Abstract
The objective of this chapter is to discuss the decision-making and surgical technique of lumbar osteotomies for treatment of malalignment. A comprehensive literature review was performed on the history, indications, preoperative evaluation, and decision-making in patients with sagittal and coronal plane malalignment, as well as surgical technique for lumbar osteotomies. There has been an evolution of many different types of osteotomies for correcting deformities; however, three general categories exist: (1) posterior column osteotomy (PCO), (2) pedicle subtraction osteotomy (PSO), and (3) vertebral column resection (VCR). More recently, the Schwab classification describes six anatomically defined osteotomies that are commonly accepted and used. Utilizing the best available evidence, we review the indications and patient selection as a first step and then discuss the decision-making and preoperative planning. Lastly, we detail the surgical technique with emphasis on complication avoidance.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Adult spinal deformity is becoming increasingly common in our aging US population [1]. In addition to degenerative etiologies , iatrogenic sagittal malalignment complications are more common with the increase in lumbar fusion procedures being performed. The critical goal in the surgical treatment of the adult deformity patient is twofold: (1) restoration of anatomic alignment and (2) preservation of function.
Sagittal balance and overall global spinal alignment have been shown to be one of the most important factors associated with improvement in patient outcomes following adult deformity surgery [2]. In the past decade, studies have found that restoration of normal or near-normal spinopelvic parameters correlates closely with health-related quality of life (HRQOL) and pain measures in both deformity and degenerative patients [3]. Although coronal alignment has not been as important as sagittal alignment, fusing the spine such that the torso is balanced over the pelvis within the cone of economy in both planes does allow better global balance of the spine and is seen as an optimal goal [4]. Fusion of the spine with significant residual coronal or sagittal malalignment can place excessive stresses through both the instrumented segments and non-instrumented segments of the spine contributing to additional degeneration, instrumentation failure, and progression of the malalignment [5, 6].
In this chapter, we will review modern surgical corrective techniques for spinal deformity focusing on lumbar osteotomies that can be utilized to improve sagittal and coronal alignment and restore global spinal alignment in the adult patient. The origins of these techniques will be briefly reviewed to help frame and appreciate the advancement of correction methodology that has occurred. Utilizing the best available evidence, we then will review the indications and patient selection as a first step and also discuss the decision-making process and preoperative planning. Lastly, we detail the surgical technique of the most common osteotomy types with emphasis on complication avoidance. Although variations exist, three general categories of osteotomy have been described: (1) posterior column osteotomy (PCO), (2) pedicle subtraction osteotomy (PSO), and (3) vertebral column resection (VCR). More recently, the Schwab classification describes six anatomically defined osteotomies that are commonly accepted and used [7].
History
The surgical techniques for restoration of spinal alignment continue to evolve (Fig. 22.1). The posterior column osteotomy (PCO) includes both the Smith-Petersen osteotomy (SPO) and the Ponte osteotomy . In 1945, Smith-Petersen et al. described a posterior extension or chevron-type osteotomy combined with anterior osteoclasis for single-level correction of kyphosis in the setting of ankylosing spondylitis [8]. The Smith-Petersen osteotomy involves bilateral removal of the facet joints or fusion mass allowing the spine to pivot along the middle column increasing segmental lordosis and causing an extension in length of the anterior column [9]. In modern practice, the SPO is usually performed across multiple segments for correction of a multi-segmental deformity [10]. The osteotomies can be performed asymmetrically to allow for some degree of coronal plane correction [11]. Because SPO requires lengthening of the anterior column, the patient must have a mobile anterior disc in theory; thus, it cannot be optimally effective across a fully ankylosed segment .
The Ponte-type osteotomy was first described by Ponte et al. in 1984 for Scheuermann kyphosis and is described as segmental osteotomies followed by posterior decompression along unfused regions of kyphotic deformity [12]. Although today the terms Smith-Petersen osteotomy and Ponte osteotomy are used interchangeably, the modern technique more closely resembles the procedure described by Alberto Ponte. In fact, these osteotomies have also become a mainstay in correction of coronal plane deformities , such as in adolescent idiopathic scoliosis .
Pedicle subtraction osteotomy (PSO) was first introduced by Thomasen in 1985 [13]. The PSO has further been referred to as a transpedicular wedge procedure , wedge osteotomy , and eggshell osteotomy . PSO has found widespread use for fixed, angular sagittal plane deformity resulting from multiple etiologies [14]. Like vertebral column resection (VCR ), PSO has been associated with significant perioperative complications; however, modern advancements in anesthetic management, surgical technique, and postoperative critical care have all led to improved patient outcomes [15]. Neurological injury is the most devastating complication when performing osteotomies; evolution from the “wake-up test ” popularized by Vauzelle in 1973 to the use of somatosensory evoked potentials (SSEPs) by Nash and motor evoked potentials (MEPs) by Tamaki together has allowed direct feedback regarding spinal cord function with a high degree of accuracy to more widely perform these procedures safely [16,17,18]. Additionally, in part because of the aforementioned advancements, the utilization of these procedures has dramatically increased, as much as fourfold, over the last decade [19]. Although the complication rate with regard to neurological deficit is still significant, neurologic complications can be minimized with the use of modern neuromonitoring techniques [20,21,22].
Vertebral column resection (VCR) was first described by MacLennan in 1922 for the treatment of severe scoliosis via posterior vertebrectomy and postoperative casting [23]. The approach to VCR has undergone its own evolution in the past decades. Bradford described a circumferential approach when performing a VCR, performing a circumferential VCR with concave rib osteotomies , convex thoracoplasty , and segmental spinal instrumentation [24]. Often staging of anterior and posterior approaches was done due to long operative times [25]. Suk et al. reported on a posterior-only approach (PVCR) allowing for simultaneous control of the spinal column and access to the neural elements [26]. VCR consists of complete resection of at least one vertebral segment through either a posterior alone or combined anterior-posterior approach for multiplanar correction of severe rigid spinal deformity [24]. Often concomitant with the PVCR, posterior releases of the ligaments and facets via adjacent level PCO’s are done [9].
At present, there are many variations of established techniques including hybrid and minimally invasive techniques [27]. Despite these variations, an anatomically based classification can provide a common language among spine surgeons to describe osteotomy types. A comprehensive and widely accepted classification has been described by Schwab and Lafage et al. [7]. This classification system is based on six anatomical grades of resection (1, 6, through) corresponding to the extent of bone resection and increasing degree of destabilizing potential. Grades 1 and 2 include PCOs and involve partial (Grade 1) or full (Grade 2) resection of the facet joints. Grades 3 and 4 represent PSO or extended PSO, thus involving resection of the pedicle, partial vertebral body (Grade 3), and possibly the cranial disc (Grade 4). Grades 5 and 6 represent VCR so that the complete vertebral body and disc are removed (Grade 5) or multiple vertebral bodies (Grade 6) and discs. In addition, a surgical approach modifier can be added (posterior approach or combined anterior and posterior approaches).
Indications and Patient Selection
In general, the type of osteotomy chosen should take many factors into consideration including but not limited to the severity of deformity and underlying pathology, flexibility of the spine, bone density/quality, operative goals, surgeon’s experience and comfort level, and critical care support. Age, regional and global alignment, comorbidities, psychosocial status, and amount of postoperative activity also influence the decision-making process including whether surgical or conservative therapy is indicated. Furthermore, symptoms such as radiculopathy or axial back pain will also influence the extent of decompression and arthrodesis. Patients with radicular leg pain were more likely to proceed with surgery than those with back pain [28]. Furthermore, it has been demonstrated that sagittal spinopelvic alignment varies with age, and thus operative realignment goals should also account for age with younger patients requiring more rigorous alignment objectives [29].
The surgeon should develop an algorithmic approach to this complex decision-making process. The mnemonic TEAMS can aid in developing a comprehensive decision : (1) Type of curve, (2) End points of deformity, (3) Apex of deformity, (4) Mobile disc segments, and (5) Stable cone of economy. Table 22.1 provides a quick reference for selection of osteotomy procedure.
Posterior Column Osteotomy (PCO)
Indications for considering PCO’s would include a deformity with a mobile anterior column, where adequate disc height and mobility of the disc space anteriorly can add to the corrective potential. The deformity may be either in the sagittal plane such as kyphosis or in the coronal plane. For sagittal plane deformity, typically symmetric shorting of the posterior column yields 1° of correction per millimeter of bone resected, thus requiring correction to be carried out over multiple levels [9]. This type of osteotomy lends itself very well to any mild to moderate malalignment that is degenerative in origin.
The PCO provides roughly 5–10° of angular correction per level. Three PCOs are able to achieve a degree of correction comparable to a single PSO with no difference in fusion rates or patient-reported outcome [9]. A PCO may be combined with an anterior release or performed as a stand-alone posterior approach. In a patient with combined sagittal and coronal deformity and shoulder angulation tilted to the concavity, an anterior release followed by multilevel PCOs can be a useful technique.
Fixed angular deformity and ossification of the anterior longitudinal ligament are relative contraindications to a posterior column osteotomy. Compression of instrumentation after multilevel PCO results in gradual, harmonious correction of a smooth kyphotic curve rather than angular correction. The classic indication for a PCO is a long smooth kyphosis such as in Scheuermann kyphosis . In adult deformities, PCO is often a good option if the patient has a flexible kyphotic deformity, as evidenced by correction on hyperextension films or supine positioning such as MRI or CT scanning (Fig. 22.2). Although an anterior gap may be created after SPO, there is typically no need for an anterior bone graft. The Zielke technique involves multiple PCOs at all levels from T10 to the sacrum [10].
Case example of Ponte osteotomies . (a) Standing AP 36-inch scoliosis x-ray of patient with prior L4–L5 TLIF. (b) Standing lateral 36-inch scoliosis x-ray demonstrates severe sagittal imbalance and rounded kyphosis. Disc spaces above L4–L5 fusion are still open. (c) Prone hyperextension lateral x-ray demonstrates significant correction and relatively mobile discs. (d) Instrumentation placed with multiple Ponte osteotomies through thoracolumbar junction and upper lumbar spine. (e) Standing postoperative AP 36-inch scoliosis x-ray demonstrates T4–ilium instrumented fusion. (f) Standing postoperative lateral 36-inch scoliosis x-ray demonstrates restoration of normal spinal alignment
Pedicle Subtraction Osteotomy (PSO)
PSOs can achieve approximately 30 to 40° of correction in the sagittal plane at the level that it is performed [30]. Closure of the osteotomy occurs in a wedge fashion, bringing kyphosis into correction via posterior shortening (Fig. 22.3). Briefly, the technique consists of resection of the entire posterior elements of the vertebral body, including pedicles, followed by a wedge-shaped removal of the posterior cortex and cancellous bone from the vertebral body. A variation includes the extended PSO which, in addition, incorporates resection of the cranial disc. The closure of the osteotomy hinges on the anterior column. In the lumbar spine, there is a broad anterior cortical surface that can function as a rigid pivot for PSO closure helping to prevent translation.
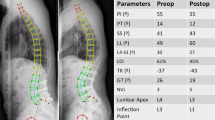
Case example of pedicle subtraction osteotomy . (a) Standing AP 36-inch scoliosis x-ray of patient with prior L2–L5 posterior fusion. (b) Standing lateral 36-inch scoliosis x-ray demonstrates sagittal imbalance with angular kyphosis above prior fusion. (c) Standing postoperative AP 36-inch scoliosis x-ray demonstrates T10–ilium fusion with pedicle subtraction osteotomy through L3. (d) Standing postoperative lateral lumbar x-ray demonstrates significant correction through PSO
PSOs are not commonly used in the distal lumbar spine because of limited fixation points distally. However, more recent studies suggest the lower the PSO is performed, the more physiologic is the restoration of lumbar lordosis as the majority of lumbar lordosis is found between L4 and S1. This appears to also correlate with patient satisfaction [31]. The best candidates for a PSO are patients with the following conditions: [1] sagittal malalignment of more than 10 cm, [2] sharp angular kyphosis, and [3] fixed sagittal malalignment caused by anterior ankylosis or circumferential fusion between multiple segments [32]. Other indications would include flat-back deformity or fixed kyphotic deformity. It is the preferred osteotomy for patients with ankylosing spondylitis who have sagittal malalignment.
The most common levels for a PSO are L2, L3, and L4. Recent studies have shown that the level of the PSO (L3 versus L4) does not affect the degree of correction; but lower lumbar PSOs correlate with an increased correction in pelvic tilt [33]. Ideally, the PSO should be performed at the apical region of the kyphosis or at the epicenter of the junctional deformity. Recent advances in pelvic fixation techniques, such as S2 alar iliac screws, have allowed these osteotomies to be performed more distally. Although the overall complication rate is high, there is high success rate with fusion due to bone contact across three columns and low reported rates of pseudarthrosis [34]. An extended PSO has been described as the wedge of vertebral body resection to include the disc space above the decancellated segment. Typically an extended PSO is used for correction of thoracolumbar junctional kyphosis and focal junctional kyphosis including arthrodesis of the interspace after the cephalad disc is resected .
Vertebral Column Resection
The VCR is reserved for malalignment that is severe enough that other osteotomies cannot correct the deformity, especially in patients who have combined coronal and sagittal malalignment. It is also more commonly used for rigid deformities in the thoracic and thoracolumbar spine, whereas PSO is more likely used in the lumbar spine. The VCR can result in 40 to 60° of correction at a single level.
Indications for VCR include fixed trunk translation , severe scoliosis (often of a congenital or neuromuscular origin), spondyloptosis , spinal tumor , rigid spinal deformity of more than 80° in the coronal plane, and severe asymmetry between the length of the convex column and length of concave column of the deformity [24].
The VCR essentially is an extension of the three-column resection of the PSO, involving opening of the anterior column and closing of the posterior column after complete removal of the posterior elements and vertebral body, with placement of an anterior cage or strut graft to serve as the pivot (Fig. 22.4). Nerve roots can be ligated and sacrificed in the thoracic spine to improve exposure to the vertebral body. The vertebral body is then completely resected, including the anterior cortex. Because the entire vertebra is removed, this is a highly unstable osteotomy; the anterior cortex is not left as a pivot point, as in the PSO. Thus, some type of structural graft, typically a structural cage, must be placed in the vertebrectomy defect in order to create a pivot point. A closing of the posterior portion of the osteotomy is then done to correct kyphosis. The surgery can be performed by a posterior approach only or combined anterior-posterior approach. Additionally, more recent data suggest that a staged approach is acceptable because of the length and complexity of these procedures [35].
Case example of vertebral column resection . (a) Standing AP 36-inch scoliosis x-ray of patient with congenital kyphosis. (b) Standing lateral 36-inch scoliosis x-ray demonstrates L1 dorsal hemivertebra with mild kyphosis. (c) CT scan sagittal reconstruction demonstrates L1 dorsal hemivertebra with significant encroachment into the spinal canal. (d) Parasagittal MRI demonstrates severe stenosis at level of congenital deformity. (e) Intraoperative photograph of VCR with posterior resection of hemivertebra. (f) Placement of cage following complete L1 vertebrectomy. (g) Standing postoperative AP 36-inch scoliosis x-ray demonstrates L1 cage with posterior T11–L3 fusion. (h) Standing postoperative lateral 36-inch scoliosis x-ray shows cage reconstruction and neutral thoracolumbar alignment
Preoperative Considerations
Scoliosis and other spinal deformities may be associated with various systemic diseases involving many different systems including cardiac, pulmonary, musculoskeletal, neurological, renal, and more. Furthermore, a patient may need optimization of other preexisting medical conditions including but not limited to asthma, diabetes, heart disease, tobacco abuse, any coagulopathies, nutrition, and bone health. Recognition of associated conditions and medical comorbidities, whether part of a syndrome or not, may benefit from consultation with a medical subspecialist.
It is important for the surgeon and patient to have an understanding about management and optimization of medical comorbidities before the decision is made to operate. Thus, some specific recommendations the surgeon (as well as the medical physicians) should make include the following: (1) pulmonary optimization , (2) cardiac optimization , (3) glycemic control , (4) bone health , and (5) nutritional support . Respiratory system : Thoracic curves can affect pulmonary function, and tobacco abuse is known to negatively affect spinal fusion and increase susceptibility to postoperative infection [36]. Also, smoking may place the patient at risk for perioperative respiratory infections. It is important to emphasize smoking cessation 4–6 weeks prior to surgery to allow recovery of the respiratory system [37]. Nicotine blood and urine testing is becoming more and more common in presurgical evaluation of patients undergoing spinal fusion. Cardiac system : High degree curves and pulmonary hypertension place a patient at risk for cor pulmonale. In patients with known or suspected cardiac compromise, consultation with a cardiologist during the perioperative period, as well as possible invasive cardiac monitoring during surgery, may be warranted [38]. Glycemic control : Uncontrolled diabetes mellitus has been found to be a risk factor for wound infection, nonunion, postoperative hemorrhage, acute renal failure, deep vein thrombosis, and mortality [39]. Despite the fact that even well-controlled diabetics have higher than normal complication rates, every effort should be made to maintain tight glycemic control in the perioperative setting. Bone health : Bone mineral density and physical preparation should be considered prior to surgery as well. The surgeon should always screen for osteoporosis clinically with a detailed history and obtain dual-energy x-ray absorptiometry (DEXA) testing if indicated. A useful tool, if already available, is the lumbar CT scan of the patient from which Hounsfield unit (HU) measurements can be obtained to provide both local and global bone density without additional cost and minimal effort [40]. When appropriate, it is important to initiate treatment for poor bone health or refer the patient for further management. The benefits of pre-habilitation are also becoming more evidence-based in terms of optimizing bone health, weight, function, and outcomes [41]. Nutritional support : Dietary optimization and adequate protein intake need to be considered as a serum albumin >3.5 g/L and total blood lymphocyte count >1500 cells/mm3 are associated with a decreased risk of postoperative infection and wound breakdown [42].
It is also of great importance to review all of the patient’s medications in detail prior to surgery. Try to wean patients off narcotic pain medications and muscle relaxants if possible to decrease tolerance to pain medication. Many prescription medications may be taken safely prior to and on the day of surgery such as blood pressure medications; however, several medications should be stopped prior to surgery such as blood thinners, aspirin, anti-inflammatories, herbal drugs, steroids, and some diabetic medications.
The overall clinical appearance and condition of a patient with spinal malalignment can help customize the surgical approach to individual patients. The surgeon and patient need to have specific goals for each stage of the surgery including decompression, fusion, and deformity correction. These goals should be individualized so as to obtain maximum benefit while minimizing complications . Table 22.2 summarizes general preoperative considerations prior to the day of surgery. The larger or more severe the curve and thus corresponding deformity, the more important significant correction is to the patient-reported outcome of the surgery. Recent studies have emphasized the importance of patient-perceived self-image with regard to outcomes [31, 43].
Preoperative surgical planning can be carried out using numerous modeling software systems [44]. Many mathematical models for determining the degree of correction needed through osteotomies to achieve sagittal alignment have been proposed [11, 45, 46]; however, one should note that formulas alone often underestimate the amount of correction needed.
The role of the pelvis in standing alignment is now well established, and spinopelvic parameters will need to be identified, including pelvic incidence (PI) and lumbar lordosis (LL) . Pelvic incidence is a fixed parameter for any given patient. Generally speaking, the goal of surgery is to restore lumbar lordosis to within +/−9° of the patient’s pelvic incidence. Sacral slope (SS) and pelvic tilt (PT) are dynamic pelvic parameters that measure pelvic version that can change as a compensatory mechanism. Patients with spinal malalignment often compensate for lost lordosis with pelvic retroversion, hip extension, and knee flexion leading to the classic “crouched gait” [47]. Spinopelvic mismatch is an important driver in sagittal malalignment—pelvic retroversion becomes exhausted with increasing mismatch, at which point the compensation is transferred to the lower limbs with differential recruitment being affected by age [48].
In addition to gauging how much correction should be achieved, complication avoidance begins with preoperative planning. Multidisciplinary discussion involving the anesthesia team and neuromonitoring team should emphasize the importance of maintaining normal blood pressure throughout surgery to maintain adequate spinal cord perfusion and prevent blindness [49]. Patients benefit from arterial and central venous monitoring. The coagulation profile and normothermia should be monitored [50]. Neurophysiological monitoring with measurement of SSEPs and MEPs is often used for PCOs and routinely used for PSOs and VCRs. MEP monitoring consists of transcranial, spinal, neurogenic, and muscle MEPs to evaluate descending motor pathways; as such complexity exist in the pathway, there are variations in how various institutions monitor MEPs [51]. Obtaining good baseline neuromonitoring and being prepared to deal with any changes detected are of great importance [52]. Patients with preoperative myelopathy are difficult candidates for optimal neuromonitoring, but often require extensive osteotomies. Proper preoperative counseling of patients regarding the risks of this complex surgery is essential [53]. Despite patients undergoing spinal deformity surgery being well informed about potential risks, studies have shown that patients cannot recall most surgical risks discussed and recall declines over time [54].
Surgical Technique
General Principles
At the time of surgery, patients need to be appropriately padded and positioned on a radiolucent table that permits the abdomen to float freely to decrease epidural bleeding and allows gravity to assist pulling the lumbar spine back into lordosis. Placing additional chest pads can help to achieve further lordosis if the spine is flexible. It is recommended that the patient’s head be placed level or higher than the heart [55]. Preoperatively, the amount of correction that will occur from general anesthesia and prone positioning with the abdomen dependent can be estimated on supine preoperative imaging such as MRI or CT. Furthermore, proper positioning and operating room setup can aid in closure of the osteotomy. For instance, the patient may be positioned on a four-poster frame with supports under the thighs and hips extended to assist in maintaining or increasing lumbar lordosis. Additionally, some operating tables allow a break in the table for initial positioning and the break in the table can be reduced to help close the osteotomy when it is complete. The four-poster frame can be positioned with its lower end at the break in the operating table, and the table is flexed to facilitate patient positioning. The flex is reduced and table straightened after the osteotomy is completed to assist in closure of the posterior wedge. Thus, the surgeon needs to be aware that the osteotomy gap can be closed while the operating table is brought from a flexed to a straight position. The level of the osteotomy should be aligned with the break in the operating table .
General Osteotomy Techniques
As previously stated, there are many different types of spinal osteotomies, but three general categories exist and more detailed techniques can be found below for each one. However, there are some generic steps that all osteotomies share, and we will review the general sequence of procedure here. It will be a surgeon’s discretion as to whether or not to perform preoperative halo-gravity traction. Firstly, meticulous exposure is required including areas for grafting, decompression, and instrumentation. Secondly, insertion of pedicle screw at predetermined levels is completed. Decompression (laminectomies) can then be performed at indicated levels including the level of the osteotomy and adjacent levels. Any available bone graft is removed and saved for later use as fusion material. Care should be taken not to tear the dura. A temporary rod may be inserted on one side capturing three levels above and below the planned resection site to maintain alignment. Next, the planned osteotomy is carried out with further details provided below. It is important to avoid injury to the segmental artery and vein that lie just lateral to the vertebral body. Lastly, after closure of the osteotomy and hardware placement, bone grafting is completed to remaining facet joints and transverse processes.
Posterior Column Osteotomy
PCO includes both SPO and Ponte techniques . Furthermore, PCOs include Grade 1 or 2 osteotomies according to the comprehensive anatomical spinal osteotomy classification [7]. The inferior aspect of the spinous process is removed followed by removal of the interspinous ligament using a standard rongeur or osteotome . Next the ligamentum flavum (LF) is removed with a Kerrison rongeur ; it is important to highlight that the LF arises from the lower half of the anterior surface of the cephalad lamina and attaches to the posterior surface and upper margin of the caudal lamina.
The surgeon must be vigilant not to penetrate deeply against the dura or tear the dura. The bilateral facet joints are removed either with a Kerrison rongeur , high-speed burr, or combination. One may choose to remove the LF intact during resection of bony elements to aid a barrier and protect the dura.
Partial facetectomy , complete facetectomy , or asymmetric facetectomy may be performed. For partial facetectomy, resection of the inferior facet and joint capsule at a given spinal level is done versus for a complete facet joint resection where both superior and inferior facets at a given spinal level are resected. This results in a V-shaped gutter with the width of the gutter typically between 10 and 15 mm.
Correction is performed gradually over multiple segments at the same time by compression of the pedicle screws closing the gap in the posterior elements. It is important to ensure that wider cranial and caudal laminectomies are performed so as not to trap or compress the thecal sac during osteotomy compression. This is done so as to redistribute corrective forces over a large area of the spinal column. Rods are set followed by decortication before wound closure. A cross table radiograph should be taken prior to closure .
Pedicle Subtraction Osteotomy
PSOs can be customized to patient-specific pathology depending on the amount of correction needed. The surgeon may resect bilateral pedicles and partial vertebral body; bilateral pedicles, partial vertebral body, and cephalad disc; or bilateral pedicles and asymmetric wedge of vertebral body. These osteotomies would include Grades 3 and 4 according to Schwab classification [7].
PCOs can be performed at the upper and lower level of the planned PSO vertebra. A wide laminectomy is performed from mid-pars region of the vertebra cephalad to the PSO vertebra distal to the lower-pars level of the PSO vertebra. The laminectomy should be in excess of the posterior element closure to minimize dural impingement. Furthermore, if there is extensive dural scarring from prior surgery, this will also need to be resected so that the plane between dura and scar is identified and mobilized cranially and caudally until normal dura is identified; otherwise, this can lead to compression upon closure.
The goal is to isolate and surround both pedicles so that they may be resected down to the base of the vertebral body. Of note, the surgeon must be careful to protect the exiting nerve roots that lie just against the medial and inferior aspect of the pedicle. The vertebral body is then decancellated of the cancellous bone to thin out the vertebral body and provide collapse and wedging of that segment. The surgeon needs to maintain the anterior vertebral body wall to act as the pivot point during closure of the osteotomy as well as maintain a protective barrier between the surgical field and viscera/major blood vessels. This will provide significant bone graft in addition to any graft harvested from prior PCOs. It is important to save all bone to be used later as fusion material. Additionally, if performing a traditional PSO, the vascularity of the remaining bone segment should be considered and preserved. Thus, if not removing the cranial disc, we recommend resection of the pedicle with the cranial cut just inside the pedicle itself.
Both lateral portions of the PSO vertebral body are exposed subperiosteally with Penfield 1 and Kittner dissectors, and a wedge of the lateral vertebral body is removed from superficial to deep. The subperiosteal dissection is of high importance to help protect and prevent injury to the segmental artery and vein that lie just lateral to the vertebral body. The lateral vertebral body cuts are made with straight osteotomes in a precise wedge based upon the desired closure so that the pivot point is the apex is the anterior vertebral wall. Of note, special retractor blades are available that allow access to the lateral wall and protect the segmental vessels. The cancellous bone is removed with a combination of curettes and rongeurs. Using angled curettes, the cancellous bone in the vertebra is pushed anteriorly to further create a cavity. Osteotomy contouring can be tailored using high-speed drill.
The final step involves dissecting the posterior vertebral body wall away from the ventral dural surface. An impaction technique is used with curettes or specialized impactors to push the posterior wall into the vertebral body, thus freeing up the entire ventral dural surface. If extensive anterior resection or thinning of the anterior cortex is performed, temporary rod stabilization is required to prevent translation. It is important not to place excessive stretch or tension on the dura during this portion of the procedure. PSO closure is performed by gentle compression across temporary rods. If excessive compression is required, the resection is likely inadequate. Temporary rods are then replaced with permanent rods that cover all instrumented segments: segmental pedicle screws at all predetermined levels at least three levels above and below the osteotomy site.
Vertebral Column Resection
VCR would include anatomic classification Grades 5 and 6 [7]. The extent of resection may include a complete vertebra with adjacent discs or multiple vertebrae and discs. Posterior alone or a combined anterior-posterior approach may be utilized. Please see the general steps for osteotomy above; we will begin this discussion as if exposure has been completed and pedicle screws have been placed.
PCOs are performed above and below the planned VCR level, and the posterior exposure is similar to the technique described for a PSO except that the laminectomy is done for the entire lamina of the VCR vertebrae and cephalad to the level of pars of the cranial lamina. Typically, the entire lamina of the level to be resected and the lamina cephalad to the pedicles above and caudad to the pedicles below are removed. Normally, for a one-level resection procedure, a posterior column laminectomy will result in a 5–6 cm exposure of the dura and neural elements. It is important not to minimize the posterior column exposure to gain thorough access to the spinal cord and/or cauda equina circumferentially, to aid in the resection procedure and also for visualizing any dural impingement during the correction.
In the thoracic spine , 5–6 cm of the medial rib associated with the level to be resected may be removed. Subperiosteal dissection of the medial aspect of the rib is performed. It is cut approximately 5–6 cm lateral to the vertebral attachment, and then as much of the rib as possible is removed down to the head anteriorly and is kept intact for later placement on top of the laminectomy defect. This is performed prior to the laminectomy to avoid canal intrusion if needed.
Pedicle screws have been placed at the predetermined levels. Prior to removing the anterior body, a temporary, stabilizing rod should be placed and attached to at least two or three pedicle screws both above and below the resection area. Classically, a unilateral rod is used; however, in severe angular kyphotic or kyphoscoliotic deformities, bilateral rods are recommended to prevent spinal subluxation. In the thoracic spine , the surgeon may elect to sacrifice one or both of the exiting nerve roots to provide increased exposure; however, this is generally not done in the lumbar spine, as nerve root function is critical to motor function of the lower extremities. Resection of the thoracic roots should be done medial to the dorsal root ganglia to reduce the chance of chronic pain. Sacrificing L1 or L2 in isolation will produce weakness, but over time many patients are able to compensate for the loss quite well. Nevertheless, sacrifice of these roots is not recommended. Loss of nerve root function below L2 will generally lead to a significant deficit.
The lateral vertebral body walls are subperiosteally dissected using protective instruments against the anterior and lateral margins to safely protect adjacent viscera and vasculature from harm. The lateral vertebral body walls are removed to allow entrance into the remainder of the vertebral body and to facilitate removal of all cancellous bone from endplate to endplate of the adjacent discs above and below. In primary procedures, super-periosteal dissection around the lateral aspect of the pedicles and vertebral body is performed using Penfield elevators . The soft tissues and the anterior vasculature are protected with either malleable retractors or special lateral wall vertebral body elevators. In revision cases, a subperiosteal dissection will be required due to previous scarring with a similar approach to gain access circumferentially around the vertebrae to be resected. In both circumstances, the segmental vessels are kept lateral in a soft tissue cuff and should not be violated if possible; otherwise, they may require ligation.
During resection of the pedicles, the surgeon must not only be careful of the exiting nerve roots but also of the spinal cord/dura when removing the concave pedicle as any coronal malalignment can allow this to rest against the pedicle. Careful dural protection with minimal retraction is the goal, and often using a high-speed burr to remove bone in high-risk areas is advised. For a scoliosis or kyphoscoliosis deformity , resecting the apical concave pedicle can be quite challenging since it is very cortical, and in a pure scoliosis deformity, the entire spinal cord/dural sac is resting on the medial concave pedicle which does not have any ventral vertebral body associated with it since the body is swung lateral and dorsal in its rotated position on the convexity. In this regard, using a small, high-speed burr is helpful to carefully burr away the cortical bone along this concave region.
The vertebral body is then decancellated of the cancellous bone in order to thin out the vertebra. Thus, in scoliosis and kyphoscoliosis deformities , the majority of the vertebral body will be removed from the convexity of the deformity since that is where the vertebral body is located. We prefer to perform the concave resection of the pedicle prior to the convex removal so there is no bleeding into this dependent concave region. This also allows the concave spinal cord to drift somewhat more medial and remove tension prior to going to the convexity for completion of the corpectomy . Again, it is important to save as much bone as possible to use in fusion later. Also, preservation of the cortices allows for temporary packing and tamponade of excess bleeding.
Both the anterior and posterior vertebral walls have been left intact thus far. The discs cephalad and caudad to the VCR are then removed using curettes. It is important not to violate the endplates of the superior and infero-adjacent regions as placement of a structural intracorporeal cage may be required. The last part of the vertebral resection is the posterior vertebral body wall. It is carefully dissected from the ventral dural surface and impacted into the vertebral body. Here it will be essential to control epidural bleeding with the judicious use of bipolar cauterization, topical hemostatic agents, and cottonoids. The dural sac must be circumferentially freed and exposed and then separated from the epidural venous complex as well as the posterior longitudinal ligament (PLL) . The entire body is removed except for the anterior shell, as we like to keep a thin rim of bone intact on the anterior longitudinal ligament (ALL) for fusion purposes. However, if this bone is cortical, then it must be thinned to allow easy closure of the resection area. It is important not to place excessive stretch or tension on the dura during this step of the procedure. It is imperative that the ventral spinal cord is completely free of any bony prominences to avoid impingement during closure. This is especially true at the disc levels, especially above but also below, as there tends to be osteophytic lipping in that region which can cause ventral compression if not removed.
The deformity is then ready for correction by the temporary instrumentation always beginning with spinal shortening by convex rod compression to avoid excessive stretch on the spinal cord. This is performed either with individual pedicle screws in primary cases where a good bony grip of the vertebrae is found or in a construct-to-construct closure mechanism utilizing dominoes at the apex of the resected area. In this method, closing from a construct rod above to a construct rod below to distribute the forces of correction over several levels is performed. It is imperative to compress slowly as subluxation and/or dural impingement can occur along the way. In any deformity that has a degree of kyphosis, we place an anteriorly based structural cage to prevent over-shortening of the deformity, and it also acts as a hinge to provide further kyphosis correction. Typically, the spinal column will be shortened by 1 to 1.5 cm, an appropriate height and length cage will be inserted, and then further closure onto the cage to make it snug and fixed will be performed as a final correction maneuver. It is important to have the anesthesia team elevate the mean arterial pressure for cord perfusion and frequently communicate with the neuromonitoring team during this step.
Once closure has been fully performed, a permanent contralateral rod is placed with appropriate correction maneuvers performed. Then the temporary closing rod is removed and a permanent, final rod is placed on the contralateral side as well. Appropriate compression and distraction forces, in situ contouring, and other correction techniques may be performed always being mindful of any resultant effect on the resected area with respect to subluxation or dural impingement. Next, adequate alignment is confirmed by intraoperative radiographs. Decortication and bone grafting follow with copious amounts of local graft obtained from the resection procedure. The laminectomy defect is covered with the previously harvested ribs for the costotransversectomy approach . These ribs are split in half longitudinally with the cancellous surface placed along the entire laminectomy defect from the lamina above to the lamina below. This creates a rib “bridge” of bone to protect the dura, as well as to provide a posterior onlay fusion. The rib is held in place with sutures or a cross-link if there is room and no prominence. To confirm the absence of impingement, final implant security is documented as well as a final circumferential check of the exposed dura.
Illustrative Case (Fig. 22.4a–h)
History
A 12-year-old young male presented with a visible dorsal prominence at the thoracolumbar junction with mild pain. His parents state that this “bump” had increased in size in the previous 2 years.
Physical Examination
On inspection, a visible dorsal prominence was seen at the thoracolumbar junction. No tenderness. Patient had full motor strength in all lower extremity muscle groups, with normal sensation. Hyperreflexia was evident with patellar tendon reflex testing with 3–4 beats of clonus evident. Babinski reflex testing was equivocal.
Radiographic Imaging
Standing AP (4a) and lateral (4b) 36-inch scoliosis x-rays demonstrate L1 dorsal hemivertebra with mild kyphosis. CT scan with sagittal reconstruction (4c) and MRI (4d) demonstrate significant encroachment into the spinal canal with stenosis and spinal cord compression.
Treatment
He underwent a vertebral column resection (VCR) with posterior resection of the hemivertebra (4e). A structural cage was placed following completion of the L1 vertebrectomy (4f), prior to corrective maneuvers through the instrumentation.
Outcome
Standing postoperative AP (4g) and lateral (4h) 36-inch scoliosis x-rays demonstrate L1 cage in place and posterior instrumented T11–L3 fusion. His thoracolumbar alignment has returned to neutral. At 2-year follow-up, he has maintained correction of deformity and has normal neurologic function.
Technical Pearls
General Principles
-
A bear hugger placed underneath the operating table covering the free abdomen aids in maintaining normothermia. Preoperatively elevating room temperatures to excess levels while the patient is exposed aids with this as well.
-
Placing the head 10° above the heart helps minimize the risk of visual complications [56].
-
Special attention should always be applied to the intraoperative SSEP and MEPS at the time of osteotomy closure.
-
At the time of closure, the surgeon should make sure that blood pressure and hematocrit are optimized.
-
Patients with a mobile anterior column are often able to achieve correction of deformity by proper positioning alone .
Posterior Column Osteotomy
-
Compression during closure of SPOs can lead to narrowing of the neural foramina which necessities a preceding wide facetectomy to prevent nerve root impingement. It is advised to palpate the foramina and nerve roots of levels involved prior to closure.
-
Patients with anterior column fusion are unlikely to gain significant correction with multiple SPOs , and therefore a PSO may be a better option.
Pedicle Subtraction Osteotomy/Vertebral Column Resection
-
Most ideal in lumbar spine (L3 or L4) or in an ankylosed spine .
-
Avoid leaving big open disc spaces (consider extended PSO, TLIF/PLIF below PSO, anterior fusion).
-
Wide decompression of foramen and early identification of nerve roots.
-
Leave anterior cortical wall intact to prevent translocation.
-
Place temporary rods prior to removal of lateral and posterior cortical walls.
-
Wide central canal decompression to accommodate dural buckling with resection of any scarred dura.
-
A pedicle pilot hole created at the level of the PSO is useful to maintain orientation during bony removal.
-
By performing the wider portion of the osteotomy on the convex side of the curve, coronal correction can be obtained at the same time as sagittal correction.
Complications and Strategies for Avoidance
PSO and VCR are technically more demanding and associated with longer operative times, greater blood loss, and higher risk of neurological complications than PCOs [57]. Complications related to the surgery include pseudarthrosis, proximal junctional kyphosis, instrumentation failure, adjacent spinal stenosis/adjacent segment disease, and infection. Postoperative medical complications include deep vein thrombosis, pulmonary embolus, small bowel ileus or obstruction, blindness, myocardial infraction, or stroke [58]. Table 22.3 reviews potential complications along with avoidance and management strategies.
Durotomies are sometimes unavoidable, especially in revision surgery. Emphasis should be placed on repair of the cerebrospinal fluid leak with direct repair or sealants, as it is important to prevent pseudarthrosis.
Neurological complications can be minimized with good intraoperative neuromonitoring and adequate bony resection; however, radiculopathy may be noted postoperatively due to compression of nerve roots as they exit the foramina; thus, care must be taken to perform a wide facetectomy and palpate the nerve roots after osteotomy closure.
Achievement of “ideal global sagittal realignment” has been shown to be protective against the development of reoperation and proximal junctional kyphosis [59]. Patients of concern may be evaluated with postoperative thin-cut CT scans to assess osteotomy closure and accuracy of implant placement. For all patients, standing AP and lateral 14 × 36 inch scoliosis radiographs are obtained before hospital discharge and at follow-up appointments, typically every 3 to 6 months. The patient should stand in a natural position without knee flexion or hip hyperextension. Correction of the osteotomy should be measured using preoperative and postoperative Cobb angles on lateral radiographs across the superior and inferior endplates of the vertebrae at which the osteotomies were performed. Global sagittal balance should be evaluated using a C7 plumb line and noting its relationship to the posterior superior corner of the sacrum.
Conclusion
The surgical treatment of spinal deformity is challenging. Traditionally, a circumferential approach with anterior releases via discectomies, followed by posterior instrumentation and fusion, has been the standard of care. However, the evolution of posterior approaches and osteotomies has allowed the modern era of spinal deformity surgery to promote posterior-only procedures. Currently, six anatomically defined osteotomies are accepted which fall into three general categories: (1) posterior column resection, (2) pedicle subtraction osteotomy, and (3) vertebral column resection. When considering an osteotomy for deformity correction, it is of great importance to match the correct osteotomy required by the malalignment. Thus, patient selection, preoperative planning, and decision-making are key to success. Restoration of satisfactory sagittal global alignment with thresholds of pelvic tilt <25°, sagittal vertical axis < 50 mm, and harmony between pelvic incidence and lumbar lordosis correlates with health-related quality-of-life scores. Furthermore, the surgeon needs to be aware of medical comorbidities and general health optimization prior to any surgery.
References
Cheng JS. The epidemiology of adult spinal deformity and the aging population. In: Wang YM, Lu Y, Anderson GD, Mummaneni VP, editors. Minimally invasive spinal deformity surgery: an evolution of modern techniques. Vienna: Springer Vienna; 2010.
Glassman SD, Berven S, Bridwell K, et al. Correlation of radiographic parameters and clinical symptoms in adult scoliosis. Spine (Phila Pa 1976). 2005;30(6):682–8.
O’Shaughnessy BA, Ondra SL. Measuring, preserving, and restoring sagittal spinal balance. Neurosurg Clin N Am. 2007;18(2):347–56.
Schwab F, Lafage V, Boyce R, Skalli W, Farcy JP. Gravity line analysis in adult volunteers: age-related correlation with spinal parameters, pelvic parameters, and foot position. Spine. 2006;31(25):E959–67.
Umehara S, Zindrick MR, Patwardhan AG, et al. The biomechanical effect of postoperative Hypolordosis in instrumented lumbar fusion on instrumented and adjacent spinal segments. Spine. 2000;25(13):1617–24.
Aebi M. The adult scoliosis. Eur Spine J. 2005;14(10):925–48.
Schwab F, Blondel B, Chay E, et al. The comprehensive anatomical spinal osteotomy classification. Neurosurgery. 2013;74(1):112–20.
Smith-Petersen MN, Larson CB, Aufranc OE. Osteotomy of the spine for correction of flexion deformity in rheumatoid arthritis. Clin Orthop Relat Res. 1969;66:6–9.
Cho KJ, Lenke LG, Berra A, et al. Comparison of Smith-Petersen versus pedicle subtraction osteotomy for the correction of fixed sagittal imbalance. Spine. 2005;30(18):2030–7.
Hehne HJ, Zielke K, Bohm H. Polysegmental lumbar osteotomies and transpedicled fixation for correction of long-curved kyphotic deformities in ankylosing spondylitis. Clin Orthop Relat Res. 1990a;258:49–55.
Ondra SL, Marzouk S, Koski T, et al. Mathematical calculation of pedicle subtraction osteotomy size to allow precision correction of fixed sagittal deformity. Spine. 2006;31(25):E973–9.
Geck MJ, Macagno A, Ponte A, Shufflebarger HL. The Ponte procedure: posterior only treatment of Scheuermann’s kyphosis using segmental posterior shortening and pedicle screw instrumentation. J Spinal Disord Tech. 2007;20(8):586–93.
Thomasen E. Vertebral osteotomy for correction of kyphosis in ankylosing spondylitis. Clin Orthop Relat Res. 1985;194:142–52.
Wang MY, Berven SH. Lumbar pedicle subtraction osteotomy. Neurosurgery. 2007;60(2 Suppl 1):ONS140–6.
Bridwell KH, Lewis SJ, Edwards C, et al. Complications and outcomes of pedicle subtraction osteotomies for fixed sagittal imbalance. Spine. 2003;28(18):2093–101.
Vauzelle C, Stagnara P, Jouvinroux P. Functional monitoring of spinal cord activity during spinal surgery. Clin Orthop Relat Res. 1973;93:173–8.
Nash CL, Loring RA, Schatzinger LA, et al. Spinal cord monitoring during operative treatment of the spine. Clin Orthop Relat Res. 1977;126:100–5.
Tamaki T, Kubota S. History of the development of intraoperative spinal cord monitoring. Eur Spine J. 2007;16(2):S140–6.
Gum JL, Buchowski JM, Lenke L, et al. Utilization trends of pedicle subtraction osteotomies compared to posterior spinal fusion for deformity: a national database analysis between 2008–2011. Scoliosis. 2016: In Press.
Sponseller PD, Jain A, Lenke LG, et al. Vertebral column resection in children with neuromuscular spine deformity. Spine (Phila Pa 1976). 2012;37(11):E655–61.
Kelly MP, Lenke LG, Shaffrey CI, et al. Evaluation of complications and neurological deficits with three column spine reconstructions for complex spinal deformity: a retrospective Scoli-risk 1 study. Neurosurg Focus. 2014;36(5):E17.
Lenke LG, Fehlings MG, Shaffrey CI, et al. Neurologic outcomes of complex adult spinal deformity surgery: results of the prospective, Multicenter Scoli-RISK-1 study. Spine. 2016;41(3):204–12.
MacLennan A. Scoliosis. Br Med J. 1922;2:865–6.
Bradford DS. Vertebral column resection for the treatment of rigid coronal decompensation. Spine. 1997;22(1):1590–9.
Dick J, Boachie-Adjei O, Wilson M. One-stage versus two-stage anterior and posterior spinal reconstruction in adults. Comparison of outcomes including nutritional status, complication rates, hospital costs, and other factors. Spine. 1992;17(Suppl):S310–6.
Suk SI, Chung ER, Kim JH, Kim SS, Lee JS, Choi WK. Posterior vertebral column resection for severe rigid scoliosis. Spine. 2005;30:1682–7.
Voyadzis JM, Gala VC, O’Toole JE, Eichholz KM, Fessler RG. Minimally invasive posterior osteotomies. Neurosurgery. 2008;63(3 Suppl):204–10.
Glassman SD, Schwab FJ, Bridwell KH, et al. The selection of operative versus nonoperative treatment in patients with adult scoliosis. Spine. 2007;32:93–7.
Lafage R, Schwab F, Challier V, et al. International spine study group. Defining Spino-pelvic alignment thresholds: should operative goals in adult spinal deformity surgery account for age? Spine (Phila Pa 1976). 2016;41(1):62–8.
Gill JB, Levin A, Burd T, et al. Corrective osteotomies in spine surgery. J Bone Joint Surg Am. 2008;90:2509–20.
Gum JL, Bridwell KH, Lenke LG, Bumpass DB, Sugrue PA, Karikari IO, Carreon LY. SRS22R appearance domain correlates most with patient satisfaction after adult deformity surgery to the sacrum at 5-year follow-up. Spine (Phila Pa 1976). 2015;40(16):1297–302.
Bridwell K. Decision-making regarding Smith-Petersen vs. pedicle subtraction osteotomy vs. vertebral column resection for spinal deformity. Spine. 2006;31(19 Suppl):S171–8.
Lafage V, Schwab F, Vira S, et al. Does vertebral level of pedicle subtraction osteotomy correlate with degree of spinopelvic parameter correction? J Neurosurg Spine. 2011;14(2):184–91.
Kim YH, Bridwell KH, Lenke LG, et al. Results of lumbar pedicle subtraction osteotomies for fixed sagittal imbalance: a minimum 5-year follow-up study. Spine. 2007;32(20):2189–97.
Gum, JL, Lenke LG, Bumpass D, et al. Does planned staging for posterior-only vertebral column resections in spinal deformity surgery increase perioperative complications? Spine Deform. 2016; 4(2):131–137.
Brown CW, Orme TJ, Richardson HD. The rate of pseudoarthrosis (surgical nonunion) in patients who are smokers and patients who are nonsmokers: a comparison study. Spine. 1986;11:942–3.
West J. Respiratory physiology: the essentials. 6th ed. Philadelphia: Lippincott Williams & Williams; 2000. p. 122.
Bertorini TE. Perisurgical management of patients with neuromuscular disorders. Neurol Clin. 2004;22:293–313.
Shin JI, Phan K, Kathari P, et al. Impact of glycemic control on morbidity and mortality in adult idiopathic scoliosis patients undergoing spinal fusion. Clin Spine Surg. 2016: Oct 19. [Epub ahead of print].
Pickhardt PJ, Pooler BD, Lauder T, et al. Opportunistic screening for osteoporosis using abdominal computed tomography scans obtained for other indications. Ann Intern Med. 2013;158(8):588–95.
Snow R, Granata J, Ruhil AV, et al. Associations between preoperative physical therapy and post-acute care utilization patterns and cost in total joint replacement. J Bone Joint Surg Am. 2014;96(12):e165.
Jevsevar DS, Karlin LI. The relationship between preoperative nutritional status and complication after an operation for scoliosis in patients who have cerebral palsy. J Bone Joint Surg Am. 1993;75:880–994.
Tones MJ, Moss ND. The impact of patient self assessment of deformity on HRQL in adults with scoliosis. Scoliosis. 2007;2(1):1–9.
Aurouer N, Obeid I, Gille O, et al. Computerized preoperative planning for correction of sagittal deformity of the spine. Surg Radiol Anat. 2009;31(10):781–92.
Rose PS, Bridwell KH, Lenke LG, et al. Role of pelvic incidence, thoracic kyphosis, and patient factors on sagittal plane correction following pedicle subtraction osteotomy. Spine (Phila Pa 1976). 2009;34(8):785–91.
Akbar M, et al. Use of Surgimap spine in sagittal plane analysis, osteotomy planning, and correction calculation. Neurosurg Clin N Am. 2013;24(2):163–72.
Lafage V, Schwab F, Patel A, et al. Pelvic tilt and truncal inclination: two key radiographic parameters in the setting of adults with spinal deformity. Spine (Phila Pa 1976). 2009;34(17):E599–606.
Diebo BG, Ferrero E, Lafage R, et al. Recruitment of compensatory mechanisms in sagittal spinal malalignment is age and regional deformity dependent: a full-standing axis analysis of key radiographical parameters. Spine (Phila Pa 1976). 2015;40(9):642–9.
Turner JD, Eastlack RK, Mirzadeh Z, et al. Fluctuations in spinal cord perfusion during adult spinal deformity correction identify neurologic changes: proof of concept. World Neurosurg. 2016;85:365.e361–6.
Hart SR, Bordes B, Hart J, et al. Unintended perioperative hypothermia. Ochsner J. 2011;11(3):259–70.
Park J-H, Hyun S-J. Intraoperative neurophysiological monitoring in spinal surgery. World J Clin Cases. 2015;3(9):765–73.
Vitale MG, Skaggs DL, et al. Best practices in intraoperative Neuromonitoring in spine deformity surgery: development of an intraoperative checklist to optimize response. Spine Deform. 2014;2(5):333–9.
Biscevic M, Biscevic S, Ljuca F, Smrke BU, et al. Motor evoked potentials in 43 high risk spine deformities. Med Arch. 2014;68(5):345–9.
Saigal R, Clark AJ, Scheer JK, et al. Adult spinal deformity patients recall fewer than 50% of the risks discussed in the informed consent process Preoperatively and the recall rate worsens significantly in the postoperative period. Spine (Phila Pa 1976). 2015;40(14):1079–85.
Apfelbaum JL, Roth S, Connis RT, Domino KB, et al. Practice advisory for perioperative visual loss associated with spine surgery. Anesthesiology. 2012;116(2):274–85.
Emery SE, Daffner SD, France JC, et al. Effect of head position on intraocular pressure during lumbar spine fusion: a randomized, prospective study. J Bone Joint Surg Am. 2015;97(22):1817–23.
Daubs MD, Lenke LG, Cheh G, et al. Adult spinal deformity surgery: complications and outcomes in patients over age 60. Spine. 2007;32(20):2238–44.
Good CR, Auerbach JD, O’Leary PT, et al. Adult spinal deformity. Curr Rev Musculoskelet Med. 2011;4:159–67.
Maruo K, Ha Y, Inoue S, et al. Predictive factors for proximal junctional kyphosis in long fusions to the sacrum in adult spinal deformity. Spine. 2013;38(23):E1469–76.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this chapter
Cite this chapter
Nazar, R., Gum, J., Dimar, J., Djurasovic, M. (2017). Lumbar Osteotomy Techniques. In: Holly, L., Anderson, P. (eds) Essentials of Spinal Stabilization . Springer, Cham. https://doi.org/10.1007/978-3-319-59713-3_22
Download citation
DOI: https://doi.org/10.1007/978-3-319-59713-3_22
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-59712-6
Online ISBN: 978-3-319-59713-3
eBook Packages: MedicineMedicine (R0)