Abstract
Ovarian cancer is the seventh most common cancer in women worldwide. Several systematic reviews and meta-analyses have shown a positive association between obesity and ovarian cancer, and the American Institute for Cancer Research and World Cancer Research Fund recently concluded that body fatness (marked by body mass index) is a probable risk factor for ovarian cancer. The positive relation of body fatness to ovarian cancer appears to be more evident among non-users of hormone therapy. Furthermore, compared to normal weight, obesity is associated with poorer ovarian cancer survival. Possible biological mechanisms linking obesity with ovarian cancer risk and progression include insulin resistance and hyperinsulinaemia, increased levels of circulating growth factors, chronic inflammation, and altered levels of sex hormones. Thus, obesity, as a modifiable risk factor, should be targeted for preventing ovarian cancer and for improving ovarian cancer survival.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Ovarian cancer age standardized incidence rate
- Ovarian cancer risk factor
- Obesity
- Ovarian cancer mortality
- Insulin resistance
Introduction
The ovaries – as reproductive glands – are the sites of ovum production and they are also the main source of the sex hormones oestrogen and progesterone in premenopausal women. Ovarian cancer can originate from the three types of cells that make up the ovaries: epithelial cells, which cover the outer surface of the ovary; hormone producing stromal cells (structural tissue cells); and egg producing germ cells. Up to 95% of ovarian tumors are epithelial cell tumors.
Ovarian cancer is the seventh most common cancer in women worldwide [1]. In 2012, approximately 239,000 cases of ovarian cancer were recorded, accounting for 3.6% of all new cancer cases in women [1]. Almost half of all new ovarian cancer cases were reported in Asia (N = 112,000).
The age-standardized incidence rate of ovarian cancer is 6.1 per 100,000. Incidence rates are lower in less developed regions of the world (ASR 4.9 per 100,000) than more developed regions of the world (ASR 9.1 per 100,000) and they range from 3.6 per 100,000 in Western Africa to ≥11 per 100,000 women in Central, Eastern, and Northern Europe (Fig. 2.1) [1]. The estimated cumulative risk of developing ovarian cancer before the age of 75 years ranges from 0.5% in less developed regions of the world to 1% in more developed regions, and it reaches 1.3% in Central and Eastern Europe [1].
Estimated age-standardized incidence rates of ovarian cancer worldwide in 2012 (reproduced with permission from the International Agency for Research on Cancer [29])
Ovarian cancer is the eighth most common cause of death from cancer in women, with an estimated number of 152,000 deaths worldwide in 2012 (4.3% of deaths from cancer in women) [1]. Similar to its incidence rates, estimated age-standardized mortality rates (ASR) of ovarian cancer are lower in less developed regions of the world (ASR 3.1 per 100,000) and higher in more developed regions (ASR 5.0 per 100,000), such as North America (ASR 5.0), Northern Europe (ASR 5.9), Central and Eastern Europe (ASR 6.0), and Melanesia (ASR 6.5) [1].
According to the Global Burden of Disease Study, prevalent ovarian cancer cases contributed to an estimated 135,000 years lived with disability (YLDs) in 2013 – a figure that is comparable to the YLDs due to kidney cancer and malignant skin melanoma [2]. Thus, ovarian cancer is a relevant public health issue and it is crucial to gain a deeper understanding of its major risk factors – particularly those that are preventable, such as obesity.
Ovarian Cancer Characteristics and Risk Factors
Ovarian cancer frequently has no clinical symptoms in its early stages. Therefore, the disease is generally advanced when it is diagnosed. The 5-year survival rate ranges from approximately 30–50% [3].
Ovarian cancer is a heterogeneous disease with distinct histologic subtypes and thus, it is characterized by differences in epidemiologic and genetic risk factors, clinical presentation, response to treatment, and prognosis [4]. Five different tumor types account for 98% of ovarian cancers: high-grade serous carcinoma (70%), endometrioid carcinoma (10%), clear-cell carcinoma (19%), mucinous carcinoma (5%), and low-grade serous carcinoma (3%) [4].
Although ovarian cancer risk factors differ between distinct tumor histologic types, there are a number of established risk factors for total ovarian cancer, including age, reproductive history, modifiable lifestyle factors, family history, and genetic mutations.
Several factors concerning the reproductive history and life events during a woman’s lifetime may influence the risk of developing ovarian cancer. Whereas oral contraceptives seem to have a beneficial effect on the risk of developing ovarian cancer [5], intrauterine device use may pose a potential risk factor for ovarian cancer [6]. Early menarche and late natural menopause, and consecutively a higher number of menstrual cycles during a woman’s lifetime, increase the risk of ovarian cancer. In line with this, late menarche, breast feeding (lactation), early menopause, and number of pregnancies are beneficial factors that decrease the risk of developing ovarian cancer [5, 7]. It has been shown that the use of hormone therapy (HT) increases the risk of ovarian cancer [8, 9].
Polycystic ovarian syndrome is a potential risk factor for developing ovarian cancer [10]. However, the available evidence is not yet clear [11]. Furthermore, endometriosis is a risk factor for certain but not all histologic types of ovarian cancer [12]. Findings from a meta-analysis show positive associations between self-reported endometriosis and risks of clear-cell, low-grade serous, and endometrioid invasive ovarian cancers [12].
Smoking – as a modifiable lifestyle factor – is a risk factor for mucinous ovarian cancer, but not for other types of ovarian cancers [13]. Other lifestyle factors including obesity have been evaluated and the American Institute for Cancer Research and World Cancer Research Fund recently concluded that there is probable evidence for a positive association between obesity and ovarian cancer [14]. By comparison, the relations with other lifestyle factors, such as physical activity or dietary factors and ovarian cancer remain unclear [14].
Hereditary ovarian cancer makes up about 5–10% of all cases of ovarian cancer. The majority of hereditary ovarian cancers are based on mutations in the BRCA1 and BRCA2 genes [15]. In contrast to the lifetime risk of developing ovarian cancer in the general population (approximately 1%), women with a BRCA1 mutation have a lifetime risk of approximately 40% [16]. Mean cumulative ovarian cancer risk for BRCA2 mutation carriers is somewhat lower, at approximately 20% at age 70 [16]. Another type of hereditary ovarian cancer is based on mutations in genes such as MSH2 or MLH1, which represent DNA mismatch repair genes that are linked to hereditary non-polyposis colorectal cancer (HNPCC; also called Lynch syndrome), an autosomal dominant disorder that predisposes to colorectal, endometrial, and ovarian cancers, among others [15]. In women with Lynch syndrome, lifetime risk of ovarian cancer is between 3 and 14% [17]. Overall, at least 16 genes have been associated with ovarian cancer [15] – and it is likely that advances in genomic technologies will detect more genes associated with ovarian cancer in the future.
Association Between Obesity and Ovarian Cancer Incidence and Mortality
Numerous observational studies have investigated the association between obesity and the risk of ovarian cancer. However, results have not been entirely consistent. The current section aims at providing an overview of the existing evidence by summarizing the main findings from published meta-analyses, reviews, and observational studies.
Research on the relation between obesity and ovarian cancer risk has increased substantially in the past decade. In 2007, the World Cancer Research Fund/American Institute for Cancer Research stated that the evidence relating body fatness, abdominal fatness and weight change to ovarian cancer risk was inconclusive [18]. Since then, several systematic reviews and meta-analyses have been conducted, reflecting the increased number of available epidemiologic studies on adiposity and ovarian cancer.
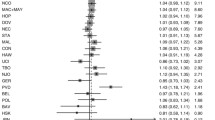
The Continuous Update Project “Ovarian Cancer 2014 Report” published by the World Cancer Research Fund and the American Institute for Cancer Research concluded that greater body fatness (marked by body mass index (BMI)) is a probable cause of ovarian cancer [14]. The systematic literature review underlying that report compared the highest versus lowest BMI levels and it included 26 prospective studies on ovarian cancer incidence and mortality [14]. The dose-response meta-analysis of that report included a total of 15,899 cases from 25 prospective studies (22 risk estimates) and it showed a statistically significant increased ovarian cancer risk of 6% per 5 BMI units (relative risk (RR) = 1.06; 95% confidence interval (CI): 1.02–1.11) (Fig. 2.2). However, there was evidence of substantial heterogeneity between studies (I2 = 55%). Results from additional analyses identified several possible sources of heterogeneity, such as tumor type, use of HT, and menopausal status. With respect to tumor type, the positive association between BMI and risk for ovarian cancer was slightly more pronounced for borderline serous, invasive endometrioid, and invasive mucinous tumors, with pooled RRs per 5 BMI units of 1.24 (95% CI: 1.18–1.30), 1.17 (95% CI: 1.11–1.23), and 1.19 (95% CI: 1.06–1.32), respectively [14]. By comparison, there was no association with serous invasive cancer (pooled OR per 5 BMI units: 0.98; 95% CI: 0.94–1.02).
Dose-response meta-analysis of BMI and ovarian cancer (conducted by and reproduced with permission from the World Cancer Research Fund/American Institute for Cancer Research [14])
In addition to BMI, the Continuous Update Project summarized the findings on weight, waist circumference, and waist-to-hip ratio in relation to ovarian cancer risk. With respect to weight, a dose-response meta-analysis of three cohort studies revealed a summary RR of 1.05 (95% CI: 1.02–1.07) per 5 kg increase in weight. A dose-response meta-analysis of four studies on the association between waist circumference and ovarian cancer risk showed a statistically non-significant positive association, with a RR of 1.03 (95% CI: 0.97–1.10 per 10 cm). Furthermore, four studies were included in a dose-response meta-analysis for waist-to-hip ratio and ovarian cancer and no association was observed (RR = 0.99; 95% CI: 0.92–1.06 per 10 cm).
The Continuous Update Project concluded that there was evidence of positive association between obesity (as assessed by BMI) and ovarian cancer risk , with the exception of serous invasive cancer. By comparison, the evidence for abdominal fatness (as assessed by waist circumference and waist-to-hip ratio) was judged limited and inconclusive [14].
A recently published meta-analysis included 13 case-control and 13 cohort studies with a total of 12,963 ovarian cancer cases and 2,164,977 participants [19]. As compared with normal weight (BMI = 18.5–24.9 kg/m2), that meta-analysis showed a pooled RR for overweight (BMI = 25.0–29.9 kg/m2) of 1.07 (95% CI: 1.02–1.12) and a pooled RR for obesity (BMI ≥ 30 kg/m2) of 1.28 (95% CI: 1.16–1.41) [19]. The positive association held true for both Caucasian and Asian studies. However, subgroup analyses showed that overweight and obesity were associated with an increased risk of ovarian cancer in premenopausal women only (RR for overweight = 1.31; 95% CI: 1.04–1.65; RR for obesity = 1.50; 95% CI: 1.12–2.00), but showed no relation in postmenopausal women [19].
The Collaborative Group on Epidemiological Studies of Ovarian Cancer conducted an individual participant meta-analysis on the association between body size (height and BMI) and risk of ovarian cancer [13]. The investigators included 47 studies and a total of 25,157 ovarian cancer cases and found a statistically significant positive association between BMI and ovarian cancer risk that did not substantially vary by age, year of birth, ethnicity, education, age at menarche, parity, family history of ovarian or breast cancer, use of oral contraceptives, menopausal status, hysterectomy, smoking, or alcohol consumption. However, there was significant heterogeneity between ever-users and never-users of HT. Specifically, a 5 kg/m2 increase in BMI was associated with a RR of 1.10 (95% CI: 1.07–1.13) in HT never-users, whereas it was related to a RR of 0.95 (95% CI: 0.92–0.99) in HT ever-users [13]. Data showing that the association between BMI and ovarian cancer incidence is modified by HT had first been reported by Leitzmann and colleagues [20]. They found that among never users of HT, the risk of ovarian cancer for obese versus normal weight women was 1.83 (95% CI: 1.18–2.84), whereas no association between BMI and ovarian cancer was noted among ever HT users (RR = 0.96; 95% CI: 0.65–1.43; P for interaction = 0.02).
Dixon and colleagues pooled data from 39 studies of the International Ovarian Cancer Association Consortium in a Mendelian randomization study, including a total of 14,047 ovarian cancer cases, to investigate the association between BMI and subtypes of ovarian cancer [21]. Mendelian randomization uses genetic markers (instrumental variables) as proxies for risk factors . In that study, a weighted genetic risk score for BMI was constructed by summing alleles associated with higher BMI across a predefined number of single nucleotide polymorphisms that had previously been associated with BMI. The researchers found that genetically predicted increasing BMI (per 5 kg/m2) was associated with an increased risk of non-high grade serous ovarian cancer (pooled OR = 1.29; 95% CI: 1.03–1.61) but was unrelated to the more common high grade serous ovarian cancer (pooled OR = 1.06; 95% CI: 0.88–1.27).
Compared to BMI as a metric of adiposity, adult weight gain better reflects the dynamic pattern of weight trajectories throughout adult life. Whereas BMI captures both fat mass and lean body mass, adult weight gain primarily captures increasing fat mass. Keum and colleagues conducted a dose-response meta-analysis of prospective observational studies to investigate the association between adult weight gain and adiposity-related cancers [22]. The dose-response meta-analysis was based on two eligible prospective studies among postmenopausal women. Findings showed that each 5 kg increase in adult weight gain was associated with a 13% increase in risk of developing ovarian cancer (RR = 1.13; 95% CI: 1.03–1.23) in postmenopausal women with no/low HT use [22].
Summarizing the results from meta-analyses and reviews, it can be concluded that there is a positive relationship between BMI and risk of developing ovarian cancer. An increase of 5 BMI units is associated with a 6% increased risk of ovarian cancer. However, the strength of the association varies according to menopausal status, HT use, and tumor histologic type.
Association Between Obesity and Ovarian Cancer Survival
Obesity may not only be associated with an increased risk of developing ovarian cancer, but may also produce poor survival among women with ovarian cancer. As individual studies on the association between obesity and ovarian cancer survival have yielded conflicting results, the following section summarizes the main findings from published meta-analyses.
Bae et al. conducted a meta-analysis on obesity five years before diagnosis, obesity at young age, and obesity at diagnosis in relation to ovarian cancer survival [23]. The pooled results from three cohort studies that investigated the relationship between obesity in adolescence and ovarian cancer survival yielded a summary hazard ratio (HR) of 1.67 (95% CI: 1.29–2.16). Three cohort studies on obesity 5 years before ovarian cancer diagnosis and ovarian cancer survival showed a weaker relation (HR = 1.35; 95% CI: 1.03–1.76), as did studies examining the association between obesity at diagnosis and ovarian cancer survival (HR = 1.11; 95% CI: 0.97–1.27).
A meta-analysis by Protani and colleagues included 14 cohort studies and showed that ovarian cancer survival was poorer in obese women compared to non-obese women (HR = 1.17; 95% CI: 1.03–1.34) [24]. The pooled risk estimates did not vary between studies that measured pre-diagnosis BMI (HR = 1.13; 95% CI: 0.95–1.35), BMI at the time of diagnosis (HR = 1.13; 95% CI: 0.81–1.57), or BMI at the time of chemotherapy (HR = 1.13; 95% CI: 0.92–1.39), although all risk estimates were statistically non-significant.
Nagle and colleagues used data from 21 case-control studies, including 12,390 women with ovarian cancer from the Ovarian Cancer Association Consortium to investigate the association between pre-diagnosis BMI and progression-free survival, ovarian cancer-specific survival, and overall survival [25]. Multivariate analyses showed that overweight and obese women experienced worse survival than women with normal weight, although associations were not statistically significant. Furthermore, each 5-unit increase in BMI was related to a borderline significant 3% increased risk of death (95% CI: 1.00–1.07). Results stratified by tumor histologic type revealed a borderline significant positive association for survival among women with high-grade serous cancer, with a pooled HR of 1.04 (95% CI: 1.00–1.09) for each 5-unit increase in BMI. Positive but statistically non-significant associations were noted for survival among women with low-grade serous and endometrioid cancers. No associations were noted for mucinous and clear cell tumors [25]. Compared to women with normal weight, obese women showed poorer progression-free and overall survival, with HRs of 1.10 (95% CI: 0.99–1.23) and 1.12 (95% CI: 1.01–1.26), respectively.
Taken together, the evidence regarding the relationship between obesity and ovarian cancer survival is less clear than that between obesity and ovarian cancer incidence, but results from epidemiologic studies suggest that obesity is associated with poor ovarian cancer survival.
In addition to ovarian cancer survival, several studies investigated the relation between adiposity and surgical morbidity and clinical outcomes in ovarian cancer patients. A meta-analysis of five studies showed that compared to non-obese ovarian cancer patients, obese patients had an increased incidence of wound complications (odds ratio (OR) = 4.81; 95% CI: 2.40–9.62) [26]. However, there were no significant associations between BMI and febrile complications, ileus, or venous thromboembolism. In addition, there were no significant relations between BMI and intra-operative outcomes, such as cytoreduction status, estimated blood loss, or operation time. While obese patients showed a statistically significantly longer hospital stay than non-obese patients, there were no differences between obese and non-obese patients regarding 30-day mortality or transfusion rates [26].
Potential Biological Mechanisms
Obesity has been associated with increased risk and poor survival regarding cancers at multiple body sites, including several gynecological malignancies [27]. Possible mechanisms linking obesity with ovarian cancer risk and progression include insulin resistance and hyperinsulinaemia , increased levels of circulating growth factors, chronic inflammation, and altered levels of sex hormones [28].
Circulating levels of insulin and leptin are elevated in obese people and may promote the growth of cancer cells. In addition, obesity-related insulin resistance leads to compensatory increased insulin production and thus to hyperinsulinemia, which, in turn, may increase the risk of cancer. Furthermore, sex hormones, including estrogens, androgens, and progesterone, are likely to play a mechanistic role in ovarian cancer development. Additionally, obesity is related to a chronic state of low-grade inflammation. Compared to people with normal weight, levels of pro-inflammatory factors, such as tumor necrosis factors (TNF-) alpha, interleukin 6, and C-reactive protein are increased in obese people. Chronic inflammation can promote cancer development.
Chapter 6 of this book provides detailed information on the underlying biologic mechanisms linking obesity with ovarian cancer .
Conclusions
As outlined in this chapter, BMI is associated with an increased risk of developing ovarian cancer. The positive relation of body fatness to ovarian cancer is more evident among HT non-users than HT users. Furthermore, obesity appears to be associated with poor survival among ovarian cancer patients. Additional studies are needed to strengthen the evidence and to further investigate the underlying biological mechanisms.
References
Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136(5):E359–86.
Global Burden of Disease Study 2013 Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet (London, England). 2015;386(9995):743–800.
De Angelis R, Sant M, Coleman MP, Francisci S, Baili P, Pierannunzio D, et al. Cancer survival in Europe 1999-2007 by country and age: results of EUROCARE--5-a population-based study. Lancet Oncol. 2014;15(1):23–34.
Prat J. Ovarian carcinomas: five distinct diseases with different origins, genetic alterations, and clinicopathological features. Virchows Arch. 2012;460(3):237–49.
Beral V, Doll R, Hermon C, Peto R, Reeves G. Ovarian cancer and oral contraceptives: collaborative reanalysis of data from 45 epidemiological studies including 23,257 women with ovarian cancer and 87,303 controls. Lancet (London, England). 2008;371(9609):303–14.
Tworoger SS, Fairfield KM, Colditz GA, Rosner BA, Hankinson SE. Association of oral contraceptive use, other contraceptive methods, and infertility with ovarian cancer risk. Am J Epidemiol. 2007;166(8):894–901.
Jordan SJ, Cushing-Haugen KL, Wicklund KG, Doherty JA, Rossing MA. Breast-feeding and risk of epithelial ovarian cancer. Cancer Causes Control. 2012;23(6):919–27.
Rodriguez C, Patel AV, Calle EE, Jacob EJ, Thun MJ. Estrogen replacement therapy and ovarian cancer mortality in a large prospective study of US women. JAMA. 2001;285(11):1460–5.
Beral V, Gaitskell K, Hermon C, Moser K, Reeves G, Peto R. Menopausal hormone use and ovarian cancer risk: individual participant meta-analysis of 52 epidemiological studies. Lancet (London, England). 2015;385(9980):1835–42.
Chittenden BG, Fullerton G, Maheshwari A, Bhattacharya S. Polycystic ovary syndrome and the risk of gynaecological cancer: a systematic review. Reprod Biomed Online. 2009;19(3):398–405.
Barry JA, Azizia MM, Hardiman PJ. Risk of endometrial, ovarian and breast cancer in women with polycystic ovary syndrome: a systematic review and meta-analysis. Hum Reprod Update. 2014;20(5):748–58.
Pearce CL, Templeman C, Rossing MA, Lee A, Near AM, Webb PM, et al. Association between endometriosis and risk of histological subtypes of ovarian cancer: a pooled analysis of case-control studies. Lancet Oncol. 2012;13(4):385–94.
Collaborative Group on Epidemiological Studies of Ovarian C. Ovarian cancer and body size: individual participant meta-analysis including 25,157 women with ovarian cancer from 47 Epidemiological Studies. PLoS Med. 2012;9(4):e1001200.
World Cancer Research Fund and American Institute for Cancer Research. Continuous update project: ovarian cancer 2014 report: food, nutrition, physical activity, and the prevention of ovarian cancer. 2014.
Pennington KP, Swisher EM. Hereditary ovarian cancer: beyond the usual suspects. Gynecol Oncol. 2012;124(2):347–53.
Chen S, Parmigiani G. Meta-analysis of BRCA1 and BRCA2 penetrance. J Clin Oncol. 2007;25(11):1329–33.
Koornstra JJ, Mourits MJ, Sijmons RH, Leliveld AM, Hollema H, Kleibeuker JH. Management of extracolonic tumours in patients with Lynch syndrome. Lancet Oncol. 2009;10(4):400–8.
World Cancer Research Fund & American Institute for Cancer Research. Food, nutrition, physical activity, and the prevention of cancer: a global perspective. Washington DC: AICR; 2007.
Liu Z, Zhang TT, Zhao JJ, Qi SF, Du P, Liu DW, et al. The association between overweight, obesity and ovarian cancer: a meta-analysis. Jpn J Clin Oncol. 2015;45(12):1107–15.
Leitzmann MF, Koebnick C, Danforth KN, Brinton LA, Moore SC, Hollenbeck AR, et al. Body mass index and risk of ovarian cancer. Cancer. 2009;115(4):812–22.
Dixon SC, Nagle CM, Thrift AP, Pharoah PD, Pearce CL, Zheng W, et al. Adult body mass index and risk of ovarian cancer by subtype: a Mendelian randomization study. Int J Epidemiol. 2016;45(3):884–95.
Keum N, Greenwood DC, Lee DH, Kim R, Aune D, Ju W, et al. Adult weight gain and adiposity-related cancers: a dose-response meta-analysis of prospective observational studies. J Natl Cancer Inst. 2015;107(2)
Bae HS, Kim HJ, Hong JH, Lee JK, Lee NW, Song JY. Obesity and epithelial ovarian cancer survival: a systematic review and meta-analysis. J Ovarian Res. 2014;7:41.
Protani MM, Nagle CM, Webb PM. Obesity and ovarian cancer survival: a systematic review and meta-analysis. Cancer Prev Res (Phila). 2012;5(7):901–10.
Nagle CM, Dixon SC, Jensen A, Kjaer SK, Modugno F, de Fazio A, et al. Obesity and survival among women with ovarian cancer: results from the Ovarian Cancer Association Consortium. Br J Cancer. 2015;113(5):817–26.
Smits A, Lopes A, Das N, Kumar A, Cliby W, Smits E, et al. Surgical morbidity and clinical outcomes in ovarian cancer - the role of obesity. BJOG. 2016;123(2):300–8.
Bhaskaran K, Douglas I, Forbes H, dos-Santos-Silva I, Leon DA, Smeeth L. Body-mass index and risk of 22 specific cancers: a population-based cohort study of 5.24 million UK adults. Lancet (London, England). 2014;384(9945):755–65.
Allott EH, Hursting SD. Obesity and cancer: mechanistic insights from transdisciplinary studies. Endocr Relat Cancer. 2015;22(6):R365–86.
International Agency for Research on Cancer. GLOBOCAN 2012: Estimated cancer incidence, mortality and prevalence worldwide in 2012 2012. http://globocan.iarc.fr/Pages/Map.aspx. Accessed13 Sept 2016.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG
About this chapter
Cite this chapter
Jochem, C., Schlecht, I., Leitzmann, M. (2018). Epidemiologic Relationship Between Obesity and Ovarian Cancer. In: Berger, N., Klopp, A., Lu, K. (eds) Focus on Gynecologic Malignancies. Energy Balance and Cancer, vol 13. Springer, Cham. https://doi.org/10.1007/978-3-319-63483-8_2
Download citation
DOI: https://doi.org/10.1007/978-3-319-63483-8_2
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-63482-1
Online ISBN: 978-3-319-63483-8
eBook Packages: MedicineMedicine (R0)