Abstract
In the healthy lung, macrophages maintain homeostasis by clearing inhaled particles, bacteria, and removing apoptotic cells from the local pulmonary environment. However, in respiratory diseases including chronic obstructive pulmonary disease (COPD), asthma, and cystic fibrosis, macrophages appear to be dysfunctional and may contribute to disease pathogenesis. In COPD, phagocytosis of bacterial species and apoptotic cells by both alveolar macrophages and monocyte-derived macrophages is significantly reduced, leading to colonization of the lung with pathogenic bacteria. COPD macrophages also release high levels of pro-inflammatory cytokines and chemokines, including CXCL8, TGFβ, and CCL2, driving recruitment of other inflammatory cells including neutrophils and monocytes to the lungs and promoting disease progression.
In asthma, defective phagocytosis and efferocytosis have also been reported, and macrophages appear to have altered cell surface receptor expression; however, it is as yet unclear how this contributes to disease progression but may be important in driving Th2-mediated inflammation. In cystic fibrosis, macrophages also display defective phagocytosis, and reduced bacterial killing, which may be driven by the pro-inflammatory environment present in the lungs of these patients.
The mechanisms behind defective macrophage function in lung diseases are not currently understood, but potential mechanisms include alterations in phagocytic receptor expression levels, oxidative stress, but also the possibility that specific diseases are associated with a specific, altered, macrophage phenotype that displays reduced function. Identification of the mechanisms responsible may present novel therapeutic opportunities for treatment.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Chronic Obstructive Pulmonary Disease
- Cystic Fibrosis
- Chronic Obstructive Pulmonary Disease Patient
- Alveolar Macrophage
- Idiopathic Pulmonary Fibrosis
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
As the most abundant leukocyte in the airways, macrophages were, until recently, thought to maintain the sterility of the lung, through phagocytosis of bacteria and by homeostasis via removal of apoptotic cells (Kopf et al. 2015). However, more recent studies have shown that the airways are colonized by a lung microbiome that changes with disease (Han et al. 2012). This suggests that macrophages do not remove all bacteria from the lungs, but nevertheless play an important role in the removal of pathogenic bacteria, inhaled particulates, and dying cells and are key in maintaining pulmonary homeostasis. In chronic lung diseases, this process of phagocytosis appears to become dysfunctional, leading to the presence of specific bacterial populations which may contribute to the underlying pathophysiology of disease (Han et al. 2012). This is further exacerbated by an increase in the number of apoptotic cells in chronic lung disease. Failure of macrophages to clear these cells leads to secondary necrosis, promoting inflammation and contributing to disease pathophysiology (Henson and Tuder 2008). Failure to clear apoptotic cells also promotes maintenance of the macrophage in a pro-inflammatory phenotype that lacks the capacity to resolve inflammation and thus may be key in driving the chronic inflammatory profile observed in many pulmonary conditions.
Studies into the function of pulmonary macrophage in both health and disease have been hampered by availability of cells, particularly from patient populations. Sampling has usually involved bronchoalveolar lavage, which is not without risk to the subject and is not possible in patients with more severe disease. Nevertheless, this technique has provided access to alveolar macrophages. These are not the only macrophage population found in the lung, with other populations identified within the interstitium of the lung that appear to have distinct, functional characteristics that distinguish this population from macrophages found in the airspaces (Frankenberger et al. 2000). Cell surface markers for identification of different macrophage populations have recently been identified (Desch et al. 2016) which will now allow more detailed research into the roles of these populations and their relative contributions to pulmonary disease furthering our understanding of macrophage dysfunction in chronic lung disease that will lead to novel therapeutic opportunities.
2 Chronic Lung Diseases
2.1 Chronic Obstructive Pulmonary Disease
Chronic obstructive pulmonary disease (COPD) is an umbrella term for three underlying pathophysiologies: chronic bronchitis, small airways disease, and emphysema. The contribution of each of these can vary between patients leading to heterogeneity of the population with some patients experiencing one, two, or all three of the pathophysiologies. Regardless of aetiology, COPD is characterized by a slowly progressive development of airflow limitation that is poorly reversible (Barnes 2004b). Exacerbations of symptoms can occur, leading to increased hospital admissions, morbidity, and mortality (Wedzicha and Donaldson 2003). Respiratory infections are an important feature of exacerbations, with viruses being detected in two-thirds of cases and bacteria being detected in half of cases (Sapey and Stockley 2006). Recent data has shown that bacterial infections often follow viral infection, suggesting a link between an initial viral infection and secondary bacterial infection (George et al. 2014; Mallia et al. 2011). The main bacterial species detected in the COPD lungs are Haemophilus influenzae, Streptococcus pneumoniae, and Moraxella catarrhalis, which are detected despite a 20-fold increase in the number of alveolar macrophages found in the lungs of COPD patients, indicating dysfunctional bacterial clearance in this disease (Hill et al. 2000; Wilkinson et al. 2003). The presence of lower airway bacterial colonization is strongly associated with increased exacerbations and worsening of lung function (Donaldson et al. 2002) leading to more rapid disease progression.
The first studies into phagocytes in COPD utilized the dimorphic fungus Candida albicans and showed no difference in phagocytosis by peripheral granulocytes (largely neutrophils) in COPD patients (Ritts et al. 1976); however, later studies indicated reduced phagocytosis of the same species by peripheral monocytes in chronic bronchitis (Nielsen and Bonde 1986). Subsequent observations using alveolar macrophages showed reduced phagocytosis and killing of C. albicans in cells from COPD patients compared with controls (Vecchiarelli et al. 1991; Ferrara et al. 1996).
Using more relevant bacterial species, multiple studies have shown defective phagocytosis of H. influenzae not only in alveolar macrophages taken from COPD patients compared to healthy controls (Berenson et al. 2006) but also in monocyte-derived macrophages differentiated from peripheral blood from COPD patients and exposed to both H. influenzae and S. pneumoniae (Taylor et al. 2010). These data support the theory that there exists a systemic macrophage defect in COPD, and that exposure of macrophages in the lungs to toxins and oxidative stress is not the primary cause of this defect, but this pulmonary exposure may impact further upon an already reduced baseline response. Similar experiments using inert latex beads have failed to show a defect in COPD macrophages, indicating that macrophages have the capacity to phagocytose, but that the bacteria-specific response is reduced (Lundborg et al. 2001; Hodge et al. 2003; Taylor et al. 2010).
Alveolar macrophages from COPD patients also display defective efferocytosis (clearance of apoptotic cells), and this is more apparent in current smokers possibly due to modification of extracellular proteins on the macrophage surface due to exposure to cigarette smoke (Hodge et al. 2007; Kirkham et al. 2004); however, the mechanism underlying this has yet to be elucidated but may be due to oxidative stress. Failure to remove apoptotic cells in the lungs, such as airway epithelial cells and T cells, leads to secondary necrosis, release of inflammatory mediators, and promotion of lung damage (Hodge et al. 2005).
The mechanisms behind these defects in the removal of pathogens and apoptotic cells from COPD lungs remain unclear. Phagocytosis of prey depends on recognition and engagement with various receptors expressed on the macrophage cell surface, and it has been postulated that reduced receptor expression might be the reason for impaired clearance of bacteria and apoptotic cells in COPD. Multiple studies have attempted to look into the role of these receptors in COPD macrophages. The mannose receptor (CD206) which recognizes the terminal mannose on bacterial cell wall glycosides has been shown to be reduced in alveolar macrophages from patients with COPD compared with that of nonsmokers (Hodge et al. 2008). The Toll-like receptors (TLR) are also key receptors in the recognition of bacterial proteins. TLR-4, which binds lipopolysaccharide (LPS) found on the cell wall of gram-negative bacteria, has been shown to not be altered in COPD macrophages (Metcalfe et al. 2014); however, TLR2 which binds lipopeptides from H. influenzae and S. pneumoniae has been shown to be reduced on COPD alveolar macrophages (Droemann et al. 2005). A host of other scavenger receptors are also implicated in macrophage phagocytosis; however, their study has brought about conflicting results. In alveolar macrophages from COPD patients, studies have shown reduced levels of CD31, CD91, CD44, and CD71 (Hodge et al. 2007). However, other studies have not seen differences in expression of CD11b (CR3a), CD14, CD58, CD80, CD7, or human leukocyte antigen-DR (HLA-DR), but have reported reduced expression of CD86 and CD11a (Lofdahl et al. 2006), whereas others have reported no difference in expression of CD44, CD36, CD61, CD14, CD86, or CD40 but did observe reduced expression of HLA-DR and CD80 (Pons et al. 2005).
The role of receptors is further complicated in monocyte-derived macrophages where defects in bacterial phagocytosis were reported, but there were no differences in the number of cell surface recognition molecules between cells from COPD patients and healthy controls (Taylor et al. 2010). As multiple receptors are likely to be involved in the phagocytic process, and different receptors required for the recognition and uptake of different prey, it is likely that changes in a single, specific receptor are unlikely to be responsible for the defects in phagocytosis seen in COPD macrophages. However, downstream signaling pathways may be implicated.
The sphingosine-1-phosphate (S1P) signaling pathways have been shown to be elevated in COPD alveolar macrophages, and antagonism of S1PR5 improved phagocytosis in one study, implicating this pathway in phagocytosis (Barnawi et al. 2015), but further research is required. Other studies have also shown that efferocytosis can be improved by macrolide antibiotics such as azithromycin (Hodge et al. 2008), the antioxidant procysteine (Hodge et al. 2010), or the Nrf2 activator sulforaphane (Harvey et al. 2011) suggesting that this defect can be resolved.
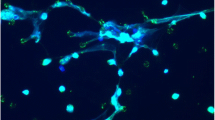
Macrophages have been considered to be the orchestrators of COPD (Barnes 2004a) due to their capacity to produce many of the mediators that are highly expressed in the lungs of these patients (Fig. 12.1). For example, macrophages produce increased levels of CXCL8 (interleukin (IL)-8) and granulocyte-macrophage colony-stimulating factor (GM-CSF) (Russell et al. 2002a; Culpitt et al. 2003), which drive neutrophil recruitment and macrophage maturation, respectively. They also produce increased levels of CCL2 (Frankenberger et al. 2011), which in turn leads to the recruitment of monocytes into the lung, which subsequently differentiate into macrophages. These cells also produce CXCR3 chemokines, CXCL9, CXCL10, and CXCL11 (Shaykhiev et al. 2009), which could account for the elevated levels of these chemokines in COPD sputum (Costa et al. 2008). Finally, COPD macrophages produce increased levels of proteases including matrix metalloproteinases (MMP) 2 and 9 (Finlay et al. 1997; Russell et al. 2002b), which are considered important in driving destruction of the extracellular matrix associated with emphysema. Furthermore, this inflammatory macrophage phenotype is not amenable to inhibition by the administration of glucocorticosteroids, and as such these cells are considered steroid insensitive (Culpitt et al. 2003). The mechanism underlying this observation has been elucidated and is due to oxidant-mediated downregulation of histone deacetylase (HDAC)2 (Ito et al. 2005) that can be restored by addition of theophylline (Cosio et al. 2004).
Role of macrophages in COPD pathogenesis. Exposure of the lungs to cigarette smoke causes damage to macrophages and activates pro-inflammatory pathways. Macrophages release an array of cytokines and chemokines to promote monocyte recruitment to the lungs to increase macrophage numbers, recruit neutrophils which release neutrophil elastase, activate CD8+ T cells which release granzymes and perforins, and promote macrophage release of MMP, cathepsins, and TGFβ, all of which contribute to COPD pathogenesis
These alterations in macrophage function in COPD have led to speculation that there is a specific COPD phenotype or an abnormal skewing of phenotype in this disease. Shaykhiev and colleagues suggested that this skewing was due to cigarette smoking (2009), and, more recently, a distinct macrophage phenotype has been identified in lung tissue that is glucocorticoid insensitive (Chana et al. 2014), suggesting that targeting these aberrant COPD macrophages and either removing them or pushing them toward a “healthy” phenotype could be beneficial in restoring their defective function and halting the progression of COPD.
2.2 Asthma
Asthma is defined as reversible airflow obstruction that can be long-term or remitting. It is characterized by persistent airway inflammation, bronchial hyperresponsiveness, and airway remodeling (Busse and Lemanske 2001). While bacterial colonization is not considered a characteristic of stable asthma, patients have a propensity to develop exacerbations, led by viral or bacterial infection as well as other causes such as allergens and occupational exposures (Singh and Busse 2006). The role of macrophages in asthma has been largely overlooked (Park and Christman 2016) as their absolute numbers do not increase compared to healthy subjects (Jeffery 1999); nevertheless, there are clear phenotypic and functional differences in the asthmatic pulmonary macrophage that may contribute to disease pathophysiology (Pappas et al. 2013).
Initial studies looking at macrophage phagocytosis in asthma were performed using opsonized zymosan, a glucan found on the surface of yeast. Sputum macrophages showed a reduction in zymosan uptake in children with eosinophilic asthma (Alexis et al. 2001); however, their studies showed an increase in opsonized zymosan uptake both in vivo and ex vivo in macrophages from mild asthmatics compared to healthy volunteers (Lay et al. 2009). Further studies showed that in children, there was decreased uptake of Staphylococcus aureus in alveolar macrophages from moderate and severe asthmatics compared to healthy controls (Fitzpatrick et al. 2008). Similar data was observed when H. influenzae was used as prey in experiments using cells from more severe asthmatics, which was also observed in monocyte-derived macrophages compared to mild asthmatics (Liang et al. 2014). This suggests that, as with COPD, there may be a systemic defect in macrophage phagocytic function and that the local environment is not solely responsible for driving this effect.
Similarly to COPD, efferocytosis has also been shown to be reduced in asthmatic macrophages. Influx of eosinophils to the lungs during asthma leads to increased levels of apoptotic eosinophils in the lungs of asthmatics compared to healthy controls (Walsh 2008; Duncan et al. 2003). Alveolar macrophages from severe asthmatics display reduced uptake of apoptotic cells compared to healthy subjects and those with mild asthma and showed reduced release of cytokines and prostaglandins (Huynh et al. 2005).
Approximately 5% of patients are described as having severe asthma with reduced responsiveness to conventional therapies including glucocorticosteroids (Adcock et al. 2008). Furthermore, similar to COPD, there appears to be a macrophage insensitivity to these drugs (Bhavsar et al. 2008). In addition, there is increased p38 pathway activation (Bhavsar et al. 2008) leading to increased output of a number of inflammatory cytokines. This is accompanied by changes in phenotype toward an “M2”-like, alternatively activated cell that expresses higher levels of chemokines including CCL17 (Staples et al. 2012) that has been reported to not fully comply with an “M2” phenotype. However, recently Girodet and colleagues have shown that macrophages from severe asthmatic patients show increased levels of CD206 and MHC-II expression together with increases in IL-6, IL-10, and IL-12p40 (Girodet et al. 2016). Moreover, the authors suggest that within this MHC-IIhi CD206hi population of macrophages, those that also expressed high levels of histamine receptor (HRH) 1 correlated with increased airway obstruction. They also showed that E-cadherin was highly expressed on these macrophages (Girodet et al. 2016). However, the functional consequence of this finding to macrophage responsiveness is yet to be elucidated.
2.3 Cystic Fibrosis
Cystic fibrosis (CF) is a chronic progressive disease characterized by various mutations in the CF transmembrane regulator protein (CFTR) which, in the lung epithelium, leads to reduced uptake of Cl− ions and reduced hydration of the airway fluid, thereby affecting mucociliary clearance (Chmiel et al. 2002). As with asthma, research into the role of macrophages in this disease has been lacking, but there are clear changes in both the innate immune response and the macrophage in the lung of patients with CF (Bruscia and Bonfield 2016). Exactly how this cell may contribute to disease pathophysiology and progression remains unclear, but there is now increasing interest in this field. For example, the CFTR protein is also expressed by macrophages and is thought to be necessary for the acidification of the phagolysosome required for killing (Di et al. 2006); however, others have failed to see this effect, suggesting that other factors may be important in bacterial killing (Haggie and Verkman 2007). The CF lung is colonized by a number of bacterial species, with Pseudomonas aeruginosa, S. aureus, H. influenzae, and Burkholderia cepacia being among the most prevalent (Valenza et al. 2008). Colonization with these bacterial species suggests that there are defects in the innate response that may be attributable to reduced macrophage clearance of these pathogens.
Studies on macrophage phagocytosis in CF have shown varying results, with some studies showing that alveolar macrophages from CF patients display reduced phagocytosis of Escherichia coli compared to healthy controls, alongside increased cytokine release (Simonin-Le Jeune et al. 2013), while a study using a more relevant bacteria showed that while phagocytosis of P. aeruginosa did not appear to be impaired in CF macrophages, the bacteria had increased survival within the cell (Del Porto et al. 2011). The mechanisms behind any defects in CF macrophages are not clear but may be driven by the lung environment. Bronchoalveolar lavage fluid from CF patients was able to decrease phagocytosis by healthy macrophages, and this has been attributed to the increased levels of neutrophil elastase present (Alexis et al. 2006). Neutrophil elastase cleaves the phosphatidylserine receptor on macrophages, which disrupts efferocytosis indicating a possible mechanism for reduced macrophage uptake in the CF lung (Vandivier et al. 2002). Toxins released by the bacteria are also able to reduce phagocytosis, including pyocyanin, a toxin released from P. aeruginosa which impairs efferocytosis, but not uptake of latex beads, and which could be restored by antioxidants, suggesting an oxidative stress effect on cell surface receptors (Bianchi et al. 2008). Other possible mechanisms include the presence of a thick mucus layer preventing contact between alveolar macrophages and the bacteria themselves, thereby contributing to increased colonization of the lungs (Vandivier et al. 2006).
There is clear evidence that macrophages in the lungs of patients with CF are highly activated, as they display increased release of a number of cytokines (Bonfield et al. 1995) supportive of the concept that these cells contribute to the inflammatory milieu in CF. Further evidence of macrophage dysfunction has arisen from study of sputum macrophages with small sputum macrophages showing decreased expression of the macrophage receptor with collagenous structure (MARCO) and CD206 receptors involved in non-opsonic phagocytosis (Wright et al. 2009). However, further work is required to understand whether these changes in macrophage function are due to the local environment in the CF lung or whether inherent differences in macrophages from these patients are causative.
2.4 Other Lung Diseases
As methodology has improved for studies into human pulmonary macrophages together with increased availability of tools to study these cells, there has been increased interest in the role of these cells in other lung disease such as idiopathic pulmonary disease (IPD) and acute respiratory distress syndrome (ARDS). As with other pulmonary conditions, there appears to be a skewing of macrophage phenotype in interstitial lung diseases with an increase in CD40 expression in cells from sarcoid patients and increased CD163 in cells from those with idiopathic pulmonary fibrosis (IPF) (Wojtan et al. 2016). How these observations translate to macrophage function remains to be elucidated, but early studies showed that macrophages from IPF patients were unable to kill bacteria (Savici et al. 1989) with more recent studies showing reduced clearance of apoptotic cells (Morimoto et al. 2012) similar to that seen in COPD. Alveolar macrophages from IPF patients also show increased responses to collagen by releasing increased levels of CCL18, CCL2, and IL-1ra via increased upregulation of CD204 (Stahl et al. 2013), again demonstrating changes in macrophage function which appears characteristic of disease.
3 Conclusion
Macrophage dysfunction appears to be common across multiple chronic lung diseases; however, why this is the case remains unclear. There are many proposed mechanisms; however, further work is required in order to elucidate the underlying reasons for these observations, but may relate to differing local microenvironments due to specific pulmonary inflammatory insults, e.g., exposure to cigarette smoke or specific pathogens.
There appears to be common changes in the capacity of macrophages to clear pathogens and/or apoptotic cells, and one theory is that alveolar macrophages are already full or satiated due to clearance of environmental particles (e.g., tar or particles from pollution). The increased presence of bacteria, apoptotic cells, and, in the case of smokers, tar and other particulates could lead to the hypothesis that the cells simply do not have enough capacity to consume any additional material. However, since monocyte-derived macrophages from asthmatics, COPD and CF patients, still show a defective phagocytic phenotype, the concept of satiety cannot solely explain these observations. This instead suggests a systemic defect, which may appear early in the disease process, and, instead of being resultant of the damage in the lungs, actually contributes to drive this process.
As mentioned previously, phagocytosis occurs via a multitude of cell surface receptors and requires complex intracellular signaling mechanisms, actin reorganization, and phagolysosome formation to be successful. It is postulated that any number of these processes could be defective. For example, downregulation of the receptors involved in recognition and phagocytosis of prey would lead to a reduction in the cells’ ability to phagocytose. Proteases have been shown to degrade cell surface receptors, and cigarette smoke has been shown to downregulate receptors including CD91, CD31, CD44, and CD71, suggesting oxidative stress may also damage receptors (Hodge et al. 2010), which could be potential mechanisms in both CF and COPD.
Other factors that could also alter macrophage function include viral infection. Viruses are known to be a cause of exacerbations in COPD and asthma, and rhinovirus is able to enter macrophages, although may not be able to replicate inside the cell (Gern et al. 1996). It is possible, therefore, that viruses may alter the function of macrophages during exacerbations in respiratory disease. Oliver et al. demonstrated that this may be the case, showing that rhinovirus suppressed phagocytosis of E. coli by alveolar macrophages (2008), and suggesting that treating viral infections may prevent subsequent bacterial infection in respiratory diseases.
Other proposed mechanisms are that inhaled medications could alter cell function; however, there is little evidence to support this theory. In fact, studies have shown that in vitro, budesonide, formoterol, and azithromycin did not alter phagocytosis of H. influenzae in monocyte-derived macrophages from COPD patients (Taylor et al. 2010) and that dexamethasone and formoterol had no effect in cells from severe asthmatics (Liang et al. 2014). In vivo, it has been shown that low-dose azithromycin increased efferocytosis of bronchial epithelial cells and neutrophils in alveolar macrophages from COPD patients, but this was not due to changes in receptor expression (Hodge et al. 2008), indicating that further research is required into the effects of various treatments on improving phagocytosis.
Improving clearance of bacteria by macrophages may prove beneficial in many chronic lung diseases, leading to reduced incidence of exacerbation, and improved morbidity and mortality. Opsonization is known to improve phagocytosis of bacteria (Wellington et al. 2003), and so promoting the production of opsonins in the lungs may improve phagocytosis. However, this could prove difficult in the CF where thick mucus may prevent opsonization from occurring. Increasing receptor expression by macrophages may also increase phagocytosis, demonstrated by the use of sulforaphane, a chemical found in broccoli and other green vegetables, which has been shown to improve phagocytosis of H. influenzae by alveolar macrophages via upregulation of the phagocytic receptor MARCO (Harvey et al. 2011).
Other strategies that could be beneficial involve changing macrophage phenotype toward a more homeostatic phenotype and restoring the skewed populations observed in many diseases. Resolvins are lipid mediators that have been described as “specialized pro-resolving mediators” with key roles in the resolution of inflammation including regulating macrophage phenotype by promoting a more anti-inflammatory macrophage and have been shown to reverse the effects of cigarette smoke extract on suppression of phagocytosis (Croasdell et al. 2015). This suggests that manipulation of phenotype might improve bacterial clearance and restore macrophage function to that of a homeostatic cell type and hence be a possible target for therapeutics.
References
Adcock IM, Ford PA, Bhavsar P, Ahmad T, Chung KF (2008) Steroid resistance in asthma: mechanisms and treatment options. Curr Allergy Asthma Rep 8(2):171–178
Alexis NE, Soukup J, Nierkens S, Becker S (2001) Association between airway hyperreactivity and bronchial macrophage dysfunction in individuals with mild asthma. Am J Physiol Lung Cell Mol Physiol 280:369–375
Alexis NE, Muhlebach MS, Peden DB, Noah TL (2006) Attenuation of host defense function of lung phagocytes in young cystic fibrosis patients. J Cyst Fibros 5(1):17–25
Barnawi J, Tran H, Jersmann H, Pitson S, Roscioli E, Hodge G, Meech R, Haberberger R, Hodge S (2015) Potential link between the sphingosine-1-phosphate (S1P) system and defective alveolar macrophage phagocytic function in chronic obstructive pulmonary disease (COPD). PLoS One 10(10):e0122771. doi:10.1371/journal.pone.0122771
Barnes PJ (2004a) Macrophages as orchestrators of COPD. J COPD 1:50–70
Barnes PJ (2004b) Mediators of chronic obstructive pulmonary disease. Pharmacol Rev 56(4):515–548. doi:10.1124/pr.56.4.2
Berenson CS, Garlipp MA, Grove LJ, Maloney J, Sethi S (2006) Impaired phagocytosis of nontypeable Haemophilus influenzae by human alveolar macrophages in chronic obstructive pulmonary disease. J Infect Dis 194(10):1375–1384. doi:10.1086/508428
Bhavsar P, Hew M, Khorasani N, Torrego A, Barnes PJ, Adcock I, Chung KF (2008) Relative corticosteroid insensitivity of alveolar macrophages in severe asthma compared with non-severe asthma. Thorax 63(9):784–790. doi:10.1136/thx.2007.090027
Bianchi SM, Prince LR, McPhillips K, Allen L, Marriott HM, Taylor GW, Hellewell PG, Sabroe I, Dockrell DH, Henson PW, Whyte MK (2008) Impairment of apoptotic cell engulfment by pyocyanin, a toxic metabolite of Pseudomonas aeruginosa. Am J Respir Crit Care Med 177(1):35–43. doi:10.1164/rccm.200612-1804OC
Bonfield TL, Panuska JR, Konstan MW, Hilliard KA, Hilliard JB, Ghnaim H, Berger M (1995) Inflammatory cytokines in cystic fibrosis lungs. Am J Respir Crit Care Med 152(6 Pt 1):2111–2118. doi:10.1164/ajrccm.152.6.8520783
Bruscia EM, Bonfield TL (2016) Cystic fibrosis lung immunity: the role of the macrophage. J Innate Immun 8(6):550–563. doi:10.1159/000446825
Busse WW, Lemanske RF (2001) Asthma. N Engl J Med 344:350–362
Chana KK, Fenwick PS, Nicholson AG, Barnes PJ, Donnelly LE (2014) Identification of a distinct glucocorticosteroid-insensitive pulmonary macrophage phenotype in patients with chronic obstructive pulmonary disease. J Allergy Clin Immunol 133(1):207–216 (e201–211). doi:10.1016/j.jaci.2013.08.044
Chmiel JF, Berger M, Konstan MW (2002) The role of inflammation in the pathophysiology of CF lung disease. Clin Rev Allergy Immunol 23(1):5–27. doi:10.1385/CRIAI:23:1:005
Cosio BG, Tsaprouni L, Ito K, Jazrawi E, Adcock IM, Barnes PJ (2004) Theophylline restores histone deacetylase activity and steroid responses in COPD macrophages. J Exp Med 200(5):689–695. doi:10.1084/jem.20040416
Costa C, Rufino R, Traves SL, Lapa ESJR, Barnes PJ, Donnelly LE (2008) CXCR3 and CCR5 chemokines in induced sputum from patients with COPD. Chest 133(1):26–33. doi:10.1378/chest.07-0393
Croasdell A, Thatcher TH, Kottmann RM, Colas RA, Dalli J, Serhan CN, Sime PJ, Phipps RP (2015) Resolvins attenuate inflammation and promote resolution in cigarette smoke-exposed human macrophages. Am J Physiol Lung Cell Mol Physiol 309(8):L888–L901. doi:10.1152/ajplung.00125.2015
Culpitt SV, Rogers DF, Shah P, De Matos C, Russell RE, Donnelly LE, Barnes PJ (2003) Impaired inhibition by dexamethasone of cytokine release by alveolar macrophages from patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 167(1):24–31. doi:10.1164/rccm.200204-298OC
Del Porto P, Cifani N, Guarnieri S, Di Domenico EG, Mariggio MA, Spadaro F, Guglietta S, Anile M, Venuta F, Quattrucci S, Ascenzioni F (2011) Dysfunctional CFTR alters the bactericidal activity of human macrophages against Pseudomonas aeruginosa. PLoS One 6(5):e19970. doi:10.1371/journal.pone.0019970
Desch AN, Gibbings SL, Goyal R, Kolde R, Bednarek J, Bruno T, Slansky JE, Jacobelli J, Mason R, Ito Y, Messier E, Randolph GJ, Prabagar M, Atif SM, Segura E, Xavier RJ, Bratton DL, Janssen WJ, Henson PM, Jakubzick CV (2016) Flow cytometric analysis of mononuclear phagocytes in nondiseased human lung and lung-draining lymph nodes. Am J Respir Crit Care Med 193(6):614–626. doi:10.1164/rccm.201507-1376OC
Di A, Brown ME, Deriy LV, Li C, Szeto FL, Chen Y, Huang P, Tong J, Naren AP, Bindokas V, Palfrey HC, Nelson DJ (2006) CFTR regulates phagosome acidification in macrophages and alters bactericidal activity. Nat Cell Biol 8(9):933–944. doi:10.1038/ncb1456
Donaldson GC, Seemungal TAR, Bhowmik A, Wedzicha JA (2002) Relationship between exacerbation frequency and lung function decline in chronic obstructive pulmonary disease. Thorax 57(10):847–852. doi:10.1136/thorax.57.10.847
Droemann D, Goldmann T, Tiedje T, Zabel P, Dalhoff K, Schaaf B (2005) Toll-like receptor 2 expression is decreased on alveolar macrophages in cigarette smokers and COPD patients. Respir Res 8(6):68
Duncan CJ, Lawrie A, Blaylock MG, Douglas JG, Walsh GM (2003) Reduced eosinophil apoptosis in induced sputum correlates with asthma severity. Eur Respir J 22(3):484–490. doi:10.1183/09031936.03.00109803a
Ferrara F, D’Adda D, Falchi M, Dall’Asta L (1996) The macrophagic activity of patients affected by pneumonia or chronic obstructive pulmonary disease. Int J Tissue React 18(4–6):109–114
Finlay GA, O’Driscoll LR, Russell KJ, D’Arcy EM, Masterson JB, FitzGerald MX, O’Connor CM (1997) Matrix metalloproteinase expression and production by alveolar macrophages in emphysema. Am J Respir Crit Care Med 156(1):240–247
Fitzpatrick AM, Holguin F, Teague WG, Brown LAS (2008) Alveolar macrophage phagocytosis is impaired in children with poorly controlled asthma. J Allergy Clin Immunol 121(6):1372–1378. doi:10.1016/j.jaci.2008.03.008
Frankenberger M, Passlick B, Hofer T, Siebeck M, Maier KL, Ziegler-Heitbrock LH (2000) Immunologic characterization of normal human pleural macrophages. Am J Respir Cell Mol Biol 23(3):419–426
Frankenberger M, Eder C, Hofer TP, Heimbeck I, Skokann K, Kassner G, Weber N, Moller W, Ziegler-Heitbrock L (2011) Chemokine expression by small sputum macrophages in COPD. Mol Med 17(7–8):762–770. doi:10.2119/molmed.2010.00202
George SN, Garcha DS, Mackay AJ, Patel ARC, Singh R, Sapsford RJ, Donaldson GC, Wedzicha JA (2014) Human rhinovirus infection during naturally occurring COPD exacerbations. Eur Respir J 44:87–96
Gern JE, Dick EC, Lee WM, Murray S, Meyer K, Handzel ZT, Busse WW (1996) Rhinovirus enters but does not replicate inside monocytes and airway macrophages. J Immunol 156(2):621–627
Girodet PO, Nguyen D, Mancini JD, Hundal M, Zhou X, Israel E, Cernadas M (2016) Alternative macrophage activation is increased in asthma. Am J Respir Cell Mol Biol 55(4):467–475. doi:10.1165/rcmb.2015-0295OC
Haggie PM, Verkman AS (2007) Cystic fibrosis transmembrane conductance regulator-independent phagosomal acidification in macrophages. J Biol Chem 282(43):31422–31428. doi:10.1074/jbc.M705296200
Han MK, Huang YJ, LiPuma JJ, Boushey HA, Boucher RC, Cookson WO, Curtis JL, Erb-Downward J, Lynch SV, Sethi S, Toews GB, Young VB, Wolfgang MC, Huffnagle GB, Martinez FJ (2012) Significance of the microbiome in obstructive lung disease. Thorax 67(5):456–463. doi:10.1136/thoraxjnl-2011-201183
Harvey CJ, Thimmulappa RK, Sethi S, Kong X, Yarmus L, Brown RH, Feller-Kopman D, Wise R, Biswal S (2011) Targeting Nrf2 signaling improves bacterial clearance by alveolar macrophages in patients with COPD and in a mouse model. Sci Transl Med 3(78):78ra32. doi:10.1126/scitranslmed.3002042
Henson PM, Tuder RM (2008) Apoptosis in the lung: induction, clearance and detection. Am J Physiol Lung Cell Mol Physiol 294(4):L601–L611. doi:10.1152/ajplung.00320.2007
Hill AT, Campbell EJ, Hill SL, Bayley DL, Stockley RA (2000) Association between airway bacterial load and markers of airway inflammation in patients with stable chronic bronchitis. Am J Med 109(4):288–295
Hodge S, Hodge G, Scicchitano R, Reynolds PN, Holmes M (2003) Alveolar macrophages from subjects with chronic obstructive pulmonary disease are deficient in their ability to phagocytose apoptotic airway epithelial cells. Immunol Cell Biol 81(4):289–296. doi:10.1046/j.1440-1711.2003.t01-1-01170.x
Hodge S, Hodge G, Holmes M, Reynolds PN (2005) Increased airway epithelial and T-cell apoptosis in COPD remains despite smoking cessation. Eur Respir J 25(3):447–454
Hodge S, Hodge G, Ahern J, Jersmann H, Holmes M, Reynolds PN (2007) Smoking alters alveolar macrophage recognition and phagocytic ability: implications in chronic obstructive pulmonary disease. Am J Respir Cell Mol Biol 37(6):748–755. doi:10.1165/rcmb.2007-0025OC
Hodge S, Hodge G, Jersmann H, Matthews G, Ahern J, Holmes M, Reynolds PN (2008) Azithromycin improves macrophage phagocytic function and expression of mannose receptor in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2008(178):2
Hodge S, Matthews G, Mukaro V, Ahern J, Shivam A, Hodge G, Holmes M, Jersmann H, Reynolds PN (2010) Cigarette smoke-induced changes to alveolar macrophage phenotype and function is improved by treatment with procysteine. Am J Respir Cell Mol Biol 44(5):673–681. doi:10.1165/rcmb.2009-0459OC
Huynh ML, Malcolm KC, Kotaru C, Tilstra JA, Westcott JY, Fadok VA, Wenzel SE (2005) Defective apoptotic cell phagocytosis attenuates prostaglandin E2 and 15-hydroxyeicosatetraenoic acid in severe asthma alveolar macrophages. Am J Respir Crit Care Med 172(8):972–979. doi:10.1164/rccm.200501-035OC
Ito K, Ito M, Elliott WM, Cosio B, Caramori G, Kon OM, Barczyk A, Hayashi S, Adcock IM, Hogg JC, Barnes PJ (2005) Decreased histone deacetylase activity in chronic obstructive pulmonary disease. N Engl J Med 352(19):1967–1976. doi:10.1056/NEJMoa041892
Jeffery PK (1999) Differences and similarities between chronic obstructive pulmonary disease and asthma. Clin Exp Allergy 29(Suppl 2):14–26
Kirkham PA, Spooner G, Rahman I, Rossi AG (2004) Macrophage phagocytosis of apoptotic neutrophils is compromised by matrix proteins modified by cigarette smoke and lipid peroxidation products. Biochem Biophys Res Commun 318(1):32–37. doi:10.1016/j.bbrc.2004.04.003
Kopf M, Schneider C, Nobs SP (2015) The development and function of lung-resident macrophages and dendritic cells. Nat Immunol 16(1):36–44. doi:10.1038/ni.3052
Lay JC, Alexis NE, Zeman KL, Peden DB, Bennett WD (2009) In vivo uptake of inhaled particles by airway phagocytes is enhanced in patients with mild asthma compared with normal volunteers. Thorax 64(4):313–320
Liang Z, Zhang Q, Thomas CM, Chana KK, Gibeon D, Barnes PJ, Chung KF, Bhavsar PK, Donnelly LE (2014) Impaired macrophage phagocytosis of bacteria in severe asthma. Respir Res 15:72
Lofdahl JM, Wahlstrom J, Skold CM (2006) Different inflammatory cell pattern and macrophage phenotype in chronic obstructive pulmonary disease patients, smokers and non-smokers. Clin Exp Immunol 145(3):428–437. doi:10.1111/j.1365-2249.2006.03154.x
Lundborg M, Johard U, Lastbom L, Gerde P, Camner P (2001) Human alveolar macrophage phagocytic function is impaired by aggregates of ultrafine carbon particles. Environ Res 86(3):244–253. doi:10.1006/enrs.2001.4269
Mallia P, Message SD, Gielen V, Contoli M, Gray K, Kebadze T, Aniscenko J, Laza-Stanca V, Edwards MR, Slater L, Papi A, Stanciu LA, Kon OM, Johnson M, Johnston SL (2011) Experimental rhinovirus infection as a human model of chronic obstructive pulmonary disease exacerbation. Am J Respir Crit Care Med 183(6):734–742. doi:10.1164/rccm.201006-0833OC
Metcalfe HJ, Lea S, Hughes D, Khalaf R, Abbott-Banner K, Singh D (2014) Effects of cigarette smoke on Toll-like receptor (TLR) activation of chronic obstructive pulmonary disease (COPD) macrophages. Clin Exp Immunol 176(3):461–472. doi:10.1111/cei.12289
Morimoto K, Janssen WJ, Terada M (2012) Defective efferocytosis by alveolar macrophages in IPF patients. Respir Med 106(12):1800–1803. doi:10.1016/j.rmed.2012.08.020
Nielsen H, Bonde J (1986) Association of defective monocyte chemotaxis with recurrent acute exacerbations in chronic obstructive lung disease. Eur J Respir Dis 68(3):200–206
Oliver BG, Lim S, Wark P, Laza-Stanca V, King N, Black JL, Burgess JK, Roth M, Johnston SL (2008) Rhinovirus exposure impairs immune responses to bacterial products in human alveolar macrophages. Thorax 63(6):519–525
Pappas K, Papaioannou AI, Kostikas K, Tzanakis N (2013) The role of macrophages in obstructive airways disease: chronic obstructive pulmonary disease and asthma. Cytokine 64(3):613–625. doi:10.1016/j.cyto.2013.09.010
Park GY, Christman JW (2016) Hidden in plain sight: the overlooked role of pulmonary macrophages in the pathogenesis of asthma. Am J Respir Cell Mol Biol 55(4):465–466. doi:10.1165/rcmb.2016-0188ED
Pons AR, Noguera A, Blanquer D, Sauleda J, Pons J, Agustí AGN (2005) Phenotypic characterisation of alveolar macrophages and peripheral blood monocytes in COPD. Eur Respir J 25:647–652
Ritts RE, Miller RD, LeDuc PV, Offord KP (1976) Phagocytosis and cutaneous delayed hypersensitivity in patients with chronic obstructive pulmonary disease. Chest 69(4):474–478
Russell RE, Culpitt SV, DeMatos C, Donnelly L, Smith M, Wiggins J, Barnes PJ (2002a) Release and activity of matrix metalloproteinase-9 and tissue inhibitor of metalloproteinase-1 by alveolar macrophages from patients with chronic obstructive pulmonary disease. Am J Respir Cell Mol Biol 26(5):602–609. doi:10.1165/ajrcmb.26.5.4685
Russell RE, Thorley A, Culpitt SV, Dodd S, Donnelly LE, Demattos C, Fitzgerald M, Barnes PJ (2002b) Alveolar macrophage-mediated elastolysis: roles of matrix metalloproteinases, cysteine, and serine proteases. Am J Physiol Lung Cell Mol Physiol 283(4):L867–L873
Sapey E, Stockley RA (2006) COPD exacerbations: aetiology. Thorax 61(3):250–258
Savici D, Campbell PA, King TE Jr (1989) Bronchoalveolar macrophages from patients with idiopathic pulmonary fibrosis are unable to kill facultative intracellular bacteria. Am Rev Respir Dis 139(1):22–27. doi:10.1164/ajrccm/139.1.22
Shaykhiev R, Krause A, Salit J, Strulovici-Barel Y, Harvey BG, O’Connor TP, Crystal RG (2009) Smoking-dependent reprogramming of alveolar macrophage polarization: implication for pathogenesis of chronic obstructive pulmonary disease. J Immunol 183(4):2867–2883. doi:10.4049/jimmunol.0900473
Simonin-Le Jeune K, Le Jeune A, Jouneau S, Belleguic C, Roux PF, Jaguin M, Dimanche-Boitre MT, Lecureur V, Leclercq C, Desrues B, Brinchault G, Gangneux JP, Martin-Chouly C (2013) Impaired functions of macrophage from cystic fibrosis patients: CD11b, TLR-5 decrease and sCD14, inflammatory cytokines increase. PLoS One 8(9):e75667. doi:10.1371/journal.pone.0075667
Singh AM, Busse WW (2006) Asthma exacerbations. 2: aetiology. Thorax 61(9):809–816. doi:10.1136/thx.2005.045179
Stahl M, Schupp J, Jäger B, Schmid M, Zissel G, Müller-Quernheim J, Prasse A (2013) Lung collagens perpetuate pulmonary fibrosis via CD204 and M2 macrophage activation. PLoS One 8(11):e81382. doi:10.1371/journal.pone.0081382
Staples KJ, Hinks TS, Ward JA, Gunn V, Smith C, Djukanovic R (2012) Phenotypic characterization of lung macrophages in asthmatic patients: overexpression of CCL17. J Allergy Clin Immunol 130(6):1404–1412 (e1407). doi:10.1016/j.jaci.2012.07.023
Taylor AE, Finney-Hayward TK, Quint JK, Thomas CM, Tudhope SJ, Wedzicha JA, Barnes PJ, Donnelly LE (2010) Defective macrophage phagocytosis of bacteria in COPD. Eur Respir J 35(5):1039–1047. doi:10.1183/09031936.00036709
Valenza G, Tappe D, Turnwald D, Frosch M, Konig C, Hebestreit H, Abele-Horn M (2008) Prevalence and antimicrobial susceptibility of microorganisms isolated from sputa of patients with cystic fibrosis. J Cyst Fibros 7(2):123–127
Vandivier RW, Fadok VA, Hoffmann PR, Bratton DL, Penvari C, Brown KK, Brain JD, Accurso FJ, Henson PM (2002) Elastase-mediated phosphatidylserine receptor cleavage impairs apoptotic cell clearance in cystic fibrosis and bronchiectasis. J Clin Invest 109(5):661–670. doi:10.1172/JCI13572
Vandivier RW, Henson PM, Douglas IS (2006) Burying the dead: the impact of failed apoptotic cell removal (efferocytosis) on chronic inflammatory lung disease. Chest 129(6):1673–1682. doi:10.1378/chest.129.6.1673
Vecchiarelli A, Dottorini M, Puliti M, Todisco T, Cenci E, Bistoni F (1991) Defective candidacidal activity of alveolar macrophages and peripheral blood monocytes from patients with chronic obstructive pulmonary disease. Am Rev Respir Dis 143(5 Pt 1):1049–1054. doi:10.1164/ajrccm/143.5_Pt_1.1049
Walsh GM (2008) Defective apoptotic cell clearance in asthma and COPD—a new drug target for statins? Trends Pharmacol Sci 29(1):6–11. doi:10.1016/j.tips.2007.11.002
Wedzicha JA, Donaldson GC (2003) Exacerbations of chronic obstructive pulmonary disease. Respir Care 48(12):1204–1213. Discussion 1213–1205
Wellington M, Bliss JM, Haidaris CG (2003) Enhanced phagocytosis of Candida species mediated by opsonization with recombinant human antibody single chain variable fragment. Infect Immun 71(12):7228–7231
Wilkinson TM, Patel IS, Wilks M, Donaldson GC, Wedzicha JA (2003) Airway bacterial load and FEV1 decline in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 167(8):1090–1095. doi:10.1164/rccm.200210-1179OC
Wojtan P, Mierzejewski M, Osinska I, Domagala-Kulawik J (2016) Macrophage polarization in interstitial lung diseases. Cent Eur J Immunol 41(2):159–164. doi:10.5114/ceji.2016.60990
Wright AK, Rao S, Range S, Eder C, Hofer TP, Frankenberger M, Kobzik L, Brightling C, Grigg J, Ziegler-Heitbrock L (2009) Pivotal advance: expansion of small sputum macrophages in CF: failure to express MARCO and mannose receptors. J Leukoc Biol 86(3):479–489. doi:10.1189/jlb.1108699
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this chapter
Cite this chapter
Belchamber, K.B.R., Donnelly, L.E. (2017). Macrophage Dysfunction in Respiratory Disease. In: Kloc, M. (eds) Macrophages. Results and Problems in Cell Differentiation, vol 62. Springer, Cham. https://doi.org/10.1007/978-3-319-54090-0_12
Download citation
DOI: https://doi.org/10.1007/978-3-319-54090-0_12
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-54089-4
Online ISBN: 978-3-319-54090-0
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)