Abstract
We describe a simple method of tracking oxygen in real-time with injectable, tissue-integrating microsensors. The sensors are small (500 μm × 500 μm × 5 mm), soft, flexible, tissue-like, biocompatible hydrogel s that have been shown to overcome the foreign body response for long-term sensing. The sensors are engineered to change luminescence in the presence of oxygen or other analytes and function for months to years in the body. A single injection followed by non-invasive monitoring with a hand-held or wearable Bluetooth optical reader enables intermittent or continuous measurements. Proof of concept for applications in high altitude, exercise physiology, vascular disease, stroke, tumors, and other disease states have been shown in mouse, rat and porcine models. Over 90 sensors have been studied to date in humans. These novel tissue-integrating sensors yield real-time insights in tissue oxygen fluctuations for research and clinical applications.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Poor tissue oxygenation is linked to microvascular disease , critical limb ischemia, poor outcomes in cancer therapies, compartment syndrome, sepsis, wound healing, and a variety of other disease states and tissue malfunctions [1,2,3,4]. Few techniques exist for continuously monitoring tissue oxygen levels (e.g. electrochemical probes, microdialysis, MRI, EPR), and they are time intensive, require costly large equipment, lack accuracy, and/or typically require anesthesia or restraint, thereby excluding the possibility for real-time monitoring during daily life [5]. This report summarizes ongoing NIH and DARPA funded research on the development of novel, low-cost, tissue-integrating sensors that enable real-time continuous measurement of tissue oxygen for months to years, with special focus on continuous hypoxia monitoring for localized tissue ischemia and systemic oxygenation inferred from local measurements in healthy tissue.
The foreign body response (FBR) has long been known as the major culprit in developing long-term accurate in vivo biosensor s [6,7,8]. To overcome the FBR in designing long-term oxygen sensors, we begin with soft, tissue-like, hydrogel scaffold materials [9, 10], originally developed for tissue engineering applications. Within this hydrogel, nano/molecular sensors are engineered to optically report oxygen levels (or other analyte levels of interest depending on the recognition element selected). Dyes are synthetically engineered to emit in the near infra-red (optical window of the skin), covalently link to the hydrogel backbone, and be stable under in vivo conditions. The specially designed micro-architecture of the hydrogel sensor contains over 60% void space and encourages tissue and capillary growth into and throughout the entire sensor (Fig. 49.1). Unlike other implantable sensors, the porous hydrogel has a large surface area for analyte diffusion. In addition, the use of soft, tissue-like materials reduces the likelihood of biomechanical factors affecting the long-term sensor acceptance in tissue [11, 12].
Overview of tissue-integrating sensing system. (a) Miniature fluorescent hydrogel sensor. (b) Mobile health platform vision for continuous metabolic monitoring with a multi-analyte sensor. (c) Optical reader patch (black arrow) sits on the surface of skin and non-invasively interrogates the hydrogel sensor (white fiber) and sends data wirelessly to a computer interface or cell phone. (d) Tissue-integration without fibrous encapsulation of the soft, porous hydrogel sensor enables long term continuous monitoring of body analytes
2 Methods
2.1 Tissue-Integrating Sensor
The particular injectable microsensors reported here are composed of a biocompatible hydrogel, poly (2-hydroxyethyl methacrylate) (pHEMA) and a near infrared (NIR) oxygen-sensitive palladium-benzoporphyrin molecule (Pd-MABP) [13]. The microsensor measures oxygen in the body based on the principle of phosphorescence quenching of metalloporphyrins, a well-established technique with excellent sensitivity and specificity to physiologic oxygen [14,15,16,17]. The pHEMA hydrogel is biocompatible, has good oxygen permeability, excellent mechanical properties, and a long history of use in medical devices [18]. The Pd-MABP molecules are covalently attached to the pHEMA hydrogel, ensuring that the sensing chemistry is retained in the hydrogel structure. To create the tissue-integrating properties, pre-polymer solution is filled into tubes of various sizes into which quality-controlled, monodisperse templating beads have been close-packed and sintered. Pre-polymer solution is crosslinked, and tubes and sintering beads are removed through solvent dissolution [9, 10]. The miniature sensors (0.5 mm × 0.5 mm × 5 mm) are designed to remain in the body permanently; they are soft and tissue-like to minimize stress at the material-tissue interface caused by motion and pressure, which can damage or stimulate adjacent immune cells and prolong the inflammatory phase [11, 19].
2.2 Non-invasive Optical Reader
A non-invasive optical reader for use on animals and humans was designed to read the signals from injected tissue-integrating sensors (Concept in Fig. 49.1c and prototype shown in 49.2d). A reader is manually positioned over a sensor and taped into place. A thermometer built into the surface of the reader continuously allows for temperature correction. An LED pulses illumination light into the skin above the sensors, and a photodetector collects emission light emanating from the sensor.
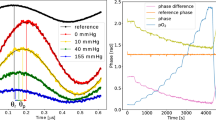
Sensor performance in vivo. Color shading in C, D, and G indicate periods at 1.00, 0.21 (1st grey bar) and <0.2 fiO2 (2nd grey bar). (a) Critical Limb Ischemia: Hindlimb sensor measured sudden changes in O2 upon application and release of a tourniquet (arrow). (b) Stroke Research: Sensor in mouse brain shows reduced tissue O2 due to induced stroke (carotid artery occlusion) and subsequent recovery after resolving the occlusion. (c) Tumor Metabolism: Sensors in a tumor (circles) and control tissue (line) measure oxygenation during hypoxia. Sensors can be utilized to measure the real-time action of oncological drugs on tumor metabolism and physiology. (d) Hypoxia Research in Pigs: Sensor in pig subcutis measures tissue O2 during acute hypoxia episodes with prototype handheld reader (described in 2.3). (e) Foot O 2 in Humans (>2 years): Elevating (white area) and lowering (grey area) of foot causes change in tissue O2 monitored by sensors 2.5 years post-injection. Foot O2 is important to healing chronic wounds. (f) Exercise Physiology: Tissue deoxygenation from isotonic exercise is observed in sensors placed near tricep. (g) Comparison to OxyLite: O2 Sensors (open circle and filled square) respond similarly to a percutaneously inserted fiber optic sensor (Oxylite, Oxford Optronics) (solid line). (h) Glucose Sensor Prototype: Presented is the same O2-sensitive platform with the addition of glucose oxidase to measure glucose concentrations in a rat. The sensors were monitored 3 weeks post-injection. Capillary blood glucose is indicated with triangles. These preliminary data demonstrate the proof-of-concept application of the luminescent hydrogel sensor to extend beyond continuous measurement of oxygen
The phosphorescent lifetime, a property of the oxygen sensitive dye, is measured, thereby providing a signal unaffected by optical path permutations such as blood flow fluctuations, tissue ingrowth, oxy/deoxyhemoglobin ratio, melanin content and hydration [20].
The current oxygen sensing system can measure lifetime to within 2 μs or better, which equates to ~1 μM O2, allowing good resolution within the observable range to date (2–70 μM).
2.3 In Vivo Application
In the work presented here sensors are injected with a 16 or 18-gauge needle in the subcutaneous tissue or other soft tissue of interest (brain, muscle, tumor). Sensors are visualized with the Perkins Elmer IVIS Imager in small animal models. Fluorescence from serial IVIS images is plotted to show changes in relative oxygen over time in response to challenges such as cycling fraction of inspired oxygen (fiO2) from 1.00 down to 0.12 in anesthetized mice, rats, and pigs. For quantitative O2 measurements derived from phosphorescent lifetime decay, the prototype optical reader described above and pictured in Fig. 49.2d is placed over the sensors. For the purpose of this manuscript, O2 is reported in relative units to clearly visualize fluctuation in response to oxygen challenges. Several hundred sensors have been optimized in mice, rats, and pigs. Over 90 sensors have been tested in humans including 50 in healthy volunteers and 40 in critical limb ischemia patients [21].
3 Results
Figure 49.2 summarizes data from pre-clinical models and human studies showing sensor response up to 2.5 years after injection. Sensors have been histologically verified to reside between 2 and 8 mm under the skin and to avoid the foreign body response. Sensors respond to changes in O2 concentration within a few seconds in response to breathable (fiO2) or physical (pressure) oxygen challenges in mice, rats, pigs, and humans.
The benefits of such O2 sensing technology is the ability to non-invasively monitor status of tissue in a continuous, mobile format. The cost of instrumentation is orders of magnitude cheaper than MRI or EPR, however with lower spatial resolution. Repeated insertions and perturbations of tissue that are required by percutaneous fiber optics or Clark electrodes are eliminated. Furthermore, the luminescent lifetime measurement technique is immune to errors from movement, injection depth (<1 cm), or other optical artifacts (e.g., blood flow, oxy/deoxyhemoglobin ratio) [20].
Some challenges of the luminescent tissue-integrating technology include temperature sensitivity and depth. Current surface temperature correction may be improved in the future by incorporation of temperature sensitive luminophores into the hydrogel . Current injectable sensors are limited to ~1 cm depth due to sensor brightness, which could be enhanced by creating larger sensors, though must be balanced with trade-offs (e.g., patient inconvenience). Sensors may be engineered through formulation optimization to enhance brightness for monitoring deeper tissues.
4 Conclusions
Tissue-integrating hydrogel microsensors enable continuous in vivo monitoring to provide powerful insights into tissue-level physiology with the potential to help make more informed therapeutic, real-time decisions about various disease states. The methods discussed present potential cost- and time-effective methods to monitor tissue oxygenation long-term in pre-clinical and clinical situations.
References
Kara A, Akin S, Ince C (2016) Monitoring microcirculation in critical illness. Curr Opin Crit Care 22:413–512
Giatromanolaki A, Harris AL (2001) Tumour hypoxia, hypoxia signaling pathways and hypoxia inducible factor expression in human cancer. Anticancer Res 21:4317–4324
Guo S, DiPietro LA (2010) Factors affecting wound healing. J Dent Res 89:221–229
Weick JW, Kang H, Lee L et al (2016) Direct measurement of tissue oxygenation as a method of diagnosis of acute compartment syndrome. J Orthop Trauma 30:585–591
Paul DW, Stenken JA (2015) A review of flux considerations for in vivo neurochemical measurements. Analyst 40:3709–3730
Anderson JM, Rodriguez A, Chang DT (2008) Foreign body reaction to biomaterials. Semin Immunol 20:86–100
Nichols SP, Koh A, Storm WL et al (2013) Biocompatible materials for continuous glucose monitoring devices. Chem Rev 113:2528–2549
Wisniewski N, Moussy F, Reichert WM (2000) Characterization of implantable biosensor membrane biofouling. Fresen J Anal Chem 366:611–621
Kotov NA, Liu Y, Wang S et al (2004) Inverted colloidal crystals as three-dimensional cell scaffolds. Langmuir 20:7887–7892
Marshall AJ, Irvin CA, Barker T et al (2004) Biomaterials with tightly controlled pore size that promote vascular in-growth. ACS Polym Prepr 45:100–101
Helton KL, Ratner BD, Wisniewski NA (2011a) Biomechanics of the sensor-tissue interface-effects of motion, pressure, and design on sensor performance and the foreign body response-part I: theoretical framework. J Diabetes Sci Technol 5:632–646
Helton KL, Ratner BD, Wisniewski NA (2011b) Biomechanics of the sensor-tissue interface-effects of motion, pressure, and design on sensor performance and foreign body response-part II: examples and application. J Diabetes Sci Technol 5:647–656
Gamsey S, Wisniewski N, Helton K et al (2016) Oxygen sensors. US Patent 9375494, 28 Jun 2016
Rumsey WL, Vanderkooi JM, Wilson DF (1988) Imaging of phosphorescence: a novel method for measuring oxygen distribution in perfused tissue. Science 241:1649–1651
Lo LW, Koch CJ, Wilson DF (1996) Calibration of oxygen-dependent quenching of the phosphorescence of pd-meso-tetra (4-carboxyphenyl) porphine: a phosphor with general application for measuring oxygen concentration in biological systems. Anal Biochem 236:153–160
Vinogradov SA, Grosul P, Rozhkov V et al (2003) Oxygen distributions in tissue measured by phosphorescence quenching. Adv Exp Med Biol 510:181–185
Wilson DF, Vinogradov SA, Grosul P et al (2006) Imaging oxygen pressure in the rodent retina by phosphorescence lifetime. Adv Exp Med Biol 578:119–124
Montheard JP, Chatzopoulos M, Chappard D (1992) 2-hydroxyethyl methacrylate (HEMA): chemical properties and applications in biomedical fields. J Macromol Sci Rev Macromol Chem Phys 32:1–34
Klueh U, Liu Z, Feldman B et al (2011) Metabolic biofouling of glucose sensors in vivo: role of tissue microhemorrhages. J Diabetes Sci Technol 5:583–595
Nagl S, Stich MI, Schaeferling M, Wolfbeis OS (2009) Method for simultaneous sensing of two species using optical probes of different decay time, and its application to an enzymatic reaction at varying temperature. Anal Bioanal Chem 393:1199–1207
Montero-Baker M, Au-Yeung KY, Wisniewski NA et al (2015) The use of micro-oxygen sensors (MOXYs) to determine dynamic relative oxygen indices in the feet of patients with limb-threatening ischemia during endovascular therapy: the first-in-man “Si Se Puede” study. J Vasc Surg 61:1501–1509
Acknowledgments
This work was funded in part by R01EB016414, R43DK093139 and R43DK09115 from the National Institutes of Health, W911NF-11-1-0119 and W31P4Q-12-C-0205 from the Defense Advanced Research Projects Agency and the U.S. Army Research Office and sponsored research projects from Profusa, Inc. with Duke University.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this chapter
Cite this chapter
Wisniewski, N.A. et al. (2017). Tissue-Integrating Oxygen Sensors: Continuous Tracking of Tissue Hypoxia. In: Halpern, H., LaManna, J., Harrison, D., Epel, B. (eds) Oxygen Transport to Tissue XXXIX. Advances in Experimental Medicine and Biology, vol 977. Springer, Cham. https://doi.org/10.1007/978-3-319-55231-6_49
Download citation
DOI: https://doi.org/10.1007/978-3-319-55231-6_49
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-55229-3
Online ISBN: 978-3-319-55231-6
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)