Abstract
Cognitive dysfunction syndrome (CDS) is a progressive, neurodegenerative disease of aged dogs and cats that manifests as behavioral changes, impaired learning and memory, awareness (response to stimuli), and confusion. CDS can severely impact animal welfare and the human-animal bond which may ultimately lead to shortened life span of the pet. Clinical signs in dogs and cats may include deficits in one or more categories. These categories represented by the acronym DISHAA include disorientation, alterations in social interactions, changes in sleep-wake cycles, loss of housetraining and other learned behaviors, altered activity levels (increased or decreased), and increased anxiety. Changes may also be seen with self-hygiene, appetite, and response to stimuli. CDS is diagnosed by exclusion of any medical and primary behavioral conditions, whose symptoms mimic that might be a cause of the signs. In addition, the presence of concurrent medical issues may confound a CDS diagnosis. Validated neuropsychological laboratory tests objectively quantify measures of learning and memory impairment that likely correspond to CDS signs. These tests provide a mechanism by which the effect of therapeutic agents can be assessed. However, as these tests require a trained personnel, standardized methodology, a cognitive assessment apparatus, and both time and consistency to assess the pet, they are a not a practical option in the clinical setting for family-owned pets. Although highly prevalent, signs of CDS are severely underreported to veterinarians by owners. Therefore, veterinarians must question owners proactively, obtain a thorough history, and screen for signs of CDS to ensure early identification which will then yield the greatest opportunity to treat early, slow decline, and improve CDS signs.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Cognitive dysfunction syndrome (CDS) is a progressive, neurodegenerative disease of aged dogs and cats that manifests as behavioral changes, impaired learning and memory, awareness (response to stimuli), and confusion. CDS can severely impact animal welfare and the human-animal bond which may ultimately lead to shortened life span of the pet. Clinical signs in dogs and cats may include deficits in one or more categories. These categories represented by the acronym DISHAA include disorientation, alterations in social interactions, changes in sleep-wake cycles, loss of housetraining and other learned behaviors, altered activity levels (increased or decreased), and increased anxiety. Changes may also be seen with self-hygiene, appetite, and response to stimuli. CDS is diagnosed by exclusion of any medical and primary behavioral conditions, whose symptoms mimic that might be a cause of the signs. In addition, the presence of concurrent medical issues may confound a CDS diagnosis. Validated neuropsychological laboratory tests objectively quantify measures of learning and memory impairment that likely correspond to CDS signs. These tests provide a mechanism by which the effect of therapeutic agents can be assessed. However, as these tests require a trained personnel, standardized methodology, a cognitive assessment apparatus, and both time and consistency to assess the pet, they are a not a practical option in the clinical setting for family-owned pets. Although highly prevalent, signs of CDS are severely underreported to veterinarians by owners. Therefore, veterinarians must question owners proactively, obtain a thorough history, and screen for signs of CDS to ensure early identification which will then yield the greatest opportunity to treat early, slow decline, and improve CDS signs.
1.1 Clinical Signs of Cognitive Dysfunction
Clinical signs of CDS have been described by the acronym DISH as a basis for screening and diagnosis. DISH refers to a disorientation, altered social interactions with people or other pets, altered sleep-wake cycles, and house soiling and loss of other learned behaviors (Azkona et al. 2009; Gonzalez-Martinez et al. 2011; Gunn-Moore et al. 2007; Madari et al. 2015; Landsberg et al. 2013; Landsberg et al. 2012; Osella et al. 2007; Rème et al. 2008; Neilson et al. 2001; Ruehl et al. 1995). Alternately, the use of the acronym DISHAA to include the categories of altered activity levels and increasing anxiety provides a more inclusive and potentially more sensitive screening questionnaire, based on studies that document alterations in these two clinical signs with increasing cognitive decline (Fast et al. 2013; Rosado et al. 2012). Other signs might include altered responsiveness to stimuli (i.e., exaggerated or reduced), altered interest in appetite or self-hygiene (i.e., increased or reduced), and altered control of feeding or drinking behaviors (Colle et al. 2000; Pugliese et al. 2005; Rofina et al. 2006) (Table 1.1).
Some dogs and cats might exhibit a single behavioral sign from one category, whereas others might exhibit multiple signs in a variety of categories. Similarly, there is a broad range in severity, including the number of presenting signs, number of affected categories, and intensity of signs that increases with advancing age (Azkona et al. 2009; Bain et al. 2001; Fast et al. 2013; Madari et al. 2015; Pugliese et al. 2005; Salvin et al. 2011a, b). In one study of dogs 8 years and older, signs that deteriorated most with age were activity and play levels, response to commands, and fears and phobias; however, for each of these signs underlying medical issues were a potential cause that had yet to be ruled out (Salvin et al. 2011a, b). In a study that examined the most common signs and their progression from non-affected to markedly affected, the most common signs in dogs with CDS were sleeping more during the day and restlessness at night (57%), altered social interactions (51%), disorientation (49%), and anxiety (46%). For dogs with mild cognitive dysfunction, the principal sign was increased daytime sleep (70%), with anxiety in 11%. In the non-CDS group, signs of anxiety were only reported in 4% of the dogs (Fast et al. 2013). In this study, the workup to rule out underlying medical causes was extensive including physical examination, blood, urine, and MRI where indicated. Madari and coworkers found that of the four categories of DISH, social interactions and sleep-wake cycles were most affected. In dogs with the most severe impairment, 67% were impaired in all four domains, while in the dogs with moderate dysfunction, 67% were affected in two domains (primarily social interactions and sleep-wake cycles), while with mild dysfunction, owners seldom reported changes unless asked with social changes being most affected (Madari et al. 2015). Azkona et al. reported alterations in social interactions and house training as the most commonly reported signs (Azkona et al. 2009). In another study, intermittent manifestations of anxiety were reported in 61% of dogs with CDS (Rème et al. 2008). In fact, because of their effects on the health and well-being of both the pet and the owner, signs of fear and anxiety may be among the most common owner-presented behavior complaints in senior pets (Landsberg et al. 2010, 2011, 2013). These signs may include noise sensitivity, fear of people, fear of other animals, fear of new places or objects, hyperattachment, separation anxiety, and difficulty adapting to change. In some cases, anxiety may appear to be “generalized” with signs that exhibit in a variety of situations.
Another recent study further supports that senior dogs are more sensitive to emotional distress. Aged dogs (>7 years old) showed greater separation distress than did adult dogs (<7 years old) when separated from their primary caregiver. Although aged dogs showed a more passive response in a stranger separation test (SST), the physiological stress response as measured by salivary cortisol levels was higher in aged dogs (Mongillo et al. 2013b). Thus, fear and anxiety in senior pets may be associated with more passive (introverted) signs that are more likely to go underreported and undiagnosed if owners are not effectively educated in identifying and reporting these signs.
Dogs and cats with cognitive decline may also display the onset or progression of aggressive behavior toward household pets or family members. Pets with CDS may become the target of aggression by another household pet. In addition to an increase in anxiety and irritability, decreased awareness, perhaps in combination with sensory decline, may cause the pet to stumble upon another dog/cat or approach them when in possession of valued resources and locations. As well, pets with CDS may have concurrent health issues including sensory decline and pain and may not respond appropriately to social cues or warning signs. Senior dogs with CDS or other medical problems may require more attention or altered housing and care to address their infirmities, further contributing to instability in the dynamic among household pets.
In cats, the predominant sign in 11–14-year-old cats was altered social interactions, while changes in activity including aimless activity and vocalization were most common in cats 15 and over (Gunn-Moore et al. 2007, Landsberg et al. 2010, 2011).
1.2 Prevalence of Behavior Signs in Senior Pets
Prevalence of behavior signs in senior pets falls into two categories. Behavioral signs with the highest level of owner reporting but lower prevalence are those that have the greatest impact on the health, behavior, and well-being of the pet and its owner. Behavioral signs with the highest prevalence but lowest owner reporting are those that are sufficiently subtle or mild that they go unnoticed or are of minimal concern to the pet owner.
-
(a)
Distribution of owner-reported behavior problems
In one study of 270 dogs over 7 years of age presented for behavior problems, 32% displayed aggression to family members, 16% aggression to family dogs, 9% barking, 8% separation anxiety, 6% disorientation and aggression toward unfamiliar people, 5% house soiling, 4% destructive and compulsive disorders, and 3% noise fears (Mariotti et al. 2009). Of 83 cats referred for behavioral consultations, most cats presented with marking or soiling (73%), followed by aggression (16%), vocalization (6%), and restlessness (6%) (Gunn-Moore et al. 2007). While CDS may be an underlying factor causing or contributing to many of these signs, other neurologic diseases, sensory impairment, endocrine and metabolic disorders, musculoskeletal disease, and other causes of pain must be ruled out.
-
(b)
Prevalence of cognitive dysfunction syndrome
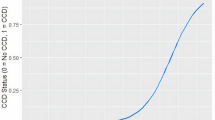
CDS is a highly prevalent yet grossly underreported condition of senior dogs and cats in which both prevalence and severity increase with age (Azkona et al. 2009; Bain et al. 2001; Gunn-Moore et al. 2007; Fast et al. 2013; Neilson et al. 2001; Madari et al. 2015, Salvin et al. 2010). While there is no cure, early detection and intervention may slow progression, prevent complications, and increase quality of life and life span.
Overall prevalence of CDS in dogs over 8 years of age has been reported to range from 14% to over 60% (Azkona et al. 2009; Neilson et al. 2001; Madari et al. 2015; Osella et al. 2007; Salvin et al. 2010). In a University of California, Davis, study of 180 owners of aged dogs, of those dogs 11–12 years of age, 28% were reported to have at least one category of DISHAA affected and 10% were positive for two or more categories, while in dogs 15–16 years old, 68% were positive for at least one category and 36% positive for two or more categories (Neilson et al. 2001). Twenty-two percent of dogs that did not have any signs developed signs 12–18 months later, while 48% of dogs with impairment in one category displayed impairment in two or more categories during this time period (Bain et al. 2001). Salvin and coworkers reported a prevalence of 5% in dogs 10–12 years of age, 23% aged 10–12, and 41% in dogs over 14 with an overall prevalence of 14.2% (Salvin et al. 2010). Katina et al. reported a prevalence of 13–16% for moderate to marked cognitive dysfunction in dogs aged 8–11 and 87%–100% in dogs > 13 (Katina et al. 2016). Madari et al. reported that of 300 dogs over 8 years of age, 159 of 215 dogs displayed signs of cognitive dysfunction after ruling out 85 dogs because of medical problems. Of these dogs, 42% with no impairment progressed to mild impairment, and 24% with mild impairment progressed to moderate over 6 months (Madari et al. 2015). After 1 year, 71.4% converted from none to mild impairment and 50% from moderate to severe (Madari et al. 2015). In yet another study in dogs over 8 years of age, over the course of approximately 3 years, 58% of those with no signs progressed to borderline CDS, and 11% of dogs moved from borderline to CDS (Fast et al. 2013). In a study of cats 11 years and older, 35% were diagnosed with CDS; this included 28% of 95 cats aged 11–15 years and 50% of 46 cats over 15 years of age (Gunn-Moore et al. 2007).
1.3 Pet Owner Reporting
As discussed, while many senior pets have signs of CDS, reporting is exceptionally low. In one study, 48% of pet owners reported at least one CDS sign in their senior dog 7 years of age or older, and only 17% of these owners informed their veterinarians (Proprietary market research 1999, Pfizer Animal Health). Another study found an estimated prevalence of 14.2% (68/479) in dogs greater than 8 years of age, but only 1.9% (9/479) of all dogs and 13% (9/68) of affected dogs had been diagnosed by a veterinarian previously. Madari et al. (2015) showed that pet owners did not usually report signs in dogs with mild cognitive impairment, until they were asked. Underreporting may be a result of owners who are unaware of the subtle signs or view them as untreatable, insignificant, or typical aspects of aging. Owners may not notify their veterinarians until signs advance to a point where they negatively impact the owner and it is evident that the pet is suffering. Therefore, to insure the earliest possible reporting of signs, veterinarians must be proactive in educating owners that any change in behavior or the emergence of new behavioral signs may be the earliest signs of medical conditions including pain, organ decline and dysfunction, endocrine disorders, and neurological conditions including CDS and that early diagnosis and treatment provide the greatest opportunity to improve signs, slow decline, and address pet welfare. In addition, to facilitate the earliest possible detection of CDS, veterinarians should consider the use of a broad-based screening questionnaire that includes all possible signs (Table 1.1) that can be provided to the client in advance of the visit or at the time of the visit.
1.4 Diagnosis
CDS, medical conditions and primary behavior problems must first be excluded (see Chap. 2). Neurological disease, sensory decline, musculoskeletal disease, and endocrine and metabolic disorders are the primary medical differentials (Gunn-Moore et al. 2007; Landsberg et al. 2010, 2011, 2012, 2013; Salvin et al. 2011a). While for most medical problems, concurrent medical signs or abnormal findings on physical and neurological examination and diagnostic tests are likely to be found, in some cases behavioral signs may be the first or only indication of an underlying health concern.
Since medical issues are common in the aged population and often coexist with CDS, this can be confounding. Medical issues, once diagnosed, may explain some behaviors, but concurrent CDS or other primary behavior problems may also contribute to a common sign. This necessitates continued investigation of primary behavior conditions other than those related to degenerative brain changes such as those that result from changes to the pet’s environment and household composition. As dogs with CDS are more sensitive and less able to adapt to change, this may exacerbate or contribute to these issues.
Senior pets should be examined twice a year, for optimal screening of both medical and behavioral health. As discussed above, in dogs over 8 years of age, new behavioral signs may arise, and existing signs are likely to progress over the course of 6–12 months (Bain et al. 2001; Gonzalez-Martinez et al. 2014; Fast et al. 2013; Madari et al. 2015; Salvin et al. 2011b;). In a study of dogs over 8 years of age, changes in frequency and severity of behavioral signs were seen over the course of 6 months in over half of the behavioral signs, with the oldest dogs >12 years generally showing the greatest deterioration and highest change in frequency. More than two-thirds of responses showed significant age-related deterioration over 6 months with the greatest effects on play, activity, response to commands, and fears and phobias. As this was an Internet-based survey, further medical workup was required to determine if underlying medical pathology or cognitive dysfunction was responsible for the increased severity and frequency of the behavioral signs (Salvin et al. 2010).
Once signs of CDS are identified, the diagnostic workup should include a thorough medical history including the use of cognitive screening questionnaire, complete physical and neurologic exam, and laboratory/diagnostic tests. Video footage of the behaviors can help to describe, characterize, and determine frequency and time of occurrence. This is particularly important for the diagnosis and treatment of separation anxiety, attention-seeking behavior, compulsive disorders, and behaviors that occur with no obvious environmental trigger.
A complete blood count, serum biochemistry profile, thyroid level, and urinalysis should be obtained as a minimum database. Further diagnostic tests including endocrine testing, radiographs, ultrasound, and advanced imaging may need to be considered depending upon presenting signs and physical examination findings. While an MRI may demonstrate a decrease in total brain volume and hippocampal volume, frontal lobe atrophy, temporal lobe atrophy, ventricular enlargement, an increase in lesions in the frontal cortex and caudate nucleus, a decline in regional cerebral blood volume, and a decrease in diameter of interthalamic adhesions that might be consistent with a diagnosis of CDS, it is primarily indicated for ruling out other intracranial pathology that may mimic CDS (Hasegawa et al. 2005; Su et al. 2005; Tapp et al. 2004, 2006).
In order to determine if there is a primary behavior issue, the clinician should ask questions about the onset of the problem, frequency, time of the day, duration, and any other changes in health or behavior as well as assess a video recording of the problem. Information about the characteristics of vocalizations may help to determine motivation.
For animals who demonstrate night waking, attempts should be made to identify triggers or a triggering event, whether there has been an increase in reactivity in the pet’s response to visual and audible stimuli and whether the pet has a chronic or more acute history of nocturnal signs. Evaluation of the pet’s daily schedule including level of exercise and enrichment may determine if daytime activity is decreased or altered or if the pet is sleeping more during the day. A prior association with a fear-evoking event such as fireworks or thunder could cause the pet to display signs of anxiety at night in association with these events despite the absence of an obvious trigger. There may also be different diagnostic considerations for pets that have difficulty falling asleep, restless sleep, or waking early. Human responses will further influence the behavior (e.g., pet is rewarded with food, attention, toys, or outdoor access).
To differentiate between medical, behavioral, and environmental causes for house soiling, the history should include information about preferred locations, substrate, frequency, pattern (e.g., indiscriminate or specific location), litter box cleaning, and possible stressors within the home. Household changes or events that possibly correlate with the onset of increasing fear or anxiety should be identified. In addition to neurological disease and CDS, health issues that impact pain, irritability, altered mobility, and sensory decline (e.g., vision, hearing) might alter behavior or social signaling leading to displays of fear and anxiety.
1.5 Senior Cognition and Decline in Learning and Memory
While learning and memory deficits are likely to be among the earliest indicators of the pathology of brain aging and associated cognitive decline, the use of screening questionnaires is unlikely to be sufficiently sensitive for early identification by the average pet owner (Landsberg et al. 2011, 2013; Salvin et al. 2011b). In fact, other than those few behaviors that have been trained on cue, learning their name and housetraining, there are few trained behaviors on which most pets can be effectively assessed, and a moderate to marked decline might be expected before these behaviors might be affected. While a decline in learning and performance might be recognized at an earlier stage in dogs that have been trained for more complex tasks such as in working dogs, service dogs, or those trained for agility, the increased level of enrichment that their work provides may improve cognitive function and slow the onset of cognitive decline.
1.6 Neuropsychological and Behavioral Assessment
While pet owners may not begin to report behavior changes associated with cognitive decline until 11 years or older, deficits in learning and memory tasks in dogs and cats and functional changes in the neurons of the caudate nucleus in cats leading to impaired information processing have been demonstrated as early as 6 years of age (Araujo et al. 2005; Cotman and Head 2008; Levine et al. 1987a; Levine et al. 1987a, b; Pan et al. 2013; Salvin et al. 2010; Studzinski et al. 2006). These deficits have been shown to correlate with alterations in activity, social interactions and exploration, disorientation, house soiling and other learned behaviors, and sleep disturbances (Colle et al. 2000; Milgram et al. 1994; Rofina et al. 2006; Rosado et al. 2012; Siwak et al. 2001, 2003; Tapp et al. 2003). In addition, these neuropsychological models provide a standardized and validated means of assessing the efficacy of therapeutic drugs, diets, and supplements to slow decline or improve performance on these tasks (Araujo et al. 2012; Araujo et al. 2011; Cotman and Head 2008; Head et al. 2009; Milgram et al. 1994; Pan et al. 2010, 2013; Studzinski et al. 2006; Tapp et al. 2003, 2004).
Using a standardized test apparatus, several cognitive domains can be independently evaluated for age-related cognitive deficits (Adams et al. 2000a; Head et al. 1995; Milgram et al. 1994; Studzinksi et al. 2006; Zanghi et al. 2015). These tests involve training dogs and cats to use visual and/or spatial information to solve different problems. In simple discrimination learning, the animal is presented with two different objects, one of which covers a food reward. The rate of learning of simple discrimination tasks does not differ from younger dogs and cats (Adams et al. 2000a; b; Landsberg et al. 2009; Tapp et al. 2003, 2004). In the reversal task, reward contingencies are reversed such that food is now hidden under the object that was not previously rewarded (Tapp et al. 2003, 2004). In contrast to simple learning tasks, older dogs and cats require significantly more trials to learn to alter their response in this task compared to young dogs and are not readily able to modify learned behaviors, indicating dysfunction of the prefrontal cortex (Milgram et al. 1994; Landsberg et al. 2009; Tapp et al. 2003, 2004; Zanghi et al. 2015). Other behaviors that might be associated with prefrontal cortex dysfunction might include changes in personality including fearfulness and aggression, stereotypic pacing or circling, and a loss of previously learned behaviors, e.g., house soiling.
The aging process has also been demonstrated to affect spatial memory, which is measured by the ability of dogs to remember where they had last obtained a food reward. In fact, the level at which performance declines on memory tasks (e.g., DNMP) might be categorized to correspond to the stages of Alzheimer’s disease (Adams et al. 2000a, b; Araujo et al. 2012; Head et al. 1995; Landsberg et al. 2009; McCune et al. 2008; Milgram et al. 1994; Pan et al. 2013; Studzinski et al. 2006; Zanghi et al. 2015). Clinically, this may present as wandering, getting lost, disorientation as well as disrupted sleep-wake cycles, and a decline in recognition of familiar people and animals.
Memory and spatial learning were also assessed in cats using a hole board task. Old cats (8–15) did not show differences in spatial learning compared to younger cats (<3 years old); however, memory errors were more abundant (McCune et al. 2008).
Adapting and validating these tasks for clinical use in pet dogs and cats are challenging as these tests are lengthy and complex and require trained personnel to administer (Gonzalez-Martinez et al. 2013; Heckler et al. 2014; Mongillo et al. 2013a; Nagasawa et al. 2012). However, one task, a food search test, may provide a methodology for pet owners to assess and track their pets in the home environment as it has been demonstrated to decline with age (>9 years) and with increasing cognitive dysfunction (but does not separate successful agers from those with cognitive dysfunction) (Gonzalez-Martinez et al. 2013).
Age-related behavioral differences have also been demonstrated in reactivity tests (Siwak et al. 2001, 2003; Rosado et al. 2012). The curiosity test assesses the dog’s reaction and attention to objects (toys) in an open field arena. In this test, young dogs show significantly more exploration and contact with novel objects than old dogs, while cognitively impaired aged dogs showed the least object contact (Siwak et al. 2001). Cognitively, impaired dogs also demonstrated higher levels of locomotion than their age-matched unimpaired peers, which may be linked to stereotypy or wandering behavior (Siwak et al. 2001; Rosado et al. 2012). Assessment of exploratory behavior might offer a more practical measure of cognitive dysfunction in aged pets.
1.7 Summary
Clinical signs of CDS in dogs and cats as defined by DISHAA have a significant impact on the lives of pets and their owners. Laboratory tests are available to assess multiple domains that correlate to decreased capacity of learning and memory, spatial abilities, attention, psychomotor ability, and executive function. Many of these tests may not be practical for clinical use. However, client education and increased awareness to improve reporting rates as well as careful screening by veterinarians will aid in the early identification of CDS-like signs that may warrant further diagnostics to rule out physical causes that mimic CDS. Although there is no cure, early identification and intervention are critical to reducing the rate of cognitive decline and can mitigate the risk of premature end of life decisions while improving the quality and longevity of the pet’s life.
References
Adams B, Chan A, Callahan H et al (2000a) Use of a delayed non-matching to position task to model age-dependent cognitive decline in the dog. Behav Brain Res 108(1):47–56
Adams B, Chan A, Callahan H, Milgram NW (2000b) The canine as a model of human cognitive aging: recent developments. Progr Neuro-Psychopharmacol Biol Psychiatry 24(5):675–692
Araujo JA, Studzinski CM, Head E, Cotman CW, Milgram NW (2005) Assessment of nutritional interventions for modification of age-associated cognitive decline using a canine model of human aging. Age 27(1):27–37
Araujo JA, Nobrega JN, Raymond R, Milgram NW (2011) Aged dogs demonstrate both increased sensitivity to scopolamine impairment and decreased muscarinic receptor density. Pharmacol Biochem Behav 98(2):203–209
Araujo JA, Faubert ML, Brooks ML, Landsberg GM, Lobprise H (2012) NOVIFIT®(NoviSAMe®) Tablets improve executive function in aged dogs and cats: implications for treatment of cognitive dysfunction syndrome. Int J Appl Res Veterinary Med 10(1):91–98
Azkona G, García-Belenguer S, Chacón G, Rosado B, León M, Palacio J (2009) Prevalence and risk factors of behavioural changes associated with age-related cognitive impairment in geriatric dogs. J Small Animal Practice 50(2):87–91
Bain MJ, Hart BL, Cliff KD, Ruehl WW (2001) Predicting behavioral changes associated with age-related cognitive impairment in dogs. J Am Veterinary Med Assoc 218(11):1792–1795
Colle MA, Hauw JJ, Crespeau F, Uchihara T, Akiyama H, Checler F et al (2000) Vascular and parenchymal Aβ deposition in the aging dog: correlation with behavior. Neurobiol Aging 21(5):695–704
Cotman CW, Head E (2008) The canine (dog) model of human aging and disease: dietary, environmental and immunotherapy approaches. J Alzheimer’s Dis 15(4):685–707
Fast R, Schütt T, Toft N, Møller A, Berendt M (2013) An observational study with long-term follow-up of canine cognitive dysfunction: clinical characteristics, survival, and risk factors. J Veterinary Intern Med 27(4):822–829
González-Martínez Á, Rosado B, Pesini P et al (2011) Plasma β-amyloid peptides in canine aging and cognitive dysfunction as a model of Alzheimer’s disease. Exp Gerontol 46(7):590–596
González-Martínez Á, Rosado B, Pesini P et al (2013) Effect of age and severity of cognitive dysfunction on two simple tasks in pet dogs. Veterinary J 198(1):176–181
Gonzalez-Martinez A, Rosado B, Pesini P et al (2014) Cognitive dysfunction syndrome progress in dogs: a 6 month long study. In: ESVCE/ECAWBM Proceedings, Avignon, France, pp 97–98
Gunn-Moore D, Moffat K, Christie LA, Head E (2007) Cognitive dysfunction and the neurobiology of ageing in cats. J Small Animal Practice 48(10):546–553
Hasegawa D, Yayoshi N, Fujita Y, Fujita M, Orima H (2005) Measurement of interthalamic adhesion thickness as a criteria for brain atrophy in dogs with and without cognitive dysfunction (dementia). Veterinary Radiol Ultrasound 46(6):452–457
Head E, Mehta R, Hartley J et al (1995) Spatial learning and memory as a function of age in the dog. Behavioral neuroscience 109(5):851–858
Head E, Nukala VN, Fenoglio KA, Muggenburg BA, Cotman CW, Sullivan PG (2009) Effects of age, dietary, and behavioral enrichment on brain mitochondria in a canine model of human aging. Exp Neurol 220(1):171–176
Heckler MC, Tranquilim MV, Svicero DJ, Barbosa L, Amorim RM (2014) Clinical feasibility of cognitive testing in dogs (Canis lupus familiaris). J Veterinary Behavior: Clin Appl Res 9(1):6–12
Katina S, Farbakova J, Madari A, Novak M, Zilka N (2016) Risk factors for canine cognitive dysfunction syndrome in Slovakia. Acta Veterinaria Scandinavica 58(1):1
Landsberg G, Araujo JA, de Rivera C et al (2009) Validation of a cognitive test battery in cats. Abstract. In: Heath S (ed). In: Proceedings of seventh international veterinary behaviour meeting. ESVCE, Belgium, pp. 142–145
Landsberg GM, Denenberg S, Araujo JA (2010) Cognitive dysfunction in cats: a syndrome we used to dismiss as ‘old age’. J Feline Med Surg 12(11):837–848
Landsberg GM, DePorter T, Araujo JA (2011) Clinical signs and management of anxiety, sleeplessness, and cognitive dysfunction in the senior pet. Veterinary Clin N Am: Small Animal Practice 41(3):565–590
Landsberg GM, Nichol J, Araujo JA (2012) Cognitive dysfunction syndrome: a disease of canine and feline brain aging. Veterinary Clin N Am: Small Animal Practice 42(4):749–768
Landsberg GM, Hunthausen W, Ackerman LA (2013) The effect of aging on behavior in senior pets. In: Behavior problems of the dog and cat, 3rd edn. Saunders, Edinburgh, pp 211–235
Levine MS, Lloyd RL, Hull CD, Fisher RS, Buchwald NA (1987a) Neurophysiological alterations in caudate neurons in aged cats. Brain Res 401(2):213–230
Levine MS, Lloyd RL, Fisher RS, Hull CD, Buchwald NA (1987b) Sensory, motor and cognitive alterations in aged cats. Neurobiol Aging 8(3):253–263
Madari A, Farbakova J, Katina S et al (2015) Assessment of severity and progression of canine cognitive dysfunction syndrome using the CAnine DEmentia Scale (CADES). Appl Animal Behav Sci 171:138–145
Mariotti VM, Landucci M, Lippi I et al (2009) Epidemiological study of behavioural disorders in elderly dogs. Abstract. In: Heath S (ed) Proceedings seventh international meeting of veterinary behaviour medicine, ESVCE, Belgium, pp 241–243
McCune S, Stevenson J, Fretwell L, Thompson A, Mills DS (2008) Ageing does not significantly affect performance in a spatial learning task in the domestic cat (Felis silvestris catus). Appl Animal Behav Sci 112(3):345–356
Milgram NW, Head E, Weiner E, Thomas E (1994) Cognitive functions and aging in the dog: acquisition of nonspatial visual tasks. Behav Neurosci 108(1):57–68
Mongillo P, Araujo JA, Pitteri E, Carnier P, Adamelli S, Regolin L, Marinelli L (2013a) Spatial reversal learning is impaired by age in pet dogs. Age 35(6):2273–2282
Mongillo P, Pitteri E, Carnier P, Gabai G, Adamelli S, Marinelli L (2013b) Does the attachment system towards owners change in aged dogs? Physiol Behav 120:64–69
Nagasawa M, Yatsuzuka A, Mogi K, Kikusui T (2012) A new behavioral test for detecting decline of age-related cognitive ability in dogs. J Veterinary Behav: Clin Appl Res 7(4):220–224
Neilson JC, Hart BL, Cliff KD, Ruehl WW (2001) Prevalence of behavioral changes associated with age-related cognitive impairment in dogs. J Am Veterinary Med Assoc 218(11):1787–1791
Osella MC, Re G, Odore R, Girardi C, Badino P, Barbero R, Bergamasco L (2007) Canine cognitive dysfunction syndrome: prevalence, clinical signs and treatment with a neuroprotective nutraceutical. Appl Animal Behav Sci 105(4):297–310
Pan Y, Araujo JA, Burrows J, de Rivera C, Gore A, Bhatnagar S, Milgram NW (2013) Cognitive enhancement in middle-aged and old cats with dietary supplementation with a nutrient blend containing fish oil, B vitamins, antioxidants and arginine. Br J Nutr 110(01):40–49
Pan Y, Larson B, Araujo JA et al (2010) Dietary supplementation with medium-chain TAG has long-lasting cognition-enhancing effects in aged dogs. Br J Nutr 103:1746–1754
Pugliese M, Carrasco JL, Andrade C, Mas E, Mascort J, Mahy N (2005) Severe cognitive impairment correlates with higher cerebrospinal fluid levels of lactate and pyruvate in a canine model of senile dementia. Progr Neuro-Psychopharmacol Biol Psychiatry 29(4):603–610
Rème CA, Dramard V, Kern L, Hofmans J, Halsberghe C, Mombiela DV (2008) Effect of S-adenosylmethionine tablets on the reduction of age-related mental decline in dogs: a double-blinded, placebo-controlled trial. Veterinary Therapeut: Res Appl Veterinary Med 9(2):69–82
Rofina JE, Van Ederen AM, Toussaint MJM et al (2006) Cognitive disturbances in old dogs suffering from the canine counterpart of Alzheimer’s disease. Brain Res 1069(1):216–226
Rosado B, González-Martínez Á, Pesini P et al (2012) Effect of age and severity of cognitive dysfunction on spontaneous activity in pet dogs—part 1: locomotor and exploratory behaviour. Veterinary J 194(2):189–195
Ruehl WW, Bruyette DS, DePaoli A, Cotman CW, Head E, Milgram NW, Cummings BJ (1995) Canine cognitive dysfunction as a model for human age-related cognitive decline, dementia and Alzheimer’s disease: clinical presentation, cognitive testing, pathology and response to 1-deprenyl therapy. Progr Brain Res 106:217–225
Salvin HE, McGreevy PD, Sachdev PS, Valenzuela MJ (2010) Under diagnosis of canine cognitive dysfunction: a cross-sectional survey of older companion dogs. Veterinary J 184(3):277–281
Salvin HE, McGreevy PD, Sachdev PS, Valenzuela MJ (2011a) Growing old gracefully—behavioral changes associated with “successful aging” in the dog, Canis familiaris. J Veterinary Behav: Clin Appl Res 6(6):313–320
Salvin HE, McGreevy PD, Sachdev PS, Valenzuela MJ (2011b) The canine cognitive dysfunction rating scale (CCDR): a data-driven and ecologically relevant assessment tool. Veterinary J 188(3):331–336
Siwak CT, Tapp PD, Milgram NW (2001) Effect of age and level of cognitive function on spontaneous and exploratory behaviors in the beagle dog. Learn Memory 8(6):317–325
Siwak CT, Tapp PD, Zicker SC et al (2003) Locomotor activity rhythms in dogs vary with age and cognitive status. Behav Neurosci 117(4):813–824
Studzinski CM, Christie LA, Araujo JA, Burnham WM, Head E, Cotman CW, Milgram NW (2006) Visuospatial function in the beagle dog: an early marker of cognitive decline in a model of human aging and dementia. Neurobiol Learn Memory 86(2):197–204
Su MY, Tapp PD, Vu L et al (2005) A longitudinal study of brain morphometrics using serial magnetic resonance imaging analysis in a canine model of aging. Progr Neuro-Psychopharmacol Biol Psychiatry 29(3):389–397
Tapp PD, Siwak CT, Estrada J, Head E, Muggenburg BA, Cotman CW, Milgram NW (2003) Size and reversal learning in the beagle dog as a measure of executive function and inhibitory control in aging. Learn Memory 10(1):64–73
Tapp PD, Siwak CT, Gao FQ, Chiou JY, Black SE, Head E et al (2004) Frontal lobe volume, function, and β-amyloid pathology in a canine model of aging. J Neurosci 24(38):8205–8213
Tapp PD, Head K, Head E, Milgram NW, Muggenburg BA, Su MY (2006) Application of an automated voxel-based morphometry technique to assess regional gray and white matter brain atrophy in a canine model of aging. Neuroimage 29(1):234–244
Zanghi BM, Araujo J, Milgram NW (2015) Cognitive domains in the dog: independence of working memory from object learning, selective attention, and motor learning. Animal Cognit 18(3):789–800
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this chapter
Cite this chapter
Landsberg, G.M., Malamed, R. (2017). Clinical Picture of Canine and Feline Cognitive Impairment. In: Landsberg, G., Maďari, A., Žilka, N. (eds) Canine and Feline Dementia. Springer, Cham. https://doi.org/10.1007/978-3-319-53219-6_1
Download citation
DOI: https://doi.org/10.1007/978-3-319-53219-6_1
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-53218-9
Online ISBN: 978-3-319-53219-6
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)