Abstract
The impact of comorbidity on the outcomes of interest in rheumatic diseases is noteworthy: comorbidity has proven to be a more significant predictor of premature death than shared epitope, rheumatoid factor, or erosions in inflammatory arthritis. Therefore, controlling for coexisting clinical conditions, or comorbidities, booked its place as a main confounder, both in standard healthcare practice and in research. Comorbidity indices are tools used to quantify the total burden of comorbidity contributing to the patient’s overall illness. The simplest method to measure comorbidity is to use the summation of each comorbid illness to generate a total value of comorbidity, often termed a “comorbidity count.” However, not all comorbid diseases have the same impact on the outcome of interest. Thus, more complex comorbidity indices were created to select and weight specific comorbid illnesses to measure more accurately the burden and impact of overall comorbidity. Comorbidities can also be categorized based on the way they have been recorded, whether by administrative data, e.g., the International Classification of Diseases, or by self-administered questionnaires. With the substantial impact that comorbidity exerts on health outcomes in patients with rheumatic diseases, and given the lack of a standardized comorbidity index for clinical or research use, there is an obvious need for an accurate tool to measure the burden of comorbidity in patients with rheumatic disease. This chapter discusses the most commonly used instruments, as well as the recently developed comorbidity indices, their implication onto standard rheumatology clinical practice as well as on patients’ management.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Comorbidity in rheumatic disease
- Rheumatic diseases
- Psoriasis
- Comorbidity index
- Multimorbidity
- Charlson Comorbidity Index
- Charlson-Deyo Index
- Elixhauser Comorbidity Measure
- The Functional Comorbidity Index
- The Multimorbidity Index
- The Rheumatic Disease Comorbidity Index
- RACI (Rheumatoid Arthritis Comorbidity Index)
- Psoriatic Arthritis Comorbidity Index
Though the treatment paradigm for chronic inflammatory arthritic conditions has changed dramatically over the last 15 years, with more effective interventions introduced, able to prevent joint damage and functional impairment, managing the complexity of rheumatic diseases in clinical practice remains as a great challenge. Meta-analyses revealed that, while the long-term prognosis of inflammatory arthritic conditions has improved significantly following the introduction of new diagnostic and management guidelines, the life span of rheumatic patients has not improved accordingly [1,2,3]. This higher mortality rate has been attributed to associated comorbidities. By definition, comorbidity refers to the coexistence of other chronic diseases in patients with an index disease [4]. In inflammatory arthritic conditions, the chronic active inflammatory process may predispose to the development of some of these comorbidities (e.g., increased prevalence of cardiovascular disease, a greater incidence of infections, and the development of certain malignancies [5,6,7,8,9]). However, medications used to treat the arthritic conditions (e.g., steroids and nonsteroidal anti-inflammatory medications [8]) have been linked also to the occurrence of further comorbidities. Therefore, it has become essential to consider the synergism of treating the index disease and comorbid conditions concomitantly. Calculating the patient risk before commencing therapy would have a positive impact on the way these patients are managed as it would make care fit for arthritic patients.
Comorbidities can be assessed via two approaches: either recording each comorbidity separately (e.g., cardiovascular, osteoporosis, infection, malignancy, diabetes mellitus, etc.) or summing the comorbidity risk into a single score which provides a single measure for multiple comorbidities (e.g., comorbidity indices). In real-life practice, the advantage of comorbidity indices is that by reducing all coexistent illnesses and the severity of those into a single numeric score, monitoring of the patient as well as comparison of comorbidity between patients is possible, whereas in scientific research, the greatest advantage of these indices is to adjust multivariate analysis in observational studies giving a single and highly informative score. Comorbidity indices can be classified according to the outcome of interest such as mortality/hospitalization, physical function, or quality of life or the source of data, such as administrative, e.g., International Classification of Diseases such as ICD-9/ICD-10, or self-administered questionnaires (Table 16.1).
In this chapter, commonly used comorbidity indices and self-administered comorbidity questionnaires will be discussed with their implication onto standard rheumatology clinical practice as well as on the patients’ management.
Comorbidity Indices
Comorbidity indices are tools developed to enable the physician to quantify the total comorbidity burden which contributes to the patient’s overall illness. Comorbidity indices have several clinical and research benefits, including the identification of patients (or research participants) with worse prognosis in terms of declines in health-related quality of life, functional ability, risk of hospitalization or mortality [10]. The simplest method to measure comorbidity is to use the summation of each comorbid illness to generate a total value of comorbidity, often termed as “comorbidity counts.” However, not all comorbid diseases have the same impact on the outcome of interest. Thus, more complex comorbidity indices were created to select and weight specific comorbid illnesses to measure more accurately the burden and impact of overall comorbidity [11,12,13,14,15,16]. Table 16.1 shows a list of the most comorbidity indices used in rheumatology research which will be discussed in this chapter.
Charlson Comorbidity Index (CCI)
The Charlson Comorbidity Index (CCI) [11], published in 1987, was based on the mortality rates of 607 patients admitted to the general internal medicine service for 1-month period. The aim was to develop a prospective measure which can be applied to classify comorbidities, which might alter the mortality risk, for use in longitudinal studies. Seventeen diseases were included in this index, with different weights, and were selected and weighted based on the strength of their association with mortality (Table 16.2). All weights are summed to obtain a numeric comorbidity score (range, 0–33) for any particular patient.
CCI Characteristics
The CCI was developed to predict 1-year patient mortality using comorbidity data obtained from hospital chart review. Later on, comorbidities of patients were categorized based on the International Classification of Diseases (ICD) diagnosis codes found in administrative data (such as hospital abstracts or medical services data). Each comorbidity category has an associated weight (from 1 to 6), based on the adjusted risk of mortality or resource use, and the sum of all the weights results in a single comorbidity score for a patient. A score of zero indicates no comorbidities in the list. The higher the score, the more likely the predicted outcome will result in mortality or higher resource use.
Clinical conditions and associated scores are as follows:
-
1 point each: myocardial infarct, congestive heart failure, peripheral vascular disease, dementia, cerebrovascular disease, chronic lung disease, connective tissue disease, ulcer, chronic liver disease, diabetes
-
2 points each: hemiplegia, moderate or severe kidney disease, diabetes with end-organ damage, tumor, leukemia, lymphoma
-
3 points each: moderate or severe liver disease
-
6 points each: malignant tumor, metastasis, AIDS
Regarding the content validity (the completeness and relevance of the items content to measuring what they claimed to measure [17]) of the CCI, the items and the weights included were statistically derived by the relative risk estimates of the proportional regression model to predict mortality using clinical data. As far as construct validity (which refers to the degree to which a test measures what it claims, or purports, to be measuring), in the study carried out by Kiefe et al. [18], outcomes suggested a good construct validity of the CCI. Criterion validity refers to the correlation of a scale with some other measure of the disorder under study, ideally, a gold standard that has been used and accepted in the field [19]. However, as there is no gold standard that exists for measuring comorbidity, another comorbidity measure is usually used for comparison. Earlier studies revealed that CCI presented moderate to good correlation with other comorbidity indices [20,21,22], as well as other outcome criteria such as disability, mortality, and length of stay [19, 23]. Lastly, the reliability of the CCI (which refers to the overall consistency of a measure and also has been defined as the extent to which repeated measurements of a stable phenomenon by different people, at different times and places, get similar results and are usually assessed by the intra-class correlation coefficient (ICC) in case of several assessors [24]) was reported to be moderate to very good indicating good reliability of the CCI [25, 26].
Development and Changes to the CCI
Over time, there have been changes to the original index. A summary of these variations includes:
-
The original index was developed with 19 categories [11] but has been modified to 17 categories published by Deyo et al. in 1992 [27].
-
The list of specific ICD diagnosis codes that are used to identify different categories of comorbidity has been modified as reported in the Romano et al. study published in 1993 [28] and updated from ICD-9-CM to work with ICD-10 coding as reported in the Halfon et al. study (2002) [29] and then in the Quan et al. study (2005) [30].
-
The original weights developed for use with the index have also been modified (Schneeweiss et al. 2003) [31].
Critical Analysis of the CCI
The Charlson Comorbidity Index (CCI) is the most widely used comorbidity index. CCI has been adapted and verified as applicable and valid tool for predicting the outcome and risk of death from many comorbid diseases [32, 33]. However, while the CCI was created to predict death in a sample of hospitalized patients, it has been widely used outside its originally intended scope. A systematic review of the CCI using Canadian administrative databases was carried out by Needham et al. (2005) [34] with a perspective on risk adjustment in critical care research. Results revealed lower predictive ability of the CCI in comparison to Acute Physiology and Chronic Health Evaluation (APACHE), yet the study highlighted the advantages of using the CCI instrument for population-based research . Another study reported that some comorbidities collected in other indices, such as alcoholism, were not included in the CCI [35]. Rheumatology-wise, in the current RA management context, the CCI can be considered as outdated. Being developed in 1987, most (if not all) of the rheumatoid arthritis or other connective disease patients included in the CCI, most likely, have not been treated according to the treatment protocols approved in the last 20 years. Furthermore, it is worth noting that some diseases such as fibromyalgia have not been included in the comorbidity index.
Elixhauser Comorbidity Measure (ECM)
The Elixhauser Comorbidity Measure (ECM) [16] is a method of categorizing comorbidities of patients based on the International Classification of Diseases (ICD) diagnosis codes found in administrative data, such as hospital abstracts data. Each comorbidity category is dichotomous, i.e., it is either present or absent. The index can be used to predict hospital resource use and in-hospital mortality. The ECM was developed using administrative data from a state-wide California inpatient database (n = 1,779,167). Its original aim was to identify a list of 30 comorbidities (the 17 from the CCI + 13 new ones), relying on the ICD-9-CM, that had a major impact on short-term outcomes in acute hospital inpatients (Table 16.3). Elixhauser et al. [16] treated conditions separately or as a count. The comorbidities identified in the ECM were significantly associated with in-hospital mortality and include both acute and chronic conditions.
ECM Characteristics
Regarding its content validity, the ECM comprises a larger number of items compared to the CCI. In addition to the empirical-generated items (that were also included in the CCI), 13 additional judgmental items were added, based on a systematic literature review. On the other hand, no weight was given to the comorbidities included, implicitly assuming that all conditions are equally important in their relationship to outcomes, which is unlikely to be true. There were no studies published to evaluate the construct validity of the ECM. Interestingly, assessment of the ECM criterion validity revealed that when ECM was compared to CCI, in most of the studies ECM tended to outperform the CCI tool [36,37,38,39], while in others performances were similar [40]. In concordance, a systematic review and comparative analysis showed that, among various comorbidity indices, the Elixhauser index predicts the risk better, especially beyond 30 days of hospitalization [41]. ECM also tended to perform better, when compared to other illness indicators, such as “previous years expenditures” [42]. As far as reliability, no data were available on the ECM. However, the inter-rater reliability may appear less relevant since it uses administrative data. Furthermore, its developers highlighted the fact that diagnoses from administrative data may be less accurate than those from physicians , although diagnoses from physicians are not perfectly accurate.
Development and Changes to the ECM
Over time, there have been changes to the ECM index based on different research studies. A summary of these variations includes:
-
While the original index was developed including 30 categories [16], Garland et al. 2012 [43] suggested increasing them to 31 categories.
-
The list of specific ICD diagnosis codes used to identify different categories of comorbidity has been modified and updated from ICD-9-CM to work with ICD-10 coding. Results were published in the Quan et al. study (2005) [30].
-
In the study carried out by van Walraven et al. (2009), a weighting algorithm was developed, based on the association between comorbidity and death, in order to produce an overall score for the Elixhauser Total Score (ETS) [44].
Critical Analysis of the ECM
Generally, one of the ECM limitations is that the index has been designed for use with very specific ICD coding (up to 5-digit ICD-9-CM codes and 7-digit ICD-10 codes) found in the hospital abstracts data. This is due to the specificity required to distinguish between diagnoses that should/should not be included in the index and to be able to properly identify and place codes into the appropriate category. Therefore, using only 3-digit ICD codes to calculate the ECM is not recommended as they lack the specificity required to properly categorize diagnoses in the Elixhauser Comorbidity Index.
Rheumatology -wise, similar to the CCI, ECM index has been applied in situations extending beyond its intended scope, and, in the current RA management context, Elixhauser indices can be also considered as outdated. Being developed in 1998, the majority of the RA patients included in the ECM original study, most likely, have missed the biologic therapy era or are treated according to the management protocols approved in the last 18 years. Furthermore, ECM uses a comorbidity count and not weights. The use of comorbidity counts is discouraged because they vary in the number and types of conditions included, and wide variability in predictive ability should be expected.
The Functional Comorbidity Index (FCI)
Prior comorbidity indices have been developed primarily to predict mortality or administrative outcomes such as length of stay in acute care or disease-specific populations [13, 45]. These indices typically include diagnoses, often asymptomatic, such as hypertension, that are important in predicting mortality, and exclude diagnoses, such as arthritis, that impact physical function but are unlikely to result in short-term mortality. Research using indices designed to predict mortality have concluded that comorbid illnesses have little relationship with physical disability [46, 47], a finding that seems intuitively false but underscores the need to consider the purpose for which an index was designed. This paved the way to develop new indices with different outcomes of interest such as physical function or quality of life.
The Functional Comorbidity Index [48] was developed using two databases: a cross-sectional, simple random sample of 9423 Canadian adults and a sample of 28,349 US adults seeking treatment for spine ailments. The purpose was to develop a self-administered, general population index of comorbid diseases with physical function, assessed by the physical function subscale of the SF-36, as the outcome of interest. The underlying premise was that diagnoses associated with impairments in physical function would be, at least in part, different from those associated with mortality, and therefore, an index designed with physical function as the outcome would perform better in the previous context—i.e., spinal problems—than indices designed with mortality as the outcome of interest.
The FCI Characteristics
Multiple linear regression identified 18 variables that were associated with the SF-36 physical function score (Table 16.4) [48]. The FCI was scored as both a simple count (yes/no) and a weighted count of the diagnoses. “Weights” were derived from the standardized beta coefficients from the regression analysis. A score of “0” indicates no comorbid illnesses, and a score of “18” indicates the highest number of comorbid illnesses. The weighted count did not perform significantly better, and therefore, it is not used. Simple counts are clearly easier to score and use. The FCI scores correlated weak to moderate with both the SF-36 physical function and role physical subscale scores (−.53 and −.31, respectively). When the SF-36 physical function subscale score was dichotomized into “high” and “low,” the FCI simple count correctly classified 76.6% of people, whereas using a weighted count, the FCI correctly classified 77.0%. Compared with the CCI [11] and the Kaplan-Feinstein index [13], the FCI accounted for more variation in the physical function subscale scores (R 2 = 0.29, 0.18, and 0.07%, respectively).
Critical Analysis of the FCI
The Functional Comorbidity Index was developed specifically for use in the general population with physical function, not mortality, as the outcome of interest. The Functional Comorbidity Index contains conditions such as visual impairment, osteoporosis, and arthritis, which do not appear in the most widely used indices, namely, the CCI or the Kaplan-Feinstein index. However, the FCI does not take into consideration the severity of the diagnoses, an important factor to be considered when dealing with diseases such as inflammatory arthritis. Severity ratings are likely to provide better adjustment. Furthermore, the FCI study relied mainly on secondary data sources for development and thus may have overlooked some diagnoses associated with functional status. For example, HIV/AIDS was not explicitly collected in either database and may contribute significantly to functional disability.
The Rheumatic Disease Comorbidity Index (RDCI)
The RDCI [49] was created from self-report questionnaires from patients with RA, osteoarthritis, systemic lupus erythematosus, or fibromyalgia. The RDCI is characterized by having multiple outcomes of interest. Comorbid illnesses were assessed for impact on six outcomes: direct medical costs, work disability, social security disability, Health Assessment Questionnaire (HAQ) functional disability, hospitalization, and death.
The RDCI Characteristics
While 22 comorbid illnesses were assessed, the final score encompasses 11 comorbid illnesses (Table 16.5); the range is 0–9. The RDCI was compared to six comorbidity indices: the Charlson-Deyo Index (CDI), Functional Comorbidity Index (FCI), Elixhauser Comorbidity Measure (ECM), Elixhauser Point System (EPS), and a simple comorbidity count (COUNT) using a US cohort of rheumatoid arthritis patients [10]. Relative to other common comorbidity indices, the RDCI and ECM Score were superior indices for predicting death and physical disability in an administrative data set composed of individuals with RA. The RDCI predicted physical disability with self-report data from a clinic questionnaire. In contrast to the Elixhauser Comorbidity Measure (ECM) which is composed of 30 different comorbidities, the RDCI relies on only 11 comorbidities. The RDCI may also be used as a foundation to tailor to a specific outcome of interest. For example, if death from myocardial infarction is being studied, additional predictive power is obtained by adding certain binary comorbid conditions (previous myocardial infarction, hypertension, and hyperlipidemia) to the RDCI [10]. In contrast to other indices such as CCI and FCI which perform optimally only for one outcome, RDCI can perform well in multiple outcomes.
Critical Analysis
The RDCI is the first comorbidity index addressing diseases commonly associated to rheumatic diseases specifically. The RDCI can be used with administrative data sets as well as with patient-reported data. This ability to use both sources allows the index to be more widely applicable and to serve as a standardized measure of comorbidity within rheumatology. Furthermore, the RDCI relies on relatively smaller number of comorbidities (only 11) and was assessed for variable relevant outcomes of interest. However, the RDCI has some limitations. First, the index was fixed at baseline values for analysis, thus removing the chronological component of comorbidity during the follow-up period. This reduces the predictive power of comorbidity indices [50]. Additionally, the ICD-9-CM codes were collected from outpatient visits, which rely on the providers to maintain an accurate list of comorbid conditions. There is usually a delay in data recording, which represents a significant limitation to the index (in the RDCI validation study mortality data collected through the National Death Index had approximately a 2-year delay; thus, deaths collected through the National Death Index from 2008 to 2010 may have been missed and not included in the analysis). Thirdly, the population in the RDCI administrative data set was composed entirely of individuals with RA and was predominantly male. Thus, generalizability of the results to other populations may not be appropriate.
The Multimorbidity Index (MMI)
The notion of multimorbidity was introduced based on the fact that rheumatology patients are typically afflicted by more than one disease; therefore, considering multimorbidity is vital when deciding on diagnostic or therapeutic strategies. Furthermore, multimorbidity can cause polypharmacy, an increasing treatment burden, which might also impact patients’ overall HRQoL. Therefore, the concept was that developing an index reflecting multimorbidity that is based on HRQoL might be helpful to better address the disease-related aspects of patients’ overall well-being, which could also be useful for application in both clinical trials and epidemiological studies.
The MMI [51] was developed based on health-related quality of life (HRQoL) in an observational RA cohort. The MMI identified quality of life as the main outcome, associated with physical function, pain, and global health. The hypothesis was that, incorporating a multidimensional patient-centered concept, quality of life reflects patients’ overall well-being and can be considered a main treatment target. This was supported by the findings of an earlier study which reported that an increasing number of morbidities lead to a decrease of HRQoL [52].
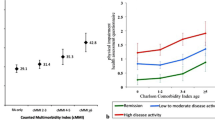
The MMI Characteristics
The index includes 40 morbidities, all identified using ICD-9 codes (Table 16.6). MMIs of two types were calculated: one by enumerating morbidities (MMI count) and the other by weighting morbidities based on their association with HRQoL as assessed by the European Quality of Life – 5 dimensions (EQ-5D) questionnaire in multiple linear regression analysis. Criterion validity was assessed by comparing the MMI to CCI and FCI indices as well as HRQoL, all measured at the baseline visit. Both MMI count and MMI weight indices were more strongly associated with EQ-5D than CCI (Spearman: MMI count = −0.20, MMI weight = −0.26, and CCI = −0.10; p < 0.01). R 2 obtained by linear regression using EQ-5D as a dependent variable and the various indices as independent variables, adjusted for age and gender, was the highest for MMI (R 2: MMI count = 0.05, MMI weight = 0.11, and CCI = 0.02). When accounting for clinical disease activity index (CDAI), R2 increased (MMI count = 0.18, MMI weight = 0.22, and CCI = 0.17), still showing higher values of MMI compared with CCI but in any case rather small. External validation in different RA cohorts [51] showed good performance of both Indices. In view of this, and considering that not much improvement was gained by weighting, the authors endorsed a simple MMI count index for its use in the assessment of multimorbidity in RA patients and its impact on the patients’ overall well-being.
Critical Analysis
Similar to the FCI which considered physical function as the main outcome, the MMI addressed the patients’ overall well-being (QoL) as the main outcome. This comes in contrast to the earlier existing indices such as CCI and ECM which are based on other specific outcomes, such as mortality, costs, or hospitalization. However, for the MMI, the diseases were selected as either recommended as a core for any multimorbidity measure by a systemic literature review or defined as chronic (long-term) disorders with important impact as proposed by the National Health Service Scotland . These selection criteria may be the explanation for the long list of comorbidities, a good number of which are not commonly reported in inflammatory arthritic conditions. This may, in turn, explain the poor criterion validity shown in the study and why the average range of the multimorbidity count ranged from 1 to 16 only, while the total score is 40. This, also, may elucidate the low correlation of the MMI count when compared with the FCI despite both of them used HRQoL as the outcome of interest. Furthermore, the MMI was developed in a disease-specific cohort, namely, RA patients, yet it has not been assessed in non-RA patients.
Self-administered Comorbidity Questionnaires
Self-administered comorbidity questionnaires for assessing comorbidities have been introduced [53, 54] as an alternative to medical records or administrative data approach. The self-administered comorbidity questionnaire (SCQ) , which was first published by Sangha et al. in 2003 [54], requires the patients to indicate whether they suffer at the moment from 12 medical conditions in addition to the index disease (Table 16.7). The comorbidities listed were selected by an expert panel based on the ones captured by the CCI. The score of the SCQ ranges from 0 to 45 points. Construct validity was assessed by the correlation between SCQ and CCI and was moderate (0.55). Test-retest reliability was very good (ICC 0.94 [95%CI 0.72–0.99]). Criterion validity was evaluated through the correlation of SCQ with SF-36 and was weak to fair (from r = 0.03 to 0.39 depending on the SF-36 subscale, with better correlations observed for physical-related subscales) and fairly correlated with the number of prescriptions in a year (r = 0.37). Stolwijk et al. [55] have published a validation study for SCQ in patients with ankylosing spondylitis (AS), where criterion validity was assessed by the agreement between the SCQ answers and comorbidities identified in medical records and was moderate to perfect for most conditions (κ 0.47–1.00), except for ulcer disease, depression, and OA. Other validation studies using this questionnaire in other pathologies are currently on going.
Disease-Specific Comorbidity Indices
In view of the recent developments in the diagnosis and management of inflammatory arthritic conditions and the reports showing variable comorbidity patterns in patients suffering from different rheumatic diseases [56], there has been an unmet need for new comorbidity indices addressing these points. The recently published Rheumatoid Arthritis Comorbidity Index (RACI) [57] and Psoriatic Arthritis Comorbidity Index (PsACI) [58] were created from self-report questionnaires completed by patients with early rheumatoid and psoriatic arthritis. Both indices are disease specific and are characterized by having multiple outcomes of interest. In both RACI and PsACI , comorbid illnesses were assessed for impact on four outcomes: functional disability, quality of life, medication-associated comorbidities, and hospitalization and death.
The RACI and PsACI Characteristics
Original studies for both questionnaires [57, 58] revealed that the patients included were suffering from early inflammatory as well as psoriatic arthritis (disease duration <6 months and <12 months, respectively). The patients were monitored over 10-year period and received treatment in the form of DMARDs and biologic therapy according to the recently published guidelines; hence, both indices were not fixed to baseline data. Furthermore, each index addressed its specific disease activity. The development of both RACI and PsACI was based on patient self-administered questionnaire as well as ICD-10 data record. Results revealed variation of the comorbidity prevalence over the 10-year study period. While depression and anxiety were more prevalent in the first few years of the disease course, other comorbidities including cardiovascular, osteoporosis, and medication-associated comorbidities were more prevalent at later stages of the disease course. Thirty-one comorbidities were identified in the RACI with a score ranging between 0 and 36 (Table 16.8), whereas the PsACI included 29 items with a score ranging between 0 and 36 (Table 16.9). Criterion validity was evaluated through the index correlation with both functional disability and quality of life. Multivariate linear regression analysis for functional disability score prediction using RACI adjusted for age and gender revealed significant correlations at 1, 3, 5, and 10 years (R 2, 0.743, 0.767, 0.908, and 0.835, respectively). Similarly PsACI showed significant correlation with the functional disability score (R 2, 0.725, 0.773, 0.847, and 0.872 at 1, 3, 5, and 10 years, respectively). Construct validity was assessed by studying the correlation between the RACI and four comorbidity indices: the CCI, FCI, RDCI, and MMI. Relative to other comorbidity indices, the RACI and RDCI showed high correlation for predicting death and physical disability in data set composed of individuals with RA (1 year, 0.963; 3 years, 0.598; 5 years, 0.966; 10 years,0.919). Similarly, PsACI was compared to the CCI, FCI, RDCI, and MMI. In concordance with the RACI, both PsACI and RDCI had the highest correlations at 1 year (r = 0.863), 3 years (0.798), 5 years (0.886), and 10 years (0.916). Test-retest reliability for both RACI and PsACI was very good (ICC 0.97 and 0.96, respectively). Receiver operating characteristic (ROC) illustrating the discriminating ability of the RACI revealed that a score of 8/36 gave an area under the curve (AUC) of 0.967, whereas in the PsACI a score of 8/36 gave an AUC of 0.987. External validation studies for both RACI and PsACI revealed that both indices were able to predict outcomes of physical disability, quality of life, as well as hospitalization/death and showed significant correlation with all the other comorbidity indices (CCI, FCI, RDCI, and MMI).
Critical Analysis
Both RACI and PsACI are the first disease-specific comorbidity indices which include disease activity as a comorbid factor with the highest weight in contrast to the other disease-associated comorbidities. Similarly, both indices are the first to address medication-associated comorbidities as an outcome of interest. Both the RACI and PsACI were able to predict outcomes of physical disability, quality of life, as well as hospitalization/death. Both indices outperformed CCI, which is commonly used but not validated for outcomes such as health-related quality of life (HRQoL) . Both comorbidity indices can be measured with either patient-reported questionnaire (part of a patient-reported outcome measure) or administrative data (ICD-9 or ICD-10) for comorbidity assessment and management.
Comorbidity Indices in Standard Practice and Research
Though guidelines such as NICE [59] and EULAR [60] have stressed on the importance of screening inflammatory arthritic patients regularly for associated comorbidities, assessment of these in standard clinical practice has yet to be widely implemented. The Comorbidities in Rheumatoid Arthritis (COMORA) study [61], which included 3920 patients from 17 countries around the world, revealed that the management of comorbidities in RA patients is far from optimum and that there have been disparities in the screening process in different countries. Furthermore, the studies used to assess the associated comorbidity risk, for example, the cardiovascular risk, were based on cohorts assembled in 1955–1973 [62,63,64,65]. Longitudinal studies which included RA patients diagnosed and treated before the introduction of methotrexate into clinical practice in 1986 [66] would bias the results toward poor outcomes as they will not be representative of the modern disease management or the current clinical presentation of RA. In addition, the inclusion of RA disease duration >10 years as a risk factor for cardiovascular risk may undermine its risk assessment earlier in the disease course when the disease activity is at its peak.
The findings that the occurrence of comorbidities varies across rheumatic diseases and that separate patterns of comorbidity may be identified in patients who have rheumatoid arthritis, psoriatic arthritis, systemic lupus, as well as fibromyalgia syndrome highlighted the unmet need for systems to assess specific comorbidity risk in these patients [56]. To date, no gold standard exists on how to measure comorbidity. This was supported by the outcomes of a systematic literature review [67] on assessing comorbidity and multimorbidity, which identified 39 different indices showing heterogeneity in terms of types and numbers of conditions included and outcomes the indices are based on. Perhaps that is the reason why comparisons of comorbidity indices in rheumatic diseases are limited. Gabriel et al. [21] showed that the CCI and the Index of Coexistent Disease (designed mainly for patients on hemodialysis [68]) were both highly statistically significant predictors of death in an administrative data set of 450 RA and 441 OA patients. In another study, both RDCI and ETS were reported to best predict death in RA patients [49]. These results are similar to those previously published in myocardial infarction and cancer, which showed that ECM outperforms CDI in predicting death when the source was administrative data [37, 69]. As for physical disability, the FCI was found to predict MDHAQ best in RA with considerable support. In a random sampling of Canadian adults and a sample of US adults seeking treatment for spine ailments, Groll et al. [12] showed the FCI outperformed CCI in correlating with physical function, as measured by the physical function subscale of the Short Form 36 Health Survey. The most recently published comorbidity indices specific for RA and psoriatic arthritis pave the way for a new approach to comorbidity risk assessment and management tailored to the individual patient’s status.
There has been a misconception in that, clinically, comorbidity indices have limited use. The window of opportunity and treat to target approaches highlighted the importance of assessing for the comorbid conditions or its risk on regular basis when managing the disease or prescribing therapeutics. The comorbid conditions important for these roles in standard clinical practice may not always be applicable in research settings, as highlighted by the recently published EULAR points to consider for reporting, screening for, and preventing selected comorbidities in chronic inflammatory rheumatic diseases [70].
Several important steps should be considered when selecting a comorbidity index for research. First, one must determine the outcome of interest. While some indices like ETS and RDCI can perform well in multiple outcomes, other indices such as CDI and FCI may only perform optimally for a single outcome. Second, investigators must determine the source of data. Many of the indices can only be used in administrative data sets with ICD-9-CM codes (CDI, ETS, EPS). Furthermore, one must consider the data available for model construction as evidenced by the robust improvement in model fit with the administrative and clinical models. Last, the comorbid conditions available must be considered. Many indices require a substantial number of comorbid conditions, but if these are not available, a comorbidity count can be used, though with less predictive ability. Use of a comorbidity count is discouraged because comorbidity counts vary in the number and types of conditions included, and wide variability in predictive ability have been reported [10]. Therefore, it is strongly recommend that researchers use a standardized and validated comorbidity index in rheumatology analysis for improved comparability and reproducibility.
In conclusion, considering the recent developments in the diagnosis and management of inflammatory arthritic conditions, there is a still a need for systems to assess for comorbidity in standard clinical settings. Periodic assessment for comorbidities should be carried out by the treating healthcare physician as one of the management outcome measures. Electronic comorbidity calculators would be a step forward toward implementing comorbidity screening in the day-to-day patient management. This should be carried out in collaboration with primary care providers and other specialists. Developing a disease-specific comorbidity index able to predict morbidity, mortality, cost, and hospitalization would be a step forward on the way to achieve full disease remission.
References
Wolfe F, Mitchell DM, Sibley JT, et al. The mortality of rheumatoid arthritis. Arthritis Rheum. 1994;37:481–94.
Gabriel SE, Michaud K. Epidemiological studies in incidence, prevalence, mortality, and comorbidity of the rheumatic diseases. Arthritis Res Ther. 2009;11:229.
Gabriel SE. Why do people with rheumatoid arthritis still die prematurely? Ann Rheum Dis. 2008;67:30–4.
Feinstein AR. The pre-therapeutic classification of co-morbidity in chronic disease. J Chronic Dis. 1970;23(7):455–68.
Avina-Zubieta JA, Choi HK, Sadatsafavi M, et al. Risk of cardiovascular mortality in patients with rheumatoid arthritis: a meta-analysis of observational studies. Arthritis Rheum. 2008;59:1690–7.
Lindhardsen J, Ahlehoff O, Gislason GH, et al. The risk of myocardial infarction in rheumatoid arthritis and diabetes mellitus: a Danish nationwide cohort study. Ann Rheum Dis. 2011;70:929–34.
Listing J, Gerhold K, Zink A. The risk of infections associated with rheumatoid arthritis, with its comorbidity and treatment. Rheumatology (Oxford). 2013;52:53–61.
Wotton CJ, Goldacre MJ. Risk of invasive pneumococcal disease in people admitted to hospital with selected immune-mediated diseases: record linkage cohort analyses. J Epidemiol Community Health. 2012;66:1177–81.
Uresson C, Matteson EL. Malignancy as a comorbidity in rheumatic diseases. Rheumatology (Oxford). 2013;52:5–14.
England B, Sayles H, Mikuls TED, Johnson D, Michaud A. Validation of the rheumatic disease comorbidity index. Arthritis Care Res. 2015;67(6):865–72.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–83.
Groll DL, To T, Bombardier C, Wright JG. The development of a comorbidity index with physical function as the outcome. J Clin Epidemiol. 2005;58:595–602.
Kaplan MH, Feinstein AR. The importance of classifying initial co-morbidity in evaluating the outcome of diabetes mellitus. J Chronic Dis. 1974;27:387–404.
Miller MD, Paradis CF, Houck PR, Mazumdar S, Stack JA, Rifai AH, et al. Rating chronic medical illness burden in geropsychiatric practice and research: application of the cumulative illness rating scale. Psychiatry Res. 1992;41:237–48.
Von Korff M, Wagner EH, Saunders K. A chronic disease score from automated pharmacy data. J Clin Epidemiol. 1992;45:197–203.
Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27.
Hall SF. A user’s guide to selecting a comorbidity index for clinical research. J Clin Epidemiol. 2006;59:849–55.
Kiefe CI, Funkhouser E, Fouad MN, May DS. Chronic disease as a barrier to breast and cervical cancer screening. J Gen Intern Med. 1998;13:357–65.
Streiner DL, Norman GR. Health measurement scales. A practical guide to their development and use, vol. 2. Oxford: Oxford University Press; 1995. p. 1–230.
Rochon PA, Katz JN, Morrow LA, et al. Comorbid illness is associated with survival and length of hospital stay in patients with chronic disability. A prospective comparison of three comorbidity indices. Med Care. 1996;34:1093–101.
Gabriel SE, Crowson CS, O’Fallon WM. A comparison of two comorbidity instruments in arthritis. J Clin Epidemiol. 1999;52:1137–42.
Kieszak SM, Flanders WD, Kosinski AS, Shipp CC, Karp H. A comparison of the Charlson comorbidity index derived from medical record data and administrative billing data. J Clin Epidemiol. 1999;52:137–42.
Poses RM, McClish DK, Smith WR, Bekes C, Scott WE. Prediction of survival of critically ill patients by admission comorbidity. J Clin Epidemiol. 1996;49:743–7.
Fletcher RH, Fletcher SW, WAGNER EH. Clinical epidemiology: the essentials. 3rd ed. Baltimore: Williams & Wilkins; 1996.
de Groot V, Beckerman H, Lankhorst GJ, Bouter LM. How to measure comorbidity. A critical review of available methods. J Clin Epidemiol. 2003;56:221–9.
Katz JN, Chang LC, Sangha O, Fossel AH, Bates DW. Can comorbidity be assessed by questionnaire rather than medical record review ? Med Care. 1996;34:73–84.
Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45(6):613–9.
Romano PS, Roos LL, Jollis JG. Adapting a clinical comorbidity index for use with ICD-9-CM administrative data: differing perspectives. J Clin Epidemiol. 1993;46(10):1075–9.
Halfon P, Eggli Y, van Melle G, Chevalier J, Wasserfallen JB, Burnand B. Measuring potentially avoidable hospital readmissions. J Clin Epidemiol. 2002;55(6):573–87.
Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi JC, Saunders LD, Beck CA, Feasby TE, Ghali WA. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43(11):1130–9.
Schneeweiss S, Wang PS, Avorn J, Glynn RJ. Improved comorbidity adjustment for predicting mortality in Medicare populations. Health Serv Res. 2003;38(4):1103–20.
Sarfati D, Tan L, Blakely T, et al. Comorbidity among patients with colon cancer in New Zealand. N Z Med J. 2011;124(1338):76–88.
Mnatzaganian G, Ryan P, Norman PE, et al. Accuracy of hospital morbidity data and the performance of comorbidity scores as predictors of mortality. J Clin Epidemiol. 2012;65(1):107–15.
Needham DM, Scales DC, Laupacis A, Pronovost PJ. A systematic review of the Charlson comorbidity index using Canadian administrative databases: a perspective on risk adjustment in critical care research. J Crit Care. 2005;20(1):12–9.
Moltó A, Dougados M. Comorbidity indices. Clin Exp Rheumatol. 2014;32(Suppl. 85):S131–4.
Condon JR, You J, McDonnell J. Performance of comorbidity indices in measuring outcomes after acute myocardial infarction in Australian indigenous and non-indigenous patients. Intern Med J. 2012;42:e165–73.
Southern DA, Quan H, Ghali WA. Comparison of the Elixhauser and Charlson/Deyo methods of comorbidity measurement in administrative data. Med Care. 2004;42:355–60.
Menendez ME, Neuhaus V, van Dijk CN, Ring D. The Elixhauser comorbidity method outperforms the Charlson index in predicting inpatient death after orthopaedic surgery. Clin Orthop Relat Res. 2014;472:2878–86.
Dominick KL, Dudley TK, Coffman CJ, Bosworth HB. Comparison of three comorbidity measures for predicting health service use in patients with osteoarthritis. Arthritis Rheum. 2005;53:666–72.
Antoniou T, Ng R, Glazier RH, Kopp A, Austin PC. Comparison of comorbidity classification methods for predicting outcomes in a population-based cohort of adults with human immunodeficiency virus infection. Ann Epidemiol. 2014;24:532–7.
Gandjour A, Ku-Goto MH, Ho V. Comparing the validity of different measures of illness severity: a hospital-level analysis for acute myocardial infarction. Health Serv Manag Res. 2012;25:138–43.
Sharabiani M, Aylin P, Bottle A. Systematic review of comorbidity indices for administrative data. Med Care. 2012;50(12):1109–18.
Garland A, Fransoo R, Olafson K, Ramsey C, Yogendran M, Chateau D, McGowan K. The epidemiology and outcomes of critical illness in Manitoba. Winnipeg: Manitoba Centre for Health Policy; 2012.
Van Walraven C, Austin PC, Jenings A, Quan H, Forster AJ. A modification of the Elixhauser comorbidity measures into a point system for hospital death using administrative data. Med Care. 2009;47(6):626–33.
Linn BS, Linn MW, Gurel L. Cumulative illness rating scale. J Am Geriatr Soc. 1968;16:622–6.
Extermann M, Overcash J, Lyman G, Parr J, Balducci L. Comorbidity and functional status are independent in older cancer patients. J Clin Oncol. 1998;16(4):1582–7.
Repetto L, Fratino L, Audisio RA, Venturino A, Gianni W, Vercelli M, Parodi S, Dal Lago D, Gioia F, Monfardini S, Aapro MS, Serraino D, Zagonel V. Comprehensive geriatric assessment adds information to Eastern Cooperative Oncology Group performance status in elderly cancer patients: an Italian Group for Geriatric Oncology Study. J Clin Oncol. 2002;20(2):494–502.
Grolla D, Tob T, Bombardierc C, Wrightd J. The development of a comorbidity index with physical function as the outcome. J Clin Epidemiol. 2005;58:595–602.
Michaud K, Wolfe F. Comorbidities in rheumatoid arthritis. Best Pract Res Clin Rheumatol. 2007;21:885–906.
Chang TI, Paik J, Greene T, Miskulin DC, Chertow GM. Updated comorbidity assessments and outcomes in prevalent hemodialysis patients. Hemodial Int. 2010;14:478–85.
Rander H, Yoshida K, Mjaavatten M, Aletaha D, et al. Development of a multimorbidity index: impact on quality of life using a rheumatoid arthritis cohort. Semin Arth Rheumatsim. 2015;45(2):167–73.
Radner H, Smolen JS, Aletaha D. Comorbidity affects all domains of physical function and quality of life in patients with rheumatoid arthritis. Rheumatology (Oxford). 2010;50:381–8.
Frenkel WJ, Jongerius EJ, Mandjes-van Uitert MJ, van Munster BC, de Rooij SE. Validation of the Charlson comorbidity index in acutely hospitalized elderly adults: a prospective cohort study. J Am Geriatr Soc. 2014;62:342–6.
Sangha O, Stucki G, Liang M, Fossel AH, Katz JN. The self-administered comorbidity questionnaire: a new method to assess comorbidity for clinical and health services research. Arthritis Rheum. 2003;49:156–63.
Stolwijk C, van Tubergen A, Ramiro S, et al. Aspects of validity of the self-administered comorbidity questionnaire in patients with ankylosing spondylitis. Rheumatology (Oxford). 2014;53:1054–64.
El Miedany Y. Co-morbidity index in rheumatoid arthritis: time to think. Clin Rheumatol. 2015;34(12):1995–2000.
El Miedany Y, El Gaafary M, Youssef S, Bahlas S, Ahmed I, Hegazi M. Rheumatoid arthritis comorbidity index: development and validation of a new specific tool for classifying prognostic comorbidity in rheumatoid arthritis patients. Ann Rheum Dis. 2016;75(Suppl2):154.
El Miedany Y, El Gaafary M, Youssef S, Bahlas S, Hegazi M. Psoriatic arthritis comorbidity index: development and validation of a new specific tool for classifying prognostic comorbidity in psoriasis and psoriatic arthritis patients. Rheumatol Orthop Med. 2017;2 doi: 10.15761/ROM.1000117.
NICEguidelines [CG79]. Rheumatoidarthritis:the management of rheumatoid arthritis in adults. http://www.nice.org.uk/guidance/cg79. 2009.
Smolen J, Landewé R, Breedveld F, et al. EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2013 update. Ann Rheum Dis. 2014;73(3):492–509. doi:10.1136/annrheumdis-2013204573.
Dougados M, Soubrier M, Antunez A, et al. Prevalence of comorbidities in rheumatoid arthritis and evaluation of their monitoring: results of an international, cross-sectional study (COMORA). Ann Rheum Dis. 2013;1:1–7. doi:10.1136/annrheumdis2013-204223.
Jacobsson LT, Knowler WC, Pillemer S, et al. Rheumatoid arthritis and mortality. A longitudinal study in pima Indians. Arthritis Rheum. 1993;36:1045–53.
Turesson C, McClelland RL, Christianson TJ, et al. Severe extra-articular disease manifestations are associated with an increased risk of first ever cardiovascular events in patients with rheumatoid arthritis. Ann Rheum Dis. 2007;66:70–5.
Nicola PJ, Maradit-Kremers H, Roger VL, et al. The risk of congestive heart failure in rheumatoid arthritis: a population-based study over 46 years. Arthritis Rheum. 2005;52:412–20.
Gabriel SE, Crowson CS, Kremers HM, et al. Survival in rheumatoid arthritis: a population-based analysis of trends over 40 years. Arthritis Rheum. 2003;48:54–8.
Weinblatt ME, Coblyn JS, Fox DA, et al. Efficacy of lowdose methotrexate in rheumatoid arthritis. N Engl J Med. 1985;312:818–22.
Radner H, Yoshida K, Smolen J, Solomon D. Multimorbidity and rheumatic conditions—enhancing the concept of comorbidity. Nat Rev Rheumatol. 2014;10:252–6.
Miskulin DC, Athienites NV, Yan G, Martin AA, Ornt DB, et al. Comorbidity assessment using the index of coexistent diseases in a multicenter clinical trial. Kidney Int. 2001;60(4):1498–510.
Lieffers JR, Baracos VE, Winget M, Fassbender K. A comparison of Charlson and Elixhauser comorbidity measures to predict colorectal cancer survival using administrative health data. Cancer. 2011;117:1957–65.
Baillet A, Gossec L, Carmona L, de Wit M, et al. Points to consider for reporting, screening for and preventing selected comorbidities in chronic inflammatory rheumatic diseases in daily practice: a EULAR initiative. Ann Rheum Dis. 2014;73(3):492–509. doi:10.1136/annrheumdis-2016-209233.
Acknowledgment
Special thanks to Dr. Loreto Carmona, MD, PhD, Research Director, Instituto de Salud Musculoesquelética, Madrid, Spain, for peer reviewing this chapter.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this chapter
Cite this chapter
El Miedany, Y. (2017). Comorbidity Index. In: El Miedany, Y. (eds) Comorbidity in Rheumatic Diseases. Springer, Cham. https://doi.org/10.1007/978-3-319-59963-2_16
Download citation
DOI: https://doi.org/10.1007/978-3-319-59963-2_16
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-59962-5
Online ISBN: 978-3-319-59963-2
eBook Packages: MedicineMedicine (R0)