Abstract
Breast cancer is a significant international public health problem and is the leading cause of cancer death in women worldwide [1]. In high-income countries, women under the age of 45 are more likely to die of breast cancer than of any other disease or injury [2]. Women with hereditary breast and ovarian cancer syndromes, including carriers of deleterious mutations in the BRCA1 or 2 genes, not only are at approximately fivefold increased risk of breast cancer but also develop malignancy approximately 10 years earlier than those with non-hereditary disease, often during their reproductive years [3,4,5]. In such patients, often referred to as BRCA-positive/+ or carriers, the potential for early onset disease combined with the potential adverse impact on fertility of cancer prevention strategies and treatment if disease develops necessitates proactive, careful counseling about reproductive planning. This should be considered for both previvors (patients who are BRCA + but have not developed disease) and BRCA + survivors (patients who have developed disease in the setting of a hereditary predisposition). While male BRCA carriers are at increased risk of developing malignancies, most present later in life, not during reproductive years, and there are no standard risk-reducing strategies employed that are associated with infertility for male previvors. Nevertheless, potential concerns regarding reproduction should be addressed for young male patients as well. In this manuscript, we review the unique considerations surrounding reproduction, fertility, and fertility preservation for carriers of BRCA gene mutations. We address the relevant fertility concerns for the previvor and survivor populations, including strategies for patients with a new cancer diagnosis as well as consideration of preimplantation genetic diagnosis (PGD), even in the absence of infertility, to avoid passing on a deleterious germ line mutation to progeny. Available options are discussed, including gamete (egg or sperm) and embryo cryopreservation, as well as the more controversial use of LHRH agonists for ovarian suppression to preserve fertility. We also highlight future directions such as ovarian tissue cryopreservation. The available data regarding the safety of current assisted reproductive technologies (ART) for BRCA carriers will be reviewed. Finally, we describe some of the salient ethical concerns in this area.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Breast cancer is a significant international public health problem and is the leading cause of cancer death in women worldwide [1]. In high-income countries, women under the age of 45 are more likely to die of breast cancer than of any other disease or injury [2]. Women with hereditary breast and ovarian cancer syndromes, including carriers of deleterious mutations in the BRCA1 or 2 genes, are not only at an approximately fivefold increased risk of developing breast cancer, but also develop malignancy approximately 10 years earlier than those with non-hereditary disease, often during their reproductive years [3,4,5]. In such patients, often referred to as BRCA-positive/+ or carriers , the potential for early onset disease combined with the potential adverse impact on fertility of cancer prevention strategies and treatment if disease develops necessitates proactive, careful counseling about reproductive planning. This should be considered for both previvors (patients who are BRCA+ but have not developed disease) and BRCA+ survivors (patients who have developed disease in the setting of a hereditary predisposition). While male BRCA carriers are at increased risk of developing malignancies, most present later in life, not during reproductive years, and there are not standard risk-reducing strategies employed that are associated with infertility for male previvors. Nevertheless, potential concerns regarding reproduction should be addressed for young male patients as well.
In this manuscript, we review the unique considerations surrounding reproduction, fertility, and fertility preservation for carriers of BRCA gene mutations. We address the relevant fertility concerns for the previvor and survivor populations, including strategies for patients with a new cancer diagnosis as well as consideration of preimplantation genetic diagnosis (PGD) , even in the absence of infertility, to avoid passing on a deleterious germ line mutation to progeny. Available options are discussed, including gamete (egg or sperm) and embryo cryopreservation, as well as the more controversial use of LHRH agonists for ovarian suppression to preserve fertility. We also highlight future directions such as ovarian tissue cryopreservation. The available data regarding the safety of current assisted reproductive technologies (ART) for BRCA carriers will be reviewed. Finally, we describe some of the salient ethical concerns in this area.
Whether BRCA carriers are previvors, newly diagnosed with cancer, or longer term survivors, reproductive goals may weigh heavily on their minds, particularly regarding how treatment may impact their fecundity. Fertility preservation discussions prior to initiating treatment, and preservation of the ability to have biological children, have been shown to increase quality of life and improve psychological outcomes for cancer patients [6, 7]. In particular, for young women with breast cancer , international guidelines recommend early referral to reproductive endocrinology and infertility specialists (REIs) to discuss reproductive goals [2, 8]. However, there are a number of potential barriers and concerns surrounding fertility preservation and subsequent pregnancy in BRCA carriers with or without a history of cancer including utility, efficacy, timing, and safety of any intervention [9]. BRCA carriers require special consideration as detailed below.
Reproductive Considerations for Previvors (BRCA Carriers Who Have not Developed Cancer)
In order to reduce the lifetime risk of cancer in previvors, it is recommended that patients consider prophylactic mastectomy and bilateral salpingo-oophorectomy, surgery that results in sterilization. Carriers of the BRCA1 mutation have a 15–45% lifetime risk of developing ovarian cancer and ≤85% risk of developing breast cancer. A BRCA2 mutation confers a lifetime risk of ovarian cancer of 10–20% and a breast cancer risk of 40% [3]. By undergoing prophylactic bilateral mastectomy, breast cancer risk and mortality can be reduced by 90–95% [10]. Bilateral salpingo-oophorectomy reduces the risk of ovarian cancer by approximately 85–90% and reduces the risk of breast cancer by 40–70% [11, 12]. Based on international guidelines, patients should undergo bilateral salpingo-oophorectomy once childbearing is completed, or by the age of 35–40, given the increased risk of ovarian cancer with age [2, 13].
Previvors may desire to complete childbearing prior to undergoing prophylactic surgery. These patients, in the absence of other fertility concerns, may be able to conceive naturally. The optimal timing of reproduction is a very personal decision. However, even in patients who are not infertile, IVF for the purposes of PGD is still a consideration for BRCA carriers.
Preimplantation Genetic Diagnosis
PGD is useful in hereditary disorders when intended parents wish to avoid passing a specific gene on to their offspring. BRCA genes demonstrate an autosomal dominant pattern of inheritance, conferring a 50% chance that a child will be a carrier. Following IVF, PGD allows parents to know in advance the carrier status of each embryo. By transferring only non-carrier embryos, intended parents can prevent the propagation of the BRCA gene in their family [14].
For PGD, the woman must undergo ovarian stimulation with subsequent oocyte harvesting, and sperm must be available for IVF. Once embryos are fertilized via IVF, they are allowed to develop in the embryology laboratory. At day five and/or six of development, the external cells of the blastocyst (trophectoderm cells, destined to become the placenta) can be biopsied and genetically tested for the presence of specific gene, such as BRCA1 or 2 mutations. PGD may be an attractive option for pre-surgical BRCA patients, who can later have a cryopreserved embryo thawed and transferred. The ethical implications of PGD for BRCA carriers, and the disposition of non-carrier and indeterminate embryos after PGD testing, are discussed later. For some women, particularly those needing urgent neoadjuvant chemotherapy , BRCA status may be unknown at the time of embryo banking. Additional consideration should be taken when discussing the timing of embryo banking, and the option of PGD, under these circumstances.
Preimplantation genetic screening can also provide information about other chromosomal abnormalities, such as aneuploidy , prior to the transfer or storage of embryos. This may help eliminate the need for invasive testing in the first trimester of pregnancy, such as chorionic villus sampling or amniocentesis, after which some women opt to terminate. If under time constraints, this consideration may be particularly relevant.
IVF with or without PGD and cryopreservation of embryos allows patients to plan for the future, aligning with the modern trend toward delaying childbearing until later in life [15]. Since prophylactic salpingo-oophorectomy is recommended by age 40, some patients may wish to undergo surgery with the plan to delay pregnancy and family building. For patients who do not wish to carry a pregnancy, or are of an age where becoming pregnant may be difficult or dangerous, the option of using a gestational carrier may also be considered.
Reproductive Considerations for BRCA Carriers with a Cancer Diagnosis, Survivors
Options for reproduction and family building may be different for carriers of the BRCA gene with a new diagnosis of cancer, when time constraints may be more pressing. Prior to initiating treatment, these patients should be counseled on the potential risks of therapy to fertility, and on the current options for fertility preservation, namely gamete or embryo cryopreservation [16]. Alternatively, ovarian suppression, with the use of luteinizing hormone-releasing hormone agonists during chemotherapy, may offer some ovarian protection, an option discussed in more detail below [17]. In patients with ER-positive disease in particular, there may be concern surrounding the safety of fertility preservation strategies with regard to disease outcomes given the associated maintenance or temporary elevation of reproductive hormones, and this should be considered on a case-by-case basis. In BRCA1-associated breast cancers, 10–24% are ER-positive, compared to 65–79% ER positivity in BRCA2-associated breast cancers [18]. Survivors of cancer who may have completed chemotherapy and/or radiation but still have their ovaries in situ may consider ART after treatment. However, patients may have subsequent diminished ovarian reserve, chemotherapy-induced amenorrhea, or premature menopause due to treatments received and may require fertility assistance [15]. Barton and colleagues compared female cancer survivors with all other patients undergoing IVF/ICSI and demonstrated that survivors were low responders and had poorer outcomes overall. Survivors had significantly fewer oocytes retrieved and embryos available for transfer. Pregnancy and live birth rates were lower among survivors as well with odds ratios of 0.30 (95% CI 0.13–0.68) and 0.27 (95% CI 0.10–0.69), respectively [19]. Patients should be counseled that following treatment with chemotherapy or radiation, ART may be challenging; some may ultimately need a donor egg in order to achieve pregnancy.
Female Fertility Preservation: Existing Options
The most established method of fertility preservation is embryo cryopreservation [16]. Following a protocol of controlled ovarian stimulation (COS) to promote the development of the greatest numbers of follicles, oocytes are harvested, fertilized, then the resultant embryos cryopreserved and stored until ready for use.
Oocyte cryopreservation is also now a standard option, which involves similar COS, oocyte retrieval followed by cryopreservation of mature oocytes in their unfertilized state. Fertilization, pregnancy, and live birth rates reported with thawed oocytes appear to be equivalent to fresh oocytes, making oocyte cryopreservation an accepted, non-experimental practice [20]. Specific data for breast cancer patients regarding success with cryopreserved oocytes versus embryos are not yet available, though it is presumed these are roughly equivalent. As of 2012, of the 387 US IVF clinics registered as Society for Assisted Reproductive Technology members, 200 (51.7%) offered oocyte cryopreservation [21].
For patients that are either single or not in a relationship with a potential co-parent, gamete cryopreservation may be a good option. Alternatively, embryo cryopreservation is appropriate if a couple decides they would like to parent a biological child in the future. A single female can also opt to freeze embryos using her oocytes and a donor sperm. However, in cases of divorce, courts may not necessarily grant ownership and control of the embryos to the cancer survivor. Therefore, it is important to inform women that oocyte cryopreservation, or cryopreservation of eggs fertilized with anonymous donor sperm, is the only way to guarantee that they will have complete control of embryos in the future. The option of embryo or gamete freezing allows for substantial flexibility on a case-by-case basis (Table 10.1).
Ovarian Suppression During Chemotherapy
Recently, regimens that suppress and thereby theoretically protect ovarian function during chemotherapy have emerged as potential options for reproductive age women with cancer. Chemotherapy can have a negative impact on ovarian reserve, and alkylating agents commonly used to treat breast cancer can be particularly gonadotoxic [22]. The extent of potential damage to ovarian reserve is related to the choice of chemotherapy regimen, dosage, and temporal exposure, as well as patient age [22].
For women who maintain their ovaries during therapy, luteinizing hormone-releasing hormone analogues (LHRHa) , when given concomitantly with chemotherapy, may offer some ovarian protection against such gonadal cytotoxicity [23]. Expert opinion and meta-analyses of available data indicate that LHRH agonists do seem to help preserve ovarian function during chemotherapy exposure [17]. In a recent randomized control trial of 281 women, patients who received LHRHa were significantly more likely to resume menses after treatment compared to the control group (73% vs. 64%), and the LHRHa patients reported more pregnancies compared to the control group (8 vs. 3, p < 0.05) [17]. In this trial, there was no difference in disease-free survival between the two groups [17, 23].
Importantly, two large randomized controlled trials, the Tamoxifen and Exemestane Trial (TEXT) and the Suppression of Ovarian Function Trial (SOFT) , evaluated potential benefits of ovarian suppression regimens during chemotherapy for premenopausal breast cancer with hormone-receptor-positive breast cancer. Combined analysis of these data demonstrates a reduced risk of breast cancer recurrence for women treated with ovarian suppression plus the aromatase inhibitor exemestane, compared to ovarian suppression plus tamoxifen [17, 24]. Thus, use of ovarian suppression is increasingly being used routinely for breast cancer treatment in the setting of early-stage hormone-receptor-positive breast cancer in premenopausal women. Further, there is no apparent harm with regard to disease outcome in this setting with the use of ovarian suppression through chemotherapy, whether for treatment or for fertility preservation. Nevertheless, the potential role for ovarian suppression for fertility preservation in women with early breast cancer remains controversial, whether they are mutation carriers or not. In treating BRCA carriers, this should be considered on a case-by-case basis.
Future Directions
Ovarian tissue cryopreservation is considered an experimental technique for fertility preservation. It involves surgical biopsy or stripping of the ovarian cortex, or removing the entire ovary, then cryopreserving the specimen for future use. The ovarian tissue can later be thawed and reimplanted in the patient once therapy is completed, either in or outside the pelvis [25]. As of January 2016, more than 60 live births have resulted from ovarian tissue cryopreservation, with all deliveries resulting from orthotopic (in the pelvis) tissue replacement [26]. A recent study from Israel of 20 patients, the majority of which had hematologic malignancies, reported 53% of patients successfully conceived following ovarian tissue transplantation. Sixteen pregnancies were achieved (six spontaneous and 10 following IVF), with 10 subsequent live births, and two ongoing pregnancies [26].
Ovarian tissue cryopreservation avoids exposing the ovaries to the toxic effects of chemotherapy and/or radiation. It also eliminates the need to delay treatment because the surgery can be done at any time in the cycle and does not require any ovarian stimulation. Similar to oocyte cryopreservation, ovarian tissue cryopreservation does not require a partner.
Ovarian tissue cryopreservation is performed with the intention to reimplant the tissue in the future. This may not be the safest option for BRCA carriers, given their increased risk of ovarian malignancy. It is theoretically possible that the ovarian tissue may be reimplanted for a brief time, stimulated to retrieve oocytes, and then removed soon thereafter, to minimize exposure to potentially pre-malignant or malignant cells. However, this remains experimental, without data related to outcomes in BRCA patients. In addition, it is likely contraindicated in patients with metastatic disease, as breast cancer may metastasize to ovaries. Only select centers are offering ovarian tissue cryopreservation, and it is not widely available [4, 25].
Female Fertility Preservation: Potential Risks and Challenges
BRCA carriers with a new diagnosis of cancer may have concerns that cryopreservation of oocytes or embryos may lead to a dangerous delay in treatment [27]. In order to maximize the yield of oocytes harvested for cryopreservation, most providers recommend controlled ovarian stimulation (COS) , a process that requires an average of two weeks [4]. In order to reduce delay in cancer treatment, some providers will begin COS as soon as possible, rather than waiting for the early follicular phase, as is traditional practice. This random-start protocol using gonadotropin antagonists has been shown to have similar outcomes compared to follicular phase-start protocols, with no difference in the number of total and mature oocytes retrieved, oocyte maturity rate, and fertilization rates [28]. However, data including live birth rates are scant. In an emergency situation, random-start protocols are most appropriate.
Most women, however, may be able to undergo at least one IVF cycle without significantly delaying the initiation of their therapy. In 2007, a study by Madrigano et al. highlighted the importance of early referral to an REI in order to avoid delays while still maximizing potential fertility preservation. For 23 patients with breast cancer, the mean time from fertility evaluation to egg retrieval was 33.3 (10–65) days [29]. On average, patients underwent ovarian stimulation for 11.5 (9–20) days prior to egg retrieval [29]. The average time from definitive surgery to initiation of chemotherapy was 46.8 days in the women who underwent fertility preservation [29]. Time from diagnosis to initiation of chemotherapy was not statistically different between women who opted for fertility preservation compared to those who did not (71 days vs. 67 days). For women undergoing egg retrieval, time from diagnosis to definitive surgery was longer by 15 days, but this was not statistically significant. Standard of care treatment for breast cancer was not delayed in any clinically significant way by undergoing fertility preservation treatment [29, 30].
A second concern exists regarding risks of exposure to the hormonal protocol used to induce ovarian stimulation. Typical regimens for stimulation protocols use high-dose gonadotropins that result in supraphysiologic systemic levels of estradiol , as much as 10–20 times normal [15, 31]. This allows for the recruitment of multiple follicles, maximizing the number of oocytes retrieved. Patients also receive GnRH agonists or antagonists to try to prevent premature luteinization and ovulation [31]. Exposure to such high levels of estradiol may be of particular concern for women that have estrogen-receptor-positive breast cancer, keeping in mind that 65–79% of breast cancers will be estrogen-receptor-positive in BRCA2 carriers, compared to 10–24% of breast cancers in BRCA1 carriers [18].
Alternative regimens, utilizing the selective estrogen-receptor modulator tamoxifen or the aromatase inhibitor letrozole during COS, have been well described and may help limit exposure to high levels of estradiol [4, 31, 32]. Both tamoxifen and letrozole can be used as ovulation induction agents, and the use of either agent is associated with improvement in IVF cycle outcomes [29, 33].
One study by Oktay et al. reported that the use of low-dose FSH with letrozole or tamoxifen results in improved embryo yield compared to the use of tamoxifen alone, but use of letrozole may be preferential as it produces lower levels of estradiol [33]. The same study indicated that tamoxifen alone may briefly result in increased levels of estradiol during stimulation. There are, however, no studies comparing live birth rates with different ovulation induction regimens in breast cancer patients. Again, this may be of particular relevance to patients with ER-positive breast cancers.
Importantly, limited data show that the use of letrozole or tamoxifen as part of the COS protocol does not appear to negatively impact breast cancer outcomes, or increase the risk of recurrence [31]. Data also show that fertility treatments in general do not increase risk of epithelial ovarian cancer for patients specifically with BRCA mutations [34].
A natural cycle is also a possibility, in which COS is not performed. The follicles produced by a woman in her natural cycle are aspirated, with as many eggs harvested as possible, though typically the yield is much lower than with ovarian stimulation and would be expected to result in much lower chances of future pregnancy [33]. This treatment has largely been abandoned by most large fertility preservation centers.
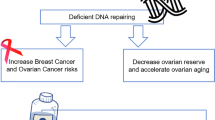
Ovarian Reserve and BRCA Carriers
Some data suggest that BRCA carriers may have inherent diminished ovarian reserve compared to non-carriers and may have fewer oocytes retrieved after COS [35]. There is evidence that BRCA1 carriers have poorer serum markers of ovarian reserve, specifically a fourfold greater chance of having anti-Mullerian hormone (AMH) <1 ng/mL compared with non-BRCA1 carriers [36]. However, having poorer ovarian reserve based on serum markers may not translate into meaningful clinical outcomes.
A recent study out of Israel reviewed IVF data for BRCA carriers and non-carriers, specifically evaluating response to COS. Carriers and non-carriers had comparable oocyte yield (13.75 vs. 14.75) and low response rates (8.06% vs. 6.45%) [37]. There were no differences in ovarian response, fertilization rates (70.6% vs. 59.66%), or resultant embryos (8.4 vs. 7.19) [37].
BRCA carriers and non-carriers appear to be at similar risk for chemotherapy-induced amenorrhea [38]. Though BRCA carriers generally experience menopause 1–2 years earlier than non-carriers, this does not appear to have any meaningful impact on fertility outcomes, such as age at first parity or need for fertility treatments [39]. Compared to non-BRCA breast cancer patients, BRCA carriers do not appear to be more susceptible to gonadotoxic side effects of chemotherapy and do not appear to have worse fertility outcomes.
Recent data reported by Sabatini et al. over a 17-year experience demonstrate that cancer patients in general have fertility outcomes that are equivalent to women without a history of cancer. The study reported no difference in outcomes for frozen embryo transfers between cancer patients and patients with tubal factor infertility. Both groups had equivalent number of oocytes retrieved and embryos frozen. Similarly, there were no differences between cumulative pregnancy rate per transfer for cancer patients (37%) compared to controls (43%), and cumulative live birth rate per transfer (30% vs. 32%, respectively) [40].
There has been concern regarding the safety of pregnancy for patients with a history of breast cancer, particularly with estrogen-receptor-positive cancers. Pregnancy, however, appears to be safe for patients who have undergone curative treatment. Regardless of receptor status, women who achieve pregnancy after therapy have no difference in survival or risk or recurrence compared to women who do not get pregnant, recognizing that data are limited to retrospective analyses or registry studies [41].
Male Fertility Preservation: Existing Options
Discussions regarding fertility preservation are relevant to male BRCA carriers as well. Although male carriers of BRCA1 have a lifetime breast cancer risk of less than 2%, they may be twice as likely to develop prostate cancer before age 65, for example [42].
Though most of the cancers seen in male BRCA patients present later in life, they can affect a man of reproductive age. If so, the patient should be given the option to bank sperm prior to initiating therapy [16]. Semen collection and freezing is the standard of care for men of reproductive age with a new diagnosis of cancer and can usually be arranged in a matter of days [8]. These patients should also be offered the opportunity to pursue PGD if they wish to eliminate the BRCA gene in their offspring (Table 10.2).
Socioeconomic, Cultural, and Ethical Considerations
It is an inherent right to parent and to have a family. The Universal Declaration of Human Rights , proclaimed by the United Nations General Assembly in 1948, states men and women have a right to found a family. BRCA carriers may require additional efforts to protect their reproductive rights, given the heritability of the mutation, and that standard treatment for these patients often involves procedures that affect their fertility.
In young women with breast cancer, concerns about fertility are associated with significant psychosocial stress [43]. BRCA carriers need early discussion regarding reproductive goals and early referral to appropriate providers, namely REI physicians, to review the available options [2, 8]. Unfortunately, consultation with an REI is not yet the standard of care, and access to such subspecialists may be limited. One study found that in women with localized breast cancer diagnosed at 40 years of age or younger, only 68% had discussed fertility options and only 10% underwent fertility preservation prior to initiating treatment [9]. A 2011 survey of over 1000 women diagnosed with cancer at ages 15–40 reported only 61% of women were counseled about fertility risks prior to initiating treatment, and only 4% pursued fertility preservation [44].
Though it does not require stimulation protocols or invasive procedures, referral rates for sperm banking can be low as well. In one recent study, 29% of male cancer patients received fertility counseling and only 11% attempted sperm banking [45].
In the USA alone, access varies tremendously based on location. The highest percentages of IVF clinics are located in northeastern and western states [46]. In areas with fewer hospitals and fewer subspecialty practices, it may not be possible to refer patients to an REI physician. Access to genetic testing to even confirm BRCA carrier status may be difficult as well though most insurance policies, including Medicare, will cover the cost of genetic screening in appropriate patients [13].
Interestingly, even among women who undergo fertility preservation prior to therapy, few seem to pursue attempts at pregnancy after treatment [30]. This may in part be due to patient and/or provider concerns about pregnancy safety. It should be reinforced that pregnancy does not appear to increase risk of recurrence or mortality [41].
Cultural differences may also limit patients’ access to care. In Italy, for example, embryo cryopreservation was forbidden in 2004 [47]. Federal law mandated that all created embryos were used for transfer and outlawed cryopreserving embryos for future use. Italy allows only gamete banking, but even this limitation can significantly impair options surrounding fertility preservation.
Socioeconomic and racial impacts on fertility options should not be underestimated either. Survey data suggest that women without bachelor’s degrees, for example, are less likely to be counseled on reproductive risks of cancer treatment, with an odds ratio of 0.7. The same study found trends toward disparities in access to reproductive services for women over 35, Latina and African American women, and parous women [44].
Financial barriers can also pose a significant problem for many patients. There is no insurance mandate to cover fertility treatments for patients with hereditary cancer syndromes, so for many patients, the cost of IVF cycles and the cost of preserving gametes or embryos are paid out-of-pocket. This can be prohibitively expensive. In 2010, the average cost for a female cancer patient to undergo fertility preservation with oocyte or embryo cryopreservation was $8655. It cost approximately $1495 (17%) more for embryo cryopreservation than oocyte cryopreservation [48]. More recent data indicate that in 2016, it costs between $12,000–15,000 for egg freezing and $15,000–$18,000 for embryo freezing. Storage fees average $900 per year [49]. One retrospective review found that breast cancer patients who were wealthier and older were more likely to pursue fertility preservation treatment [50].
However, some large fertility centers are able to offer discount services for patients with cancer in recognition that these patients do not have time to save for this expense. There are 15 states (Arkansas, California, Connecticut, Hawaii, Illinois, Louisiana, Maryland, Massachusetts, Montana, New Jersey, New York, Ohio, Rhode Island, Texas, and West Virginia) that offer coverage for some infertility diagnosis and treatment, but the extent of coverage varies on a state-by-state basis [51].
The opportunity for PGD , given the heritability of the BRCA genes, introduces unique ethical concerns that merit consideration as well. The option to undergo PGD is increasingly desired in patients with hereditary cancer syndromes. A meta-analysis of 13 studies found that, of the 370 respondents affected by a hereditary cancer syndrome, 28% felt their syndrome impacted family planning, 72% felt that PGD should be offered, and 43% would consider using PGD [52]. In a survey of 22 couples affected by hereditary breast and ovarian cancer, half chose to undergo PGD because they “believed it was their moral duty to protect their future child(ren) from suffering” [14]. For patients who have had cancer as a direct result of a BRCA mutation, PGD may be a particularly important option for their psychological well-being and family planning goals.
PGD poses additional potential ethical quandaries as it is not universally agreed upon that BRCA carrier status is an appropriate indication for PGD. There is no mandated insurance coverage for PGD, and coverage for this indication again varies widely state-by-state. Since BRCA carrier status predisposes to a potentially fatal adult-onset disease, many IVF centers will allow PGD. However, some may have concerns that it inappropriately eliminates potential offspring that have a significant chance of being healthy and disease-free [53].
Identifying carrier and non-carrier embryos, as well as those with indeterminate status through the use of PGD, has led to ethical debate regarding the fate of such embryos [53]. The potential outcomes of PGD should be explicitly discussed with patients prior to initiating testing. Patients opting for PGD should understand that the goal of PGD is to identify and transfer a non-carrier embryo. If this does not align with the patient’s goal, the patient should not elect for PGD.
Finally, emphasis should be placed on safeguarding the future of any gametes or embryos produced via ART. Following any fertility preservation technique, it is advisable to create legal documents guiding the disposition of any embryos or gametes that are stored for the future, particularly outlining ownership [54]. This can help avoid debate regarding the posthumous use of stored gametes or embryos.
Conclusion
BRCA carriers require special consideration regarding reproduction. Prophylactic and therapeutic management of these patients may compromise their ability to achieve their reproductive goals. A multidisciplinary team approach to this sensitive issue is warranted including oncology, reproductive endocrinology as well as psychosocial supportive providers to assist patients and their loved ones in making the best decisions for themselves in their medical and social situations.
References
Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer (Internet). 2010;127(12):2893–917. Available from: http://doi.wiley.com/10.1002/ijc.25516 (Cited 30 July 2016).
Paluch-Shimon S, Pagani O, Partridge AH, Bar-Meir E, Fallowfield L, Fenlon D, et al. Second international consensus guidelines for breast cancer in young women (BCY2). Breast. 2016;26:87–99.
Ledermann JA, Raja FA, Fotopoulou C, Gonzalez-Martin A, Colombo N, Sessa C, et al. Newly diagnosed and relapsed epithelial ovarian carcinoma: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol (Internet). 2013;24 Suppl 6(suppl 6):vi24–32. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24078660 (cited 31 July 2016).
Lambertini M, Ginsburg ES, Partridge AH. Update on fertility preservation in young women undergoing breast cancer and ovarian cancer therapy. Curr Opin Obstet Gynecol (Internet). 2015;27(1):98–107. Available from: http://content.wkhealth.com/linkback/openurl?sid=WKPTLP:landingpage&an=00001703-201502000-00017 (Cited 30 Jul 2016).
Antoniou A, Pharoah PD, Narod S, Risch HA, Eyfjord JE, Hopper JL, et al. Average risks of breast and ovarian cancer associated with BRCA1 or BRCA2 mutations detected in case series unselected for family history: a combined analysis of 22 studies. Am J Hum Genet. 2003;72:1117–30.
Letourneau JM, Ebbel EE, Katz PP, Katz A, Ai WZ, Chien AJ, et al. Pretreatment fertility counseling and fertility preservation improve quality of life in reproductive age women with cancer. Cancer (Internet). 2012;118(6):1710–7. Available from: http://doi.wiley.com/10.1002/cncr.26459 (Cited 18 July 2016).
Schover LR, Rybicki LA, Martin BA, Bringelsen KA. Having children after cancer. Cancer (Internet). 1999;86(4):697–709. Available from: http://doi.wiley.com/10.1002/%28SICI%291097-0142%2819990815%2986%3A4%3C697%3A%3AAID-CNCR20%3E3.0.CO%3B2-J (Cited 18 July 2016).
Lee SJ, Schover LR, Partridge AH, Patrizio P, Wallace WH, Hagerty K, et al. American Society of Clinical Oncology recommendations on fertility preservation in cancer patients. J Clin Oncol [Internet). 2006;24(18):2917–31. Available from: http://www.ncbi.nlm.nih.gov/pubmed/16651642 (Cited 2 Aug 2016).
Ruddy KJ, Gelber SI, Tamimi RM, Ginsburg ES, Schapira L, Come SE, et al. Prospective Study of Fertility Concerns and Preservation Strategies in Young Women With Breast Cancer. J Clin Oncol (Internet). 2014;32(11):1151–6. Available from: http://jco.ascopubs.org/cgi/doi/10.1200/JCO.2013.52.8877 (Cited 31 July 2016).
Senkus E, Kyriakides S, Ohno S, Penault-Llorca F, Poortmans P, Rutgers E, et al. Primary breast cancer: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol (Internet). 2015;26 Suppl 5(suppl 5):v8–30. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26314782 (Cited 31 July 2016).
Kauff ND, Satagopan JM, Robson ME, Scheuer L, Hensley M, Hudis CA, et al. Risk-reducing salpingo-oophorectomy in Women with a BRCA1 or BRCA2 Mutation. J Clin Oncol. 2008;26(8):1331–37. http://dx.doi.org.ezp-prod1.hul.harvard.edu/101056/NEJMoa020119.
Haber D. prophylactic oophorectomy to reduce the risk of ovarian and breast cancer in carriers of BRCA mutations. N Engl J Med 2002;346:1660–62. http://dx.doi.org.ezp-prod1.hul.harvard.edu/101056/NEJMed020044.
ACOG. Pb103_Brca. Obstet Gynecol (Internet). 2009;114(106):192–202. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21422879.
Derks-Smeets IAP, Gietel-Habets JJG, Tibben A, Tjan-Heijnen VCG, Meijer-Hoogeveen M, Geraedts JPM, et al. Decision-making on preimplantation genetic diagnosis and prenatal diagnosis: a challenge for couples with hereditary breast and ovarian cancer. Hum Reprod (Internet). 2014;29(5):1103–12. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24603131 (Cited 31 July 2016).
Shapira M, Raanani H, Meirow D. IVF for fertility preservation in breast cancer patients—efficacy and safety issues. J Assist Reprod Genet (Internet). 2015;32(8):1171–8. Available from: http://springerlink.bibliotecabuap.elogim.com/10.1007/s10815-015-0519-x (Cited 18 July 2016).
Loren AW, Mangu PB, Beck LN, Brennan L, Magdalinski AJ, Partridge AH, et al. Fertility preservation for patients with cancer: American Society of Clinical Oncology clinical practice guideline update. J Clin Oncol (Internet). 2013;31(19):2500–10. Available from: http://jco.ascopubs.org/cgi/doi/10.1200/JCO.2013.49.2678 (Cited 3 Aug 2016).
Lambertini M, Ceppi M, Poggio F, Peccatori FA, Azim HA, Ugolini D, et al. Ovarian suppression using luteinizing hormone-releasing hormone agonists during chemotherapy to preserve ovarian function and fertility of breast cancer patients: a meta-analysis of randomized studies. Ann Oncol (Internet). 2015;26(12):2408–19. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26347105 (Cited 30 July 2016).
Wieand S, Hale K, Lee M, Walsh T, Owens K, Tait J, et al. Tamoxifen Breast Cancer Incidence. 2014;286(18):2251–6.
Barton SE, Missmer SA, Berry KF, Ginsburg ES. Female cancer survivors are low responders and have reduced success compared with other patients undergoing assisted reproductive technologies. Fertil Steril. 2012;97(2):381–6.
Pfeifer S, Gldberg J, McClure R, Lobo R, Thomas M, Widra E, et al. Practice Committees of American Society for reproductive medicine; society for assisted reproductive technology. mature oocyte cryopreservation: a guideline. Fertil Steril. 2013;99(1):37–43.
Avraham S, Machtinger R, Cahan T, Sokolov A, Racowsky C, Seidman DS. What is the quality of information on social oocyte cryopreservation provided by websites of society for assisted reproductive technology member fertility clinics? Fertil Steril. 2014;101(1):222–6.
Meirow D, Biederman H, Anderson RA, Wallace WHB. Toxicity of chemotherapy and radiation on female reproduction. Clin Obstet Gynecol (Internet). 2010;53(4):727–39. Available from: http://content.wkhealth.com/linkback/openurl?sid=WKPTLP:landingpage&an=00003081-201012000-00004 (Cited 18 Jul 2016).
Partridge AH. Prevention of premature menopause and preservation of fertility in young cancer survivors. JAMA (Internet). 2015;314(24):2625. Available from: http://jama.jamanetwork.com/article.aspx?doi=10.1001/jama.2015.17299 (Cited 29 July 2016).
Pagani O, Regan MM, Walley BA, Fleming GF, Colleoni M, Láng I, et al. Adjuvant exemestane with ovarian suppression in premenopausal breast cancer. N Engl J Med (Internet). 2014;371(2):107–18. Available from: http://www.nejm.org/doi/abs/10.1056/NEJMoa1404037 (Cited 3 Aug 2016).
Pfeifer S, Goldberg J, Lobo R, Pisarska M, Thomas M, Widra E, et al. Practice Committee of American Society for reproductive medicine. Ovarian tissue cryopreservation: a committee opinion. Fertil Steril. 2014;101(5):1237–43.
Meirow D, Ra H, Shapira M, Brenghausen M, Derech Chaim S, Aviel-Ronen S, et al. Transplantations of frozen-thawed ovarian tissue demonstrate high reproductive performance and the need to revise restrictive criteria. Clin trial regist number NCT02659592. Fertil Steril (Internet). 2016;106:467–74. Available from: http://fertstertforum.com/meirowd-ovarian-transplantation/ (Cited 3 Aug 2016).
Cakmak H, Rosen MP. Random-start ovarian stimulation in patients with cancer. Curr Opin Obstet Gynecol (Internet). 2015;27(3):215–21. Available from: http://content.wkhealth.com/linkback/openurl?sid=WKPTLP:landingpage&an=00001703-201506000-00011 (Cited 2 Aug 2016).
Cakmak H, Katz A, Cedars MI, Rosen MP. Effective method for emergency fertility preservation: random-start controlled ovarian stimulation. Fertil Steril. 2013;100(6):1673–80.
Madrigrano A, Westphal L, Wapnir I. Egg retrieval with cryopreservation does not delay breast cancer treatment. Am J Surg. 2007;194(4):477–81.
Westphal LM, Wapnir IL. Integration and safety of fertility preservation in a breast cancer program. Gynecol Oncol. 2012;124(3):474–6.
Azim AA, Costantini-Ferrando M, Oktay K. Safety of fertility preservation by Ovarian stimulation With Letrozole and gonadotropins in patients with breast cancer: A prospective controlled study. J Clin Oncol (Internet). 2008;26(16):2630–5. Available from: http://jco.ascopubs.org/cgi/doi/10.1200/JCO.2007.14.8700 (Cited 1 Aug 2016).
Meirow D, Raanani H, Maman E, Paluch-Shimon S, Shapira M, Cohen Y, et al. Tamoxifen co-administration during controlled ovarian hyperstimulation for in vitro fertilization in breast cancer patients increases the safety of fertility-preservation treatment strategies. Fertil Steril. 2014;102(2):488–495.e3.
Oktay K, Buyuk E, Libertella N, Akar M, Rosenwaks Z. Fertility preservation in breast cancer patients: a prospective controlled comparison of ovarian stimulation with tamoxifen and letrozole for embryo cryopreservation. J Clin Oncol (Internet). 2005;23(19):4347–53. Available from: http://www.jco.org/cgi/doi/10.1200/JCO.2005.05.037 (Cited 31 Jul 2016).
Perri T, Lifshitz D, Sadetzki S, Oberman B, Meirow D, Ben-Baruch G, et al. Fertility treatments and invasive epithelial ovarian cancer risk in Jewish Israeli BRCA1 or BRCA2 mutation carriers. Fertil Steril. 2015;103(5):1305–12.
Oktay K, Kim JY, Barad D, Babayev SN. Association of BRCA1 mutations with occult primary ovarian insufficiency: a possible explanation for the link between infertility and breast/ovarian cancer risks. J Clin Oncol (Internet). 2010;28(2):240–4. Available from: http://jco.ascopubs.org/cgi/doi/10.1200/JCO.2009.24.2057 (Cited 18 July 2016).
Wang ET, Pisarska MD, Bresee C, Ida Chen Y-D, Lester J, Afshar Y, et al. BRCA1 germline mutations may be associated with reduced ovarian reserve. Fertil Steril. 2014;102(6):1723–8.
Shapira M, Raanani H, Feldman B, Srebnik N, Dereck-Haim S, Manela D, et al. BRCA mutation carriers show normal ovarian response in in vitro fertilization cycles. Fertil Steril. 2015;104(5):1162–7.
Valentini A, Finch A, Lubinski J, Byrski T, Ghadirian P, Kim-Sing C, et al. Chemotherapy-induced amenorrhea in patients with breast cancer with a BRCA1 or BRCA2 Mutation. J Clin Oncol (Internet). 2013;31(31):3914–9. Available from: http://jco.ascopubs.org/cgi/doi/10.1200/JCO.2012.47.7893 (Cited 31 July 2016).
Finch A, Valentini A, Greenblatt E, Lynch HT, Ghadirian P, Armel S, et al. Frequency of premature menopause in women who carry a BRCA1 or BRCA2 mutation. Fertil Steril (Internet). 2013;99:1724–8 (Cited 18 Jul 2016).
Cardozo ER, Thomson AP, Karmon AE, Dickinson KA, Wright DL, Sabatini ME. Ovarian stimulation and in-vitro fertilization outcomes of cancer patients undergoing fertility preservation compared to age matched controls: a 17-year experience. J Assist Reprod Genet. 2015;32(4):587–96.
Azim HA, Kroman N, Paesmans M, Gelber S, Rotmensz N, Ameye L, et al. Prognostic impact of pregnancy after breast cancer according to estrogen receptor status: a multicenter retrospective study. J Clin Oncol (Internet). 2013;31(1):73–9. Available from: http://jco.ascopubs.org/cgi/doi/10.1200/JCO.2012.44.2285 (Cited 18 Jul 2016).
Euhus DM, Robinson L. Genetic predisposition syndromes and their management. Surg Clin North Am. 2013;93(2):341–62.
Howard-Anderson J, Ganz PA, Bower JE, Stanton AL. Quality of life, fertility concerns, and behavioral health outcomes in younger breast cancer survivors: a systematic review. J Natl Cancer Inst (Internet). 2012;104(5):386–405. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22271773 (Cited 31 July 2016).
Letourneau JM, Smith JF, Ebbel EE, Craig A, Katz PP, Cedars MI, et al. Racial, socioeconomic, and demographic disparities in access to fertility preservation in young women diagnosed with cancer. Cancer. 2012;118(18):4579–88.
Grover NS, Deal AM, Wood WA, Mersereau JE. Young men with cancer experience low referral rates for fertility counseling and sperm banking. J Oncol Pract (Internet). 2016;12(5):465–471. Available from: http://www.ncbi.nlm.nih.gov/pubmed/27118159.
Rudick B, Opper N, Paulson R, Bendikson K, Chung K. The status of oocyte cryopreservation in the United States. Fertil Steril. 2010;94:2642–6.
IVF Italy 2004.pdf.
Beck L, Sileo M, Copperman A. The average cost of fertility preservation for female cancer patients. Fertil Steril. 2010;94:S105.
Center MSKC. Fertility preservation: options for women who are starting cancer treatment.
Kim J, Oktay K, Gracia C, Lee S, Morse C, Mersereau JE. Which patients pursue fertility preservation treatments? A multicenter analysis of the predictors of fertility preservation in women with breast cancer. Fertil Steril. 2012;97(3):671–6.
American Society for Reproductive Medicine. ASRM: state infertility coverage at a glance (Internet). Available from: http://www.asrm.org/insurance.aspx.
Rich TA, Liu M, Etzel CJ, Bannon SA, Mork ME, Ready K, et al. Comparison of attitudes regarding preimplantation genetic diagnosis among patients with hereditary cancer syndromes. Fam Cancer (Internet). 2014;13(2):291–9. Available from: http://springerlink.bibliotecabuap.elogim.com/10.1007/s10689-013-9685-0 (Cited 31 July 2016).
Insogna IG, Ginsburg E, Rich T, Liu M, Etzel C, Bannon S, et al. Transferring embryos with indeterminate PGD results: the ethical implications. Fertil Res Pract (Internet). 2016;2(1):2. Available from: http://fertilityresearchandpractice.biomedcentral.com/articles/10.1186/s40738-016-0014-9 (Cited 12 Sept 2016).
Ethics Committee of the American Society for Reproductive Medicine T. Fertility preservation and reproduction in patients facing gonadotoxic therapies: a committee opinion. Fertil Steril (Internet). 2013;100:1224–31. (Cited 12 Sept 2016).
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this chapter
Cite this chapter
Insogna, I.G., Ginsburg, E.S., Partridge, A.H. (2017). Fertility Preservation in BRCA Carriers: Special Considerations. In: B. Chagpar, A. (eds) Managing BRCA Mutation Carriers . Springer, Cham. https://doi.org/10.1007/978-3-319-59198-8_10
Download citation
DOI: https://doi.org/10.1007/978-3-319-59198-8_10
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-59197-1
Online ISBN: 978-3-319-59198-8
eBook Packages: MedicineMedicine (R0)