community-based and technologically sophisticated approach to address the gaps in coordinated care and service delivery for patients with chronic conditions . These programs utilize physicians, nurses, pharmacists, social workers, community health workers, emergency medicine professionals, and other resources and personnel. Central elements of the mobile integrated health-care model include an interprofessional team that is available around the clock, an operational dispatch and communications center, a transitional care team, longitudinal high-risk care involving in-home/at-work visits, advanced illness management involving the patient’s family and caregivers, and utilization of mobile clinicians and telemedicine to coordinate care for unplanned acute episodes (Clarke et al. 2016, pp. 27–28). This type of integration holds the potential to efficiently and effectively provide patient-centered care for individuals with poly chronic conditions , which in turn can result in improved health outcomes and reduced costs.
5 Conclusions and Implications
The health care and outcomes for patients with poly chronic conditions can be improved through the integration of multiple domains of the PHM approach and comprehensive coordination across multiple levels utilizing interdisciplinary care teams and appropriate applications of health information technology . Patient identification and risk stratification enable health-care providers to focus the appropriate resources on the patients with the greatest needs. By preventing acute events and worsening health status in higher-risk patients and providing preventative and wellness services for lower-risk patients, care management efforts can achieve optimal impact on health outcomes and cost-effectiveness . Consideration for environmental and geographic characteristics provides the opportunity to better understand patterns of need distribution and potential hazards to health and well-being. Purposeful engagement strategies and communication facilitate patient involvement in interventions tailored to their specific health-care needs and personal health goals. Innovative uses of technology and analytic tools are essential throughout this process.
The use of technology to address complex medical problems is an area that continues to expand and evolve. A research report developed by Healthcare Informatics states that “applications for registries, care gap identification, risk stratification , predictive modeling, utilization management, benchmarking, clinical dashboards, patient outreach, and automated work queues” are required for PHM (Healthcare Informatics 2016, p. 13). While the level of resources and capabilities varies across the organizations and communities providing health care, there must be continuous efforts toward adopting health information technology that facilitates interoperability, data sharing , and effective communication to ensure that applicable knowledge is derived from the information available.
Multiple implications of PHM for poly chronic conditions suggest that concerted efforts in promoting preventive strategies can yield numerous benefits. For example, these efforts will not only provide the opportunity to positively impact both patients and health-care providers but also offer alternatives to institutional care of the vulnerable population. Patients can experience improvements in health behaviors, self-efficacy , health status, quality of life , and health services utilization. Clinicians can experience improvements in resource efficiency, understanding patient health risks, quality care , and patient satisfaction and outcomes (Care Continuum Alliance 2012, p. 19). Sustainable improvements in the coordination of care require empowered patients who are able to self-advocate and utilize preventive care services and health-care providers who have new ways of viewing complex patients (Miller et al. 2013, p. S18). The process of integrating contextual and individual patient-centered domains of the PHM approach entails effort from clinicians, patients, caregivers, and other stakeholders. Continuous improvement efforts through impact evaluation and a commitment to the adoption of the health information technology resources needed are also critical aspects of this process. Patients with poly chronic conditions have complex needs and are often high utilizers of health services. Great potential exists to improve the health and health care of these individuals through improved coordination, integrating multiple domains of the PHM approach.
References
Agency for Healthcare Research and Quality. (2014). The guide to patient and family engagement: Enhancing the quality and safety of hospital care. Rockville: AHRQ. www.ahrq.gov/research/findings/finalreports/ptfamilyscan/ptfamily1.html.
Allen, A., Des Jardins, T. R., Heider, A., Kanger, C. R., Lobach, D. F., McWilliams, L., … & Sorondo, B. (2014). Making it local: Beacon communities use health information technology to optimize care management. Population Health Management, 17(3), 149–158.
Care Continuum Alliance. (2012, October). Implementation and evaluation: A population health guide for primary care models. Washington, DC: Care Continuum Alliance.
Center for Medicare and Medicaid Services. Quality payment program. Accessed from https://qpp.cms.gov/ on 1 Apr 2017.
Clarke, J. L., Bourn, S., Skoufalos, A., Beck, E. H., & Castillo, D. J. (2016). An innovative approach to health care delivery for patients with chronic conditions. Population Health Management, 20(1), 23–30.
Cromley, E. K., Wilson-Genderson, M., Heid, A. R., & Pruchno, R. A. (2016). Spatial associations of multiple chronic conditions among older adults. Journal of Applied Gerontology, 1–25. https://doi.org/10.1177/0733464816672044.
Healthcare Informatics. (2016, June). A roadmap for population health management. https://www.pcpcc.org/sites/default/files/resources/PHM-IBM_Watson-RR.pdf. Accessed 20 Mar 2017.
Jackson, C., Kasper, E. W., Williams, C., & DuBard, C. A. (2016). Incremental benefit of a home visit following discharge for patients with multiple chronic conditions receiving transitional care. Population Health Management, 19(3), 163–170.
Janosky, J. E., Armoutliev, E. M., Benipal, A., Kingsbury, D., Teller, J. L., Snyder, K. L., & Riley, P. (2013). Coalitions for impacting the health of a community: The Summit County, Ohio, experience. Population Health Management, 16(4), 246–254.
Kronick, R. G., Bella, M., Gilmer, T. P., & Somers, S. A. (2007). The faces of Medicaid II: Recognizing the care needs of people with multiple chronic conditions. Hamilton: Center for Health Care Strategies, Inc.
Kronick, R. G., Bella, M., & Gilmer, T. P. (2009). The faces of Medicaid III: Refining the portrait of people with multiple chronic conditions. Hamilton: Center for Health Care Strategies, Inc.
Lochner, K. A., & Cox, C. S. (2013). Prevalence of multiple chronic conditions among medicare beneficiaries, United States, 2010. Preventing Chronic Disease, 10, 120–137.
Lochner, K. A., Goodman, R. A., Posner, S., & Parekh, A. (2013). Multiple chronic conditions among medicare beneficiaries: State-level variations in prevalence, utilization, and cost, 2011. Medicare & Medicaid Research Review, 3(3), E1–E19.
McDonald, K. M., Schultz, E., Albin, L., Pineda, N., Lonhart, J., Sundaram, V., Smith-Spangler, C., Brustrom, J., Malcolm, E., Rohn, L., & Davies, S. (2014, June). Care coordination atlas version 4 (Prepared by Stanford University under subcontract to American Institutes for Research on Contract No. HHSA290-2010-00005I). AHRQ Publication No. 14–0037- EF. Rockville: Agency for Healthcare Research and Quality.
Miller, A., Cunningham, M., & Ali, N. (2013). Bending the cost curve and improving quality of care in America’s poorest city. Population Health Management, 16(S1), S–17.
Proctor, J., Rosenfeld, B. A., & Sweeney, L. (2016, January). Implementing a successful population health management program (Rep.). Retrieved March 20, 2017, from Philips website: https://www.usa.philips.com/c-dam/b2bhc/us/Specialties/community-hospitals/Population-Health-White-Paper-Philips-Format.pdf
Rocca, W. A., Boyd, C. M., Grossardt, B. R., Bobo, W. V., Rutten, L. J. F., Roger, V. L., … & Sauver, J. L. S. (2014, October). Prevalence of multimorbidity in a geographically defined American population: Patterns by age, sex, and race/ethnicity. In Mayo Clinic Proceedings, 89(10), 1336–1349. Elsevier.
Sears, M. E., & Genuis, S. J. (2012). Environmental determinants of chronic disease and medical approaches: Recognition, avoidance, supportive therapy, and detoxification. Journal of Environmental and Public Health, 2012, 1–15.
Stoto, M. A. (2013). Population health in the Affordable Care Act era (Vol. 1). Washington, DC: AcademyHealth.
Suter, P., Suter, W. N., & Johnston, D. (2011). Theory-based telehealth and patient empowerment. Population Health Management, 14(2), 87–92.
Tinetti, M. E., Esterson, J., Ferris, R., Posner, P., & Blaum, C. S. (2016). Patient priority-directed decision making and care for older adults with multiple chronic conditions. Clinics in Geriatric Medicine, 32, 261–275.
To, T., et al. (2015). Health risk of air pollution on people living with major chronic diseases: A Canadian population-based study. British Medical Journal, 5, 1–8.
U.S. Department of Health and Human Services. (2010). Multiple chronic conditions—A strategic framework: Optimum health and quality of life for individuals with multiple chronic conditions. Washington, DC: U.S. Dept. of Health and Human Services.
Wan, T. T. H. (2002). Evidence-based health management: Multivariate modeling approaches. Boston: Kluwer Academic Publishers.
Wan, T. T. H. (2014). A transdisciplinary approach to health policy research and evaluation. International Journal of Public Policy, 10(4–5), 161–177.
Ward, B. W. (2017). Barriers to health care for adults with multiple chronic conditions: United States, 2012–2015 (NCHS data brief, no 275). Hyattsville: National Center for Health Statistics.
Author information
Authors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG
About this chapter
Cite this chapter
Wan, T.T.H. (2018). Integration of Principles in Population Health Management. In: Population Health Management for Poly Chronic Conditions. Springer, Cham. https://doi.org/10.1007/978-3-319-68056-9_3
Download citation
DOI: https://doi.org/10.1007/978-3-319-68056-9_3
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-68055-2
Online ISBN: 978-3-319-68056-9
eBook Packages: Business and ManagementBusiness and Management (R0)