Abstract
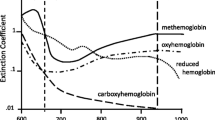
Pulse oximetry is a noninvasive technique to estimate the arterial oxygen saturation (SaO2) of hemoglobin. It is based on the differential absorption of light by oxyhemoglobin and deoxyhemoglobin. The oxygenated hemoglobin allows red light through and absorbs infrared light, while the deoxygenated hemoglobin allows infrared light through and absorbs more red light. A photodetector in the sensor measures unabsorbed light from the LEDs. Ratios of oxygenated to deoxygenated hemoglobin help calculate the saturation of hemoglobin in the arterial blood (SpO2).
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords

Fig. 8.1 Absorption spectra for oxyhemoglobin and reduced hemoglobin
Questions
-
1.
How is the pulse oximeter value obtained?
-
2.
What principle does it utilize?
-
3.
What is isosbestic point?
-
4.
What are the normal pulse oximeter values and how accurate is it?
-
5.
What are the common sources of error?
-
6.
What are the signs and symptoms of hypoxemia?
-
7.
What other information can you obtain from a pulse oximeter?
-
8.
What is perfusion index?
Answers/Discussion
-
1.
A sensor in the form of a probe is generally placed on the finger, toe, or earlobe of the patient. The probe has diodes which emit light of two different wave lengths—660 nm in the visible red light range and 940 nm in the infrared range in a rapid on—off mechanism. The oxygenated hemoglobin allows red light through and absorbs infrared light, while the deoxygenated hemoglobin allows infrared light through and absorbs more red light. The ratio of oxygenated to deoxygenated hemoglobin determines the amount of red and infrared light absorbed which is read by a sensor attached to a photodetector. Comparison of their absorption at these wavelengths enables the oximeter to calculate the oxygen saturation which is read during the pulsatile component of the blood. The microprocessor displays SpO2, heart rate, and a plethysmograph on the screen [1].
-
2.
Pulse oximeters work on the principle of absorption spectrophotometry explained by Beer’s and Lambert’s laws. Beer’s law states that the absorption of radiation by a given thickness of a solution of a given concentration is the same as that of twice the thickness of a solution of half the concentration [5]. Lambert’s law states that each layer of equal thickness absorbs an equal fraction of radiation which passes through [3].
-
3.
Isosbestic points are wavelengths at which both oxyhemoglobin and deoxyhemoglobin absorption is similar which is 808 nm, and the absorbance at this point depends only on the hemoglobin concentration. Earlier pulse oximeter models used a wavelength at an isosbestic point to compensate for hemoglobin concentration but newer models use various wavelengths.
-
4.
Pulse oximeter data are accurate on average to ±2% of a simultaneously obtained arterial blood gas value. The SpO2 values correlate with PO2 values in the range from 70 to 100% given the variability between individuals, where the pulse oximeter probe is placed (finger versus earlobe, distal versus closer to the heart) and the manufacturer’s variability range for healthy volunteers at sea level. Values greater than 95% are considered to be within the normal range. In healthy subjects, hypoxemia is defined as a pulse oximeter value less than 92% at sea level when breathing room air [2].
-
5.
Common sources of error [4]:
-
Strength of Arterial Pulse: Any factor that reduces arterial pulsations will reduce the ability of the instrument to obtain and analyze the signal—hypothermia, hypotension, and vasopressor use.
-
Body Movement: Extraneous movements can cause interference—shivering and Parkinsonian tremors [6].
-
Carboxyhemoglobin (CoHb): CO binds to heme competitively with 250 times the affinity of oxygen, and COHb has the same absorption pattern of 660 nm light as O2Hg causing artificial high SpO2 readings.
-
Methemoglobin: Methemoglobin absorbs as much 660 nm red light as it does the 940 nm infrared. Saturation approaches 85% and is falsely low at high SpO2 and falsely high at low SpO2.
-
Methylene blue, indigo carmine, and indocyanine green cause a drop in SpO2.
-
Color Interference: Pulse oximetry is not affected by skin color but is affected by artificial or opaque nail finishes that may interfere with transmission of light.
-
Physical factors like electrocautery and restriction of blood flow during BP cuff inflation.
-
Venous pulsations secondary to AV fistulas.
-
Saturations below 80% are inferred and the saturation is overestimated.
-
-
6.
Some of the common signs and symptoms of hypoxemia are:
-
Restlessness
-
Altered or deteriorating mental status
-
Increased or decreased pulse rate
-
Increased or decreased respiratory rate
-
Decreased oxygen oximetry readings
-
Cyanosis (late sign)
-
-
7.
Additional information received from pulse oximeter include heart rate and perfusion index if the oximeter is designed with this special feature. Pleth variability index (PVI) is an automatic and continuous monitor of the respiratory variation of the pulse oximeter’s plethysmographic waveform amplitude [7]. This has been shown to predict fluid responsiveness noninvasively in mechanically ventilated patients.
-
8.
Ratio between the pulsatile and the nonpulsatile blood is used to measure the (3) perfusion index (PI) in the peripheral tissues. Optimum monitoring sites may be chosen based on relatively high PI. Another use would be a spike in PI indicating that epidural anesthesia has initiated peripheral vasodilatation which occurs before the onset of anesthesia.
References
Pulse Oximeter. American Thoracic Society. Patient Information Series. Am J Respir Crit Care Med. 2011;184:1. Online Version: www.thoracic.org. ATS Patient Education Series © 2011 American Thoracic Society. 2013;1–2.
Pulse Oximetry Training Manual. Lifebox. WHO surgical safety checklist. Safe surgery saves lives. World Health Organization. Patient safety. A World Alliance for Safer Health Care. ISBN 979 92 4 150113 2. NLM Classification: WO 178. 1–24. http://www.who.int/patientsafety/safesurgery/en/index.html. http://www.who.int/patientsafety/safesurgery/pulse_oximetry/en/index.html
Fearnley SJ. Pulse oximetry. Update in anaesthesia. http://www.nda.ox.ac.uk/wfsa/html/u05/u05_003.htm
Hill E, Stoneham MD. Practical applications of pulse oximetry. http://www.nda.ox.ac.uk/wfsa/html/u11/u1104_01.htm
Principles of pulse oximetry. http://www.oximeter.org/pulseox/principles.htm
Goldman JM, Petterson MT, Kopotic RJ, Barker SJ. Masimo signal extraction pulse oximetry. J Clin Monit Comput. 2000;16:475–83.
Cannesson M, Desebbe O, Rosamel P, et al. Pleth variability index to monitor the respiratory variations in the pulse oximeter plethysmographic waveform amplitude and predict fluid responsiveness in the operating theatre. Br J Anaesth. 2008;101(2):200–6.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this chapter
Cite this chapter
de Armendi, A.J., Govindaraj, R. (2017). Pulse Oximetry. In: Raj, T. (eds) Data Interpretation in Anesthesia. Springer, Cham. https://doi.org/10.1007/978-3-319-55862-2_8
Download citation
DOI: https://doi.org/10.1007/978-3-319-55862-2_8
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-55861-5
Online ISBN: 978-3-319-55862-2
eBook Packages: MedicineMedicine (R0)