Abstract
Immunohistochemical techniques are pivotal tools for achieving a correct diagnosis in both the histological and cytological fields and in predicting the clinical course of the disease. Immunohistochemical stainings are helpful in identifying the nature of the cells composing the thyroid neoplasms, especially those arising primarily in the gland. Some antibodies (defined as markers of malignancy, among which Hector Battifora mesothelial (HBME)-1, galectin-3, and cytokeratin 19 are the most effective) are expressed only in malignant follicular cells allowing the differential diagnosis between benign and malignant tumors. From the prognostic viewpoint, some antibodies such as connective tissue growth factor (CTGF), metalloprotease 2, caspase 3, and CD56 (NCAM) are especially expressed in differentiated carcinomas pursuing an unfavorable course. Analogously, CSC (cancer stem cell) markers, beta-catenin, and FOX A-1 are expressed in poorly differentiated and undifferentiated carcinomas which do not respond to the radioiodine treatment. Finally, some antibodies directed toward mutated genes may be used for identifying those patients who present the gene mutation and thus are candidates to a treatment with targeted drugs.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
1 Introduction
Thyroid neoplasms represent the first endocrine tumors with an incidence of 8.7 cases/100,000 people per year in Europe although its overall mortality rate is less than 0.1% of all tumor cases [1, 2].
The classification of thyroid neoplasms [3] includes benign and malignant epithelial tumors, the latter being derived either from the follicular cells or from the parafollicular C cells. Papillary thyroid carcinoma (PTC) is the most frequent tumor type, accounting for almost 90% of all thyroid tumors, and usually it pursues a favorable course characterized by frequent nodal spreading though uncommon distant metastatic spread. PTC encompasses two main tumor variants: classic and follicular. The former exhibits the distinctive papillary structures from which the name derives, while the histological hallmark of the latter is the predominant microfollicular pattern. Regardless of the structure, the diagnosis of papillary carcinoma relies upon the distinctive nuclear features (clearing, elongation, and pseudoinclusions) which can be detected in all histotypes.
Some cases of PTC show an obvious infiltration of either the capsule or the adjacent vessels which witnesses the malignant nature of the tumor. However, some cases do not show aggressive features so that the histological definition of carcinoma can be questionable.
The field of epithelial tumors encompasses also the follicular thyroid carcinoma (FTC), which accounts for about 5% of all thyroid malignant tumors. It is characterized by a follicular pattern made up of follicular cells (thyrocytes) showing variably pleomorphic and dark nuclei. The distinction between FTC and its benign counterpart (follicular adenoma, FA) relies upon the detection of histologic parameters of aggressiveness, notably capsular and vascular invasion. If only one of such features is observed in a follicular-patterned neoplasm, the diagnosis of follicular carcinoma is warranted. The same diagnostic parameters of malignant evolution apply to tumors composed exclusively by Hurthle (or oxyphilic or oncocytic) cell carcinomas (HCC) which represent hypoxic changes of the thyrocytes. FTC and HCC are less likely to metastasize to regional nodes rather than to distant sites such as lungs and bones.
Less frequent carcinomas arising in the thyroid gland are poorly differentiated (PDTC, also called insular thyroid carcinoma) and undifferentiated (anaplastic, ATC) carcinomas. They represent no more than 3% of all thyroid tumors and pursue a less favorable course than the previous types. From the thyroid tissue, some other tumors may arise which are not of follicular derivation: the most important are medullary thyroid carcinoma (MTC) and primary malignant non-Hodgkin lymphoma (PML).
2 Immunochemistry in Follicular-Derived Tumors
Immunohistochemistry (IHC) has been introduced since the beginning of the 1970s in the routine pathology practice. It has been traditionally used in thyroid pathology for the identification of the cell origin in differentiated tumors arising in the gland or metastasizing outside it, such as thyroglobulin, calcitonin, or parathyroid hormone [4]. There are some tumor types which immunophenotyping deserves a more detailed discussion. Hyalinizing trabecular tumors (HTT) are uncommon neoplasms sharing with PTC some clinical and pathological features. In fact HTT exhibits a trabecular pattern with hyalinization of the stroma composed by thyrocytes showing nuclear pseudoinclusions resembling those of PTC, and in some cases, RET/PTC rearrangements have been identified [5, 6] . On the other hand, this tumor generally pursues a benign course with uncommon malignant forms [7]. Leonardo and coll. [8] have proposed an immunohistochemical method for differentiating HTT from PTC: the cytoplasmic expression of MIB-1 antibody, directed toward the cell-cycle protein Ki-67, instead of the usual nuclear expression of Ki-67 which is used as proliferative index in many tumors. The unusual experimental conditions (room temperature instead of 37 °C) and the strict histological criteria for diagnosing pure forms have somewhat hindered the diffusion of this diagnostic marker.
Hurthle cell tumors (or oxyphilic and oncocytic tumors, HCT) are usually included in the category of FTC although they do not share all its histological characteristics. Hurthle cells represent a different status of the follicular cells induced by either local hypoxia or hormone withdrawal: their morphology is quite distinctive as it shows large pleomorphic nuclei and abundant cytoplasms which, at the ultrastructural level, are engulfed with mitochondria. This unique cytoplasmic composition is responsible of the granular oxyphilic staining of the cytoplasms of HC and, at immunohistochemistry, of the mild nonspecific positivity of these cells for the majority of the IHC reactions. Thus, the real positivity of Hurthle cells should be assessed only in the presence of a strong expression in the majority of the cellular component (like thyroglobulin usually does) or when the antibody expression is mostly at the nuclear level (like thyroid transcription factor-1, TTF-1). The immunohistochemical stainings which are helpful in the other differentiated tumors (such as galectin-3, HBME-1, and cytokeratin 19; see below) provide controversial results in HCT and are regarded as unreliable to discriminate benign from malignant neoplasms. Some studies involving HCT have reported that some proliferative markers such as Ki-67 and cyclin D1 may be of help in this differential diagnosis [9]. A different approach to oncocytic tumors has been studied by Gasparre and coll. [10]. They have observed that the oncocytic metaplasia, originated by a marked increase of the mitochondrial component in the cytoplasm of the follicular cells, is often associated to a nonsense mutation of the ND-5 subunit of the respiratory chain complex I of the mitochondria. The expression of the human mitochondrial antibody (HMA) against this subunit reveals the presence of oncocytic cells, regardless of their malignant nature, in every lesion in which they are present. In this case, the HMA does not represent a marker of malignancy, but, nonetheless, this is an important parameter to take into account for a diagnosis of follicular-patterned neoplasm since oncocytic cells may sometimes be misdiagnosed as PTC cells. From a clinical viewpoint, the diagnosis of PTC does not need the presence of capsular or vascular invasion unlike the oncocytic carcinoma, which is diagnosed only when histological features of invasion are detected. Thus, the expression of HMA in a wholly encapsulated follicular neoplasm favors the diagnosis of benign oncocytic adenoma, whereas its negativity suggests a papillary carcinoma.
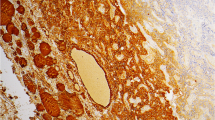
Anaplastic thyroid carcinoma is made up of highly undifferentiated cells which lose the distinctive immunophenotype of thyroid carcinoma, such as the expression of thyroglobulin (TGB) and the thyroid transcription factor-1 (TTF-1) (Figs. 1.1 and 1.2).
Thus, the diagnosis of ATC relies mainly on the cellular morphology with the nonspecific cytoplasm expression of low- and high-molecular-weight cytokeratins [11]. Another important diagnostic marker is p53 which is often overexpressed in the majority of nuclei of ATC and represents an important marker for this tumor since it is not present in differentiated and PDTC [12] (Fig. 1.3).
Although the decreasing frequency of ATC would not justify the introduction of specific antibodies for the undifferentiated cells, a study [13] has focused on the expression of some cancer stem cell markers (SOX-2, ABC, CXCR4, MRP-1, and LRP antibodies) in this tumor in respect to the differentiated carcinomas with the perspective of using these antibodies as prognostic or predictive markers (see also below).
3 Immunomarkers of Malignancy
One of the most puzzling problems in thyroid histological diagnosis is the differentiation between benign and malignant follicular-patterned neoplasms [14]. The traditional identification of features of aggressiveness of the tumor capsule and its surrounding structures (normal parenchyma, vessels, skeletal muscle) is the pivotal criterion on which this distinction is founded. Although some cases of papillary carcinoma do not exhibit the abovementioned features, nonetheless the nuclear features of PTC warrant a diagnosis of malignant tumor. However, a few cases of encapsulated lesions exhibiting a follicular structure either do not show the nuclear hallmark of PTC in a large amount of cells or display only focal nuclear clearing and irregularity which cannot allow a reliable diagnosis of malignancy. The introduction of the markers of malignancy, which may distinguish malignant from benign lesions irrespective of the histological features of carcinomatous transformation (especially capsular or vascular invasion), has represented a pillar of the morphologic diagnostics of thyroid cancer [15]. HBME-1 (Hector Battifora mesothelial-1) antigen, originally produced for being applied in the discrimination between mesothelioma and adenocarcinoma of the lung, has been one of the first antibodies to be used for the diagnosis of thyroid carcinoma [16]. Since then more than 20 antibodies have been tested with the perspective of overlooking the problem of the nuclear features of the thyrocytes. A meta-analysis by Correia Rodrigues and coll. [17] has evaluated the clinical results of 25 antibodies which have been tested in about 100 different studies on thyroid FNA, and similar findings were registered by Griffith and coworkers [15]. The most studied markers of malignancy are HBME-1, galectin-3, and cytokeratin 19. Apart from HBME-1, whose epitope in the microvilli of the mesothelial is still unknown, the others are well-characterized molecules: for example, galectin-3 is a member of the lectin family molecules which recognize and binds beta-galactoside residues in glycoproteins and glycolipids which have extensively been studied in histological and cytological samples [18,19,20]. Cytokeratin 19 is a low-molecular-weight intermediate filament of the cytoplasm which has also been extensively studied [21, 22].
Each of the abovementioned antibodies exhibits a characteristic expression pattern which may be helpful in some diagnostic settings. HBME-1 membranous staining is specific for the malignant thyrocytes and is often useful in identifying microcarcinomas as small as a few millimeters which are hardly detectable during t4e usual histological examination (Fig. 1.4).
Galectin-3 shows a strong cytoplasmic positivity which highlights the largest lesions as compared to the HBME-1 expression but may be detected in nonmalignant cells with clear cytoplasms: it also marks the wall of small vessels which can be used as internal positive controls. Cytokeratin 19 exhibits a strong cytoplasmic expression which emphasizes the presence of the neoplastic cells although the same staining may be detected also in benign thyrocytes [22]. Many studies have been undertaken concerning the reliability of each one of these antibodies in distinguishing benign from malignant neoplasms on both histological formalin-fixed paraffin-embedded (FFPE) sections and fine-needle aspiration biopsy material. The unanimous conclusion has been that no single antibody achieves such a high accuracy for being used in this crucial diagnostic task. Thus, the best combination of these antibodies, and others that will be mentioned below, has been investigated with the aim of harmonizing the high positive predictive value (PPV) of cytokeratin 19 and HBME-1 with the high negative predictive value (NPV) of galectin-3. According to the review of Griffith and coll. [15], the best results on FFPE sections were obtained with the panel made up of cytokeratin 19, galectin-3, and HBME-1 with different combinations of two of them. De Matos and coll. [23], in their large series of thyroid neoplasms, reported a good sensitivity (SE, 84–96.5%) and diagnostic accuracy (DA, 84.9%) for the combination of the three markers in the diagnosis of PTC, whereas the same parameters resulted significantly lower for FTC (63.1%). Similar results were obtained by Park and coll. [24], Scognamiglio and coll. [25], and Rossi and coll. [26] using different combinations of the abovementioned antibodies: they reported a diagnostic accuracy higher than 90%. Indeed, a recent paper by Nechifor-Boila and coll. [27] has investigated the accuracy of a panel made up of four antibodies (HBME-1, galectin-3, CK19, and CD56) in providing the correct discrimination between a malignant and a benign follicular neoplasm. Their results do not support the use of a combination of more than three antibodies especially when the diagnosis concerns the follicular variant of PTC. In the review by Correia Rodrigues and coll. [17], galectin-3 has proven to be the most reliable and effective malignancy marker in both FFPE and cytological materials followed by HBME-1, thyroid peroxidase (TPO), and cytokeratin 19. These authors, evaluating a great amount of studies, concluded that although galectin-3 shows on average a positive predictive value (PPV) and negative predictive value (NPV) of, respectively, 84.1% and 81% and a DA of about 83%, these results were not sufficient for recommending the use of this antibody alone for the differential diagnosis between malignant and benign differentiated neoplasms. Nonetheless, in the field of thyroid cytology, galectin-3, especially in combination with HBME-1, may be helpful in identifying neoplastic and malignant lesions in the indeterminate cytological categories which represent a clinical problem [28,29,30].
Among the antibodies which have been tested as malignancy markers in thyroid differentiated tumors, TPO, CD57, CD44v6, and Rb-1 [27, 31, 32] have also been proven to be effective in identifying malignant neoplasms irrespective of the presence of either capsular or vascular invasion, although the results are controversial because of the poor reproducibility of some experiments (TPO and Rb1).
Eventually, there are some recently investigated markers of malignancy which have revealed a good accuracy in identifying the malignant cells of a follicular-patterned neoplasm. FGFR-2 is an isoform of the fibroblast growth factor receptor family which is underexpressed in PTC and FA but exhibits a strong cytoplasmic positivity in normal and hyperplastic thyrocytes [33]. The retinoic acid receptors (RARs) and the retinoid X receptors (RXRs), including isoforms A and B, have shown good sensitivity (RARs) and specificity (RXRs) in PTCs. It is remarkable that the expression of these antibodies is different in malignant and benign cells: the latter present a strong nuclear expression, whereas the former are identified by a marked cytoplasmic staining [34].
The malignancy markers have been also studied in thyroid tumors different than PTC and FTC [35]. In these instances, the IHC does not focus on the identification of malignant cells, since the histological hallmarks of malignancy are usually well detectable, but on the correct recognition of the poorly differentiated component which can be important for the prognosis and the treatment of the tumor.
4 Prognostic and Predictive Markers
The immunohistochemical expression of antibodies which may either anticipate the degree of aggressiveness or predict the clinical course of a malignant tumor has since long been investigated. Traditional proliferative markers such as Ki-67, p27/kip1, and cyclins D1 and E have been tested first in the differential diagnosis of malignant versus benign differentiated tumors and then as prognostic parameters in the same neoplastic category with controversial results [36,37,38].
In this setting, the paper by Wang and coll. [39] has underlined that a score based on the expression of the connective tissue growth factor (CTGF, also known as CCN2) may predict with high statistical significance the possibility of a high tumor stage at diagnosis and the likelihood of regional nodal metastases. Similar results were reported by Saffar and coll. [40] who tested MMP2 (matrix metalloprotease 2) and CCP3 (caspase-3) in PTC. MMP2 did not show a significant correlation with necrosis or extrathyroid invasion but was significantly associated with a higher likelihood of lymphatic spread, whereas CCP3 showed a specular correlation with the same prognostic parameters. The authors suggest the combined use of both antibodies for assessing the aggressiveness of PTC for therapeutic purposes. The expression of NCAM (CD56) and OCIAD-1 in thyroid differentiated tumors is associated with a lower aggressiveness, whereas a decreased or absent positivity in the neoplastic cells may be predictive of nodal or distant metastatic spread: it is noteworthy that in a few cases the metastatic thyrocytes retrieve the expression of CD56 [41]. In our paper, CD56 was negative in 96% of the PM, while 68.5% of the BNs showed cytoplasm positivity for this marker, with an overall high sensitivity (96%) but lower specificity (69%). In specific, our 96% of the PMs did not show any follicular cell with CD56 expression [42].
More interesting are the recent investigations leading to the application of prognostic markers to less differentiated and undifferentiated tumors, especially ATC, for which new pharmacological treatment (sorafenib, axitinib, withaferin A) with monoclonal antibodies directed against the growth factor receptors of the neoplastic cells has been recently introduced [43, 44]. In this setting, the expression of cancer stem cell markers, which have been mentioned in the previous paragraph [13], has been reported as associated with a worst prognostic course of the tumor, and it might be evaluated in patients who are candidate for target therapies.
PDTC is an uncommon finding in routine practice, and it is usually observed as a pattern in the context of a differentiated carcinoma. Nevertheless, many authors have reported a decrease of the disease-free interval and of the overall survival in tumors showing a predominant insular pattern (usually higher the 40% of the tumor area). Recently, a paper by Rossi and coll. [35] has found, in a small series of pure PD insular carcinomas, a statistically significant correlation with the expression of beta-catenin compared to more traditional malignancy markers (HBME-1 and galectin-3) in PTC.
5 Antibodies Directed Against Mutated Genes
The recent discoveries of the involvement of the most important signaling pathways of the follicular cells in the thyroid carcinogenesis have led the investigation to the role of each single-gene mutation in the cell transformation. As a consequence, the studies involving the mutations of the genes of the MAP kinase cascade have provided brilliant data supporting the pivotal importance of RAF and RAS mutations in the origin of thyroid carcinoma, and the point mutations of the RET gene have been regarded as a key mechanism for MTC [45,46,47]. Many of these investigations have been carried out at the molecular level, but, as a natural consequence, some antibodies directed toward the mutated proteins have been produced and released for different clinical purposes.
RET proto-oncogene, an antibody with cytoplasmic expression, has been used at the beginning of this century as a malignancy marker for follicular differentiated tumors [15, 26]. Unfortunately, because of technical problems or of a significant lack of specificity, its application for this important differential diagnosis has been discontinued in many institutions.
For similar reasons, the use of PAX8/PPARgamma antibody, which was regarded as a robust diagnostic marker of FTC [47–49], showed a significant rate of positive expression in in FA (31%, [50]) which blurred its role in this diagnostic field.
More recently, an antibody directed toward the B-RAF mutated protein kinase (VE-1) has been commercialized as diagnostic and prognostic marker [51]. Its expression, according to the authors who have published on this subject, would reveal the presence of the V600E mutation of the B-RAF gene, which is the most common gene mutation in PTC, and it is primarily involved in the occurrence of this tumor [46, 47, 52]. The identification of a B-RAF mutation can be helpful in two different clinical settings: (a) on cytological material, when an indeterminate diagnosis is made on a fine-needle aspiration biopsy, and (b) on both cytological and FFPE materials, when the diagnosis of PTC is already evident. In the former case, the B-RAF mutation, as is regarded as 99% specific for PTC, identifies those patients who should be addressed to the surgical thyroidectomy, sparing many unnecessary thyroid removals. In the latter case, the identification of B-RAF V600E mutation would provide the surgeon with an additional tool for a more aggressive approach to either the tumor or the central neck compartment nodes [53].
Rossi and coll. [54] suggest that also in case with a diagnosis of suspicious for carcinoma, which is associated with a high likelihood of papillary carcinoma (60–80%), the identification of a B-RAF mutation might induce the surgeon to a more aggressive approach to suspicious nodules at cytology [54, 55]. The most important condition for the use of the antibody VE-1 as a morphologic substitute of the molecular change is the nearly complete overlapping between molecular and IHC findings [56].
Conclusions
The recent insights in the molecular mechanisms of thyroid carcinogenesis, also prompted by the need of understanding the processes of occurrence and progression of the infantile tumors induced by the exposure to ionizing radiation after the Chernobyl accident, have led to a flourishment of studies involving new antibodies. With the introduction of new molecular targeted therapies, these new antibodies may represent useful predictors of therapeutic response in tumors which either do not respond any more to the radioiodine treatment (dedifferentiated and oncocytic carcinomas) or are not sensitive to any conventional antitumor treatment. At the same time, some new antibodies are being tested for the identification of tumors which, in some instances, may be misdiagnosed as malignant (HTT and oncocytic tumors), with negative consequences for the patients. Some markers of malignancies have been introduced although their efficacy has to be tested on both large series by evaluating different prognostic parameters than before. Finally, the use of antibodies directed to proteins generated by mutated genes may represent a cost-effective method for diagnosing and managing patients affected by thyroid tumors.
A nosological entity recently described by Nikiforov YE and coll. [57] has been defined NIFTP (noninvasive follicular thyroid neoplasm with papillary-like nuclear features). It represents the less aggressive counterpart of the follicular variant of papillary carcinoma. Although their morphologic and molecular features have been somewhat described in the abovementioned study, the immunohistochemical profile of NIFTP needs a more detailed investigation, especially in order to identify the most distinctive features helpful in distinguishing this prognostically favorable tumor from its aggressive counterpart.
References
Hundahl SA, Cady B, Cunningham MP, Mazzaferri E, McKee RF, Rosai J, Shah JP, Fremgen AM, Stewart AK, Hölzer S. Initial results from a prospective cohort study of 5583 cases of thyroid carcinoma treated in the united states during 1996. U.S. and German Thyroid Cancer Study Group. An American College of Surgeons Commission on Cancer Patient Care Evaluation study. Cancer. 2000;89(1):202–17.
Gimm O. Mini-review: Thyroid cancer. Cancer Lett. 2001;163:143–56.
De Lellis RA, Lloyd RV, Heitz PU, Eng C. World Health Organisation pathology and genetics of tumours of endocrine organs. Lyon: IARC press/ Agency for Research on Cancer; 2004.
Khan A, Nosè V. Pathology of the thyroid gland. In: Lloyd RV, editor. Endocrine pathology. Totowa (NJ): Humana Press; 2004.
Carney JA, Hirokawa M, Lloyd RV, Papotti M, Sebo TJ. Hyalinizing trabecular tumors of the thyroid gland are almost all benign. Am J Surg Pathol. 2008;32(12):1877–89.
Cheung CC, Boerner SL, MacMillan CM, Ramyar L, Asa SL. Hyalinizing trabecular tumor of the thyroid: a variant of papillary carcinoma proved by molecular genetics. Am J Surg Pathol. 2000;24(12):1622–6.
Papotti M, Volante M, Giuliano A, Fassina A, Fusco A, Bussolati G, Santoro M, Chiappetta G. RET/PTC activation in hyalinizing trabecular tumors of the thyroid. Am J Surg Pathol. 2000;24(12):1615–21.
Leonardo E, Volante M, Barbareschi M, Cavazza A, Dei Tos AP, Bussolati G, Papotti M. Cell membrane reactivity of MIB-1 antibody to Ki67 in human tumors: fact or artifact? Appl Immunohistochem Mol Morphol. 2007;15:220–3.
Erickson LA, Jin L, Goellner JR, Lohse C, Pankratz VS, Zukerberg LR, Thompson GB, van Heerden JA, Grant CS, Lloyd RV. Pathologic features, proliferative activity, and cyclin D1 expression in Hurthle cell neoplasms of the thyroid. Mod Pathol. 2000;13(2):186–92.
Gasparre G, Porcelli AM, Bonora E, Pennisi LF, Toller M, Iommarini L, Ghelli A, Moretti M, Betts CM, Martinelli GN, Ceroni AR, Curcio F, Carelli V, Rugolo M, Tallini G, Romeo G. Disruptive mitochondrial DNA mutations in complex I subunits are markers of oncocytic phenotype in thyroid tumors. Proc Natl Acad Sci U S A. 2007;104(21):9001–6.
Niu D, Kondo T, Nakazawa T, Kawasaki T, Yamane T, Mochizuki K, Kato Y, Matsuzaki T, Takata K, Katoh R. Differential expression of aquaporins and its diagnostic utility in thyroid cancer. PLoS One. 2012;7(7):e40770.
Gauchotte G, Philippe C, Lacomme S, Léotard B, Wissler MP, Allou L, Toussaint B, Klein M, Vignaud JM, Bressenot A. BRAF, p53 and SOX2 in anaplastic thyroid carcinoma: evidence for multistep carcinogenesis. Pathology. 2011;43(5):447–52.
Yun JY, Kim YA, Choe JY, Min H, Lee KS, Jung Y, Oh S, Kim JE. Expression of cancer stem cell markers is more frequent in anaplastic thyroid carcinoma compared to papillary thyroid carcinoma and is related to adverse clinical outcome. J Clin Pathol. 2013;67(2):125–33.
Baloch ZW, LiVolsi VA. Follicular-patterned lesions of the thyroid: the bane of the pathologist. Am J Clin Pathol. 2002;117:143–50.
Griffith OL, Chiu CG, Gown AM, Jones SJM, Wiseman SM. Biomarker panel diagnosis of thyroid cancer: a critical review. Exp Rev Anticancer Ther. 2008;8:1399–413. Review
Miettinen M, Kovatich AJ. HBME-1 monoclonal antibody useful in the differential diagnosis of mesothelioma, adenocarcinoma and soft tissue and bone tumors. Appl Immunohistochem. 1995;3:115–22.
Correia Rodrigues HG, de Pontes AA, Adan LF. Use of molecular markers in samples obtained from preoperative aspiration of thyroid. Endocr J. 2012;59(5):417–24. Review
Bartolazzi A, Gasbarri A, Papotti M, Bussolati G, Lucante T, Khan A, Inohara H, Marandino F, Orlandi F, Nardi F, Vecchione A, Tecce R, Larsson O. Application of an immunodiagnostic method for improving preoperative diagnosis of nodular thyroid lesions. Lancet. 2001;357:1644–50.
Papotti M, Volante M, Saggiorato E, Deandreis D, Veltri A, Orlandi F. Role of galectin-3 immunodetection in the cytological diagnosis of thyroid cystic papillary carcinoma. Eur J Endocrinol. 2002;147:515–21.
Herrmann ME, LiVolsi VA, Pasha TL, Roberts SA, Wojcik EM, Baloch ZW. Immunohistochemical expression of Galectin-3 in benign and malignant thyroid lesions. Arch Pathol Lab Med. 2002;126:710–3.
Dencic TI, Cvejic D, Paunovic I, Tatic S, Havelka M, Savin S. Cytokeratin19 expression discriminates papillary thyroid carcinoma from other thyroid lesions and predicts its aggressive behavior. Med Oncol. 2013;30:362–71.
Sahoo S, Hoda SA, Rosai J, DeLellis RA. Cytokeratin 19 immunoreactivity in the diagnosis of papillary thyroid carcinoma: a note of caution. Am J Clin Pathol. 2001;116(5):696–702.
De Matos LL, Del Giglio AB, Matsubayashi CO, de Lima FM, Del Giglio A, da Silva Pinhal MA. Expression of CK-19, galectin-3 and HBME-1 in the differentiation of thyroid lesions: systematic review and diagnostic meta-analysis. Diagn Pathol. 2012;7:97–106. Review
Park YJ, Kwak SH, Kim DC, Kim H, Choe G, Park do J, Jang HC, Park SH, Cho BY, Park SY. Diagnostic value of galectin-3, HBME-1, cytokeratin 19, high molecular weight cytokeratin, cyclin D1 and p27(kip1) in the differential diagnosis of thyroid nodules. J Korean Med Sci. 2007;22(4):621–8.
Scognamiglio T, Hyjek E, Kao J, Chen YT. Diagnostic usefulness of HBME1, galectin-3, CK19, and CITED1 and evaluation of their expression in encapsulated lesions with questionable features of papillary thyroid carcinoma. Am J Clin Pathol. 2006;126(5):700–8.
Rossi ED, Raffaelli M, Mule’ A, Miraglia A, Lombardi CP, Vecchio FM, Fadda G. Simultaneous immunohistochemical expression of HBME-1 and galectin-3 differentiates papillary carcinomas from hyperfunctioning lesions of the thyroid. Histopathology. 2006;48:795–800.
Nechifor-Boila A, Borda A, Sassola A, Hafdi-Nejjari A, Borson-Chazot F, Lifante JC, Sturm N, Lavérriere MH, Berger M, Decaussin-Petrucci M. Immunohistochemical markers in the diagnosis of papillary thyroid carcinomas: The promising role of combined immunostaining using HBME-1 and CD56. Pathol Res Pract. 2013;209:585–92.
Rossi ED, Raffaelli M, Minimo C, Mule’ A, Lombardi CP, Vecchio FM, Fadda G. Immunocytochemical evaluation of thyroid neoplasms on thin-layer smears from fine-needle aspiration biopsies. Cancer Cytopathol. 2005;105:87–95.
Saggiorato E, De Pompa R, Volante M, Cappia S, Arecco F, Dei Tos AP, Orlandi F, Papotti M. Characterization of thyroid “follicular neoplasms” in fine-needle aspiration cytologic specimens using a panel of immunohistochemical markers: a proposal for clinical application. Endocr Relat Cancer. 2005;12:305–17.
Fadda G, Rossi ED, Raffaelli M, Pontecorvi A, Sioletic S, Morassi F, Lombardi CP, Zannoni GF, Rindi G. Follicular thyroid neoplasms can be classified as low and high risk according to HBME-1 and Galectin 3 expression on liquid based fine needle cytology. Eur J Endocrinol. 2011;165:447–53.
Anwar F, Emond MJ, Schmidt RA, Hwang HC, Bronner MP. Retinoblastoma expression in thyroid neoplasms. Mod Pathol. 2000;13:562–9.
Nasir A, Catalano E, Calafati S, Cantor A, Kaiser HE, Coppola D. Role of p53, CD44V6 and CD57 in differentiating between benign and malignant follicular neoplasms of the thyroid. In Vivo. 2004;18:189–95.
Redler A, Di Rocco G, Giannotti D, Frezzotti F, Bernieri MG, Ceccarelli S, D’Amici S, Vescarelli E, Mitterhofer AP, Angeloni A, Marchese C. Fibroblast growth factor receptor-2 expression in thyroid tumor progression: potential diagnostic application. PLoS One. 2013;8:e72224.
Gauchotte G, Lacomme S, Brochin L, Tournier B, Cahn V, Monhoven N, Piard F, Klein M, Martinet N, Rochette-Egly C, Vignaud JM. Retinoid acid receptor expression is helpful to distinguish between adenoma and well-differentiated carcinoma in the thyroid. Virchows Arch. 2013;462:619–32.
Rossi ED, Straccia P, Palumbo M, Stigliano E, Revelli L, Lombardi CP, Santeusanio G, Pontecorvi A, Fadda G. Diagnostic and prognostic role of HBME-1, galectin-3, and β-catenin in poorly differentiated and anaplastic thyroid carcinomas. Appl Immunohistochem Mol Morphol. 2013;21:237–41.
Erickson LA, Jin L, Wollan PC, Thompson GB, van Heerden J, Lloyd RV. Expression of p27kip1 and Ki-67 in benign and malignant thyroid tumors. Mod Pathol. 1998;11:169–74.
Wang S, Wuu J, Savas L, Patwardhan N, Khan A. The role of cell cycle regulatory proteins, cyclin D1, cyclin E, and p27 in thyroid carcinogenesis. Hum Pathol. 1998;29:1304–9.
Konturek A, Barczyński M, Nowak W, Richter P. Prognostic factors in differentiated thyroid cancer—a 20-year surgical outcome study. Langenbeck’s Arch Surg. 2012;397:809–15.
Wang G, Zhang W, Meng W, Liu J, Wang P, Lin S, Xu L, Li E, Chen G. Expression and clinical significance of connective tissue growth factor in thyroid carcinomas. J Int Med Res. 2013;41:1214–20.
Saffar H, Sanii S, Emami B, Heshmat R, Panah VH, Azimi S, Tavangar SM. Evaluation of MMP2 and Caspase-3 expression in 107 cases of papillary thyroid carcinoma and its association with prognostic factors. Pathol Res Pract. 2013;209:195–9.
Yang AH, Chen JY, Lee CH, et al. Expression of NCAM and OCIAD1 in well-differentiated thyroid carcinoma: correlation with the risk of distant metastasis. J Clin Pathol. 2012;65:206–12.
Bizzarro T, Martini M, Marrocco C, D’amato D, Traini E, Lombardi CP, Pontecorvi A, Fadda G, Larocca LM, Rossi ED. The role of CD56 in FNAC: A pilot study performed on LBC. PLoS One. 2015;10(7):e0132939. https://doi.org/10.1371/journal.pone.0132939.
Denaro N, Nigro CL, Russi EG, Merlano MC. The role of chemotherapy and latest emerging target therapies in anaplastic thyroid cancer. Onco Targets Ther. 2013;9:1231–41. Review
Cohen SM, Mukerji R, Timmermann BN, Samadi AK, Cohen MS. A novel combination of withaferin A and sorafenib shows synergistic efficacy against both papillary and anaplastic thyroid cancers. Am J Surg. 2012;204:895–900.
Soares P, Trovisco V, Rocha AS, Feijão T, Rebocho AP, Fonseca E, Vieira de Castro I, Cameselle-Teijeiro J, Cardoso-Oliveira M, Sobrinho-Simões M. Braf mutations typical of papillary thyroid carcinoma are more frequently detected in undifferentiated than in insular and insular-like poorly differentiated carcinomas. Virchows Arch. 2004;444:572–6.
Eszlinger M, Paschke R. Molecular fine-needle aspiration biopsy diagnosis of thyroid nodules by tumor specific mutations and gene expression patterns. J Mol Cell Endocrin. 2010;322:29–37.
Xing M. Braf mutation in papillary thyroid cancer: pathogenic role, molecular bases, and clinical implications. Endocr Rev. 2007;28:742–62.
Kroll TG, Sarraf P, Pecciarini L, Chen CJ, Mueller E, Spiegelmen BM, Fletcher JA. Pax8-PPARgamma1 fusion oncogene in human thyroid carcinoma. Science. 2000;25(289):1357–60.
Nikiforova MN, Biddinger PW, Caudill CM, Kroll TG, Nikiforov YE. PAX8-PPARgamma rearrangement in thyroid tumors: RT-PRC and immunohistochemical analyses. Am J Surg Pathol. 2002;26:1016–23.
Marques AR, Espadhina C, Catarino AL, Moniz S, Pereira T, Sobrinho LG, Leite V. Expression of PAX8-PPARgamma 1 rearrangements in both follicular thyroid carcinomas and adenomas. J Clin Endocrinol Metab. 2002;87:3947–52.
Koperek O, Kornauth C, Capper D, Berghoff AS, Asari R, Niederle B, von Deimling A, Birner P, Preusser M. Immunohistochemical detection of the BRAF V600E-mutated protein in papillary thyroid carcinoma. Am J Surg Pathol. 2012;36:844–50.
Nikiforova MN, Nikiforov Y. Molecular diagnostics and predictors in thyroid cancer. Thyroid. 2009;19:1351–61.
Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee SL, Mandel SJ, Mazzaferri EL, McIver B, Pacini F, Schlumberger M, Sherman SI, Steward DL, Tuttle RM. Revised management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 2009;19:1167–214.
Rossi ED, Martini M, Capodimonti S, Straccia P, Cenci T, Lombardi CP, Pontecorvi A, Larocca LM, Fadda G. Diagnostic and prognostic value of immunocytochemistry and BRAF mutation analysis on liquid based biopsies of thyroid neoplasms suspicious for carcinoma. Eur J Endocrinol. 2013;168:853–9.
Rossi ED, Zannoni GF, Moncelsi S, et al. Application of liquid based cytology to fine-needle aspiration biopsyof the thyroid gland. Front Endcorinol. 2012;3:57.
Ghossein RA, Katabi N, Fagin JA. Immunohistochemical detection of mutated BRAF V600E supports the clonal origin of BRAF-induced thyroid cancers along the spectrum of disease progression. J Clin Endocrinol Metab. 2013;98:e1414–21.
Nikiforov YE, Seethala RR, Tallini G, Baloch ZW, Basolo F, Thompson LD, Barletta JA, Wenig BM, Al Ghuzlan A, Kakudo K, Giordano TJ, Alves VA, Khanafshar E, Asa SL, El-Naggar AK, Gooding WE, Hodak SP, Lloyd RV, Maytal G, Mete O, Nikiforova MN, Nosé V, Papotti M, Poller DN, Sadow PM, Tischler AS, Tuttle RM, Wall KB, LiVolsi VA, Randolph GW, Ghossein RA. Nomenclature revision for encapsulated follicular variant of papillary thyroid carcinoma: a paradigm shift to reduce overtreatment of indolent tumors. JAMA Oncol. 2016;2(8):1023–9.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG
About this chapter
Cite this chapter
Rossi, E.D., Fadda, G. (2018). Pathology and Immunohistochemistry in Thyroid Tumors. In: Giovanella, L. (eds) Atlas of Thyroid and Neuroendocrine Tumor Markers. Springer, Cham. https://doi.org/10.1007/978-3-319-62506-5_1
Download citation
DOI: https://doi.org/10.1007/978-3-319-62506-5_1
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-62505-8
Online ISBN: 978-3-319-62506-5
eBook Packages: MedicineMedicine (R0)