Abstract
Central endobronchial carcinoid represents often the subtype characterised by the least aggressive behaviour in the entire spectrum of differentiation of neuroendocrine tumours of the lung. Being central, they became generally early symptomatic and therefore is not unfrequent, an early diagnosis when their diffusion is still locoregional. As is well known, WHO Classification subdivides carcinoid on the basis of the mitotic count and the presence or lack of necrosis in typical (TC) and atypical (AC). It should be remarked that these tumours, although may have an indolent biological behaviour, are not benign and even the lower-grade TC may be associated with a haematogenous and lymphatic spread. Therefore the therapeutic approach, either surgical, interventional endoscopic or medical, requires always a careful multidisciplinary planning at the light of the distinctive peculiarities of these subcategories. Finally, an accurate and extensive follow-up plays a crucial role even in the cases apparently radically cured. This chapter will review, starting from the clinics of two evidence-based practice cases, the therapeutic options available for locoregional bronchial carcinoids in a multidisciplinary setting.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
FormalPara OverviewCentral endobronchial carcinoid represents often the subtype characterised by the least aggressive behaviour in the entire spectrum of differentiation of neuroendocrine tumours of the lung. Being central, they became generally early symptomatic and therefore is not unfrequent, an early diagnosis when their diffusion is still locoregional. As is well known, WHO Classification [1] subdivides carcinoid on the basis of the mitotic count and the presence or lack of necrosis in typical (TC) and atypical (AC). It should be remarked that these tumours, although may have an indolent biological behaviour, are not benign and even the lower-grade TC may be associated with a haematogenous and lymphatic spread. Therefore the therapeutic approach, either surgical, interventional endoscopic or medical, requires always a careful multidisciplinary planning at the light of the distinctive peculiarities of these subcategories. Finally, an accurate and extensive follow-up plays a crucial role even in the cases apparently radically cured. This chapter will review, starting from the clinics of two evidence-based practice cases, the therapeutic options available for locoregional bronchial carcinoids in a multidisciplinary setting.
Clinical Case 1
A 21-year-old male (C.D.) was hospitalised for progressive episodes of dyspnoea on exertion and the persistence, in the past 6 months, of recurrent episodes of inspiratory siblings and concomitant cough with haemoptoic sputum. A CT scan showed the presence of a 11 mm diameter left endobronchial polypoid lesion . Fibrebronchoscopy evidenced a pedunculated lesion partially occluding the main left bronchus (◘ Fig. 19.1a). Under general anaesthesia, a rigid bronchoscopy with endobronchial neodymium:yttrium-aluminium-garnet (Nd:YAG) laser disobliteration was performed. The residual tissue scar was spotted at the mucosal area of the segmental bronchi for the apical segment (B6) of the lower lobe.
Endoscopic appearance a of the typical carcinoid tumour resected with neodymium:yttrium-aluminium-garnet (Nd:YAG) laser. At the final pathology report on the lung specimen, in the submucosal space, under the area treated endoscopically [b; black spots of photocoagulation], a 0.7 cm area of disease was detected [c; highlighted brownish area obtained with Chromogranin A staining]
The final pathology report described an atypical carcinoid (AC) due to the presence of necrosis. Despite that the excision was apparently radical at bronchoscopy and CT, after discussion with the patients, we convene, for a curative intent, to proceed for surgery. The patient underwent therefore to a left lower sleeve lobectomy (◘ Fig. 19.2) with systematic lymph node dissection for a pathological stage IA (T1b N0 M0, AJCC 8th Edition [2]) low-grade typical carcinoid (TC) detected under the scar tissue of the previous laser treatment site (◘ Fig. 19.1a, c). The patient started postsurgical follow-up according to the current ENETS and ESMO Guidelines 8 [3]. At 7 years no recurrence has been detected, but the patient will continue the follow-up at least till 15 years postsurgery.
Left lower lobe sleeve re section [drawing] of the endobronchial submucosal remnant of typical carcinoid. The two sides of the bronchi without the disease a were attached b with separate 3-0 Vicryl stitches. Final result of the procedure c and suture coverage with a pedunculated fat pad d from the mediastinum
1 Comments to the Case
This case is an emblematic example of how the locoregional treatment with only Nd:YAG laser disobliteration for an endobronchial TC cannot sufficiently eradicate the disease. Indeed, despite an apparent radical endobronchial excision, under the scar, a persistence of disease was demonstrated by surgery (◘ Fig. 19.1b, c). Furthermore endobronchial resection does not allow the lymph-nodal resection and is now well known how lymph-nodal metastases may be present at diagnosis up to 20% of TC and in more than 50% of AC [4]. In these cases endobronchial treatment may result incomplete in a significant percentage of patients, while surgical treatment may offer the definitive cure to the patient if done with a proper lymph nodal dissection [4, 5]. The young age, like in this case, may be crucial to choose a treatment that offers a higher possibility of cure, while in elderly patients, with a lower performance status and/or co-morbidity, an endoscopic treatment with palliative intent may be justified [4].
Pathology report, such as in this patient, may be misleading [5] if the multiple samples are collected after laser treatment, due to the fact that the presence of artificial coagulative necrosis, induced by the treatment, may lead to a diagnosis of AC rather than TC. In the postsurgical histological diagnosis, the mitotic rate less than 2 mitoses per 10 HPF and the absence of necrosis (Ki-67 wa s less than 2%) were consistent with the definitive diagnosis of TC according to the WHO criteria [1].
Questions
-
1.
May endoscopic treatment (i.e. laser or brachytherapy) be considered a valid alternative to surgery in bronchial carcinoids?
-
2.
May carcinoid have metastatic spread? How is the cancer specific survival rate? Is recurrence more frequently locoregional or at distance?
-
3.
Besides CT scan, are there other diagnostic tools to evaluate metastatic diffusion?
-
4.
Is lung parenchyma-sparing resection a valid substitute of major lung resection (i.e. lobectomy or pneumonectomy) for endobronchial lesions?
Answers
-
1.
Endobronchial disobliteration using neodymium:yttrium-aluminium-garnet (Nd:YAG) laser or other local treatments such as photodynamic therapy, cryotherapy and mechanical removal has been described in some series in literature [6, 7], in a cohort of highly selected patients, associated with good outcome after short-term follow-up in an interval time ranging from 1 to a maximum of 5 years. It should be however remarked that an accurate and protracted follow-up is always necessary [8] to consider the patient cured. The peak of recurrence is generally located within 5 years in AC and over 10 years in TC [4, 8, 9]. Furthermore the impossibility to evaluate and remove lymph node candidates an high percentage of patients (around 20% of the total in TC and more than 50% in AC) to a persistence of disease, while in most of the patients surgery may obtain an R0 resection [4, 9, 10] with distant metastases detected during the follow-up [4, 5].
Surgery should therefore still be considered the treatment of choice. However endobronchial resections may play an important role in a multidisciplinary setting to allow presurgical disobliteration or in the palliative setting in the elderly patients with/without relevant co-mor bidities who cannot be candidates for surgery [3, 4, 11].
-
2.
Histological distinction between TC and AC represents the most important prognostic factor [1, 3, 4]. Haematogenous and lymphatic metastatic spread may be possible in both subtype but more common in AC [1, 4]. In older series, overall cancer-specific survival for resectable tumours, after the Travis Classification [12, 13], was reported to be for TC 95% (range 87–100%) at 5 years, 91% (range 82–87%) at 10 years and 85% (range 83–87%) at 15 years and for AC 72% (range 56–78%) at 5 years, 55% (range 73–98%) at 10 years and 53% at 15 years [4].
In a recent meta-analyses study done by Detterbeck [4], most of the patient had the disease distally recurred (74% TC and 82% AC). A 13% of local or local + distant metastases were described in TC, while a 7% of local and 11% local + distant recurrences were evident in AC patients. Bone metastases have been reported in the only prospective study in around 70% of the cases (Ferolla et al. LUNA Trial NCT01563354 presented at ESMO 2016 in submission).
-
3.
A careful preoperative, surgical and postoperative diagnostic workup is of crucial importance [3, 8, 9, 11, 13]. Recently new endoscopic tools such as endobronchial ultrasound probes or fibre optic narrowband images and 3-D navigation system guidance may add some value [14]. Nuclear medicine techniques like SRS and Ga68-DOTA PET may play a relevant role in the staging, and MR of the spine may be associated to evaluate bone metastatic spread in the symptomatic patients [3].
-
4.
Data from the literature highlight how lobectomies are the predominant operations [4, 5, 7, 9, 10]. Among the other available techniques, there is a tendency towards conservative surgery (sublobar resections and sleeve lobectomies), although a considerable number of pneumonectomies are still reported (up to 27%) [4]. The main concern in surgical treatment of carcinoids is to avoid unnecessary removal of functioning pulmonary tissue [3, 8,9,10,11]. However, while parenchyma-sparing operations such as sleeve lobectomies or tracheo-bronchoplasties represent the procedure of choice for centrally located carcinoid tumours in experienced centres [4, 5, 9, 10], the outcome might be questionable if the lymphadenectomy is not properly performed and the endoscopic follow-up not periodically done [4, 9].
Clinical Case 2
A 39-year-old male was referred to our hospital for metastatic typical bronchial carcinoid. When he was 25, he underwent in another hospital bilobectomy of the lower and middle lobe without lymphadenectomy for a typical carcinoid. He then developed multiple recurrences after 8 years with metastatic diffusion to the liver, lungs, lymph nodes and bones (spine, sternum, iliac). Subsequent treatments, including locoregional procedures for metachronous liver metastases and for a single lesion of the lower part of the sternum, were performed. After radiological progression of the metastatic spread at the liver, bone and lymph nodes, the patients were treated with long-acting somatostatin analogues obtaining a stable disease according to RECIST 1.0 criteria for 36 months. After a new RECIST progression of the patient at lymph node and liver level, the patient was enrolled in a phase III trial with a combination of octreotide LAR 30 mg every 28 days and everolimus 10 mg/day obtaining a stable disease for the following 30 months.
In March 2010, the patient was admitted at our institution complaining with cough, dyspnoea and fever. Chest-abdomen CT scan revealed partial atelectasis of the residual right lung, multiple pulmonary nodules in the left lung (◘ Fig. 19.3, panel 1a) and increasing in size and number of liver and lymph-nodal metastasis. Fibrebronchoscopy showed a centimetric red polypoid neoplasm originating from the stump of the intermediate bronchus and partially obliterating the upper lobar bronchus (◘ Fig. 19.3, panel 1b). Furthermore, three lesions on the vertebral body of T2, sternum and the right sacrum ala were detected at MR imaging. Multimodality therapy was indicated. External radiation therapy was delivered to sternum, right sacral ala and vertebral body. The patient received also palliative endobronchial high-dose rate BT (Iridium 192) with a total dose of 20 Gy in four weekly fractions over 1 month (◘ Fig. 19.3, panel 2a and 2b). Although a complete change in the vascularization of the endobronchial lesion was observed (◘ Fig. 19.3, panel 3b), no changes in the tumour volume were noted in this phase. Furthermore the residual right lung was completely atelectasic (◘ Fig. 19.3, panel 3a). Adjuvant temozolomide (TMZ) 200 mg/m2 per os for 5 days associated with octreotide LAR 30 mg in every 28 days was administered. After 1 month from the start of the therapy with TMZ, a partial reduction in the tumour volume was observed (◘ Fig. 19.3, panel 4b) that allowed the re-expansion of the residual right lung parenchyma (◘ Fig. 19.3, panel 4a). Eighteen months later, clinical and radiological workup with CT scan and MRI demonstrated partial remission of disease in the liver, bone, lymph nodes and bilateral pulmonary parenchyma; fibrebronchoscopy revealed complete disappearance of the bronchial polypoid lesion (◘ Fig. 19.3, panel 5b). No relevant side effects were observed. Three years later, with stable disease, the patient passed away for other causes not related to his disease (traumatic death).
The CT scan initial appearance of the carcinoid tumour (◘ Fig. 19.1 panel 1a) shows a metastatic spread in both lungs and an endobronchial recurrence of the typical carcinoid in the stump of the bronchus intermedius (◘ Fig. 19.1 panel 1b). Furthermore the endoscopic view of the carcinoid tumour (◘ Fig. 19.1 panel 1b) was surrounded by capillary web particularly on the cartilaginous part of the main right bronchus mucosa (arrow). After the first fraction of brachytherapy (◘ Fig. 19.1 panel 2a, arrows on the two beads of the centring intraluminal guide probe, asterisk, whereas the HDR field was performed), the endobronchial lesion increased in volume due to the necrotic tissue (◘ Fig. 19.1 panel 2b). At the third fraction of BT, the right lung was completely atelectasic (◘ Fig. 19.1 panel 3a) with fibrous tissue occluding completely the lumen of the bronchus for the right upper lobe at the endoscopic view (◘ Fig. 19.1 panel 3b). Furthermore decreased extension of the capillary web, covered by white induitus of fibrin, was fairly present (◘ Fig. 19.1 panel 3b arrow). During this period chemotherapy with TMZ was started (red fading field). At the 6-month period after the initial TMZ treatment, the endobronchial lesion shrinks 20% (◘ Fig. 19.1 panel 4b) with a slight decrease of the previously described capillary area (arrow). At the CT scan was clearly evident the re-expansion of the right upper lobe (◘ Fig. 19.1 panel 4a). Control after 1 year of treatment shows a reduction in size and numbers of the lung metastatic lesions (◘ Fig. 19.1 panel 5a) and a complete disappearance of the endobronchial lesion as well as the capillary web on the cartilaginous part of the main right bronchus (◘ Fig. 19.1 panel 5b arrow)
2 Comments to the Case
This case leads to some considerations:
-
1.
The multimodal approach to an endobronchial carcinoid has been associated in this case with a significant efficacy and low toxicity, probably superior to an only systemic medical approach. Although the timing of the clinical response does not indicate a sure direct correlation, TMZ is a drug that is well known to increase radio sensitivity; therefore a synergistic late addictive effect [15] of the BT may be suspected.
-
2.
Being associated with a major rate of objective response when compared to everolimus utilised in the previous case, TMZ may be of choice when a tumour shrinkage is the main aim of the treatment.
-
3.
Disobliteration may be an important aim in bronchial carcinoid, which is generally associated with a long-time survival also in the metastatic phase. In this case the disobliteration allowed the resolution of the obstructive pneumonitis and the re-expansion of the collapsed lung.
-
4.
The patients several years before underwent in another hospital surgical resection without lymphadenectomy. The brief time between surgery and recurrence raises reasonable doubt on the radicality of the intervention. Again it should in fact be remembered that also in TC the percentage of lymph-nodal metastatic spread may reach 20% of the cases. We recommend therefore always the systematic lymph nodal dissection, particularly in young patient like this.
Questions
-
1.
Is TMZ alone or in combination with BT an option in metastatic bronchial carcinoids?
Answers
-
1.
Temozolomide (TMZ) [15, 16] is an alkylating drug inserted as a possible therapeutic option both in ESMO and ENETS Guidelines [3, 11]. The activity of this drug has been showed in retrospective NET phase II clinical trials [16], while the first prospective trial in lung NET is actually ongoing (Ferolla et al. ATLANT study NCT02698410 enrolling). Brachytherapy (BT) has been used so far as a palliative treatment of NSCLC but not clearly codified for the treatment of well-differentiated neuroendocrine tumours of the lung [17], and further evidences are needed for a routinely use in these tumours.
Up to Date of the Topic
The bronchial tree represents one of the most frequent sites of origin of neuroendocrine tumours (NET) with a prevalence ranging between 25% and 30% of all NET [1, 3, 4, 20]. Approximately 70% of carcinoid tumours present as an endoscopically visible tumour, usually located in a segmental bronchus, less often in main bronchi, rarely in the carina or trachea [4].
When feasible, surgery represents the treatment of choice in well-differentiated lung NET (TC and AC) and the only procedure that can cure the patients [4, 5, 9, 10]. It should always be remarked however that the definitive cure should be established in these tumours only after an accurate and protracted follow-up, reaching more than 15 years till in the case associated with a radical resection [8]. Since the advent of the minimally invasive surgery in the early 1990s and recently the robotic surgery as well as the renaissance of sublobar resections as a possible alternative tool for the low-grade neuroendocrine tumours of the lung, the best surgical treatment for primary lung carcinoid tumours represents a benchmark for the surgeon [10]. Minimally invasive surgery is based upon limited access (from one to three centimetric incisions) to the thoracic cavity achieved through video-assisted or pure videothoracoscopic techniques. In both cases standard lobectomies or sublobar resections may be performed. The main controversy concerning the minimally invasive approach with sublobar or bronchoplastic resections lies in the possibility of performing a true systematic lymph node dissection. Several authors claim their results with this technique are equal to those obtained with thoracotomies [4, 10]. However, until randomised trials will prove or disprove this assertion, we believe that an open access, with a small muscle-sparing thoracotomy particularly in young patients, for bronchoplastic procedures represents the safest approach for centrally located tumours. Furthermore limited resection or bronchoplastic procedures might be applicable in the TC or patient with limited lung function and/or cardiovascular impairment [21]; AC carcinoid should be treated with more oncological aggressiveness with a mandatory lymph nodal dissection. Considering the frequent occurrence of metastatic lymph nodes even in TC, a lymph node sampling cannot be accepted, and a systematic mediastinal dissection should always be done [5]. In our experience, this technique yielded over 13% of metastatic lymph nodes in patients affected by TC [9, 21].
Endobronchial laser treatment and cryotherapy or photodynamic clearance of the affected site are justified as palliative management in patients not fit for operative treatment and as a useful adjunct to surgery since preoperative removal of obstructing lesions allows clearing of the bronchial tree from secretions [4, 9, 11, 21]. These techniques should not be used with a curative intent because, according to our experience, residual nests of tumour cells can be detected in the submucosa after an apparent radical removal. However in the rare cases of primary multiple endobronchial lesions, laser treatment might allow a more limited resection and a systematic oncological treatment.
Moreover lymphatic spread cannot be assessed unless proven by mediastinoscopy or with the recent endobronchial ultrasound technique [14].
A particular word needs to be spent on multiple neuroendocrine forms such as diffuse idiopathic pulmonary neuroendocrine cell hyperplasia (DIPNECH) and tumourlets detected in the lung parenchyma around the primary resected tumour: should it be considered neoplasm? The pathologist should always be aware about these possible findings and always search carefully in the lung parenchyma. In our experience [9], 25% of patients had the presence of these lesions when the parenchyma was carefully analysed by our pathologist. The final answer will be obtained from molecular biology studies. Conversely, multiple endobronchial carcinoids, as primitive lesions, are rare and should always beware of the possibility that they might represent just a sign of submucosal lymphatic spread.
At the moment there are no prospective studies evaluating the role of an adjuvant medical therapy after a radical surgery, and no indication is actually expressed in the main international guidelines [3, 11]. The design of specific randomised prospective trials, particularly in the AC associated with nodal involvement, employing low-toxicity drugs like long-acting somatostatin analogues would be of interest but will require a prolonged time of observation to be significant.
Medical therapy may play a role in the palliative setting till in the locoregional disease, whenever surgical treatment may be not feasible both for the extension of the disease both for the performance status and co-morbidity of the patients [18, 19].
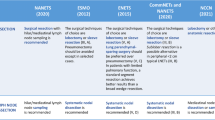
The choice of the therapy should be evaluated in the course of a multidisciplinary tumour board. The options start with the control of the hormonal hypersecretions when present to the anti-proliferative intent. The main aim of the medical treatment is generally a stabilisation of the tumour growth rather than an objective response. The first-line therapy in TC and AC with locoregional disease is generally based on long-acting somatostatin. Their use is generally extrapolated from the results of two phase III studies performed in GEP NET (the PROMID study using octreotide LAR and CLARINET study using lanreotide) [22]. However at the time of publication of this chapter, a phase III study with lanreotide dedicated to lung NET (the SPINET study) is ongoing and enrolling. Another study exploring the efficacy and safety of the combination of lanreotide and temozolomide in TC and AC with progressive disease (ATLANT study) is ongoing and enrolling. Another somatostatin analogue, pasireotide, has shown activity in TC and AC alone or in combination with everolimus (LUNA study presented at ESMO 2016, in submission).
As second line, the drug everolimus has shown activity in TC and AC in the phase III trial RADIANT IV and in the cited LUNA study alone or in combination with pasireotide [23, 24]. Retrospective series report efficacy of temozolomide in retrospective series, and the first prospective study in this context is ongoing. PRRT has been evaluated in small retrospective series [25].
In conclusion every decision in the palliative setting, particularly when facing with locoregional disease, should be evaluated in a multidisciplinary setting weighing the balance between toxicities and benefit, and the therapeutic approach should be always tailored on the single patients in centre with high level of expertise.
Bibliography
Beasley MB, Brambilla E, Chirieac LR, Austin JHM, Devesa SS, Hasleton P, Jett J, Marchevsky AM, Nicholson S, Papotti M, Pelosi G, Rami-Porta R, Scagliotti G, Thunnissen E, Travis WD, van Schil P, Yang P (2015) Carcinoid tumour. In: Travis WD, Brambilla E, Burke AP, Marx A, Nicholson AG (eds) WHO classification of tumours of lung, pleura, thymus and heart, 4th edn. IARC, Lyon, pp 73–77
Rami-Porta R, Asamura H, Travis WD, Rusch VW (2017) Chapter 36: Lung. In: American Joint Committee on Cancer (AJCC) staging manual, 8th edn. Springer, pp 431–457
Öberg K, Hellman P, Ferolla P, Papotti M, ESMO Guidelines Working Group (2012) Neuroendocrine bronchial and thymic tumors: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 23 Suppl 7:vii120–vii123
Escalon JC, Detterbeck FC (2009) Chapter 122: Carcinoid tumors. In: Shields TW, Locicero III J, Reed CE, Feins RH (eds) General thoracic surgery, 7th edn. Wolters Kluwer and Lippincott Williams & Wilkins, pp 1539–1554
Daddi N, Schiavon M, Filosso PL, Cardillo G, Ambrogi MC, De Palma A, Luzzi L, Bandiera A, Casali C, Ruffato A, De Angelis V, Andriolo LG, Guerrera F, Carleo F, Davini F, Urbani M, Mattioli S, Morandi U, Zannini P, Gotti G, Loizzi M, Puma F, Mussi A, Ricci A, Oliaro A, Rea F, Multi-Institutional Italian Pathology Group (2014) Prognostic factors in a multicentre study of 247 atypical pulmonary carcinoids. Eur J Cardiothorac Surg 45(4):677–686
Boxxen study and Neyman K, Sundset A, Naalsund A, Espinoza A, Solberg S, Kongerud J, Fosse E (2012) Endoscopic treatment of bronchial carcinoids in comparison to surgical resection: a retrospective study. J Bronchology Interv Pulmonol 19(1):29–34
Raz DJ, Nelson RA, Grannis FW, Kim JY (2015) Natural history of typical pulmonary carcinoid tumors: a comparison of nonsurgical and surgical treatment. Chest 147(4):1111–1117
Ferolla P, Daddi N, Puma F, Crinò L (2014) Postsurgical follow-up is always necessary in bronchial carcinoid. Ann Thorac Surg 98(3):1143–1144
Ferolla P, Daddi N, Urbani M, Semeraro A, Ribacchi R, Giovenali P, Ascani S, De Angelis V, Crinò L, Puma F, Daddi G (2009) Tumorlets, multicentric carcinoids, lymph-nodal metastases, and long-term behavior in bronchial carcinoids. J Thorac Oncol 4(3):383–387
Fox M, Van Berkel V, Bousamra M 2nd, Sloan S, Martin RC 2nd (2013) Surgical management of pulmonary carcinoid tumors: sublobar resection versus lobectomy. Am J Surg 205(2):200–208
Caplin ME, Baudin E, Ferolla P, Filosso P, Garcia-Yuste M, Lim E, Oberg K, Pelosi G, Perren A, Rossi RE, Travis WD, ENETS consensus conference participants (2015) Pulmonary neuroendocrine (carcinoid) tumors: European Neuroendocrine Tumor Society expert consensus and recommendations for best practice for typical and atypical pulmonary carcinoids. Ann Oncol 26(8):1604–1620
Travis WD, Rush W, Flieder DB, Falk R, Fleming MV, Gal AA, Koss MN (1998) Survival analysis of 200 pulmonary neuroendocrine tumors with clarification of criteria for atypical carcinoid and its separation from typical carcinoid. Am J Surg Pathol 22(8):934–944
Faggiano A, Ferolla P, Grimaldi F, Campana D, Manzoni M, Davì MV, Bianchi A, Valcavi R, Papini E, Giuffrida D, Ferone D, Fanciulli G, Arnaldi G, Franchi GM, Francia G, Fasola G, Crinò L, Pontecorvi A, Tomassetti P, Colao A (2012) Natural history of gastro-entero-pancreatic and thoracic neuroendocrine tumors. Data from a large prospective and retrospective Italian epidemiological study: the NET management study. J Endocrinol Investig 35(9):817–823
Lee P, Colt HG (2010) Bronchoscopy in lung cancer: appraisal of current technology and for the future. J Thorac Oncol 5(8):1290–1300
Stupp R, Mason WP, van den Bent MJ et al (2005) Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med 352:987–996
Ekeblad S, Sundin A, Janson ET, Welin S, Granberg D, Kindmark H, Dunder K, Kozlovacki G, Orlefors H, Sigurd M, Oberg K, Eriksson B, Skogseid B (2007) Temozolomide as monotherapy is effective in treatment of advanced malignant neuroendocrine tumors. Clin Cancer Res 13(10):2986–2991
Chalmers AJ, Ruff EM, Martindale C, Lovegrove N, Short SC (2009) Cytotoxic effects of temozolomide and radiation are additive- and schedule-dependent. Int J Radiat Oncol Biol Phys 75(5):1511–1519
Ferolla P (2014) Medical treatment of advanced thoracic neuroendocrine tumors. Thorac Surg Clin 24(3):351–355
Ferolla P (2015) Medical therapy of pulmonary neuroendocrine neoplasms: targeted, symptomatic and chemotherapy. Front Horm Res 44:193–197
Ferolla P, Faggiano A, Avenia N, Milone F, Masone S, Giampaglia F, Puma F, Daddi G, Angeletti G, Lombardi G, Santeusanio F, Colao A (2007) Epidemiology of non-gastroenteropancreatic (neuro) endocrine tumours. Clin Endocrinol 66(1):1–6
Daddi N, Ferolla P, Urbani M, Semeraro A, Avenia N, Ribacchi R, Puma F, Daddi G (2004 Oct) Surgical treatment of neuroendocrine tumors of the lung. Eur J Cardiothorac Surg 26(4):813–817
Caplin ME, Pavel M, Ćwikła JB, Phan AT, Raderer M, Sedláčková E, Cadiot G, Wolin EM, Capdevila J, Wall L, Rindi G, Langley A, Martinez S, Blumberg J, Ruszniewski P, CLARINET Investigators (2014) Lanreotide in metastatic enteropancreatic neuroendocrine tumors. N Engl J Med 371(3):224–233
Yao JC, Fazio N, Singh S, Buzzoni R, Carnaghi C, Wolin E, Tomasek J, Raderer M, Lahner H, Voi M, Pacaud LB, Rouyrre N, Sachs C, Valle JW, Delle Fave G, Van Cutsem E, Tesselaar M, Shimada Y, Oh DY, Strosberg J, Kulke MH, Pavel ME, RAD001 in Advanced Neuroendocrine Tumours, Fourth Trial (RADIANT-4) Study Group (2016) Everolimus for the treatment of advanced, non-functional neuroendocrine tumours of the lung or gastrointestinal tract (RADIANT-4): a randomised, placebo-controlled, phase 3 study. Lancet 387(10022):968–977
Yao J, Fazio N, Buzzoni R, Delle Fave G, Tesselaar M, Wolin E, Van Cutsem E, Tomassetti P, Strosberg J, Voi M, Pacaud L, Ridolfi A, Singh S, Pavel M, Kulke M (2016) ORAL02.02: efficacy and safety of everolimus in advanced, progressive, nonfunctional neuroendocrine tumors (NET) of the lung: RADIANT-4 Subgroup Analysis: Topic: Medical Oncology. J Thorac Oncol 11(11S):S253
Parghane RV, Talole S, Prabhash K, Basu S (2017) Clinical Response Profile of Metastatic/Advanced Pulmonary Neuroendocrine Tumors to Peptide Receptor Radionuclide Therapy with 177Lu-DOTATATE. Clin Nucl Med 42(6):428–435
Author information
Authors and Affiliations
Corresponding authors
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG
About this chapter
Cite this chapter
Daddi, N., Tassi, V., Lupattelli, M., Minotti, V., Puma, F., Ferolla, P. (2018). Therapy for Locoregional Disease: Bronchi. In: Colao, A., Faggiano, A., de Herder, W. (eds) Neuroendocrine Tumors in Real Life. Springer, Cham. https://doi.org/10.1007/978-3-319-59024-0_19
Download citation
DOI: https://doi.org/10.1007/978-3-319-59024-0_19
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-59022-6
Online ISBN: 978-3-319-59024-0
eBook Packages: MedicineMedicine (R0)