Abstract
Stent thrombosis is a rare complication of percutaneous coronary intervention and carries a poor prognosis. Recent improvements in stent technology and new antiplatelet therapies have reduced the incidence of stent thrombosis.
Coronary stent thrombosis has been defined by the Academic Research Consortium criteria. Four types of thrombosis are defined according to the time of occurrence from stent implantation: acute (<24 h), subacute (<30 days), late (between 1 month and 1 year), and very late (>1 year). Management consists primarily of urgent restoration of antegrade coronary flow. The concurrent management of platelet aggregation is of paramount importance; compliance with the regimen should be confirmed and a possible resistance to the selected antiplatelet agent should be excluded.
Coronary angiography is limited to determination of the causes of thrombosis. Intracoronary imaging, particularly optical coherence tomography (OCT), can identify the underlying pathology in most cases, allowing selection of the most appropriate management. By employing OCT, a number of pathologies such as malapposition, rupture of neoatherosclerosis, uncovered struts, restenosis, evagination, underexpansion, and dissection of the borders have been identified as risk factors for coronary stent thrombosis, allowing causal and specific treatments. Recommended duration of antiplatelet therapy is regulated by current European Society of Cardiology and American Heart Association/American College of Cardiology guidelines.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
One of the most serious complications of percutaneous coronary intervention (PCI) is stent thrombosis (ST). It can be difficult, or even impossible, to detect ST in routine clinical practice early on, ideally before it induces an acute coronary syndrome presentation with permanent ST-segment elevation myocardial infarction (STEMI) or less frequently with non-ST-segment elevation myocardial infarction (NSTEMI) [1]. ST also represents an important cause of sudden cardiac death [2]. Pathological mechanisms leading to ST are multifactorial. In this chapter, we review ST definitions, incidences, and predictive factors, and then focus on the diagnosis and management of ST.
2 Nomenclature and Definitions
In 2007, The Academic Research Consortium (ARC) proposed the following consensus classification of ST [3] (► Box 59.1):
-
Definite: Angiographic confirmation of the presence of a thrombus that originates in the stent or in the segment 5 mm proximal or distal to the stent, and presence of myocardial ischemia criteria or confirmation of stent thrombosis at autopsy.
-
Probable: Considered to have occurred after intracoronary stenting in case of any unexplained death within the first 30 days or any myocardial infarction that is related to documented acute ischemia in the territory of the implanted stent without angiographic confirmation of stent thrombosis and in the absence of any other obvious cause.
-
Possible: Considered to have occurred with any unexplained death from 30 days after intracoronary stenting until the end of trial follow-up.
Depending on the time of the occurrence, stent thrombosis has been categorized into the following four types:
-
Acute: 0 to 24 h after stent implantation
-
Subacute: >24 h to 30 days after stent implantation
-
Late: >30 days to 1 year after stent implantation
-
Very late: >1 year after stent implantation

3 Epidemiology
Over the past several decades, a large body of data on ST has accumulated. Generally, «definite and probable stent thrombosis» has been classified as ST in the literature.
-
The rate of early ST for bare-metal stents (BMSs) ranged between 10% and 15% before the era of dual antiplatelet therapy (DAPT) with aspirin and ticlopidin. Following introduction of DAPT, the incidence of early ST has dropped to less than 1% [4]. The most recent data on early, late, and very late ST suggest rates of 2.1% at 1 month and 2.4% at 1 year in the BVS EXAMINATION study [5]; at 3 years, this rate increases to 2.6% [6].
-
As far as drug-eluting stents (DESs) are concerned, first-generation DESs must be differentiated from second-generation DESs. First-generation DESs, designed to reduce the restenosis rate of BMSs, have been associated with higher ST rates than BMSs, largely due to late and very late ST probably caused by failed re-endothelialization of the struts, positive arterial remodeling, and early neoatherosclerosis. This issue was a main topic of the 2006 European Society Congress «Black Sunday» at which Camenzind et al. presented data documenting the excess risk of mortality associated with use of first-generation DESs. One of the positive results of this debate was the agreement to standardize the definition of the diagnostic criteria of ST, which were subsequently formulated and published by the ARC [3]. Currently, the ST rate for first-generation DES stents is estimated at 2.2% [7] at 3 years. For second-generation DESs, the estimated ST rates are 0.3% at 1 month and 1.4% at 1 year in the BVS EXAMINATION study [5], and 1.7% at 3 years [6].
The availability of DESs with a biocompatible polymer or biodegradable polymer coating has been associated with significantly lower ST incidence compared with first-generation DESs [8]. According to the most recent data, it appears that the lowest ST rates are associated with implantation of the latest generation of DESs such as the platinum-chromium everolimus-eluting stent (PtCr-EES), the hybrid sirolimus-eluting stent (H-SES), and the cobalt-chromium everolimus-eluting stent (CoCr-EES) [9].
-
As far as bioresorbable stents (BVSs) are concerned, current studies suggest ST rates of 1.8% at 1 month, 2.3% at 6 month, and 3.0% at 1 year. Thus, ST rates for BVSs appear to be higher than those for the latest DESs [9]. To date, no long-term data regarding the ST of bioresorbable stents have been published.
4 Predictors and Mechanisms
Numerous risks factors for ST have been identified and can be classified according to (1) the patient’s characteristics, (2) the characteristics of the treated lesion, (3) the characteristics of the procedure, (4) the characteristics of the type of stent, and (5) the characteristics of the antiplatelet therapy. Overlap between these various classes of risk factors can occur.
-
Patient-related risk factors
Numerous biological and clinical parameters can induce an excess risk of ST caused by increased thrombogenicity. Hence, for example, diabetes [10, 11] and renal failure [2] are associated with higher rates of late ST.
The initial clinical context of the stent implantation is also important; hence, acute coronary syndrome (ACS) is associated with a higher ST rates [10, 11] and excess mortality. In this context, independent risk factors include no-reflow, reduced left ventricular ejection fraction, neoplasia, anemia, and a stent diameter smaller than 3 mm [2, 12]. In addition, individual resistance to antiplatelet therapies [13], mainly to clopidogrel, has been also correlated with increased ST rates.
-
Treated lesion-related risk factors
Predictive factors for ST reported in the literature include a long target lesion [14] and, specifically for BVSs, a small diameter of the target vessel (≤2.5 mm), possibly associated with underexpansion of the BVS [15]. Furthermore, type C complex lesions according to the American College of Cardiology/American Heart Association (ACC/AHA) classification, ostium lesions [10], lesions involving a bifurcation [2, 10], and coronary artery vein graft lesions [14] have also been associated with increased ST rates [14]. Excess risk of ST has also been reported in patients with ACS [14], possibly as a result of secondary thrombus resolution, coronary artery wall remodeling, and potentially primary malapposition [16]. According to the expert’s consensus [17], malapposition is present when the axial distance between the strut’s surface and the luminal surface is greater than the strut thickness.
-
Procedure-related risk factors
Technical risk factors for ST include the length of the implanted stent [11] and a suboptimal angiographic result characterized by final low minimal lumen diameter (MLD). For late and very late ST, endocoronary imaging studies such as intravascular ultrasound (IVUS) and optical coherence tomography (OCT) revealed higher ST rates in cases of stent underexpansion [18], malapposition [19, 20], and uncovered struts [20]. In cases of early ST, endocoronary imaging also incriminated malapposition [21], stent underexpansion [21], and edge dissection [22]. In addition, an excess risk of ST has been reported in segments with stent overlap [1].
-
Risk factors related to the type of stent
Follow-up after stenting has related ST to healing failure of the coronary wall, especially in cases with late and very late ST. Indeed, any of the stent features can become a potential source of impaired healing and, consequently, of ST. For example, thicker struts have been correlated with healing failure, as assessed by OCT [7], and with increased ST rates [23].
As far as the polymer used is concerned (durable, biodegradable, or absence of polymer), recent data show the superiority of the latest generation of durable polymers compared with biodegradable polymers (although the latter remain superior to the first generation of durable polymers) [8]. Hence, second-generation DESs such as the CoCr-EES have demonstrated a decrease in ST rates compared with BMSs [24], even in patients with STEMI [25].
Stent fractures have also been shown to increase ST rates [9].
-
Risk factors related to antiplatelet therapies:
DAPT plays a major role in the incidence of ST. Premature discontinuation of antiplatelet therapy is the strongest predictive factor for ST [2, 11, 15, 26]. The duration of antiplatelet therapy after stent implantation is controversial and remains a matter of scientific debate. Some studies, such as the DAPT study (12 versus 30 months of antiplatelet therapy), showed a decrease in ST rates at the cost of an increase in moderate to severe bleeding complications [27]. Unlike the DAPT study, other studies did not show any excess of ST rates, despite the discontinuation of DAPT after 30 days [26]. Currently, American [28] and European guidelines [29] recommend a duration of DAPT of 1 month after BMS implantation and 6 months after DES implantation in stable ischemic heart disease. In patients with ACS treated with BMS or DES implantation, DAPT should be given for at least 12 months [28, 29].
The pharmacology of the platelet anti-aggregating molecule used is also important. Hence, the new P2Y12 receptor blockers have shown a reduction in ST compared with clopidogrel (TRITON-TIMI 38 study for prasugrel [30] and PLATO for ticagrelor [31]). This difference can be partly explained by the concept of resistance to clopidogrel, which can occur in up to 44% of cases and results in a triple risk of ST [32]. Nevertheless, several cases of prasugrel resistance have been also reported [33].
Risk factors for ST differ depending on whether early or late ST is being considered. Hence, stent undersizing, uncovered dissections, nonoptimal flow at the end of the procedure, presence of a stable intermediate lesion proximally or distally to the culprit lesion, presence of a neoplasia, and use of a DES are independent risk factors for early ST [1]. In cases with late ST [1], stent undersizing, neoplasia, stable intermediate lesion proximally to the culprit lesion, peripheral coronaropathy, diabetes, bifurcation lesions or long stented segments, and younger age of the patients are more frequent.
5 Diagnostic Evaluations
ST is primarily diagnosed by coronary angiography. In the majority of cases, the clinical presentation is ACS. In a report from the US CathPCI Registry, among 7100 patients with cases of ST identified during a 16-month follow-up period, approximately 60% presented with STEMI, 23% with NSTEMI, and 17% with unstable angina [34]. At the time of coronary angiography, most patients had complete thrombotic occlusion (TIMI flow grade 0) of the involved vessel. A diagnosis of definite ST on the coronary angiogram is considered as the presence of a thrombus that originates in the stent or within a segment 5 mm proximal or distal to the stent, with or without vessel occlusion.
Patient prognosis with ACS secondary to ST is less favorable than in patients with ACS of a native artery. Consequently, an emergency coronary angiography must be performed in all patients with PCI for whom the diagnosis of ST has been considered.
In the case of complete thrombotic occlusion, thrombus aspiration could help to obtain a TIMI 3 coronary flow. Successful reperfusion rates seemed to be lower in patients with ST than in patients with de novo coronary thrombosis; ST was also accompanied by higher rates of distal embolization and major adverse cardiac or cerebrovascular events [35]. The periprocedural antithrombotic regimen, including the use of parenteral antiplatelet and anticoagulant therapies, does not differ from that recommended for patients with acute STEMI [29].
It is always important to evaluate the antiplatelet therapy regimen at the time of the ST and to search for potential resistance to clopidogrel and noncompliance.
6 Management of Stent Thrombosis
There are no specific standardized recommendations regarding ST PCI management. Nevertheless, different therapeutic approaches have been suggested, depending on the specific mechanism of the ST. For example, postdilatations have been suggested for treatment of underdeployment rather than stent-in-stent stenting [29].
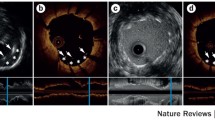
Unfortunately, X-ray coronary angiography does not differentiate between the various mechanisms of ST. Thus, to determine the cause of ST, endocoronary imaging is mandatory (◘ Fig. 59.1). IVUS was the first endocoronary imaging technique used to study the pathological mechanisms of very late ST.
In 2010, Lee et al. published in the Journal of the American College of Cardiology a series of 30 cases of very late ST (23 DES and 7 BMS) analyzed with IVUS [36]. No cases of BMS malapposition were found, although malapposition was present and potentially responsible in 73% of DES cases. The very late BMS thromboses were related to neointimal rupture. Representing a more recent concept, in 2011 Nakazawa et al. highlighted the presence and importance of neoatherosclerosis, which develops at a later stage following coronary stent implantation and can then rupture and induce thrombosis. This neoatherosclerosis seems to appear earlier in DESs than in BMSs [37]. Nevertheless, IVUS imaging is limited because of its lower spatial resolution in the range of 100 μm, depending on the imaging frequency of the probe, and does not seem to be the optimum tool for study of the underlying pathology, particularly if strut coverage or a malapposition [38] are of concern (◘ Fig. 59.2).
Endoluminal imaging employing OCT features a resolution that is approximately ten times higher than that of IVUS. OCT has become the principal tool for studying the pathological mechanisms of ST and guiding therapy. OCT allows detailed analysis of the stents and potential complications such as strut malapposition (a malapposed strut is defined as a strut with a measured distance between its surface and the adjacent vessel surface greater than the thickness of the strut plus polymer), failure of strut coverage (an uncovered strut is defined as a strut with neointimal hyperplasia thickness of 0 μm), coronary evagination (defined as the presence of an outward bulge in the luminal vessel contour between apposed struts, with the maximum depth of the bulge exceeding that of the thickness), underexpansion (underexpansion is defined by the ratio of the stent minimal surface to the reference surface lumen being <80%), defect of the neointimal strut coverage, upstream or downstream dissection to the stent, presence of neoatherosclerosis, rupture of a plaque, and endoluminal thrombus. OCT also allows differentiation of the red thrombus, which generates the shadow cone of the fibrin plug.
Based on OCT findings, identification of the causes of the ST provides guidance for management. Thrombus aspiration, adjustment of the medical treatment, stent implantation, or a balloon postdilatation may be considered.
Two recent studies by Miayazaki et al. [39] and Guagliumi et al. [40] compared OCT analyses of patients with thrombosed stents to a control thrombosis-free group. Both studies evidenced that there are significantly more uncovered and malapposed struts in the group of patients with ST.
Kang SJ et al. studied patients with late thrombosed stents, both after DES and BMS (33 stents) implantation [41]. In this study, OCT evidenced a rupture of neoatherosclerosis in all patients with a thrombosed BMS and in 70% of patients with DES. A limitation of this study was that the OCT was performed without thrombus aspiration; however, in the presence of a large thrombotic load, OCT was difficult to interpret. Nevertheless, rupture of the neoatherosclerosis appears to be one of the major causes of very late ST. Considering the «aging» of the implanted stents, increased prevalence of ST has to be expected in the future and OCT represents the reference diagnostic tool for evaluating causes of ST and the primary tool for guiding treatment, particularly in the case of rupture [42, 29] (◘ Fig. 59.3).
Thrombosis of a bare stent at the end of the mid-segment of the right coronary artery 2 years after implantation and discontinuation of antiplatelet therapy. OCT helped to find a fibrin plug hanging on uncovered struts. Patient medically treated. Red asterisks: thrombus. White arrow: uncovered struts
The causes of ST seem to differ according to the time to thrombosis. Indeed, underexpansion seems to be more frequent in patients with subacute ST compared with late or very late ST [43].
Two multicenter studies have recently validated the European Society of Cardiology (ESC) guideline recommendations.
Räber and colleagues studied the mechanisms of very late ST of DES (median time 4.7 years) [44]. Employing OCT, a mechanical cause was identified in more than 98% of cases in 58 patients. Malapposition was the most frequently identified cause of ST, followed by neoatherosclerosis and uncovered struts. Two major elements of malapposition evaluation using OCT emerged from this study: a malapposition distance greater than 300 μm on at least 1 mm length seem to be the most critical findings correlated with ST.
The PESTO multicenter study included 134 patients with ST [21]. Of these, 120 benefited from an OCT examination after thrombus aspiration. Very late ST was observed in 75% of cases. In 69% of cases, OCT was delayed (median lead time 4 days), which helped to discover a mechanical cause of the thrombosis in 97% of cases. The main causes of ST were malapposition (34%), rupture of neoatherosclerosis (22%), underdeployment (11%), uncovered struts (8%), and edge disease progression (8%).
In the PESTO study, following OCT evaluation of the target site, the therapeutic strategy was modified and adapted to the OCT findings by the operators. Medical treatment was selected in 32% of cases, redilatation in 37%, and stenting in 31%. These results differ from the NCDR register, where management was based on angiography; redilatation and stenting were systematically performed in all cases [34].
The following are treatment options based on OCT imaging:
-
Balloon postdilation in the case of malapposition or underexpansion
-
New stenting in the case of rupture of neoatherosclerosis or intrastent restenosis
-
Medical therapy for uncovered struts
Antiplatelet therapy has been related to ST, even very late ST. In the PESTO study, a recent change in antiplatelet therapy preceded ST in 22% of cases. It is now well established that continuation of DAPT beyond 1 year reduces the incidence of ST, but increases the risk of bleeding [27]. Longer duration of DAPT has to be discussed individually with all patients; in patients with low risk of bleeding, extension of DAPT beyond 1 year seems to be a reasonable treatment option (◘ Figs. 59.4 and 59.5).
Acute thrombosis on a drug-eluting stent by the ostium of LAD. Angiographic evolution: before angioplasty a, DES implantation b, angiographic result c, stent thrombosis d, after thrombus aspiration e. OCT showing an intimal dissection upstream of the stent (W, X) and presence of intrastent thrombus (Y)
7 Conclusion
Coronary ST is a rare complication of PCI with multifactorial causes. The improvements in coronary stents and antiplatelet therapy have reduced ST rates. OCT provides an excellent tool for guiding therapy in patients with ST by clearly defining the underlying pathology. Optimum strategies to match a specific underlying pathology with specific treatments have yet to be fully defined.
References
van Werkum JW, Heestermans AA, Zomer AC, Kelder JC, Suttorp M-J, Rensing BJ, Koolen JJ, Brueren BRG, Dambrink J-HE, Hautvast RW, Verheugt FW, ten Berg JM. Predictors of coronary stent thrombosis: the Dutch Stent Thrombosis Registry. J Am Coll Cardiol. 2009;53:1399–409.
Iakovou I, Schmidt T, Bonizzoni E, Ge L, Sangiorgi GM, Stankovic G, Airoldi F, Chieffo A, Montorfano M, Carlino M, Michev I, Corvaja N, Briguori C, Gerckens U, Grube E, Colombo A. Incidence, predictors, and outcome of thrombosis after successful implantation of drug-eluting stents. JAMA. 2005;293:2126–30.
Cutlip DE, Windecker S, Mehran R, Boam A, Cohen DJ, van Es G-A, Steg PG, Morel M, Mauri L, Vranckx P, McFadden E, Lansky A, Hamon M, Krucoff MW, Serruys PW, Consortium AR. Clinical end points in coronary stent trials: a case for standardized definitions. Circulation. 2007;115:2344–51.
Cutlip DE, Baim DS, Ho KK, Popma JJ, Lansky AJ, Cohen DJ, Carrozza JP, Chauhan MS, Rodriguez O, Kuntz RE. Stent thrombosis in the modern era: a pooled analysis of multicenter coronary stent clinical trials. Circulation. 2001;103:1967–71.
Brugaletta S, Gori T, Low AF, Tousek P, Pinar E, Gomez-Lara J, Scalone G, Schulz E, Chan MY, Kocka V, Hurtado J, Gomez-Hospital JA, Münzel T, Lee C-H, Cequier A, Valdés M, Widimsky P, Serruys PW, Sabaté M. Absorb bioresorbable vascular scaffold versus everolimus-eluting metallic stent in ST-segment elevation myocardial infarction: 1-year results of a propensity score matching comparison: the BVS-EXAMINATION study (bioresorbable vascular scaffold-a clinical evaluation of everolimus eluting coronary stents in the treatment of patients with ST-segment elevation myocardial infarction). JACC Cardiovasc Interv. 2015;8:189–97.
Kereiakes DJ, Yeh RW, Massaro JM, Driscoll-Shempp P, Cutlip DE, Steg PG, Gershlick AH, Darius H, Meredith IT, Ormiston J, Tanguay J-F, Windecker S, Garratt KN, Kandzari DE, Lee DP, Simon DI, Iancu AC, Trebacz J, Mauri L, Study Investigators DAPT. Stent thrombosis in drug-eluting or bare-metal stents in patients receiving dual antiplatelet therapy. JACC Cardiovasc Interv. 2015;8:1552–62.
Tada T, Byrne RA, Simunovic I, King LA, Cassese S, Joner M, Fusaro M, Schneider S, Schulz S, Ibrahim T, Ott I, Massberg S, Laugwitz K-L, Kastrati A. Risk of stent thrombosis among bare-metal stents, first-generation drug-eluting stents, and second-generation drug-eluting stents: results from a registry of 18,334 patients. JACC Cardiovasc Interv. 2013;6:1267–74.
Bangalore S, Toklu B, Amoroso N, Fusaro M, Kumar S, Hannan EL, Faxon DP, Feit F. Bare metal stents, durable polymer drug eluting stents, and biodegradable polymer drug eluting stents for coronary artery disease: mixed treatment comparison meta-analysis. BMJ. 2013;347:f6625.
Kang S-H, Chae I-H, Park J-J, Lee HS, Kang D-Y, Hwang S-S, Youn T-J, Kim H-S. Stent thrombosis with drug-eluting stents and bioresorbable scaffolds: evidence from a network meta-analysis of 147 trials. JACC Cardiovasc Interv. 2016;9:1203–12.
D’Ascenzo F, Bollati M, Clementi F, Castagno D, Lagerqvist B, de la Torre Hernandez JM, ten Berg JM, Brodie BR, Urban P, Jensen LO, Sardi G, Waksman R, Lasala JM, Schulz S, Stone GW, Airoldi F, Colombo A, Lemesle G, Applegate RJ, Buonamici P, Kirtane AJ, Undas A, Sheiban I, Gaita F, Sangiorgi G, Modena MG, Frati G, Biondi-Zoccai G. Incidence and predictors of coronary stent thrombosis: evidence from an international collaborative meta-analysis including 30 studies, 221,066 patients, and 4276 thromboses. Int J Cardiol. 2013;167:575–84.
Iqbal J, Sumaya W, Tatman V, Parviz Y, Morton AC, Grech ED, Campbell S, Storey RF, Gunn J. Incidence and predictors of stent thrombosis: a single-centre study of 5,833 consecutive patients undergoing coronary artery stenting. EuroIntervention. 2013;9:62–9.
Gross CM, Posch MG, Geier C, Olthoff H, Krämer J, Dechend R, Dietz R, Ozcelik C. Subacute coronary stent thrombosis in cancer patients. J Am Coll Cardiol. 2008;51:1232–3.
Aradi D, Kirtane A, Bonello L, Gurbel PA, Tantry US, Huber K, Freynhofer MK, ten Berg J, Janssen P, Angiolillo DJ, Siller-Matula JM, Marcucci R, Patti G, Mangiacapra F, Valgimigli M, Morel O, Palmerini T, Price MJ, Cuisset T, Kastrati A, Stone GW, Sibbing D. Bleeding and stent thrombosis on P2Y12-inhibitors: collaborative analysis on the role of platelet reactivity for risk stratification after percutaneous coronary intervention. Eur Heart J. 2015;36:1762–71.
Généreux P, Redfors B, Witzenbichler B, Maehara A, Yadav M, Weisz G, Francese DP, Parvataneni R, Brener SJ, Mehran R, Kirtane AJ, Stone GW. Angiographic predictors of 2-year stent thrombosis in patients receiving drug-eluting stents: insights from the ADAPT-DES study. Catheter Cardiovasc Interv. 2016;89:26–35.
Puricel S, Cuculi F, Weissner M, Schmermund A, Jamshidi P, Nyffenegger T, Binder H, Eggebrecht H, Münzel T, Cook S, Gori T. Bioresorbable coronary scaffold thrombosis: multicenter comprehensive analysis of clinical presentation, mechanisms, and predictors. J Am Coll Cardiol. 2016;67:921–31.
Karanasos A, Van Mieghem N, van Ditzhuijzen N, Felix C, Daemen J, Autar A, Onuma Y, Kurata M, Diletti R, Valgimigli M, Kauer F, van Beusekom H, de Jaegere P, Zijlstra F, van Geuns R-J, Regar E. Angiographic and optical coherence tomography insights into bioresorbable scaffold thrombosis: single-center experience. Circ Cardiovasc Interv. 2015;8:e002369. https://doi.org/10.1161/CIRCINTERVENTIONS.114.002369.
Tearney GJ, Regar E, Akasaka T, Adriaenssens T, Barlis P, Bezerra HG, Bouma B, Bruining N, Cho J, Chowdhary S, Costa MA, de Silva R, Dijkstra J, Di Mario C, Dudeck D, Falk E, Feldman MD, Fitzgerald P, Garcia H, Gonzalo N, Granada JF, Guagliumi G, Holm NR, Honda Y, Ikeno F, Kawasaki M, Kochman J, Koltowski L, Kubo T, Kume T, et al. Consensus standards for acquisition, measurement, and reporting of intravascular optical coherence tomography studies: a report from the international working group for intravascular optical coherence tomography standardization and validation. J Am Coll Cardiol. 2012;59:1058–72.
Aoki J, Lansky AJ, Mehran R, Moses J, Bertrand ME, McLaurin BT, Cox DA, Lincoff AM, Ohman EM, White HD, Parise H, Leon MB, Stone GW. Early stent thrombosis in patients with acute coronary syndromes treated with drug-eluting and bare metal stents: the acute catheterization and urgent intervention triage strategy trial. Circulation. 2009;119:687–98.
Cook S, Ladich E, Nakazawa G, Eshtehardi P, Neidhart M, Vogel R, Togni M, Wenaweser P, Billinger M, Seiler C, Gay S, Meier B, Pichler WJ, Jüni P, Virmani R, Windecker S. Correlation of intravascular ultrasound findings with histopathological analysis of thrombus aspirates in patients with very late drug-eluting stent thrombosis. Circulation. 2009;120:391–9.
Nakamura D, Attizzani GF, Toma C, Sheth T, Wang W, Soud M, Aoun R, Tummala R, Leygerman M, Fares A, Mehanna E, Nishino S, Fung A, Costa MA, Bezerra HG. Failure mechanisms and neoatherosclerosis patterns in very late drug-eluting and bare-metal stent thrombosis. Circ Cardiovasc Interv. 2016;9:e003785. https://doi.org/10.1161/CIRCINTERVENTIONS.116.003785.
Souteyrand G, Amabile N, Mangin L, Chabin X, Meneveau N, Cayla G, Vanzetto G, Barnay P, Trouillet C, Rioufol G, Rangé G, Teiger E, Delaunay R, Dubreuil O, Lhermusier T, Mulliez A, Levesque S, Belle L, Caussin C, Motreff P, Investigators PESTO. Mechanisms of stent thrombosis analysed by optical coherence tomography: insights from the national PESTO French registry. Eur Heart J. 2016;37:1208–16.
Prati F, Kodama T, Romagnoli E, Gatto L, Di Vito L, Ramazzotti V, Chisari A, Marco V, Cremonesi A, Parodi G, Albertucci M, Alfonso F. Suboptimal stent deployment is associated with subacute stent thrombosis: optical coherence tomography insights from a multicenter matched study. From the CLI foundation investigators: the CLI-THRO study. Am Heart J. 2015;169:249–56.
Kolandaivelu K, Swaminathan R, Gibson WJ, Kolachalama VB, Nguyen-Ehrenreich K-L, Giddings VL, Coleman L, Wong GK, Edelman ER. Stent thrombogenicity early in high-risk interventional settings is driven by stent design and deployment and protected by polymer-drug coatings. Circulation. 2011;123:1400–9.
Palmerini T, Biondi-Zoccai G, Della Riva D, Stettler C, Sangiorgi D, D’Ascenzo F, Kimura T, Briguori C, Sabatè M, Kim H-S, De Waha A, Kedhi E, Smits PC, Kaiser C, Sardella G, Marullo A, Kirtane AJ, Leon MB, Stone GW. Stent thrombosis with drug-eluting and bare-metal stents: evidence from a comprehensive network meta-analysis. Lancet Lond Engl. 2012;379:1393–402.
Sabate M, Cequier A, Iñiguez A, Serra A, Hernandez-Antolin R, Mainar V, Valgimigli M, Tespili M, den Heijer P, Bethencourt A, Vazquez N, Gómez-Hospital JA, Baz JA, Martin-Yuste V, van Geuns R-J, Alfonso F, Bordes P, Tebaldi M, Masotti M, Silvestro A, Backx B, Brugaletta S, van Es GA, Serruys PW. Everolimus-eluting stent versus bare-metal stent in ST-segment elevation myocardial infarction (EXAMINATION): 1 year results of a randomised controlled trial. Lancet Lond Engl. 2012;380:1482–90.
Naidu SS, Krucoff MW, Rutledge DR, Mao VW, Zhao W, Zheng Q, Wilburn O, Sudhir K, Simonton C, Hermiller JB. Contemporary incidence and predictors of stent thrombosis and other major adverse cardiac events in the year after XIENCE V implantation: results from the 8,061-patient XIENCE V United States study. JACC Cardiovasc Interv. 2012;5:626–35.
Yeh RW, Kereiakes DJ, Steg PG, Windecker S, Rinaldi MJ, Gershlick AH, Cutlip DE, Cohen DJ, Tanguay J-F, Jacobs A, Wiviott SD, Massaro JM, Iancu AC, Mauri L, Study Investigators DAPT. Benefits and risks of extended duration dual antiplatelet therapy after PCI in patients with and without acute myocardial infarction. J Am Coll Cardiol. 2015;65:2211–21.
Levine GN, Bates ER, Bittl JA, Brindis RG, Fihn SD, Fleisher LA, Granger CB, Lange RA, Mack MJ, Mauri L, Mehran R, Mukherjee D, Newby LK, O’Gara PT, Sabatine MS, Smith PK, Smith SC. 2016 ACC/AHA guideline focused update on duration of dual antiplatelet therapy in patients with coronary artery disease: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines: an update of the 2011 ACCF/AHA/SCAI guideline for percutaneous coronary intervention, 2011 ACCF/AHA guideline for coronary artery bypass graft surgery, 2012 ACC/AHA/ACP/AATS/PCNA/SCAI/STS guideline for the diagnosis and management of patients with stable ischemic heart disease, 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction, 2014 AHA/ACC guideline for the management of patients with non–ST-elevation acute coronary syndromes, and 2014 ACC/AHA guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery. Circulation. 2016;134:e123–55.
Authors/Task Force members, Windecker S, Kolh P, Alfonso F, Collet J-P, Cremer J, Falk V, Filippatos G, Hamm C, Head SJ, Jüni P, Kappetein AP, Kastrati A, Knuuti J, Landmesser U, Laufer G, Neumann F-J, Richter DJ, Schauerte P, Sousa Uva M, Stefanini GG, Taggart DP, Torracca L, Valgimigli M, Wijns W, Witkowski A. 2014 ESC/EACTS guidelines on myocardial revascularization: the task force on myocardial revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS) developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur Heart J. 2014;35:2541–619.
Montalescot G, Wiviott SD, Braunwald E, Murphy SA, Gibson CM, McCabe CH, Antman EM. TRITON-TIMI 38 investigators. Prasugrel compared with clopidogrel in patients undergoing percutaneous coronary intervention for ST-elevation myocardial infarction (TRITON-TIMI 38): double-blind, randomised controlled trial. Lancet Lond Engl. 2009;373:723–31.
Cannon CP, Harrington RA, James S, Ardissino D, Becker RC, Emanuelsson H, Husted S, Katus H, Keltai M, Khurmi NS, Kontny F, Lewis BS, Steg PG, Storey RF, Wojdyla D, Wallentin L, PLATO Investigators. Comparison of ticagrelor with clopidogrel in patients with a planned invasive strategy for acute coronary syndromes (PLATO): a randomised double-blind study. Lancet Lond Engl. 2010;375:283–93.
Buonamici P, Marcucci R, Migliorini A, Gensini GF, Santini A, Paniccia R, Moschi G, Gori AM, Abbate R, Antoniucci D. Impact of platelet reactivity after clopidogrel administration on drug-eluting stent thrombosis. J Am Coll Cardiol. 2007;49:2312–7.
Fiore M, Horovitz A, Pons A-C, Leroux L, Casassus F. First report of a subacute stent thrombosis in a prasugrel resistant patient successfully managed with ticagrelor. Platelets. 2014;25:636–8.
Armstrong EJ, Feldman DN, Wang TY, Kaltenbach LA, Yeo K-K, Wong SC, Spertus J, Shaw RE, Minutello RM, Moussa I, Ho KKL, Rogers JH, Shunk KA. Clinical presentation, management, and outcomes of angiographically documented early, late, and very late stent thrombosis. JACC Cardiovasc Interv. 2012;5:131–40.
Chechi T, Vecchio S, Vittori G, Giuliani G, Lilli A, Spaziani G, Consoli L, Baldereschi G, Biondi-Zoccai GGL, Sheiban I, Margheri M. ST-segment elevation myocardial infarction due to early and late stent thrombosis a new group of high-risk patients. J Am Coll Cardiol. 2008;51:2396–402.
Lee CW, Kang S-J, Park D-W, Lee S-H, Kim Y-H, Kim J-J, Park S-W, Mintz GS, Park S-J. Intravascular ultrasound findings in patients with very late stent thrombosis after either drug-eluting or bare-metal stent implantation. J Am Coll Cardiol. 2010;55:1936–42.
Nakazawa G. Stent thrombosis of drug eluting stent: pathological perspective. J Cardiol. 2011;58:84–91.
Alfonso F, Dutary J, Paulo M, Gonzalo N, Pérez-Vizcayno MJ, Jiménez-Quevedo P, Escaned J, Bañuelos C, Hernández R, Macaya C. Combined use of optical coherence tomography and intravascular ultrasound imaging in patients undergoing coronary interventions for stent thrombosis. Heart Br Card Soc. 2012;98:1213–20.
Miyazaki S, Hiasa Y, Takahashi T, Yano Y, Minami T, Murakami N, Mizobe M, Tobetto Y, Nakagawa T, Chen P-M, Ogura R, Miyajima H, Yuba K, Hosokawa S, Kishi K, Ohtani R. In vivo optical coherence tomography of very late drug-eluting stent thrombosis compared with late in-stent restenosis. Circ J Off J Jpn Circ Soc. 2012;76:390–8.
Guagliumi G, Sirbu V, Musumeci G, Gerber R, Biondi-Zoccai G, Ikejima H, Ladich E, Lortkipanidze N, Matiashvili A, Valsecchi O, Virmani R, Stone GW. Examination of the in vivo mechanisms of late drug-eluting stent thrombosis: findings from optical coherence tomography and intravascular ultrasound imaging. JACC Cardiovasc Interv. 2012;5:12–20.
Kang S-J, Lee CW, Song H, Ahn J-M, Kim W-J, Lee J-Y, Park D-W, Lee S-W, Kim Y-H, Mintz GS, Park S-W, Park S-J. OCT analysis in patients with very late stent thrombosis. JACC Cardiovasc Imaging. 2013;6:695–703.
Amabile N, Souteyrand G, Ghostine S, Combaret N, Slama MS, Barber-Chamoux N, Motreff P, Caussin C. Very late stent thrombosis related to incomplete neointimal coverage or neoatherosclerotic plaque rupture identified by optical coherence tomography imaging. Eur Heart J Cardiovasc Imaging. 2014;15:24–31.
Parodi G, La Manna A, Di Vito L, Valgimigli M, Fineschi M, Bellandi B, Niccoli G, Giusti B, Valenti R, Cremonesi A, Biondi-Zoccai G, Prati F. Stent-related defects in patients presenting with stent thrombosis: differences at optical coherence tomography between subacute and late/very late thrombosis in the Mechanism Of Stent Thrombosis (MOST) study. EuroIntervention. 2013;9:936–44.
Taniwaki M, Radu MD, Zaugg S, Amabile N, Garcia-Garcia HM, Yamaji K, Jørgensen E, Kelbæk H, Pilgrim T, Caussin C, Zanchin T, Veugeois A, Abildgaard U, Jüni P, Cook S, Koskinas KC, Windecker S, Räber L. Mechanisms of very late drug-eluting stent thrombosis assessed by optical coherence tomography. Circulation. 2016;133:650–60.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Souteyrand, G., Combaret, N., Amabile, N., Motreff, P. (2018). Coronary Stent Thrombosis. In: Lanzer, P. (eds) Textbook of Catheter-Based Cardiovascular Interventions. Springer, Cham. https://doi.org/10.1007/978-3-319-55994-0_59
Download citation
DOI: https://doi.org/10.1007/978-3-319-55994-0_59
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-55993-3
Online ISBN: 978-3-319-55994-0
eBook Packages: MedicineMedicine (R0)