Abstract
Resource planning plays a central role in health care. Especially when it comes to the healthcare workforce, planning is crucial in order to avoid shortages. Workforce planning takes place on different stakeholder levels and is based on different planning methodologies, namely supply-based, demand-based, needs-based models, and benchmarking. A challenge in applying any of these models, however, lies in dealing adequately with uncertainty by making plausible assumptions. Another weakness shared by all four models is that they are rooted in traditional care processes, as opposed to integrated, team-based, and partly digital models of care. Therefore, the article closes by highlighting some of the new approaches to workforce planning.
“Plans are worthless, but planning is everything”
(Dwight D. Eisenhower, 1957)
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
1 Introduction
1.1 The Need for Planning
Resource planning plays a central role in health care. There are many supplies which we consider essential to our daily lives, such as food, clothing, fuel etc. Nonetheless, there is no public planning of supermarkets, warehouses, or gas stations. Health care, however, is different: Firstly, there is a broad consensus in many societies that prices and volume in health services markets should not be determined (solely) by supply and demand as health is a fundamental human right (Dussault et al. 2010; WHO 2013). Equitable access to health care is deemed to be one of the central building blocks of that right (WHO 2013). Thus, in the context of this rights-based framework planning is required in order to allocate resources to health care by normative and ethical standards, and not simply market mechanisms.
Another reason for planning in health care is the need for excess capacity in order to be prepared for emergency situations. Since the time to treatment can be a decisive factor in emergencies, excess capacity for health care provision is necessary, especially in locations where it would not be efficient by market standards. That applies, for instance, to workforce planning: On the one hand, policymakers do not want to risk a shortage of health professionals which would put a timely provision of health care at risk. On the other hand, payer organizations and the (healthy) population seek to avoid a costly oversupply. Therefore, the challenge lies in estimating exactly the “right” number of health professionals required in the future. This is especially difficult for the physician workforce as medical education takes up to 15 years, meaning that forecasts have to be made for a considerable time span in order to bridge the time lag between recognizing a gap between supply and demand and being able to close that gap (Dussault et al. 2010).
1.2 Planning Taxonomy
The allocation of health care resources and the planning process can be looked at from a variety of angles:
-
By stakeholder: Who is planning?
-
By time frame: What time span does the planning process cover?
-
By geography: Which catchment area is covered?
-
By criteria: By what criteria and methodology are resources allocated?
-
By subject: Which resources are considered?
In terms of stakeholders, the responsibility for planning can lie with national, regional, and/or local governments. It can be devolved to public authorities (like the National Health Service (NHS) in the UK) or multi-stakeholder bodies (such as the Joint Federal Commission in Germany assembling insurers and providers) (Ono et al. 2013). It can also be up to insurers, provider organizations, or integrated care providers.
The time frame for planning varies widely based on the specific subject of planning. As elaborated above, modifying the intake of medical students is rather a long-term measure in order to influence the future number of available physicians. Changing the number of nurses in an intensive care unit, on the other hand, has an immediate effect on the quality of care.
Planning can take place on all geographical levels: Large pharmaceutical and medical technology companies, for instance, are serving the global market. Therefore, when the avian influenza virus H5N1 started to spread in the early 2000s, the World Health Organization (WHO) issued a recommendation to all governments to stockpile the antiviral drug Tamiflu® for at least 25% of its population. As many countries followed that recommendation, the license holder Roche ran into considerable shortages of the drug on a global level (Greene and Moline 2006). Many other planning activities take place on a national, regional or local level. Medical student intake, for instance, is determined at a national level in many Western countries (Bloor and Maynard 2003). Training posts for nurses, on the other hand, are either planned on a national, a regional level or not at all, as an overview by the Organisation for Economic Co-operation and Development (OECD) showed (Simoens et al. 2005). The planning process for a certain type of resource does not necessarily have to rest exclusively with one institution for a certain catchment area. Instead, there may be competing or coexisting organizations which are planning health care resources for the same catchment area. In the Netherlands, for instance, competing insurance companies sign contracts with different hospitals based on their own criteria—yet, all of the companies have to ensure adequate access to hospital care for their insured (Krabbe-Alkemade et al. 2017).
Planning criteria also differ immensely. Allocations of health care resources are planned to ensure accessibility in terms of quantity, quality, and an adequate distance. At the same time (cost) efficiency and profitability of health care institutions also plays an important role as resources are limited. The goals of service provision can easily contrast with financial objectives, requiring decisions between competing criteria. In addition, there are typically complex webs of regulatory requirements that need to be observed. In Germany, for instance, hospitals are subject to minimum-volume standards for certain complex surgeries, e.g., hospitals are required to demonstrate 20 liver transplantations and 50 knee arthroplasties per year in order to be allowed to perform the respective intervention (de Cruppé et al. 2015). On January 2016, a new law was enacted, which excludes those hospital services not meeting the standards from reimbursement (Art 136b para. 4 German Social Code V). In addition to the two sometimes competing criteria addressed above, insurers and providers are usually motivated to maintain positive reputations—both in terms of patient satisfaction and as employers. These considerations can also influence decisions on resource allocation.
Finally, the question of what is being planned is, of course, crucial for any of the variables mentioned before: There are various resources that are subject to planning: Infrastructure, such as hospitals, emergency care units, medical devices and further equipment need to be sufficiently available. Denmark, for instance, has recently sought to strengthen the efficiency and quality of its inpatient care by cutting the number of hospitals by at least half and re-building many older hospitals according to state-of-the-art equipment and technology (Møller Pedersen 2009). Schools and faculties for medical studies and other health care professions are also an important resource. In addition, budget planning plays an important role: Investments in infrastructure, technology, and human resources require sufficient levels of financial resources. However, in the largely publicly-owned or public policy-driven health care sector, funding may not necessarily be available when needed and be subject to political cycles (e.g., elections) and the general economic environment (as both taxes and contributions to the statutory health insurance suffer during an economic downturn).
Many of the examples cited above relate to workforce planning as it is one of the most central resources in health care—due to the fact that health care is highly labour-intensive (Baumol and De Ferranti 2012). The health care workforce includes a large variety of professions: medical doctors, dentists, nurses, midwives, physiotherapists, and many others—with each profession containing many different sub-specializations. These complexities make workforce planning a great challenge. At the same time, workforce planning is also difficult since human capital cannot be easily shifted from one location to another and their output is challenging to quantify. Therefore, this chapter will largely focus on workforce planning.
Workforce planning would be impossible without a sound estimate of patient numbers and interventions both for the present and the future. Understanding (future) demand is essential to avoid both excess capacities and shortages. Therefore, this aspect will also be looked at in more detail throughout this chapter.
2 Workforce Planning Methodologies
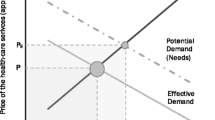
Workforce planning always pertains to two essential components: supply on the one hand, and demand/need on the other (Roberfroid et al. 2008). We require an estimate for both components in order to identify possible gaps between the two and define appropriate actions.
As straightforward as this model is—the crux of planning lies in the details. The selection of variables for the forecasting model, the size of the catchment area as well as the choice between forecasting either expected actual utilization of health care services or expected need for services are not only technically complex, but they also rely on fundamental normative assumptions regarding equity, access, and health system responsiveness.
This purpose of this section is to give a broad overview of the different methodologies and their pros and cons, especially as it relates to health workforce planning in an integrated care setting.
Researchers differentiate between four different methodologies of workforce planning (Roberfroid et al. 2008): Many workforce plans start by forecasting physician and/or non-physician workforce supply. Then there are demand-based and needs-based models projecting the population’s future health care requirements. A fourth approach to forecasting lies in benchmarking which relates to both, the supply and the demand side.
2.1 Planning of Supply
Supply analyses usually rely on a stock inflow-outflow model. Based on the current number of health workers (differentiated by specialty) the following drivers of future supply are quantified (Ono et al. 2013; Roberfroid et al. 2008):
-
Education: The number of graduates from medical studies, training posts for medical specializations, and figures for the various non-physician training programs (nurses, midwives, physician assistants, physiotherapists, etc.) need to be taken into account. In addition, their location should also be a matter of concern: Studies show that maintaining medical schools and training posts in or close to rural, remote or underserved areas increases the chance of a more equitable geographic distribution of staff (Laven and Wilkinson 2003; Wilson et al. 2009).
-
Migration: Immigration rates of health professionals from other countries and emigration of health professionals trained domestically need to be considered. Mobility within a country becomes relevant when workforce planning is to be applied to a certain region only.
-
Retirement and retention/attrition: The number of health professionals retiring from work as well as those leaving the medical field to work in other industries are decisive variables.
-
Productivity: The change in workload carried by health professionals is an important variable. Recently, this aspect has moved to the centre of attention, as the generation of so called “Millenials” is less willing to work long hours and puts greater emphasis on maintaining a work-life balance. Therefore, even with a stable headcount, overall productivity may decrease, so it becomes highly important to measure health professionals not in terms of headcount, but rather as full time equivalents (FTEs) (Ono et al. 2013). Ideally, FTEs should not be measured by the budgeted but rather by actual working hours. That is particularly relevant for physicians and other health professions who do not work on a salaried basis. As data on working hours is often unavailable, many forecasts estimate FTEs by benchmarking individual service provision against a peer group average (JAHWPF 2015; Roberfroid et al. 2008). Alternatively, productivity gains may be achieved through new treatment methods, higher quality of care (e.g., avoiding readmission), the use of technology (e.g., clinical decision support systems), and larger practice size with more efficient processes (Cunningham 2013). In a systematic review, Weiner et al. (2013) estimated that health information technology (IT)-supported workflow changes may lower the number of required physicians by 4–8% (assuming that 70% of physicians make full use of health IT available, such as electronic health records, and clinical decision support).
-
Delegation of tasks: Delegation of tasks from higher to lower qualified personnel as well as an increasing differentiation of health professions may significantly reduce the need for highly qualified professionals: Altschuler et al. (2012) modelled three different scenarios varying by the degree of delegation. Based on their models, they identified a potential for increasing panel sizes per physician (and team) by 40–100%. Weiner et al. (2013) estimated that health IT-induced delegation from specialists (SPs) to general practitioners (GPs) or from GPs to nurses may decrease the need for physicians by a total of 12–26% (again at 70% penetration).
The reliability of supply models is, of course, highly dependent on the reliability of these driver variables. While some of these input variables are fairly predictable or controllable, such as retirement rates or number of graduates, other variables are less reliable: Macroeconomic trends impacting the labour market, generational trends (such as “Millenials”), and the potential of health IT are difficult to accurately forecast. An important determinant for the reliability is the longevity of the forecast: In order to account for the uncertainties inherent in long-term forecasts, many workforce plans calculate multiple scenarios (Crettenden et al. 2014).
Another aspect to consider is the geographic area for which the supply model is estimated: Within the geographic area qualifications and degrees should be largely recognized and there should be a reasonable degree of mobility of health care professionals. Otherwise, the overall supply may appear sufficient but large geographic variations could arise.
2.2 Demand-Based Planning
The demand-based or utilization-based approach aims at projecting future demand for health care in the population. It is based on current and/or historical utilization data, e.g., from claims data, and tries to project that information into the future. Basic models only take into account demographics, however, there are also highly complex forecasting models in order to account for various dynamics:
-
Demographics: The change in size, age and sex structure of the population is the most common variable in demand projections. However, the impacts of these shifts are not always understood. For instance, it is up for debate whether the ageing of the population will lead to a compression or expansion of morbidity as there is evidence for both hypotheses (Crimmins and Beltran-Sanchez 2011; Fries et al. 2011). Therefore, the Swiss Health Care Observatory has, for instance, modeled separate scenarios for both hypotheses in its projections of health workforce requirements until 2030 (Seematter-Bagnoud et al. 2008).
-
Socioeconomics: People with a lower socioeconomic status suffer from higher morbidity and mortality rates that in turn lead to higher utilization of health care resources. There is mixed evidence on the level of health care utilization when controlling for morbidity: Shadmi et al. (2011) find no difference in utilization by socioeconomic status among the Israeli population when controlling for morbidity. Thode et al. (2005), on the other hand, conclude that persons with the same morbidity level but low socioeconomic status consult more GPs compared to people with a high socioeconomic status while the effect are reversed for SPs.
-
Technology: Health IT is accredited an enormous potential to fundamentally change the delivery of care. Not only could it affect the supply side (in terms of communication efficiency between health care providers), but it could also change communication and utilization patterns between health care providers and patients. Weiner et al. (2013) concluded that health IT may decrease physician demand as it enables more self-care and it allows for asynchronous care. This might reduce physician demand by 4–11% (at 70% penetration rate of health IT) (Weiner et al. 2013).
-
Health System Changes: Health system variables have an important influence on utilization. For instance, limitations on direct access to certain providers or changes in the patients’ benefits package have a good chance of influencing (supplier-induced) demand. One example is gatekeeping: Gatekeeping is generally thought to have the potential to optimize patient pathways, thereby leading to fewer unnecessary visits to SPs. In a systematic review, Garrido et al. (2011) found a decrease in specialized care utilization and mixed evidence on the effect of gatekeeping on overall ambulatory care. Thus, if regulators chose to introduce (or incentivize) gatekeeping, this may have an impact on the demand for health services. Another example for the effect of a change in the benefits package is the reimbursement of chemotherapy drugs in the US: As of 2004, the Medicare Prescription Drug, Improvement, and Modernization Act cut payment rates for chemotherapy drugs administered to Medicare patients after Congress realized there had been a significant overpayment for certain drugs. Prices for some drugs were reduced by as much as 90%. In consequence, Jacobson et al. (2010) showed that prescription patterns of physicians changed while overall access to chemotherapy was not hampered.
-
Insurance Status: Data from the United States show that utilization rates of health care vary significantly by insurance status (Bureau of Health Professions 2008): Namely, patients with “traditional” insurance contracts remunerating physicians on a fee-for-service basis displayed significantly higher levels of service use as opposed to patients enrolled in Health Maintenance Organizations (HMOs). That gap was even more apparent when comparing these figures to those that are uninsured: For instance, service use levels for surgery and internal medicine was between to three- to fivefold higher for people in traditional contracts compared to uninsured persons (Bureau of Health Professions 2008). Therefore, the reduction in number of uninsured persons resulting from the Affordable Care Act is expected to impact physician demand (Petterson et al. 2012). In addition, the US is one of the most dynamic health care markets when it comes to provider models. Medicare as well as private insurers have experimented with new models of care, e.g., through HMOs, Accountable Care Organizations (ACOs), Patient-Centered Medical Homes (PCMH), and Preferred Provider Organizations. These models are aimed at managing the patient and his or her pathway through the health care system and realigning provider incentives accordingly. Therefore, they have a significant impact on the required number of health professionals (Weiner 2004; Weiner et al. 1986). As the share of the population registered in these different provider models has seen relevant fluctuations, demand forecasts also need to take these changes into account.
The fundamental critique of demand-based models lies in the fact that current levels of health care utilization are strongly influenced by current supply levels and structure: A shortage of locally accessible physicians may lead to lower utilization in ambulatory care and, possibly, in a higher number of hospitalizations (Ozegowski and Sundmacher 2014; Sundmacher and Kopetsch 2014). An oversupply of physicians may, as explained above, induce higher utilization than “objectively” needed. Remuneration systems are also known to have a considerable effect on utilization of care: Fee-for-service models increase utilization, while health systems with capitation or salary-based remuneration usually have lower utilization rates (Gosden et al. 2000). Quarterly lump-sum fees might induce physicians to set the next appointment for their patients for the next quarter even when a lower (or higher) frequency would be appropriate.
Therefore, demand-based models have a tendency to reproduce current levels of over- or under-supply rather than estimating an optimal allocation of resources.
2.3 Needs-Based Planning
Needs-based planning is an attempt to overcome the problems rooted in demands-based models and, therefore, takes a fundamentally different approach.
The United States’ Graduate Medical Education National Advisory Committee (GMENAC), which undertook one of the most comprehensive efforts in setting up a needs-based model, defined ‘need’ as “that quantity of medical services which expert medical opinion believes ought to be consumed over a relevant time period in order for its members to remain or become as healthy as possible given by existing medical knowledge” (GMENAC 1980, 5). This definition implies that there is a “right” level and type of health care services for each patient and that these decisions are not made by the patient him- or herself but rather by an “objective” medical expert.
In order to arrive at a needs-based estimation of health care services, it is necessary to approximate the morbidity of the population, the type and complexity of care (per provider) required for each morbidity, and to project future changes in both morbidity and (evidence-based) health care service provision.
Case Example 1
The GMENAC was chartered from 1976 to 1980 by the US Department of Health and Human Services to develop such an approach. The committee was comprised of 22 health care experts and it was supported by more than 300 consultants (McNutt 1981). Its goal was to estimate physician requirements for 23 different specialty groups as of 1990. In order to do so it set up Delphi panels for each physician specialty group consisting of 8–10 experts with different professional backgrounds. Each of these Delphi panels applied the following methodology (GMENAC 1980):
-
It identified the incidence and prevalence of the major diseases based on epidemiological data;
-
it determined the relevance of each disease for the specific specialty based on utilization data and expert judgment;
-
it projected the changes in morbidity for each disease considered until the year 1990 based on changes in population size and (age- and sex-specific) structure;
-
it adjusted for known measurement problems;
-
it took into account the “knowledge of the realities of provider and consumer behavior” (GMENAC 1980, 11), i.e., supplier- or patient-induced over-supply as well as undersupply from unmet needs, e.g., due to the limited ability to pay;
-
it added a lump sum for the diseases which were not considered specifically.
These steps left each panel with an estimation of the burden of disease relevant for the health system. In the next step it converted these figures into resource requirements:
-
It estimated the number and time of required units of care;
-
it adjusted these findings by assumptions on increased potential for delegation of services to non-physician practice staff;
-
it estimated physician productivity.
Thereby, each panel arrived at an estimation of the number of physicians required for each specialty. In order to account for the uncertainties in the model, the panels phrased their outcome in terms of a range of required physicians. The size of these ranges oscillated between ±1% (hematology/oncology) and ±25% (psychiatry) (own calculations based on GMENAC 1980, 22). Overall, the committee came to the conclusion that there would be a 15% surplus in physicians by 1990 and a 30% surplus by 2000.
The GMENAC was chartered from 1976 to 1980 by the US Department of Health and Human Services to forecast future physician supply requirements based on a needs-based planning approach. In a complex process that took more than three years to be completed it developed an analytical framework based on projecting changes in morbidity and applied it to all major physician specialties (see Case Example 1 for further details). The GMENAC findings led to an outcry at the time of publication and have been questioned by stakeholders (Reinhardt 1981). Harris (1986) brought forward many examples where the GMENAC projections were significantly off the reality (e.g., with regards to HIV, caesarean sections, etc.). Especially since the 2000s, many feared a shortage of physicians rather than a 30% surplus, mainly due to an expected surge in demand and lower productivity per physician (Cooper 1995; Weiner 2002). Nonetheless, the GMENAC work has remained the largest effort in implementing an (adjusted) needs-based model to date. The physician-patient ratios the GMENAC predicted are still used by providers today despite the heavy criticism and the fact that they were only updated once in 1990 (Camden Group 2011).Footnote 1
2.4 Benchmarks
A fourth approach to workforce planning is benchmarking. Benchmarks are formulated in terms of physician-population ratios, nurse-population ratios or other ratios of health professionals set in relation to the population. The degree of refinement of benchmarks can vary immensely: On the broadest level there may be a health workforce-to-population ratio. On a very refined level, it is possible to derive benchmarks for each specialty health professional group in relation to age- and sex-specific population cohorts.
There are various sources for benchmarks: The GMENAC ratios are still used, as mentioned above. Other benchmarks have been retrieved from HMOs or hospital referral regions (Goodman et al. 1996). A clear advantage of benchmarks is that they are simple to use and easy to apply. Also they may avert some of the problems rooted in demand-based models: Namely, demand-based models usually rest on the assumption that current utilization and supply levels reflect optimal care, without proving that assumption. Benchmarks, on the other hand, are drawn from integrated care systems which are deemed best practice (e.g., HMOs), from national average ratios or they rely on scientific evidence (e.g., GMENAC ratios). These benchmark staff ratios are then applied to the specific setting of the workforce planner, possibly after being modified to reflect the specificities of the setting. While this approach is easy to implement, it also has its disadvantages: Benchmarks show an immense variation based on their source. Therefore, the choice of the “right” benchmark is highly critical. Weiner (2004) compared three different HMOs (Kaiser Permanente, Group Health Cooperative, HealthPartners) against the national US average health workforce density. Despite adjustments for differences in demographics and services provided, HMO ratios ranged between 62% and 86% (primary care physicians), 63% and 71% (specialist physicians), and 63% and 93% (nonphysician health professionals) compared to the US average. In an older survey of 54 HMOs, Dial et al. (1995) also reported wide variations in physician-population ratios between HMOs and identified the HMO size to be one of the critical determinants for staffing ratios: HMOs with more than 80,000 enrollees were much more homogeneous in their physician-to-population ratios than were smaller ones. In a more recent comparison between nine patient-centred medical homesFootnote 2 (PCMH), Patel et al. (2013) found a variation in panel sizes from 625 to 2500. Even within one HMO (Kaiser Permanente), differences in panel sizes between sites were reported due to different models of care (Neuwirth et al. 2007).
Therefore, the use of benchmarks is certainly helpful as it reduces complexity of planning. However, the applicability of a benchmark ratio should be critically reviewed when used in a different setting.
2.5 Limitations of Current Planning Approaches in Integrated Care Settings
Despite the extensive research and practical experience, workforce planning remains a difficult task. The fundamental challenge to workforce planning is that it is subject to a large degree of uncertainty. Planning models have dealt with that uncertainty by applying one of two available strategies: They have either used very simple models, e.g., benchmarks or rules of thumb, which were then adjusted in the daily operations or timeline models extrapolating future trends based on past levels of physician demand and supply (Dial et al. 1995). A second strategy is to build complex models assessing all possible influencing variables and requiring the planner to make assumptions for those variables that are uncertain. An example of that is the needs-based approach.
A study estimating the future need for otolaryngologists in the US has illustrated these challenges: Applying the demand-based model by the US Bureau of Health Professionals, the needs-based model according to the GMENAC methodology, and benchmarks from different HMOs, Anderson et al. (1997) resulted in a large variability of results both within and between models. Each model could predict both, a considerable shortage or a considerable oversupply of otolaryngologists, based on the precise assumptions and despite the fact that the forecasting period of six years was rather short. Similarly, in a retrospective analysis of different forecasts, Roberfroid et al. (2009) found considerable margins of error between forecast and reality. This underlines that workforce planning will never become an exact science but should be seen as a dynamic process requiring regular re-evaluation in light of actualities.
A second challenge in these modelling approaches arises with respect to integrated care: These models are rooted in systems with a single physician at the nexus of care. Hence these planning models attempt to estimate the “right” number of each physician specialty and non-physician provider separately. This ignores the fact that many patients suffer from multiple chronic conditions requiring team-based approaches to care. Dial et al. (1995) showed that the model of care played a large role for staffing levels of HMOs: HMOs with fewer primary care physicians had a much higher ratio of advanced practice nurses in comparison, and vice versa. Thus, applying the primary care physician ratio of one HMO to another setting may be very misleading if the models of care are different.
Thirdly, recent changes in models of care also involve a shift in the physician-patient relationship which in turn clashes with some of the planning models outlined above (Institute of Medicine 2001). The needs-based planning model in particular is rooted in a paternalistic notion of the physician-patient relationship: It is the physician who determines by “objective” criteria the “projected biologic requirements” (GMENAC 1980, 6) of patients. Taking into account patients’ preferences and subjectively perceived needs, which is standard in a physician-patient relationship with shared decision making, is in clear contradiction to that planning model.
3 New Approaches to Workforce Planning in Integrated Care
In order to address these limitations, new approaches have evolved over the past several years. With regard to integrated care, the techniques applied by managed care-based provider models, such as HMOs and PCMHs, are of interest.
3.1 Team-Based Workforce Planning
As outlined above, modelling the demand for single professional groups has serious limitations in an integrated care setting. As integrated care relies on the notion of sharing the patient across different professional groups—both physicians and non-physicians—according to the specific qualification of each professional role, the team-based model of care also needs to be reflected in workforce planning. The Veterans Health Administration in the US has adopted such a team-based planning model. Each team consists of 1 FTE primary care practitioner (PCP) and a support staff of 2.17 FTE (such as registered nurses, pharmacists, medical assistants, etc.) and is expected to handle a panel size of 1200 patients of an average case-mix. However, teams with larger support staff are encouraged: For every additional (reduced) 10% of FTE support staff, panel sizes are expected to increase (decrease) by 2.5%. If the PCP is not a medical doctor, but a nurse practitioner or physician assistant, expected panel sizes are decreased by 25% (Department of Veterans Affairs 2009). These benchmarks have been collected over time from the Veterans Health Administration.
Are these benchmarks applicable to other providers? A comparison of several studies of integrated healthcare delivery systems showed that the fraction of primary care visits handled by nurse practitioners varied between 9 and 70% (Green et al. 2013). Such large ranges are also found for advanced practice nurses (Grover and Niecko-Najjum 2013). These variations clearly illustrate that it can be very misleading to pick out benchmarks for just one professional group from an integrated healthcare delivery system. Instead, the benchmarks can only be reliably copied when the entire model of care is comparable.
Another challenge for learning from international best practices in team-based workforce planning lies in the differences in regulatory requirements. In the US, for instance, each state has different regulatory requirements for non-physician professionals, which makes workforce planning and transferability of proven models of care rather difficult (Grover and Niecko-Najjum 2013). In Germany, both regulatory and political aspects play a large role when it comes to non-physician health care professionals: There is strong opposition to a greater differentiation of health workforce qualifications. Especially the Physicians’ Chamber and the Federal Association of SHI Physicians fear that physicians may lose their exclusive right to the vast set of tasks that they perform today, and that they might in conjunction have to render a share of their budget to other professional groups. Therefore, the recent setup of academic programs for physician assistants has been met by an outcry by the Federal Association of SHI Physicians (Beerheide 2014). In that context, workforce planning becomes a real challenge: On the one hand, the Associations of SHI Physicians have the obligation (as public institutions) to ensure adequate access to outpatient care, which is a challenge for primary care in many rural areas. On the other hand, the associations represent the political interests of outpatient care physicians and, therefore, combat any changes that (seemingly) dilute current privileges of physicians.
3.2 Pro-active Management of Health Care Utilization
The application of managed care instruments, such as gatekeeping, case management/panel management, disease management, and financial incentives, plays a large role in patient pathways and influences actual utilization patterns. Kaiser Permanente has, for instance, developed the concept of total panel ownership which advocates a proactive role for primary care teams in identifying unmet patient needs (Livaudais et al. 2006; Neuwirth et al. 2007). GroupHealth, an integrated care provider based in Seattle (US), piloted a project in 2006 in which it significantly reduced panel sizes for primary care physicians, extending the time physicians spent with each patient by 50%, and introducing further care modules, such as Chronic Care Management, to its model of care. These reforms resulted in a significant decrease in emergency care visits, an increase in patient satisfaction, and a decrease in total costs compared to other GroupHealth sites (Reid et al. 2010).
Another important factor is the degree of integration, e.g., whether long-term care providers and social services are also part of the system. Montefiore Medical Center, which serves 500,000 residents in the Bronx, one of the poorest urban communities in the United States, has tightly integrated health and social care services (Chase 2010). It considers this as one of its key success factors as it shifts demand from physicians to nurses and social workers, which conserves physician resources and is expected to be more sustainable in the long-term.
Finally, during the 1990s and early 2000s, many HMOs struggled with significant wait times for their patients, which both hurt their reputation as a provider among patients and as an employer among health professionals (Murray and Berwick 2003). In response, the model of “advanced access” (or “open access”) was developed. It was based on queuing theory which shows that transferring work to the future leads to inefficiencies. Thus, advanced access rejects appointment-based practice management and triage systems and, instead, relies on the idea of “doing today’s work today” (Murray and Berwick 2003). Any patient who calls for an appointment is offered an appointment on the same day with his or her preferred provider. Implementing advanced access has significant consequences for panel sizes and, thus, workforce planning (Murray et al. 2007). However, empirical results of advanced access are mixed: While some provider-specific studies reported significant improvements in workforce productivity (Lewandowski et al. 2006), a systematic review reported mixed results on patient satisfaction and patient outcomes (Rose et al. 2011). Thus, it remains to be seen to what degree advanced access models will be implemented in the future.
3.3 Tackling Geographic Variations Through Technology
The use of technology and its (future) impact on health services has been commented on several times. One of its potentials lies in alleviating problems related to the geographic location of health care providers. A recent Cochrane systematic review illustrated that interactive telemedicine can substitute for face-to-face care while health outcomes remain comparable to usual care or improved (Flodgren et al. 2015). Structured telephone support, telemonitoring and text messaging have also shown to improve outcomes compared to usual care (Free et al. 2013; Inglis et al. 2010).
Kaiser Permanente Hawaii introduced two new elements in its delivery system: (1) an electronic health record to facilitate communication and coordination between health professionals, and (2) telephone access and secure messaging services between patients and their PCP. An initial study revealed that the number of total office visits decreased by 26% within three years; at the same time, scheduled phone calls and secure messaging rose considerably (Chen et al. 2009). Overall, ambulatory care contacts rose by 8% within the 3-year study period. Unfortunately, as the study did not include a control group, it remains unknown whether previously unmet needs were addressed by the new delivery model. Also, possible effects on process or outcomes quality were not assessed. However, this study and the systematic reviews cited above illustrate that the importance of geographic vicinity for service delivery may be reduced through the use of technology. This also impacts workforce planning: If patients need to visit their health care provider less frequently, longer travel times may be acceptable, which in turn allows for larger catchment areas in the planning process. In fact, if certain services no longer require face-to-face visits, geographic vicinity would no longer be a constraint for these services/providers.
4 Conclusion
Planning, especially workforce planning, has been high on the agenda of health policy makers, practitioners, and researchers for the past 40 years. Various methods have been developed and become more and more refined. Recent changes to models of care have again called into question much of the established methodologies. That applies in particular to integrated care where clearly specified tasks for single practitioners are replaced by a team-based, pro-active approach to care delivery.
Where does that leave us in terms of planning? I propose four key lessons:
-
1)
Setting objectives and standards of care
-
Before making a plan, it is central to formulate the objectives and minimum service level standards of the specific delivery system—either in terms of structural and process indicators (such as minimum service level standards, geographic catchment areas, or maximum wait times), and/or in terms of health outcomes. This step is essential for assessing the performance of a plan—especially, if we accept the hypothesis that demand for health care services is infinite and will thus never be fully met.
-
2)
Aligning planning approaches with the specific model of care
-
As we have seen, there is not one perfect methodology for workforce planning. A number of methodologies exist all of which have their pros and cons. The chosen planning approach and in particular the use of benchmarks should be tightly linked to the specified objectives, the specific model of care, and its particular setting.
-
3)
Monitor and adapt constantly
-
Workforce planning is not a one-time exercise, but should be seen as a dynamic process which serves to (1) set a baseline for the required (human) resources at the start, and (2) on a meta level establish an agreement on the objectives of the delivery system and consistently verify and re-negotiate that agreement. Once adopted, the assumptions made in the workforce plan should be monitored against reality and adapted accordingly.
-
4)
Integrated care calls for integrated planning
-
Integrated care moves away from the narrow focus on physicians as the central providers of health care, makes extensive use of technology, and aims for patient-centred, proactive models of care. Such a fundamental change in the understanding of health care also implies a fundamental change in workforce planning: It requires team-based, integrated planning approaches, it involves taking into account all the available communication channels, and it implies a shift of resources towards care coordination as well as fast and easy access to primary care in order to avert unnecessary utilization of highly-specialized (and often costly) care providers.
Notes
- 1.
To the merit of the GMENAC, it should also be said that the US health care system is probably one of the most difficult for which to forecast physician supply requirements. First of all, it is a very large country with many different subcultures affecting health demand and patient preferences. Secondly, the provider structure is highly fragmented leaving providers with very different abilities in managing patient demand.
- 2.
PCMH is a model of care from the United States which puts primary care in the centre and rests on the notion of transforming health care structures to ensure patient-centred, accessible, and coordinated health care (Agency for Healthcare Research and Quality, n.d.).
References
Agency for Healthcare Research and Quality. (n.d.). Defining the PCMH. Retrieved February 28, 2016, from https://pcmh.ahrq.gov/page/defining-pcmh
Altschuler, J., Margolius, D., Bodenheimer, T., & Grumbach, K. (2012). Estimating a reasonable patient panel size for primary care physicians with team-based task delegation. Annals of Family Medicine, 10(5), 396–400.
Anderson, G. F., Han, K. C., Miller, R. H., & Johns, M. E. (1997). A comparison of three methods for estimating the requirements for medical specialists: The case of otolaryngologists. Health Services Research, 32(2), 139–153.
Baumol, W. J., & De Ferranti, D. M. (2012). The cost disease: Why computers get cheaper and health care doesn’t. London: Yale University Press.
Beerheide, R. (2014). Scharfe Kritik an neuen Studiengängen. Ärzte Ztg. Retrieved October 18, 2015, from http://www.aerztezeitung.de/politik_gesellschaft/berufspolitik/article/861854/substitution-scharfe-kritik-neuen-studiengaengen.html
Bloor, K., & Maynard, A. (2003). Planning human resources in health care: Towards an economic approach. An international comparative review. Ottawa: Canadian Health Services Research Foundation. Retrieved October 18, 2015, from http://www.chsrf.ca/Migrated/PDF/ResearchReports/CommissionedResearch/bloor_report.pdf
Bureau of Health Professions. (2008). The physician workforce: Projections and research into current issues affecting supply and demand (p. 111). Retrieved October 20, 2015, from http://bhpr.hrsa.gov/healthworkforce/supplydemand/medicine/physiciansupplyissues.pdf
Camden Group (2011). Final physician needs assessment. Report as of July 2010. Bellingham, Washington. Retrieved October 20, 2015, from http://www.whatcomalliance.org/wp-content/uploads/2011/02/Camden1-28-11.pdf
Chase, D. (2010). Montefiore medical center: Integrated care delivery for vulnerable populations. Case study. The Commonwealth Fund, 53(1448). Retrieved October 20, 2015, from http://www.commonwealthfund.org/~/media/files/publications/case-study/2010/oct/1448_chase_montefiore_med_ctr_case_study_v2.pdf
Chen, C., Garrido, T., Chock, D., Okawa, G., & Liang, L. (2009). The Kaiser Permanente electronic health record: Transforming and streamlining modalities of care. Health Affairs, 28(2), 323–333.
Cooper, R. A. (1995). Perspectives on the physician workforce to the year 2020. Journal of the American Medical Association, 274(19), 1534–1543.
Crettenden, I. F., McCarty, M. V., Fenech, B. J., Heywood, T., Taitz, M. C., & Tudman, S. (2014). How evidence-based workforce planning in Australia is informing policy development in the retention and distribution of the health workforce. Human Resources for Health, 12, 7.
Crimmins, E. M., & Beltran-Sanchez, H. (2011). Mortality and morbidity trends: Is there compression of morbidity? The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 66B(1), 75–86.
Cunningham, R. (2013). Health workforce needs: Projections complicated by practice and technology changes. Issue Brief George Washington University. National Health Policy Forum., 851, 1–15.
de Cruppé, W., Malik, M., & Geraedts, M. (2015). Minimum volume standards in German hospitals: Do they get along with procedure centralization? A retrospective longitudinal data analysis. BMC Health Services Research, 15.
Department of Veterans Affairs (2009). VHA handbook 1101.02: Primary care management module (PCMM). Washington, DC. Retrieved October 18, 2015, from http://www.va.gov/vhapublications/ViewPublication.asp?pub_ID=2017
Dial, T. H., Palsbo, S. E., Bergsten, C., Gabel, J. R., & Weiner, J. (1995). Clinical staffing in staff- and group-model HMOs. Health Affairs, 14(2), 168–180.
Dussault, G., Buchan, J., Walter, S., & Padaiga, Z. (2010). Assessing future health workforce needs. Retrieved October 20, 2015, from http://www.euro.who.int/__data/assets/pdf_file/0019/124417/e94295.pdf
Flodgren, G., Rachas, A., Farmer, A. J., Inzitari, M., & Shepperd, S. (2015). Interactive telemedicine: Effects on professional practice and health care outcomes. In The Cochrane Collaboration (Ed.), Cochrane database of systematic review. Chichester: Wiley.
Free, C., Phillips, G., Galli, L., Watson, L., Felix, L., Edwards, P., et al. (2013). The effectiveness of mobile-health technology-based health behaviour change or disease management interventions for health care consumers: A systematic review. PLoS Medicine, 10(1), e1001362.
Fries, J. F., Bruce, B., & Chakravarty, E. (2011). Compression of morbidity 1980–2011: A focused review of paradigms and progress. Journal of Aging Research, 2011, 1–10.
Garrido, M. V., Zentner, A., & Busse, R. (2011). The effects of gatekeeping: A systematic review of the literature. Scandinavian Journal of Primary Health Care, 29(1), 28–38.
GMENAC (1980). Report of the graduate medical education national advisory committee to the secretary, department of health and human services: Vol. II. Modeling, research, and data technical panel (p. 348). Hyattsville, MD: The US American Graduate Medical Education National Advisory Committee. Report No. HRA-81-652. Retrieved October 20, 2015, from http://eric.ed.gov/?id=ED203766
Goodman, D. C., Fisher, E. S., Bubolz, T. A., Mohr, J. E., Poage, J. F., & Wennberg, J. E. (1996). Benchmarking the US physician workforce: An alternative to needs-based or demand-based planning. Journal of the American Medical Association, 276(22), 1811–1817.
Gosden, T., Forland, F., Kristiansen, I., Sutton, M., Leese, B., Giuffrida, A., et al. (2000). Capitation, salary, fee-for-service and mixed systems of payment: Effects on the behaviour of primary care physicians. Cochrane Database of Systematic Review, 3, CD002215.
Green, L. V., Savin, S., & Lu, Y. (2013). Primary care physician shortages could be eliminated through use of teams, nonphysicians and electronic communication. Health Affairs, 32(1), 11–19.
Greene, J., & Moline, K. (2006). The bird flu pandemic: Can it happen? Will it happen? How to protect yourself and your family if it does (1st ed.). New York: Thomas Dunne Books.
Grover, A., & Niecko-Najjum, L. M. (2013). Primary care teams: Are we there yet? Implications for workforce planning. Academic Medicine, 88(12), 1827–1829.
Harris, J. E. (1986). How many doctors are enough? Health Affairs, 5(4), 73–83.
Inglis, S. C., Clark, R. A., McAlister, F. A., Ball, J., Lewinter, C., Cullington, D., et al. (2010). Structured telephone support or telemonitoring programmes for patients with chronic heart failure. Cochrane Database of Systematic Review, 8, CD007228.
Institute of Medicine (2001). Crossing the quality chasm: A new health system for the 21st century. Washington, DC: National Academy Press.
Jacobson, M., Earle, C. C., Price, M., & Newhouse, J. P. (2010). How medicare’s payment cuts for cancer chemotherapy drugs changed patterns of treatment. Health Affairs, 29(7), 1391–1399.
JAHWPF (2015). Handbook on health workforce planning – methodologies across EU countries. Release 1. Retrieved October 20, 2015, from http://euhwforce.weebly.com/uploads/2/3/0/5/23054358/d052_-_handbook_on_planning_methodologies_-_release_1.pdf
Krabbe-Alkemade, Y. J. F. M., Groot, T. L. C. M., & Lindeboom, M. (2017). Competition in the Dutch hospital sector: An analysis of health care volume and cost. European Journal of Health Economics, 18(2), 139–153.
Laven, G., & Wilkinson, D. (2003). Rural doctors and rural backgrounds: How strong is the evidence? A systematic review. The Australian Journal of Rural Health, 11(6), 277–284.
Lewandowski, S., O’Connor, P. J., Solberg, L. I., Lais, T., Hroscikoski, M., & Sperl-Hillen, J. M. (2006). Increasing primary care physician productivity: A case study. The American Journal of Managed Care, 12(10), 573–576.
Livaudais, G., Unitan, R., & Post, J. (2006). Total panel ownership and the panel support tool--“It’s all about the relationship”. The Permanente Journal, 10(2), 72–79.
McNutt, D. R. (1981). GMENAC: Its manpower forecasting framework. American Journal of Public Health, 71(10), 1116–1124.
Møller Pedersen, K. (2009). Restructuring & modernizing the hospital sector. Health Policy Monitor. Retrieved October 20, 2015, from http://www.hpm.org/survey/dk/a13/5
Murray, M., & Berwick, D. M. (2003). Advanced access: reducing waiting and delays in primary care. Journal of the American Medical Association, 289(8), 1035–1040.
Murray, M., Davies, M., & Boushon, B. (2007). Panel size: How many patients can one doctor manage? Family Practice Management, 14(4), 44–51.
Neuwirth, E. B., Schmittdiel, J. A., Tallman, K., & Bellows, J. (2007). Understanding panel management: A comparative study of an emerging approach to population care. The Permanente Journal, 11(3), 12–20.
Ono, T., Schoenstein, M., & Lafortune, G. (2013, June). Health workforce planning in OECD countries: A review of 26 projection models from 18 countries (Report No. 62). Retrieved October 20, 2015, from http://www.oecd-ilibrary.org/social-issues-migration-health/health-workforce-planning-in-oecd-countries_5k44t787zcwb-en
Ozegowski, S., & Sundmacher, L. (2014). Understanding the gap between need and utilization in outpatient care—The effect of supply-side determinants on regional inequities. Health Policy, 114(1), 54–63.
Patel, M. S., Arron, M. J., Sinsky, T. A., Green, E. H., Baker, D. W., Bowen, J. L., et al. (2013). Estimating the staffing infrastructure for a patient-centered medical home. The American Journal of Managed Care, 19(6), 509–516.
Petterson, S. M., Liaw, W. R., Phillips, R. L., Rabin, D. L., Meyers, D. S., & Bazemore, A. W. (2012). Projecting US primary care physician workforce needs: 2010–2025. Annals of Family Medicine, 10(6), 503–509.
Reid, R. J., Coleman, K., Johnson, E. A., Fishman, P. A., Hsu, C., Soman, M. P., et al. (2010). The group health medical home at year two: Cost savings, higher patient satisfaction, and less burnout for providers. Health Affairs, 29(5), 835–843.
Reinhardt, U. E. (1981). The GMENAC forecast: An alternative view. American Journal of Public Health, 71(10), 1149–1157.
Roberfroid, D., Leonard, C., & Stordeur, S. (2009). Physician supply forecast: Better than peering in a crystal ball? Human Resources for Health, 7, 10.
Roberfroid, D., Stordeur, S., Camberlin, C., Van de Voorde, C., Vrijens, F., & Léonard, C. (2008). Physician workforce supply in Belgium: Current situation and challenges. Health Services Research (HSR). Brussels: Belgian Health Care Knowledge Centre (KCE). Retrieved October 20, 2015, from https://kce.fgov.be/sites/default/files/page_documents/d20081027309.pdf
Rose, K. D., Ross, J. S., & Horwitz, L. I. (2011). Advanced access scheduling outcomes: A systematic review. Archives of Internal Medicine, 171(13), 1150–1159.
Seematter-Bagnoud, L., Junod, J., Ruedin, H. J., Roth, M., Foletti, C., & Santos-Eggimann, B. (2008). Offre et recours aux soins médicaux ambulatoires en Suisse - Projections à l’horizon 2030. Neuchâtel: Schweizerisches Gesundheitsobservatorium (Obsan). Retrieved October 20, 2015, from http://www.obsan.admin.ch/sites/default/files/publications/2015/arbeitsdokument-33.pdf
Shadmi, E., Balicer, R. D., Kinder, K., Abrams, C., & Weiner, J. P. (2011). Assessing socioeconomic health care utilization inequity in Israel: Impact of alternative approaches to morbidity adjustment. BMC Public Health, 11(1), 609.
Simoens, S., Villeneuve, M., & Hurst, J. (2005). Tackling nurse shortages in OECD countries (OECD Health Working Papers Report No. 19). Retrieved October 20, 2015, from http://www.oecd-ilibrary.org/social-issues-migration-health/tackling-nurse-shortages-in-oecd-countries_172102620474
Sundmacher, L., & Kopetsch, T. (2014). The impact of office-based care on hospitalizations for ambulatory care sensitive conditions. European Journal of Health Economics, 16(4), 365–375.
Thode, N., Bergmann, D. E., Kamtsiuris, P., & Kurth, B.-M. (2005). Einflussfaktoren auf die ambulante Inanspruchnahme in Deutschland. Bundesgesundheitsblatt Gesundheitsforsch Gesundheitsschutz, 48(3), 296–306.
Weiner, J. P. (2002). A shortage of physicians or a surplus of assumptions? Health Affairs, 21(1), 160–162.
Weiner, J. P. (2004). Prepaid group practice staffing and U.S. physician supply: Lessons for workforce policy. Health Affairs. Suppl Web Exclusives:W4-43-59.
Weiner, J. P., Steinwachs, D. M., & Williamson, J. W. (1986). Nurse practitioner and physician assistant practices in three HMOs: Implications for future US health manpower needs. American Journal of Public Health, 76(5), 507–511.
Weiner, J. P., Yeh, S., & Blumenthal, D. (2013). The impact of health information technology and e-health on the future demand for physician services. Health Affairs, 32(11), 1998–2004.
WHO. (2013). The right to health. Retrieved October 20, 2015, from http://www.who.int/mediacentre/factsheets/fs323/en/
Wilson, N. W., Couper, I. D., De Vries, E., Reid, S., Fish, T., & Marais, B. J. (2009). A critical review of interventions to redress the inequitable distribution of healthcare professionals to rural and remote areas. Rural and Remote Health, 9(2), 1060.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this chapter
Cite this chapter
Ozegowski, S. (2017). Planning. In: Amelung, V., Stein, V., Goodwin, N., Balicer, R., Nolte, E., Suter, E. (eds) Handbook Integrated Care. Springer, Cham. https://doi.org/10.1007/978-3-319-56103-5_12
Download citation
DOI: https://doi.org/10.1007/978-3-319-56103-5_12
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-56101-1
Online ISBN: 978-3-319-56103-5
eBook Packages: Business and ManagementBusiness and Management (R0)