Abstract
Helicobacter pylori infection can lead to the occurrence of many diseases of the upper gastrointestinal tract and is one of the most common causes of peptic ulcer disease (PUD). This discovery of H. pylori made possible not only to understand the origin of the disease, but also to use an appropriate treatment and prevent PUD recurrence.
Current guidelines do not recommend an active search for H. pylori infection in an asymptomatic population. Nevertheless, prevention of H. pylori infection is possible and even simple recommendations can minimize the spread of bacteria.
The following section contains information regarding epidemiology, transmission routes, symptoms of infection, and contribution of H. pylori into the development of PUD.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Gastric ulcer
- Helicobacter pylori
- Nonsteroidal anti-inflammatory drugs
- Peptic ulcer disease
- Virulence factors
1 Background
Helicobacter pylori (H. pylori, previously also known as Campylobacter pyloridis) is a gram-negative, microaerophilic, and spiral-shaped bacteria 0.5–1 μm in width and 2.5–5 μm in length, which colonizes the gastric mucosa of approximately one-half of the world population. H. pylori was first isolated by John Robin Warren and Barry Marshall in 1983 from the gastric mucus of patients with chronic inflammation [1]. Both scientists were awarded the Nobel Prize in Physiology or Medicine in 2005 for the discovery of H. pylori and explanation of its role in the induction of inflammatory gastritis and peptic ulcer [2].
Peptic ulcer disease (PUD) usually develops as a consequence of H. pylori infection or use of nonsteroidal anti-inflammatory drugs (NSAIDs), which include drugs commonly available without prescription, such as aspirin, ibuprofen, and naproxen, as well as many prescription-strength NSAIDs. H. pylori also plays a role in the multifactorial process of gastric cancer development which is the second leading cause of cancer-related mortality worldwide [3].
2 Epidemiology, Prevalence, and Sources of H. pylori Infection
H. pylori infection is one of the most common infections in human [4]. It is believed that more than half of the population may be infected but the clinical symptoms occur in only a small portion, and the tumor grows only in about 1% of infected humans. However, H. pylori is found in 95% of patients with duodenal ulcers and in 70% of those with gastric ulcers [5]. Furthermore, it is estimated that H. pylori is the cause of about 65% of all stomach tumors [6]. Overall, the prevalence of the infection, which can last for years, varies considerably between countries and depends mostly on socioeconomic status of their inhabitants. In developed countries, the infection affects approximately 70–90% of adults whereas in developing countries it ranges between 25–50% [7]. In South America, Africa, and in some regions of Asia, the infection can affect even up to 100% of population. The disease progression primarily depends on bacterial virulence factors, the individual characteristics of the host, and to some degree, on environmental factors, e.g. cigarette smoking and diet [4].
The H. pylori infection is thought to spread by personal contacts, either the fecal-oral route during early childhood or by oral-oral and gastro-oral route of transmission. It is generally believed that acquisition mostly occurs in early childhood, most likely from close family members [8]. H. pylori has been isolated from saliva, vomitus, gastric refluxate, and feces [9], but there is no conclusive evidence for transmission via any of these products. The presence of H. pylori was also detected in pet animals. Thus pets may be a risk factor for infection [10].
3 H. pylori vs. Peptic Ulcer
H. pylori dwells in the stomach’s acidic environment. Urease enzyme produced by bacteria enables them not only to survive in acidic gastric juice but also to reach the epithelial cells. Urease catalyzes the hydrolysis of urea to carbon dioxide and ammonia. Ammonia, by alkalizing the environment causes neutralization of gastric juice and thus enables H. pylori to pierce through the layer of mucus and reach the epithelium. In addition, H. pylori induces directly or indirectly the formation of damage of the gastric mucosa [11]. Hydroxide ions from dissociation of ammonia in an aqueous medium are cytotoxic to the gastric epithelial cells [11]. Increased pH leads to an increased release of gastrin and stimulation of the parietal cells to the hydrochloric acid production. Therefore, ammonia has been implicated in the development of micro-erosions of the mucosa, which in turn is accompanied by the release of many nutrients for the bacteria [12]. There are important H. pylori virulence factors that, along with host characteristics and the external environment, have been associated with the occurrence of the disease. The basic virulence factors of H. pylori are urease, flagella, adhesins, lipopolysaccharide (LPS), catalase, lipases, phospholipases, proteases, activity of two proteins—cytotoxin-associated gene A antigen (CagA) and vacuolating cytotoxin A (VacA), variability of strains, adhesion to the epithelium surface and bacterial transport systems of proteins to the cell surface (Fig. 8.1) [13]. All these factors allow H. pylori to colonize and damage gastric mucosa.
The main cause of the pathogenicity of bacteria is its ability to induce chronic inflammation which results from excessive stimulation of the host immune response involving all types of immune cells and various types of cytokines. The continuous stimulation of the immune system, which normally allows the spontaneous elimination of microorganisms from the body, leads to the development of lesions in the gastric mucosa. The results of numerous studies also indicate the ability of H. pylori to inhibit the activity of immune cells [14]. Thus, the adaptation processes and the host immune response to bacterial infection provide the survival of H. pylori in the unique environment of the stomach.
Several cohort studies demonstrated that the risk of PUD in H. pylori-infected subjects is 3–10 times higher than in healthy controls [15] and 10–15% of H. pylori-positive subjects developed ulcer disease. Furthermore, 50% of patients with H. pylori-associated PUD suffered ulcer recurrence within 1 year [16]. Eradication of H. pylori prevents almost completely ulcer recurrence [17]. However, recurrences of ulcer after successful eradication therapy can be due to renewed H. pylori infection, use of NSAIDs, or idiopathic ulcer disease.
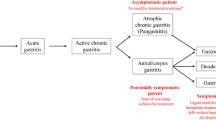
4 Disturbing Symptoms
Most people with H. pylori infection do not have any signs or symptoms for a long time and currently there is no evidence that testing healthy people with no symptoms is useful. However, the bacteria may cause symptoms of acute gastritis such as indigestion, bloating, abdominal pain (especially ache or burning pain in the abdomen), nausea, vomiting, fever, and diarrhea. The other symptoms of H. pylori infection, which patients also should be aware of, are loss of appetite, frequent burping, and unintentional weight loss. These symptoms may quickly disappear. However, this does not mean that the bacteria has been eliminated. Patients with symptoms mentioned above should see their doctor to discuss appropriate testing.
Patients should also know that it is hard to avoid infection with H. pylori. However, first and foremost, the basic principles of hygiene must be maintained, including washing hands and brushing teeth regularly. One of the factors that increase the risk of recurrence of bacterial infection is tooth decay or other dental diseases that require dental treatment [18].
5 Diagnosis
There are two general ways in which a diagnosis of infection by H. pylori can be made: invasive and non-invasive methods. The choice of method is determined by the current clinical situation and the need to perform endoscopic examination of the upper gastrointestinal tract (invasive methods such as the rapid urease test (RUT), histology, culture, and molecular biology techniques). Non-invasive procedures include tests using readily available materials research, such as exhaled air, feces, or saliva (13C-urea breath test (13C-UBT), stool antigen test (SAT), and serological tests). (For detailed information, see (Chap. 4).
5.1 Selection of Diagnostic Test
In-house and online pharmacies propose several rapid blood tests. These tests are designed to detect antibodies produced in response to the H. pylori infection. If the antibodies are present, the test gives a positive result. Of note, these tests have some limits that everyone should be aware of. Blood tests cannot differentiate between a past infection and the current status of an H. pylori infection. In other words, if patient has already been infected with H. pylori in the past and the infection was eliminated using antibiotics, this test may yield a positive reading even more than 1 year following treatment, even though the infection is no longer present. Another limitation is due to the fact that the test is done by the patients themselves at home, so it may give false results. However, if you suspect being infected, and if you have never been treated for H. pylori before, you may test yourself. If you obtain a positive result—then you are likely to be infected with H. pylori. In that case, consult a physician for definitive diagnosis and possible treatment.
Selection of an appropriate procedure by the physician is determined by cost, availability of equipment and reagents, expertise, and pre-test probability for H. pylori. The selection of the test depends also on the sensitivity, specificity, and availability. Currently, none of the methods cover these criteria perfectly. Although biopsy-based methods have a very high specificity, only a moderate sensitivity is observed in these procedures. Furthermore, RUT, histopathology, and culture may be used in patients who did not take antibiotics and PPIs over the past 2 weeks.
Polymerase chain reaction (PCR) is a highly sensitive and specific method and may be applicable in the detection of H. pylori infection and in the assessment of treatment [19]. However, the main disadvantage of PCR is the low level of availability of this procedure in poor regions of the world due to high cost of the diagnostic equipment.
Without any doubt, none of the tests shows 100% accuracy, thus two procedures with different mechanisms should be used. However, satisfactory results may be obtained with UBT in combination with SAT or serological tests. A positive serology must be also confirmed by other methods due to variable sensitivity and specificity [20]. The result of the meta-analysis showed clearly that UBT has high diagnostic accuracy for detecting H. pylori infection in patients with dyspepsia among non-invasive procedures [21]. Monoclonal SAT is less accurate, but it seems a good option, especially in children.
6 Treatment
6.1 Standard Therapy vs. Sequential Therapy
There is no perfect and reliable drug regimen for the treatment of H. pylori so far. Typically, treatment lasts 10–14 days. First-line therapy consists of two of the three commonly used antibiotics such as amoxicillin, clarithromycin, and metronidazole, and PPIs. Dual therapies are not as effective as triple therapy and are not recommended. After failure, a quadruple therapy regimen is recommended with the addition of tetracycline or bismuth. When a second-line therapy fails, the management strategy includes an assessment of the sensitivity of H. pylori to amoxicillin, clarithromycin, metronidazole, and tetracycline. Of note, clarithromycin and metronidazole show the highest rates of resistance. The main factors associated with the resistance are geographic region, sex, ethnicity, and age of patients [22].
Sequential therapy allows to use more antibiotics, in successive stages which typically lasts 5–7 days. An example of such therapy is as follows: amoxicillin + PPIs for 5 days, and PPIs + clarithromycin + metronidazole for the next 5 days. In consequence, different mechanisms of antibacterial activity with a lower risk of side effects are expected [23]. Sequential therapy has been showed to be more effective than the standard treatment [24].
6.2 Fluoroquinolones
Finding new molecules for treatment of H. pylori infection is a part of ongoing research programs, which include study of the fluoroquinolones. These compounds have a fluorine atom and exhibit concentration-dependent activity by inhibiting DNA gyrase and topoisomerase, enzymes essential for bacterial DNA replication.
There are many attempts to use levofloxacin (LEV)-based triple therapy. In a multicenter clinical trial, patients received omeprazole + amoxicillin for the first 5 days, followed by 5 days omeprazole + tinidazole, and depending on the group—clarithromycin and LEV. Results showed that eradication rate with clarithromycin sequential therapy was 80.8%, while administration of LEV reported 96.0% eradication rate, respectively. Furthermore, no differences in prevalence of antimicrobial resistance or incidence of adverse effects were observed between the groups [25].
In a randomized trial by Bago et al., 150 patients underwent an alternative therapy with a fourth-generation synthetic fluoroquinolone—moxifloxacin [26]. One group of patients received moxifloxacin once daily, and amoxicillin and lansoprazole for 7 days, while the other group received the same drug for 10 days. Eradication rates reached 84% in the first group of patients, and 90% in the second group. The treatment was well-tolerated. Mild gastrointestinal symptoms and headache were more frequently reported (without statistical significance) in patients who underwent a 10-day treatment.
Another fluoroquinolone taken into account in therapy regimens is sitafloxacin, in combination with PPIs and amoxicillin or metronidazole [27]. The effectiveness of such antibacterial therapy was 100 and 91.6%, respectively. Studies showed that fluoroquinolones had higher antibacterial activity [28].
Detailed recommendations for the pharmacological treatment has been described in Chap. 5.
7 H. pylori and Non-steroidal Anti-Inflammatory Drugs
H. pylori infection is associated with increased risk of complicated or uncomplicated gastric and duodenal ulcers during the use of NSAIDs or low doses of aspirin. Infection of H. pylori and NSAIDs are independent risk factors for PUD and PUD-related complications, mainly bleeding [29]. Eradication reduces the risk of ulcers at the time of application of these drugs and should be performed before NSAIDs treatment, especially in patients with a history of gastric ulcers [30]. However, eradication alone does not reduce the risk of ulcers in patients already using NSAIDs and besides eradication, PPIs should be constantly used [31]. Eradication of H. pylori should also be performed in patients with PUD who take a low-dose of aspirin. After successful eradication, the risk of bleeding in these patients is reduced even without gastroprotective treatment [32].
8 Basic Recommendations for the Patient
People who are suffering from H. pylori should regularly eat their meals. Under no circumstances can you allow neither feeling hungry nor surfeit, which results in overproduction of stomach acid. Therefore, the interval between meals should be 2–3 h. Moreover, patients should eat 4–6 small meals a day and meals should be eaten slowly, thoroughly chewing each bite (preferably, all meals should be well cooked and shredded). The first meal should be eaten shortly after waking, and the last no later than 2–3 h before bedtime.
A diet in patients with H. pylori infection should support a pharmacological treatment process aimed at removing H. pylori from the stomach. It should also help to lower the levels of stomach acid, which is responsible for most of the ailments associated with H. pylori infection. The purpose of the diet is also to allow the regeneration of the gastric and duodenal mucosa.
9 Eradication of H. pylori
Testing for eradication of H. pylori is recommended for all patients diagnosed with H. pylori-associated PUD [33], severe forms of gastritis, early gastric cancer, mucosa associated lymphoid tissue lymphoma (MALT), partial resection of gastric cancer, family history of gastric cancer or Ménétrier’s disease, and also in case of recurrence after treatment. The tests evaluating the efficacy of H. pylori eradication should be carried out 4 weeks after completion of therapy, preferably after 6–8 weeks. Preferred invasive methods are RUT or histological examination. However, all tests are less accurate in therapy based on bismuth-containing compounds. Furthermore, PPIs therapy within 1–2 weeks of testing can cause false-negative results [34].
Eradication rates can be increased using probiotic supplementation. Lactobacillus sp. have shown to increase eradication rates by 10% when compared to placebo [35, 36]. Probiotics may also decrease side effects of antibiotic therapy, including diarrhea, without increasing adverse effects [37]. Furthermore, recent meta-analysis showed positive results with administration of Saccharomyces boulardii yeast [38]. However, a rational prescribing of antibiotics (to avoid H. pylori strains resistant) and strict adherence to the recommendations of physicians by patients have the greatest impact on improving the results of eradication therapy. Patients should also be aware of the simplest recommendations such as washing hands and separate sleeping places for children because it is a significant factor in the spread of infection.
10 Untreated H. pylori
An increased risk of PUD and gastric adenocarcinoma is associated with untreated H. pylori infection [39]. Furthermore, both use of NSAIDs and cigarette smoking in combination with H. pylori synergistically increase the risk of PUD.
H. pylori infection has also an impact on the absorption of drugs [40]. It has been demonstrated that there is a need for supplementation with higher doses of thyroxine in patients with hypothyroidism infected with H. pylori. In patients infected with H. pylori and HIV-positive, a 15% increase in absorption of antiviral drugs was observed as a result of eradication therapy, and in patients treated with L-3,4-dihydroxyphenylalanine (L-DOPA) during treatment of Parkinson’s disease, eradication therapy increased the absorption of drugs to 54%. These examples indicate that the H. pylori infection reduces the secretion of hydrochloric acid and impairs the absorption of pH gastric acid-dependent drugs.
H. pylori infection is associated with increased risk of gastric MALT lymphoma. However, successful eradication may cause regression of MALT lymphoma [41]. Furthermore, some studies have also linked H. pylori with unexplained iron deficiency anemia, idiopathic thrombocytopenic purpura (ITP), and B12 vitamin deficiency [42].
Conclusion
Most people do not realize they may have H. pylori infection, because they never get any symptoms. Risk factors for H. pylori infection are related to living conditions, such as: living in a developing country, living without a reliable supply of clean water, and living with someone who has an H. pylori infection. H. pylori may be also passed from person to person through direct contact with saliva, vomit or fecal matter or be spread through contaminated food and water. Thus, if you develop any signs and symptoms, you should see your doctor as soon as possible. Furthermore, patients with peptic ulcer disease, dyspepsia symptoms, or MALT lymphoma should also be evaluated for possible H. pylori infection.
Abbreviations
- CagA:
-
Cytotoxin-associated gene A
- LEV:
-
Levofloxacin
- LPS:
-
Lipopolysaccharide
- MALT:
-
Mucosa associated lymphoid tissue lymphoma
- NSAIDs:
-
Nonsteroidal anti-inflammatory drugs
- PCR:
-
Polymerase chain reaction
- PPIs:
-
Proton pump inhibitors
- PUD:
-
Peptic ulcer disease
- RUT:
-
Rapid urease test
- SAT:
-
Stool antigen test
- UBT:
-
Urea breath test
- VacA:
-
Vacuolating cytotoxin A
References
Marshall BJ, Warren JR. Unidentified curved bacilli in the stomach of patients with gastritis and peptic ulceration. Lancet. 1984;8390:1311–5.
Mégraud F. A humble bacterium sweeps this year’s Nobel Prize. Cell. 2005;123:975–6.
Qadri Q, Rasool R, Gulzar GM, Naqash S, Shah ZA. H. pylori infection, inflammation and gastric cancer. J Gastrointest Cancer. 2014;45:126–32.
Amieva MR, El-Omar EM. Host-bacterial interactions in Helicobacter pylori infection. Gastroenterology. 2008;134:306–23.
Ford AC, Delaney BC, Forman D, Moayyedi P. Eradication therapy for peptic ulcer disease in Helicobacter pylori positive patients. Cochrane Database Syst Rev. 2006;2:CD003840.
Benjamin JB, Jayanthi V, Devaraj H. MUC1 expression and its association with other aetiological factors and localization to mitochondria in preneoplastic and neoplastic gastric tissues. Clin Chim Acta. 2010;411:2067–72.
Farinha P, Gascoyne RD. Helicobacter pylori and MALT lymphoma. Gastroenterology. 2005;128:1579–605.
Raymond J, Thiberg JM, Chevalier C, Kalach N, Bergeret M, Labigne A, Dauga C. Genetic and transmission analysis of Helicobacter pylori strains within a family. Emerg Infect Dis. 2004;10:1816–21.
Kabir S. Detection of Helicobacter pylori DNA in feces and saliva by polymerase chain reaction: a review. Helicobacter. 2004;9:115–23.
Brown LM, Thomas TL, Ma JL, Chang YS, You WC, Liu WD, Zhang L, Gail MH. Helicobacter pylori infection in rural China: exposure to domestic animals during childhood and adulthood. Scand J Infect Dis. 2001;33:686–91.
Smoot DT, Mobley HL, Chippendale GR, Lewison JF, Resau JH. Helicobacter pylori urease activity is toxic to human gastric epithelial cells. Infect Immun. 1990;58:1992–4.
Salama NR, Hartung ML, Müller A. Life in the human stomach: persistence strategies of the bacterial pathogen Helicobacter pylori. Nat Rev Microbiol. 2013;11:385–99.
Cooke CL, Huff JL, Solnick JV. The role of genome diversity and immune evasion in persistent infection with Helicobacter pylori. FEMS Immunol Med Microbiol. 2005;45:11–23.
Sundrud MS, Torres VJ, Unutmaz D, Cover TL. Inhibition of primary human T cell proliferation by Helicobacter pylori vacuolating toxin (VacA) is independent of VacA effects on IL-2 secretion. Proc Natl Acad Sci U S A. 2004;101:7727–32.
Nomura A, Stemmermann GN, Chyou PH, Perez-Perez GI, Blaser MJ. Helicobacter pylori infection and the risk for duodenal and gastric ulceration. Ann Intern Med. 1994;120:977–81.
Hentschel E, Brandstätter G, Dragosics B, Hirschl AM, Nemec H, Schütze K, Taufer M, Wurzer H. Effect of ranitidine and amoxicillin plus metronidazole on the eradication of Helicobacter pylori and the recurrence of duodenal ulcer. N Engl J Med. 1993;328:308–12.
Treiber G, Lambert JR. The impact of Helicobacter pylori eradication on peptic ulcer healing. Am J Gastroenterol. 1998;93:1080–4.
Al Asqah M, Al Hamoudi N, Anil S, Al Jebreen A, Al-Hamoudi WK. Is the presence of Helicobacter pylori in dental plaque of patients with chronic periodontitis a risk factor for gastric infection? Can J Gastroenterol. 2009;23:177–9.
Patel SK, Mishra GN, Pratap CB, Jain AK, Nath G. Helicobacter pylori is not eradicated after triple therapy: a nested PCR based study. Biomed Res Int. 2014;2014:483136.
Malfertheiner P, Megraud F, O’Morain CA, Atherton J, Axon AT, Bazzoli F, Gensini GF, Gisbert JP, Graham DY, Rokkas T, El-Omar EM, Kuipers EJ, European Helicobacter Study Group. Management of Helicobacter pylori infection- the Maastricht IV/Florence Consensus report. Gut. 2012;61(5):646–64.
Ferwana M, Abdulmajeed I, Alhajiahmed A, Madani W, Firwana B, Hasan R, Altayar O, Limburg PJ, Murad MH, Knawy B. Accuracy of urea breath test in Helicobacter pylori infection: meta-analysis. World J Gastroenterol. 2015;21:1305–14.
Meyer JM, Silliman NP, Wang W, Siepman NY, Sugg JE, Morris D, Zhang J, Bhattacharyya H, King EC, Hopkins RJ. Risk factors for Helicobacter pylori resistance in the United States: the surveillance of H. pylori antimicrobial resistance partnership (SHARP) study, 1993–1999. Ann Intern Med. 2002;136:13–24.
Luther J, Higgins PD, Schoenfeld PS, Moayyedi P, Vakil N, Chey WD. Empiric quadruple vs. triple therapy for primary treatment of Helicobacter pylori infection: systematic review and meta-analysis of efficacy and tolerability. Am J Gastroenterol. 2010;105:65–73.
Paoluzi OA, Visconti E, Andrei F, Tosti C, Lionetti R, Grasso E, Ranaldi R, Stroppa I, Pallone F. Ten and eight-day sequential therapy in comparison to standard triple therapy for eradicating Helicobacter pylori infection: a randomized controlled study on efficacy and tolerability. J Clin Gastroenterol. 2010;44:261–6.
Romano M, Cuomo A, Gravina AG, Miranda A, Iovene MR, Tiso A, Sica M, Rocco A, Salerno R, Marmo R, Federico A, Nardone G. Empirical levofloxacin-containing versus clarithromycin-containing sequential therapy for Helicobacter pylori eradication: a randomised trial. Gut. 2010;59:1465–70.
Bago J, Majstorović K, Belosić-Halle Z, Kućisec N, Bakula V, Tomić M, Bago P, Troskot R. Antimicrobial resistance of H. pylori to the outcome of 10-days vs. 7-days moxifloxacin based therapy for the eradication: a randomized controlled trial. Ann Clin Microbiol Antimicrob. 2010;9:13.
Furuta T, Sugimoto M, Codaira C. Comparison of triple rabeprazole/metronidazol/sitafloxacin therapy with triple rabeprazole/amoxicillin/sitafloxacin therapy as the third rescue regimen for eradication of H. pylori. Helicobacter. 2010;14:28.
Otani T, Tanaka M, Ito E, Kurosaka Y, Murakami Y, Onodera K, Akasaka T, Sato K. In vitro and in vivo antibacterial activities of DK-507k, a novel fluoroquinolone. Antimicrob Agents Chemother. 2003;47:3750–9.
Huang JQ, Sridhar S, Hunt RH. Role of Helicobacter pylori infection and non-steroidal anti-inflammatory drugs in peptic-ulcer disease: a meta-analysis. Lancet. 2002;359:14–22.
Chan FK, To KF, Wu JC, Yung MY, Leung WK, Kwok T, Hui Y, Chan HL, Chan CS, Hui E, Woo J, Sung JJ. Eradication of Helicobacter pylori and risk of peptic ulcers in patients starting long-term treatment with non-steroidal anti-inflammatory drugs: a randomised trial. Lancet. 2002;359:9–13.
Vergara M, Catalán M, Gisbert JP, Calvet X. Meta-analysis: role of Helicobacter pylori eradication in the prevention of peptic ulcer in NSAID users. Aliment Pharmacol Ther. 2005;21:1411–8.
Chan FK, Ching JY, Suen BY, Tse YK, Wu JC, Sung JJ. Effects of Helicobacter pylori infection on long-term risk of peptic ulcer bleeding in low-dose aspirin users. Gastroenterology. 2013;144:528–35.
Talley NJ, Vakil N, Practice Parameters Committee of the American College of Gastroenterology. Guidelines for the management of dyspepsia. Am J Gastroenterol. 2005;100:2324–37.
Chey WD, Wong BC. American College of Gastroenterology guideline on the management of Helicobacter pylori infection. Am J Gastroenterol. 2007;102:1808–25.
Tong JL, Ran ZH, Shen J, Zhang CX, Xiao SD. Meta-analysis: the effect of supplementation with probiotics on eradication rates and adverse events during Helicobacter pylori eradication therapy. Aliment Pharmacol Ther. 2007;25:155–68.
Homan M, Orel R. Are probiotics useful in Helicobacter pylori eradication? World J Gastroenterol. 2015;21:10644–53.
Zou J, Dong J, Yu X. Meta-analysis: Lactobacillus containing quadruple therapy versus standard triple first-line therapy for Helicobacter pylori eradication. Helicobacter. 2009;14:97–107.
Szajewska H, Horvath A, Piwowarczyk A. Meta-analysis: the effects of Saccharomyces boulardii supplementation on Helicobacter pylori eradication rates and side effects during treatment. Aliment Pharmacol Ther. 2010;32:1069–79.
Rosenstock S, Jørgensen T, Bonnevie O, Andersen L. Risk factors for peptic ulcer disease: a population based prospective cohort study comprising 2416 Danish adults. Gut. 2003;52:186–93.
Lahner E, Annibale B, Delle FG. Systematic review: Helicobacter pylori infection and impaired drug absorption. Aliment Pharmacol Ther. 2009;29:379–86.
Fischbach W, Goebeler-Kolve ME, Dragosics B, Greiner A, Stolte M. Long term outcome of patients with gastric marginal zone B cell lymphoma of mucosa associated lymphoid tissue (MALT) following exclusive Helicobacter pylori eradication therapy: experience from a large prospective series. Gut. 2004;53:34–7.
Malfertheiner P. Helicobacter pylori eradication does not exacerbate gastro-oesophageal reflux disease. Gut. 2004;53(2):312–3.
Acknowledgments
The work is supported by grants from the Medical University of Lodz (#502-03/1-156-04/502-14-239 to AW, #502-03/1-156-04/502-14-299 to PM, and #503/1-156-04/503-11-001 to JF) and grant from National Science Centre [#UMO-2016/21/N/NZ5/01932 to PM].
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this chapter
Cite this chapter
Wasilewski, A., Mosińska, P. (2017). Patient’s Guide: Helicobacter pylori in Peptic Ulcer Disease. In: Fichna, J. (eds) Introduction to Gastrointestinal Diseases Vol. 2. Springer, Cham. https://doi.org/10.1007/978-3-319-59885-7_8
Download citation
DOI: https://doi.org/10.1007/978-3-319-59885-7_8
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-59884-0
Online ISBN: 978-3-319-59885-7
eBook Packages: MedicineMedicine (R0)