Abstract
Background: A type II odontoid fracture, if unstable, can cause spinal cord damage. In this case, it is essential to choose the correct treatment—but the issues of what the correct treatment is and which of the different surgical options is best are quite controversial. In this paper we present strategies for treatment of type II odontoid fracture.
Materials and Methods: Thirty consecutive cases of type II odontoid fracture were treated at the Division of Neurosurgery at Villa Sofia Hospital in Palermo (23 cases) and at the Neurosurgical Clinic, University Hospital of Palermo (seven cases), from January 2011 to August 2016. Four patients were treated with external immobilization. Twenty-six patients underwent a surgical procedure.
Results: There was no mortality related to the surgical procedure. One patient had a pre- and postoperative neurological deficit, and remained tetraparetic. Follow-up radiological studies in the surgically treated group showed bone union in 21 patients and stable fibrous union in one.
Conclusion: In our and other authors’ experience, when the direction of the fracture line is down and forward, external immobilization can be sufficient for healing. Anterior odontoid screw fixation can be considered the treatment of choice for unstable odontoid fractures (with a horizontal, down and back, or comminuted fracture line) without dislocation or with dislocation less than 7 mm.
When the odontoid fracture is associated with a Jefferson fracture or dislocation greater than 7 mm, stabilization of C1–C2 may be necessary. In this case, placement of screws in the dens and in the joints through a single approach represents the most valid technique.
In the case of an inveterate fracture of the dens with severe C1–C2 dislocation, the surgical operation that offers the best prospects is posterior stabilization, utilizing the Guo technique.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Odontoid fractures represents about 20% of all cervical fractures. Of these, the Anderson and d’Alonzo type II fracture (on the base of the dens) is the most common, occurring in more than 60% of cases; when it is unstable, it can cause spinal cord damage. In this case, it is essential to choose the correct treatment [1,2,3]—but the issues of what the correct treatment is and which of the surgical options is best are quite controversial [4,5,6,7]. We present a strategy for treatment of type II odontoid fractures.
Materials and Methods
Thirty consecutive cases of type II odontoid fracture were treated at the Neurosurgery Division of Villa Sofia Hospital in Palermo (23 cases) and at the Neurosurgical Clinic, University Hospital of Palermo (seven cases), from January 2011 to August 2016. There were 19 males and 11 females. The median age was 58.3 years (range 12–89 years). The direction of the fracture line was oblique, down and forward without dislocation in four patients, and they were treated with external immobilization (a sternal–occipital–mandibular immobilizer [SOMI] brace). In 18 cases the fractured dens had no dislocation or had a dislocation less than 7 mm (the direction of the fracture line was horizontal in six cases and oblique, down and back in 12 cases), and they were treated with odontoid screw fixation. The fractured dens was associated with a Jefferson fracture in two cases and with a dislocation greater than 7 mm in five patients. These seven patients were treated with anterior screw fixation of the dens and bilateral C1–C2 anterior transarticular screw fixation. Finally, one patient had an inveterate odontoid fracture with severe lateral C1–C2 luxation and was treated with manual reduction followed by posterior stabilization utilizing the Guo technique (bilateral C1–C2 transarticular screws, C1 laminar hook fixation and bone graft fusion). Clinical and radiological follow-up was performed in all but three of the patients.
Results
The follow-up of the patients ranged from 4 months to 5 years. In the conservatively treated group, bone fusion was observed in three patients and fibrous union in one. In the surgically treated group there were no deaths except for one woman in a coma due to a severe head injury, who died from pneumonia after 40 days. One patient, who had an inveterate fracture, had a pre- and postoperative neurological deficit and remained tetraparetic. In the early postoperative period, 11 patients experienced mild dysphagia, which required no treatment beyond dietary modification. In the patients undergoing surgery, radiological studies showed bone union in 21 patients and stable fibrous union in one.
Case Illustration
Case 1
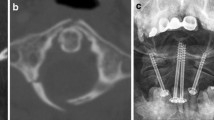
This 17-year-old boy sustained a head and neck injury in a diving accident. No neurological deficit was noted. A computed tomography (CT) scan showed a type II odontoid fracture. The direction of the fracture line was oblique, down and back without dislocation. He was treated with odontoid screw fixation. A postoperative CT scan demonstrated correct placement of the screw (Fig. 1). One year later, dynamic radiography showed no dislocation, and bone fusion was evident.
Case 2
This 75-year-old man sustained a head and neck injury in an accidental fall from body height. The neurological examination was normal. A CT scan disclosed a type II odontoid fracture, with the direction of the fracture line being oblique down and back, with 10-mm posterior dislocation of the fractured dens and of the C1 joint facets with respect to C2. The patient underwent manual reduction under the guidance of image intensification. A subsequent CT scan showed good alignment of the fracture and of the joint facets; therefore, anterior screw fixation of the odontoid fracture and of the bilateral C1–C2 joints was performed. A postoperative CT scan showed correct placement of the screws (Fig. 2). In the first 10 days the patient had slight dysphagia. At follow-up after 9 months a CT scan documented bone fusion of the fracture.
Computed tomography (CT) scan on admission, showing an odontoid fracture with 10-mm posterior dislocation of the fractured dens and of the C1 articular facet with respect to C2 (a, b). CT reconstruction after manual reduction, demonstrating good alignment (c, d). Postoperative three-dimensional CT scan (e)
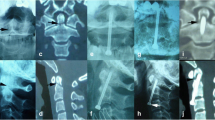
Case 3
This 68-year-old man presented with immediate tetraparesis after mild cervical trauma. He stated that he had experienced neck pain after a head injury 5 months earlier. A neuroradiological study showed an inveterate odontoid fracture with severe lateral C1–C2 dislocation. The patient underwent manual reduction under the guidance of image intensification. A CT scan showed good alignment of the fractured dens and of the C1–C2 articular facets. Posterior stabilization with the Guo technique (bilateral C1–C2 transarticular screws, C1 laminar hook fixation and bone graft fusion) was performed. A postoperative x-ray and CT scan showed the alignment of C1–C2 and correct placement of the implant system (Fig. 3). At follow-up after 6 months, the patient’s neurological deficits were unchanged and a CT scan documented bone union in relation to the bone graft.
Discussion
Type II odontoid fractures in young people tend to be due to high-energy trauma, but in the elderly population they can occur through low-impact mechanisms because the dens becomes significantly less robust with age. Some of these fractures can be considered unstable, with a risk of spinal cord damage. But when exactly can this fracture be considered unstable? On the basis of studies by Roy-Camille et al. [8] and clinical experiences at the Hôpital Pitié-Salpêtrière in Paris [9], we agree that type II odontoid fractures are unstable and need surgical treatment when they are (1) horizontal, (2) oblique down and back, or (3) comminuted. Therefore, in these cases—and if the fractured dens is not dislocated or is dislocated by less than 5 mm—it is essential to choose the correct treatment, and this issue is quite controversial [4,5,6]. Conservative treatment with use of external immobilization (a halo vest, SOMI brace or cervical collar) guarantees fusion of the fracture in only a small proportion of patients—particularly in elderly patients—with a risk of dislocation and spinal cord compression [1]. Some authors have reported deaths due to cardiopulmonary compromise in elderly patients with odontoid fractures treated with halo vest immobilization. For these reasons there is a trend for many of these cases to be treated surgically [1, 10]. Posterior cervical fusion has historically been the first option for patients with odontoid fractures and for patients with C1–C2 instability. One of the earliest types of fixation for C1–C2 fusion was described by Gallie. It involved fixation of the posterior arch of C1 and of the lamina or spinous process of C2, using a cerclage wire technique with an onlay bone graft, but the failure rate was high. A modification of this technique by Brooks [11] also had limited success, with a 30% failure rate. Also, use of Halifax clamps with C1 and C2 laminar hooks, united by screws, had a 30% failure rate [12]. These discouraging results prompted research into new approaches; therefore, since the early 1980s, other techniques have been devised for treatment of odontoid fracture and C1–C2 instability.
In 1982, Bohler [13] presented the surgical technique of anterior screw fixation of odontoid fractures. This is an osteosynthetic technique that provides immediate stability, promotes healing and may preserve C1–C2 rotational motion. It also offers several advantages, including reduction of soft tissue trauma, a decreased risk of vertebral artery injury, lack of requirement for bone grafting, a shorter operating time and a shorter hospital stay. The most significant complication is represented by dysphagia. Use of this technique may not be possible in patients with a barrel-shaped chest, a short neck and impossibility of extending the neck. The fusion rate, using this technique, is 81–90%. In 1986, Magerl [14] proposed a new technique for C1–C2 fusion, using posterior transarticular screws associated with cerclage wiring and bone graft. With this technique a 90–100% fusion rate was achieved. Later, similar results were reported with use of posterior transarticular screws without cerclage wiring and bone grafting, avoiding the risks of passage of sublaminar wire and of graft migration [15]. However, insertion of posterior screws can be difficult or impossible in anatomical conditions such as a narrow pars interarticularis or a high-riding foramen transversarium, which places the vertebral artery at high risk of injury. This technique also carries risks of spinal cord and vertebral artery injury, screw breakage and infection. In 2001, Harms [16] presented a technique of C1–C2 fixation with bilateral insertion of polyaxial-head screws into the lateral mass of C1 and into the pedicle of C2, with rod fixation; with this technique it is also possible to treat irreducible fractures with a 100% fusion rate. But, of course, this is also a technically demanding operation. The most recently presented technique for posterior stabilization of C1–C2 was published in 2014 by Guo et al. [17]: use of bilateral C1–C2 transarticular screws with C1 laminar hook fixation and bone graft fusion. This operation is more advantageous than the Magerl technique because it avoids sublaminar passage of wiring, and it is more advantageous than the Harms technique because it provides three-point fixation instead of two-point fixation. The risks and technical difficulty of C1–C2 posterior stabilization had stimulated surgeons to research an easier and less dangerous approach to treat C1–C2 instability, so the surgical technique of C1–C2 anterior transarticular screw fixation has been disseminated [18,19,20]. This technique offers several advantages: the positioning of the patient is much simpler; the surgical approach is less traumatic with a lower infection rate; and the risks of spinal cord and vertebral artery injury are lower. The good clinical results achieved with this technique have been confirmed by a biomechanical study published by Sen et al. [21], who demonstrated that there was not a large difference in the strength of C1–C2 fixation between use of anterior transarticular screws and use of posterior transarticular screws alone. Furthermore, when C1–C2 instability is combined with odontoid fractures, treatment of both can be done through a single anterior approach. But what causes C1–C2 instability? Current opinions cite transverse ligament injury, odontoid fracture dislocation greater than 5 mm and associated fractures of C1 and C2, while less importance or attention is given to C1–C2 joint injury. The physiological C1–C2 range of motion in flexion and extension is minimal—only 13 grades—and occurs on the sagittal plane without loss of alignment of the articular facets. So is C1–C2 joint integrity conceivable if the dislocation of the fractured odontoid process is greater than 7 mm? Moreover, can it be speculated that dislocation of the fractured odontoid process, which sometimes exceeds 1 cm, happens without slippage of both C1 lateral masses forward or backward with respect to the C2 facets and without capsular ligament injury? As shown in Fig. 4, T2-weighted magnetic resonance imaging (MRI) performed in case 2 showed high signal intensity of the tissues posterior to the C1–C2 joints, expression of distension and rupture of the capsular ligaments. Therefore, C1–C2 joint instability in odontoid fractures is an underestimated event, in our opinion. Unrecognized C1–C2 joint instability could be the cause of some failures of odontoid screw fixation: non-union, breakage of the anterior portion of the C2 vertebral body, and screw breakage.
Therefore, if the dislocation of the fractured dens is greater than 7 mm, an accurate CT reconstruction of the joints can reveal C1–C2 subluxation, and MRI can reveal distension and rupture of the capsular ligaments of the C1–C2 joints. In this case, odontoid screw fixation alone may be insufficient and stabilization C1–C2 may be necessary. Moreover, in cases of inveterate fracture of the dens with severe C1–C2 dislocation, as in our patient, the surgical operation that offers the best prospects is posterior stabilization according to the Guo technique [17]. In fact, in such cases, screw placement in the dens cannot cause bone fusion and healing for the interposition of fibrous tissue in the rims of an ancient fracture, and anterior or posterior transarticular screws may be insufficient for healing, whereas the Guo technique, involving three-point fixation, may be an appropriate treatment.
The numbers in the present case series are too small to permit us to affirm that our treatment strategy is definitely effective. However, the results we achieved appear to indicate that this is a promising direction. Moreover, the 7-mm cut-off point for dislocation of the fracture and of the C1–C2 articular facets that we have considered as a boundary for deciding between more simple odontoid screw fixation and anterior placement of screws in the dens and the C1–C2 articular facets could be too low. But to solve this question, more studies will be necessary.
Conclusion
Despite the frequency of type II odontoid fracture, the most appropriate treatment is still a matter of discussion. In our and other authors’ experiences, when the direction of the fracture line is down and forward, external immobilization can be sufficient for healing. For us, anterior odontoid screw fixation can be considered the treatment of choice for unstable odontoid fractures (with a horizontal, down and back, or comminuted fracture line) without dislocation or with dislocation less than 7 mm.
In our opinion, the presence of C1–C2 joint injury in odontoid fractures is underestimated, and this could be the cause of some failures of anterior odontoid screw fixation. Therefore, when an odontoid fracture is associated with C1–C2 dislocation greater than 7 mm, stabilization of C1–C2 could be necessary. C1–C2 instability is now commonly treated with posterior screw fixation, but these technically demanding operations can be limited by anatomical conditions and carry severe risks. Therefore, we—like many authors—think that C1–C2 anterior transarticular screws can be considered an effective alternative procedure. However, if C1–C2 instability is associated with a type II odontoid fracture, screw placement in the dens and in the joints through a single approach represents the most valid technique.
Finally, in cases of inveterate fracture of the dens with severe C1–C2 dislocation, the surgical operation that offers the best prospects is posterior stabilization utilizing the Guo technique. To date there is insufficient evidence to establish a standard or guideline for odontoid fracture management [6]. A randomized trial or serial case–control studies will be necessary. Our work must be considered preliminary, and other studies are necessary to confirm this treatment strategy.
References
Dailey AT, Hart D, Finn MA, Schmidt MH, Apfelbaum RI. Anterior fixation of odontoid fractures in an elderly population. J Neurosurg Spine. 2010;12(1):1–8. https://doi.org/10.3171/2009.7.SPINE08589.
Di Paolo A, Piccirilli M, Pescatori L, Santoro A, D’Elia A. Single institute experience on 108 consecutive cases of type II odontoid fractures: surgery versus conservative treatment. Turk Neurosurg. 2014;24(6):891–6. https://doi.org/10.5137/1019-5149.JTN.9731-13.0.
Joaquim AF, Ghizoni E, Tedeschi H, Yacoub AR, Brodke DS, Vaccaro AR, Patel AA. Upper cervical injuries: clinical results using a new treatment algorithm. J Craniovertebr Junction Spine. 2015;6(1):16–20. https://doi.org/10.4103/0974-8237.151585.
Denaro V, Papalia R, Di Martino A, Denaro L, Maffulli N. The best surgical treatment for type II fractures of the dens is still controversial. Clin Orthop Relat Res. 2011;469(3):742–50. https://doi.org/10.1007/s11999-010-1677-x.
Joaquim AF, Patel AA. Surgical treatment of type II odontoid fractures: anterior odontoid screw fixation or posterior cervical instrumented fusion? Neurosurg Focus. 2015;38(4):E11. https://doi.org/10.3171/2015.1.FOCUS14781.
Julien TD, Frankel B, Traynelis VC, Ryken TC. Evidence-based analysis of odontoid fracture management. Neurosurg Focus. 2000;8(6):e1.
Tian NF, Hu XQ, Wu LJ, Wu XL, Wu YS, Zhang XL, Wang XY, Chi YL, Mao FM. Pooled analysis of non-union, re-operation, infection, and approach related complications after anterior odontoid screw fixation. PLoS One. 2014;9(7):e103065. https://doi.org/10.1371/journal.pone.0103065.
Roy-Camille R, Saillant G, Judet T, de Botton G, Michel G. Factors of severity in the fractures of the odontoid process (author’s transl). Rev Chir Orthop Reparatrice Appar Mot. 1980;66(3):183–6.
Steltzlen C, Lazennec JY, Catonné Y, Rousseau MA. Unstable odontoid fracture: surgical strategy in a 22-case series, and literature review. Orthop Traumatol Surg Res. 2013;99(5):615–23. https://doi.org/10.1016/j.otsr.2013.02.007.
Fountas KN, Kapsalaki EZ, Karampelas I, Feltes CH, Dimopoulos VG, Machinis TG, Nikolakakos LG, Boev AN, Choudhri H, Smisson HF, Robinson JS. Results of long-term follow-up in patients undergoing anterior screw fixation for type II and rostral type III odontoid fractures. Spine (Phila Pa 1976). 2005;30(6):661–9.
Brooks AL, Jenkins EB. Atlanto-axial arthrodesis by the wedge compression method. J Bone Joint Surg Am. 1978;60(3):279–84.
Statham P, O’Sullivan M, Russell T. The Halifax interlaminar clamp for posterior cervical fusion: initial experience in the United Kingdom. Neurosurgery. 1993;32(3):396–9.
Böhler J. Anterior stabilization for acute fractures and non-unions of the dens. J Bone Joint Surg Am. 1982;64(1):18–27.
Magerl F, Seeman PS. Stable posterior fusion of the atlas and axis by transarticular screw fixation. In: Cervical spine. Vienna: Springer; 1986. p. 312–27.
Gleizes V, Jacquot FP, Signoret F, Feron JM. Combined injuries in the upper cervical spine: clinical and epidemiological data over a 14-year period. Eur Spine J. 2000;9(5):386–92.
Harms J, Melcher RP. Posterior C1–C2 fusion with polyaxial screw and rod fixation. Spine (Phila Pa 1976). 2001;26(22):2467–71.
Guo X, Ni B, Xie N, Lu X, Guo Q, Lu M. Bilateral C1–C2 transarticular screw and C1 laminar hook fixation and bone graft fusion for reducible atlantoaxial dislocation: a seven-year analysis of outcome. PLoS One. 2014;9(1):e87676. https://doi.org/10.1371/journal.pone.0087676.
Apostolides PJ, Theodore N, Karahalios DG, Sonntag VK. Triple anterior screw fixation of an acute combination atlas–axis fracture. Case report. J Neurosurg. 1997;87(1):96–9.
Etter C. Combined anterior screw fixation of an odontoid fracture and the atlanto-axial joints (C1/C2) in a geriatric patient. Eur Spine J. 2016;25(Suppl 2):280–4. https://doi.org/10.1007/s00586-016-4625-y.
Reindl R, Sen M, Aebi M. Anterior instrumentation for traumatic C1–C2 instability. Spine (Phila Pa 1976). 2003;28(17):E329–33.
Sen MK, Steffen T, Beckman L, Tsantrizos A, Reindl R, Aebi M. Atlantoaxial fusion using anterior transarticular screw fixation of C1–C2: technical innovation and biomechanical study. Eur Spine J. 2005;14(5):512–8.
Competing Interests
The authors declare that they have no competing interests.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Ethics declarations
No financial support was received for this work.
Rights and permissions
Copyright information
© 2019 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Fiumara, E. et al. (2019). Type II Odontoid Fracture: a case series highlighting the treatment strategies. In: Visocchi, M. (eds) New Trends in Craniovertebral Junction Surgery. Acta Neurochirurgica Supplement, vol 125. Springer, Cham. https://doi.org/10.1007/978-3-319-62515-7_46
Download citation
DOI: https://doi.org/10.1007/978-3-319-62515-7_46
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-62514-0
Online ISBN: 978-3-319-62515-7
eBook Packages: MedicineMedicine (R0)