Abstract
Despite the increasing availability of genetic panels and their diminishing cost genetic screening for myasthenic conditions in children remains difficult. Additionally some children with undoubted myasthenic conditions have yet to be genetically characterised. For this reason a neurophysiological test for the diagnosis of disorders of the neuromuscular junction (NMJ) is valuable. Of the options available repetitive nerve stimulation up (RNS) is relatively insensitive and uncomfortable and reliance on a form of single fibre EMG (SFEMG) is essential. Volitional SFEMG presents formidable challenges in children and is unlikely to be successful in any child under the age of eight years. Stimulation techniques increase the feasibility of studies in children. A modification of stimulation SFEMG using concentric needle electrodes has been developed. Because multiple motor units are stimulated true single-fibre potentials are not seen with this technique and we therefore describe the technique as Stimulated Potential Analysis using Concentric needle Electrodes under the acronym SPACE. Examinations are conducted on orbicularis oculi being the most sensitive muscle in most myasthenic conditions. With the use of local anaesthetic it is possible to effect successful examination in most children. Monopolar needles are placed near the facial nerve as it crosses the zygomatic arch with the potentials recorded from orbicularis oculi. The use of peak detection algorithms on most EMG machines allows some quantification of the results producing a value for the Mean Consecutive Difference (MCD) and these are unaffected by the high-frequency filter used. Quantification of the MCD becomes increasingly difficult with increasing abnormality of the underlying NMJ. Normative data have been derived from the extrapolated norms (e-norms) technique. When applied to a large cohort of patients the technique demonstrates sensitivity 84%, specificity 71%, negative predictive value 96%, and positive predictive value 36% for the diagnosis of myasthenia. Specificity can be further enhanced if those conditions caused by a neurogenic abnormality are excluded. The technique is within the competence of any trained clinical neurophysiologist and is well tolerated by patients and parents alike. It is an important neurophysiological technique for the diagnosis of neuromuscular junction abnormality.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Introduction
Despite the increasing availability of gene panels, an accessible and cost-effective genetic screen for children with myasthenic conditions remains elusive for many clinicians. The number of genes associated with the condition increases yearly [1,2,3,4,5,6,7,8,9,10,11,12,13]. The clinical manifestations are so protean that it is very likely that without some direction by neurophysiological testing a large number of children will be screened unnecessarily. Of the different tests available repetitive nerve stimulation will be discussed in another chapter and has its proponents. However, it is not always sensitive, especially for certain diagnoses such as ocular myasthenia gravis, and when performed to its greatest extent uncomfortable for many children [14]. Performing it under general anaesthesia is a considerable undertaking and usually not necessary. Single fibre EMG (SFEMG) is a technique developed by Erik Stålberg in the 1970s that detects excessive variations in neuromuscular transmission, termed “jitter”, among single muscle fibers. This test modality has higher sensitivity than repetitive stimulation for disorders of the neuromuscular junction, but has less specificity as increased jitter may be seen in other neuromuscular disorders. In its purest form, namely with volition activating the potentials, SFEMG is really technically impossible in children under 8 years of age consistently. It is true that on occasion experts in the technique will be able to achieve it in a particularly cooperative younger child but this is not a basis for universal application particularly if one is hoping to develop a neurophysiological screening test for myasthenia. It is therefore necessary to talk about the use of stimulated techniques for producing potentials that can be analysed. In most centres this would be called stimulated single-fibre EMG (stimSFEMG) [15, 16] but this name is most probably a misnomer because even when studying a normal neuromuscular junction it is very difficult to be sure that one is recording from single fibre potentials as opposed to small compound motor potentials representing a few fibers. As the test becomes more abnormal, reflecting abnormality of the neuromuscular junction, this becomes increasingly impossible. The technique evolved in our department from the work of Dr. Payan [17] using the “blanket technique” to reveal the components of a motor unit potential and by these means identify any instability that might be present. It was never intended to be a single fibre assessment and was unequivocally distanced from classic single fibre methodology by the author. In its original form it was used qualitatively and was a very useful adjunct to pediatric EMG allowing identification of likely abnormalities not only of the neuromuscular junction, but also other conditions affecting the peripheral nervous system such as neurogenic disorders. The technique lends itself very easily to quantification using peak detection algorithms used for the single fibre recording, particularly around the normal range of responses.
To avoid any possible confusion with single fibre methodology and also to remove it from the legitimate criticisms of proponents of traditional single fibre methodology, our group calls the test “SPACE”, which is an acronym for Stimulated Potential Analysis with Concentric needle Electrodes. Because it does not include single fibre within its definition, SPACE is a neutral term and will be the focus of the remainder of this chapter. Concentric needle electrodes (CNE) enter into the definition of SPACE because the neurophysiological world has been obliged to turn to single use needles as a result of the discovery of prion disease, which cannot be eliminated by autoclaving. Reusable needles can no longer be used, one example of which is the single fibre electrode (SFE). Official SFE are quite costly, hence the previous practice of autoclaving and reusing them. In contrast concentric needles are significantly cheaper and are thus disposable. Until the price drops for single-use single fibre EMG needles it is likely that the situation of using a CNE, usually the facial needle with the smallest diameter, will continue for some time into the future.
Methods
The technique of SPACE is well recognisable in the descriptions of stimSFEMG and the important elements ensuring success of the technique will be summarised here. One of the most important is how you prepare the parents and the child, if old enough. It is very important that parents realise the importance of the condition that we are attempting to identify. While it may be vanishingly rare with only 10 per million of population affected [18], it is a condition that is treatable and should not be missed as it is associated with significant morbidity and in some cases mortality. If the parents understand the importance of the test and the reason you are doing it, even if in all honesty it is unlikely to show an abnormality in nearly 90% of the studies, they are complicit in what follows. It is also very important to stress to the parents that the technique when using local anaesthetic produces a minimal amount of discomfort, and therefore any distress that is displayed by the child is more likely to be a reaction to the unfamiliar settings and people as discomfort. Ametop (active ingredient tetracaine 4%) is the anaesthetic used in some centers in preference to EMLA (active ingredients lidocaine 2.5%, prilocaine 2.5%) as the former is approved for use in children down to the age of 1 month and has a more rapid onset of action, reaching its maximum anaesthetic level at around 30 minutes. After application over the orbicularis oculi (taking care not to expose the eye itself) and covering of the anaesthetic with an occlusive dressing the parents and child are sent away for that period. On their return it is very important to wash the dressing off the face as otherwise you may inadvertently pull the hair which may set the child on edge and make future investigation difficult.
The studies are performed using any modern EMG machine, in our department this is a KeyPoint. The filter settings for the recording are 3–10 kHz. The low-frequency filter setting derives from the work of Dr. Payan, already mentioned, which was the forerunner of the development of SPACE in our department. There have been criticisms of using such a high low-frequency filter with recommendations that it should not exceed 1 kHz mainly because of the phenomenon of ringing when potentials appear that are not real. In a study of normal subjects we were unable to demonstrate this phenomenon and also identified the peak detection algorithm showed no difference in the jitter measurements according to the low-frequency filter setting [19]. The stimulus duration is set at 0.04 ms. Surface electrodes are placed on the forehead as the earth (known as the ground in North America) and just below the tragus as the indifferent (known as the reference in North America). A monopolar stimulating electrode of 15 mm length and 30G diameter (SpesMedicaS.r.l, Genoa, Italy) is inserted just above the midpoint of the upper margin of the zygomatic arch (Fig. 10.1). The operator will press with the digit of his/her non-dominant hand on the zygomatic arch and while the pressure is being exerted place the needle just above it with the dominant hand. The Ametop removes the sting from the insertion but not the pressure and disguising the insertion with the pressure on the zygomatic arch is very effective. The needle is secured with tape to avoid accidental injuries to delicate structures, and then stimulation applied while slowly increasing the threshold to 1 mA. Looking for a twitch in the orbicularis oculi, it is anticipated that this should be seen before the 1 mA stimulation threshold is reached. If it is not the stimulating needle is repositioned and if this is still ineffective the needle is removed and placed in a different point. It is crucial to have the stimulation threshold below 1 mA as it means that the child does not experience any discomfort, and equally important the operator can be certain that the needle is placed close to the nerve and can expect an “all or nothing response” to increasing levels of stimulation. If any abnormality occurs this is then more likely to be pathological than technical. Even saying this most of us when seeing abnormal jitter or blocking will increase the stimulus further to be sure this is not a technical effect. Usually the response, if your insertion technique has been good, is that the abnormality remains in the potentials you identified but other potentials are recruited, sometimes with normal jitter. Next the recording electrode, a concentric needle electrode of the facial type (French gauge 30G) (Ambu A/S DK-2750 Ballerup) with a recording surface of 0.019 mm2 is placed at the outer margin of the eyebrow aiming at the ipsilateral hip and protecting the eye by placing the thumb of the non-EMG hand into the corner of the orbit, lying gently over the eyeball.
The stimulation is given individually by single shocks gradually increasing the intensity until waveforms are seen. The threshold is returned to 0 and the rate increased to 10 Hz. Continuous low frequency repetitive stimulation is given until the waveforms appear and continue until a screen full of potentials is recorded which approximates to around 25 repetitions. The process is repeated with single shocks being given with the needle moved slightly in order to obtain a different population of potentials. When seen the process is repeated. The aim is to collect at least 25 different potentials. The technique itself if everything goes smoothly will take less than 10 minutes although sometimes if there is difficulty identifying the potentials it may take longer.
If no abnormality is found on SPACE, the study is followed by a routine nerve and EMG study. Whatever the finding on the examination of the jitter it is important to leave the needle in orbicularis oculi and get the children to contract the muscle to see the interference pattern in the muscle. If the traces are abnormal this examination of the interference pattern in orbicularis oculi allows the determination of whether there is neurogenic change, which is an important cause for abnormalities of jitter and is associated with a bulbar palsy. If there is any doubt of the normality of the interference pattern in orbicularis oculi, particularly if the jitter is abnormal, it is obligatory to study the genioglossus, easily approached from the submental route. Whatever the findings in all of the initial investigations, nerve conduction studies and sampling of a peripheral muscle must be performed, the latter is particularly important if a bulbar palsy is identified as it may demonstrate that the neurogenic changes are part of a widespread motor neuronopathy.
SPACE of orbicularis oculi may miss some of the limb girdle myasthenias and particularly some of the more recently described disorders of N-glycosylation such as GMPPB and DPAGT [20,21,22,23]. Reports so far have demonstrated significant abnormalities on repetitive nerve stimulation of a peripheral muscle and if the jitter is normal and this is the suspected diagnosis it is necessary to perform repetitive nerve stimulation (RNS). RNS of the accessory nerve recording trapezius is very well tolerated by many children and can be reliably performed.
Interpretation of Results
Our software package uses a peak detection algorithm. The work on filter settings was performed using that algorithm and therefore what follows in the description here may not apply to programs using an algorithm which is triggered by the slope of the potential as this may be affected by the low-frequency filter settings. There is good deal of debate as to what the potentials produced by stimulation of the nerve or muscle represent [24,25,26]. It is for this reason that we have tried to distance ourselves from strict single fibre methodology because the requirements for single-fibre potentials to be accurately identified are necessarily extremely stringent and very rarely met by the technique of SPACE. The number of potentials that can safely be considered to be from a single fibre are very few indeed in most examinations. Using the alternative term apparent single fibre action potentials (ASFAP) [24] to cover this in many ways does not go far enough. Our technique is to use the peak detection algorithm to identify the potentials by the algorithm set by the software. If the study is normal and the peaks do not show much variation clearly the peak detection algorithm will have little difficulty in identifying jitter. However, sometimes several potentials may be seen with varying confidence as to their origin. Such a situation is shown in Fig. 10.2 where five potentials are seen none of which would fulfil criteria for a single fibre potential but the measurement, albeit inaccurate, does give you some indication of the degree of abnormality when compared with normative data obtained from similar technique. Once the abnormality becomes pronounced the abnormality on peak detection increases exponentially and any linear relationship between degree of abnormality of the neuromuscular junction and abnormality on jitter measurement can be discounted (Fig. 10.3).
When analysing the data as we increase the intensity from zero until the threshold for individual potentials is reached there is a need to remove those first potentials particularly as they may show some minor jitter until supramaximal stimulation is achieved. Once this is done it is normally acceptable to use the measurements provided by the peak detection algorithm. The only time this is contested is if the program is clearly picking up alternating peaks from a potential with two peaks. This is shown in Fig. 10.4. It is possible to go through and identify those waveforms which only focus on one peak, or more easily, discount that potential from your examination.
Normative Data
Early on in our departmental experience with the technique we formed the impression that the neuromuscular junction was extraordinarily mature with samples of seemingly unaltered potentials appearing in children as young as 6 weeks of age which were indistinguishable to the blinded observer from a child in their teenage years. For this reason we used for a while the normative data obtained in stimulated single fibre EMG or volition SFEMG with the correction factor applied (×0.8) [27] in normal adults [24, 28,29,30,31,32,33,34] . With E-norm methodology, which extracts the normative data from laboratory attendances we have been able to confirm the jitter measurements in older children are indeed very similar to adults [35]. From a cohort of 600 cases, we derived an upper limit of normal of 26 μs for the mean jitter for children 2 years of age and older. More detailed analysis of the group under 2 years of age suggested that while some may have extraordinarily mature neuromuscular junctions this state is by no means the rule and we therefore found that under 1 year an upper limit of the mean jitter was 45 μs decreasing in the next year to 33 μs with the adult level being reached at 2 years of age [36]. Our results are calculated as the mean consecutive difference index or MCD-I which is calculated as the value obtained divided by the upper limit of normal.
Results
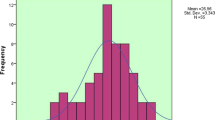
There are few if any centres that have much experience of the use of this technique in children, which is inexplicable, and whilst there have been a few papers [37, 38] reporting results in limited numbers of subjects our experience is unique. For a period of time certainly from around 1997–2007 our attempts to perform the technique were often greeted by failure and the numbers done per year were very few (Fig. 10.5). Sometimes a maximum of only ten would come through our department in a year. However, after that time possibly related to changes in technique such as using shorter stimulating electrodes, which did not need to be held in position and also the more frequent application of local anaesthetic we saw an exponential increase in the number of cases, which are now at around 120 per year. A recent audit of our experience from 7 July 2007 to 8 February 2016 identified a total of 878 investigations, 501 boys and 377 girls [39]. The mean age was just over 5 years (66 months) but was skewed towards the younger age group with the median 46.5 months. Our hospital is a tertiary referral centre and because of this 114 cases were lost to follow-up. Many of these were from overseas often attending for one visit only. In this group 23 had an abnormal MCD-I ranging between 101 and 294% with 10% of them having MCD-I significantly elevated, defined as greater than 125%. A further group of 104 patients had not completed their investigations and were excluded from the analysis. Thirty six of these had a raised MCD-I, 25 of which were greater than 125%. The remaining cohort was 660 children in whom a diagnosis had been made or neuromuscular abnormality had been ruled out by a neuromuscular specialist.
Diagnoses
The diagnosis of myasthenia was considered definite if an associated genetic abnormality was identified or antibodies against the acetylcholine receptor or the MuSK protein had been identified. A further category of probable myasthenia was included in which the diagnosis of myasthenia was felt to be highly likely based on examination by a neuromuscular specialist with additional support from response to pyridostigmine. Ninty four patients had a diagnosis of myasthenia and these are shown in Table 10.1 along with other causes of NMJ abnormality such as botulism, when persistence of neuromuscular blocking agents (NMBA), bringing the total to 106.
In 554 alternative diagnoses were made (Table 10.2). The diagnoses were made with combination of clinical assessment, genetic, histopathological and other ancillary investigations. The diagnosis of a neurogenic abnormality was felt to be secure on neurophysiological grounds only. A proportion of these other cases had abnormalities of jitter and the range of that abnormality as an MCD-I is also shown.
Analysis of Test Parameters
Analysis showed sensitivity 84%, specificity 71%, negative predictive value 96%, and finally positive predictive value 36%. Certain subgroups within this cohort are worthy of additional comment. The sensitivity for the diagnosis of myasthenia was a little reduced, when compared to other studies [31, 40,41,42] but this was influenced by such cases as the five patients with GMPPB mutations, who are known not to have abnormalities of jitter when testing orbicularis oculi [21]. When looking at figures for sensitivity for the diagnosis of myasthenia gravis our figures (91% sensitivity) are comparable with other studies. The two cases of autoimmune myasthenia gravis (AIMG) where autoantibodies had been demonstrated but no jitter abnormality was present included one patient in whom the abnormality appeared to be restricted to the ocular muscles. Amongst those patients with alternative diagnoses to myasthenia but abnormalities of jitter, the most important are those with neurogenic abnormalities and these were either isolated bulbar palsies or generalised motor neuronopathies. In the age group of under 2 years of age an isolated bulbar palsy as a reason for the apparent jitter abnormality was more common than myasthenia. If these cases, that is the generalised and bulbar motor neuronopathies, are removed from the analysis of test parameters the specificity is improved to 74% and the positive predictive value to 46%, with no alteration to sensitivity. The final group of interest are those are patients with myopathies either specified or non-specified in whom a proportion have been shown to have jitter abnormalities. What is emerging is that there are certain myopathies that do seem to have an associated neuromuscular transmission disorder and determining whether the condition is one of these or whether the myopathic changes are from the severity of the myasthenic syndrome can be a very difficult in practice [43,44,45] . As a rough guideline most myasthenics, with the exception of DOK7 mutations, which may show patchy change, usually show severe abnormalities of jitter.
Discussion
SPACE is an imprecise and rather inelegant technique, which must be clearly delineated from the volitional single fibre EMG, which must be considered the gold standard for the diagnosis of neuromuscular junction abnormalities. However, whatever the criticisms that can be levelled at the former, it is highly practical and applicable in children and it is better to have an imperfect technique that you can do rather than a perfect technique that you cannot. While the author could additionally be criticised in calling this anything other than stimulated single fibre EMG, there is a strong feeling that the identification with single fibre methodology has led to the technique being resisted in its more widespread application in children. It evolved not only from single fibre methodology in particular use of peak detection algorithms but also from the “blanket technique” as a very useful technique for analysing the components of the motor unit potential [17]. The discoverer of the “blanket technique” was adamant when he described it that this was not single fibre methodology and our group would certainly agree.
With attention to some of the details given here it is possible to perform the technique in most conscious children of any age. Resort to general anaesthetic is very rarely needed and is to be resisted as it prevents the all-important EMG examination of bulbar and limb muscles taking place in the same attendance. The technique itself is quickly performed and we have shown that its results are to be trusted. It has formed an important part of the examination of children with hypotonia in our hospital with clinicians using it freely to examine those difficult cases in which myasthenia has not been excluded. The high negative predictive value is of particular importance in this subgroup. As a rule if the jitter abnormality is highly abnormal and a neurogenic abnormality has been excluded it has been our experience that the most likely cause is a myasthenic syndrome rather than a myopathic process with secondary neuromuscular junction changes. In the cases where the jitter is elevated but perhaps not very significantly, less than 115% [39], most clinicians would still arrange for a muscle biopsy while screening for some of the more common myasthenic conditions.
Further work that is needed in the development of this technique is to determine the normal range in the very youngest babies, under 3 months of age, for example. Most congenital myasthenic conditions are symptomatic from birth and to have a test that can identify these patients early on in the course of their disease, at a time when they are perhaps the most vulnerable from the consequences of serious associated symptoms, such as episodic apnoea, would be very useful. Additionally, but certainly not likely to find a solution in paediatric practice, refinement of this technique such that one could restrict the number of fibres stimulated and thus enable the indisputable identification of single fibre potentials, is awaited eagerly.
References
Beeson D. Congenital myasthenic syndromes: recent advances. Curr Opin Neurol. 2016;29:565–71.
Ravenscroft G, Davis MR, Lamont P, Forrest A, Laing NG. New era in genetics of early-onset muscle disease: breakthroughs and challenges. Semin Cell Dev Biol. 2017;64:160–70.
Shelton GD. Myasthenia gravis and congenital myasthenic syndromes in dogs and cats: a history and mini-review. Neuromuscul Disord. 2016;26:331–4.
Engel AG, Shen XM, Selcen D, Sine SM. Congenital myasthenic syndromes: pathogenesis, diagnosis, and treatment. Lancet Neurol. 2015;14:420–34.
Eymard B, Hantai D, Fournier E, Nicole S, Sternberg D, Richard P, Fardeau M. Congenital myasthenic syndromes; French experience. Bull Acad Natl Med. 2014;198:257–70.
Rodriguez Cruz PM, Palace J, Beeson D. Congenital myasthenic syndromes and the neuromuscular junction. Curr Opin Neurol. 2014;27:566–75.
Eymard B, Hantai D, Estournet B. Congenital myasthenic syndromes. Handb Clin Neurol. 2013;113:1469–80.
Finlayson S, Beeson D, Palace J. Congenital myasthenic syndromes: an update. Pract Neurol. 2013;13:80–91.
Hantai D, Nicole S, Eymard B. Congenital myasthenic syndromes: an update. Curr Opin Neurol. 2013;26:561–8.
Engel AG. Current status of the congenital myasthenic syndromes. Neuromuscul Disord. 2012;22:99–111.
Lorenzoni PJ, Scola RH, Kay CS, Werneck LC. Congenital myasthenic syndrome: a brief review. Pediatr Neurol. 2012;46:141–8.
Nance JR, Dowling JJ, Gibbs EM, Bonnemann CG. Congenital myopathies: an update. Curr Neurol Neurosci Rep. 2012;12:165–74.
Barisic N, Chaouch A, Muller JS, Lochmuller H. Genetic heterogeneity and pathophysiological mechanisms in congenital myasthenic syndromes. Eur J Paediatr Neurol. 2011;15:189–96.
Pitt M. Neurophysiological strategies for the diagnosis of disorders of the neuromuscular junction in children. Dev Med Child Neurol. 2008;50:328–33.
Trontelj JV, Khuraibet A, Mihelin M. The jitter in stimulated orbicularis oculi muscle: technique and normal values. J Neurol Neurosurg Psychiatry. 1988;51:814–9.
Trontelj JV. Stimulation SFEMG in myasthenia gravis. Muscle Nerve. 1990;13:458–9.
Payan J. The blanket principle: a technical note. Muscle Nerve. 1978;1:423–6.
Parr JR, Andrew MJ, Finnis M, Beeson D, Vincent A, Jayawant S. How common is childhood myasthenia? The UK incidence and prevalence of autoimmune and congenital myasthenia. Arch Dis Child. 2014;99:539–42.
Patel A, Gosk M, Pitt M. The effect of different low-frequency filters on concentric needle jitter in stimulated orbicularis oculi. Muscle Nerve. 2016;54:317–9.
Rodriguez Cruz PM, Belaya K, Basiri K, Sedghi M, Farrugia ME, Holton JL, Liu WW, Maxwell S, Petty R, Walls TJ, Kennett R, Pitt M, Sarkozy A, Parton M, Lochmuller H, Muntoni F, Palace J, Beeson D. Clinical features of the myasthenic syndrome arising from mutations in GMPPB. J Neurol Neurosurg Psychiatry. 2016;87:802–9.
Belaya K, Rodriguez Cruz PM, Liu WW, Maxwell S, McGowan S, Farrugia ME, Petty R, Walls TJ, Sedghi M, Basiri K, Yue WW, Sarkozy A, Bertoli M, Pitt M, Kennett R, Schaefer A, Bushby K, Parton M, Lochmuller H, Palace J, Muntoni F, Beeson D. Mutations in GMPPB cause congenital myasthenic syndrome and bridge myasthenic disorders with dystroglycanopathies. Brain. 2015;138:2493–504.
Klein A, Robb S, Rushing E, Liu WW, Belaya K, Beeson D. Congenital Myasthenic syndrome caused by mutations in DPAGT. Neuromuscul Disord. 2015;25:253–6.
Selcen D, Shen XM, Brengman J, Li Y, Stans AA, Wieben E, Engel AG. DPAGT1 myasthenia and myopathy: genetic, phenotypic, and expression studies. Neurology. 2014;82:1822–30.
Ertas M, Baslo MB, Yildiz N, Yazici J, Oge AE. Concentric needle electrode for neuromuscular jitter analysis. Muscle Nerve. 2000;23:715–9.
Sanders DB. Measuring jitter with concentric needle electrodes. Muscle Nerve. 2013;47:317–8.
Stalberg E. Jitter analysis with concentric needle electrodes. Ann N Y Acad Sci. 2012;1274:77–85.
Stalberg EV, Trontelj JV, Sanders DB. Single fibre EMG. Fiskebackskil, Lysekil: Edshagen Publishing House; 2010.
Gilchrist JM. Single fiber EMG reference values: a collaborative effort. Ad hoc committee of the AAEM special interest group on single fiber EMG. Muscle Nerve. 1992;15:151–61.
Kouyoumdjian JA, Stalberg EV. Reference jitter values for concentric needle electrodes in voluntarily activated extensor digitorum communis and orbicularis oculi muscles. Muscle Nerve. 2008;37:694–9.
Kouyoumdjian JA, Stalberg EV. Concentric needle jitter on stimulated orbicularis oculi in 50 healthy subjects. Clin Neurophysiol. 2011;122:617–22.
Sarrigiannis PG, Kennett RP, Read S, Farrugia ME. Single-fiber EMG with a concentric needle electrode: validation in myasthenia gravis. Muscle Nerve. 2006;33:61–5.
Stalberg E, Trontelj JV. Single fiber electromyography studies in healthy and disease muscle. New York: Raven Press Ltd; 1994.
Trontelj JV, Fernandez JM. Single fiber EMG in juvenile idiopathic scoliosis. Muscle Nerve. 1988;11:297–300.
Valls-Canals J, Povedano M, Montero J, Pradas J. Stimulated single-fiber EMG of the frontalis and orbicularis oculi muscles in ocular myasthenia gravis. Muscle Nerve. 2003;28:501–3.
Jabre JF, Pitt MC, Deeb J, Chui KK. E-norms: a method to extrapolate reference values from a laboratory population. J Clin Neurophysiol. 2015;32:265–70.
Pitt MC, Jabre JF. Determining jitter values in the very young by use of the e-norms methodology. Muscle Nerve. 2017;55(1):51–4.
Verma S, Lin J. Stimulated jitter analysis for the evaluation of neuromuscular junction disorders in children. Muscle Nerve. 2016;53:471–2.
Verma S, Lin J, Barkhaus PE. Stimulated jitter analysis in the early diagnosis of infant botulism. Muscle Nerve. 2015;52:309–10.
Pitt MC, McHugh JC, Deeb J, Smith RA. Assessing neuromuscular junction stability from stimulated EMG in children. Clin Neurophysiol. 2017;128:290–6.
Lyu RK, Cheng SY, Tang LM. Electrodiagnostic studies in myasthenia gravis. Changgeng Yi Xue Za Zhi. 1993;16:164–9.
SJ O, Kim DE, Kuruoglu R, Bradley RJ, Dwyer D. Diagnostic sensitivity of the laboratory tests in myasthenia gravis. Muscle Nerve. 1992;15:720–4.
Sanders DB, Howard JF Jr. AAEE minimonograph #25: single-fiber electromyography in myasthenia gravis. Muscle Nerve. 1986;9:809–19.
Illingworth MA, Main M, Pitt M, Feng L, Sewry CA, Gunny R, Vorstman E, Beeson D, Manzur A, Muntoni F, Robb SA. RYR1-related congenital myopathy with fatigable weakness, responding to pyridostigimine. Neuromuscul Disord. 2014;24:707–12.
Munot P, Lashley D, Jungbluth H, Feng L, Pitt M, Robb SA, Palace J, Jayawant S, Kennet R, Beeson D, Cullup T, Abbs S, Laing N, Sewry C, Muntoni F. Congenital fibre type disproportion associated with mutations in the tropomyosin 3 (TPM3) gene mimicking congenital myasthenia. Neuromuscul Disord. 2010;20:796–800.
Robb SA, Sewry CA, Dowling JJ, Feng L, Cullup T, Lillis S, Abbs S, Lees MM, Laporte J, Manzur AY, Knight RK, Mills KR, Pike MG, Kress W, Beeson D, Jungbluth H, Pitt MC, Muntoni F. Impaired neuromuscular transmission and response to acetylcholinesterase inhibitors in centronuclear myopathies. Neuromuscul Disord. 2011;21:379–86.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this chapter
Cite this chapter
Pitt, M. (2017). The Use of Stimulated EMG in the Diagnosis of Neuromuscular Junction Abnormality. In: McMillan, H., Kang, P. (eds) Pediatric Electromyography. Springer, Cham. https://doi.org/10.1007/978-3-319-61361-1_10
Download citation
DOI: https://doi.org/10.1007/978-3-319-61361-1_10
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-61360-4
Online ISBN: 978-3-319-61361-1
eBook Packages: MedicineMedicine (R0)