Abstract
Umbilical cord blood (UCB) is a valuable alternative source of hematopoietic stem and progenitor cells (HSPCs) for patients in need of allogeneic hematopoietic stem cell transplantation (HSCT), who lack suitable human leukocyte antigen (HLA)-matched adult donors. Compared to peripherally mobilized or bone marrow, HSPC units from unrelated adult donors, UCB grafts have the advantage of immediate availability, absence of risk to the donors and lower immunogenicity, which allows for a greater degree of HLA incompatibility. However, UCB grafts contain a lower number of nucleated cells and mostly naïve T cells that do not transfer protective T-cell memory, resulting in delayed engraftment and immune reconstitution, especially in the early posttransplant period. As a result, control of viral infections remains a challenge, and patients undergoing UCB transplantation (UCBT) are at increased risk for infectious complications and mortality. In this chapter, we will review the unique characteristics of UCB grafts, the factors that account for the pattern and kinetics of immune reconstitution after UCBT, and the significance of the adaptive immune system recovery for long-term outcomes in adult recipients of UCBT.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
1 Unique Characteristics of Immune Cells in the UCB Graft
The unique composition and properties of cells contained in UCB units (Table 12.1) may account, at least in part, for the distinct patterns of hematopoietic and immune reconstitution after UCBT. UCB contains higher numbers of CD4+ and CD8+ T-cells compared to adult peripheral blood (PB) (Szabolcs et al. 2003), although the absolute counts of immune cells are lower compared to peripherally mobilized or bone marrow (BM) adult stem cell grafts (Storek 2008). In addition, the majority of UCB CD4+ and CD8+ T-cells are phenotypically naïve (CD45RA+CD62L+), in contrast to adult PB, which contains predominantly memory T-cells (Szabolcs et al. 2003; Chalmers et al. 1998). UCB T-cells produce less IL-2, IL-4, IFN-γ, and TNF-α in response to mitogens (Chalmers et al. 1998). The deficient production of cytokines by stimulated UCB T-cells may be due to the reduced expression of NFAT1 or NFAT-associated genes (Kadereit et al. 1999; Kaminski et al. 2003). While UCB T-cells display vigorous proliferation after allogeneic stimulation, they have decreased antigen-specific cytotoxicity (Risdon et al. 1994). This might be explained by aberrations in the Fas ligand pathway and the decreased perforin expression (Sato et al. 1999; Berthou et al. 1995). Despite an intrinsic Tc2-Th2 bias (Szabolcs and Niedzwiecki 2007), UCB T-cells can rapidly acquire Tc1/Th1 function and mediate enhanced antitumor effects compared to adult PB T-cells in a murine model of B-cell lymphoma (Hiwarkar et al. 2015).
UCB is enriched in CD4+CD25+ T regulatory cells (Tregs), which express Foxp3 and exhibit potent suppression function, independent of IL-10 or TGF-β (Godfrey et al. 2005). UCB Tregs are characterized by higher expression of the naïve markers CD45RA and CD38 and lower expression of activation markers CD45RO and HLA-DR in comparison to adult PB Tregs. Freshly isolated UCB Tregs are incapable of suppressing alloantigen-induced proliferation (Wing et al. 2003; Chang et al. 2005), a property that has been attributed to their naïve state, but can effectively suppress T-cell responses after stimulation (Wing et al. 2003; Takahata et al. 2004). Interestingly, after allogeneic stimulation, CTLA4 expression on Tregs derived from UCB CD4+CD25– T-cells is induced at a higher rate compared to CD4+CD25– T-cells derived from adult HSPC grafts (Chang et al. 2005). UCB Tregs also have a higher expansion capacity to anti-CD3, anti-CD28 and IL-2, which correlates with overexpression of genes involved in proliferation and chromatin remodeling (Torelli et al. 2012).
Similarly to T-cells, UCB B-cells are predominantly naïve and are characterized by the expression of CD5 and sIgM (B1 cells), whereas CD23-expressing B-cells are less frequent compared to adult PB (Szabolcs et al. 2003). These UCB B-cells can produce poly-reactive IgM antibodies but display decreased capacity for Ig class switching and production of IgA or IgG upon stimulation (Hayward and Lawton 1977; Durandy et al. 1990). Furthermore, UCB B-cells have increased susceptibility to spontaneous apoptosis (Kessel et al. 2006). CD56bright and CD56dim NK subsets are present at similar proportions in UCB and PB, although UCB also contains a significant population of NK progenitors, including CD16+CD56– cells (Verneris and Miller 2009; Gaddy and Broxmeyer 1997; Gaddy et al. 1995). UCB NK cells have high-level expression of the inhibitory receptor NKG2A/CD94 and low-level expression of granzyme B, resulting in decreased NK-cell activity compared to adult NK cells (Wang et al. 2007). Decreased expression of adhesion molecules may also account for the decreased NK-cell activity (Tanaka et al. 2003). UCB dendritic cells (DCs) also display unique properties and are characterized by lower surface expression of major histocompatibility complex (MHC) and cell adhesion molecules (Hunt et al. 1994), decreased upregulation of costimulatory molecules or activation markers (CD80, CD86, CD86), and markedly decreased production of IL-12 in response to LPS stimulation (Langrish et al. 2002; Wong et al. 2005). Thus, UCB DCs are functionally immature with impaired ability to stimulate T-cell responses. Instead, UCB DCs efficiently induce CD4+ T-cells with a Treg phenotype (Encabo et al. 2007). UCB is also characterized by a higher ratio of plasmacytoid to myeloid DCs compared to adult PB (Crespo et al. 2004). These observations support the notion that UCB DCs are biased against Th1 responses and toward induction of immune tolerance (Langrish et al. 2002; Wong et al. 2005; Crespo et al. 2004).
2 Mechanisms and Pathways of T-Cell Reconstitution After UCBT
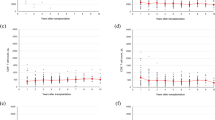
While the innate immune system recovers within weeks after transplantation, the restoration of the adaptive T-cell immunity is delayed for several months. Recovery of T-cells after HSCT follows two different pathways, one peripheral or thymus-independent and one central or thymus-dependent pathway. These two pathways of T-cell reconstitution act in parallel but follow different kinetics (Williams et al. 2007) (Fig. 12.1).
Reconstitution of the T-cell compartment after UCBT. Conditioning chemoradiation prior to UCBT results in profound lymphopenia and immunodeficiency of the host. T-cell reconstitution after UCBT is achieved by two independent mechanisms: The thymus-independent pathway of T-cell reconstitution predominates in the early post transplant period and is mediated by adoptively transferred UCB T-cells, which are uniformly naïve and do not transfer protective immune memory, or recipient T-cells that survive conditioning. These T-cell populations undergo peripheral expansion in response to lymphopenia and high cytokine levels (IL-7, IL-15 etc), or oligoclonal proliferation upon interaction with cognate antigen. Overtime, this early peripheral T-cell expansion results in late effector memory T-cell skewing and contraction of the T-cell repertoire diversity, and is associated with impaired immunologic responses to antigens. Reconstitution of a functionally competent T-cell compartment with broad antigenic specificity eventually requires the de novo production of naïve T-cells by the thymus of the USCT recipient. This thymus-dependent pathway of T-cell reconstitution is a prolonged multistep process. LMPs contained in the UCB graft or arising from the engrafted donor-derived HSCs migrate via circulation and repopulate the thymus with thymocyte precursors that can reconstitute thymopoiesis. The thymus provides the essential microenvironment (stroma) that supports T-cell proliferation, selection and differentiation into Recent Thymic Emigrants. Several factors can delay the recovery of thymopoiesis after UCBT, including low number of LMPs (as a result of low nucleated cell dose of UCB and delayed engraftment), advanced recipient age with resultant thymic involution and thymic damage from the conditioning chemoradiation or GvHD. Although slow, the thymus-dependent mechanism is imperative for the renewal of peripheral T-cell pool and constant export of new naïve T-cells with broad TCR repertoire diversity, capable of responding to a great spectrum of antigens. (This research was originally published in Blood. Politikos I and Boussiotis VA. The role of thymus in T-cell immune reconstitution after umbilical cord blood transplantation. Blood. 2014; Vol 124:3201–3211. © the American Society of Hematology)
2.1 Peripheral or Thymus-Independent Pathway of T-Cell Reconstitution
In the early posttransplant period, the thymus-independent pathway predominates and is mediated by adoptively transferred donor T-cells contained in the graft or recipient T-cells surviving conditioning chemotherapy. These T-cells proliferate following antigen encounter (Mackall et al. 1996) or undergo lymphopenia-driven homeostatic peripheral expansion (HPE) through low-affinity interactions with self-peptide MHC complexes under the influence of homeostatic cytokines, which are highly elevated during this posttransplant period (Goldrath and Bevan 1999). Among these cytokines, IL-7 is a critical regulator of the thymus-independent pathway (Fry et al. 2001). Studies in HSCT recipients have shown that IL-7 levels rise in the posttransplant period and inversely correlate with T-cell counts, most likely due to decreased consumption (Bolotin et al. 1999; Dean et al. 2008). In double unit UCBT (dUCBT) recipients, IL-7 levels remain elevated for a prolonged time compared to recipients of adult donor HSPC, and inversely correlate with T-cell counts, especially CD4+ T-cells (Politikos et al. 2015).
In contrast to BM or peripherally mobilized HSPC grafts that contain a large number of memory T-cells, UCB grafts contain T-cells that are almost exclusively naïve. As a consequence, UCB T-cells display a complete T-cell receptor (TCR) repertoire at birth (Garderet et al. 1998). However, they are subject to the stringent requirements of naïve T-cells during mounting of primary immune responses which cannot provide efficient protection, in contrast to memory T-cells which develop rapid antigen-specific recall responses. As a result, protection against pathogens during the early posttransplant period is impaired and depends on memory T-cells of host origin that survive conditioning chemotherapy (Chalandon et al. 2006). During HPE, UCB T-cells lose their naïve phenotype and acquire an effector or memory-like phenotype in an antigen-independent manner (Mackall et al. 1993; Cho et al. 2000). At the same time, antigen-driven proliferation of UCB T-cells circulating in the UCBT recipient results in oligoclonal expansion and contraction of TCR repertoire diversity. Moreover, apoptotic cell death of the activated T-cells during homeostatic activation and/or antigen exposure may lead to contraction of the T-cell compartment over time (Hakim et al. 1997). As a result of these concurrent mechanisms, the thymus-independent pathway cannot sustain a diverse TCR repertoire with broad antigenic specificity that ensures immune competence (Roux et al. 1996).
2.2 Central or Thymus-Dependent Pathway of T-Cell Reconstitution
The central or thymus-dependent pathway of T-cell recovery involves the de novo production of T-cells by the thymus, which is critical for successful long-term immune reconstitution (Politikos and Boussiotis 2014). This pathway generates naive T-cells with broad antigenic specificity, and it is essential for the restoration of TCR repertoire diversity (Roux et al. 2000; Dumont-Girard et al. 1998). Restoration of thymopoiesis is a multistep process that begins with the seeding of the thymus with lymphoid-myeloid progenitors (LMPs) derived from the engrafted donor HSPCs. Upon entry in the thymic cortex, LMPs undergo T-cell lineage commitment under the influence of Notch signaling and interactions with cortical thymic epithelial cells (TECs) (De Smedt et al. 2002; Taghon et al. 2009). During intrathymic T-cell development, thymocytes undergo sequential rearrangement of the TCR beta (TCRB) and alpha (TCRA) loci and develop into double-positive (DP) thymocytes, which are subject to positive selection based on their ability to bind self-peptide/self-MHC complexes with appropriate affinity. Positively selected DP thymocytes continue their development into CD4 or CD8 single-positive (SP) thymocytes, migrate to the medulla via the upregulation of the chemokine receptor CCR7, and undergo negative selection by medullary TECs, which have the unique capability to promiscuously express tissue-restricted antigens (TSAs) under the influence of the transcription factor Aire (Anderson et al. 2002, 2005). The negative selection process ensures the elimination of self-reactive lymphocytes. The small number of T-cells that successfully proceed through these intrathymic steps is exported to the periphery and is termed recent thymic emigrants (RTEs).
3 Factors Influencing T-Cell Immune Reconstitution After UCBT
3.1 Graft-Related Factors
Several factors can affect the timing and efficiency of immune reconstitution after UCBT. Graft-related factors such as limited number of stem cells and lymphocytes, T-cell naivety, immaturity, and lack of memory T-cells have the greatest impact on the thymus-independent pathway of T-cell recovery. Specifically, total nucleated cell (TNC) and CD3+ T-cell content in UCB units positively correlate with lymphocyte recovery in the early posttransplant period after UCBT (Niehues et al. 2001; Castillo et al. 2016). It is conceivable that the low stem cell dose of UCB grafts and the delayed engraftment result in delayed emergence of LMPs that repopulate the thymus and restore thymopoiesis. Thus, the properties of the UCB graft may also affect the thymus-dependent pathway of immune reconstitution. Interestingly, although the number of HSPC clones contributing to thymic seeding and intrathymic T-cell development is restricted, this very limited number of HSPC clones can give rise to a fully diverse TCR repertoire. Thus, immunodeficiency after UCBT may not be a consequence of low HSPC numbers but may rather be related to intrathymic events (Brugman et al. 2015). An additional important mechanism regulating immune reconstitution is related to the frequent HLA discordance between the UCB graft and the host, due to the less stringent requirements for HLA matching during UCBT. The intrathymic positive and negative selection is dictated by MHC expression of thymic epithelial cells, which remain of host origin after transplantation, in contrast to the donor-derived LMPs that repopulate the thymus (Krenger and Hollander 2008). As a result, MHC mismatches between graft and the host might adversely impact immune reconstitution, by compromising thymic selection and leading to skewed TCR repertoire diversity (Roux et al. 2000; Krenger and Hollander 2008; Eyrich et al. 2003).
3.2 Host-Related Factors
Host-related factors also influence immune reconstitution. Recipient’s age has a critical impact on T-cell reconstitution. Compared to adults, pediatric patients receive higher TNC and CD3+ cell doses adjusted per body weight resulting in faster neutrophil engraftment and lymphocyte recovery. In addition, the decreased thymic function that occurs with aging as a result of thymic involution (Mackall et al. 1995; Douek et al. 1998) might pose a rate-limiting step in the immune reconstitution after HSCT. In support of this hypothesis, the recipient’s age is inversely associated with the onset and extent of thymopoietic recovery after HSCT or UCBT (Klein et al. 2001; Clave et al. 2009; Uhlin et al. 2012). Furthermore, the pretransplant thymic function of the host plays a role in the rate of thymic recovery (Mackall et al. 1995; Chen et al. 2005; Clave et al. 2005).
3.3 Treatment-Related Factors
Factors related to the transplantation procedure or posttransplant complications may affect the rate and success of immune reconstitution. The use of in vivo T-cell depletion by means of ATG has a detrimental effect on the early thymus-independent T-cell recovery (Admiraal et al. 2015; Lindemans et al. 2014). A negative effect of ATG on the thymus-dependent pathway has also been implied (Sairafi et al. 2012). Reduced intensity conditioning (RIC) regimens may provoke less damage to the peripheral niches in which T-cell proliferation takes place, thus allowing for a faster immune recovery (Uhlin et al. 2012; Sairafi et al. 2012; Chao et al. 2002). Furthermore, radiation-based conditioning regimens may lead to delayed thymus-dependent T-cell reconstitution, likely by inducing greater thymic destruction (Glowala-Kosinska et al. 2016; Chung et al. 2001). It should also be noted that the thymus is a target organ of graft-versus-host disease (GvHD), which affects both its lymphoid and stromal compartments (Krenger and Hollander 2008). Importantly, the development of acute and chronic GvHD has been associated with delayed T-cell reconstitution (Clave et al. 2009; Uhlin et al. 2012; Weinberg et al. 2001) not only because the thymus is a target organ of GvHD, but also because corticosteroid therapy for the treatment of GvHD can lead to lymphodepletion.
4 Assessment of Immune Reconstitution After UCBT
Several tools are available for the study of immune recovery after transplantation, both in the clinical or research settings. Hemograms provide an assessment of myeloid engraftment and quantitative recovery of lymphocytes by measurement of absolute lymphocyte count (ALC). Flow cytometry provides a means for the enumeration of lymphocyte subsets and monitoring of CD4+, CD8+, B, and NK cells is commonly used in the clinical practice to guide decisions regarding the management of transplant recipients, such as discontinuation of prophylactic antiviral therapy and timing of vaccination. Flow cytometry is also a valuable tool for the study of thymopoieisis because it allows quantification of RTEs based on the expression of the CD45 isoform, CD45RA (Mackall et al. 1993). Additional surface markers, such as CCR7, CD31, CD62L, and CD27, have improved the differentiation between naïve and memory T-cells (McFarland et al. 2000). Quantification of T-cell receptor excision circles (TRECs), which are DNA by-products of the intrathymic TCR sequential rearrangement events, also provides an excellent assessment of the thymic function (Politikos and Boussiotis 2014; Douek et al. 1998). Additionally, because diversification of the T-cell repertoire after HSCT depends on the de novo production of naïve T-cells, assessment of the TCR diversity by CDR3 spectratyping or by sequencing of the TCR β chain can also provide information about the ability of thymopoiesis to reconstitute a competent T-cell immune system (Douek et al. 2000; Robins et al. 2009). Because these assays provide only quantitative assessment, approaches to evaluate pathogen-specific T-cell responses such as cytokine flow cytometry (CFC) or enzyme-linked immunosorbent spot (ELISpot) are valuable tools for the assessment of immune competence.
5 Quantitative Immune Reconstitution After UCBT
5.1 Immune Reconstitution in Adults After Single-Unit UCBT
Adult patients undergoing single-unit CBT (sUCBT) after ATG-containing myeloablative conditioning (MAC) have delayed neutrophil engraftment and slower ALC recovery during the first 2 months after transplantation compared to matched unrelated donor (MUD) transplant recipients. However, ALC recovery in the sUCBT group surpassed that of MUD recipients beyond day 180 and reached normal range by day +200. While bacterial infections were more common in the sUCBT group early posttransplant, there was no significant difference in the infection rates between the two groups beyond day 50 (Hamza et al. 2004). However, adult patients who receive sUCBT after ATG-containing conditioning may have protracted lymphopenia for up to 2 years posttransplant (Klein et al. 2001). This is most pronounced for the CD4+ T-cells, which remain below normal range until 2 years, whereas CD8+ T-cells reach low normal levels by 1 year. The kinetics of T-cell recovery in adult patients is markedly delayed compared to pediatric UCBT recipients. Moreover, the majority of T-cells during the first year have a memory phenotype.
An important observation is that TREC levels in adult sUCBT recipients remain below the age-adjusted normal range for up to 3 years after transplantation, suggesting a profound thymic deficiency compared to the pediatric control group (Klein et al. 2001). This finding explains, at least in part, the protracted delay in T-cell recovery. Similarly, sUCBT after ATG-containing RIC is associated with extremely suppressed CD4+ and CD8+ numbers at least through 6 months post-UCBT (Komanduri et al. 2007). Under these conditions, CD8+ T-cells approach near-normal levels at 1 year after transplantation, but CD4+ T-cells remain low. Thymopoiesis, as assessed by sjTRECs, is nearly absent in the first year and is associated with a paucity of naïve and central memory T-cells and expansion of terminally differentiated T effector cells. In contrast, NK and B-cells develop a marked expansion to supranormal levels, as early as 30 days post-UCBT.
5.2 Immune Reconstitution in Adults After Double-Unit UCBT
The use of dUCBT has been employed to circumvent the cell dose limitation in adult patients and to enhance hematopoietic and immune reconstitution. Analysis of immune reconstitution in adult patients undergoing dUCBT (Cutler et al. 2011) and comparison between dUCB and peripherally mobilized HSPC MUD transplantation after RIC (Jacobson et al. 2012) revealed that CD3+, naïve and memory CD4+, CD8+, and CD4+CD25+ Treg numbers were significantly lower in dUCBT recipients during the first 6 months after transplantation. The inclusion of ATG only in the dUCBT group may have contributed to this observation. By 12 months, no significant difference was observed between the two groups, and, by 24 months, the median number of naïve CD4+ T-cells in the dUCBT cohort surpassed that in the MUD cohort. In addition, dUCBT recipients seemed to have higher CD123+ plasmacytoid DCs in the first year compared to MUD, but the difference disappeared at later time points. Infections were more frequent in the dUCBT group, but the non-relapse mortality (NRM) was not different (Jacobson et al. 2012). In addition, ATG may also cause a delay in the emergence of IFN-γ-secreting T-cells in response to immunogenic viral antigens, suggesting that the early post-UCBT period after ATG-containing conditioning is characterized not only by quantitative but also by qualitative/functional immunologic defect in adaptive immunity (Saliba et al. 2015).
Comparison of immune reconstitution patterns between adult patients undergoing dUCBT and patients undergoing HSCT from matched sibling donors (MSD) or HSCT from MUD after ATG-free MAC regimens has provided evidence that ALC is lower in dUCBT recipients at 1.5 months but reaches similar levels to those in MSD/MUD recipients by 3 months (Kanda et al. 2012). CD3+, CD4+, CD8+, CD4+CD25+CD62L+ (Treg), and CD4+CD45RA+CD62L+, which represent RTE counts, are significantly lower after dUCBT during the first 3–6 months, but at 1 year after transplantation, there is no difference in T-cell subsets between dUCBT and MSD/MUD recipients. As a result of the delayed T-cell recovery, dUCBT recipients have a significantly higher incidence of CMV reactivation and CMV disease, compared to MSD/MUD recipients. Notably, at 6 months after transplantation, an increase in TRECs was comparable in dUCBT and MSD/MRD recipients. Moreover, at 12 months, TCRβ repertoire was comparable between the two cohorts. A vigorous recovery of B and NK cells was detected in the dUCBT cohort in this study (Kanda et al. 2012), consistent with previous observations (Jacobson et al. 2012; Brown et al. 2010). UCBT is mainly reserved for patients who lack an MSD or MUD but may have mismatched unrelated donors (MMUD). Comparison between recipients of UCBT and 9/10 MMUD HSCT, after various conditioning regimens, showed largely similar kinetics of lymphocyte recovery and infectious complications (Servais et al. 2014).
Memorial Sloan Kettering Cancer Center (MSKCC) has reported their experience in adult patients after ATG-free dUCBT and RIC to high-intensity MAC (Sauter et al. 2011). Median ALC was within normal range by day 60. Median CD4+ T-cell count >200 cells/uL was reached by day 120, and both CD4+ and CD8+ median counts were at the lower limit of normal range by day 180. The infectious risk was heightened during the first 4 months, especially in the context of GvHD, but no infection-related deaths were seen beyond that time point. The use of deep sequencing technology to assess TCR diversity showed that dUCBT recipients have the highest CD4+ and CD8+ TCR diversity compared to recipients of conventional or T-cell-depleted (TCD) HSCT at 6 and 12 months after transplantation (van Heijst et al. 2013). This increased TCR diversity correlated with a substantially greater fraction of naive CD4+ T-cells. An important observation of the study is that diversity of CD4+ T-cells was 50 times higher than that of CD8+ T-cells in all patients. Notably, acute GvHD and steroid therapy did not restrict repertoire recovery, whereas CMV or EBV infections had a negative impact.
An important benefit of double UCB unit infusion is the recovery of thymopoiesis, as assessed by increasing TREC levels, by 6 months post-UCBT. This is in marked contrast to the thymopoietic failure seen in adult patients who receive single UCB unit infusion, especially after in vivo T-cell depletion by ATG (Komanduri et al. 2007). Early thymopoietic recovery is observed in adult dUCBT recipients both after ATG-containing RIC or MAC regimens (Politikos et al. 2015; Brown et al. 2010; Ballen et al. 2012). In both groups, more than half of the patients had detectable, yet below normal range, TRECs at 6 months. By 1 year, median TREC levels reached low normal values. Interestingly, circulating levels of SCF inversely correlate with TRECs at 6 and 12 months post-dUCBT, as well as CD4+CD45RA+ naïve T-cells at 1 year (Politikos et al. 2015). This outcome is likely due to consumption of SCF in the early intrathymic stages of T-cell development, consistent with the critical role of this cytokine in the thymus-dependent pathway of immune reconstitution.
6 Prognostic Significance of Immune Reconstitution for Clinical Outcomes After UCBT
As a result of the delayed neutrophil engraftment and the lack of adoptive immunoprotection due to the naivety of UCB lymphocytes, UCBT is associated with increased risk of infectious complications, which contribute greatly to the early transplant related mortality (TRM) after UCBT (Rubinstein et al. 1998; Laughlin et al. 2004; Rocha et al. 2004). Reactivation of latent viruses that require intact cellular immunity for their control is a major concern after UCBT. Among them, CMV is one of the most commonly reactivated viruses and is associated with significant morbidity and mortality (Szabolcs and Niedzwiecki 2007; Sauter et al. 2011; Dahi et al. 2015; Beck et al. 2010). The rate of CMV reactivation after UCBT ranges widely from 21 to 100% and the rate of CMV disease between 6 and 27% (Beck et al. 2010; Milano et al. 2011; Matsumura et al. 2007; Takami et al. 2005) depending on the characteristics of the study population, such as the number of seropositive patients at risk for reactivation (Albano et al. 2006; Mikulska et al. 2012); method of monitoring CMV reactivation, e.g., pp65 antigenemia vs. PCR viral load monitoring (Dahi et al. 2015; Milano et al. 2011); type of prophylaxis; and use of preemptive treatment (Milano et al. 2011). With the use of sensitive PCR assays essentially all seropositive UCBT recipients develop CMV viremia, although this can be mitigated with intensified antiviral prophylaxis (Dahi et al. 2015; Milano et al. 2011). Notably, the omission of in vivo T-cell depletion by ATG appears to provide protection against CMV reactivation or CMV disease after UCBT (Sauter et al. 2011; Dahi et al. 2015).
Similarly to CMV reactivation, the use of ATG is associated with increased risk of EBV reactivation and an incidence of post-transplant lymphoproliferative disorder (PTLD) as high as 21% (Cutler et al. 2011; Brunstein et al. 2006; Dumas et al. 2013). The risk can be greatly reduced by the avoidance of ATG, close monitoring of EBV viral load, and preemptive therapy with rituximab (Dumas et al. 2013; Blaes et al. 2010; Barker et al. 2001). An increased frequency of HHV-6 reactivation and related complications has also been observed after UCBT (Scheurer et al. 2013; Hill et al. 2012, 2015; Le Bourgeois et al. 2014), although the incidence of encephalitis appears to be low when ATG is omitted (Olson et al. 2014). Similarly, UCBT is associated with increased rate and severity of VZV disease (Vandenbosch et al. 2008), BK viremia, and increased risk of BKV disease (Rorije et al. 2014; Satyanarayana et al. 2015; Silva Lde et al. 2010), as well as higher risk for disseminated adenovirus infection (Robin et al. 2007).
The increased risk for infectious complications in UCBT recipients is most pronounced in the early posttransplant period, as studies have shown comparable infection-related mortality in recipients of UCBT and HSCT from adult donors beyond the first 3–4 months (Sauter et al. 2011; Laughlin et al. 2004; Parody et al. 2006; Barker et al. 2005a). The restoration of adaptive immunity via the thymus-dependent pathway, as well as the lower rates of GvHD, may account for this observation. Furthermore, dUCBT has been associated with enhanced GvL effect and low relapse risk (Ponce et al. 2011; Verneris et al. 2009; Brunstein et al. 2010; Rodrigues et al. 2009). As a result, long-term outcomes of UCBT are comparable to HSCT from conventional graft sources (Ponce et al. 2011).
The prognostic effect and the pathophysiologic link between different immune reconstitution metrics on the clinical outcomes of UCBT have been extensively investigated both in pediatric and adult patients undergoing UCBT. It has been determined that ALC > 200 × 106/L at day 30 after MAC and at day 42 after RIC is independently associated with superior 2-year overall survival (OS) and progression-free survival (PFS) (Burke et al. 2011). For the MAC cohort, ALC > 200 × 106/L at day 30 was also associated with lower number of infections prior to day 30 and lower TRM. However, no significant relationship between ALC and relapse has been observed. An ALC > 150 × 106/L on day 30 after dUCBT is also highly predictive of TRM and OS (Saliba et al. 2015). However, no difference between patients who did or did not develop viral reactivations or infections was identified. Because ALC offers only a crude assessment of immune reconstitution, other studies have focused on lymphocyte subsets to identify the most clinically relevant cell types for successful transplantation outcomes. Among such subsets, CD4+ T-cells are of great importance, and their impact on TRM and survival outcomes after allo-HCT from conventional donors (Berger et al. 2008) or sUCBT in children (Admiraal et al. 2015; Bartelink et al. 2013) has been established. Furthermore, in adult recipients of sUCBT, it has been observed that preservation of CCR7+ T-cells, which identify naïve and central memory T-cell subsets within the CD4+ T-cell compartment, has been associated with significantly longer survival (Komanduri et al. 2007).
The most objective measure of successful immune reconstitution is the ability of the new immune system to provide protection against infections and leukemia relapse. The presence of a proliferative response against herpes viruses has been associated with decreased risk of infection-related death, but is also associated with marked reduction in leukemia relapse, and improved PFS (Parkman et al. 2006). Detection of CMV-specific CD4+ and CD8+ T-cells by CFC in the early post-UCBT period (Komanduri et al. 2007; McGoldrick et al. 2013) suggests that UCB-derived T-cells are primed early after transplantation and can initiate a primary immune response against CMV. However, the development of antigen-specific T-cell responses does not correlate with the recovery of ALC and lymphocyte subsets (Saliba et al. 2015; Cohen et al. 2006), suggesting that quantitative T-cell recovery is not an optimal surrogate of functional immunity after transplantation. Moreover, CMV-specific T-cells detected early after UCBT fail to control viral reactivation in vivo (McGoldrick et al. 2013).
Our group has examined the immunological mechanisms involved in the restoration of successful anti-CMV immunity and control of CMV viremia in a cohort of dUCBT recipients (Brown et al. 2010). CMV-specific effectors were detected by IFN-γ ELISpot assay as early as 8 weeks posttransplant. In spite of the presence of CMV-specific effectors, clearance of CMV viremia was not achieved at this early time point after transplantation but was increasingly observed after 6 months. Notably, clearance of CMV was associated with the recovery of naïve CD4+CD45RA+ T-cells, a finding consistent with the need of CD4+ T-helper cells for the development of a functional CD8+ T-cell response (Shedlock and Shen 2003). Clearance of CMV viremia was associated with the emergence of thymopoiesis as assessed by TREC levels, and patients who attained normal TREC levels (>2000 copies/ug) were more likely to display absence of CMV viremia (Brown et al. 2010). These findings suggest a critical contribution of the thymopoiesis on CD4+ T-cell recovery, anti-CMV immunity, and in vivo control of the virus. Further analysis was performed to examine whether the development of CMV-specific responses and thymic reconstitution might be linked to improved long-term outcomes after dUCBT, which might correlate with restoration of immune responses against other pathogens or tumor antigens. CMV-specific immune responses were associated with improved PFS and OS. Furthermore, patients with TREC levels >2000 copies/ug DNA had superior OS compared with patients whose TRECs remained below 2000 copies/ug (Brown et al. 2010).
These observations were extended in a subsequent study, which assessed the role of thymic reconstitution on long-term outcomes in adult dUCBT recipients. In time-dependent regression analysis, higher TREC levels were associated with lower TRM and superior PFS and OS (Politikos et al. 2015). In contrast, high plasma levels of SCF, a cytokine critically involved in the early intrathymic T-cell development, inversely correlated with TREC levels and predicted for higher TRM and worse OS. No association of TREC levels with relapse was detected. This is in contrast to a study in pediatric recipients of UCBT or haploidentical HSCT, in which low levels of βTREC and sjTRECs before transplantation and at 3–6 months posttransplant were associated with increased incidence of relapse (Clave et al. 2013). These discrepancies between pediatric and adult recipients of UCBT might be related to an age-dependent effect on the thymus-dependent pathway of immune reconstitution and suggest that impaired thymic reconstitution might have a stronger negative prognostic value for the prediction of long-term clinical outcomes in pediatric than in adult UCBT recipients.
7 Expert Point of View
UCB is a valuable source of HSPC and has extended allograft availability to patients who lack suitable adult donors. UCB grafts contain a limited number of stem cells and lymphocytes with unique proliferative and functional properties compared to their adult counterparts. As a result of the UCB composition and transplantation practices, immune reconstitution following UCBT is characterized by the absence of transferred immune memory and prolonged T-cell lymphopenia, with compensatory marked expansion of NK and B-cells in the early posttransplant period. The omission of pharmacologic in vivo T-cell depletion from the conditioning regimen has led to faster quantitative recovery during the thymus-independent phase of immune reconstitution. However, increased infectious risk and TRM remain a concern early post-UCBT. Recovery of thymopoiesis is critical for the restoration of peripheral T-cell compartment and diversification of T-cell repertoire. The kinetics and efficiency of the thymus-dependent immune reconstitution after sUCBT in children and dUCBT in adults appear to be at least as efficient as that observed after allo-HCT from adult donors and provide excellent reconstitution of long-term T-cell immunity. Whether this is due to inherent properties of UCB-derived lymphoid progenitors or due to the lower rates and severity of GvHD, thereby diminishing the immunosuppression burden, remains unknown. Several measures of quantitative, thymus-specific, and pathogen-specific recovery correlate with infectious complications and long-term clinical outcomes of UCBT and have allowed the identification of patients at greatest risk for poor outcome after UCBT. Newer technologies, such as deep sequencing, may allow a global and more comprehensive assessment of the immune system. Future efforts should focus on the development of strategies to enhance the immune reconstitution process in order to improve outcomes of UCB transplantation.
8 Future Directions
Because immune reconstitution has a significant impact on morbidity and mortality at the early posttransplant stage but also on long-term clinical outcomes of UCBT, several approaches have been developed to shorten the period of immune deficiency and to improve reconstitution of adaptive immunity. The use of two UCB units in adults resulted in improved recovery of innate immunity, by enhancing neutrophil engraftment and reducing the risk of graft failure (Barker et al. 2005b; Ballen et al. 2007). Moreover, dUCBT may lead to faster thymic reconstitution compared to sUCBT (Komanduri et al. 2007; Kanda et al. 2012; Brown et al. 2010). This outcome might be related to a cell-dose effect or yet unidentified mechanisms, considering that the majority of patients display single-unit chimerism within 1–3 months post-dUCBT (Barker et al. 2005b) and long-term hematopoiesis and lymphopoiesis by a single UCB unit.
Several groups have investigated methods to reduce the duration of neutropenia after UCBT, either by ex vivo culture of the UCB graft to increase the stem cell dose or by ex vivo priming of UCB grafts to improve homing (Cutler et al. 2013; Delaney et al. 2010; de Lima et al. 2012; Wagner et al. 2016; Popat et al. 2015). Most of these strategies have been tested in the setting of dUCBT platform, in which patients receive one manipulated and one unmanipulated UCB unit. While these approaches have resulted in faster recovery of neutrophils derived from the ex vivo-manipulated UCB unit, long-term hematopoietic engraftment is provided by the unmanipulated unit. Moreover, a beneficial effect on reconstitution of adaptive immunity has not been observed to date.
Cytokine-based approaches to improve posttransplant immune reconstitution are being investigated in preclinical models or early clinical trials, albeit not yet in the setting of UCBT. KGF is a mitogen of TECs and has been shown to enhance thymopoiesis and peripheral T-cell reconstitution by protecting TECs from damage induced by radiation, chemotherapy, or GvHD (Min et al. 2002). A beneficial effect of KGF administration has been observed in murine experimental UCBT models (Wang et al. 2011). However, in human trials, administration of KGF has not shown a discernible benefit on immune recovery (Rizwan et al. 2011). IL-7 is a lymphopoietic cytokine and in mouse studies of allogeneic BMT it has been shown to promote both the thymus-dependent and thymus-independent pathways of T-cell regeneration, as well as B-cell recovery (Mackall et al. 2001). Administration of rhIL-7 has been tested in a phase I trial of patients undergoing T-cell-depleted HSCT and resulted in expansion of effector memory T-cells, increase of virus-specific T-cell responses, and broader TCR diversity (Perales et al. 2012). Sex steroid ablation with LHRH-A in murine BMT models is associated with increased numbers of LMPs in the bone marrow and enhanced peripheral T-cell recovery, perhaps by reversing thymic atrophy (Goldberg et al. 2009). In humans undergoing autologous or allogeneic transplantation, LHRH-A administration before transplant resulted in enhanced naïve and total CD4+ T-cell recovery, diversification of T-cell repertoire, and improved T-cell function (Sutherland et al. 2008). Other candidate cytokines include FLT3L (Fry et al. 2004), IL-15 (Alpdogan et al. 2005), IL-22 (Dudakov et al. 2012), SCF (Wils et al. 2011), and several combinations, which often display synergistic effects (Wils et al. 2012; Kelly et al. 2008). These approaches may form the basis of new clinical trials that might improve reconstitution of adoptive immunity and provide clinical benefit in UCBT recipients.
A different approach to overcome immunodeficiency due to delayed immune reconstitution after UCBT involves the adoptive transfer of cell products that can confer protection against pathogens. In that regard, multi-specific cytotoxic T lymphocytes (CTLs) recognizing multiple viruses including CMV, EBV, HHV-6, BK, and adenovirus can be generated from UCB T-cell populations (Papadopoulou et al. 2014). These multi-specific CTLs may be highly beneficial for the prevention or treatment of viral disease in UCBT recipients. The use of third party, partially HLA matched, in vitro-expanded EBV-specific CTLs have already been used with success in the treatment of post-UCBT EBV-associated PTLD (Barker et al. 2010). This “off-the-shelf” approach, which is currently being extended to the generation of CTL with specificity for other pathogens, might be particularly beneficial to UCBT recipients, who cannot rely on donor-derived CTLs for transfer of protective immunity. Adoptive transfer of UCB NK cells to prevent relapse is also being evaluated in early studies (Verneris and Miller 2009). As mentioned above, a major complication of UCBT is the prolonged impairment of thymic function. Recently, it was discovered that human progenitor T-cells, differentiated in vitro from UCB stem cells with the use of OP9-DL1 culture system, could be a source of thymus-seeding progenitors when infused in NSG mice. Importantly, a subset of in vitro-derived progenitor human T-cell populations could also restore thymic architecture and, when co-infused with HSPCs, were able to promote HSPC-derived T-cell lymphopoiesis (Awong et al. 2013). Together these ongoing research approaches are expected to form the basis for the development of new clinical trials. Such novel strategies to improve either the thymus-dependent or thymus-independent pathways of immune reconstitution may further enhance the outcomes of UCB transplantation.
Abbreviations
- ALC:
-
Absolute lymphocyte count
- CMV:
-
Cytomegalovirus
- CTL:
-
Cytolytic T-cell
- CTLA-4:
-
Cytotoxic T-lymphocyte-associated (protein) 4
- EBV:
-
Epstein-Barr virus
- FLT3:
-
Fms-related tyrosine kinase 3
- HHV-6:
-
Human herpesvirus 6
- HLA:
-
Human lymphocyte antigen (system)
- IFN-γ:
-
Interferon-γ
- IL-2:
-
Interleukin-2
- IL-4:
-
Interleukin-4
- IL-7:
-
Interleukin-7
- IL-10:
-
Interleukin-10
- IL-15:
-
Interleukin-15
- IL-22:
-
Interleukin-22
- KGF:
-
Keratinocyte growth factor
- LHRH-A:
-
Luteinizing hormone-releasing hormone analog
- LMP:
-
Lymphoid-myeloid progenitors
- LPS:
-
Lipopolysaccharide
- NFAT:
-
Nuclear factor of activated T-cells
- NK:
-
Natural killer
- NSG:
-
NOD SCID gamma (mouse strain)
- RTE:
-
Recent thymic emigrants
- SCF:
-
Stem cell factor
- sIgM:
-
Surface immunoglobulin M
- Tc1/2:
-
T cytotoxic 1/T cytotoxic 2
- TEC:
-
Thymic epithelial cells
- TGF-β:
-
Transforming growth factor-β
- Th1/2:
-
T helper 1/ T helper 2
- TNF-α:
-
Tumor necrosis factor-α
- TREC:
-
T-cell receptor excision circles
- Treg:
-
T regulatory
- VZV:
-
Varicella zoster virus
References
Admiraal R, van Kesteren C, Jol-van der Zijde CM, Lankester AC, Bierings MB, Egberts TC, van Tol MJ, Knibbe CA, Bredius RG, Boelens JJ (2015) Association between anti-thymocyte globulin exposure and CD4+ immune reconstitution in paediatric haemopoietic cell transplantation: a multicentre, retrospective pharmacodynamic cohort analysis. Lancet Haematol 2(5):e194–e203
Albano MS, Taylor P, Pass RF, Scaradavou A, Ciubotariu R, Carrier C, Dobrila L, Rubinstein P, Stevens CE (2006) Umbilical cord blood transplantation and cytomegalovirus: posttransplantation infection and donor screening. Blood 108(13):4275–4282
Alpdogan O, Eng JM, Muriglan SJ, Willis LM, Hubbard VM, Tjoe KH, Terwey TH, Kochman A, van den Brink MR (2005) Interleukin-15 enhances immune reconstitution after allogeneic bone marrow transplantation. Blood 105(2):865–873
Anderson MS, Venanzi ES, Klein L, Chen Z, Berzins SP, Turley SJ, von Boehmer H, Bronson R, Dierich A, Benoist C, Mathis D (2002) Projection of an immunological self shadow within the thymus by the aire protein. Science 298(5597):1395–1401
Anderson MS, Venanzi ES, Chen Z, Berzins SP, Benoist C, Mathis D (2005) The cellular mechanism of Aire control of T-cell tolerance. Immunity 23(2):227–239
Awong G, Singh J, Mohtashami M, Malm M, La Motte-Mohs RN, Benveniste PM, Serra P, Herer E, van den Brink MR, Zuniga-Pflucker JC (2013) Human pro T-cells generated in vitro facilitate hematopoietic stem cell-derived T-lymphopoiesis in vivo and restore thymic architecture. Blood 122(26):4210–4219
Ballen KK, Spitzer TR, Yeap BY, McAfee S, Dey BR, Attar E, Haspel R, Kao G, Liney D, Alyea E, Lee S, Cutler C, Ho V, Soiffer R, Antin JH (2007) Double unrelated reduced-intensity umbilical cord blood transplantation in adults. Biol Blood Marrow Transplant 13(1):82–89
Ballen K, Mendizabal AM, Cutler C, Politikos I, Jamieson K, Shpall EJ, Dey BR, Attar E, McAfee S, Delaney C, McCarthy P, Ball ED, Kamble R, Avigan D, Maziarz RT, Ho VT, Koreth J, Alyea E, Soiffer R, Wingard JR, Boussiotis V, Spitzer TR, Antin JH (2012) Phase II trial of parathyroid hormone after double umbilical cord blood transplantation. Biol Blood Marrow Transplant 18(12):1851–1858
Barker JN, Martin PL, Coad JE, DeFor T, Trigg ME, Kurtzberg J, Weisdorf DJ, Wagner J (2001) Low incidence of Epstein-Barr virus-associated posttransplantation lymphoproliferative disorders in 272 unrelated-donor umbilical cord blood transplant recipients. Biol Blood Marrow Transplant 7(7):395–399
Barker JN, Hough RE, van Burik JA, DeFor TE, MacMillan ML, O'Brien MR, Wagner JE (2005a) Serious infections after unrelated donor transplantation in 136 children: impact of stem cell source. Biol Blood Marrow Transplant 11(5):362–370
Barker JN, Weisdorf DJ, DeFor TE, Blazar BR, McGlave PB, Miller JS, Verfaillie CM, Wagner JE (2005b) Transplantation of 2 partially HLA-matched umbilical cord blood units to enhance engraftment in adults with hematologic malignancy. Blood 105(3):1343–1347
Barker JN, Doubrovina E, Sauter C, Jaroscak JJ, Perales MA, Doubrovin M, Prockop SE, Koehne G, O'Reilly RJ (2010) Successful treatment of EBV-associated posttransplantation lymphoma after cord blood transplantation using third-party EBV-specific cytotoxic T lymphocytes. Blood 116(23):5045–5049
Bartelink IH, Belitser SV, Knibbe CA, Danhof M, de Pagter AJ, Egberts TC, Boelens JJ (2013) Immune reconstitution kinetics as an early predictor for mortality using various hematopoietic stem cell sources in children. Biol Blood Marrow Transplant 19(2):305–313
Beck JC, Wagner JE, DeFor TE, Brunstein CG, Schleiss MR, Young JA, Weisdorf DH, Cooley S, Miller JS, Verneris MR (2010) Impact of cytomegalovirus (CMV) reactivation after umbilical cord blood transplantation. Biol Blood Marrow Transplant 16(2):215–222
Berger M, Figari O, Bruno B, Raiola A, Dominietto A, Fiorone M, Podesta M, Tedone E, Pozzi S, Fagioli F, Madon E, Bacigalupo A (2008) Lymphocyte subsets recovery following allogeneic bone marrow transplantation (BMT): CD4+ cell count and transplant-related mortality. Bone Marrow Transplant 41(1):55–62
Berthou C, Legros-Maida S, Soulie A, Wargnier A, Guillet J, Rabian C, Gluckman E, Sasportes M (1995) Cord blood T lymphocytes lack constitutive perforin expression in contrast to adult peripheral blood T lymphocytes. Blood 85(6):1540–1546
Blaes AH, Cao Q, Wagner JE, Young JA, Weisdorf DJ, Brunstein CG (2010) Monitoring and preemptive rituximab therapy for Epstein-Barr virus reactivation after antithymocyte globulin containing nonmyeloablative conditioning for umbilical cord blood transplantation. Biol Blood Marrow Transplant 16(2):287–291
Bolotin E, Annett G, Parkman R, Weinberg K (1999) Serum levels of IL-7 in bone marrow transplant recipients: relationship to clinical characteristics and lymphocyte count. Bone Marrow Transplant 23(8):783–788
Brown JA, Stevenson K, Kim HT, Cutler C, Ballen K, McDonough S, Reynolds C, Herrera M, Liney D, Ho V, Kao G, Armand P, Koreth J, Alyea E, McAfee S, Attar E, Dey B, Spitzer T, Soiffer R, Ritz J, Antin JH, Boussiotis VA (2010) Clearance of CMV viremia and survival after double umbilical cord blood transplantation in adults depends on reconstitution of thymopoiesis. Blood 115(20):4111–4119
Brugman MH, Wiekmeijer AS, van Eggermond M, Wolvers-Tettero I, Langerak AW, de Haas EF, Bystrykh LV, van Rood JJ, de Haan G, Fibbe WE, Staal FJ (2015) Development of a diverse human T-cell repertoire despite stringent restriction of hematopoietic clonality in the thymus. Proc Natl Acad Sci USA 112(44):E6020–E6027
Brunstein CG, Weisdorf DJ, DeFor T, Barker JN, Tolar J, van Burik JA, Wagner JE (2006) Marked increased risk of Epstein-Barr virus-related complications with the addition of antithymocyte globulin to a nonmyeloablative conditioning prior to unrelated umbilical cord blood transplantation. Blood 108(8):2874–2880
Brunstein CG, Gutman JA, Weisdorf DJ, Woolfrey AE, Defor TE, Gooley TA, Verneris MR, Appelbaum FR, Wagner JE, Delaney C (2010) Allogeneic hematopoietic cell transplantation for hematologic malignancy: relative risks and benefits of double umbilical cord blood. Blood 116(22):4693–4699
Burke MJ, Vogel RI, Janardan SK, Brunstein C, Smith AR, Miller JS, Weisdorf D, Wagner JE, Verneris MR (2011) Early lymphocyte recovery and outcomes after umbilical cord blood transplantation (UCBT) for hematologic malignancies. Biol Blood Marrow Transplant 17(6):831–840
Castillo N, Garcia-Cadenas I, Diaz Heredia C, Martino R, Barba P, Ferra C, Canals C, Elorza I, Olive T, Badell I, Sierra J, Valcarcel D, Querol S (2016) Cord blood units with high CD3 cell counts predict early lymphocyte recovery after in vivo T-cell-depleted single cord blood transplantation. Biol Blood Marrow Transplant 22:1073–1079
Chalandon Y, Degermann S, Villard J, Arlettaz L, Kaiser L, Vischer S, Walter S, Heemskerk MH, van Lier RA, Helg C, Chapuis B, Roosnek E (2006) Pretransplantation CMV-specific T-cells protect recipients of T-cell-depleted grafts against CMV-related complications. Blood 107(1):389–396
Chalmers IM, Janossy G, Contreras M, Navarrete C (1998) Intracellular cytokine profile of cord and adult blood lymphocytes. Blood 92(1):11–18
Chang CC, Satwani P, Oberfield N, Vlad G, Simpson LL, Cairo MS (2005) Increased induction of allogeneic-specific cord blood CD4+CD25+ regulatory T (Treg) cells: a comparative study of naive and antigenic-specific cord blood Treg cells. Exp Hematol 33(12):1508–1520
Chao NJ, Liu CX, Rooney B, Chen BJ, Long GD, Vredenburgh JJ, Morris A, Gasparetto C, Rizzieri DA (2002) Nonmyeloablative regimen preserves “niches” allowing for peripheral expansion of donor T-cells. Biol Blood Marrow Transplant 8(5):249–256
Chen X, Barfield R, Benaim E, Leung W, Knowles J, Lawrence D, Otto M, Shurtleff SA, Neale GA, Behm FG, Turner V, Handgretinger R (2005) Prediction of T-cell reconstitution by assessment of T-cell receptor excision circle before allogeneic hematopoietic stem cell transplantation in pediatric patients. Blood 105(2):886–893
Cho BK, Rao VP, Ge Q, Eisen HN, Chen J (2000) Homeostasis-stimulated proliferation drives naive T-cells to differentiate directly into memory T-cells. J Exp Med 192(4):549–556
Chung B, Barbara-Burnham L, Barsky L, Weinberg K (2001) Radiosensitivity of thymic interleukin-7 production and thymopoiesis after bone marrow transplantation. Blood 98(5):1601–1606
Clave E, Rocha V, Talvensaari K, Busson M, Douay C, Appert ML, Rabian C, Carmagnat M, Garnier F, Filion A, Socie G, Gluckman E, Charron D, Toubert A (2005) Prognostic value of pretransplantation host thymic function in HLA-identical sibling hematopoietic stem cell transplantation. Blood 105(6):2608–2613
Clave E, Busson M, Douay C, Peffault de Latour R, Berrou J, Rabian C, Carmagnat M, Rocha V, Charron D, Socie G, Toubert A (2009) Acute graft-versus-host disease transiently impairs thymic output in young patients after allogeneic hematopoietic stem cell transplantation. Blood 113(25):6477–6484
Clave E, Lisini D, Douay C, Giorgiani G, Busson M, Zecca M, Moretta F, Acquafredda G, Brescia LP, Locatelli F, Toubert A (2013) Thymic function recovery after unrelated donor cord blood or T-cell depleted HLA-haploidentical stem cell transplantation correlates with leukemia relapse. Front Immunol 4:54
Cohen G, Carter SL, Weinberg KI, Masinsin B, Guinan E, Kurtzberg J, Wagner JE, Kernan NA, Parkman R (2006) Antigen-specific T-lymphocyte function after cord blood transplantation. Biol Blood Marrow Transplant 12(12):1335–1342
Crespo I, Paiva A, Couceiro A, Pimentel P, Orfao A, Regateiro F (2004) Immunophenotypic and functional characterization of cord blood dendritic cells. Stem Cells Dev 13(1):63–70
Cutler C, Stevenson K, Kim HT, Brown J, McDonough S, Herrera M, Reynolds C, Liney D, Kao G, Ho V, Armand P, Koreth J, Alyea E, Dey BR, Attar E, Spitzer T, Boussiotis VA, Ritz J, Soiffer R, Antin JH, Ballen K (2011) Double umbilical cord blood transplantation with reduced intensity conditioning and sirolimus-based GvHD prophylaxis. Bone Marrow Transplant 46(5):659–667
Cutler C, Multani P, Robbins D, Kim HT, Le T, Hoggatt J, Pelus LM, Desponts C, Chen YB, Rezner B, Armand P, Koreth J, Glotzbecker B, Ho VT, Alyea E, Isom M, Kao G, Armant M, Silberstein L, Hu P, Soiffer RJ, Scadden DT, Ritz J, Goessling W, North TE, Mendlein J, Ballen K, Zon LI, Antin JH, Shoemaker DD (2013) Prostaglandin-modulated umbilical cord blood hematopoietic stem cell transplantation. Blood 122(17):3074–3081
Dahi PB, Perales MA, Devlin SM, Olson A, Lubin M, Gonzales AM, Scaradavou A, Kernan NA, O’Reilly RJ, Giralt S, Jakubowski A, Koehne G, Papadopoulos EB, Ponce DM, Sauter C, Papanicolaou G, Barker JN (2015) Incidence, nature and mortality of cytomegalovirus infection after double-unit cord blood transplant. Leuk Lymphoma 56(6):1799–1805
De Smedt M, Reynvoet K, Kerre T, Taghon T, Verhasselt B, Vandekerckhove B, Leclercq G, Plum J (2002) Active form of Notch imposes T-cell fate in human progenitor cells. J Immunol 169(6):3021–3029
Dean RM, Fry T, Mackall C, Steinberg SM, Hakim F, Fowler D, Odom J, Foley J, Gress R, Bishop MR (2008) Association of serum interleukin-7 levels with the development of acute graft-versus-host disease. J Clin Oncol 26(35):5735–5741
Delaney C, Heimfeld S, Brashem-Stein C, Voorhies H, Manger RL, Bernstein ID (2010) Notch-mediated expansion of human cord blood progenitor cells capable of rapid myeloid reconstitution. Nat Med 16(2):232–236
Douek DC, McFarland RD, Keiser PH, Gage EA, Massey JM, Haynes BF, Polis MA, Haase AT, Feinberg MB, Sullivan JL, Jamieson BD, Zack JA, Picker LJ, Koup RA (1998) Changes in thymic function with age and during the treatment of HIV infection. Nature 396(6712):690–695
Douek DC, Vescio RA, Betts MR, Brenchley JM, Hill BJ, Zhang L, Berenson JR, Collins RH, Koup RA (2000) Assessment of thymic output in adults after haematopoietic stem-cell transplantation and prediction of T-cell reconstitution. Lancet 355(9218):1875–1881
Dudakov JA, Hanash AM, Jenq RR, Young LF, Ghosh A, Singer NV, West ML, Smith OM, Holland AM, Tsai JJ, Boyd RL, van den Brink MR (2012) Interleukin-22 drives endogenous thymic regeneration in mice. Science 336(6077):91–95
Dumas PY, Ruggeri A, Robin M, Crotta A, Abraham J, Forcade E, Bay JO, Michallet M, Bertrand Y, Socie G, Ionescu I, Gluckman E, Milpied N, Rocha V (2013) Incidence and risk factors of EBV reactivation after unrelated cord blood transplantation: a Eurocord and Societe Francaise de Greffe de Moelle-Therapie Cellulaire collaborative study. Bone Marrow Transplant 48(2):253–256
Dumont-Girard F, Roux E, van Lier RA, Hale G, Helg C, Chapuis B, Starobinski M, Roosnek E (1998) Reconstitution of the T-cell compartment after bone marrow transplantation: restoration of the repertoire by thymic emigrants. Blood 92(11):4464–4471
Durandy A, Thuillier L, Forveille M, Fischer A (1990) Phenotypic and functional characteristics of human newborns’ B lymphocytes. J Immunol 144(1):60–65
Encabo A, Solves P, Carbonell-Uberos F, Minana MD (2007) The functional immaturity of dendritic cells can be relevant to increased tolerance associated with cord blood transplantation. Transfusion 47(2):272–279
Eyrich M, Leiler C, Lang P, Schilbach K, Schumm M, Bader P, Greil J, Klingebiel T, Handgretinger R, Niethammer D, Schlegel PG (2003) A prospective comparison of immune reconstitution in pediatric recipients of positively selected CD34+ peripheral blood stem cells from unrelated donors vs recipients of unmanipulated bone marrow from related donors. Bone Marrow Transplant 32(4):379–390
Fry TJ, Christensen BL, Komschlies KL, Gress RE, Mackall CL (2001) Interleukin-7 restores immunity in athymic T-cell-depleted hosts. Blood 97(6):1525–1533
Fry TJ, Sinha M, Milliron M, Chu YW, Kapoor V, Gress RE, Thomas E, Mackall CL (2004) Flt3 ligand enhances thymic-dependent and thymic-independent immune reconstitution. Blood 104(9):2794–2800
Gaddy J, Broxmeyer HE (1997) Cord blood CD16+56- cells with low lytic activity are possible precursors of mature natural killer cells. Cell Immunol 180(2):132–142
Gaddy J, Risdon G, Broxmeyer HE (1995) Cord blood natural killer cells are functionally and phenotypically immature but readily respond to interleukin-2 and interleukin-12. J Interf Cytokine Res 15(6):527–536
Garderet L, Dulphy N, Douay C, Chalumeau N, Schaeffer V, Zilber MT, Lim A, Even J, Mooney N, Gelin C, Gluckman E, Charron D, Toubert A (1998) The umbilical cord blood alphabeta T-cell repertoire: characteristics of a polyclonal and naive but completely formed repertoire. Blood 91(1):340–346
Glowala-Kosinska M, Chwieduk A, Smagur A, Fidyk W, Najda J, Mitrus I, Giebel S (2016) Thymic activity and T-cell repertoire recovery after autologous hematopoietic stem cell transplantation preceded by myeloablative radiotherapy or chemotherapy. Biol Blood Marrow Transplant 22(5):834–842
Godfrey WR, Spoden DJ, Ge YG, Baker SR, Liu B, Levine BL, June CH, Blazar BR, Porter SB (2005) Cord blood CD4(+)CD25(+)-derived T regulatory cell lines express FoxP3 protein and manifest potent suppressor function. Blood 105(2):750–758
Goldberg GL, King CG, Nejat RA, Suh DY, Smith OM, Bretz JC, Samstein RM, Dudakov JA, Chidgey AP, Chen-Kiang S, Boyd RL, van den Brink MR (2009) Luteinizing hormone-releasing hormone enhances T-cell recovery following allogeneic bone marrow transplantation. J Immunol 182(9):5846–5854
Goldrath AW, Bevan MJ (1999) Low-affinity ligands for the TCR drive proliferation of mature CD8+ T-cells in lymphopenic hosts. Immunity 11(2):183–190
Hakim FT, Cepeda R, Kaimei S, Mackall CL, McAtee N, Zujewski J, Cowan K, Gress RE (1997) Constraints on CD4 recovery postchemotherapy in adults: thymic insufficiency and apoptotic decline of expanded peripheral CD4 cells. Blood 90(9):3789–3798
Hamza NS, Lisgaris M, Yadavalli G, Nadeau L, Fox R, Fu P, Lazarus HM, Koc ON, Salata RA, Laughlin MJ (2004) Kinetics of myeloid and lymphocyte recovery and infectious complications after unrelated umbilical cord blood versus HLA-matched unrelated donor allogeneic transplantation in adults. Br J Haematol 124(4):488–498
Hayward AR, Lawton AR (1977) Induction of plasma cell differentiation of human fetal lymphocytes: evidence for functional immaturity of T and B-cells. J Immunol 119(4):1213–1217
van Heijst JW, Ceberio I, Lipuma LB, Samilo DW, Wasilewski GD, Gonzales AM, Nieves JL, van den Brink MR, Perales MA, Pamer EG (2013) Quantitative assessment of T-cell repertoire recovery after hematopoietic stem cell transplantation. Nat Med 19(3):372–377
Hill JA, Koo S, Guzman Suarez BB, Ho VT, Cutler C, Koreth J, Armand P, Alyea EP 3rd, Baden LR, Antin JH, Soiffer RJ, Marty FM (2012) Cord-blood hematopoietic stem cell transplant confers an increased risk for human herpesvirus-6-associated acute limbic encephalitis: a cohort analysis. Biol Blood Marrow Transplant 18(11):1638–1648
Hill JA, Boeckh M, Leisenring WM, Xie H, Adler AL, Huang ML, Fann JR, Delaney C, Zerr DM (2015) Human herpesvirus 6B reactivation and delirium are frequent and associated events after cord blood transplantation. Bone Marrow Transplant 50(10):1348–1351
Hiwarkar P, Qasim W, Ricciardelli I, Gilmour K, Quezada S, Saudemont A, Amrolia P, Veys P (2015) Cord blood T-cells mediate enhanced antitumor effects compared with adult peripheral blood T-cells. Blood 126(26):2882–2891
Hunt DW, Huppertz HI, Jiang HJ, Petty RE (1994) Studies of human cord blood dendritic cells: evidence for functional immaturity. Blood 84(12):4333–4343
Jacobson CA, Turki AT, McDonough SM, Stevenson KE, Kim HT, Kao G, Herrera MI, Reynolds CG, Alyea EP, Ho VT, Koreth J, Armand P, Chen YB, Ballen K, Soiffer RJ, Antin JH, Cutler CS, Ritz J (2012) Immune reconstitution after double umbilical cord blood stem cell transplantation: comparison with unrelated peripheral blood stem cell transplantation. Biol Blood Marrow Transplant 18(4):565–574
Kadereit S, Mohammad SF, Miller RE, Woods KD, Listrom CD, McKinnon K, Alali A, Bos LS, Iacobucci ML, Sramkoski MR, Jacobberger JW, Laughlin MJ (1999) Reduced NFAT1 protein expression in human umbilical cord blood T lymphocytes. Blood 94(9):3101–3107
Kaminski BA, Kadereit S, Miller RE, Leahy P, Stein KR, Topa DA, Radivoyevitch T, Veigl ML, Laughlin MJ (2003) Reduced expression of NFAT-associated genes in UCB versus adult CD4+ T lymphocytes during primary stimulation. Blood 102(13):4608–4617
Kanda J, Chiou LW, Szabolcs P, Sempowski GD, Rizzieri DA, Long GD, Sullivan KM, Gasparetto C, Chute JP, Morris A, McPherson J, Hale J, Livingston JA, Broadwater G, Niedzwiecki D, Chao NJ, Horwitz ME (2012) Immune recovery in adult patients after myeloablative dual umbilical cord blood, matched sibling, and matched unrelated donor hematopoietic cell transplantation. Biol Blood Marrow Transplant 18(11):1664–1676.e1661
Kelly RM, Highfill SL, Panoskaltsis-Mortari A, Taylor PA, Boyd RL, Hollander GA, Blazar BR (2008) Keratinocyte growth factor and androgen blockade work in concert to protect against conditioning regimen-induced thymic epithelial damage and enhance T-cell reconstitution after murine bone marrow transplantation. Blood 111(12):5734–5744
Kessel A, Yehudai D, Peri R, Pavlotzky E, Bamberger E, Tov N, Toubi E (2006) Increased susceptibility of cord blood B lymphocytes to undergo spontaneous apoptosis. Clin Exp Immunol 145(3):563–570
Klein AK, Patel DD, Gooding ME, Sempowski GD, Chen BJ, Liu C, Kurtzberg J, Haynes BF, Chao NJ (2001) T-Cell recovery in adults and children following umbilical cord blood transplantation. Biol Blood Marrow Transplant 7(8):454–466
Komanduri KV, St John LS, de Lima M, McMannis J, Rosinski S, McNiece I, Bryan SG, Kaur I, Martin S, Wieder ED, Worth L, Cooper LJ, Petropoulos D, Molldrem JJ, Champlin RE, Shpall EJ (2007) Delayed immune reconstitution after cord blood transplantation is characterized by impaired thymopoiesis and late memory T-cell skewing. Blood 110(13):4543–4551
Krenger W, Hollander GA (2008) The immunopathology of thymic GvHD. Semin Immunopathol 30(4):439–456
Langrish CL, Buddle JC, Thrasher AJ, Goldblatt D (2002) Neonatal dendritic cells are intrinsically biased against Th-1 immune responses. Clin Exp Immunol 128(1):118–123
Laughlin MJ, Eapen M, Rubinstein P, Wagner JE, Zhang MJ, Champlin RE, Stevens C, Barker JN, Gale RP, Lazarus HM, Marks DI, van Rood JJ, Scaradavou A, Horowitz MM (2004) Outcomes after transplantation of cord blood or bone marrow from unrelated donors in adults with leukemia. N Engl J Med 351(22):2265–2275
Le Bourgeois A, Labopin M, Guillaume T, Delaunay J, Foucher Y, Tessoulin B, Malard F, Ayari S, Peterlin P, Derenne S, Herry P, Cesbron A, Gagne K, Lode L, Illiaquer M, Imbert-Marcille BM, Le Gouill S, Moreau P, Mohty M, Chevallier P (2014) Human herpesvirus 6 reactivation before engraftment is strongly predictive of graft failure after double umbilical cord blood allogeneic stem cell transplantation in adults. Exp Hematol 42(11):945–954
de Lima M, McNiece I, Robinson SN, Munsell M, Eapen M, Horowitz M, Alousi A, Saliba R, McMannis JD, Kaur I, Kebriaei P, Parmar S, Popat U, Hosing C, Champlin R, Bollard C, Molldrem JJ, Jones RB, Nieto Y, Andersson BS, Shah N, Oran B, Cooper LJ, Worth L, Qazilbash MH, Korbling M, Rondon G, Ciurea S, Bosque D, Maewal I, Simmons PJ, Shpall EJ (2012) Cord-blood engraftment with ex vivo mesenchymal-cell coculture. N Engl J Med 367(24):2305–2315
Lindemans CA, Chiesa R, Amrolia PJ, Rao K, Nikolajeva O, de Wildt A, Gerhardt CE, Gilmour KC, B Bierings M, Veys P, Boelens JJ (2014) Impact of thymoglobulin prior to pediatric unrelated umbilical cord blood transplantation on immune reconstitution and clinical outcome. Blood 123(1):126–132
Mackall CL, Granger L, Sheard MA, Cepeda R, Gress RE (1993) T-cell regeneration after bone marrow transplantation: differential CD45 isoform expression on thymic-derived versus thymic-independent progeny. Blood 82(8):2585–2594
Mackall CL, Fleisher TA, Brown MR, Andrich MP, Chen CC, Feuerstein IM, Horowitz ME, Magrath IT, Shad AT, Steinberg SM et al (1995) Age, thymopoiesis, and CD4+ T-lymphocyte regeneration after intensive chemotherapy. N Engl J Med 332(3):143–149
Mackall CL, Bare CV, Granger LA, Sharrow SO, Titus JA, Gress RE (1996) Thymic-independent T-cell regeneration occurs via antigen-driven expansion of peripheral T-cells resulting in a repertoire that is limited in diversity and prone to skewing. J Immunol 156(12):4609–4616
Mackall CL, Fry TJ, Bare C, Morgan P, Galbraith A, Gress RE (2001) IL-7 increases both thymic-dependent and thymic-independent T-cell regeneration after bone marrow transplantation. Blood 97(5):1491–1497
Matsumura T, Narimatsu H, Kami M, Yuji K, Kusumi E, Hori A, Murashige N, Tanaka Y, Masuoka K, Wake A, Miyakoshi S, Kanda Y, Taniguchi S (2007) Cytomegalovirus infections following umbilical cord blood transplantation using reduced intensity conditioning regimens for adult patients. Biol Blood Marrow Transplant 13(5):577–583
McFarland RD, Douek DC, Koup RA, Picker LJ (2000) Identification of a human recent thymic emigrant phenotype. Proc Natl Acad Sci U S A 97(8):4215–4220
McGoldrick SM, Bleakley ME, Guerrero A, Turtle CJ, Yamamoto TN, Pereira SE, Delaney CS, Riddell SR (2013) Cytomegalovirus-specific T-cells are primed early after cord blood transplant but fail to control virus in vivo. Blood 121(14):2796–2803
Mikulska M, Raiola AM, Bruzzi P, Varaldo R, Annunziata S, Lamparelli T, Frassoni F, Tedone E, Galano B, Bacigalupo A, Viscoli C (2012) CMV infection after transplant from cord blood compared to other alternative donors: the importance of donor-negative CMV serostatus. Biol Blood Marrow Transplant 18(1):92–99
Milano F, Pergam SA, Xie H, Leisenring WM, Gutman JA, Riffkin I, Chow V, Boeckh MJ, Delaney C (2011) Intensive strategy to prevent CMV disease in seropositive umbilical cord blood transplant recipients. Blood 118(20):5689–5696
Min D, Taylor PA, Panoskaltsis-Mortari A, Chung B, Danilenko DM, Farrell C, Lacey DL, Blazar BR, Weinberg KI (2002) Protection from thymic epithelial cell injury by keratinocyte growth factor: a new approach to improve thymic and peripheral T-cell reconstitution after bone marrow transplantation. Blood 99(12):4592–4600
Niehues T, Rocha V, Filipovich AH, Chan KW, Porcher R, Michel G, Ortega JJ, Wernet P, Gobel U, Gluckman E, Locatelli F (2001) Factors affecting lymphocyte subset reconstitution after either related or unrelated cord blood transplantation in children – a Eurocord analysis. Br J Haematol 114(1):42–48
Olson AL, Dahi PB, Zheng J, Devlin SM, Lubin M, Gonzales AM, Giralt SA, Perales MA, Papadopoulos EB, Ponce DM, Young JW, Kernan NA, Scaradavou A, O'Reilly RJ, Small TN, Papanicolaou G, Barker JN (2014) Frequent human herpesvirus-6 viremia but low incidence of encephalitis in double-unit cord blood recipients transplanted without antithymocyte globulin. Biol Blood Marrow Transplant 20(6):787–793
Papadopoulou A, Gerdemann U, Katari UL, Tzannou I, Liu H, Martinez C, Leung K, Carrum G, Gee AP, Vera JF, Krance RA, Brenner MK, Rooney CM, Heslop HE, Leen AM (2014) Activity of broad-spectrum T-cells as treatment for AdV, EBV, CMV, BKV, and HHV6 infections after HSCT. Sci Transl Med 6(242):242ra283
Parkman R, Cohen G, Carter SL, Weinberg KI, Masinsin B, Guinan E, Kurtzberg J, Wagner JE, Kernan NA (2006) Successful immune reconstitution decreases leukemic relapse and improves survival in recipients of unrelated cord blood transplantation. Biol Blood Marrow Transplant 12(9):919–927
Parody R, Martino R, Rovira M, Vazquez L, Vazquez MJ, de la Camara R, Blazquez C, Fernandez-Aviles F, Carreras E, Salavert M, Jarque I, Martin C, Martinez F, Lopez J, Torres A, Sierra J, Sanz GF (2006) Severe infections after unrelated donor allogeneic hematopoietic stem cell transplantation in adults: comparison of cord blood transplantation with peripheral blood and bone marrow transplantation. Biol Blood Marrow Transplant 12(7):734–748
Perales MA, Goldberg JD, Yuan J, Koehne G, Lechner L, Papadopoulos EB, Young JW, Jakubowski AA, Zaidi B, Gallardo H, Liu C, Rasalan T, Wolchok JD, Croughs T, Morre M, Devlin SM, van den Brink MR (2012) Recombinant human interleukin-7 (CYT107) promotes T-cell recovery after allogeneic stem cell transplantation. Blood 120(24):4882–4891
Politikos I, Boussiotis VA (2014) The role of the thymus in T-cell immune reconstitution after umbilical cord blood transplantation. Blood 124(22):3201–3211
Politikos I, Kim HT, Nikiforow S, Li L, Brown J, Antin JH, Cutler C, Ballen K, Ritz J, Boussiotis VA (2015) IL-7 and SCF levels inversely correlate with T-cell reconstitution and clinical outcomes after cord blood transplantation in adults. PLoS One 10(7):e0132564
Ponce DM, Zheng J, Gonzales AM, Lubin M, Heller G, Castro-Malaspina H, Giralt S, Hsu K, Jakubowski AA, Jenq RR, Koehne G, Papadopoulos EB, Perales MA, van den Brink MR, Young JW, Boulad F, Kernan NA, Kobos R, Prockop S, Scaradavou A, Small T, O'Reilly RJ, Barker JN (2011) Reduced late mortality risk contributes to similar survival after double-unit cord blood transplantation compared with related and unrelated donor hematopoietic stem cell transplantation. Biol Blood Marrow Transplant 17(9):1316–1326
Popat U, Mehta RS, Rezvani K, Fox P, Kondo K, Marin D, McNiece I, Oran B, Hosing C, Olson A, Parmar S, Shah N, Andreeff M, Kebriaei P, Kaur I, Yvon E, de Lima M, Cooper LJ, Tewari P, Champlin RE, Nieto Y, Andersson BS, Alousi A, Jones RB, Qazilbash MH, Bashir Q, Ciurea S, Ahmed S, Anderlini P, Bosque D, Bollard C, Molldrem JJ, Chen J, Rondon G, Thomas M, Miller L, Wolpe S, Simmons P, Robinson S, Zweidler-McKay PA, Shpall EJ (2015) Enforced fucosylation of cord blood hematopoietic cells accelerates neutrophil and platelet engraftment after transplantation. Blood 125(19):2885–2892
Risdon G, Gaddy J, Stehman FB, Broxmeyer HE (1994) Proliferative and cytotoxic responses of human cord blood T lymphocytes following allogeneic stimulation. Cell Immunol 154(1):14–24
Rizwan R, Levine JE, Defor T, Ferarra JL, Weisdorf DJ, Blazar BR, Verneris MR (2011) Peritransplant palifermin use and lymphocyte recovery after T-cell replete, matched related allogeneic hematopoietic cell transplantation. Am J Hematol 86(10):879–882
Robin M, Marque-Juillet S, Scieux C, Peffault de Latour R, Ferry C, Rocha V, Molina JM, Bergeron A, Devergie A, Gluckman E, Ribaud P, Socie G (2007) Disseminated adenovirus infections after allogeneic hematopoietic stem cell transplantation: incidence, risk factors and outcome. Haematologica 92(9):1254–1257
Robins HS, Campregher PV, Srivastava SK, Wacher A, Turtle CJ, Kahsai O, Riddell SR, Warren EH, Carlson CS (2009) Comprehensive assessment of T-cell receptor beta-chain diversity in alphabeta T-cells. Blood 114(19):4099–4107
Rocha V, Labopin M, Sanz G, Arcese W, Schwerdtfeger R, Bosi A, Jacobsen N, Ruutu T, de Lima M, Finke J, Frassoni F, Gluckman E (2004) Transplants of umbilical-cord blood or bone marrow from unrelated donors in adults with acute leukemia. N Engl J Med 351(22):2276–2285
Rodrigues CA, Sanz G, Brunstein CG, Sanz J, Wagner JE, Renaud M, de Lima M, Cairo MS, Furst S, Rio B, Dalley C, Carreras E, Harousseau JL, Mohty M, Taveira D, Dreger P, Sureda A, Gluckman E, Rocha V (2009) Analysis of risk factors for outcomes after unrelated cord blood transplantation in adults with lymphoid malignancies: a study by the Eurocord-Netcord and lymphoma working party of the European group for blood and marrow transplantation. J Clin Oncol 27(2):256–263
Rorije NM, Shea MM, Satyanarayana G, Hammond SP, Ho VT, Baden LR, Antin JH, Soiffer RJ, Marty FM (2014) BK virus disease after allogeneic stem cell transplantation: a cohort analysis. Biol Blood Marrow Transplant 20(4):564–570
Roux E, Helg C, Dumont-Girard F, Chapuis B, Jeannet M, Roosnek E (1996) Analysis of T-cell repopulation after allogeneic bone marrow transplantation: significant differences between recipients of T-cell depleted and unmanipulated grafts. Blood 87(9):3984–3992
Roux E, Dumont-Girard F, Starobinski M, Siegrist CA, Helg C, Chapuis B, Roosnek E (2000) Recovery of immune reactivity after T-cell-depleted bone marrow transplantation depends on thymic activity. Blood 96(6):2299–2303
Rubinstein P, Carrier C, Scaradavou A, Kurtzberg J, Adamson J, Migliaccio AR, Berkowitz RL, Cabbad M, Dobrila NL, Taylor PE, Rosenfield RE, Stevens CE (1998) Outcomes among 562 recipients of placental-blood transplants from unrelated donors. N Engl J Med 339(22):1565–1577
Sairafi D, Mattsson J, Uhlin M, Uzunel M (2012) Thymic function after allogeneic stem cell transplantation is dependent on graft source and predictive of long term survival. Clin Immunol 142(3):343–350
Saliba RM, Rezvani K, Leen A, Jorgensen J, Shah N, Hosing C, Parmar S, Oran B, Olson A, Rondon G, Chen J, Martinez C, Hamdi A, Mehta RS, Chemaly RF, Saunders IM, Bollard CM, Shpall EJ (2015) General and virus-specific immune cell reconstitution after double cord blood transplantation. Biol Blood Marrow Transplant 21(7):1284–1290
Sato K, Nagayama H, Takahashi TA (1999) Aberrant CD3- and CD28-mediated signaling events in cord blood T-cells are associated with dysfunctional regulation of Fas ligand-mediated cytotoxicity. J Immunol 162(8):4464–4471
Satyanarayana G, Hammond SP, Broge TA Jr, Mackenzie MR, Viscidi R, Politikos I, Koralnik IJ, Cutler CS, Ballen K, Boussiotis V, Marty FM, Tan CS (2015) BK polyomavirus reactivation after reduced-intensity double umbilical cord blood cell transplantation. Transpl Immunol 32(2):116–120
Sauter C, Abboud M, Jia X, Heller G, Gonzales AM, Lubin M, Hawke R, Perales MA, van den Brink MR, Giralt S, Papanicolaou G, Scaradavou A, Small TN, Barker JN (2011) Serious infection risk and immune recovery after double-unit cord blood transplantation without antithymocyte globulin. Biol Blood Marrow Transplant 17(10):1460–1471
Scheurer ME, Pritchett JC, Amirian ES, Zemke NR, Lusso P, Ljungman P (2013) HHV-6 encephalitis in umbilical cord blood transplantation: a systematic review and meta-analysis. Bone Marrow Transplant 48(4):574–580
Servais S, Lengline E, Porcher R, Carmagnat M, Peffault de Latour R, Robin M, Sicre de Fontebrune F, Clave E, Maki G, Granier C, Xhaard A, Dhedin N, Molina JM, Toubert A, Moins-Teisserenc H, Socie G (2014) Long-term immune reconstitution and infection burden after mismatched hematopoietic stem cell transplantation. Biol Blood Marrow Transplant 20(4):507–517
Shedlock DJ, Shen H (2003) Requirement for CD4 T-cell help in generating functional CD8 T-cell memory. Science 300(5617):337–339
Silva Lde P, Patah PA, Saliba RM, Szewczyk NA, Gilman L, Neumann J, Han XY, Tarrand J, Ribeiro R, Gulbis A, Shpall EJ, Jones R, Popat U, Walker JA, Petropoulos D, Chiattone A, Stewart J, El-Zimaity M, Anderlini P, Giralt S, Champlin RE, de Lima M (2010) Hemorrhagic cystitis after allogeneic hematopoietic stem cell transplants is the complex result of BK virus infection, preparative regimen intensity and donor type. Haematologica 95(7):1183–1190
Storek J (2008) Immunological reconstitution after hematopoietic cell transplantation – its relation to the contents of the graft. Expert Opin Biol Ther 8(5):583–597
Sutherland JS, Spyroglou L, Muirhead JL, Heng TS, Prieto-Hinojosa A, Prince HM, Chidgey AP, Schwarer AP, Boyd RL (2008) Enhanced immune system regeneration in humans following allogeneic or autologous hematopoietic stem cell transplantation by temporary sex steroid blockade. Clin Cancer Res 14(4):1138–1149
Szabolcs P, Niedzwiecki D (2007) Immune reconstitution after unrelated cord blood transplantation. Cytotherapy 9(2):111–122
Szabolcs P, Park KD, Reese M, Marti L, Broadwater G, Kurtzberg J (2003) Coexistent naive phenotype and higher cycling rate of cord blood T-cells as compared to adult peripheral blood. Exp Hematol 31(8):708–714
Taghon T, Van de Walle I, De Smet G, De Smedt M, Leclercq G, Vandekerckhove B, Plum J (2009) Notch signaling is required for proliferation but not for differentiation at a well-defined beta-selection checkpoint during human T-cell development. Blood 113(14):3254–3263
Takahata Y, Nomura A, Takada H, Ohga S, Furuno K, Hikino S, Nakayama H, Sakaguchi S, Hara T (2004) CD25+CD4+ T-cells in human cord blood: an immunoregulatory subset with naive phenotype and specific expression of forkhead box p3 (Foxp3) gene. Exp Hematol 32(7):622–629
Takami A, Mochizuki K, Asakura H, Yamazaki H, Okumura H, Nakao S (2005) High incidence of cytomegalovirus reactivation in adult recipients of an unrelated cord blood transplant. Haematologica 90(9):1290–1292
Tanaka H, Kai S, Yamaguchi M, Misawa M, Fujimori Y, Yamamoto M, Hara H (2003) Analysis of natural killer (NK) cell activity and adhesion molecules on NK cells from umbilical cord blood. Eur J Haematol 71(1):29–38
Torelli GF, Maggio R, Peragine N, Chiaretti S, De Propris MS, Lucarelli B, Screnci M, Mascolo MG, Milano F, Iori AP, Girelli G, Guarini A, Foa R (2012) Functional analysis and gene expression profile of umbilical cord blood regulatory T-cells. Ann Hematol 91(2):155–161
Uhlin M, Sairafi D, Berglund S, Thunberg S, Gertow J, Ringden O, Uzunel M, Remberger M, Mattsson J (2012) Mesenchymal stem cells inhibit thymic reconstitution after allogeneic cord blood transplantation. Stem Cells Dev 21(9):1409–1417
Vandenbosch K, Ovetchkine P, Champagne MA, Haddad E, Alexandrov L, Duval M (2008) Varicella-zoster virus disease is more frequent after cord blood than after bone marrow transplantation. Biol Blood Marrow Transplant 14(8):867–871
Verneris MR, Miller JS (2009) The phenotypic and functional characteristics of umbilical cord blood and peripheral blood natural killer cells. Br J Haematol 147(2):185–191
Verneris MR, Brunstein CG, Barker J, MacMillan ML, DeFor T, McKenna DH, Burke MJ, Blazar BR, Miller JS, McGlave PB, Weisdorf DJ, Wagner JE (2009) Relapse risk after umbilical cord blood transplantation: enhanced graft-versus-leukemia effect in recipients of 2 units. Blood 114(19):4293–4299
Wagner JE Jr, Brunstein CG, Boitano AE, DeFor TE, McKenna D, Sumstad D, Blazar BR, Tolar J, Le C, Jones J, Cooke MP, Bleul CC (2016) Phase I/II trial of StemRegenin-1 expanded umbilical cord blood hematopoietic stem cells supports testing as a stand-alone graft. Cell Stem Cell 18(1):144–155
Wang Y, Xu H, Zheng X, Wei H, Sun R, Tian Z (2007) High expression of NKG2A/CD94 and low expression of granzyme B are associated with reduced cord blood NK cell activity. Cell Mol Immunol 4(5):377–382
Wang Y, Chen G, Qiao S, Ma X, Tang X, Sun A, Wu D (2011) Keratinocyte growth factor enhanced immune reconstitution in murine allogeneic umbilical cord blood cell transplant. Leuk Lymphoma 52(8):1556–1566
Weinberg K, Blazar BR, Wagner JE, Agura E, Hill BJ, Smogorzewska M, Koup RA, Betts MR, Collins RH, Douek DC (2001) Factors affecting thymic function after allogeneic hematopoietic stem cell transplantation. Blood 97(5):1458–1466
Williams KM, Hakim FT, Gress RE (2007) T-cell immune reconstitution following lymphodepletion. Semin Immunol 19(5):318–330
Wils EJ, van der Holt B, Broers AE, Posthumus-van Sluijs SJ, Gratama JW, Braakman E, Cornelissen JJ (2011) Insufficient recovery of thymopoiesis predicts for opportunistic infections in allogeneic hematopoietic stem cell transplant recipients. Haematologica 96(12):1846–1854
Wils EJ, Aerts-Kaya FS, Rombouts EJ, van Mourik I, Rijken-Schelen A, Visser TP, Braakman E, Wagemaker G, Cornelissen JJ (2012) Keratinocyte growth factor and stem cell factor to improve thymopoiesis after autologous CD34+ cell transplantation in rhesus macaques. Biol Blood Marrow Transplant 18(1):55–65
Wing K, Lindgren S, Kollberg G, Lundgren A, Harris RA, Rudin A, Lundin S, Suri-Payer E (2003) CD4 T-cell activation by myelin oligodendrocyte glycoprotein is suppressed by adult but not cord blood CD25+ T-cells. Eur J Immunol 33(3):579–587
Wong OH, Huang FP, Chiang AK (2005) Differential responses of cord and adult blood-derived dendritic cells to dying cells. Immunology 116(1):13–20
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this chapter
Cite this chapter
Politikos, I., Boussiotis, V.A. (2017). Immune Reconstitution After Cord Blood Transplantation. In: Horwitz, M., Chao, N. (eds) Cord Blood Transplantations. Advances and Controversies in Hematopoietic Transplantation and Cell Therapy. Springer, Cham. https://doi.org/10.1007/978-3-319-53628-6_12
Download citation
DOI: https://doi.org/10.1007/978-3-319-53628-6_12
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-53627-9
Online ISBN: 978-3-319-53628-6
eBook Packages: MedicineMedicine (R0)