Abstract
Traditionally, routine tests have been considered important elements of preanesthetic evaluation to determine fitness for surgery. Over the past three decades this practice has been scrutinized due to a low yield and high cost. In fact, routine tests such as complete blood count (CBC), chest X-ray, electrocardiogram (EKG), urinalysis, and electrolyte panel are of little value in detecting disease or changing management. Rather multiple investigations detect minor irrelevant abnormalities, increase patient risk, cause delay, and increases liability. Over the past three decades, many reviews and studies have confirmed these findings that routine testing does little or nothing to aid in effective preanesthetic assessment. Rather, postoperative complications were linked to higher ASA classification, longer duration of anesthesia, more complex surgery, and poor nutritional status.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
FormalPara Key Points-
1.
Routine preoperative laboratory tests rarely change the course of anesthesia.
-
2.
Approximately 1:500 tests reveal pertinent information.
-
3.
Centers for Medicare and Medicaid Services (CMS) will not pay for solely age-based tests.
-
4.
All medications should be documented, including over-the-counter drugs such as non-steroidal anti-inflammatory agents (NSAIDs) and herbal preparations.
-
5.
An understanding of drug interactions, especially as they relate to herbals, is essential.
-
6.
Multiple investigations detect minor irrelevant abnormalities, increase patient risk, cause delay, and increases liability.
-
7.
Postoperative complication can be linked to higher American Society of Anesthesiologists (ASA) classification, longer duration of anesthesia, more complex surgery, and poor nutritional status.
-
8.
Laboratory tests should be ordered only as indicated to discover a disease, verify a condition, or formulate a plan.
-
9.
Current guidelines have no recommendations for starting calcium channel blockers in the perioperative period.
-
10.
Despite the increase in hypotension, there appears to be no increased incidence of death, myocardial infarction (MI), or renal failure in patients continued on angiotensin-converting enzyme (ACE) inhibitors.
1 Introduction
“On feeling the pulse of a gentleman about twenty-one years of age, in March 1855, who had just seated himself in the chair to take chloroform…I found it to be small weak, and intermitting and it became feeble as I was feeling it. I told the patient he would feel no pain and that he had nothing whatever to apprehend. His pulse immediately improved…Now if the inhalation had commenced without inquiry or explanation, the syncope which seemed approaching would probably have taken place, and it would have had the appearance of being caused by the chloroform, although not so in reality.”
- John Snow. On Chloroform and other Anaesthetics. London: John Churchill. 1858
Although the importance of examination of the patient, especially the pulse, had been emphasized since ancient times, Dr. Snow was one of the first to stress the need for physical contact and evaluation prior to anesthesia.
Traditionally, routine tests have been considered important elements of preanesthetic evaluation to determine fitness for surgery. Over the past three decades this practice has been scrutinized due to a low yield and high cost. In fact, routine tests such as complete blood count (CBC), chest X-ray, electrocardiogram (EKG), urinalysis, and electrolyte panel are of little value in detecting disease or changing management. Rather multiple investigations detect minor irrelevant abnormalities, increase patient risk, cause delay, and increases liability [1].
Choosing Wisely was initiated in 2012 by the American Board of Internal Medicine to establish a national program to avoid unnecessary tests, treatments, and procedures through education of practitioners and patients [2, 3]. The initial 9 specialty boards and Consumer Reports were soon joined by some 70 other specialties, including anesthesiology in 2013. They were all charged with releasing 5 recommendations to facilitate decisions regarding appropriate care.
Recommendations from the American Society of Anesthesiologists (ASA) are as follows:
-
1.
Do not obtain baseline laboratory studies (“routine tests”) in patients without significant systemic disease (ASA I or II) undergoing low-risk surgery—specifically complete blood count, basic or comprehensive metabolic panel, coagulation studies when blood loss (or fluid shifts) is/are expected to be minimal.
-
2.
Do not obtain baseline diagnostic cardiac testing (trans-thoracic/esophageal echocardiography – TTE/TEE) or cardiac stress testing in asymptomatic stable patients with known cardiac disease (e.g., coronary artery disease [CAD], valvular disease) undergoing low or moderate risk non-cardiac surgery.
-
3.
Do not use pulmonary artery catheters (PACs) routinely for cardiac surgery in patients with a low risk of hemodynamic complications (especially with the concomitant use of alternative diagnostic tools; e.g., TEE).
-
4.
Do not administer packed red blood cells (PRBCs) in a young healthy patient without ongoing blood loss and hemoglobin of ≥6 g/dL unless symptomatic or hemodynamically unstable.
-
5.
Do not routinely administer colloid (dextrans, hydroxyethyl starches, and albumin) for volume resuscitation without appropriate indications.
Nevertheless, many patients, surgeons, and internists believe that the primary purpose of a preoperative evaluation is to give blood and urine samples, undergo an electrocardiogram, and have a chest X-ray. Routine testing, generally considered to include EKG, complete blood count, urinalysis, chest X-ray, electrolyte screen, blood urea nitrogen (BUN) and creatinine, blood glucose level, type and screen and a coagulation profile (PT/PTT), is not only time consuming and but also extremely costly with little benefit. An early large study challenged the usefulness of routine preoperative laboratory screening in 1985. Over a 4-month period the authors assessed the value of screening 2000 patients of all ages, estimating that 60% of these routinely ordered tests would not have been performed if testing had only been done for specific indications. Abnormalities that might influence perioperative management were identified in 0.22% although they were not acted upon and no changes were made to the planned procedure. No adverse anesthetic or surgical consequences were recorded. The authors concluded three decades ago that in the absence of specific indications, routine preoperative laboratory tests contribute little to patient care, and can be eliminated. Moreover, even when an abnormality was recorded, the results often were not read by the physician or nurse manager who had ordered the test—an oversight that could have serious malpractice consequences.
Some years later, one of the authors of the aforementioned study calculated that $40 billion a year was spent in the United States on preoperative testing and evaluation. Likening it to the statement that “if a little epinephrine is good, more is better,” he remarked that additional testing caused iatrogenic disease by pursuit and treatment of borderline and false-positive results, thereby increasing medico-legal risks (especially if an abnormal result is obtained and not acted upon), and decreasing the efficiency of practice. Rather, he remarked, perioperative physicians could turn such inefficiency to advantage by successfully employing inexpensive technology to reduce costs substantially and improve the quality of care.
Over the past three decades, many reviews and studies have confirmed these findings that routine testing does little or nothing to aid in effective preanesthetic assessment [4, 5]. Rather, postoperative complications were linked to higher ASA classification, longer duration of anesthesia, more complex surgery, and poor nutritional status. In addition, increased age may also be a factor, although a weak one.
However, even now, hospitals and specialists are reimbursed for unnecessary testing, For example, stress testing, acknowledged by the American College of Cardiology (ACC) and the American Heart Association (AHA) to have restricted benefit in the majority of patients, amounts to around US$2300. A common test sequence that includes complete blood count, basic metabolic panel, chest X-ray, and EKG bills for about $1600, which does not include the cost of interpretation. In some instances the Center for Medicare/Medicaid Services (CMS) and insurers will not reimburse for repeat testing and for tests based on age alone, placing the burden of payment on the patient. In other situations, CMS shoulders the enormous costs, almost arbitrarily. Change is slow to be realized and further studies, both larger and more diverse, must be undertaken.
2 Evaluation and Preoperative Preparation
Preanesthetic evaluation is the process of clinical assessment that precedes the delivery of anesthesia or ordering of tests for all procedures. It is the responsibility of the anesthesiologist or certified registered nurse anesthetist (CRNA) practicing alone. Consideration of information from multiple sources is essential, especially all medical records. Consultations should be sought as necessary. Further laboratory tests should be ordered only as indicated to discover a disease, verify a condition, or formulate a plan. Informed consent, as to risk benefit of different types of anesthetic management, must be obtained. A plan for postoperative pain relief must also be in place [6].
The information sought must include at a minimum:
-
1.
The procedure
-
2.
Past medical and surgical history
-
3.
Medications
-
4.
Documentation of vital signs
-
5.
Airway examination
-
6.
Informed consent
2.1 ASA Physical Status Classification
The ASA Physical Status (PS) classification system was initially created in 1941 by the American Society of Anesthetists, an organization that later became the ASA. The grading system was intended simply to evaluate the degree of a patient’s “sickness” or “physical state” before selecting the anesthetic and performing surgery. The preoperative physical status is used for recordkeeping, for communicating between colleagues, and to create a uniform system for statistical analysis. The grading system is not intended for use as a measure to predict operative risk.
The modern classification system consists of 6 categories, as follows:
-
ASA PS 1 - Healthy patients without systemic, physiologic, or psychiatric disease. No physical limitations. Good exercise tolerance.
-
ASA PS 2 - Patients with mild systemic disease that is well controlled. Controlled hypertension or diabetes with no physical effects. Mild obesity. Long-standing smoking without chronic obstructive pulmonary disease (COPD).
-
ASA PS 3 - Patients with severe systemic disease affecting >1 body system. No immediate threat of death. Controlled congestive heart failure (CHF). Morbid obesity. Chronic renal failure. Bronchospastic disease.
-
ASA PS 4 - Patients with severe systemic disease that is a constant threat to life. Possible risk of death. Symptomatic CHF and COPD.
-
ASA PS 5 - Moribund patients who are not expected to survive >24 h without surgery. Multiorgan failure. Sepsis with hemodynamic instability. Uncontrolled coagulopathy.
-
ASA PS 6 - Patients declared brain dead for organ donation.
2.2 Medical and Surgical History
Based on the medical and surgical history provided by the patient and the procedure to be performed, the American College of Surgeons, National Surgical Quality Improvement Program (ACS NSQUIP) has devised a Surgical Risk Calculator. Using standardized clinical data from almost 400 hospitals, a Web-based tool has been devised. By in-putting 21 preoperative factors such as co-morbidities and demographics, surgeons are able to estimate the risks of surgery, chance of complications including death, and length of hospital stay. Not only does this mechanism afford better informed consent for the patient, but it also allows decisions to be made regarding the type and even necessity for certain procedures. The Centers for Medicare and Medicaid Services are moving to incentivize surgeons through the Physician Quality Reporting System to discuss patient-specific risks and outcomes preoperatively. Using almost 3000 Current Procedural Terminology (CPT®) codes, several hundred operations over many subspecialties have been incorporated into the calculations. Thirty-day outcomes were ascertained from medical records or patient contact. Event rates were found to vary from 0.6% for renal failure to 9% for overall morbidity. Some of the patient and surgical information is shown in ◘ Table 24.1. Outcomes and risk factors are shown in ◘ Table 24.2.
While many surgical factors are taken into consideration, anesthetic factors are not addressed. History of previous difficult intubation or tracheostomy, or problems specific to anesthesia such as malignant hyperthermia or certain allergies might well impact outcome and hence risk.
2.3 Medications
All the medications that a patient is taking should be documented, including over-the- counter drugs such as non-steroidal anti-inflammatory agents (NSAIDs) and especially herbal preparations. The latter, while considered natural and thus safe, may indeed have many interactions (◘ Box 24.1). Problems arise mainly in interference with the cytochrome p450 isoenzymes (CYP). Inhibition of this system decreases metabolism and increases drug levels and duration of action. Induction, on the other hand, increases metabolism, while decreasing the effectiveness of the drug and its duration of action. Of most concern is the interference with CYP 3A4 in the liver as >50% of current prescription drugs depend on this system. Some of the more commonly used herbal substances and their varied effects on the CYP system is shown in ◘ Table 24.3.
Whether or not medications should be continued during the perioperative period should be made on a case-by-case basis for each individual patient by the patient care team. Of major concern are the cardiac medications. The most recent ACC/AHA guidelines, however, can provide some guidance pertaining to cardiac medications that may directly affect perioperative morbidity and mortality [7].
2.3.1 Beta Blocker Therapy
Several studies have examined the risks and benefits of perioperative beta blocker therapy. Although each study was designed to answer the same question, most resulted in different answers. It does appear that beta blocker therapy in the perioperative period decreases the number of cardiac events, such as myocardial infarction (MI). However, this benefit comes at the cost of increased hypotension, stroke, and, in some studies, composite death. The most recent systematic review examining the data came with the following recommendations [8]:
-
1.
Beta blockers should be continued in patients undergoing surgery who have been on beta blockers chronically.
-
2.
The management of beta blockers after surgery may be guided by clinical circumstances independent of when the agent was started.
-
3.
In patients with intermediate or high cardiac risk it may be reasonable to begin perioperative beta blocker therapy. If the decision is made to begin beta blocker therapy on a patient in the perioperative period, it is recommended that therapy be initiated at least 1 day prior to surgery, and preferably at least 2–7 days prior. Beginning beta blockers on the day of surgery is likely ineffective and may be harmful. Common sense would dictate that beginning a medication that could have significant changes in myocardial contractility and systemic blood pressure should occur days prior to surgery, such that the tolerability of the medication and its dose can be assessed by the patient and the physician. While there is no direct data to support this conclusion, it likely is best practice.
2.3.2 Statin Therapy
Statin therapy has been shown to be effective for primary and secondary prevention of cardiac events. Although most of the data related to statin therapy come from observational trials, the composite power suggests a protective effect on the preoperative use of these agents in either vascular surgery or high-risk patient populations [9]. The most recent guidelines therefore recommend that those on statins continue their therapy in the perioperative period. They also allow for the initiation of therapy in patients undergoing vascular surgery, as well as patients with clinical indications undergoing medium- or high-risk procedures. The mechanism of benefits from perioperative statin therapy are unknown, but are likely related to pleotropic, lipid lowering effects, as well as anti-inflammatory effects. Additionally, it is not known when is the optimal time to begin therapy, nor is it clear what the duration of therapy should be.
2.3.3 Alpha-2 Agonists
Early data on the role of alpha-2 agonists such as clonidine and mivazerol suggested that the perioperative use of these agents, especially in vascular surgery was protective. The POISE-2 (PeriOperative ISchemic Evaluation-2) trial—a large, multicenter, international, blinded study—was unable to demonstrate the benefit of clonidine. Additionally, it was found that clonidine use in the perioperative period was associated with an increase in the rate of nonfatal cardiac arrest and clinically significant hypotension. It is therefore not recommended to use alpha-2 agonists in the perioperative period for the prevention of cardiac events. Patients who are on alpha-2 agonists for other indications (such as hypertension) should continue their dose of medication; or ideally, be weaned off their medication and started on other therapies prior to surgery. The abrupt discontinuation of these medications can result in rebound hypertension, headache, agitation, and tremor.
2.3.4 Calcium Channel Blockers
The most current guidelines have no recommendations for starting calcium channel blockers in the perioperative period. A meta-analysis from 2003 examined the use of calcium channel blockers in patients with coronary disease and found trends toward reduced death and MI. It should be noted that these differences were mostly attributable to the use of diltiazem. Neither dihydropyridines nor verapamil had effects on mortality or MI; however, the use of either verapamil or diltiazem seemed to be protective for the development of perioperative supraventricular tachycardia (SVT). The authors note that the results are trends and that larger more robust studies are needed to confirm the results. As such, although it would be prudent to continue these medications in the perioperative period it is not recommended to begin therapy unless otherwise indicated.
2.3.5 Angiotensin-Converting Enzyme Inhibitors and Angiotensin Receptor Blockers
Approved for multiple indications from hypertension to prevention of diabetic nephropathy, ACE andangiotensin receptor blockers (ARBs) are some of the most commonly prescribed medications. Perioperative data on the risk/benefit profile of continuation of these medications is limited mostly to observational data. The largest study examined almost 80,000 patients (of which 13% were on ACE-I) and found that patients on therapy had an increased frequency of intraoperative hypotension. This has been found in other studies as well, with one showing an incidence of hypotension of 50% in patients on therapy. Despite the increase in hypotension, there appears to be no increased incidence of death, MI, or renal failure. The evidence on discontinuation of these medications prior to surgery is poor. There is data, however, on the risks of not restarting these medications in the perioperative period, which seems to be the greatest risk of discontinuation. In fact, maintaining the continuity of these medications in the setting of treatment for heart failure or hypertension is supported by other guidelines. Additionally, a more recent cohort study including 30,000 patients found an increased risk of mortality in patients in whom restarting ARB therapy was delayed. Due to the lack of demonstration of real harm to patients who continue therapy in the perioperative period as well as the potential risks of discontinuation, continuing these medications in the perioperative period is reasonable. If ACE/ARB therapy must be withheld, it should be restarted as soon as possible.
2.3.6 Diabetic Medication
Recommendations to discontinue oral diabetic medication remain controversial. While elevated blood sugar levels have been shown to retard wound healing, an ideal blood sugar level has not been determined. While many laboratory scales consider hyperglycemia to be values above 120 mg/dl, it is probably more important to consider the individual and the level at which he most usually functions. Thus, values of 150–170 mg/dl may be considered normal for many. Should testing indicate values exceeding 180 mg/dl, oral medications should be discontinued and an infusion of regular insulin commenced perioperatively. Further evaluation by an endocrinologist is indicated with repeated blood glucose checks.
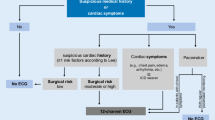
2.4 Cardiac Evaluation
While nonspecific abnormalities are found on EKG tracings in about 30% of patients, the finding rarely predicts postoperative complications and is usually insignificant.
As part of Choosing Wisely and recommendations from the ACC/AHA, the need for further cardiac testing prior to non-cardiac surgery is limited to determination of 1 of 4 criteria [10]:
-
Unstable coronary syndrome (MI, unstable angina)
-
Decompensated heart failure (New York Heart Association [NYHA] class IV or worsening disease or new onset)
-
Significant dysrhythmias; high grade or Mobitz II atrioventricular (AV) block, 3rd degree AV block, symptomatic ventricular dysrhythmias
-
Severe valvular disease
Stress testing and cardiac consultation should only be requested if any of the above findings can be made on physical examination.
2.5 Airway Assessment
Evaluation of the airway begins with a comprehensive history and physical examination. It is very important to ascertain if the patient has been told of any difficulty with intubation in the past and if he/she had a sore throat after a procedure. A short list of factors that may be indicative of a difficult airway are shown in ◘ Table 24.4.
As well as assessment for any of the conditions listed in ◘ Table 24.4, physical examination requires a systematic approach as follows:
-
1.
On nasal examination are there any polyps or a deviated septum?
-
2.
Does the mouth open to allow at least 2 fingerbreadths between upper and lower teeth?
-
3.
Is there good alignment with the upper and lower teeth? Protruding upper incisors or canines should be noted as well as carious or loose teeth and gum hypertrophy due to medication (usually dilantin). Edentulous patients often offer an easier airway, although a large tongue can cause hypopharyngeal obstruction.
-
4.
Is the palate free of any clefts, high arch, or a long, narrow anatomy?
-
5.
Can the lower jaw be protruded over the upper jaw?
-
6.
Is there any limitation of temporo-mandibular joint movement?
-
7.
Is the hyomental/thyromental distance at least >6 cm?
-
8.
Is the neck size <17 cm?
-
9.
Can a sniffing position be assumed?
-
10.
Does the patient have any stridor, previous tracheostomy, or hoarseness?
-
11.
Is the patient pregnant?
Some other specific tests can be made to determine anatomical criteria:
-
1.
Mallampati test. The test is performed with the patient sitting, and the head in a neutral position. The mouth is opened wide and the tongue protruded (◘ Fig. 24.1). The degree to which tongue size correlates to pharyngeal size is assessed. A review of 42 studies, with 34,513 participants, found that the score predicts difficult direct laryngoscopy and intubation, but does not predict difficult bag mask ventilation. Therefore, while useful in combination with other tests to predict the difficulty of a securing an airway, it is not sufficiently accurate alone. Other assessments are indicated.
-
2.
Comack and Lehane. Four grades of view are defined during direct laryngoscopy. Entire view of the laryngeal aperture is listed as Grade 1. Visualization of only the posterior commissure of the laryngeal aperture is graded as 2. If only the epiglottis is seen that is grade 3. Grade 4 view is just the soft palate.
-
3.
Mandibular space assessment involves measurement of the thyromental space, and the sterno-mental and the mandibulo-hyoid distances. The thyromental distance is measured from the mentum to the thyroid notch with the neck extended. Alignment of the laryngeal-pharyngeal axes is optimal when the distance is >6.5 cm. With the head and neck extended and the mouth closed, the distance from the suprasternal notch to the mentum should exceed 12 cm. The mandibular length from the chin to the hyoid bone should be at least 4 cm (about 4 fingerbreadths). Distance between the lower and upper teeth is normally 4.5 cm.
Class I views allow visualization of the sort palate, fauces, uvula and anterior and posterior pillars and indicates an easy intubation. Only the hard palate is visible in Class 4 (Illustration by Jmarchn - Own work, CC BY-SA 3.0, ► https://commons.wikimedia.org/w/index.php?curid=12842847. Reprinted under Creative Commons license. ► https://creativecommons.org/licenses/by-sa/3.0/)
2.6 Obstructive Sleep Apnea Syndrome
A complication often associated with obesity, but not exclusively, is obstructive sleep apnea syndrome (OSA or OSAS) [11]. The potential for airway difficulties in patients with OSA is more likely to be recognized by anesthesiologists even when the patient has not had a formal polysomnographic sleep study, which defines the patient’s apnea/hypopnea index (AHI); categorizes the severity of OSA as mild, moderate, or severe; and makes recommendations for appropriate nasal continuous positive airway pressure (nCPAP). Apnea is defined as the cessation of airflow for at least 10 s. During hypopnea airflow decreases by 50% for 10 s or decreases by 30% if there is an associated decrease in the oxygen saturation or an arousal from sleep. To grade the severity of sleep apnea, the number of events per hour is reported as the AHI. An AHI of less than 5 is considered normal, 5–15 is mild, 15–30 is moderate, and more than 30 events per hour indicate severe sleep apnea. The use of nCPAP for several weeks preoperatively has been found to be highly effective at preserving airway patency during sleep and anesthesia as well as diminishing reflex responses to hypoxia and hypercapnia. This effect may result from upper airway stabilization, a residual effect of nCPAP that begins to occur within as little as 4 h of continuous use of nCPAP. Also, chronic nCPAP preoperatively has been found to abolish mean, systolic, and diastolic blood pressure fluctuations in OSA patients. As a result, the risks of cardiac ST segment depression and recurrent atrial fibrillation are reduced. It is recommended that nCPAP and oral appliances be continued during the postoperative period. It is also important to note that patients who have had corrective surgery for OSA, such as uvulopalatopharyngoplasty, may still harbor the disease despite lessening or absence of current symptoms.
The undiagnosed OSA patient proves to be a greater diagnostic dilemma during the preoperative screening clinic examination since these patients seldom have sleep studies. A presumed diagnosis of OSAS can be inferred from a history of abnormal breathing during sleep (e.g., loud snoring and witnessed apnea periods by a bed partner), frequent arousals from sleep to wakefulness (e.g., periodic extremity twitching, vocalization, turning, and snorting), severe daytime sleepiness, a body mass index [BMI] of ≥35 kg/m2, increased neck circumference (≥ 17 inches for males, ≥ 16 inches for females), and the presence of coexisting morbidities (e.g., essential systemic hypertension, pulmonary hypertension, cardiomegaly). The STOP-Bang questionnaire has been shown reliable in correctly diagnosing the condition (◘ Fig. 24.2).
One of the simplest and easiest means to assess OSA and the one with most relevance to the anesthesiologist in a pre-anesthetic assessment clinic is application of the STOP-Bang questionnaire. The score is based on responding yes to 3 or more questions, which indicates a high probability of OSA: Snore, Tired, Observed (apnea), Pressure, Body mass index (BMI) (>35), Age (>50), Neck circumference > 40 cm or 17 in, and Gender male. This score is referenced but not illustrated in the guidelines. Age is probably a less important factor as many children are diagnosed with OSA (Adapted from [12])
The ASA task force on OSAS recommended a risk scoring system as summarized (points are assigned for each of 3 categories [a, b, c] and then totaled [d]):
-
(a)
Severity of sleep apnea: Based on a sleep study (i.e., AHI) or clinical indicators if a sleep study is not available (i.e., presumptive diagnosis). Points: 0 = None; 1 = Mild OSA; 2 = Moderate OSA; 3 = Severe OSA.
One point may be subtracted if a patient has been on CPAP or bi-level positive airway pressure (BiPAP) prior to surgery and will be using this consistently during the postoperative period. One point should be added if a patient with mild or moderate OSA has a resting PaCO2 exceeding 50 mm Hg.
-
(b)
Invasiveness of the surgical procedure and anesthesia: Based on type of surgery/anesthesia. Points: 0 = superficial surgery under local or peripheral nerve block, anesthesia without sedation; 1 = superficial surgery with moderate sedation or general anesthesia or peripheral surgery with spinal or epidural anesthesia (with no more than moderate sedation); 2 = peripheral surgery with general anesthesia or airway surgery with moderate sedation; 3 = major surgery under general anesthesia or airway surgery under general anesthesia.
-
(c)
Requirement for postoperative opioids: Points: 0 = none; 1 = low-dose oral opioids; 3 = high-dose oral opioids or parenteral or neuraxial opioids.
-
(d)
Estimation of perioperative risk: Based on the overall score (0–6) derived from the points assigned to (a) added to the greater of the points assigned to (b) or (c). Patients with overall score of ≥4 may be at increased perioperative risk from OSA. Patients with a score of ≥5 may be at significantly increased perioperative risk from OSA.
Clinical suspicion of OSAS may be the only preoperative tool available to the anesthesiologist as formal, widely used, preoperative validated questionnaires have not been established.
In addition to the OSA risk factors presented above, the anesthesiologist should consider the patient’s airway class and history of difficult intubation. To this end a morphologic OSA prediction score has been developed that includes anatomical difficulties. Cardiovascular risk assessment may require an EKG (right ventricular hypertrophy secondary to cor pulmonale, left ventricular hypertrophy secondary to ischemic heart disease), echocardiography, cardiac stress testing, or preoperative cardiologist optimization. Pulmonary risk factors of morbid obesity and chronic obstructive pulmonary disease may prompt obtaining a radiograph or arterial blood gases to detect Pickwickian syndrome or hypercapnic chronic sleep apnea syndrome. These patients may have decreased sensitivity to CO2 in the postoperative period and may need ventilatory support as their hypoxic drive to breathe may be abolished by O2 as well as subanesthetic concentrations of inhaled anesthetics or sedatives.
OSA patients may be exquisitely sensitive to all preoperative central depressants. Respiratory arrest, coma, and death can occur. Avoidance of preoperative sedation with long-acting benzodiazepines and opioids may be wise. Premedication against aspiration may include histamine-2 receptor antagonists (such as famotidine) and pro-motility agents (such as metoclopramide).
2.7 Respiratory Evaluation
Postoperative pulmonary complications (PPCs) impact recovery after surgery. It is therefore important to identify risk factors and establish whether preoperative respiratory therapy combined with adjustments to intraoperative ventilatory management, such as addition of alveolar recruitment techniques, can decrease the risk of PPCs. Risk factors include smoking, surgical site (thorax or abdomen), previous lung disease, obesity, older age, malnutrition, and long anesthesia. Pulmonary function tests are of very limited value and should be used as management tools only. A simple test such as measurement of oxygen saturation on room air, giving a value >90, may be all that is required. Chest auscultation is indicated in all patients. Should rhonchi be heard, in most instances they can be cleared by coughing.
2.8 Neurologic Evaluation
A cursory review of the neurologic system usually suffices, checking for equal and bilateral motor strength and intact sensory perception. Any abnormalities should be referred for more advanced neurologic consultation. Any family history of neuromuscular disease or delayed awakening from anesthesia should be documented. Patients should be asked to extend their necks and paresthesias or limb weakness noted. Although multiple sclerosis is probably not worsened by anesthetic agents, symptoms that might relate to this disease should be documented. The ability of the patient to understand the procedure and the alternative anesthetic techniques should be assessed in order to obtain appropriate consent.
2.9 Miscellaneous
Several groups deserve special attention. Patients who are hard of hearing or have visual problems, as well as those for whom English may not be the primary language, should be identified and notation made on the chart. Pediatric patients also have different requirements. Whether the parents should accompany the child to the operating room should be determined on a case-to-case basis. Certainly, parents should have a clear understanding of the anesthetic process, including postoperative pain management that their child will undergo and have ample time for questions. There are many rare disease and situations that require consideration such as progeria, malignant hyperthermia, Tay Sachs, xeroderma pigmentosa, hemophilia, and porphyria, to name a very few. The transgender patient may have undergone laryngeal surgery or osteotomies. The complexities of these conditions are beyond the scope of this chapter.
3 Conclusion
Tests and evaluations should have potential benefits that are greater than potential adverse effects. Benefits would include change in time or content of anesthetic care or perioperative resource use that would improve safety. Adverse effects include interventions that cause injury, discomfort, delay, cost, inconvenience, all of which are not commensurate with benefit.
Preoperative laboratory evaluations and EKG testing should be driven by history, physical findings, and surgical risk. Tests are indicated only if the results can correctly identify abnormalities, change the diagnosis, management plan or outcome. Needless tests are expensive. Improved standardization is required and it is important to remember that one size does not fit all.
4 Questions and Answers
Questions (Choose the Most Appropriate Answer)
-
1.
Which finding best provides an easy and reliable means to diagnose obstructive sleep apnea syndrome (OSAS)?
-
A.
An apnea-hypopnea index of 4
-
B.
Morbid obesity
-
C.
A STOP-BANG score of 5
-
D.
A history of loud snoring
-
A.
-
2.
Routine preoperative testing:
-
A.
Remains a major expense within the health system in the United States
-
B.
Is on the increase
-
C.
Has been shown to be very useful for developing countries
-
D.
Must be studied further before conclusions can be drawn as to its usefulness
-
A.
-
3.
Which of the following statements best describes routine preoperative testing practices?
-
A.
It is standardized in all hospitals in the United States
-
B.
About 0.2% reveal abnormalities
-
C.
It is a useful screening measures
-
D.
Problems are immediately recognized and acted upon
-
A.
-
4.
Choosing Wisely:
-
A.
Was initiated by the American Board of Internal Medicine
-
B.
Nine specialty boards and Consumer Reports quickly joined
-
C.
Later 70 other specialties including Anesthesiology contributed by 2013
-
D.
All of the above
-
A.
-
5.
Ordering tests preoperatively only as indicated will:
-
A.
Decrease the number of tests performed only by 10%
-
B.
Improve hospital efficiency and cost savings
-
C.
Have major impact on patient care
-
D.
Certainly be rejected by patients
-
A.
-
6.
Abnormality of the EKG tracing:
-
A.
Is found in up to 30% of patients
-
B.
Always signifies postoperative complications
-
C.
Changes management in almost half of patients
-
D.
Is frequently insignificant
-
A.
-
7.
Stress testing:
-
A.
Reliably indicates cardiac disease
-
B.
Is a good predictor of postoperative complications
-
C.
Should be used as a general screening test
-
D.
Is not recommended as a risk assessor in older patients based on age.
-
A.
-
8.
Regarding management of the diabetic patient:
-
A.
Blood sugar is best controlled at <120 mg/dl
-
B.
Controversy remains as to whether all medications should be discontinued
-
C.
Normoglycemia may be an individual number
-
D.
An infusion of regular insulin should be started when blood sugar levels exceed 130 mg/dl
-
A.
-
9.
Use of nCPAP preoperatively can:
-
A.
Abolish fluctuations in blood pressure in OSA patients
-
B.
Require at least 24 h to be effective
-
C.
Not help in improving airway patency
-
D.
Increase reflex responses to hypoxia
-
A.
-
10.
Indicators of a potentially difficult airway are least likely to include:
-
A.
Pierre Robin syndrome
-
B.
Neck circumference of 18 cm
-
C.
Comack-Lehane grade 2
-
D.
Thyromental distance of 4 cm.
-
A.
Answers
-
1.
C. A STOP-BANG score of 5 provides an easy and reliable means to diagnose obstructive sleep apnea (OSA). The score is based on responding yes to 3 or more questions, which indicates a high probability of OSA: snore, tired, observed (apnea), pressure, BMI (>35), age (>50), neck circumference >40 cm or 17 inches, and male gender. Age is probably a less important factor as many children are diagnosed with OSA.
-
2.
A. Routine preoperative testing remains a major expense within the U.S. health system. Traditionally routine tests have been considered important elements of preanesthetic evaluation to determine fitness for surgery. Over the past three decades this practice has been scrutinized due to a low yield and high cost. One study author calculated that $40 billion a year was spent in the United States on preoperative testing and evaluation.
-
3.
B. About 0.2% of routine preoperative testing reveals abnormalities. In fact, routine tests such as complete blood count, chest X-ray, electrocardiogram, urinalysis, and electrolyte panel are of little value in detecting disease or changing management. Rather, multiple investigations detect minor irrelevant abnormalities, increase patient risk, cause delay, and increases liability.
-
4.
D. Choosing Wisely was initiated in 2012 by the American Board of Internal Medicine to establish a national program to avoid unnecessary tests, treatments, and procedures through education of practitioners and patients. The initial 9 specialty boards and Consumer Reports were soon joined by some 70 other specialties including anesthesiology in 2013. They were all charged with releasing 5 recommendations to facilitate decisions regarding appropriate care.
-
5.
B. Ordering tests preoperatively only as indicated will improve hospital efficiency and cost savings. Preoperative laboratory evaluations and EKG testing should be driven by history, physical findings, and surgical risk. Tests are indicated only if the results can correctly identify abnormalities, change the diagnosis, management plan, or outcome. Needless tests are expensive and improved standardization is required.
-
6.
A. While nonspecific abnormalities are found on EKG tracings in about 30% of patients, the finding rarely predicts postoperative complications and is usually insignificant.
-
7.
D. Stress testing is not recommended as a risk assessor in older patients based on age. Stress testing, acknowledged by the American College of Cardiology and the American Heart association to have restricted benefit in the majority of patients, amounts to around $2300. A common test sequence that includes complete blood count, basic metabolic panel, chest X-ray and EKG bills for about $1600, which does not include the cost of interpretation. In some instances the Center for Medicare/Medicaid Services (CMS) and insurers will not reimburse for repeat testing and for tests based on age alone, placing the burden of payment on the patient.
-
8.
C. Regarding management of the diabetic patient, normoglycemia may be an individual number. Recommendations to discontinue oral diabetic medication remain controversial. While elevated blood sugar levels have been shown to retard wound healing, an ideal blood sugar level has not been determined. While many laboratory scales consider hyperglycemia to be values above 120 mg/dl, it is probably more important to consider the individual and the level at which he most usually functions. Thus, values of 150–170 mg/dl may be considered normal for many. Should testing indicate values exceeding 180 mg/dl, oral medications should be discontinued and an infusion of regular insulin commenced perioperatively. Further evaluation by an endocrinologist is indicated with repeated blood glucose checks.
-
9.
A. Use of chronic nasal continuous positive airway pressure (nCPAP) preoperatively has been found to abolish mean, systolic, and diastolic blood pressure fluctuations in OSA patients. Also, the use of nCPAP for several weeks preoperatively has been found to be highly effective at preserving airway patency during sleep and anesthesia as well as diminishing reflex responses to hypoxia and hypercapnia. This effect may result from upper airway stabilization, a residual effect of nCPAP that begins to occur within as little as 4 h of continuous use of nCPAP.
-
10.
C. Indicators of a potentially difficult airway are least likely to include Comack-Lehane grade 2. Using Comack-Lehane, 4 grades of view are defined during direct laryngoscopy. The entire view of the laryngeal aperture is listed as grade 1. Visualization of only the posterior commissure of the laryngeal aperture is graded as 2. If only the epiglottis is seen that is grade 3. Grade 4 view is just the soft palate.
References
Frost EA. Preoperative assessment: integrating information from divergent sources. Mt Sinai J. 2012;79(1):3–12.
Rao VM, Levin D. The overuse of diagnostic imaging and the choosing wisely initiative. Ann Intern Med. 2012;157(8):574–6.
Cassel CK, Guest JA. Choosing wisely – helping physicians and patients make smart decisions about their care. JAMA. 2012;307(17):1801–2.
Chung F, Yuan H, Yin L, Vairavanathan S, Wong DT. Elimination of preoperative testing in ambulatory surgery. Anesth Analg. 2009;108(2):467–75.
Katz RI, Dexter F, Rosenfeld K, Wolfe L, Redmond V, Agarwal D, et al. Survey study of anesthesiologists’ and surgeons’ ordering of unnecessary preoperative laboratory tests. Anesth Analg. 2011;112(1):207–12.
Committee on Standards and Practice Parameters, Apfelbaum JL, Connis RT, Nickinovich DG, American Society of Anesthesiologists Task Force on Preanesthesia Evaluation, Pasternak LR, Arens JF, et al. Practice advisory for preanesthesia evaluation: an updated report by the American Society of Anesthesiologists Task Force on Preanesthesia evaluation. Anesthesiol. 2012;116(3):522–38.
Fleisher LA, Fleischmann KE, Auerbach AD, Barnason SA, Beckman JA, Bozkurt B, American College of Cardiology, American Heart Association, et al. 2014 ACC/AHA Guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. J Am Coll Cardiol. 2014;64(22):e77–137.
Wijeysundera DN, Duncan D, Nkonde-Price C, Virani SS, Washam JB, Fleischmann KE, et al. Perioperative beta blockade in noncardiac surgery: a systematic review for the 2014 ACC/AHA guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. J Am Coll Cardiol. 2014;64(22):2406–25.
Ridker PM, Wilson PWF. A trial-based approach to statin guidelines. JAMA. 2013;310(11):1123–4.
Stone NJ, Robinson JG, Lichtenstein AH, Bairey Merz CN, Blum CB, Eckel RH, American College of Cardiology/American Heart Association Task Force on Practice Guidelines, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63(25 Pt B):2889–934.
Gross JB, Bachenberg KL, Benumof JL, Caplan RA, Connis RT, Coté CJ, American Society of Anesthesiologists Task Force on perioperative management, et al. Practice guidelines for the perioperative management of patients with obstructive sleep apnea: a report by the American Society of Anesthesiologists Task Force on perioperative management of patients with obstructive sleep apnea. Anesthesiology. 2006;104(5):1081–93.
Nagappa M, Liao P, Wong J, Auckley D, Ramachandran SK, Memtsoudis S, et al. Validation of the STOP-Bang questionnaire as a screening tool for obstructive sleep apnea among different populations: a systematic review and meta-analysis. PLoS One. 2015;10(12):e0143697.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG
About this chapter
Cite this chapter
Frost, E.A.M., Katz, D. (2018). Preoperative Evaluation of Patients Undergoing Non-cardiac Surgery. In: Farag, E., Argalious, M., Tetzlaff, J.E., Sharma, D. (eds) Basic Sciences in Anesthesia. Springer, Cham. https://doi.org/10.1007/978-3-319-62067-1_24
Download citation
DOI: https://doi.org/10.1007/978-3-319-62067-1_24
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-62065-7
Online ISBN: 978-3-319-62067-1
eBook Packages: MedicineMedicine (R0)