Abstract
Colon and rectal surgery has witnessed a vast increase in both the use of and subsequent publications about single-incision laparoscopic surgery (SILS). While single-incision surgery goes by several different names, it is important to keep in mind that when learning any new approach, the operative procedure (with regard to safety and outcomes) should remain the same. Although there is a learning curve that each surgeon must complete and overcome in order to become proficient, the patient should not suffer in the interim. With regard to colon and rectal surgery, special populations such as those with inflammatory bowel disease, diverticulitis, large tumors, and other inflammatory disorders may present technical challenges for open as well as other minimally invasive approaches. Therefore, it is especially important when selecting the operative approach to match it to the individual patient at hand, as well as being realistic about one’s technical expertise and experience with a particular procedure. In this chapter, we will highlight the unique challenges of single-incision surgery, discuss general patient selection and consideration issues, and examine how this approach relates to those particular cohorts such as those with inflammatory bowel disease and obesity.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Single-incision laparoscopic surgery (SILS)
- Laparo-endoscopic single-site surgery (LESS)
- Single port access surgery (SPA)
- Minimally invasive surgery
- Laparoscopic surgery
- Single-access surgery
- Single-site surgery
- “Scarless surgery,” Patient selection
- Obesity
- IBD
-
Available data supports the safety and feasibility of SILS across diverse patient populations when performed by surgeons with appropriate experience and expertise.
-
Early on in one’s SILS experience, it is wise to first select patients with no prior abdominal operations, with low BMI, as well as avoid its use in patients with bulky tumors or a history of inflammatory disease.
-
A surgeon must be honest with himself/herself regarding his or her own ability and experience when deciding a candidate for single-incision laparoscopy.
-
Do not sacrifice doing the correct operation in favor of a particular approach.
-
Special populations like those with inflammatory bowel disease and obese patients present issues beyond the operating room that you need to be prepared to evaluate and treat.
-
Straightforward laparoscopic cases in the morbidly obese patients and those with inflammatory disease present technical challenges; the single-incision approach may exacerbate the technical challenges, but with operator experience these cases can be safely and successfully completed.
-
The principles of proper operative technique apply to SILS similar to any other operative approach.
Introduction
The advantages of laparoscopic surgery over an open approach are now well accepted. Surgeons and patients alike have benefited from the decreased morbidity, faster recovery, decreased pain, and shorter hospital stays offered through minimally invasive approaches. Importantly, the COST and CLASICC I and II trials have demonstrated the oncologic equivalence of laparoscopic resection compared to open resection with regard to colorectal malignancy [1, 2]. Single-incision laparoscopic surgery (SILS) appears to be the next natural step toward ever more minimally invasive approaches in the ultimate quest for “scarless surgery.”
Although high-level evidence demonstrating superiority of SILS over traditional multi-port laparoscopy does not currently exist, there are many theoretical benefits. Advocates have suggested potential benefits to include less pain, faster return of bowel function, lower hernia rate, fewer infectious complications, and decreased inflammatory response [3]. Critics of the approach express concerns over increased operative times, higher complication rates, oncologic inferiority, and a high cost with a lack of any tangible patient benefit. Regardless, assuming equivalence (even if it is proven that no additional benefit is gained by SILS over traditional laparoscopy with regard to patient outcomes), it remains an appealing option as it offers the improved cosmesis by limiting the number of abdominal wall incisions needed. Of course, any perceived benefit gained from a single-incision approach must be weighed against the safety, feasibility, and efficacy of such an approach. For proponents of this approach, there have been numerous reports in recent years demonstrating the safety and feasibility of the SILS approach when performed by well-trained and experienced surgeons, even when applied to complex procedures. Opponents note that “experience” and “expertise” are vaguely defined, and embarking on this technique with lesser training and in suboptimal patients will lead to higher rates of untoward outcomes.
Proper exposure, triangulation of instrumentation, and traction/countertraction are fundamental tenets of laparoscopic surgery, and these do not change with single-incision over multi-port laparoscopy. Achieving these tenets is clearly more challenging with SILS over traditional laparoscopy as the manipulation of straight instruments parallel to the operating camera through a small single incision can significantly decrease the surgeon’s range of motion. The addition of curvilinear instruments attempts to overcome this, although also relies on a learning curve to master their use. In addition, SILS may be particularly challenging in colorectal procedures, which often require operating in multiple quadrants. Given these added challenges, proper patient selection is clearly paramount to the successful application of SILS. Despite these inherent difficulties, becoming facile in the technique provides another tool in the surgeon’s armamentarium that may provide certain patients benefits and improved outcomes.
General Considerations
Patient Selection
Proper patient selection depends first on the surgeon’s own personal confidence, competence, and experience —not only with the SILS approach but also with the specific operation being performed. Certainly, as the complexity of the procedure increases, so do the challenges associated with single-incision surgery. In fact, the challenges may be amplified with a single-incision approach given its unique technical characteristics mentioned above. The surgeon must be honest with himself or herself regarding their own ability and experience when deciding who is a candidate for SILS.
Perhaps one of the most important factors is the existing laparoscopic skill set of the surgeon. It has been suggested that among surgeons who have mastered traditional multi-port laparoscopy, the SILS learning curve may actually be quite minimal, generally less than 40 cases [4, 5]. However, the data with regard to the SILS learning curve are not nearly as robust as that of traditional laparoscopy, and to date there is simply too little known to make any formal credentialing suggestions. What is clear is that a strong laparoscopic skill set is a prerequisite for any surgeon who is considering adding the SILS technique to his or her surgical toolkit.
Patient factors also play an important role in deciding who is appropriate for this approach. An ileocecectomy or right hemicolectomy in a thin patient with no prior surgeries is clearly more straightforward than a total proctocolectomy with pouch reconstruction in an obese patient with ulcerative colitis and multiple prior abdominal operations. Bulky tumors, low rectal lesions, inflammatory disease, presence of fistulae, obesity, and prior abdominal operations all add to the complexity of the procedure and should be considered carefully and cautiously when determining the appropriate surgical approach.
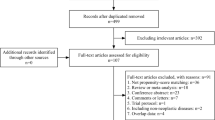
In general, it is prudent for the surgeon to select patients with low BMIs , without prior abdominal surgeries, and with either benign disease or small manageable tumors early in his or her experience with the SILS approach. Avoiding patients with previous surgeries is both due to the time-consuming lysis of adhesion in the face of what may already be a longer operation due to technique itself, as well as the potential higher risk of an enterotomy. Once he or she gains more experience in the SILS, there is mounting evidence that the technique can be safely performed across a wide variety of disease processes and patient populations [6,7,8,9,10,11,12,13,14,15,16] (Table 2.1).
It also is important to remember that this technology is still in its relatively early stages. As such, the bulk of the data currently available is retrospective or prospectively collected cohorts in which surgeons control the population, and is no doubt the subject of significant selection bias—as the majority of included patients had low BMI, no bulky malignancy, and no inflammatory disease, and the operations were performed by surgeons who were very experienced in the technique.
Indications
While SILS uses only one incision in the abdominal wall and the entire procedure is performed through this opening and traditional laparoscopy uses multiple ports, the basic tenets of minimally invasive surgery remain the same: adequate exposure, tension and counter-tension, triangulation, and safe tissue handling. Major differences may include the use of instruments and devices tailored for in-line viewing, differences in ergonomics, and relative propensity for instruments to cross with SILS. However, it is important to again point out that all types of colorectal operations have been performed safely and effectively through a SILS procedure, from a stoma to a total proctocolectomy and ileal pouch-anal anastomosis [8, 11, 12]. While opponents may claim SILS is a “gimmick” or marketing maneuver, the reality is that SILS has become the preferred approach for many surgeons.
Preoperative Planning
Regardless of the operative approach used, every patient should undergo a thorough history and physical examination, along with a generalized risk stratification to determine the potential for morbidity and mortality (Table 2.2). In addition, patients undergoing a major abdominal operation should, in general, have a complete blood count, chemistry panel and carcinoembryonic antigen [(CEA) in cases of malignancy]. Additional radiological and endoscopic examinations will allow for appropriate localization of the disease and staging for cases of malignancy. Surgeons should make a special point of ensuring prior tattooing with India ink or clips has been performed, as reliance on descriptive reports with regard to tumor location is fraught with potential for error. While still controversial, the authors prefer a mechanical bowel preparation with oral antibiotics for all colorectal resections. Intravenous antibiotics should be given perioperatively for all patients in conjunction with appropriate Surgical Care Improvement Project (SCIP) guidelines. Intraoperatively, it is important to ensure appropriate blood glucose control, normothermia, and that supplemental oxygen therapy is given [13].
Considerations in Select Populations
Ultimately, all patients eligible for laparoscopy may be considered potential candidates for SILS in the right hands. While there may be no definitive contraindications for SILS, the surgeon should carefully consider each patient and procedure individually when deciding the appropriate surgical approach. Three patient populations pose particular challenges and deserve special consideration: the obese, those with inflammatory disease, and colorectal cancer patients.
SILS and Obesity
It is well understood that obesity, particularly visceral obesity, significantly increases the complexity of any laparoscopic procedure (Fig. 2.1). While the effect of obesity on outcomes following traditional laparoscopy is still an area of active investigation, evidence clearly supports that traditional multi-port laparoscopy is safe and feasible in obese patients, with outcomes similar to those of non-obese patients, especially when compared to open surgery [14,15,16,17,23].
SILS is undeniably more technically challenging than traditional multi-port laparoscopy in this population, amplifying the effect of obesity on the difficulty of the procedure. The presence of high amounts of visceral fat makes the identification of the correct surgical plane more difficult and impedes proper surgical exposure (Fig. 2.2). Therefore, it is not surprising that much of current literature demonstrating the feasibility of SILS has centered on non-obese patients [3, 7,8,9,10]. It is revealing that in two separate systematic reviews of single-incision laparoscopic colectomy, the mean BMIs of patients included in the literature were found to be 25.5 and 25.8 kg/m2, respectively [24, 25].
Nevertheless, there have been some published data on short-term outcomes of obese patients undergoing single-incision laparoscopic colectomy. Regrettably, these studies are all based on small patient numbers and the data are somewhat conflicting. In some, visceral obesity has been associated with longer operative times, increased blood loss, and was a primary factor leading to conversion to an open procedure [26, 27]. Contrarily, others have found no difference in conversion rate, operative time, estimated blood loss, time to return of bowel function, length of stay, or reoperation and readmission rates between multi-port and single-port approaches in obese patients [15, 28]. This contrast more likely highlights the variations in surgeon experience and expertise with this approach.
Key points to consider are adhering to the simple principles of all minimally invasive surgery: proper exposure, appropriate definition of anatomy, apposite tissue handling, and technically sound operative steps. One of the initial major issues encountered is the lack of domain when establishing a pneumoperitoneum with any minimally invasive approach that often occurs in the obese patient (Fig. 2.3). Positioning the omentum in the upper abdomen, rotating the operating table to the extremes to facilitate gravity effects on the bowel, and “flipping” the mesentery of the small bowel to allow it stay in place are tricks to help ensure adequate exposure (Fig. 2.4).
While obesity is associated with increased technical challenges, it is clear that SILS can be safely applied in this patient population by experienced surgeons. However, the current data are significantly limited and further high-level studies must be done to more definitively demonstrate its feasibility in the obese population before more generalized recommendations can be made.
SILS and Inflammatory Disease
Another challenging patient population to consider in the practical application of SILS is the patient with inflammatory disease—notably Crohn’s disease, ulcerative colitis, and diverticulitis. Significant inflammation, scarring, distorted planes, fistulae, abscesses, and infectious complications all contribute to making the application of minimally invasive techniques distinctly challenging in these patients (Fig. 2.5).
One must also consider the fact that general benefits of reduced narcotic requirement and shorter length of stay in hospital with minimally invasive techniques may not be as pronounced in patients with inflammatory bowel disease (IBD) [29, 30]. Thus, it is less likely SILS will offer any additional benefit over traditional laparoscopy with regard to those issues. Still, SILS has the potential of preserving the benefits standard laparoscopy does offer, while minimizing the extent of incisions with the resultant improved cosmesis. This may be best appreciated in the young IBD patient, in whom surgical scars can have a significant psychological impact. The senior author feels the ideal SILS candidate is a young patient with inflammatory bowel disease who may require an ileocecectomy, where the majority of the operation is limited to one or two abdominal quadrants. In addition, it is important to remember that inflammatory bowel disease encompasses a spectrum of phenotypical manifestations, and those with phlegmonous or fistulizing disease present much different challenges than those with fibrostenotic manifestations.
Although well-designed, large, multicenter studies demonstrate the feasibility of SILS when performed by experienced laparoscopic surgeons [12], only a minority of patients included in the series had underlying IBD. Nevertheless, several smaller series have shown that SILS can be safely applied to IBD patients with similar outcomes to traditional laparoscopy, with no difference in operative time, conversion to open surgery, complications, or short-term clinical outcomes, even in complex and recurrent disease [6, 13, 14, 31]. In addition, in patients with isolated disease, when the inflammatory component of IBD can be safely mobilized, the remainder of the operation can be safely performed extracorporeally with relatively normal bowel (Figs. 2.6a, b).
Diverticular Disease
As with IBD patients, those with complicated diverticular disease also pose a unique and daunting challenge to the surgeon. Patients are often systemically ill, have had prior procedures, and may not tolerate a prolonged operation. Moreover, inflammation, scarring, and presence of an abscess make minimally invasive approaches challenging. Two large retrospective series have indicated that SILS sigmoidectomy can be effective for treatment of diverticular disease, even in the setting of contained perforation and prior operations [15, 16]. Operative times, conversion to open surgery, anastomotic leak, and hernia rates were found to be similar to that of traditional laparoscopy. While not mandatory, use of ureteral stents- especially lighted stents- may facilitate identification of the left ureter in patients with an associated abscess, large amounts of inflammation or if early in one’s experience (See Video 2.1).
SILS and Malignancy
As mentioned above, the COST and CLASICC Trials have proven the oncologic equivalence of multi-port laparoscopic resection to open resection for colorectal malignancy. The laparoscopic approach has since been enthusiastically applied. The same oncologic equivalence will need to be proven for the SILS approach before it can be widely accepted and applied in the resection of colorectal cancer. However, ensuring the appropriate operation that follows traditional oncological principles is performed regardless of the approach (SILS vs. multi-port vs. open) should lead to the same oncological results when SILS is performed.
A number of feasibility studies have been published regarding SILS colectomy for colorectal tumors—more for colon and less for rectal cancer. Not surprisingly, selection bias is again witnessed in the data available to date. The majority of data are heavily skewed regarding the type of procedure being performed, with most focusing on the right hemicolectomy [3, 26, 32,33,34,35,36,37,38,39,40,41]. Large case series have supported the use of SILS for right-sided malignancy, reporting similar operative times, conversion rates, mortality/morbidity, and most importantly, oncologic adequacy as demonstrated by specimen quality and lymph node retrieval when compared to multi-port laparoscopy [42, 43] (Table 2.3).
There is no question that procedures for left-sided and rectal malignancy are technically more challenging than right-sided lesions. The multi-quadrant mobilization, intracorporeal anastomosis, and generally more complicated exposures required with left-sided lesions make application of SILS approaches increasingly challenging. Not unexpectedly then, the data for single-incision resection of left-sided and rectal malignancies are much more limited. Early reports of SILS for rectal cancer were somewhat concerning with longer operative times, high stoma rates, and less than adequate mesorectal excision [44]. A few small, randomized trials have been performed comparing outcomes of single-incision resection for colon cancer to traditional laparoscopy [45, 46]. Importantly, these studies included left-sided colon and rectal tumors. Although small in size, these randomized trials show equivalence in operative outcomes and oncologic adequacy compared to multi-port laparoscopy.
Conclusions
The overarching theme in the currently available SILS literature is that SILS is safe in select patients when performed by surgeons proficient in the technique. What is not clear is what constitutes a “select patient,” and surgeon experience may be the major factor. Much of the data is retrospective, contains bias, and represents sound clinical judgment with regard to patient and case selection by experienced surgeons. There is a need for large-scale randomized controlled trials before non-inferiority, let alone superiority, to traditional laparoscopy can be definitively demonstrated. Nevertheless, the available data does seem to support the safety and feasibility of SILS across diverse patient populations in the appropriate hands.
Early on in one’s experience, it may be prudent for a surgeon to first select patients without prior abdominal operations, low BMI, small tumors, and noninflammatory disease, as these factors undoubtedly affect the complexity of the surgery. The type of surgical procedure is also important to consider early in a surgeon’s experience. One should first select procedures that they have substantial experience and familiarity with that are relatively straightforward, such as right hemicolectomy or ileocecectomy. However, as more experience is gained with the SILS approach it can be safely performed on essentially any patient who is eligible for the more traditional minimally invasive approaches.
Ultimately the surgeon must perform an honest appraisal of their experience, abilities and comfort with a given procedure, evaluate the patient in front of them, and choose an approach that is best suited for each individual case. Above all, the surgeon should not sacrifice doing the correct operation in favor of a particular surgical approach.
References
Clinical Outcomes of Surgical Therapy Study Group, Nelson H, Sargent DJ, Wieand HS, Fleshman J, Anvari M, Stryker SJ, Beart RW Jr, Hellinger M, Flanagan R Jr, Peters W, Ota D. A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med [Internet]. 2004 [cited 2014 May 8];350(20):2050–9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/15141043.
Green BL, Marshall HC, Collinson F, Quirke P, Guillou P, Jayne DG, et al. Long-term follow-up of the Medical Research Council CLASICC trial of conventional versus laparoscopically assisted resection in colorectal cancer. Br J Surg [Internet]. 2013 [cited 2014 Mar 22];100(1):75–82. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23132548.
Bucher P, Pugin F, Morel P. Single port access laparoscopic right hemicolectomy. Int J Colorectal Dis [Internet]. 2008 [cited 2015 Sep 14];23(10):1013–6. Available from: http://www.ncbi.nlm.nih.gov/pubmed/18607608.
Haas EM, Nieto J, Ragupathi M, et al. Critical appraisal of learning curve for single incision laparoscopic right colectomy. Surg Endosc 2013;27:4499–503.
Hopping JR, Bardakcioglu O. Single-port laparoscopic right hemicolectomy: the learning curve. JSLS [Internet] 2013;17(2):194–7. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3771784&tool=pmcentrez&rendertype=abstract.
Rijcken E, Mennigen R, Argyris I, Senninger N, Bruewer M. Single-incision laparoscopic surgery for ileocolic resection in Crohn’s disease. Dis Colon Rectum [Internet]. 2012 [cited 2015 Sep 12];55(2):140–6. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22228156.
Geisler D, Garrett T. Single incision laparoscopic colorectal surgery: a single surgeon experience of 102 consecutive cases. Tech Coloproctol [Internet]. 2011 [cited 2015 Sep 16];15(4):397–401. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21887555.
Miller S, Causey MW, Damle A, Maykel J, Steele S. Single-incision laparoscopic colectomy: training the next generation. Surg Endosc [Internet]. 2013 [cited 2015 Sep 16];27(5):1784–90. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23389059.
Remzi FH, Kirat HT, Geisler DP. Laparoscopic single-port colectomy for sigmoid cancer. Tech Coloproctol [Internet]. 2010 [cited 2015 Sep 16];14(3):253–5. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19953288.
Rieger NA, Lam FF. Single-incision laparoscopically assisted colectomy using standard laparoscopic instrumentation. Surg Endosc [Internet]. 2010 [cited 2015 Sep 16];24(4):888–90. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19760335.
Ross H, Steele S, Whiteford M, Lee S, Albert M, Mutch M, et al. Early multi-institution experience with single-incision laparoscopic colectomy. Dis Colon Rectum [Internet]. 2011 [cited 2015 Sep 16];54(2):187–92. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21228667.
Champagne BJ, Papaconstantinou HT, Parmar SS, Nagle DA, Young-Fadok TM, Lee EC, et al. Single-incision versus standard multiport laparoscopic colectomy: a multicenter, case-controlled comparison. Ann Surg [Internet]. 2012 [cited 2015 Sep 11];255(1):66–9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22104563.
Moftah M, Nazour F, Cunningham M, Cahill RA. Single port laparoscopic surgery for patients with complex and recurrent Crohn’s disease. J Crohn’s Colitis [Internet]. European Crohn’s and Colitis Organisation. 2014;8(9):1055–61. Available from: http://dx.doi.org/10.1016/j.crohns.2014.02.003.
Olson CH, Bedros N, Hakiman H, Araghizadeh FY. Single-site laparoscopic surgery for inflammatory bowel disease. JSLS [Internet]. 2014 [cited 2015 Sep 12];18(2):258–64. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=4035637&tool=pmcentrez&rendertype=abstract.
Rizzuto A, Lacamera U, Ulrich F, Sacco R. Single incision laparoscopic resection for diverticulitis. Int J Surg [Internet]. Elsevier Ltd; 2015;19:11–4. Available from: http://dx.doi.org/10.1016/j.ijsu.2015.05.012.
Vestweber B, Vestweber K-H, Paul C, Rink AD. Single-port laparoscopic resection for diverticular disease: experiences with more than 300 consecutive patients. Surg Endosc [Internet]. 2015;30:50. Available from: http://springerlink.bibliotecabuap.elogim.com/10.1007/s00464-015-4160-7.
Nguyen HML, Causey MW, Steele SR, Maykel JA. Single-port laparoscopic diverting sigmoid colostomy. Dis Colon Rectum [Internet]. 2011 [cited 2015 Sep 25];54(12):1585–.8. : Available from: http://www.ncbi.nlm.nih.gov/pubmed/22067189.
Qadan M, Akça O, Mahid SS, Hornung CA, Polk HC. Perioperative supplemental oxygen therapy and surgical site infection: a meta-analysis of randomized controlled trials. Arch Surg [Internet]. 2009 [cited 2015 Sep 25];144(4):359–66. discussion 366–7. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19380650.
Makino T, Trencheva K, Shukla PJ, et al. The influence of obesity on short- and long-term outcomes after laparoscopic surgery for colon cancer: a case-matched study of 152 patients. Surgery 2014;156:661–8.
Cai Y, Zhou Y, Li Z, et al. Surgical outcome of laparoscopic colectomy for colorectal cancer in obese patients: a comparative study with open colectomy. Oncol Lett 2013;6:1057–62.
Poulsen M, Ovesen H. Is laparoscopic colorectal cancer surgery in obese patients associated with an increased risk? Short-term results from a single center study of 425 patients. J Gastrointest Surg2012;16:1554–8.
Krane M. K., Allaix M. E., Zoccali M., et al. Does morbid obesity change outcomes after laparoscopic surgery for inflammatory bowel disease? review of 626 consecutive cases. Journal of the American College of Surgeons. 2013;216(5):986–996.
Hardiman K, Chang ET, Diggs BS, et al. - Laparoscopic colectomy reduces morbidity and mortality in obese patients. Surg Endosc. 2013;27:2907–10.
Fung AKY, Aly EH. Systematic review of single-incision laparoscopic colonic surgery. Br J Surg. 2012;99:1353–64.
Makino T, Milsom JW, Lee SW. Feasibility and safety of single-incision laparoscopic colectomy: a systematic review. Ann Surg [Internet]. 2012 [cited 2015 Sep 16];255(4):667–76. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22258065.
Chen WT-L, Chang S-C, Chiang H-C, Lo W-Y, Jeng L-B, Wu C, et al. Single-incision laparoscopic versus conventional laparoscopic right hemicolectomy: a comparison of short-term surgical results. Surg Endosc [Internet]. 2011 [cited 2014 May 25];25(6):1887–92. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21359907.
Keller DS, Ibarra S, Flores-Gonzalez JR, Ponte OM, Madhoun N, Pickron TB, et al. Outcomes for singleincision laparoscopic colectomy surgery in obese patients: A case-matched study. Surg Endosc. 2016;30:739–44.
Aytac E, Turina M, Gorgun E, Stocchi L, Remzi FH, Costedio MM. Single-port laparoscopic colorectal resections in obese patients are as safe and effective as conventional laparoscopy. Surg Endosc [Internet]. 2014 [cited 2015 Sep 16];28(10):2884–9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24853841.
Milsom JW, Hammerhofer KA, Böhm B, Marcello P, Elson P, Fazio VW. Prospective, randomized trial comparing laparoscopic vs. conventional surgery for refractory ileocolic Crohn’s disease. Dis Colon Rectum [Internet]. 2001 [cited 2015 Sep 11];44(1):1–8. discussion 8–9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/11805557.
Maartense S, Dunker MS, Slors JFM, Cuesta MA, Pierik EGJM, Gouma DJ, et al. Laparoscopic-assisted versus open ileocolic resection for Crohn’s disease: a randomized trial. Ann Surg [Internet]. 2006 [cited 2015 Aug 25];243(2):143–9. discussion 150–3. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=1448907&tool=pmcentrez&rendertype=abstract.
Gash KJ, Goede AC, Kaldowski B, Vestweber B, Dixon AR. Single incision laparoscopic (SILS) restorative proctocolectomy with ileal pouch-anal anastomosis. Surg Endosc [Internet]. 2011 [cited 2015 Sep 12];25(12):3877–80. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21761270.
Boni L, Dionigi G, Cassinotti E, Di Giuseppe M, Diurni M, Rausei S, et al. Single incision laparoscopic right colectomy. Surg Endosc [Internet]. 2010 [cited 2015 Sep 14];24(12):3233–6. Available from: http://www.ncbi.nlm.nih.gov/pubmed/20464415.
Keshava A, Mackenzie S, Al-Kubati W. Single-port laparoscopic right colonic resection. ANZ J Surg [Internet]. 2010 [cited 2015 Sep 14];80(1–2):30–2. Available from: http://www.ncbi.nlm.nih.gov/pubmed/20575877.
O’Connor DJ, Feinberg E, Jang J, Vemulapalli P, Camacho D. Single-incision laparoscopic-assisted right colon resection for cancer. JSLS [Internet]. 2010 [cited 2015 Sep 14];14(4):558–60. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3083049&tool=pmcentrez&rendertype=abstract.
Ramos-Valadez DI, Patel CB, Ragupathi M, Bartley Pickron T, Haas EM. Single-incision laparoscopic right hemicolectomy: safety and feasibility in a series of consecutive cases. Surg Endosc [Internet]. 2010 [cited 2015 Sep 14];24(10):2613–6. Available from: http://www.ncbi.nlm.nih.gov/pubmed/20364353.
Adair J, Gromski MA, Lim RB, Nagle D. Single-incision laparoscopic right colectomy: experience with 17 consecutive cases and comparison with multiport laparoscopic right colectomy. Dis Colon Rectum [Internet]. 2010 [cited 2015 Sep 14];53(11):1549–54. Available from: http://www.ncbi.nlm.nih.gov/pubmed/20940605.
Lim YK, Ng KH, Eu KW. Single site laparoscopic right hemicolectomy: an oncological feasible option. World J Surg Oncol [Internet]. 2010 [cited 2015 Sep 14];8:79. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=2945348&tool=pmcentrez&rendertype=abstract.
Pietrasanta D, Romano N, Prosperi V, Lorenzetti L, Basili G, Goletti O. Single-incision laparoscopic right colectomy for cancer: a single-centre preliminary experience. Updates Surg [Internet]. 2010 [cited 2015 Sep 14];62(2):111–5. Available from: http://www.ncbi.nlm.nih.gov/pubmed/20872107.
Waters JA, Guzman MJ, Fajardo AD, Selzer DJ, Wiebke EA, Robb BW, et al. Single-port laparoscopic right hemicolectomy: a safe alternative to conventional laparoscopy. Dis Colon Rectum [Internet]. 2010 [cited 2015 Sep 14];53(11):1467–72. Available from: http://www.ncbi.nlm.nih.gov/pubmed/20940593.
Wong MTC, Ng KH, Ho KS, Eu KW. Single-incision laparoscopic surgery for right hemicolectomy: our initial experience with 10 cases. Tech Coloproctol [Internet]. 2010 [cited 2015 Sep 14];14(3):225–8. Available from: http://www.ncbi.nlm.nih.gov/pubmed/20589521.
Papaconstantinou HT, Sharp N, Thomas JS. Single-incision laparoscopic right colectomy: a case-matched comparison with standard laparoscopic and hand-assisted laparoscopic techniques. J Am Coll Surg [Internet]. 2011 [cited 2015 Sep 14];213(1):72–.80 ; discussion 80–2. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21420878.
Waters JA, Rapp BM, Guzman MJ, Jester AL, Selzer DJ, Robb BW, et al. Single-port laparoscopic right hemicolectomy: the first 100 resections. Dis Colon Rectum [Internet]. 2012 [cited 2015 Sep 14];55(2):134–9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22228155.
Chew M-H, Chang M-H, Tan W-S, Wong MT-C, Tang C-L. Conventional laparoscopic versus single-incision laparoscopic right hemicolectomy: a case cohort comparison of short-term outcomes in 144 consecutive cases. Surg Endosc [Internet]. 2013 [cited 2015 Sep 14];27(2):471–7. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22806522.
Bulut O, Nielsen CB, Jespersen N. Single-port access laparoscopic surgery for rectal cancer: initial experience with 10 cases. Dis Colon Rectum [Internet]. 2011 [cited 2015 Sep 14];54(7):803–9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21654246.
Huscher CG, Mingoli A, Sgarzini G, Mereu A, Binda B, Brachini G, et al. Standard laparoscopic versus single-incision laparoscopic colectomy for cancer: early results of a randomized prospective study. Am J Surg [Internet]. 2012 [cited 2015 Sep 14];204(1):115–20. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22178484.
Poon JTC, Cheung C-W, Fan JKM, Lo OSH, Law W-L. Single-incision versus conventional laparoscopic colectomy for colonic neoplasm: a randomized, controlled trial. Surg Endosc [Internet]. 2012 [cited 2015 Sep 14];26(10):2729–34. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22538676.
Lee TH, et al. Derivation and prospective validation of a simple index for prediction of cardiac risk of major noncardiac surgery. Circulation. 1999;100(10):1043–9.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Electronic Supplementary Material
Lighted ureteric stent in the left ureter (Courtesy of Scott R. Steele, MD) (MP4 35428 kb)
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG
About this chapter
Cite this chapter
Bingham, J., Steele, S.R. (2018). Patient Selection and General Patient Considerations. In: Geisler, D., Keller, D., Haas, E. (eds) Operative Techniques in Single Incision Laparoscopic Colorectal Surgery. Springer, Cham. https://doi.org/10.1007/978-3-319-63204-9_2
Download citation
DOI: https://doi.org/10.1007/978-3-319-63204-9_2
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-63202-5
Online ISBN: 978-3-319-63204-9
eBook Packages: MedicineMedicine (R0)