Abstract
Gastric cancer is considered one of the most frequent neoplasm of the old age with a peak in the seventh decade of life. Even if the overall incidence of gastric cancer has been reduced during the last decades, it is expected an increase number of new cases among old patients because of the elderly population is on rise. The clinicopathological features of gastric cancer in elderly patients are different from those of non-elderly patients: male predominance, localization in the lower third of the stomach, more histological differentiation, advanced TNM stage at the diagnosis. In elderly, as for young patients, surgical resection remains the only curative treatment. Preoperative comorbidities and the high risk of postoperative complications influence the surgical approach. For early gastric cancer, endoscopic resection is performed when there is no evidence of lymph node metastasis. For advanced cases, if feasible, performing a subtotal gastrectomy with limited lymphadenectomy offers a better quality of life and lower mortality rather than total gastrectomy associated to extended nodes dissection, with no significant difference in overall survival. After surgery, adjuvant chemotherapy should be determined by considering the conditions of individual patients and their life expectancies.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
1 Epidemiology
In recent decades, socioeconomic habits and new medical knowledge have improved average life expectancy and quality of life as well. As a direct consequence, the geriatric population is progressively expanding, as is the risk of developing cancer.
Gastric tumour represents the fourth most common malignancy worldwide, after cancers of the lung, breast and colorectum.
The worldwide incidence of gastric neoplasm has declined rapidly over the last few decades [1]. Part of the decline may be due to the recognition of certain risk factors such as Helicobacter pylori and other dietary and environmental risks. Refrigerators have improved the storage of food, thereby reducing salt-based preservation of food and preventing bacterial and fungal contamination.
Despite the decrease in the global incidence of this disease, in endemic areas, such as Japan and Latin American countries, gastric cancer is still a major cause of mortality.
According to the Italian Network of Cancer Registries [2], gastric cancer is currently in sixth place in order of incidence among both men and women (4% of all cancers in males and 4% in females), and in 2016 new cases are expected to be nearly 13,000. This distribution is almost entirely attributable to the incidence in older age (over 70 years). Gastric tumour is considered a disease of the old age with a peak of incidence in the seventh decade of life. Although there is not a standard definition of “elderly”, the most scientific papers fix the age of 70 as the threshold. The average human life expectancy is increasing worldwide and with it also the proportion of elderly people. This is predicted to continue to increase in the coming decades [3]. As a consequence, also the incidence of gastric carcinoma in elderly patients is becoming more frequent. In Italy, the 5 years overall survival is 32.4%, higher than the European average (25.1%). The overall survival in elderly patients is lower than in non-elderly ones: 22.1 versus 41.0% [2].
2 Risk Factors
The entire process of gastric carcinogenesis involves several factors, such as, gender, age, diet, tobacco and alcohol consumption, H. pylori infections, chronic gastritis, pernicious anaemia, some type of stomach polyps and previous gastric surgery.
Stomach cancer is more common in men than in women, and, as already discussed, there is a sharp increase in people over the age of 70. An increased risk of stomach cancer is seen in people with diets that have large amounts of smoked foods, salted fish and meat and pickled vegetables. Nitrates and nitrites are substances commonly found in cured meats; they can be converted into compounds that have been shown to cause stomach cancer in lab animals. A reduced consumption of fresh fruit and vegetables is another dietary behaviour implicated in gastric carcinogenesis. The rate of stomach cancer is about doubled in smokers and is related to the duration and intensity of smoking. Smoking increases stomach cancer risk, particularly for cancers of the upper portion of the stomach, near the oesophagus [4]. On the other hand, several studies suggest that alcohol consumption increases the risk of cancer in the lower stomach.
It is demonstrated that H. pylori infection is frequent in areas of high gastric cancer incidence. Infection with H. pylori bacteria seems to be a major cause of stomach cancer, especially cancers located in the distal part of the stomach. On the contrary, this infection seems not to be related with tumours of the gastroesophageal junction. Chronic gastritis associated with pernicious anaemia is related with gastric malignancy. Chronic gastritis is often associated with intestinal metaplasia and mucosal dysplasia which are frequently observed in the mucosa adjacent to gastric cancer. Pernicious anaemia is a disease characterized by fundic mucosal atrophy, loss of parietal and chief cells, hypochlorhydria and hypergastrinemia, and it is present in 3% of people over 60 years. Polyps are growths on the lining of the stomach, and most types, such as hyperplastic polyps or inflammatory polyps, do not seem to increase the risk of gastric cancer. Endoscopic removal is a sufficient treatment; subsequent surveillance is also not necessary. In contrast, adenomatous polyps, also called adenomas, can sometimes develop into cancer; in fact dysplasia and carcinoma in situ develop inside these growths. The carcinogenesis risk has been estimated at 10–20%, and it is higher for polyps of more than 2 cm in diameter.
Gastric cancer is more likely to develop in people who have undergone previous partial gastrectomy, for example, due to a gastric ulcer. This condition is called “remnant gastric cancer”. The effective mechanism is unknown, but the potential factors seem to be the decrease of luminal pH, bacterial overgrowth with increased productions of N-nitroso carcinogens and reflux of bile acids into the stomach.
Another known risk factor is obesity, probably because of the high incidence of chronic gastroesophageal reflux disease found in obese subjects.
3 Clinicopathological Features
The clinicopathological features of gastric cancer in elderly patients are different from those of non-elderly patients [5].
3.1 Gender
Many studies have shown a male predominance in elderly patients with gastric cancer, both in endemic and nonendemic areas [6]. The meaning of this is not clear, but the prolonged exposure of the elderly male population to environmental carcinogens may play a significant role. In young patients, most authors suggest a female predominance, maybe because of the influence that oestrogens have on this pathology [7].
3.2 Location
Gastric cancer can develop both in the proximal and the distal regions. These represent two distinct entities from an epidemiological, biological, genetical and clinical point of view. Proximal tumours are more common in younger people and include tumours of the cardia and gastroesophageal junction, which currently represent about 40% of all gastric tumours. Epidemiological and morphological data shows that the majority of adenocarcinomas of the gastroesophageal junction have characteristics more similar to tumours of the oesophagus than those of the stomach. On the other hand, the majority of studies have documented; the predominance of lower or distal third gastric cancer in the elderly has been significantly more frequent than that observed in younger patients [8].
3.3 Macroscopic Features
Gastric cancer can be divided into two main entities: early and advanced gastric cancer. Early gastric cancer is defined as a tumour whose growth is confined to the mucosa and the submucosa regardless of the presence or absence of metastatic disease in the perigastric lymph nodes. The presence of lymph node metastasis is closely related to the depth of local invasion. With the submucosal invasion, lymph nodes are involved in 15–20% of cases, whereas when lesions are confined to the mucosa, lymph node involvement is uncommon (≤3%) [9]. A tumour having passed through the submucosa is defined as advanced. Macroscopic appearance, of both early and advanced stages, of gastric cancer seems to be influenced by age. According to the Japanese endoscopic classification of early gastric cancer, the most common macroscopic type in elderly people is the superficial depressed (IIc), followed by type IIa (superficial elevated) and polypoid type (I). Following Borrmann’s classification of advanced gastric cancer (type I for polypoid growth, type II for fungating growth, type III for ulcerating growth and type IV for diffusely infiltrating growth which is also referred to as linitis plastica), the most prevalent type in elderly patients is the type III.
Many studies show a significant difference regarding mean tumour size, which tends to be larger in elderly patients than in younger patients [8].
3.4 Histological Features
Gastric cancer occurs in two distinct histological subtypes, intestinal and diffuse, as described in Lauren’s classification. In the intestinal form, the malignant cells tend to form glands, and it is often associated with chronic atrophic gastritis, intestinal metaplasia and dysplasia. This subtype is more common in populations at high risk, and it occurs with increased frequency in men and older patients. For the other type, the diffuse form, the gland-forming growth is not proven, and it is prevalent in younger patients, in women and in populations with a relatively low incidence of gastric cancer. According to the criteria described by Ming and Esaky, the well-differentiated form of gastric adenocarcinoma is the predominant type in elderly patients. On the other hand, in younger patients the most common pattern is a poorly differentiated tumour. Many studies have suggested in elderly people a progression from a differentiated tumour to an undifferentiated neoplasia, whereas, in younger patients, gastric cancer manifests as an undifferentiated tumour at the initial stage [10].
3.5 Clinical Presentation
Symptoms in gastric cancer are unfortunately not specific, and they can usually closely mimic those associated with a number of non-neoplastic gastroduodenal diseases, especially benign gastric ulcer. One of the most common symptoms in the early stage of gastric cancer is epigastric pain, which is present in over 70% of patients and consists of a constant, nonradiating pain which is unrelieved by food ingestion. Symptoms as anorexia, nausea and weight loss are characteristic of the advanced stage. Dysphagia is present in 20% of patients with proximal gastric lesions. Gastrointestinal haemorrhage is present in only 5% and perforation is rare (1%). Cachexia, abdominal mass, hepatomegaly and supraclavicular adenopathy usually indicate metastatic disease. In elderly patients, the onset of symptoms is commonly related to an advanced stage of the disease. A study has shown that gastric cancer incidence in individuals without alarm symptoms is very low [11].
3.6 Family History
Familial gastric cancer is generated by a germline mutation of CDH1 gene which encodes the adhesion molecule E-cadherin, inherited by the autosomal dominant mode; it is generally associated to a poorly differentiated, infiltrative and diffuse histotype adenocarcinoma and is more common in younger patients.
3.7 Comorbidities
As shown by several studies, elderly patients have significantly more preoperative comorbidities such as cardiovascular disease, including hypertension, atrial fibrillation, ischemic heart disease, heart failure and valvular heart pathology than their younger counterparts [12]. Elderly people are characterized by a loss of renal cortical mass that reflects on a decline of renal function, the homeostatic reserve and electrolyte disorders [13, 14]. Serum creatinine may remain stable masking the underlying progressive loss of renal function. Regarding ageing modifications of pulmonary function, it is demonstrated that forced expiratory volume 1 and vital capacity, blood O2 level and lung elastic recoil are decreased. Older patients tend to have a poorer preoperative nutritional status shown by low levels of albumin in blood. Preoperative albumin levels have been shown to predict postoperative outcomes [15], and preoperative nutritional support with intravenous hyperalimentation is essential in these patients.
3.8 Synchronous Carcinomas
With regard to the incidence of multiple synchronous gastric carcinomas, many studies suggest that they are more prevalent among elderly patients and their incidence increases with advancing age [5]. Endoscopically these tumours are predominantly located in the lower third of the stomach; they are elevated, well-differentiated histological type, and they present the tendency to collide, forming single giant lesions.
3.9 Patterns of Metastasis and Staging
Regarding the pattern of metastasis, many studies demonstrate that glandular/well-differentiated/intestinal gastric cancer, which is the predominant histological type in old patients, is usually associated with haematogenous metastasis predominantly involving the liver via the tumour spreading through the portal vein. The peritoneal invasion occurs less frequently. Regarding the incidence of lymph node metastasis, observations are controversial, but it seems to be less frequent in the elderly as compared to younger patients, and this is confirmed by the examination of autopsy cases of fatal gastric cancer.
4 Diagnoses
Cancer of the stomach is difficult to diagnose before it has spread. There are no specific symptoms in the early stages, and often in elderly patients they result less clear. If stomach cancer is suspected by symptoms, tests will be needed to confirm the diagnosis. Clinical stage is determined through physical examination, blood chemistry, faecal occult blood test (FOBT), gastroscopy and ultrasonography, biopsy and imaging tests. Gastroscopy is the most definitive diagnostic method when gastric neoplasm is suspected. In the initial stages, gastric cancers can appear polypoid, flat, plaque-like lesions or as shallow ulcers. Generally advanced lesions are typically ulcerated. Although gastroscopy is important to identify a lesion, differentiation of benign from malignant gastric ulcers can only be made definitively by biopsy. When the definitive histologic diagnosis is reached, it is important to evaluate the extent of the disease in order to plan the optimal therapeutic choice of treatment.
The aim of the preoperative staging of gastric cancer is to evaluate the depth of tumour infiltration (T-stage), the extent or number of lymph nodes involved (N-stage) and distant metastasis (M-stage) before surgery. Traditional methods of preoperative staging for gastric cancer are usually imaging diagnostic techniques, such as computed tomography (CT), endoscopic ultrasonography (EUS), positron emission tomography (PET) and laparoscopic exploration.
CT is usually used as a diagnostic method to confirm gastric cancer presence, and it can reliably demonstrate infiltration of the gastric wall by tumour, gastric ulceration and the presence of distal metastasis, more frequently involving the liver. Moreover, this method is less reliable in demonstrating the invasion of adjacent organs or the presence of lymphatic metastasis. EUS is a useful tool of preoperative evaluation for locoregional staging of gastric cancer and to investigate the assessment of gastric wall involvement and the presence of infiltrated paragastric lymph nodes. Moreover, another application of EUS is to delineate subepithelial lesions that may be confused with gastric cancer and to guide biopsy of submucosal tumours within the wall of the stomach [16]. A meta-analysis including 22 studies evaluated the usefulness of EUS in stomach cancer, and it has shown that the sensitivity and specificity by stage were 88.1 and 100% for T1, 82.3 and 95.6% for T2, 89.7 and 94.7% for T3 and 99.2 and 96.7% for T4 staging, respectively [17, 18]. The accuracy of EUS presurgical N-stage evaluation is approximately 65–95% [19]. A study has suggested that in patients with locally advanced gastric cancer, PET scan is the most sensitive noninvasive imaging modality for detecting hepatic metastasis [20] and provides better diagnostic accuracy for detection of distant lymph node metastasis and bone metastasis in patients with untreated advanced gastric cancer [21]. However, especially when tumour deposits are small, the ability of radiologic imaging to detect metastatic disease is limited. The surface of the liver, the omentum and the peritoneal surfaces are common sites for gastric cancer metastasis that are difficult to evaluate preoperatively by imaging. In this case, diagnostic laparoscopy is superior to preoperative CT in detection of peritoneal, hepatic or lymphatic metastasis.
5 Treatment
5.1 Surgical Treatment
The indications for surgical treatment in elderly patients with stomach cancer have been gradually expanded. This is because the morbidity and mortality rates from postoperative complications have continued to decrease over time as a result of the improvement of anaesthesiologic techniques, intensive care, surgical devices and less invasive surgical procedures, consequently improving short-term outcomes in elderly patients. Surgical resection is the only hope for cure in gastric cancer, even if an advanced stage of disease at the time of diagnosis precludes curative resection for most patients. Radical resection (R0) represents the only treatment modality which offers possible long-term survival [5]. Data in literature regarding elderly patients with gastric cancer seems to be limited and sometimes conflicting for several reasons.
First of all, elderly patients often have age-associated physiologic problems such as decreased organ reserve and concomitant comorbidities: hypertension, diabetes mellitus, ischemic heart disease, cerebrovascular disease and renal, liver and respiratory dysfunction. Several studies have demonstrated that preoperative risk, evaluated by the ASA score (American Society of Anaesthesiologists), is significantly higher in elderly gastric cancer patients than younger patients, mainly because of the higher rate of concomitant diseases [22].
Secondly, older patients often suffer from different grades of malnutrition, reflected by a low albumin level in blood. A recent Japanese study has shown that preoperative hypoalbuminemia is an independent risk factor of postoperative morbidity and mortality. Furthermore, the important thing to note is that initial hypoalbuminemia can affect early surgical outcomes irrespective of the replacement of albumin [23]. Another study suggests that less invasive surgery should be indicated for patients with serum albumin levels below the 2.9 g/dL cutoff [14]. This serum albumin test could be a reasonably simple and cost-effective method for identifying at-risk patients.
Moreover, gastric cancer in the elderly is often diagnosed at an advanced stage; this may be attributed to the lack of symptoms in the elderly population and to the absence of a mass screening programme for this tumour.
For all these reasons, it is sometimes difficult to treat elderly patients with gastric cancer according to the guidelines [24].
With regard to early gastric cancer, endoscopic resection is performed in selected cases, when there is no evidence of lymph node metastasis. The indication criteria are mucosal cancer of any size without ulceration, mucosal cancer with ulcerations sized less or equal to 30 mm or submucosal cancer less than 30 mm and confined to the upper 0.5 mm of the submucosa without lymph-vascular invasion [25]. In endoscopic resection, the typical sequential procedure included marking, mucosal incision and submucosal dissection with simultaneous haemostasis. With this approach, postoperative bleeding or perforation has been reported in 5%, and in 17%, histological examination revealed submucosal invasion that required further operative treatment [26].
For advanced cancer, the surgical procedure in the elderly must be decided carefully by assessing the patient’s tolerance of surgical stress because, as already shown, elderly patients have declining organ capacity and the quality of life may suffer postoperatively [27].
Although guidelines indicate that gastrectomy associated with D2 lymph node dissection is the gold standard radical treatment for resectable advanced gastric cancer without any exception regarding age or comorbidities, the dominant trend among surgeons is to perform limited surgery such as subtotal gastrectomy [5, 22] in older patients.
The choice of a surgical procedure must guarantee both the control of the disease and a good result in terms of postoperative mortality and survival as well as quality of life, mainly in an aged population with a shorter life expectancy. In fact, total gastrectomy and D2 resection in this age group have been associated with higher rates of postoperative morbidity and mortality as compared to subtotal gastrectomy and D1 resection [28]. Performing a subtotal gastrectomy in the elderly, when technically feasible, is certainly related to a lower mortality and to a 5-year survival rate at least as good as after total gastrectomy, offering a better quality of life.
The suitability of subtotal gastrectomy for elderly patients is also related to the significantly shorter postoperative hospital stay for patients submitted to subtotal gastrectomy than total gastrectomy. Total gastrectomy frequently leads to considerable changes in dietary intake and absorption, which have a decisive influence on the postoperative nutrition status.
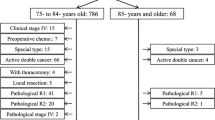
Takeshita et al. have shown that R0 resection with at least limited lymph node dissection should be considered as the treatment of first choice for elderly patients with gastric cancer, especially those between the ages of 80 and 84 years [29]. Similarly, splenectomy or combined resections of adjacent organs are less frequently performed in this group.
According to several studies about the extension of lymph node resection, D1 resection is more frequently performed than D2 resection, especially in patients with comorbidities, while D3 or greater is never performed. Surgical resection accompanied by dissection of a minimum of 14 and optimal 25 lymph nodes is the only modality that is potentially curative [5].
Egushi et al. reported that extended lymphadenectomy in elderly patients did not positively influence the 5-year survival, while it resulted in higher mortality (10 vs 1%) and morbidity rate (57 vs 27%) as compared to limited lymphadenectomy [30]. Another study confirms that after extended nodal dissection, the overall survival in highly comorbid elderly patients, even with nodal involvement, does not show clear benefits owing to the high risk of perioperative complications [31].
5.2 Postoperative Complications
Intraabdominal abscesses and pancreatic fistulae have been reported as major complications after total gastrectomy. They are thought to be associated with lymph node dissection around the pancreas that is why surgeons usually avoid lymph node dissection around the pancreas, particularly among the oldest patients.
Other possible postoperative complications include anastomotic leakage, wound infection, postoperative bleeding that required surgical or endoscopic treatment, anastomotic stenosis, ileus and respiratory and cardiac complications. These could prolong medical hospitalization, increasing costs and wasteful uses of human resources.
In elderly patients, it is not infrequent to see the onset of a postoperative delirium which can cause unexpected medical accidents, such as dementia, that prolong hospital stays and which may be associated with an unfavourable prognosis. It has been reported that 10–50% of elderly patients who undergo surgical treatment develop delirium postoperatively [32]. Although the mechanisms of delirium remain unclear, multiple factors are known to be involved; for example, systemic stress and inflammatory response may play important roles in the development of this condition [33]. Therefore, it is important to reduce perioperative stress to minimize the occurrence of delirium in elderly patients.
Although several reports have indicated that the incidence of postoperative complications increases in elderly patients, the applicability of these results to older patients with gastric cancer is arguably limited.
In fact, according to other research, no significant differences in complications, morbidity and hospital stay duration after surgery were found between patients younger and those older than 80 years [6, 34, 35]. This could be explained by a less invasive surgical procedure performed on these patients.
In order to prevent postoperative complications in the elderly, it is important to evaluate the overall preoperative status and to apply postoperative care depending on the type of surgery tailored to the patient’s condition. Besides surgical complications, it is important to prevent geriatric clinical complications, first and foremost, and pulmonary infections, and nowadays respiratory rehabilitation programmes are emphasized.
A linear relationship is reported between postoperative complications and the number of preoperative abnormal parameters.
5.3 Long-Term Outcomes
Many studies have specifically compared the long-term outcome of gastric cancer in elderly patients with that in younger or middle-aged patients. Some found no significant difference in survival between them [22]. However, most studies confirmed that the prognosis of elderly patients was poorer than that of younger and middle-aged patients [36, 37]. According to a Chinese study, patients aged ≥70 years had a significantly lower 5-year overall survival rate than younger and middle-aged patients [8]. In general, the poor prognosis of elderly patients can be attributed to the delay in diagnosis, advanced tumour stage and also the preoperative condition of the patients.
5.4 Multimodality Treatment for Elderly Gastric Cancer
The use of neoadjuvant chemotherapy may have several potential benefits including the early eradication of micro metastasis and downstaging the disease with the possibility of a curative resection. A recent meta-analysis about neoadjuvant chemotherapy in elderly patients has shown a slightly improved survival rate with no significant increase in operative complications or perioperative mortality [38]. According to ESMO Guidelines working group, adjuvant chemotherapy and radiotherapy are recommended for elderly patients with high risk gastric cancer in an attempt to reduce local or distant recurrence and to improve survival after curative resection [24]. In the past, the majority of oncologists were hesitant to prescribe adjuvant chemotherapy to elderly patients because of the high risk of complications and for the toxicity of drugs due to changes in pharmacodynamic features in these patients. However, it has been demonstrated that there are no significant differences in terms of overall survival and pharmacological toxicity between younger and older patients without any severe comorbidity. Although the addition of adjuvant chemotherapy after curative gastrectomy for gastric cancer in general shows potential survival benefit, the need for such treatment in elderly patients should be determined by considering the conditions of individual patients and their life expectancies. However, patients should be strongly involved in decision making in undergoing or in discontinuing adjuvant chemotherapy: they may be more interested in quality than duration of life. For patients who cannot undergo surgical treatment because of relapsed or metastatic gastric cancer, palliative chemotherapy can provide palliation of symptoms, improving the quality of life. In conclusion, data clearly shows that age alone is not sufficient to estimate the general performance status of an elderly patient and their eligibility for curative or palliative treatment.
References
Zhu A, Sonnenberg A. Is gastric cancer again rising? J Clin Gastroenterol. 2012;46(9):804–6.
[Internet]. Available from: http://www.registri-tumori.it/PDF/AIOM2016/I_numeri_del_cancro_2016.pdf.
Nashimoto A, Akazawa K, Isobe Y, Miyashiro I, Katai H, Kodera Y, et al. Gastric cancer treated in 2002 in Japan: 2009 annual report of the JGCA nationwide registry. Gastric Cancer. 2012;16(1):1–27.
Moy K, Fan Y, Wang R, Gao Y, Yu M, Yuan J. Alcohol and tobacco use in relation to gastric cancer: a prospective study of men in shanghai, China. Cancer Epidemiol Biomark Prev. 2010;19(9):2287–97.
Saif M, Makrilia N, Zalonis A, Merikas M, Syrigos K. Gastric cancer in the elderly: an overview. Eur J Surg Oncol. 2010;36(8):709–17.
Kunisaki C, Akiyama H, Nomura M, Matsuda G, Otsuka Y, Ono H, et al. Comparison of surgical outcomes of gastric cancer in elderly and middle-aged patients. Am J Surg. 2006;191(2):216–24.
Kim H, Kim J, Lim B, Kim H, Kim H, Park J, et al. Sex disparity in gastric cancer: female sex is a poor prognostic factor for advanced gastric cancer. Ann Surg Oncol. 2016;23(13):4344–51.
Liang Y, Liang Y, Deng J, Guo H, Ding X, Wang X, Wang B, Zhang L, Liang H. Characteristics and prognosis of gastric cancer in patients aged ≥ 70 years. World J Gastroenterol. 2013;19(39):6568.
Uedo N, Takeuchi Y, Ishihara R. Endoscopic management of early gastric cancer: endoscopic mucosal resection or endoscopic submucosal dissection: data from a Japanese high-volume center and literature review. Ann Gastroenterol. 2012;25(4):281–90.
Arai T, Esaki Y, Inoshita N, Sawabe M, Kasahara I, Kuroiwa K, et al. Pathologic characteristics of gastric cancer in the elderly: a retrospective study of 994 surgical patients. Gastric Cancer. 2004;7(3):154–9.
Fransen G, Janssen M, Muris J, Laheij R, Jansen J. Meta-analysis: the diagnostic value of alarm symptoms for upper gastrointestinal malignancy. Aliment Pharmacol Ther. 2004;20(10):1045–52.
Pisanu A, Montisci A, Piu S, Uccheddu A. Curative surgery for gastric cancer in the elderly: treatment decisions, surgical morbidity, mortality, prognosis and quality of life. Tumori. 2007;93(5):478–84.
Phoon R. Chronic kidney disease in the elderly - assessment and management. Aust Fam Physician. 2012;41(12):940–4.
Takama T, Okano K, Kondo A, Akamoto S, Fujiwara M, Usuki H, et al. Predictors of postoperative complications in elderly and oldest old patients with gastric cancer. Gastric Cancer. 2014;18(3):653–61.
Kim S, Brooks A, Groban L. Preoperative assessment of the older surgical patient: honing in on geriatric syndromes. Clin Interv Aging. 2015;10:13–27.
Papanikolaou IS, Triantafyllou M, Triantafyllou K, Rösch T. EUS in the management of gastric cancer. Ann Gastroenterol Q Publ Hellenic Soc Gastroenterol. 2015;24(1):9–15.
Cho J. The role of Endosonography in the staging of gastrointestinal cancers. Clin Endosc. 2015;48(4):297.
Puli S. How good is endoscopic ultrasound for TNM staging of gastric cancers? A meta-analysis and systematic review. World J Gastroenterol. 2008;14(25):4011.
Holt B, Rösch T, Peter S. EUS in the evaluation of gastric tumors. In: Hawes RH, Fockens P, Varadarajulu S, editors. Endosonography. Philadelphia: Saunders; 2015. p. 129–50.
Kinkel K, Lu Y, Both M, Warren R, Thoeni R. Detection of hepatic metastasis from cancers of the gastrointestinal tract by using noninvasive imaging methods (US, CT, MR imaging, PET): a meta-analysis. Radiology. 2002;224(3):748–56.
Kawanaka Y, Kitajima K, Fukushima K, Mouri M, Doi H, Oshima T, et al. Added value of pretreatment 18F-FDG PET/CT for staging of advanced gastric cancer: comparison with contrast-enhanced MDCT. Eur J Radiol. 2016;85(5):989–95.
Orsenigo E, Tomajer V, Palo S, Carlucci M, Vignali A, Tamburini A, et al. Impact of age on postoperative outcomes in 1118 gastric cancer patients undergoing surgical treatment. Gastric Cancer. 2007;10(1):39–44.
Kang S, Kim H, Kim M. Low serum albumin level, male sex, and Total Gastrectomy are risk factors of severe postoperative complications in elderly gastric cancer patients. J Gastric Cancer. 2016;16(1):43.
De Manzoni G, Roviello F, Siquini W. Surgery in the multimodal management of gastric cancer. 1st ed. Milan: Springer; 2012.
Park H, Ahn J, Jung H, Lee J, Jung K, Kim D, et al. Clinical characteristics and outcomes of gastric cancer patients aged over 80 years: a retrospective case-control study. PLoS One. 2016;11(12):e0167615.
Ono H, Kondo H, Gotoda T, Shirao K, Yamaguchi H, Saito D, Hosokawa K, Shimoda T, Yoshida S. Endoscopic mucosal resection for treatment of early gastric cancer. Gut. 2001;48(2):225–9.
Sakurai K, Muguruma K, Nagahara H, Kimura K, Toyokawa T, Amano R, et al. The outcome of surgical treatment for elderly patients with gastric carcinoma. J Surg Oncol. 2015;111(7):848–54.
Wu C, Lo S, Shen K, Hsieh M, Lui W, P'eng F. Surgical mortality, survival, and quality of life after resection for gastric cancer in the elderly. World J Surg. 2000;24(4):465–72.
Takeshita H, Ichikawa D, Komatsu S, Kubota T, Okamoto K, Shiozaki A, et al. Surgical outcomes of Gastrectomy for elderly patients with gastric cancer. World J Surg. 2013;37(12):2891–8.
Eguchi YT, Masahito IT. Is extended lymph node dissection necessary for gastric cancer in elderly patients? Eur J Surg. 2000;166(12):949–53.
Rausei S, Ruspi L, Rosa F, Morgagni P, Marrelli D, Cossu A, et al. Extended lymphadenectomy in elderly and/or highly co-morbid gastric cancer patients: a retrospective multicenter study. Eur J Surg Oncol. 2016;42(12):1881–9.
Deiner SJ. Postoperative delirium and cognitive dysfunction. Br J Anaesth. 2009;103(Supplement 1):i41–6.
Field RR, Wall MH. Delirium: past, present, and future. Semin Cardiothorac Vasc Anesth. 2013 Sep;17(3):170–9.
Yamada H, Kojima K, Inokuchi M, Kawano T, Sugihara K. Laparoscopy-assisted gastrectomy in patients older than 80. J Surg Res. 2010;161(2):259–63.
Mikami K, Hirano K, Futami K, Maekawa T. Department of surgery, Fukuoka University Chikushi Hospital 1-1-1 Zokumyoin, Chikushino City, Fukuoka: Japan; p. 818–8502.
Saito H, Osaki T, Murakami D, Sakamoto T, Kanaji S, Tatebe S, Tsujitani S, Ikeguchi M. Effect of age on prognosis in patients with gastric cancer. ANZ J Surg. 2006;76:458–61.
Sasada S, Ikeda Y, Saitsu H, Saku M. Characteristics of gastric cancer in patients over 80-years-old. Hepato-Gastroenterology. 2008;55(86–87):1931–4.
Liu K, Wan J, Yu G, Bei Y, Chen X, Lu M. The recommended treatment strategy for locally advanced gastric cancer in elderly patients aged 75 years and older: a surveillance, epidemiology, and end results database analysis. J Cancer Res Clin Oncol. 2016;143(2):313–20.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Vergari, R., Polenta, V., Marmorale, C. (2018). Cancer of the Stomach. In: Crucitti, A. (eds) Surgical Management of Elderly Patients. Springer, Cham. https://doi.org/10.1007/978-3-319-60861-7_11
Download citation
DOI: https://doi.org/10.1007/978-3-319-60861-7_11
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-60860-0
Online ISBN: 978-3-319-60861-7
eBook Packages: MedicineMedicine (R0)