Abstract
The imaging targets of bone scintigraphy are all changes of bone metabolism independent of its underlying pathology. The technical background of this imaging method will be explained briefly. The use of bone scintigraphy in connection with some selected but frequent clinical questions and entities will be outlined concerning the results of bone scintigraphy in each entity. In addition, limitations of bone scintigraphy with technetium-99m (Tc-99m)-labeled diphosphonates and a comparison to other imaging modalities will be presented.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
The imaging targets of bone scintigraphy are all changes of bone metabolism independent of its underlying pathology. The technical background of this imaging method will be explained briefly. The use of bone scintigraphy in connection with some selected but frequent clinical questions and entities will be outlined concerning the results of bone scintigraphy in each entity. In addition, limitations of bone scintigraphy with technetium-99m (Tc-99m)-labeled diphosphonates and a comparison to other imaging modalities will be presented.
5.1 Introduction
The skeleton including bone and its joints can be affected by a broad variety of disorders ranging from inflammation, benign and malignant bone tumors, bone metastases from other organs to disorders diffusely affecting bone due to changes of bone metabolism. Examples of such disorders affecting bone metabolism are osteoporosis, osteomalacia, renal osteodystrophy, or hyperthyroidism. The diagnostic approach to these bone pathologies starts with the medical history and physical examination, as in general by other organ systems, as well. However, a closer insight by physical examination into bone pathology cannot be done easily. Bone biopsy may be necessary in some circumstances to obtain information whether, e.g., an unclear pathological bone lesion is of benign or malignant origin, an information essential ahead in case of possible surgery. However, biopsies of bone are an invasive and time-consuming procedure, not to mention possible complications such as pain, bleeding, or infection. Thus, in most cases imaging results will be the easiest way to access an insight view of bone and in order to set up a diagnosis, as the different disorders reveal typical pathological changes by imaging. Various imaging modalities of bone are available in daily routine (conventional X-ray, computed tomography, magnetic resonance imaging, osteodensitometry, bone scintigraphy). Whereas conventional X-ray, computed tomography, and magnetic resonance imaging reveal information about the morphological aspects of bone and bony disorders, bone scintigraphy gives an insight into the metabolic changes associated with the different disorders. In this respect bone scintigraphy has a particular position in imaging, which stands not in competition to the other morphologically orientated bone imaging modalities; it can rather be seen as a method adding additional information.
The article will give a short introduction into the concepts of bone imaging by bone scintigraphy. Detailed information on bone scintigraphy including further indications, scintigraphic results, and diagnostic limitations can be found in specific literature [1,2,3,4,5,6,7,8,9,10].
5.2 Bone Scintigraphy: General Information
Radioisotopic bone scanning using technetium-99m-labeled phosphate and diphosphonate compounds, commonly called bone scintigraphy or bone scan, is a method of imaging metabolic changes of the skeleton. The nuclear medicine technique is sensitive to areas of unusual bone rebuilding activity, since the radiopharmaceutical is taken up by osteoblast cells which build bone. For a bone scan, the patient is injected with a small amount of a diphosphonate (most commonly methylene diphosphonate (MDP) is used), which is labeled with technetium-99m (Tc-99m) as a gamma-emitting radioactive material for tracer detection by a gamma camera (◘ Table 5.1). Diphosphonates can exchange places with bone phosphate in regions of active bone growth or bone metabolism, thus anchoring the radioisotope to that specific region. The patient can be scanned at different times, e.g., rapid imaging sequences just after injection of the radiopharmaceutical resembling the arterial perfusion phase, after a few minutes to visualize the extent of soft tissue perfusion, and after 2–4 h to image the bone phase (◘ Figs. 5.1 and 5.2). To view small lesions (less than 1 cm) – especially in the spine – the SPECT imaging technique may be required. The method has assumed major clinical importance to some bone pathologies, which will be outlined in the following section concerning the scintigraphic results. Other information in connection with these pathologies, such as epidemiology, pathology, radiological results, and course of disease, will be outlined only briefly in this chapter, if necessary for the understanding of the scintigraphic results. For further and broader information on these disorders, additional literature will have to be consulted.
5.3 Bone Disorders with Pathological Bone Scintigraphies
5.3.1 Primary Bone Tumors
Some but not all primary bone tumors, whether benign or malignant, show a pathological accumulation in bone scintigraphy. Bone scintigraphy can thus give information concerning the metabolic activity of the tumor and about whether or not additional pathological lesions are present in the skeleton. However, bone scintigraphy cannot give a conclusive information about the dignity of the tumor, as both benign and malignant bone tumors can show pathologically increased tracer accumulation (◘ Figs. 5.3 and 5.4). A list of tumors which reveals increased tracer accumulation is listed in ◘ Table 5.2.
5.3.2 Bone Metastases
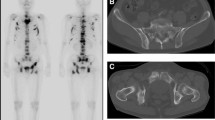
Different tumors such as breast cancer, prostate cancer, or lung cancer frequently develop bone metastases. Bone metastases with osteoblastic activity in bone scintigraphy show an increased tracer accumulation (◘ Fig. 5.5), whereas osteoclastic bone metastases in general reveal no scintigraphic abnormalities, as the tracer accumulation is mediated via the osteoblasts but not the osteoclasts. The exception will be large osteoclastic metastases which impose as «cold lesions» (◘ Fig. 5.6). In cases of diffusely spread bone metastases, the skeleton imposes with an increased tracer accumulation. As the complete tracer is bound and trapped in bone, the kidneys by which bone scintigraphic tracers are normally excreted within hours show no tracer accumulation. This scintigraphic appearance is called hyperscan (◘ Fig. 5.7). Although frequently seen in metastatic bone disease, the image of a hyperscan is not specific for metastatic bone disease, as it can also appear in cases of hypermetabolic bone disorders such as hyperthyroidism or hyperparathyroidism (see below).
5.4 Metabolic Bone Disorders
5.4.1 Osteoporosis
The decrease of bone mass and the reduction of bone strength, as by which osteoporosis is defined, cannot be visualized by bone scintigraphy. The reduction of bone mass can be measured by dual X-ray absorptiometry (DXA), and the morphological changes of bone including fractures can be imaged by different radiological methods (e.g., X-ray, computed tomography, high-resolution computed tomography). However, bone scintigraphy can be of clinical use in osteoporosis, as not all fractures can be visualized by radiology (occult fractures). After falls non-dislocated fractures are often overseen with conventional radiological methods such as X-rays, although the patients report on persistent pain or difficulties to walk. With bone scintigraphy increased tracer accumulation occurs due to bone hypermetabolism in the area of the fracture. The typical scintigraphic pattern seen in association with fractures is a linear hypermetabolic lesion (◘ Fig. 5.8).
5.4.2 Osteomalacia
Although bone scintigraphy is not the method of choice to diagnose osteomalacia, the disease reveals some signs in bone scintigraphy. In severe disease bones show deformities such as bending of long bones, and an accentuation of tracer accumulation in the cortical region of long bones can frequently be visualized (◘ Fig. 5.9).
5.4.3 Primary Hyperparathyroidism
Bone turnover is accelerated in hyperparathyroidism which can be seen in bone scintigraphy as an increased tracer accumulation in particular in the skull and the central skeleton accompanied with a decreased or missing visualization of the kidneys (hyperscan) (◘ Fig. 5.10).
In severe disease brown tumors can occur which usually show an increased tracer accumulation with bone scintigraphy. This can potentially be misled as bone tumors or bone metastases.
5.4.4 Renal Osteodystrophy
Tracer accumulation can be increased or decreased, and no typical scintigraphic features are associated with renal osteodystrophy. Usually also scintigraphic features as seen with osteomalacia, osteoporosis, or primary hyperparathyroidism can be found in patients with renal osteodystrophy. In general scintigraphy provides no relevant additional information in this metabolic bone disease.
5.4.5 Hyperthyroidism
In patients with clinical hyperthyroidism, bone turnover is extensively increased with an acceleration of bone formation and bone resorption. This increased bone turnover can be visualized by bone scintigraphy revealing a diffusely increased tracer accumulation in the whole skeleton, thus producing the image of a hyperscan (increased tracer accumulation in the whole skeleton but no visualization of the kidneys as no tracer is excreted) (◘ Fig. 5.10). This scintigraphic pattern can be also seen in patients with diffuse bone metastases (◘ Fig. 5.7).
5.4.6 Paget’s Disease of Bone
Paget’s disease of bone is a chronic disorder that can result in enlarged and misshapen bones caused by the excessive breakdown and formation of bone, followed by disorganized bone remodeling. This results in weak and misshapen bone prone to fracture, pain, and arthritis. Rarely, it can develop into a primary bone cancer known as Paget’s sarcoma. Often Paget’s disease is localized to one or only a few bones in the body. The skull, pelvis, femur, and lower lumbar vertebrae are the most commonly affected bones.
Paget’s disease can occur as monostotic or polyostotic and usually reveals an increased tracer accumulation within the affected bone (◘ Fig. 5.11).
Bone scintigraphy wherein the whole skeleton is scanned with one investigation is most useful in determining the extent and activity of the condition. If a bone scan suggests Paget’s disease, the affected bone(s) should be X-rayed to confirm the diagnosis.
5.4.7 Fibrous Dysplasia
Similar to Paget’s disease, also lesions of fibrous dysplasia can show an increased tracer accumulation. Although lesions of Paget’s disease usually show a more intense tracer accumulation in bone scintigraphy than fibrous dysplasia lesions, a clear differentiation between fibrous dysplasia and Paget’s disease by scintigraphic appearance is not possible. The differentiation can rather be made by means of localization and by other radiological methods such as X-ray or computed tomography. The major indication and value of bone scintigraphy is therefore similar to Paget’s disease, the scanning of the whole skeleton within one investigation for lesions of this hypermetabolic bone disorder.
5.5 Inflammation
5.5.1 Joint Inflammation
For the purpose of imaging joint inflammation, bone scintigraphy is usually performed in a three-phase technique with a rapid perfusion/arterial phase, delayed perfusion phase resembling soft tissue perfusion, and a late bone phase (see above). Tracer accumulation is usually not only described by optical appearance but also by a region of interest technique (ROI) with comparison of the affected joint (joint region with the similar contralateral region. In acute joint inflammation, all three phases reveal an increased tracer accumulation. In chronic joint inflammation, the arterial phase is usually normal, but the soft tissue and bone phase show pathological tracer accumulation around the affected joint (◘ Fig. 5.12).
5.5.2 Chronic Osteomyelitis
After complex fractures or orthopedic interventions, chronic osteomyelitis may develop. Bone scintigraphy can show the extent of inflammation within the bone cavity, the intensity of inflammation (◘ Fig. 5.13), or after antibiotic therapy the disappearance of inflammatory activity.
5.5.3 Degenerative Bone and Joint Changes
In particular within the spine or the large joints, an increased tracer accumulation can frequently be seen due to morphological changes of the joints (arthrosis) or pathological mechanical alterations of skeletal regions (e.g., scoliosis of the spine) (◘ Fig. 5.14). In general the increase of tracer accumulation in association with degenerative bone disease is mild to moderate, so scintigraphically in a differentiation to other focal bone pathologies such as inflammation or bone tumors, bone metastasis is possible.
5.5.4 Algodystrophy
Persistent pain or atrophy may occur after fracture within the fractured region or after surgery. Bone scintigraphy performed as three-phase scintigraphy reveals pathologic patterns in algodystrophy within the whole affected extremity, which permits the establishment of the diagnosis and extent of disturbance (◘ Fig. 5.15). The different patterns dependent on the time since the onset of symptoms are listed in ◘ Table 5.3.
5.6 Conclusion
Bone scintigraphy is a method which can easily be performed allowing to scan the whole skeleton on a metabolic level or to visualize pathological changes of defined regions including its perfusion and soft tissue accumulation. Various bone pathologies as outlined above show pathological changes. The strength of bone scintigraphy is a high sensitivity to detect pathological changes in bone metabolism; however, specificity is low. The differentiation between different pathologies can be established through different anatomical patterns of the pathological lesions seen, in combination with arterial perfusion and soft tissue accumulation adjacent to bone pathologies and to some extent by the intensity of tracer accumulation. Furthermore, scintigraphic results have to be matched with other radiological results and the clinical history of the patient. Putting all these information together, a diagnosis can frequently be established, by which bone scintigraphy can add important information of the metabolic level of the investigated pathologies.
Take-Home Message
Bone scintigraphy with technetium-99m (Tc-99m)-labeled diphosphonates is a sensitive method to image metabolic changes in bone; however, pathological tracer accumulation lacks specificity. In comparison to other imaging modalities of bone such as computed tomography and magnetic resonance imaging, bone scintigraphy is thus rather complementary to these morphologically orientated methods.
References
Avioli LV, Krane SM, editors. Metabolic bone disease and clinically related disorders. 3rd ed. San Diego: Academic Press; 1998.
Holder LE, Fogelman I, Collier BD, editors. An Atlas of planar and SPECT bone scans. 2nd ed. London: Martin Dunitz; 2000.
Elgazzar AH, editor. Orthopedic nuclear medicine. Berlin: Springer; 2004.
Hahn K, Bockisch A. Skelettsystem. In: Büll U, Schicha H, Biersack HJ, Knapp WH, Reiners C, Schober O, editors. Nuklearmedizin. Thieme, Stuttgart, 1999.
Mikosch P. Die Knochenszintigraphie in der Diagnostik metabolischer Knochenerkrankungen. Wien Med Wochenschr. 2004;154:119–26.
Ryan PJ, Fogelman I. Bone scintigraphy in metastatic bone disease. Sem Nucl Med. 1997;27:291–305.
Mari C, Catafau A, Carrio I. Bone scintigraphy and metabolic disorders. Q J Nucl Med. 1999;43:259–67.
Hendler A, Hershkop M. When to use bone scintigraphy. It can reveal things other studies cannot. Postgrad Med. 1998;104:54–66.
Cook GJ, Hannaford E, See M, Clarke SE, Fogelman I. The value of bone scintigraphy in the evaluation of osteoporotic patients with pack pain. Scand J Rheumatol. 2003;31:245–8.
Mikosch P, Pietschmann P, Kainberger F, Gallowitsch HJ, Lind P. Morbus Paget oder fibröse Dysplasie des Radius? Ein Fallbericht. Wien Med Wochenschr. 2001;151:295–9.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this chapter
Cite this chapter
Mikosch, P. (2017). Bone Imaging by Nuclear Medicine. In: Pietschmann, P. (eds) Principles of Bone and Joint Research. Learning Materials in Biosciences. Springer, Cham. https://doi.org/10.1007/978-3-319-58955-8_5
Download citation
DOI: https://doi.org/10.1007/978-3-319-58955-8_5
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-58954-1
Online ISBN: 978-3-319-58955-8
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)