Abstract
About half of the oral cancers have already reached an advanced stage (III or IV) when diagnosed, which influences survival rates (5-year survival, 20% to 50% depending upon tumour sites).
Long time intervals since the beginning of symptoms until definitive diagnosis favour advanced disease stages at diagnosis and a worse prognosis in terms of survival. Some agents seem to have responsibilities in the delay in diagnosis of oral symptomatic cancer, namely, patients, healthcare providers, the health system and the actual tumour. In fact, the symptomatic time period related to the patient appears to be the main difficulty for attaining an early diagnosis. However, and in view of the methodological weaknesses of the existing investigations, this information has to be taken with caution.
Recently, a conceptual framework and guidelines for research (Aarhus statement) have been proposed to produce high-quality studies on early diagnosis. Besides, the usage of the term “diagnostic delay” has been discouraged, and the more accurate “time interval to diagnosis and treatment” has been suggested.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
4.1 Introduction
Neoplasias of the oral cavity and nearby sites (pharynx) are quite common throughout the world (the sixth most common cancer) [1], although prevalences differ greatly between and within continents up to the point that oropharyngeal cancer (OPC) is the most common malignancy in Malaysia or Sri Lanka [1,2,3,4,5]. These differences may reach 20-fold, and about 66% of OPCs occur in developing countries [2,3,4,5].
India and Pakistan, together with Taiwan, also show very high incidences in Asia. In Europe, Hungary, Slovakia and Slovenia have the highest incidence rates. Among the American countries, Brazil, Uruguay, Puerto Rico and Cuba score the highest rates. The most affected countries in Africa are Namibia, Botswana and Mozambique; and Melanesia and Papua New Guinea rank the highest in Oceania [2,3,4,5].
The main problem with these neoplasms is that they are frequently diagnosed (about 50%) when stages III or IV have already been reached. This circumstance undoubtedly influences 5-year survival rates (20–50% depending on tumour sites), and delays in diagnosis may have something to do with it [6,7,8,9,10,11]. Avoiding diagnostic delays may be a key point for improving survival, as estimations show that if all OPCs were diagnosed and treated at early stages, survival rates would reach 80% [10].
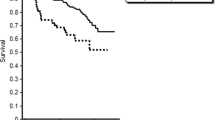
This apparently straightforward assumption is still to be demonstrated [12], and even some research groups wonder whether it would really matter [13]. When dealing with oral cancer, this hypothesis has been proved and the longer the delay in diagnosis, the more advanced the stage [9, 14], mostly due to long time intervals from first cancer symptom to referral to diagnosis. The length of this period of time resulted to be a risk factor for both advanced stage and mortality [14]. This being, studies on early detection and diagnostic delay in oral cancer have to be a research priority in secondary and tertiary prevention [2] if better outcomes are to be achieved (Fig. 4.1) [16, 17].
4.2 Historical Antecedents
Assuming that many cancers are curable if treated early and also that reducing treatment delay is the first step for increasing survival, Pack and Gallo established the basis of the concept of “diagnostic delay” 75 years ago. Their research included 1000 cancer patients, and 90 of these patients had their cancers located in the lip, floor of the mouth and tongue. In this set of patients, the responsibility for the delay was attributed to their physician in 17% of cases. In another 62.3% of the situations, patients and physicians were to blame for delayed diagnoses [18].
This issue has raised the interest of many researchers ever since, who have used a variety of criteria in their investigations [19]. About four decades ago, the prognostic value of the time lapse in diagnosis of oral cancer gained relevance, and two periods were considered: the time since first symptom until professional consultation and the period the patient spends under care until a final diagnosis is made [20, 21]. Currently, diagnostic delay is most frequently defined as “patient delay”, the period between the patient first noticing a symptom and their first consultation with a healthcare professional concerning that symptom [9, 22], and “provider/professional delay”, the period from the patient’s first consultation with a healthcare professional and the definitive pathological diagnosis [9, 22]. Therefore, the “overall or total diagnostic delay” would include the period elapsed since the first symptom or sign until the definitive diagnosis.
When facing the problem of investigating diagnostic delay from the patients’ pathway standpoint, it seemed reasonable to divide this path into steps or “stages” for a better understanding of the situation. Thus, several stages have been suggested: a first stage, lasting since the first symptom until the first contact with a clinician; a second stage, since this moment until a referral letter is prepared; a third stage referral letter to appearance at a specialised service; and the fourth stage, since the patient is seen at a specialised service until a final diagnosis is reached [23]. Besides, the time-lapse since diagnosis until treatment is sometimes also assessed [16, 24]. Although interesting, this approach to the problem makes data gathering somehow more difficult in retrospective analyses, but this effort is needed if we are to implement interventions to tackle delays in diagnosis.
Despite an early diagnosis is the cornerstone for improving survival and cure rates, it is very difficult to determine its effect on tumour stage at diagnosis (the main predictor for survival) and to measure the actual effects of interventions for reducing delays in diagnosis [16]. A useful tool in this situation is the guideline “the Aarhus statement” recently developed by an international consensus working group for improving the design and reporting of studies on early cancer diagnosis [16].
4.3 Impact of Diagnostic Delay in Oral Cancer
Although it could be expected that longer delays would always mean worse outcomes in cancer, certain paradoxical and counter-intuitive relationships have been observed in certain cancers [25]. Regarding oral cancer, as mentioned above, tumour stage at diagnosis is still the most important prognostic factor for oral squamous cell carcinoma, with advanced stages linked to high mortality [6, 11]. Unfortunately, the research efforts made for unveiling the role of delays in diagnosis in disease progression have been found to be limited by the usage of different and heterogeneous criteria for defining the concept of “delay” [8]. This limitation has not precluded meta-analytic approaches that have identified diagnostic delay as a risk factor for tumour stage of oropharyngeal carcinomas, being this association stronger when the study is limited to oral cancer, and particularly when the delay is longer than 1 month [9]. Thus, the longer the delay, the more advanced stage at diagnosis [14]. Moreover, longer time intervals from first symptom to referral for diagnosis seem to be a risk factor for mortality, being diagnostic delay a moderate risk factor for mortality from head and neck cancer [26]. Again, and due to the aforementioned limitations of the original studies included in the meta-analyses, these findings should be interpreted with caution.
4.4 Limitations and Biases of Studies on Early Symptomatic Oral Cancer Diagnosis
Studies on diagnostic delay gather an important number of biases, particularly those reporting on patient self-referred data, and this circumstance seriously limits their validity.
Biases are difficult to control in these studies mainly because of methodological restrictions, as randomised trials are impossible due to ethical reasons. Surprisingly, this problem is frequently ignored and rarely discussed in scientific literature on diagnostic delay.
For instance, hospital-based reports [27,28,29,30,31,32,33,34,35] tend to experience a selection bias, whereas community-based samples [22, 36] would ease generalisation of the obtained results to the entire study population. Another interesting example is the recall bias inherent to retrospective studies [28, 33], which may be diminished by checking patient self-referred data against their relatives [30,31,32] or their primary care clinicians [19, 32]. This effort is particularly important in this type of studies, as prospective studies on this issue are virtually impossible [22]. Certain research groups have obtained their data for clinical records, either from hospitals [28] or from primary care units [22, 36], being perhaps these ones less prone to bias, as clinicians use to record each visit detailing the reason for attendance, a tentative diagnosis and the treatment established for the patient. Particular attention has to be paid to the circumstance known as “Will Rogers phenomenon” occurring when not all patients are assessed using the same methods that can alter the results of the investigation [35].
Potential confounders have to be controlled for, namely, age [19, 28,29,30,31,32,33,34], tumour site, [28, 29, 34] degree of malignancy [36], degree of differentiation [30, 31] and co-morbidity [19, 29]. The aggressiveness of the tumour is a particularly an important factor, as survival is affected more by the proliferative activity of the neoplasm than by the actual delay in diagnosis [30] (less aggressive cancers may show good prognosis despite long delays, and more aggressive ones may have a worse prognosis without any diagnostic delay).
Another relevant issue is the differences in referral protocols, as different prioritisation policies may well imply a “confounding-by-indication” bias in observational studies [34]. Finally, it is worth mentioning that a dichotomised criteria for defining delay in diagnosis (either by arbitrary time points or statistic parameters) may also introduce a bias which could be avoided by analysing time periods as a continuous variable.
4.5 Are there Standardised Definitions for Diagnostic Delay in Oral Cancer?
Even the most widely used intervals, such as “patient delay” [22, 34, 37, 38], and “professional delay” [39,40,41,42], are not consistent in the literature because of the different milestones used to define them. These variations are particularly wide when defining the “total delay”, as in some groups the end point of their studies is the date of biopsy [43], the date of the pathological diagnosis [7, 27], the first consultation with the treating specialist [34] or the date of treatment [44].
Additional time periods have been identified where delays may exist due to the patient (appraisal, illness, behavioural and scheduling delays) [32], primary care system (referral delay) [43, 44], waiting list (specialised care scheduling interval) [44], specialist delay [32, 45] and pretreatment delay [28, 44]. The final interval of the patients’ pathway has been defined as the period between the surgical treatment and the beginning of radiotherapy [46] (Table 4.1).
A marked heterogeneity has also been observed in the way in which the outcomes of diagnostic delay have been presented in the shape of a continuous [37, 47] or a categorical variable [22, 28, 34]: when expressed as a dichotomous variable, the criterion for delay was either arbitrarily established or based upon central trend statistics of the distribution (> 3 weeks [40,41,42,43,44,45,46,47,48]; > 30 days [32, 46]; > de 45 days [31]; > 6 weeks [49]; > 2 months [50]; > 3 months [51]). Anyhow, there is no consensus on the time point beyond which a diagnosis should be considered delayed [8]. The same difficulties apply to head and neck carcinomas (Table 4.2).
4.6 Theoretical Frameworks, Key Points and Time Intervals on Early Oral Cancer Studies
Bearing in mind that studies on delays in diagnosis of oral cancer do not use any theoretical framework and also that the classical approach (patient and professional delay) is inefficient for monitoring the patients’ pathway towards the definitive diagnosis, a consensual research model has been recommended for identifying targets for interventions aimed at an early diagnosis to improve the prognosis of the disease [52].
This model of pathways to treatment [16] describes a series of events, processes, intervals and contributed factors involved in the path to the diagnosis of a symptomatic cancer and allows potential generalisations to different cancer sites and health systems [52, 53]. These events define milestones (detection of bodily changes, perception of reasons to discuss symptoms with a healthcare professional (HCP), first consultation with a HCP, diagnosis and treatment start) which in turn delineate four time intervals (appraisal, help-seeking, diagnostic and pretreatment). The main advantage of this model over the previous ones is that it is dynamic and bidirectional, without a predefined starting point, and also that it permits multiple variations in the course to final diagnosis [52, 53].
This framework (Aarhus statement) discourages the use of the term “delay”, due to its evident implications, and recommends the word “interval” as a more accurate one. However, the term “delay” has gained acceptance over the years, and the number of investigations describing intervals or stages without using it is scarce [21, 23, 24].
In an attempt to ease data comparison among reports and to improve the methodology used in this field, the Aarhus guidelines strongly recommend the use of four important dates: date of the first symptoms (bodily sensation or visible alterations), date of first presentation (first consultation with a HCP professional), date of referral (primary care provider to specialist in cancer diagnosis/management) and date of diagnosis [16, 52].
These dates define time intervals named “time to presentation”, “time to diagnosis” and “time to treatment” [52] (Fig. 4.2).
4.7 Contributing Factors to a Delayed Diagnosis in Oral Cancer. Who Is to Blame?
Mostly, studies on diagnostic delay in oral cancer or early diagnosis use a biological approach (with no theoretical scaffold) and distribute responsibilities for the delays at each time interval (patient delay [19, 28, 34], provider/professional delay [19, 28, 34], specialist delay [32, 44] and appointment/hospital/system delay [28]. An evident weakness of this conceptualisation is the existence of some overlaps [52], as different agents may act simultaneously at the same interval [54]. The Aarhus statement suggests grouping these agents as contributing factors related to patients, to healthcare providers and health system and to the disease (tumour-depending factors) [16].
4.7.1 Patient Interval. Reasons for the Delay
Güneri has recently summarised a limited number of studies to quantify this time interval within a range of 3 to 5.4 months [12], although some authors suggest a patient interval of about 3 weeks as a reasonable one [48]. Thus, the persistence of a bodily change beyond 3 weeks would make the patients seek professional advice [29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52]. This patient interval, also known as symptom interval or time to presentation, accounts for the main component of the overall time to diagnosis and treatment of oral cancer, perhaps due to cognitive and psychosocial factors, such as fate, symptom interpretation, misattribution (to infection or dental problems), belief that the symptom is trivial, stoicism and fear and also because of lack of knowledge about oral cancer [41, 51, 55]. Another factors related to longer patient interval are socioeconomic status [48], alternative medicine [34] and certain health-related behaviours (sexually transmitted disease) [40]. Apart from the difficulties some patients experience to tell symptoms as potentially dangerous (Fig. 4.3) [55], the absence of pathognomonic signs or symptoms of oral cancer may also have a role in the length of this interval. Conversely, a sore, non-healing ulceration and the worsening or persistence of the symptoms seem to be important factors to prompt patient demand for professional help [41].
The duration of the patient interval also has to do with the characteristics of the health system, such as availability [51] and accessibility [12, 54] to care. Any intervention focused at reducing this interval should increase patient awareness of early signs and symptoms of oral cancer and at easing access to the healthcare systems.
4.7.2 Healthcare Providers and System Factors in Diagnostic Delay
The interval attributed to primary care has consistently shown to be shorter than the patient interval [12]. This difference has been estimated in a 2.4 ratio (1.5–4.0) [15]. Both intervals (patient interval and primary care interval) define the pre-referral period [15, 17], which is paramount because a long pre-referral interval has proved to be a risk factor for advanced stage and mortality from oral cancer [14].
The main causes of primary care delays include a low index of suspicion and lack of knowledge about oral cancer [1], together with a lack of familiarity and experience with the disease [8], which has been shown to contribute to delayed referral and treatment [8]. Research has concluded that a standard time interval for a patient to be referred to a specialised service would range between 2 days [56] and 2–3 weeks, according to clinical guidelines [40, 57].
Oral cancer is a particular type of cancer, in the sense that diagnostic biopsies can be taken at the primary care level [70, 79], although this possibility is rarely undertaken, as the number of general dental practitioners performing biopsies ranges from 7% (Turkey [58]), 12% in Northern Ireland [59], or 21% in the UK [2] to 32% in Spain [60]. This circumstance has been put down to a training focused on theoretical aspects rather than on experience or clinical skills. In this situation, the approach “no biopsy and immediate referral” is more common, and a good referral letter and the existence of fast track for these patients become paramount. There are some evidences on the absence of differences in terms of diagnostic, treatment or total delays when the pathological diagnosis was established at the pre-referral period vs patients biopsied at a specialised setting [61].
The diagnostic interval has been defined as the period since first consultation with a HCP until definitive diagnosis [16] (the former concept of “professional delay”) [8]. The key points in this interval include the first investigation by the HCP responsible for the patient, first referral to specialised care, first contact with a specialist and definitive diagnosis [16]. This period has been estimated to range between 14 and 21 weeks [12] for oral cancer, although this information comes from studies with a series of methodological weaknesses.
Besides, planning and scheduling a tailored treatment for cancer are complex tasks undertaken during the “pretreatment” interval, which finishes when the treatment is begun. It is somehow surprising that this time period is not usually considered when investigating early diagnosis of oral cancer [19], as reports tend to consider the final pathological diagnosis as the final point of their research [7, 28, 32, 34]. This decision could influence their results particularly when the outcome of the study is patient survival after treatment. Actually, waiting times for surgery and radiotherapy (pretreatment interval) could be an issue in oral cancer, as waiting times prior radiotherapy have an influence on disease progression in head and neck carcinomas [62, 63], although not all studies on this topic support this conclusion. In this situation, and despite that the final event of the Aarhus statement model is “start to treatment” [53], it seems reasonable to consider some other events in the pathway to treatment, such as delays in the pathological processing time of surgical specimens, which may also contribute to delays and to increase the mortality by oral cancer [64].
4.7.3 Disease Factors Influencing the Time to Diagnosis (Tumour Features)
Oral cancer is a relatively proliferative neoplasm with a heterogeneous biological behaviour, being more aggressive those showing HPV negativity, aneuploidy and TP-53 mutations. Other factors to be taken into account are the expression of a series of oncogenic markers, namely, p16, p21, p27, MDM2, MGMT, ERBB2, RARB, MYC, BCR-ABL1, RAS, CCND1, STAT-3 and VGEF, which cause a faster clinical course and reduce the chances for a diagnosis at early disease stages. Some studies on proliferation of head and neck carcinomas have shown these tumours are able to duplicate their size in periods as short as 3 months [65]. Conversely, HPV-positive neoplasms, mostly within the oropharynx, and mainly wild-type TP-53 have elicited a positive prognosis.
Another important idea to keep in mind when investigating diagnostic delay is that tumours of the same type can appear to be similar, but their growth rates may be very different, as well as their aggressiveness [7]. Thus, patients with fast-growing tumours could be diagnosed early but at advanced stages, which may explain why shorter patient and professional delays have been linked to advanced stages in some oral cancer series [22, 26, 27]. We have recently demonstrated in a multivariate study that when the statistical analysis is adjusted for tumour stage at diagnosis (I–II vs III–IV), proliferative activity is an independent factor for survival and diagnostic delay has no influence on the outcome [30]. Therefore, survival to oral cancer may be more affected by the tumour growth rate than by time intervals to diagnosis. Even though some researchers link diagnostic delay to tumour stage [32], it is possible that this link may be veiled by the fact that certain cancers remain silent during their initial stages and cause symptoms only when they reach an advanced phase (silent tumour hypothesis) [7]. In these situations, the tumour growth rate can be considered a confounding factor in the relationship between diagnostic delay and tumour stage, since patients with aggressive tumours and poor prognosis do not usually show a delayed diagnosis, whereas less proliferating tumours demonstrate good prognosis despite long diagnostic delays [66, 67].
Tumour site has been also found to influence the time interval to diagnosis [68], as tumours located on the floor of the mouth, retromolar trigone and gingivae have shown significantly more extension at the moment of diagnosis [31]. When case series include tumours at different locations, a confounding factor is introduced because the patient’s self-perception and self-exploration abilities greatly depend on where the lesion is located [37, 45].
Another example of the influence of the site of the tumour is the gingiva: these locations are frequently associated to advanced stages at diagnosis due to the early invasion of neighbouring tissues (T4 primary tumour) rather independently of the time elapsed [38].
The circumstance of tongue cancer (Fig. 4.4) is interesting [22, 36], as shorter delays seem to impair survival. This paradox has been previously described in endometrial, cervix, lung, colon, renal and urethral cancer and highlights the role of the biological aggressiveness of the cancer [8, 13, 25].
Cancer on other sites close to the oral cavity elicit opposing results: patient-related delays longer than 2 months result in higher mortality rates, especially for oropharyngeal and nasopharyngeal carcinomas [26], although a recent investigation failed to establish a link between delay in diagnosis and survival to pharyngeal cancer [22]. For larynx carcinomas, diagnostic delays were found to be an independent prognostic factor for survival, as clinician-related delays exceeding 6 or 12 months were associated to worse survival rates [22], as occurred with the overall delay is considered.
In any case, the inconsistencies observed in the association between diagnostic delay and outcome in terms of tumour stage and/or survival could well be related to the variability in the biological behaviour of the neoplasms, and differences in tumour aggressiveness would explain tumour’s stage at diagnosis and patient survival better than would the mere length of the time interval to diagnosis.
4.8 Practical Implications and Suggestions for Future Research
There seems to be a change in the paradigm of oral symptomatic cancer. The need for quality data, for quantifying time intervals till diagnosis and treatment and for identifying and prioritising targets for future interventions aimed at avoiding delayed diagnoses has favoured the usage and development of theoretical models for monitoring the patients’ pathway from the first sign or symptom until the beginning of their treatments. The adherence to the Aarhus guidelines would permit the minimisation of biases and the retrieval of data that are comparable, although some modifications are required to adapt this general framework to the particularities of oral cancer.
Efficient tools have also to be developed if we are to obtain reliable data from self-reported patient experiences, as the reasons for delays at stages involving mainly patients are poorly understood [69].
Apart from patients’ or professionals’ delays, new agents potentially responsible for diagnostic delays have been incorporated to the initial model, which highlight the role of accessibility, defined as “the ability to obtain services based on patients’ health needs” that has to be prioritised in the health systems [70] (Fig. 4.1).
Conclusion
Likewise, strategies for increasing public awareness and knowledge about signs, symptoms and risk factors may decrease the burden of head and neck cancer [71], particularly among high-risk groups. Cancer educational campaigns have demonstrated to significantly increase patients’ knowledge of symptoms and risk factors, although it is not known whether this knowledge actually changes patients’ behaviour [72]. Moreover, and despite that there is no evidence that educational interventions reduce primary care delay in cancer diagnosis, training on specific skills for physicians and dentists should be facilitated [73]. The efficacy of current community-based oral cancer awareness campaigns seems to be limited [74], so future campaigns should incorporate theoretical models, target high-risk groups and consider the groups towards they are addressed within their sociocultural context to obtain better results.
References
Warnakulasuriya S. Global epidemiology of oral and oropharyngeal cancer. Oral Oncol. 2009;45:309–16.
Johnson NW, Warnakulasuriya S, Gupta PC, Dimba E, Chindia M, Otoh EC, et al. Global oral health inequalities in incidence and outcomes for oral cancer: causes and solutions. Adv Dent Res. 2011;23:237–46.
Warnakulasuriya S. Living with oral cancer: epidemiology with particular reference to prevalence and life-style changes that influence survival. Oral Oncol. 2010;46:407–10.
Krishna Rao SV, Mejia G, Roberts-Thomson K, Logan R. Epidemiology of oral cancer in Asia in the past decade- an update (2000-2012). Asian Pac J Cancer Prev. 2013;14:5567–77.
Warnakulasuriya S. Significant oral cancer risk associated with low socioeconomic status. Evid Based Dent. 2009;10:4–5.
Brandizzi D, Chuchurru J, Lanfranchi H, Cabrini R. Analysis of the epidemiological features of oral cancer in the city of Buenos Aires. Acta Odontol Latinoam. 2005;18:31–5.
Scott SE, Grunfeld EA, McGurk M. The idiosyncratic relationship between diagnostic delay and stage of oral squamous cell carcinoma. Oral Oncol. 2005;41:396–403.
Gómez I, Warnakulasuriya S, Varela-Centelles PI, et al. Is early diagnosis of oral cancer a feasible objective? Who is to blame for diagnostic delay? Oral Dis. 2010;16:333–42.
Gómez I, Seoane J, Varela-Centelles P, Diz P, Takkouche B. Is diagnostic delay related to advanced-stage oral cancer? A meta-analysis. Eur J Oral Sci. 2009;117:541–6.
Silverman S, Kerr AR, Epstein JB. Oral and pharyngeal cancer control and early detection. J Canc Educ. 2010;25:279–81.
McGurk M, Chan C, Jones J, O'regan E, Sherriff M. Delay in diagnosis and its effect on outcome in head and neck cancer. Br J Oral Maxillofac Surg. 2005;43:281–4.
Güneri P, Epstein JB. Late stage diagnosis of oral cancer: components and possible solutions. Oral Oncol. 2014;50:1131–6.
Neal RD. Do diagnostic delays in cancer matter? Br J Cancer. 2009;101:S9–S12.
Seoane J, Alvarez-Novoa P, Gomez I, Takkouche B, Diz P, Warnakulasiruya S, Seoane-Romero JM, Varela-Centelles P. Early oral cancer diagnosis: the Aarhus statement perspective. A systematic review and meta-analysis. Head Neck. 2015;38:E2182.
Lyratzopoulos G, Saunders CL, Abel GA, McPhail S, Neal RD, Wardle J, et al. The relative length of the patient and the primary care interval in patients with 28 common and rarer cancers. Br J Cancer. 2015;112:S35–40.
Weller D, Vedsted P, Rubin G, Walter FM, Emery J, Scott S, et al. The Aarhus statement: improving design and reporting of studies on early cancer diagnosis. Br J Cancer. 2012;106:1262–7.
Neal RD, Tharmanathan P, France B, Din NU, Cotton S, Fallon-Ferguson J, et al. Is increased time to diagnosis and treatment in symptomatic cancer associated with poorer outcomes? Systematic review. Br J Cancer. 2015;112:S92–107.
Pack GT, Gallo JS. The culpability for delay in treatment of cancer. Am J Cancer. 1938;33:443–62.
Allison P, Locker D, Feine JS. The role of diagnostic delays in the prognosis of oral cancer: a review of the literature. Oral Oncol. 1998;34:161–70.
Shafer WG. Initial mismanagement and delay in diagnosis of oral cancer. J Am Dent Assoc. 1975;90:1262–4.
Bruun JP. Time lapse by diagnosis of oral cancer. Oral Surg Oral Med Oral Pathol. 1976;42:139–49.
Teppo H, Alho OP. Relative importance of diagnostic delays in different head and neck cancers. Clin Otolaryngol. 2008;33:325–30.
Onizawa K, Nishihara K, Yamagata K, Yusa H, Yanagawa T, Yoshide H. Factors associated with diagnostic delay of oral squamous cell carcinoma. Oral Oncol. 2003;39:781–8.
Peacock ZS, Pogrel MA, Schmidt DC. Exploring the reasons for delay in treatment of oral cancer. J Amer Dent Assoc. 2008;139:1346–52.
Crawford SC, Davis JA, Siddiqui NA, Caestecker L, Ch G, Hole D, et al. The waiting time paradox: population based retrospective study of treatment delay and survival of women with endometrial cancer in Scotland. BMJ. 2002;325:196.
Seoane J, Takkouche B, Varela-Centelles P, Tomás I, Seoane-Romero JM. Impact of delay in diagnosis on survival to head and neck carcinomas: a systematic review with meta-analysis. Clin Otolaryngol. 2012;37:99–106.
Jovanovic A, Kostense PJ, Schulten EAJM, Snow GB, van der Waal I. Delay in diagnosis of oral squamous cell carcinoma; a report from the Netherlands. Oral Oncol. 1992;28B:37–8.
Morelatto RA, Herrera MC, Fernandez EN, Corball AG, Lopez de blanc SA Diagnostic delay in oral squamous cell carcinoma in two diagnostic centres in Cordobe Argentina. J Oral Pathol Med 2007;36: 405–408.
Scott SE, Grunfeld EA, Auyeung V, McGurk M. Barriers and triggers to seeking help for potentially malignant symptoms: implications and interventions. J Public Health Dent. 2009;69:34–40.
Seoane J, Pita S, Gómez I, Vazquez I, et al. P. Proliferative activity and diagnostic delay in oral cancer. Head Neck. 2010;32:1377–84.
Seoane-Romero JM, Vázquez-Mahía I, Seoane J, Varela-Centelles P, Tomás I, López-Cedrún JL. Factors related to late stage diagnosis of oral squamous cell carcinoma. Med Oral Patol Oral Cir Bucal. 2012;17:e35–40.
Brouha XD, Tromp DM, Hordijk GJ, Winnubst JA, de Leeuw JR. Oral and pharyngeal cancer: analysis of patient delay at different tumor stages. Head Neck. 2005;27:939–45.
Sandoval M, Font R, Mañós M, Dicenta M, Quintana MJ, Bosch FX, et al. The role of vegetable and fruit consumption and other habits on survival following the diagnosis of oral cancer: a prospective study in Spain. Int J Oral Maxillofac Surg. 2009;38:31–9.
Kerdpon D, Sriplung H. Factors related to advanced stage oral squamous cell carcinoma in southern Thailand. Oral Oncol. 2001;37:216–21.
Rubright WC, Hoffman HT, Lynch CF, Kohout FJ, Robinson RA, Graham S, et al. Risk factors for advanced-stage oral cavity cancer. Arch Otolaryngol Head Neck Surg. 1996;122:621–6.
Kantola S, Jokinen K, Hyrynkangas K, Mäntyselkä P, Alho OP. Detection of tongue cancer in primary care. Br J Gen Pract. 2001;51:106–11.
Wildt J, Bundgaard T, Bentzen SM. Delay in the diagnosis of oral squamous cell carcinoma. Clin Otolaryngol. 1995;20:21–5.
Gao W, Guo CB. Factors related to delay in diagnosis of oral squamous cell carcinoma. J Oral Maxillofac Surg. 2009;67:1015–20.
Guggenheimer J, Verbin RS, Johnson JT, Horkowitz CA, Myers EN. Factors delaying the diagnosis of oral and oropharyngeal carcinomas. Cancer. 1989;64:932–5.
Pitiphat W, Diehl SR, Laskaris G, Cartsos V, Douglass CW, Zavras AI. Factors associated with delay in the diagnosis of oral cancer. J Dent Res. 2002;81:192–7.
Rogers SN, Vedpathak SV, Lowe D. Reasons for delayed presentation in oral and oropharyngeal cancer: the patients’ perspective. Br J Oral Maxillofac Surg. 2010;49:349–53.
Esmaelbeigi F, Hadji M, Harirchi I, Omranipour R, van Rajabpour M, Zendehdel K. Factors affecting professional delay in diagnosis and treatment of oral cancer in Iran. Arch Iran Med 2014;17:253–7.
Holmes JD, Dierks EJ, Homer LD, Potter BE. Is detection of oral and oropharyngeal squamous cancer by a dental health care provider associated with a lower stage at diagnosis? J Oral Maxillofac Surg. 2003;61:285–91.
McLeod NM, Saeed NR, Ali EA. Oral cancer: delays in referral and diagnosis persist. Br Dent J. 2005;198:681–4.
Tromp DM, Brouha XD, De Leeuw JR, Hordijk GJ, Winnubst JA. Psychological factors and patient delay in patients with head and neck cancer. Eur J Cancer. 2004;40:1509–16.
Bastit L, Blot E, Debourdeau P, Menard J, Bastit P, Le Fur R. Influence of the delay of adjuvant postoperative radiation therapy on relapse and survival in oropharyngeal and hypopharyngeal cancers. Int J Radiat Oncol Biol Phys. 2001;49:139–46.
Cooke BE, Tapper-Jones L. Recognition of oral cancer. Causes of delay. Br Dent J. 1977;142:96–8.
Llewellyn CD, Johnson NW, Warnakulasuriya KA. Risk factors for oral in newly diagnosed patients aged 45 years and younger: a case-control study in southern England. J Oral Pathol Med. 2004;33:525–332.
Pitchers M, Martin C. Delay in referral of oropharyngeal squamous cell carcinoma to secondary care correlates with a more advanced stage at presentation, and is associated with poorer survival. Br J Cancer. 2006;94:955–8.
Tong XJ, Shan ZF, Tang ZG, Guo XC. The impact of clinical prognostic factors on the survival of patients with oral squamous cell carcinoma. J Oral Maxillofac Surg 2014;72:2497.e1–10.
Kumar S, Heller RF, Pandey U, Tewari V, Bala N, Oanh KTH. Delay in presentation of oral cancer: a multifactor analytical study. Natl Med J India. 2001;14:13–7.
Scott SE, Walter FM, Webster A, Sutton S, Emery J. The model of pathways to treatment: conceptualization and integration with existing theory. Br J Health Psychol. 2013;18:45–65.
Walter F, Webster A, Scott S, Emery J. The Andersen model of Total patient delay: a systematic review of its application in cancer diagnosis. J Health Serv Res Policy. 2012;17:110–8.
Diz Dios P, Padrón González N, Seoane Lestón J, Tomás Carmona I, Limeres Posse J, Varela-Centelles P. Scheduling delay in oral cancer diagnosis: a new protagonist. Oral Oncol. 2005;41:142–6.
Panzarella V, Pizzo G, Calvino F, Compilato D, Colella G, Campisi G. Diagnostic delay in oral squamous cell carcinoma: the role of cognitive and psychological variables. Int J Oral Sci. 2014;6:39–45.
Schnelter JFC. Oral cancer diagnosis and delays in referral. Br J Oral Maxillofac Surg. 1992;30:210–3.
National Institute for Health and Clinical Excellence. (2005). Referral guidelines for suspected cancers. Clinical guideline 27; London; NICE (www.nice.org.uk).
Ergun S, Ozel S, Koray M, Kürklü G, AK G, Tanyeri H. Dentist’s knowledge and opinions about oral mucosa lesions. Int J Oral Maxillofac Surg. 2009;38:1283–8.
Cowan CG, Gregg TA, Kee F. Prevention and detection of oral cancer: the views of primary care dentist in Northern Ireland. Br Dent J. 1995;5:338–42.
López-Jornet P, Camacho-Alonso F. New barriers in oral cancer. Patient accessibility to dental examination. A pilot study. Oral Oncol. 2006;42:1022–5.
Kaing L, Manchella S, Love C, Nastri A, Wiesenfeld D. Referral patterns for oral squamous cell carcinoma in Australia: 20 years progress. Aust Dent J. 2015;61:29.
Jensen AR, Nellemann HM, Overgaard J. Tumor progression in waiting time for radiotherapy in head and neck cancer. Radiother Oncol. 2007;84:5–10.
van Harten MC, Hoebers FJ, Kross KW, van Werkhoven ED, van den Brekel MW, van Dijk BA. Determinants of treatment waiting times for head and neck cancer in the Netherlands and their relation to survival. Oral Oncol. 2015;51:272–8.
Jerjes W, Upile T, Radhi H, Petrie A, Adams A, Callear J, et al. Delay in pathological tissue processing time vs. mortality in oral cancer: short communication. Head Neck Oncol. 2012;26:14.
Seoane Lestón J, Diz Dios P. Diagnostic clinical aids in oral cancer. Oral Oncol. 2010;46:418–22.
Evans SJW, Langdon JD, Rapidis AD, Johnson NW. Prognostic significance of STNMP and velocity of tumour growth in oral cancer. Cancer. 1982;49:7773–6.
Kaufman S, Grabau JC, Lore JH. Symptomatology in head and neck cancer; a quantitative review of 385 cases. Am J Public Health. 1980;70:520–2.
Kowalski LP, Franco EL, Torloni H, Fava AS, Sobrinho JA, Ramos G, et al. Lateness of diagnosis of oral and oropharyngeal carcinoma: factors related to the tumour, the patient and health professionals. Oral Oncol. 1994;30B:167–73.
Richards D. Patient delay in reporting oral cancer is poorly understood. Evid Based Dent. 2007;8:21.
Guay AH. Access to dental care: solving the problem for underserved populations. J Am Dent Assoc. 2004;135:1599–605.
Luryi AL, Yarbrough WG, Niccolai LM, Roser S, Reed SG, Nathan CA, et al. Public awareness of head and neck cancers: a cross-sectional survey. JAMA Otolaryngol Head Neck Surg. 2014;140:639–46.
Sommer L, Sommer DD, Goldstein DP, Irish JC. Patient perception of risk factors in head and neck cancer. Head Neck. 2009;31:355–60.
Mansell G, Shapley M, Jordan JL, Jordan K. Interventions to reduce primary care delay in cancer referral: a systematic review. Br J Gen Pract. 2011;61:e821–35.
Papas RK, Logan HL, Tomar SL. Effectiveness of a community-based oral cancer awareness campaign (United States). Cancer Causes Control. 2004;15:121–31.
Acknowledgements
This work has been supported by the research project PI14/01446, belonging to the Spanish National R&D&I Programme 2013–2016 and co-funded by the ISCIII-Subdirección General de Evaluación y Fomento de la Investigación and the European Regional Development Fund (ERDF).
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Varela-Centelles, P., Seoane, J., García-Pola, M.J., Seoane-Romero, J.M., García Martín, J.M. (2019). Diagnostic Delay in Symptomatic Oral Cancer. In: Panta, P. (eds) Oral Cancer Detection. Springer, Cham. https://doi.org/10.1007/978-3-319-61255-3_4
Download citation
DOI: https://doi.org/10.1007/978-3-319-61255-3_4
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-61254-6
Online ISBN: 978-3-319-61255-3
eBook Packages: MedicineMedicine (R0)